No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data
et al., BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2020-000151, Jan 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Analysis of vitamin D levels and COVID-19 cases and severity based on genetic predisposition to higher vitamin D levels or lower vitamin D deficiency, finding no significant association.
Mendelian randomization studies compare the estimated effect of SNPs
associated with variation in vitamin D levels on the health outcomes in large
numbers of patients. For more background on Mendelian randomization studies
and their limitations see1.
For reasons why Mendelian randomization may fail in this case,
see2.
Authors suggest that it may come down to the use of 25(OH)D concentration in
serum as a less than ideal proxy for vitamin D status of cells involved in the
immune response. For most other purposes, it may not matter much that unbound
(free) 25(OH)D is the better predictor of vitamin D deficiency and the
resulting unfavourable outcomes. But for the MR analysis, the genetic
instrument is strongly dominated by variation in the GC gene which modulates
the concentration of vitamin D-binding protein (VDBP) in blood and thereby
indirectly the concentrations of 25(OH)D and 1,25-dihydroxy vitamin D. Thus,
the common GC alleles rs4588A and rs7041T are both associated with much lower
than average vitamin D concentrations. In contrast, directly measured unbound
(free) vitamin D concentrations are minimally affected by these alleles, if at
all.
3 suggest that the primary reasons for Mendelien
randomization failure include that the total SNP-induced variation in 25(OH)D
has often been less than assay variance, and that genome-wide association
studies of SNP effects have been made on the full range of 25(OH)D levels,
while the data is non-linear with a significant percentage in the low and high
plateaus of the outcome relationships.
This is the 37th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments4.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
|
COVID-19 severity, 32.3% higher, RR 1.32, p = 0.20, high D levels 140,898, low D levels 35,079, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk, ≥50nmol/L vs. <25nmol/L, MR Egger, baseline risk approximated with overall risk.
|
|
risk of case, 7.6% higher, RR 1.08, p = 0.14, high D levels 140,898, low D levels 35,079, inverted to make RR<1 favor high D levels, odds ratio converted to relative risk, ≥50nmol/L vs. <25nmol/L, MR Egger, baseline risk approximated with overall risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Amin et al., 7 Jan 2021, retrospective, population-based cohort, United Kingdom, peer-reviewed, 2 authors.
No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data
BMJ Nutrition, Prevention & Health, doi:10.1136/bmjnph-2020-000151
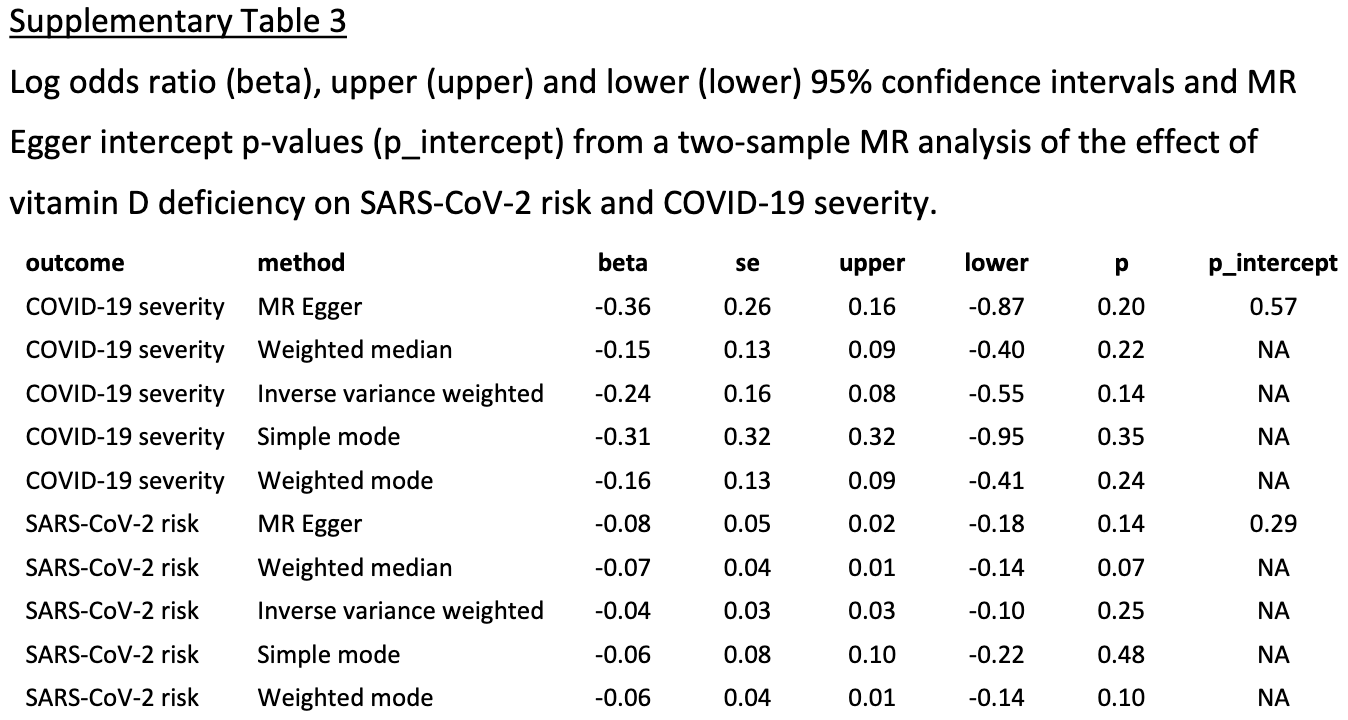
Background Upper respiratory tract infections are reportedly more frequent and more severe in individuals with lower vitamin D levels. Based on these findings, it has been suggested that vitamin D can prevent or reduce the severity of COVID-19. Methods We used two-sample Mendelian randomisation (MR) to assess the causal effect of vitamin D levels on SARS-CoV-2 infection risk and COVID-19 severity using publicly available data. We also carried out a genome-wide association analysis (GWA) of vitamin D deficiency in the UK Biobank (UKB) and used these results and two-sample MR to assess the causal effect of vitamin D deficiency on SARS-CoV-2 infection risk and COVID-19 severity. Results We found no evidence that vitamin D levels causally affect the risk of SARS-CoV-2 infection (ln(OR)=0.17 (95% CI −0.22 to 0.57, p=0.39)) nor did we find evidence that vitamin D levels causally affect COVID-19 severity (ln(OR)=0.36 (95% CI −0.89 to 1.61, p=0.57)). Based on our GWA analysis, we found that 17 independent variants are associated with vitamin D deficiency in the UKB. Using these variants as instruments for our two-sample MR analyses, we found no evidence that vitamin D deficiency causally affects the risk of SARS-CoV-2 infection (ln(OR)=−0.04 (95% CI −0.1 to 0.03, p=0.25)) nor did we find evidence that vitamin D deficiency causally affects COVID-19 severity (ln(OR)=−0.24 (95% CI −0.55 to 0.08, p=0.14)). Conclusions In conclusion, we found no evidence that vitamin D is protective against SARS-CoV-2 infection or COVID-19 severity. Our data support the recent statement by the National Institute for Health and Care Excellence that the use of vitamin D supplementation to mitigate COVID-19 is not supported by the available data.
What this paper adds ► Uncertainty remains over the use of Vitamin D for the prevention of COVID-19 and the moderation of its symptoms. ► Genetic predisposition for higher levels of vitamin D and for lower chance of vitamin D insufficiency do not have evidence of association with infection from SARS-CoV-2 or severity of COVID-19 following infection. ► Our work supports the current NICE statement that, based on the available evidence, vitamin D should not be considered as protective of infection from SARS-CoV-2 or a way to mitigate its severity.
Competing interests None declared. Patient consent for publication Not required. Provenance and peer review Not commissioned; externally peer reviewed by Dr Emmanuel Baah University of North Carolina System, USA. Data availability statement Data from the COVID-19 Host Genetics Initiative are available in a public, open access repository. UK Biobank data may be obtained from a third party and are not publicly available. The data from the COVID-19 Host Genetics Initiative that were used in this study are available here: https://www. covid19hg. org/ results/. UK Biobank data are available to all bona fide researchers for all types of health-related research which is in the public interest. Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Open access This is an open access article distributed in accordance with the Creative..
References
Allen, Sudlow, Downey, Uk Biobank: current status and what it means for epidemiology, Health Policy Technol, doi:10.1016/j.hlpt.2012.07.003
Angelantonio, Thompson, Kaptoge, Efficiency and safety of varying the frequency of whole blood donation (INTERVAL): a randomised trial of 45 000 donors, Lancet, doi:10.1016/S0140-6736(17)31928-1
Armstrong, Rudkin, Allen, Dynamic linkage of COVID-19 test results between public health England's second generation surveillance system and UK Biobank, Microb Genom, doi:10.1099/mgen.0.000397
Burgess, Davies, Thompson, Bias due to participant overlap in two-sample Mendelian randomization, Genet Epidemiol, doi:10.1002/gepi.21998
Bycroft, Freeman, Petkova, The UK Biobank resource with deep phenotyping and genomic data, Nature, doi:10.1038/s41586-018-0579-z
Cashman, Dowling, Škrabáková, Vitamin D deficiency in Europe: pandemic?, Am J Clin Nutr, doi:10.3945/ajcn.115.120873
Chakhtoura, Rahme, Chamoun, Vitamin D in the middle East and North Africa, Bone Rep, doi:10.1016/j.bonr.2018.03.004
Christakos, Dhawan, Verstuyf, Vitamin D: metabolism, molecular mechanism of action, and pleiotropic effects, Physiol Rev, doi:10.1152/physrev.00014.2015
Core, R: a language and environment for statistical computing
Craveiro, Cabral, Araújo, Association of serum 25-hydroxyvitamin D concentration with pulmonary function in young adults, Nutrients, doi:10.3390/nu10111728
D'avolio, Avataneo, Manca, 25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2, Nutrients, doi:10.3390/nu12051359
Davies, Holmes, Smith, Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians, BMJ, doi:10.1136/bmj.k601
Fasano, Cereda, Barichella, COVID-19 in Parkinson's disease patients living in Lombardy, Italy, Mov Disord, doi:10.1002/mds.28176
Finer, Martin, Khan, Cohort Profile: East London Genes & Health (ELGH), a community-based population genomics and health study in British Bangladeshi and British Pakistani people, Int J Epidemiol, doi:10.1093/ije/dyz174
Fraser, Milan, Vitamin D assays: past and present debates, difficulties, and developments, Calcif Tissue Int, doi:10.1007/s00223-012-9693-3
Fraser, Tang, Dutton, Vitamin D measurement, the debates continue, new analytes have emerged, developments have variable outcomes, Calcif Tissue Int, doi:10.1007/s00223-019-00620-2
Ginde, Mansbach, Camargo, Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the third National health and nutrition examination survey, Arch Intern Med, doi:10.1001/archinternmed.2008.560
Griffin, Wall, Blake, Vitamin D status of adults in the community, in outpatient clinics, in hospital, and in nursing homes in the West of Ireland, J Gerontol A Biol Sci Med Sci, doi:10.1093/gerona/glaa010
Hastie, Mackay, Ho, Vitamin D concentrations and COVID-19 infection in UK Biobank, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.050
Hemani, Zheng, Elsworth, The MR-Base platform supports systematic causal inference across the human phenome, Elife, doi:10.7554/eLife.34408
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin Exp Res, doi:10.1007/s40520-020-01570-8
Jiang, Reilly, Aschard, The COVID-19 host genetics initiative, a global initiative to elucidate the role of host genetic factors in susceptibility and severity of the SARS-CoV-2 virus pandemic, Eur J Hum Genet, doi:10.1038/s41431-020-0636-6
Karlson, Boutin, Hoffnagle, Building the partners healthcare Biobank at partners personalized medicine: informed consent, return of research results, recruitment lessons and operational considerations, J Pers Med, doi:10.3390/jpm6010002
Lam, Awasthi, Watson, RICOPILI: rapid imputation for COnsortias pipeline, Bioinformatics, doi:10.1093/bioinformatics/btz633
Lanham-New, Webb, Cashman, Vitamin D and SARS-CoV-2 virus/COVID-19 disease, BMJ Nutr Prev Health, doi:10.1136/bmjnph-2020-000089
Martineau, Jolliffe, Hooper, Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data, BMJ, doi:10.1136/bmj.i6583
Mogire, Mutua, Kimita, Prevalence of vitamin D deficiency in Africa: a systematic review and meta-analysis, Lancet Glob Health, doi:10.1016/S2214-109X(19)30457-7
Nice, Vitamin D deficiency in adults -treatment and prevention -NICE CKS
Palacios, Gonzalez, Is vitamin D deficiency a major global public health problem?, J Steroid Biochem Mol Biol, doi:10.1016/j.jsbmb.2013.11.003
Panagiotou, Contopoulos-Ioannidis, Ioannidis, Comparative effect sizes in randomised trials from less developed and more developed countries: a meta-epidemiological assessment, Lancet Glob Health, doi:10.1016/S2214-109X(15)70032-X
Purcell, Neale, Todd-Brown, PLINK: a tool set for wholegenome association and population-based linkage analyses, Am J Hum Genet, doi:10.1086/519795
Rhodes, Subramanian, Laird, Perspective: Vitamin D deficiency and COVID-19 severity -plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis, J Intern Med, doi:10.1111/joim.13149
Slob, Burgess, A comparison of robust Mendelian randomization methods using summary data, Genet Epidemiol, doi:10.1002/gepi.22295
Thanassoulis, Donnell, Mendelian randomization: nature's randomized trial in the post-genome era, JAMA, doi:10.1001/jama.2009.812
Turnbull, Scott, Thomas, The 100 000 Genomes Project: bringing whole genome sequencing to the NHS, BMJ, doi:10.1136/bmj.k1687
Willemsen, Vink, Abdellaoui, The adult Netherlands twin register: twenty-five years of survey and biological data collection, Twin Res Hum Genet, doi:10.1017/thg.2012.140
DOI record:
{
"DOI": "10.1136/bmjnph-2020-000151",
"ISSN": [
"2516-5542"
],
"URL": "http://dx.doi.org/10.1136/bmjnph-2020-000151",
"abstract": "<jats:sec><jats:title>Background</jats:title><jats:p>Upper respiratory tract infections are reportedly more frequent and more severe in individuals with lower vitamin D levels. Based on these findings, it has been suggested that vitamin D can prevent or reduce the severity of COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We used two-sample Mendelian randomisation (MR) to assess the causal effect of vitamin D levels on SARS-CoV-2 infection risk and COVID-19 severity using publicly available data. We also carried out a genome-wide association analysis (GWA) of vitamin D deficiency in the UK Biobank (UKB) and used these results and two-sample MR to assess the causal effect of vitamin D deficiency on SARS-CoV-2 infection risk and COVID-19 severity.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>We found no evidence that vitamin D levels causally affect the risk of SARS-CoV-2 infection (ln(OR)=0.17 (95% CI −0.22 to 0.57, p=0.39)) nor did we find evidence that vitamin D levels causally affect COVID-19 severity (ln(OR)=0.36 (95% CI −0.89 to 1.61, p=0.57)). Based on our GWA analysis, we found that 17 independent variants are associated with vitamin D deficiency in the UKB. Using these variants as instruments for our two-sample MR analyses, we found no evidence that vitamin D deficiency causally affects the risk of SARS-CoV-2 infection (ln(OR)=−0.04 (95% CI −0.1 to 0.03, p=0.25)) nor did we find evidence that vitamin D deficiency causally affects COVID-19 severity (ln(OR)=−0.24 (95% CI −0.55 to 0.08, p=0.14)).</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>In conclusion, we found no evidence that vitamin D is protective against SARS-CoV-2 infection or COVID-19 severity. Our data support the recent statement by the National Institute for Health and Care Excellence that the use of vitamin D supplementation to mitigate COVID-19 is not supported by the available data.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjnph-2020-000151"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-3054-838X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Amin",
"given": "Hasnat A",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0003-2469-5516",
"affiliation": [],
"authenticated-orcid": false,
"family": "Drenos",
"given": "Fotios",
"sequence": "additional"
}
],
"container-title": "BMJ Nutrition, Prevention & Health",
"container-title-short": "BMJNPH",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
1,
7
]
],
"date-time": "2021-01-07T17:40:08Z",
"timestamp": 1610041208000
},
"deposited": {
"date-parts": [
[
2021,
7,
27
]
],
"date-time": "2021-07-27T21:06:30Z",
"timestamp": 1627419990000
},
"funder": [
{
"DOI": "10.13039/501100007914",
"award": [
"11143103"
],
"doi-asserted-by": "publisher",
"name": "Brunel University London"
}
],
"indexed": {
"date-parts": [
[
2024,
4,
6
]
],
"date-time": "2024-04-06T07:11:27Z",
"timestamp": 1712387487086
},
"is-referenced-by-count": 30,
"issue": "1",
"issued": {
"date-parts": [
[
2021,
1,
7
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2021,
6,
30
]
]
},
"published-print": {
"date-parts": [
[
2021,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
1,
7
]
],
"date-time": "2021-01-07T00:00:00Z",
"timestamp": 1609977600000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjnph-2020-000151",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "42-48",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
1,
7
]
]
},
"published-online": {
"date-parts": [
[
2021,
1,
7
]
]
},
"published-print": {
"date-parts": [
[
2021,
6
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1152/physrev.00014.2015",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.1"
},
{
"DOI": "10.1007/s00223-012-9693-3",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.2"
},
{
"DOI": "10.3945/ajcn.115.120873",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.3"
},
{
"DOI": "10.1016/S2214-109X(19)30457-7",
"article-title": "Prevalence of vitamin D deficiency in Africa: a systematic review and meta-analysis",
"author": "Mogire",
"doi-asserted-by": "crossref",
"first-page": "e134",
"journal-title": "Lancet Glob Health",
"key": "2021072714054701000_4.1.42.4",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.jsbmb.2013.11.003",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.5"
},
{
"DOI": "10.1016/j.bonr.2018.03.004",
"article-title": "Vitamin D in the middle East and North Africa",
"author": "Chakhtoura",
"doi-asserted-by": "crossref",
"first-page": "135",
"journal-title": "Bone Rep",
"key": "2021072714054701000_4.1.42.6",
"volume": "8",
"year": "2018"
},
{
"key": "2021072714054701000_4.1.42.7",
"unstructured": "NICE . Vitamin D deficiency in adults - treatment and prevention - NICE CKS. Available: https://cks.nice.org.uk/vitamin-d-deficiency-in-adults-treatment-and-prevention#!topicSummary [Accessed 02 Aug 2020]."
},
{
"DOI": "10.3390/nu10111728",
"article-title": "Association of serum 25-hydroxyvitamin D concentration with pulmonary function in young adults",
"author": "Craveiro",
"doi-asserted-by": "crossref",
"journal-title": "Nutrients",
"key": "2021072714054701000_4.1.42.8",
"volume": "10",
"year": "2018"
},
{
"DOI": "10.1001/archinternmed.2008.560",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.9"
},
{
"DOI": "10.1136/bmj.i6583",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.10"
},
{
"DOI": "10.1016/S2214-109X(15)70032-X",
"article-title": "Comparative effect sizes in randomised trials from less developed and more developed countries: a meta-epidemiological assessment",
"author": "Panagiotou",
"doi-asserted-by": "crossref",
"first-page": "S10",
"journal-title": "Lancet Glob Health",
"key": "2021072714054701000_4.1.42.11",
"volume": "2",
"year": "2014"
},
{
"DOI": "10.1136/bmjnph-2020-000089",
"article-title": "Vitamin D and SARS-CoV-2 virus/COVID-19 disease",
"author": "Lanham-New",
"doi-asserted-by": "crossref",
"first-page": "106",
"journal-title": "BMJ Nutr Prev Health",
"key": "2021072714054701000_4.1.42.12",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"article-title": "The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality",
"author": "Ilie",
"doi-asserted-by": "crossref",
"first-page": "1195",
"journal-title": "Aging Clin Exp Res",
"key": "2021072714054701000_4.1.42.13",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.050",
"article-title": "Vitamin D concentrations and COVID-19 infection in UK Biobank",
"author": "Hastie",
"doi-asserted-by": "crossref",
"first-page": "561",
"journal-title": "Diabetes Metab Syndr",
"key": "2021072714054701000_4.1.42.14",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1002/mds.28176",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.15"
},
{
"article-title": "Perspective: Vitamin D deficiency and COVID-19 severity - plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2 and thrombosis",
"author": "Rhodes",
"journal-title": "J Intern Med",
"key": "2021072714054701000_4.1.42.16",
"year": "2020"
},
{
"article-title": "25-Hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2",
"author": "D'Avolio",
"journal-title": "Nutrients",
"key": "2021072714054701000_4.1.42.17",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1001/jama.2009.812",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.18"
},
{
"DOI": "10.1038/s41467-018-02974-x",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.19"
},
{
"DOI": "10.1038/s41431-020-0636-6",
"article-title": "The COVID-19 host genetics initiative, a global initiative to elucidate the role of host genetic factors in susceptibility and severity of the SARS-CoV-2 virus pandemic",
"doi-asserted-by": "crossref",
"first-page": "715",
"journal-title": "Eur J Hum Genet",
"key": "2021072714054701000_4.1.42.20",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1093/ije/dyz174",
"article-title": "Cohort Profile: East London Genes & Health (ELGH), a community-based population genomics and health study in British Bangladeshi and British Pakistani people",
"author": "Finer",
"doi-asserted-by": "crossref",
"first-page": "20",
"journal-title": "Int J Epidemiol",
"key": "2021072714054701000_4.1.42.21",
"volume": "49",
"year": "2020"
},
{
"DOI": "10.3390/jpm6010002",
"article-title": "Building the partners healthcare Biobank at partners personalized medicine: informed consent, return of research results, recruitment lessons and operational considerations",
"author": "Karlson",
"doi-asserted-by": "crossref",
"journal-title": "J Pers Med",
"key": "2021072714054701000_4.1.42.22",
"volume": "6",
"year": "2016"
},
{
"DOI": "10.1017/thg.2012.140",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.23"
},
{
"DOI": "10.1016/S0140-6736(17)31928-1",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.24"
},
{
"DOI": "10.1136/bmj.k1687",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.25"
},
{
"key": "2021072714054701000_4.1.42.26",
"unstructured": "deCODE genetic . Home. Available: https://www.decode.com/ [Accessed 02 Aug 2020]."
},
{
"DOI": "10.1016/j.hlpt.2012.07.003",
"article-title": "Uk Biobank: current status and what it means for epidemiology",
"author": "Allen",
"doi-asserted-by": "crossref",
"first-page": "123",
"journal-title": "Health Policy Technol",
"key": "2021072714054701000_4.1.42.27",
"volume": "1",
"year": "2012"
},
{
"DOI": "10.1038/s41586-018-0579-z",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.28"
},
{
"DOI": "10.1093/bioinformatics/btz633",
"article-title": "RICOPILI: rapid imputation for COnsortias pipeline",
"author": "Lam",
"doi-asserted-by": "crossref",
"first-page": "930",
"journal-title": "Bioinformatics",
"key": "2021072714054701000_4.1.42.29",
"volume": "36",
"year": "2020"
},
{
"article-title": "Dynamic linkage of COVID-19 test results between public health England's second generation surveillance system and UK Biobank",
"author": "Armstrong",
"journal-title": "Microb Genom",
"key": "2021072714054701000_4.1.42.30",
"volume": "6",
"year": "2020"
},
{
"key": "2021072714054701000_4.1.42.31",
"unstructured": "R Core Team . R: a language and environment for statistical computing, 2019. Available: https://www.R-project.org/"
},
{
"DOI": "10.1086/519795",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.32"
},
{
"DOI": "10.7554/eLife.34408",
"article-title": "The MR-Base platform supports systematic causal inference across the human phenome",
"author": "Hemani",
"doi-asserted-by": "crossref",
"journal-title": "Elife",
"key": "2021072714054701000_4.1.42.33",
"volume": "7",
"year": "2018"
},
{
"DOI": "10.1002/gepi.22295",
"article-title": "A comparison of robust Mendelian randomization methods using summary data",
"author": "Slob",
"doi-asserted-by": "crossref",
"first-page": "313",
"journal-title": "Genet Epidemiol",
"key": "2021072714054701000_4.1.42.34",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.1002/gepi.21998",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.35"
},
{
"DOI": "10.1093/gerona/glaa010",
"article-title": "Vitamin D status of adults in the community, in outpatient clinics, in hospital, and in nursing homes in the West of Ireland",
"author": "Griffin",
"doi-asserted-by": "crossref",
"first-page": "2418",
"journal-title": "J Gerontol A Biol Sci Med Sci",
"key": "2021072714054701000_4.1.42.36",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1136/bmj.k601",
"doi-asserted-by": "publisher",
"key": "2021072714054701000_4.1.42.37"
},
{
"DOI": "10.1007/s00223-019-00620-2",
"article-title": "Vitamin D measurement, the debates continue, new analytes have emerged, developments have variable outcomes",
"author": "Fraser",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Calcif Tissue Int",
"key": "2021072714054701000_4.1.42.38",
"volume": "106",
"year": "2020"
}
],
"reference-count": 38,
"references-count": 38,
"relation": {},
"resource": {
"primary": {
"URL": "https://nutrition.bmj.com/lookup/doi/10.1136/bmjnph-2020-000151"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Medicine (miscellaneous)",
"Health (social science)"
],
"subtitle": [],
"title": "No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "4"
}
