When Mendelian randomisation fails
et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000265, Mar 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
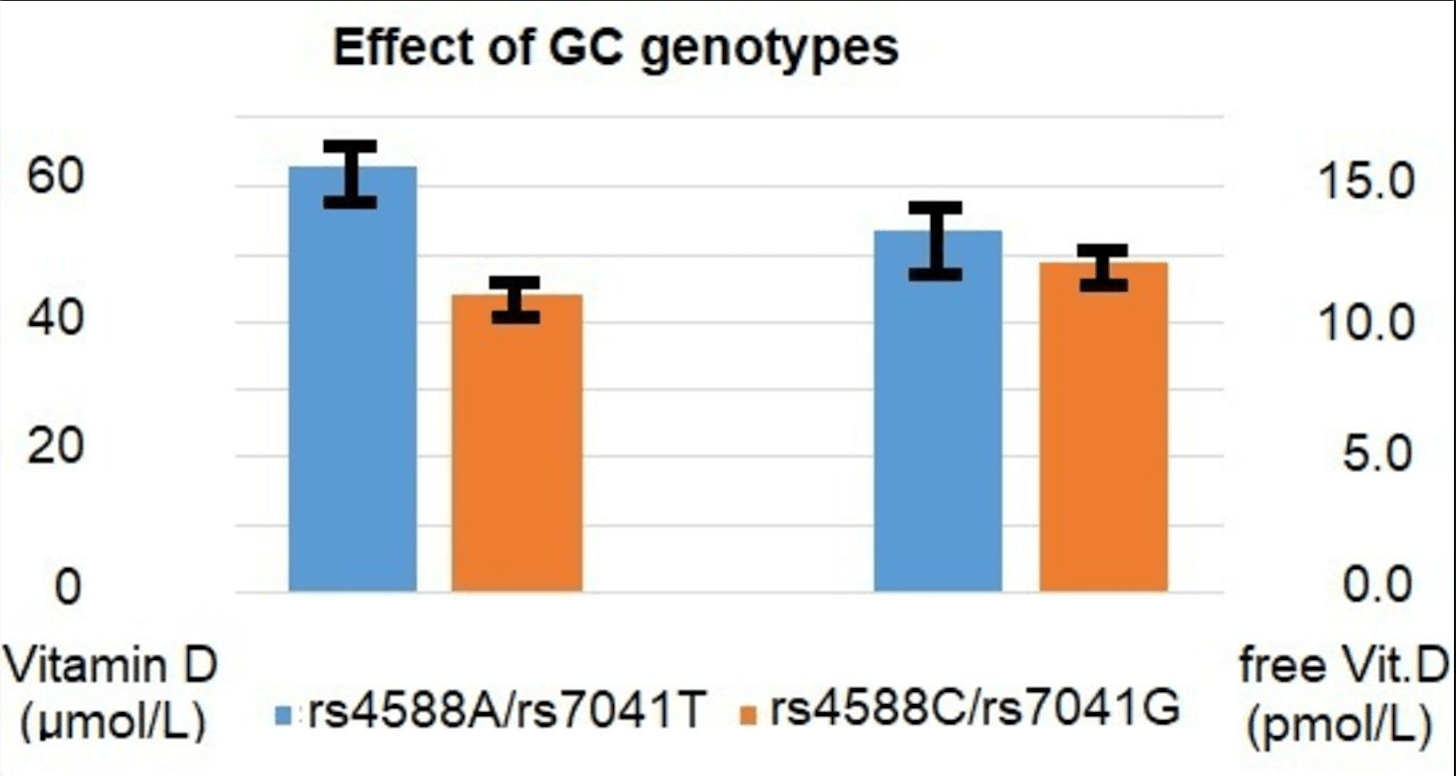
Analysis of why Mendelian randomization may fail in vitamin D studies. Authors suggest that it may come down to the use of 25(OH)D concentration in serum as a less than ideal proxy for vitamin D status of cells involved in the immune response. For most other purposes, it may not matter much that unbound (free) 25(OH)D is the better predictor of vitamin D deficiency and the resulting unfavourable outcomes. But for the MR analysis, the genetic instrument is strongly dominated by variation in the GC gene which modulates the concentration of vitamin D-binding protein (VDBP) in blood and thereby indirectly the concentrations of 25(OH)D and 1,25-dihydroxy vitamin D. Thus, the common GC alleles rs4588A and rs7041T are both associated with much lower than average vitamin D concentrations. In contrast, directly measured unbound (free) vitamin D concentrations are minimally affected by these alleles, if at all.
1.
Jaurrieta-Largo et al., A Machine Learning Approach to Understanding the Genetic Role in COVID-19 Prognosis: The Influence of Gene Polymorphisms Related to Inflammation, Vitamin D, and ACE2, International Journal of Molecular Sciences, doi:10.3390/ijms26167975.
2.
Al-Khrasani et al., Do vitamins halt the COVID-19-evoked pro-inflammatory cytokines involved in the development of neuropathic pain?, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2025.118346.
3.
Kow et al., Vitamin D and COVID‐19: How much more evidence do we need?, Nutrition in Clinical Practice, doi:10.1002/ncp.11349.
4.
Bigman et al., A Comprehensive Scoping Review on Diet and Nutrition in Relation to Long COVID-19 Symptoms and Recovery, Nutrients, doi:10.3390/nu17111802.
5.
Hewison, M., COVID-19 and our understanding of vitamin D and immune function, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2025.106710.
6.
Wimalawansa, S., Vitamin D Deficiency Meets Hill’s Criteria for Causation in SARS-CoV-2 Susceptibility, Complications, and Mortality: A Systematic Review, Nutrients, doi:10.3390/nu17030599.
7.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
8.
Fazli et al., Possible Link between Gut Microbiota, Diet, and COVID-19 Infection, Journal of Medical Bacteriology, 12:4, jmb.tums.ac.ir/index.php/jmb/article/view/525.
9.
Wojciulik et al., The impact of genetic polymorphism on course and severity of the SARS-CoV-2 infection and COVID-19 disease, Przeglad Epidemiologiczny, doi:10.32394/pe/194862.
10.
Wimalawansa (B), S., Unveiling the Interplay—Vitamin D and ACE-2 Molecular Interactions in Mitigating Complications and Deaths from SARS-CoV-2, Biology, doi:10.3390/biology13100831.
11.
Santa et al., Comparative analysis of COVID-19 responses in Japan and Africa: diet, phytochemicals, vitamin D, and gut microbiota in reducing mortality—A systematic review and meta-analysis, Frontiers in Nutrition, doi:10.3389/fnut.2024.1465324.
12.
Kaushal, A., Nutraceuticals and pharmacological to balance the transitional microbiome to extend immunity during COVID-19 and other viral infections, Journal of Translational Medicine, doi:10.1186/s12967-024-05587-9.
13.
Mu et al., Anti-inflammatory and Nutritional Interventions Against SARS-CoV-2: A Comprehensive Review, Journal of Agriculture and Food Research, doi:10.1016/j.jafr.2024.101422.
14.
Wimalawansa (C), S., Unlocking Insights: Navigating COVID-19 Challenges and Emulating Future Pandemic Resilience Strategies with Strengthening Natural Immunity, Heliyon, doi:10.1016/j.heliyon.2024.e34691.
15.
Imran et al., Therapeutic Role of Vitamin D in COVID-19 Patients, Clinical Nutrition Open Science, doi:10.1016/j.nutos.2024.07.004.
16.
Grant, W., Vitamin D and viral infections: Infectious diseases, autoimmune diseases, and cancers, Advances in Food and Nutrition Research, doi:10.1016/bs.afnr.2023.12.007.
17.
Polonowita et al., Molecular Quantum and Logic Process of Consciousness—Vitamin D Big-Data in COVID-19—A Case for Incorporating Machine Learning In Medicine, European Journal of Biomedical and Pharmaceutical sciences, doi:10.5281/zenodo.10435649.
18.
Gomaa et al., Pharmacological evaluation of vitamin D in COVID-19 and long COVID-19: recent studies confirm clinical validation and highlight metformin to improve VDR sensitivity and efficacy, Inflammopharmacology, doi:10.1007/s10787-023-01383-x.
19.
Gotelli et al., Understanding the immune-endocrine effects of vitamin D in SARS-CoV-2 infection: a role in protecting against neurodamage?, Neuroimmunomodulation, doi:10.1159/000533286.
20.
Cutolo et al., Involvement of the secosteroid vitamin D in autoimmune rheumatic diseases and COVID-19, Nature Reviews Rheumatology, doi:10.1038/s41584-023-00944-2.
21.
Schloss et al., Nutritional deficiencies that may predispose to long COVID, Inflammopharmacology, doi:10.1007/s10787-023-01183-3.
22.
Arora et al., Global Dietary and Herbal Supplement Use during COVID-19—A Scoping Review, Nutrients, doi:10.3390/nu15030771.
23.
Nicoll et al., COVID-19 Prevention: Vitamin D Is Still a Valid Remedy, Journal of Clinical Medicine, doi:10.3390/jcm11226818.
24.
Foshati et al., Antioxidants and clinical outcomes of patients with coronavirus disease 2019: A systematic review of observational and interventional studies, Food Science & Nutrition, doi:10.1002/fsn3.3034.
25.
Quesada-Gomez et al., Vitamin D Endocrine System and COVID-19: Treatment with Calcifediol, Nutrients, doi:10.3390/nu14132716.
26.
DiGuilio et al., Micronutrient Improvement of Epithelial Barrier Function in Various Disease States: A Case for Adjuvant Therapy, International Journal of Molecular Sciences, doi:10.3390/ijms23062995.
27.
Grant (B) et al., A Narrative Review of the Evidence for Variations in Serum 25-Hydroxyvitamin D Concentration Thresholds for Optimal Health, Nutrients, doi:10.3390/nu14030639.
28.
Shah Alam et al., The role of vitamin D in reducing SARS-CoV-2 infection: An update, International Immunopharmacology, doi:10.1016/j.intimp.2021.107686.
29.
Griffin et al., Perspective: Vitamin D supplementation prevents rickets and acute respiratory infections when given as daily maintenance but not as intermittent bolus: implications for COVID-19, Clinical Medicine, doi:10.7861/clinmed.2021-0035.
30.
Kohlmeier et al., When Mendelian randomisation fails, BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000265.
31.
Brenner, H., Vitamin D Supplementation to Prevent COVID-19 Infections and Deaths—Accumulating Evidence from Epidemiological and Intervention Studies Calls for Immediate Action, Nutrients, doi:10.3390/nu13020411.
32.
Mercola et al., Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity, Nutrients 2020, 12:11, 3361, doi:10.3390/nu12113361.
33.
Basha et al., Is the shielding effect of cholecalciferol in SARS CoV-2 infection dependable? An evidence based unraveling, Clinical Epidemiology and Global Health, doi:10.1016/j.cegh.2020.10.005.
34.
Xu et al., The importance of vitamin d metabolism as a potential prophylactic, immunoregulatory and neuroprotective treatment for COVID-19, Journal of Translational Medicine, doi:10.1186/s12967-020-02488-5.
35.
Alexander et al., Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19, Nutrients, doi:10.3390/nu12082358.
36.
Andrade et al., Vitamin A and D deficiencies in the prognosis of respiratory tract infections: A systematic review with perspectives for COVID-19 and a critical analysis on supplementation, SciELO preprints, doi:10.1590/SciELOPreprints.839.
37.
Grant (C) et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, 12:4, 988, doi:10.3390/nu12040988.
38.
McCullough et al., Daily oral dosing of vitamin D3 using 5000 TO 50,000 international units a day in long-term hospitalized patients: Insights from a seven year experience, The Journal of Steroid Biochemistry and Molecular Biology, doi:10.1016/j.jsbmb.2018.12.010.
39.
EFSA, Scientific Opinion on the substantiation of health claims related to vitamin D and normal function of the immune system and inflammatory response (ID 154, 159), maintenance of normal muscle function (ID 155) and maintenance of normal cardiovascular function (ID 159) pursuant to Article 13(1) of Regulation (E, EFSA Journal, doi:10.2903/j.efsa.2010.1468.
40.
EFSA (B), Scientific Opinion on the substantiation of a health claim related to vitamin D and contribution to the normal function of the immune system pursuant to Article 14 of Regulation (EC) No 1924/2006, EFSA Journal, doi:10.2903/j.efsa.2015.4096.
Kohlmeier et al., 22 Mar 2021, peer-reviewed, 2 authors.
When Mendelian randomisation fails
BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2021-000265
Mendelian randomisation (MR) is the ingenious approach of using the consistent long-term modulation of interesting exposure variables by inborn genetic differences to mimic the effect of different levels on outcomes of interest. This type of analysis is particularly important for evaluating the causal impact of nutritional exposures on longterm health outcomes. The MR approach is predicated on equivalent effects of exposure and genetic proxy on the outcome. But what happens when the proxy is not a good predictor of the outcome of interest? MR analysis of the hypothesised role of vitamin D in the pathology related to SARS-CoV-2 infection illustrates this conundrum. Up to this point, a growing number of observational studies appeared to link low 25-hydroxy vitamin D (25-OHD) concentrations to higher risk
Competing interests None declared. Patient consent for publication Not required.
References
Amin, Drenos, No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000151
Bikle, The free hormone hypothesis: when, why, and how to measure the free hormone levels to assess vitamin D, thyroid, sex hormone, and cortisol status, JBMR Plus, doi:10.1002/jbm4.10418
Butler-Laporte, Nakanishi, Mooser, Vitamin D and Covid-19 susceptibility and severity: a Mendelian randomization study, MedRxiv, doi:10.1101/2020.09.08.20190975
Calder, Nutrition, immunity and COVID-19, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000085
Castillo, Costa, Barrios, Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2020.105751
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection BMJ Nutrition, Prevention & Health in UK Biobank, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.050
Kaufman, Niles, Kroll, SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels, PLoS One, doi:10.1371/journal.pone.0239252
Kohlmeier, Avoidance of vitamin D deficiency to slow the COVID-19 pandemic, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000096
Lanham-New, Webb, Cashman, Vitamin D and SARS-CoV-2 virus/ COVID-19 disease, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000089
Louca, Murray, Klaser, Dietary supplements during the COVID-19 pandemic: insights from 445,850 users of the COVID symptom study APP, BMJ Nutr Prev Health
Ma, Zhou, Heianza, Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank, Am J Clin Nutr, doi:10.1093/ajcn/nqaa381
Meltzer, Best, Zhang, Association of vitamin D status and other clinical characteristics with COVID-19 test results, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.19722
Murai, Fernandes, Sales, Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial, JAMA, doi:10.1001/jama.2020.26848
Patchen, Clark, Hancock, Genetically predicted serum vitamin D and COVID-19: a Mendelian randomization study, BMJ Nutr Prev Health
Rastogi, Bhansali, Khare, Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled
Rhodes, Dunstan, Laird, COVID-19 mortality increases with northerly latitude after adjustment for age suggesting a link with ultraviolet and vitamin D, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000110
Smet, Smet, Herroelen, Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality, Am J Clin Pathol, doi:10.1093/ajcp/aqaa252
Sollid, Hutchinson, Berg, Effects of vitamin D binding protein phenotypes and vitamin D supplementation on serum total 25(OH)D and directly measured free 25(OH)D, Eur J Endocrinol, doi:10.1530/EJE-15-1089
Yisak, Ewunetei, Kefale, Effects of vitamin D on COVID-19 infection and prognosis: a systematic review, Risk Manag Healthc Policy, doi:10.2147/RMHP.S291584
DOI record:
{
"DOI": "10.1136/bmjnph-2021-000265",
"ISSN": [
"2516-5542"
],
"URL": "http://dx.doi.org/10.1136/bmjnph-2021-000265",
"alternative-id": [
"10.1136/bmjnph-2021-000265"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-1478-1744",
"affiliation": [],
"authenticated-orcid": false,
"family": "Kohlmeier",
"given": "Martin",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-6100-824X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Baah",
"given": "Emmanuel",
"sequence": "additional"
}
],
"container-title": "BMJ Nutrition, Prevention & Health",
"container-title-short": "BMJNPH",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
3,
22
]
],
"date-time": "2021-03-22T17:10:20Z",
"timestamp": 1616433020000
},
"deposited": {
"date-parts": [
[
2021,
7,
27
]
],
"date-time": "2021-07-27T21:06:50Z",
"timestamp": 1627420010000
},
"indexed": {
"date-parts": [
[
2023,
12,
29
]
],
"date-time": "2023-12-29T12:14:55Z",
"timestamp": 1703852095883
},
"is-referenced-by-count": 4,
"issue": "1",
"issued": {
"date-parts": [
[
2021,
3,
22
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2021,
6,
30
]
]
},
"published-print": {
"date-parts": [
[
2021,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
3,
22
]
],
"date-time": "2021-03-22T00:00:00Z",
"timestamp": 1616371200000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjnph-2021-000265",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "1-3",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
3,
22
]
]
},
"published-online": {
"date-parts": [
[
2021,
3,
22
]
]
},
"published-print": {
"date-parts": [
[
2021,
6
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.2147/RMHP.S291584",
"doi-asserted-by": "publisher",
"key": "2021072714055224000_4.1.1.1"
},
{
"DOI": "10.1371/journal.pone.0239252",
"doi-asserted-by": "publisher",
"key": "2021072714055224000_4.1.1.2"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"article-title": "Vitamin D concentrations and COVID-19 infection in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "crossref",
"first-page": "561",
"journal-title": "Diabetes Metab Syndr",
"key": "2021072714055224000_4.1.1.3",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1093/ajcp/aqaa252",
"article-title": "Serum 25(OH)D Level on Hospital Admission Associated With COVID-19 Stage and Mortality",
"author": "De Smet",
"doi-asserted-by": "crossref",
"first-page": "381",
"journal-title": "Am J Clin Pathol",
"key": "2021072714055224000_4.1.1.4",
"volume": "155",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2020.19722",
"article-title": "Association of vitamin D status and other clinical characteristics with COVID-19 test results",
"author": "Meltzer",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "2021072714055224000_4.1.1.5",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1093/ajcn/nqaa381",
"article-title": "Habitual use of vitamin D supplements and risk of coronavirus disease 2019 (COVID-19) infection: a prospective study in UK Biobank",
"author": "Ma",
"doi-asserted-by": "crossref",
"journal-title": "Am J Clin Nutr",
"key": "2021072714055224000_4.1.1.6",
"year": "2021"
},
{
"DOI": "10.1136/bmjnph-2021-000250",
"doi-asserted-by": "crossref",
"key": "2021072714055224000_4.1.1.7",
"unstructured": "Louca P , Murray B , Klaser K . Dietary supplements during the COVID-19 pandemic: insights from 445,850 users of the COVID symptom study APP. BMJ Nutr Prev Health 2021."
},
{
"DOI": "10.1016/j.jsbmb.2020.105751",
"doi-asserted-by": "publisher",
"key": "2021072714055224000_4.1.1.8"
},
{
"DOI": "10.1136/bmjnph-2020-000096",
"article-title": "Avoidance of vitamin D deficiency to slow the COVID-19 pandemic",
"author": "Kohlmeier",
"doi-asserted-by": "crossref",
"first-page": "67",
"journal-title": "BMJ Nutr Prev Health",
"key": "2021072714055224000_4.1.1.9",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1136/bmjnph-2020-000110",
"article-title": "COVID-19 mortality increases with northerly latitude after adjustment for age suggesting a link with ultraviolet and vitamin D",
"author": "Rhodes",
"doi-asserted-by": "crossref",
"first-page": "118",
"journal-title": "BMJ Nutr Prev Health",
"key": "2021072714055224000_4.1.1.10",
"volume": "3",
"year": "2020"
},
{
"article-title": "No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data",
"author": "Amin",
"first-page": "bmjnph-2020-000151",
"journal-title": "BMJ Nutr Prev Health",
"key": "2021072714055224000_4.1.1.11",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1101/2021.01.29.21250759",
"doi-asserted-by": "crossref",
"key": "2021072714055224000_4.1.1.12",
"unstructured": "Patchen BK , Clark AG , Hancock DB . Genetically predicted serum vitamin D and COVID-19: a Mendelian randomization study. BMJ Nutr Prev Health 2021."
},
{
"DOI": "10.1101/2020.09.08.20190975",
"doi-asserted-by": "crossref",
"key": "2021072714055224000_4.1.1.13",
"unstructured": "Butler-Laporte G , Nakanishi T , Mooser V . Vitamin D and Covid-19 susceptibility and severity: a Mendelian randomization study. MedRxiv 2020.doi:10.1101/2020.09.08.20190975"
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"article-title": "Nutrition, immunity and COVID-19",
"author": "Calder",
"doi-asserted-by": "crossref",
"first-page": "74",
"journal-title": "BMJ Nutr Prev Health",
"key": "2021072714055224000_4.1.1.14",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1530/EJE-15-1089",
"doi-asserted-by": "publisher",
"key": "2021072714055224000_4.1.1.15"
},
{
"DOI": "10.1002/jbm4.10418",
"article-title": "The free hormone hypothesis: when, why, and how to measure the free hormone levels to assess vitamin D, thyroid, sex hormone, and cortisol status",
"author": "Bikle",
"doi-asserted-by": "crossref",
"journal-title": "JBMR Plus",
"key": "2021072714055224000_4.1.1.16",
"volume": "5",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.26848",
"article-title": "Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial",
"author": "Murai",
"doi-asserted-by": "crossref",
"journal-title": "JAMA",
"key": "2021072714055224000_4.1.1.17",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1136/postgradmedj-2020-139065",
"article-title": "Short term, high-dose vitamin D supplementation for COVID-19 disease: a randomised, placebo-controlled, study (shade study)",
"author": "Rastogi",
"doi-asserted-by": "crossref",
"journal-title": "Postgrad Med J",
"key": "2021072714055224000_4.1.1.18",
"year": "2020"
},
{
"DOI": "10.1136/bmjnph-2020-000089",
"article-title": "Vitamin D and SARS-CoV-2 virus/COVID-19 disease",
"author": "Lanham-New",
"doi-asserted-by": "crossref",
"first-page": "106",
"journal-title": "BMJ Nutr Prev Health",
"key": "2021072714055224000_4.1.1.19",
"volume": "3",
"year": "2020"
}
],
"reference-count": 19,
"references-count": 19,
"relation": {},
"resource": {
"primary": {
"URL": "https://nutrition.bmj.com/lookup/doi/10.1136/bmjnph-2021-000265"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "When Mendelian randomisation fails",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "4"
}
