Vitamin D deficiency is associated with higher hospitalisation risk from COVID-19: a retrospective case-control study
et al., Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgab439, Jun 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 80,670 people in the UK with vitamin D levels measured within the last 12 months, showing higher risk of hospitalization with low vitamin D levels.
This is the 73rd of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
risk of hospitalization, 71.6% lower, RR 0.28, p < 0.001, adjusted per study, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk, >25 nmol/L, control prevalence approximated with overall prevalence.
|
|
risk of hospitalization, 57.9% lower, RR 0.42, p < 0.001, adjusted per study, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk, >50 nmol/L, control prevalence approximated with overall prevalence.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Jude et al., 17 Jun 2021, retrospective, United Kingdom, peer-reviewed, 5 authors.
Vitamin D Deficiency Is Associated With Higher Hospitalization Risk From COVID-19: A Retrospective Case-control Study
The Journal of Clinical Endocrinology & Metabolism, doi:10.1210/clinem/dgab439
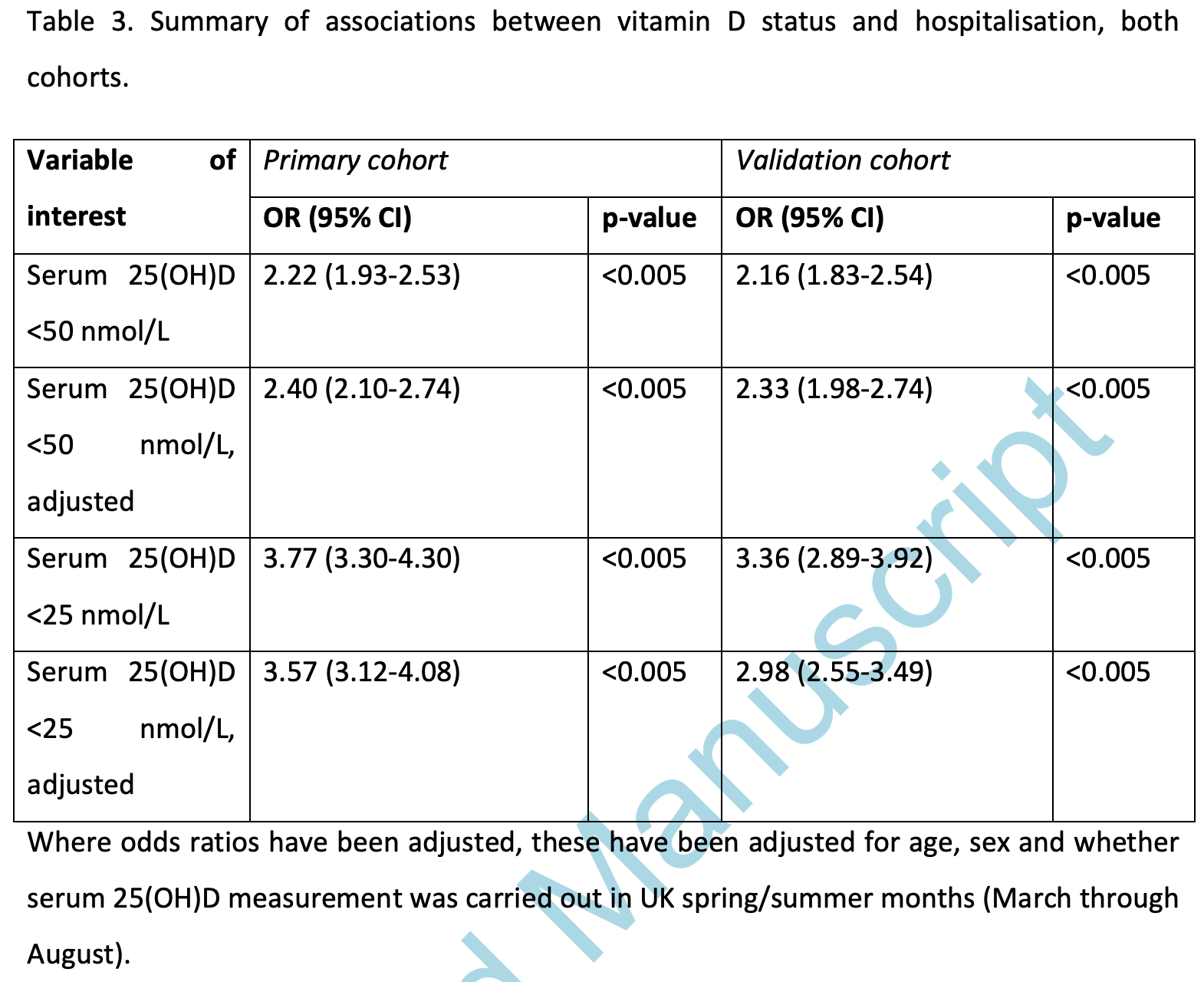
Context: One risk factor for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is postulated to be vitamin D deficiency. To better understand the role of vitamin D deficiency in the disease course of COVID-19, we undertook a retrospective case-control study in North West England. Objective: To examine whether hospitalization with COVID-19 is more prevalent in individuals with lower vitamin D levels. Methods: The study included individuals with test results for serum 25-hydroxyvitamin D (25[OH]D) between April 1, 2020, and January 29, 2021, from 2 districts in North West England. The last 25(OH)D level in the previous 12 months was categorized as "deficient" if less than 25 nmol/L and "insufficient" if 25 to 50 nmol/L. Results: The study included 80 670 participants. Of these, 1808 were admitted to the hospital with COVID-19, of whom 670 died. In a primary cohort, median serum 25(OH)D in nonhospitalized participants with COVID-19 was 50.0 nmol/L (interquartile range [IQR], 34.0-66.7) vs 35.0 nmol/L (IQR, 21.0-57.0) in those admitted with COVID-19 (P < 0.005). In a validation cohort, median serum 25(OH)D was 47.1 nmol/L (IQR, 31.8-64.7) in nonhospitalized vs 33.0 nmol/L (IQR, 19.4-54.1) in hospitalized patients. Age-, sex-, and season-adjusted odds ratios for hospital admission were 2.3 to 2.4 times higher among participants with serum 25(OH)D <50 nmol/L compared with those with normal serum 25(OH)D levels, without excess mortality risk.
Abbreviations: 25(OH)D, 25-hydroxyvitamin D; IQR, interquartile range.
Additional Information Correspondence: Professor Edward Jude, MD, DNB, MRCP, Tameside and Glossop Integrated Care NHS Foundation Trust, Fountain Street, Ashton-under-Lyne, OL6 9RW, UK. Email: Edward. jude@tgh.nhs.uk. Disclosures: None to declare in relation to this work. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed. Data Availability: Full data of this research work is available with the corresponding author and can be viewed by interested parties on request.
References
Aghili, Ebrahimpur, Arjmand, Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: a review and meta-analysis, Int J Obes (Lond)
Angelidi, Belanger, Lorinsky, Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients, Mayo Clin Proc, doi:10.1016/j.mayocp.2021.01.001
Baauw, Kist-Van Holthe, Slattery, Heymans, Chinapaw et al., Health needs of refugee children identified on arrival in reception countries: a systematic review and meta-analysis, BMJ Paediatr Open
Bilezikian, Bikle, Hewison, MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19, Eur J Endocrinol
Brandão, Chiamolera, Biscolla, No association between vitamin D status and COVID-19 infection in São Paulo, Brazil, Arch Endocrinol Metab, doi:10.20945/2359-3997000000343
Castillo, Costa, Barrios, Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J Steroid Biochem Mol Biol
Charoenngam, Shirvani, Reddy, Vodopivec, Apovian et al., Association of vitamin D status with hospital morbidity and mortality in adult hospitalized patients with COVID-19, Endocr Pract
Chen, Chen, Zhou, A risk score based on baseline risk factors for predicting mortality in COVID-19 patients, Curr Med Res Opin, doi:10.1080/03007995.2021.1904862
Clift, Coupland, Keogh, Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study, BMJ
D'avolio, Avataneo, Manca, 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients
Duarte, Carvalheiro, Rodrigues, Correction to: Prevalence of vitamin D deficiency and its predictors in the Portuguese population: a nationwide population-based study, Arch Osteoporos
Ferrari, Locatelli, Faraldi, Lombardi, Changes in 25-(OH) Vitamin D levels during the SARS-CoV-2 outbreak: lockdown-related effects and first-to-second wave difference-an observational study from Northern Italy, Biology
Gavioli, Miyashita, Hassaneen, Siau, An evaluation of serum 25-hydroxy Vitamin D levels in patients with COVID-19 in New York City, J Am Coll Nutr, doi:10.1080/07315724.2020.1869626
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr
Holick, Cancer, sunlight and vitamin D, J Clin Transl Endocrinol
Jain, Chaurasia, Sengar, Singh, Mahor et al., Analysis of vitamin D level among asymptomatic and critically e4715 ill COVID-19 patients and its correlation with inflammatory markers, Sci Rep
Jevalikar, Mithal, Singh, Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19, Sci Rep
Jolliffe, Camargo, Jr, Sluyter, Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials, Lancet Diabetes Endocrinol
Katz, Yue, Xue, Increased risk for COVID-19 in patients with vitamin D deficiency, Nutrition
Li, Cao, Yang, Zhang, Xu et al., Metabolic healthy obesity, vitamin D status, and risk of COVID-19, Aging Dis
Ling, Broad, Murphy, High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: a cross-sectional multi-centre observational study, Nutrients
Liu, Sun, Wang, Zhang, Zhao et al., Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta-analysis, Int J Infect Dis
Luo, Liao, Shen, Li, Cheng, Vitamin D deficiency is associated with COVID-19 incidence and disease severity in Chinese people
Ma, Zhou, Heianza, Qi, Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank, Am J Clin Nutr, doi:10.1093/ajcn/nqaa381
Manios, Moschonis, Lambrinou, A systematic review of vitamin D status in southern European countries, Eur J Nutr
Merzon, Tworowski, Gorohovski, Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, Febs J
Niculescu, Capatina, Dusceac, Caragheorgheopol, Ghemigian et al., Seasonal variation of serum vitamin D levels in Romania, Arch Osteoporos
Panagiotou, Tee, Ihsan, Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin Endocrinol (Oxf)
Pereira, Damascena, Azevedo, De Almeida Oliveira, Da et al., Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis, Crit Rev Food Sci Nutr, doi:10.1080/10408398.2020.1841090
Pham, Rahman, Majidi, Waterhouse, Neale, Acute respiratory tract infection and 25-Hydroxyvitamin D concentration: a systematic review and meta-analysis, Int J Environ Res Public Health
Pugach, Pugach, Strong correlation between prevalence of severe vitamin D deficiency and population mortality rate from COVID-19 in Europe, Wien Klin Wochenschr, doi:10.1007/s00508-021-01833-y
Smet, Smet, Herroelen, Gryspeerdt, Martens, Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality, Am J Clin Pathol
Sulli, Gotelli, Casabella, Vitamin D and lung outcomes in elderly COVID-19 patients, Nutrients
Yadav, Birdi, Tomo, Charan, Bhardwaj et al., Association of Vitamin D status with COVID-19 infection and mortality in the Asia Pacific region: a cross-sectional study, Indian J Clin Biochem, doi:10.1007/s12291-020-00950-1
Yisak, Ewunetei, Kefale, Effects of Vitamin D on COVID-19 infection and prognosis: a systematic review, Risk Manag Healthc Policy
Zhou, Luo, Qin, The association between vitamin D deficiency and community-acquired pneumonia: a metaanalysis of observational studies, Medicine
DOI record:
{
"DOI": "10.1210/clinem/dgab439",
"ISSN": [
"0021-972X",
"1945-7197"
],
"URL": "http://dx.doi.org/10.1210/clinem/dgab439",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:sec>\n <jats:title>Context</jats:title>\n <jats:p>One risk factor for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is postulated to be vitamin D deficiency. To better understand the role of vitamin D deficiency in the disease course of COVID-19, we undertook a retrospective case-control study in North West England.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Objective</jats:title>\n <jats:p>To examine whether hospitalization with COVID-19 is more prevalent in individuals with lower vitamin D levels.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>The study included individuals with test results for serum 25-hydroxyvitamin D (25[OH]D) between April 1, 2020, and January 29, 2021, from 2 districts in North West England. The last 25(OH)D level in the previous 12 months was categorized as “deficient” if less than 25 nmol/L and “insufficient” if 25 to 50 nmol/L.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>The study included 80 670 participants. Of these, 1808 were admitted to the hospital with COVID-19, of whom 670 died. In a primary cohort, median serum 25(OH)D in nonhospitalized participants with COVID-19 was 50.0 nmol/L (interquartile range [IQR], 34.0-66.7) vs 35.0 nmol/L (IQR, 21.0-57.0) in those admitted with COVID-19 (P &lt; 0.005). In a validation cohort, median serum 25(OH)D was 47.1 nmol/L (IQR, 31.8-64.7) in nonhospitalized vs 33.0 nmol/L (IQR, 19.4-54.1) in hospitalized patients. Age-, sex-, and season-adjusted odds ratios for hospital admission were 2.3 to 2.4 times higher among participants with serum 25(OH)D &lt;50 nmol/L compared with those with normal serum 25(OH)D levels, without excess mortality risk.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>Vitamin D deficiency is associated with higher risk of COVID-19 hospitalization. Widespread measurement of serum 25(OH)D and treatment of insufficiency or deficiency may reduce this risk.</jats:p>\n </jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-3186-4122",
"affiliation": [
{
"name": "Tameside and Glossop Integrated Care NHS Foundation Trust, Fountain Street, Ashton-under-Lyne, OL6 9RW, UK"
},
{
"name": "The University of Manchester, Oxford Road, Manchester, M13 9PL, UK"
},
{
"name": "Manchester Metropolitan University, All Saints Building, Manchester, M15 6BH, UK"
}
],
"authenticated-orcid": false,
"family": "Jude",
"given": "Edward B",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Tameside and Glossop Integrated Care NHS Foundation Trust, Fountain Street, Ashton-under-Lyne, OL6 9RW, UK"
},
{
"name": "The University of Manchester, Oxford Road, Manchester, M13 9PL, UK"
}
],
"family": "Ling",
"given": "Stephanie F",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Royal Preston Hospital, Lancashire Teaching Hospitals NHS Foundation Trust, Sharoe Green Lane, Fulwood, Preston, PR2 9HT, UK"
}
],
"family": "Allcock",
"given": "Rebecca",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "The University of Manchester, Oxford Road, Manchester, M13 9PL, UK"
}
],
"family": "Yeap",
"given": "Beverly X Y",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0886-5255",
"affiliation": [
{
"name": "The University of Manchester, Oxford Road, Manchester, M13 9PL, UK"
},
{
"name": "Manchester Metropolitan University, All Saints Building, Manchester, M15 6BH, UK"
},
{
"name": "Royal Preston Hospital, Lancashire Teaching Hospitals NHS Foundation Trust, Sharoe Green Lane, Fulwood, Preston, PR2 9HT, UK"
}
],
"authenticated-orcid": false,
"family": "Pappachan",
"given": "Joseph M",
"sequence": "additional"
}
],
"container-title": "The Journal of Clinical Endocrinology & Metabolism",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
6,
17
]
],
"date-time": "2021-06-17T23:19:01Z",
"timestamp": 1623971941000
},
"deposited": {
"date-parts": [
[
2021,
12,
1
]
],
"date-time": "2021-12-01T13:39:44Z",
"timestamp": 1638365984000
},
"indexed": {
"date-parts": [
[
2024,
4,
2
]
],
"date-time": "2024-04-02T14:17:55Z",
"timestamp": 1712067475311
},
"is-referenced-by-count": 35,
"issue": "11",
"issued": {
"date-parts": [
[
2021,
6,
17
]
]
},
"journal-issue": {
"issue": "11",
"published-online": {
"date-parts": [
[
2021,
6,
17
]
]
},
"published-print": {
"date-parts": [
[
2021,
10,
21
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://academic.oup.com/journals/pages/open_access/funder_policies/chorus/standard_publication_model",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
6,
17
]
],
"date-time": "2021-06-17T00:00:00Z",
"timestamp": 1623888000000
}
}
],
"link": [
{
"URL": "http://academic.oup.com/jcem/advance-article-pdf/doi/10.1210/clinem/dgab439/38997824/dgab439.pdf",
"content-type": "application/pdf",
"content-version": "am",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/jcem/article-pdf/106/11/e4708/41378499/dgab439.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://academic.oup.com/jcem/article-pdf/106/11/e4708/41378499/dgab439.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "80",
"original-title": [],
"page": "e4708-e4715",
"prefix": "10.1210",
"published": {
"date-parts": [
[
2021,
6,
17
]
]
},
"published-online": {
"date-parts": [
[
2021,
6,
17
]
]
},
"published-other": {
"date-parts": [
[
2021,
11,
1
]
]
},
"published-print": {
"date-parts": [
[
2021,
10,
21
]
]
},
"publisher": "The Endocrine Society",
"reference": [
{
"DOI": "10.1016/j.nut.2020.111106",
"article-title": "Increased risk for COVID-19 in patients with vitamin D deficiency",
"author": "Katz",
"doi-asserted-by": "crossref",
"first-page": "111106",
"journal-title": "Nutrition.",
"key": "2021120108533366700_CIT0001",
"volume": "84",
"year": "2021"
},
{
"DOI": "10.3390/nu12123799",
"article-title": "High-dose cholecalciferol booster therapy is associated with a reduced risk of mortality in patients with COVID-19: a cross-sectional multi-centre observational study",
"author": "Ling",
"doi-asserted-by": "crossref",
"first-page": "3799",
"issue": "12",
"journal-title": "Nutrients",
"key": "2021120108533366700_CIT0002",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-85809-y",
"article-title": "Lack of association of baseline 25-hydroxyvitamin D levels with disease severity and mortality in Indian patients hospitalized for COVID-19",
"author": "Jevalikar",
"doi-asserted-by": "crossref",
"first-page": "6258",
"issue": "1",
"journal-title": "Sci Rep.",
"key": "2021120108533366700_CIT0003",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3390/nu13030717",
"article-title": "Vitamin D and lung outcomes in elderly COVID-19 patients",
"author": "Sulli",
"doi-asserted-by": "crossref",
"first-page": "717",
"issue": "3",
"journal-title": "Nutrients",
"key": "2021120108533366700_CIT0004",
"volume": "13",
"year": "2021"
},
{
"article-title": "Strong correlation between prevalence of severe vitamin D deficiency and population mortality rate from COVID-19 in Europe",
"author": "Pugach",
"first-page": "1",
"journal-title": "Wien Klin Wochenschr.",
"key": "2021120108533366700_CIT0005",
"year": "2021"
},
{
"article-title": "Vitamin D status is associated with in-hospital mortality and mechanical ventilation: a cohort of COVID-19 hospitalized patients",
"author": "Angelidi",
"first-page": "S0025",
"journal-title": "Mayo Clin Proc.",
"key": "2021120108533366700_CIT0006",
"year": "2021"
},
{
"DOI": "10.1080/07315724.2020.1869626",
"article-title": "An evaluation of serum 25-hydroxy Vitamin D levels in patients with COVID-19 in New York City",
"author": "Gavioli",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "J Am Coll Nutr.",
"key": "2021120108533366700_CIT0007",
"year": "2021"
},
{
"article-title": "Association of Vitamin D status with COVID-19 infection and mortality in the Asia Pacific region: a cross-sectional study",
"author": "Yadav",
"first-page": "1",
"journal-title": "Indian J Clin Biochem.",
"key": "2021120108533366700_CIT0008",
"year": "2021"
},
{
"DOI": "10.14336/AD.2020.1108",
"article-title": "Metabolic healthy obesity, vitamin D status, and risk of COVID-19",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "61",
"issue": "1",
"journal-title": "Aging Dis.",
"key": "2021120108533366700_CIT0009",
"volume": "12",
"year": "2021"
},
{
"article-title": "Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank",
"author": "Ma",
"first-page": "nqaa381",
"journal-title": "Am J Clin Nutr.",
"key": "2021120108533366700_CIT0010",
"year": "2021"
},
{
"DOI": "10.2147/RMHP.S291584",
"article-title": "Effects of Vitamin D on COVID-19 infection and prognosis: a systematic review",
"author": "Yisak",
"doi-asserted-by": "crossref",
"first-page": "31",
"journal-title": "Risk Manag Healthc Policy.",
"key": "2021120108533366700_CIT0011",
"volume": "14",
"year": "2021"
},
{
"article-title": "Vitamin D deficiency aggravates COVID-19: systematic review and meta-analysis",
"author": "Pereira",
"first-page": "1",
"journal-title": "Crit Rev Food Sci Nutr.",
"key": "2021120108533366700_CIT0012",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.12.077",
"article-title": "Low vitamin D status is associated with coronavirus disease 2019 outcomes: a systematic review and meta-analysis",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "58",
"journal-title": "Int J Infect Dis.",
"key": "2021120108533366700_CIT0013",
"volume": "104",
"year": "2021"
},
{
"article-title": "Changes in 25-(OH) Vitamin D levels during the SARS-CoV-2 outbreak: lockdown-related effects and first-to-second wave difference-an observational study from Northern Italy",
"author": "Ferrari",
"first-page": "237",
"issue": "3",
"journal-title": "Biology (Basel).",
"key": "2021120108533366700_CIT0014",
"volume": "10",
"year": "2021"
},
{
"article-title": "No association between vitamin D status and COVID-19 infection in São Paulo, Brazil",
"author": "Brandão",
"first-page": "2359",
"journal-title": "Arch Endocrinol Metab.",
"key": "2021120108533366700_CIT0015",
"year": "2021"
},
{
"author": "National Institute for Health and Clinical Care Excellence (NICE).",
"key": "2021120108533366700_CIT0016"
},
{
"author": "Vitamin D External Quality Assessment Scheme",
"key": "2021120108533366700_CIT0017"
},
{
"author": "Randox Laboratories Ltd",
"key": "2021120108533366700_CIT0018"
},
{
"DOI": "10.1097/MD.0000000000017252",
"article-title": "The association between vitamin D deficiency and community-acquired pneumonia: a meta-analysis of observational studies",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "e17252",
"issue": "38",
"journal-title": "Medicine (Baltimore).",
"key": "2021120108533366700_CIT0019",
"volume": "98",
"year": "2019"
},
{
"DOI": "10.3390/ijerph16173020",
"article-title": "Acute respiratory tract infection and 25-Hydroxyvitamin D concentration: a systematic review and meta-analysis",
"author": "Pham",
"doi-asserted-by": "crossref",
"first-page": "3020",
"issue": "17",
"journal-title": "Int J Environ Res Public Health.",
"key": "2021120108533366700_CIT0020",
"volume": "16",
"year": "2019"
},
{
"DOI": "10.1111/cen.14276",
"article-title": "Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity",
"author": "Panagiotou",
"doi-asserted-by": "crossref",
"first-page": "508",
"issue": "4",
"journal-title": "Clin Endocrinol (Oxf).",
"key": "2021120108533366700_CIT0021",
"volume": "93",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"article-title": "Vitamin D concentrations and COVID-19 infection in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "crossref",
"first-page": "561",
"issue": "4",
"journal-title": "Diabetes Metab Syndr.",
"key": "2021120108533366700_CIT0022",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1038/s41598-020-77093-z",
"article-title": "Analysis of vitamin D level among asymptomatic and critically ill COVID-19 patients and its correlation with inflammatory markers",
"author": "Jain",
"doi-asserted-by": "crossref",
"first-page": "20191",
"issue": "1",
"journal-title": "Sci Rep.",
"key": "2021120108533366700_CIT0023",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"article-title": "Serum 25(OH)D level on hospital admission associated with COVID-19 stage and mortality",
"author": "De Smet",
"doi-asserted-by": "crossref",
"first-page": "381",
"issue": "3",
"journal-title": "Am J Clin Pathol.",
"key": "2021120108533366700_CIT0024",
"volume": "155",
"year": "2021"
},
{
"DOI": "10.3390/nu12051359",
"article-title": "25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2",
"author": "D’Avolio",
"doi-asserted-by": "crossref",
"first-page": "1359",
"issue": "5",
"journal-title": "Nutrients.",
"key": "2021120108533366700_CIT0025",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1111/febs.15495",
"article-title": "Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study",
"author": "Merzon",
"doi-asserted-by": "crossref",
"first-page": "3693",
"issue": "17",
"journal-title": "Febs J.",
"key": "2021120108533366700_CIT0026",
"volume": "287",
"year": "2020"
},
{
"DOI": "10.1093/jn/nxaa332",
"article-title": "Vitamin D deficiency is associated with COVID-19 incidence and disease severity in Chinese people [corrected]",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "98",
"issue": "1",
"journal-title": "J Nutr.",
"key": "2021120108533366700_CIT0027",
"volume": "151",
"year": "2021"
},
{
"article-title": "Cancer, sunlight and vitamin D",
"author": "Holick",
"first-page": "179",
"issue": "4",
"journal-title": "J Clin Transl Endocrinol.",
"key": "2021120108533366700_CIT0028",
"volume": "1",
"year": "2014"
},
{
"DOI": "10.1530/EJE-20-0665",
"article-title": "MECHANISMS IN ENDOCRINOLOGY: Vitamin D and COVID-19",
"author": "Bilezikian",
"doi-asserted-by": "crossref",
"first-page": "R133",
"issue": "5",
"journal-title": "Eur J Endocrinol.",
"key": "2021120108533366700_CIT0029",
"volume": "183",
"year": "2020"
},
{
"DOI": "10.1007/s11657-017-0407-3",
"article-title": "Seasonal variation of serum vitamin D levels in Romania",
"author": "Niculescu",
"doi-asserted-by": "crossref",
"first-page": "113",
"issue": "1",
"journal-title": "Arch Osteoporos.",
"key": "2021120108533366700_CIT0030",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.1007/s11657-020-00728-1",
"article-title": "Correction to: Prevalence of vitamin D deficiency and its predictors in the Portuguese population: a nationwide population-based study",
"author": "Duarte",
"doi-asserted-by": "crossref",
"first-page": "55",
"issue": "1",
"journal-title": "Arch Osteoporos.",
"key": "2021120108533366700_CIT0031",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1136/bmjpo-2019-000516",
"article-title": "Health needs of refugee children identified on arrival in reception countries: a systematic review and meta-analysis",
"author": "Baauw",
"doi-asserted-by": "crossref",
"first-page": "e000516",
"issue": "1",
"journal-title": "BMJ Paediatr Open.",
"key": "2021120108533366700_CIT0032",
"volume": "3",
"year": "2019"
},
{
"DOI": "10.1007/s00394-017-1564-2",
"article-title": "A systematic review of vitamin D status in southern European countries",
"author": "Manios",
"doi-asserted-by": "crossref",
"first-page": "2001",
"issue": "6",
"journal-title": "Eur J Nutr.",
"key": "2021120108533366700_CIT0033",
"volume": "57",
"year": "2018"
},
{
"DOI": "10.1016/S2213-8587(21)00051-6",
"article-title": "Vitamin D supplementation to prevent acute respiratory infections: a systematic review and meta-analysis of aggregate data from randomised controlled trials",
"author": "Jolliffe",
"doi-asserted-by": "crossref",
"first-page": "276",
"issue": "5",
"journal-title": "Lancet Diabetes Endocrinol.",
"key": "2021120108533366700_CIT0034",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"article-title": "“Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study”",
"author": "Entrenas Castillo",
"doi-asserted-by": "crossref",
"first-page": "105751",
"journal-title": "J Steroid Biochem Mol Biol.",
"key": "2021120108533366700_CIT0035",
"volume": "203",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m3731",
"article-title": "Living risk prediction algorithm (QCOVID) for risk of hospital admission and mortality from coronavirus 19 in adults: national derivation and validation cohort study",
"author": "Clift",
"doi-asserted-by": "crossref",
"first-page": "m3731",
"journal-title": "BMJ.",
"key": "2021120108533366700_CIT0036",
"volume": "371",
"year": "2020"
},
{
"article-title": "A risk score based on baseline risk factors for predicting mortality in COVID-19 patients",
"author": "Chen",
"first-page": "1",
"journal-title": "Curr Med Res Opin",
"key": "2021120108533366700_CIT0037",
"year": "2021"
},
{
"DOI": "10.1038/s41366-021-00776-8",
"article-title": "Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: a review and meta-analysis",
"author": "Aghili",
"doi-asserted-by": "crossref",
"first-page": "998",
"issue": "5",
"journal-title": "Int J Obes (Lond).",
"key": "2021120108533366700_CIT0038",
"volume": "45",
"year": "2021"
},
{
"DOI": "10.1016/j.eprac.2021.02.013",
"article-title": "Association of vitamin D status with hospital morbidity and mortality in adult hospitalized patients with COVID-19",
"author": "Charoenngam",
"doi-asserted-by": "crossref",
"first-page": "271",
"issue": "4",
"journal-title": "Endocr Pract.",
"key": "2021120108533366700_CIT0039",
"volume": "27",
"year": "2021"
}
],
"reference-count": 39,
"references-count": 39,
"relation": {},
"resource": {
"primary": {
"URL": "https://academic.oup.com/jcem/article/106/11/e4708/6303537"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Biochemistry (medical)",
"Clinical Biochemistry",
"Endocrinology",
"Biochemistry",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Vitamin D Deficiency Is Associated With Higher Hospitalization Risk From COVID-19: A Retrospective Case-control Study",
"type": "journal-article",
"volume": "106"
}
