Course and Survival of COVID-19 Patients with Comorbidities in Relation to the Trace Element Status at Hospital Admission
et al., Nutrients, doi:10.3390/nu13103304, Sep 2021
Zinc for COVID-19
2nd treatment shown to reduce risk in
July 2020, now with p = 0.00000028 from 47 studies, recognized in 23 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
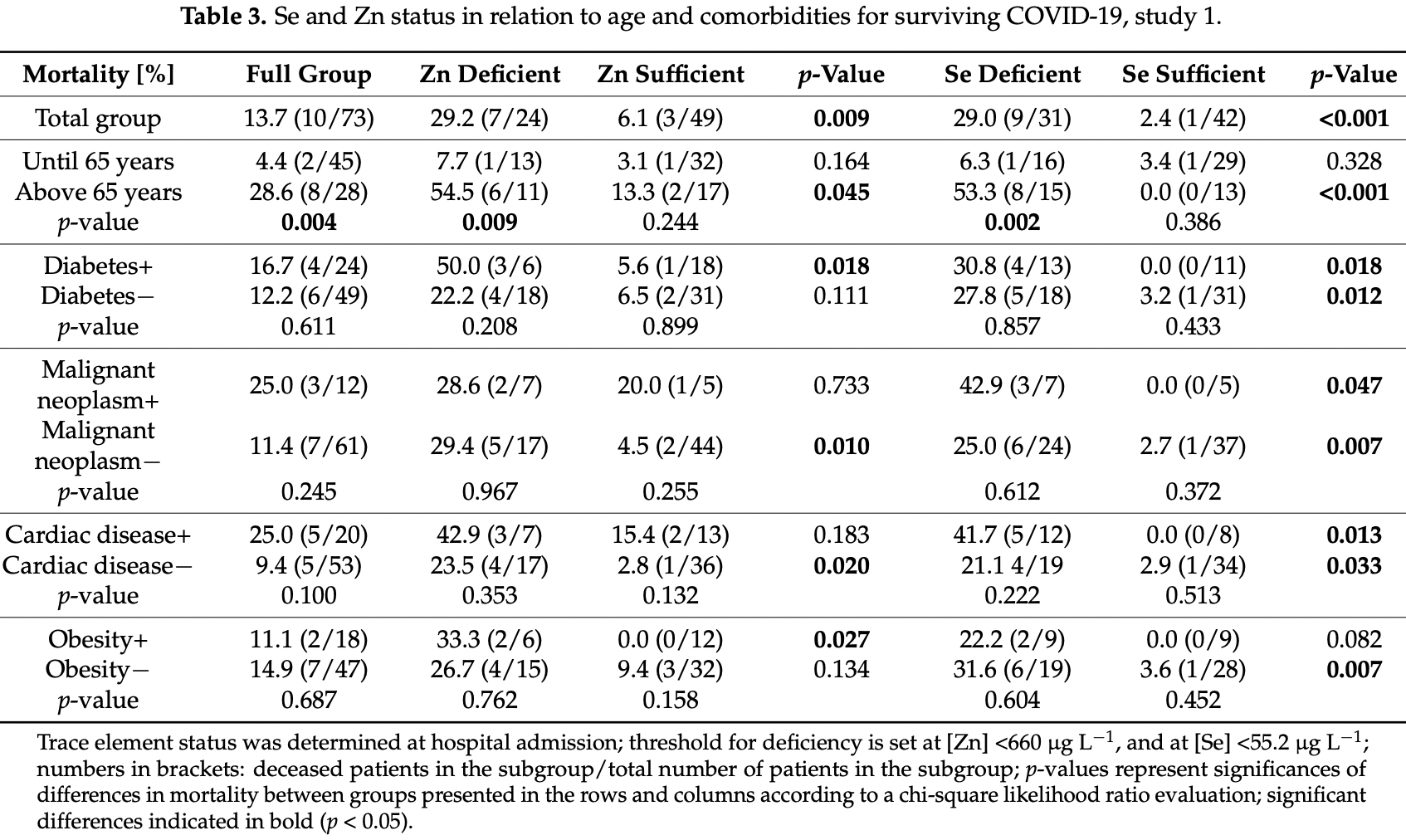
Retrospective 73 hospitalized COVID-19 patients in Belgium, showing higher risk of mortality with selenium deficiency and zinc deficiency.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
Study covers selenium and zinc.
|
risk of death, 79.0% lower, RR 0.21, p = 0.01, high zinc levels (≥660µg/L) 3 of 49 (6.1%), low zinc levels (<660µg/L) 7 of 24 (29.2%), NNT 4.3.
|
|
risk of death, 78.4% lower, RR 0.22, p = 0.03, high zinc levels (≥660µg/L) 2 of 17 (11.8%), low zinc levels (<660µg/L) 6 of 11 (54.5%), NNT 2.3, >65 years.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Du Laing et al., 22 Sep 2021, retrospective, Belgium, peer-reviewed, 11 authors.
Course and Survival of COVID-19 Patients with Comorbidities in Relation to the Trace Element Status at Hospital Admission
Nutrients, doi:10.3390/nu13103304
Selenium (Se) and zinc (Zn) are essential trace elements needed for appropriate immune system responses, cell signalling and anti-viral defence. A cross-sectional observational study was conducted at two hospitals in Ghent, Belgium, to investigate whether Se and/or Zn deficiency upon hospital admission correlates to disease severity and mortality risk in COVID-19 patients with or without co-morbidities. Trace element concentrations along with additional biomarkers were determined in serum or plasma and associated to disease severity and outcome. An insufficient Se and/or Zn status upon hospital admission was associated with a higher mortality rate and a more severe disease course in the entire study group, especially in the senior population. In comparison to healthy European adults, the patients displayed strongly depressed total Se (mean ± SD: 59.2 ± 20.6 vs. 84.4 ± 23.4 µg L −1 ) and SELENOP (mean ± SD: 2.2 ± 1.9 vs. 4.3 ± 1.0 mg L −1 ) concentrations at hospital admission. Particularly strong associations were observed for death risk of cancer, diabetes and chronic cardiac disease patients with low Se status, and of diabetes and obese patients with Zn deficiency. A composite biomarker based on serum or plasma Se, SELENOP and Zn at hospital admission proved to be a reliable tool to predict severe COVID-19 course and death, or mild disease course. We conclude that trace element assessment at hospital admission may contribute to a better stratification of patients with COVID-19 and other similar infectious diseases, support clinical care, therapeutic interventions and adjuvant supplementation needs, and may prove of particular relevance for patients with relevant comorbidities.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The analytical measurements and research in the lab of LS are supported by the Deutsche Forschungsgemeinschaft (DFG), Research Unit FOR-2558 "TraceAge" (Scho 849/6-2), and CRC/TR 296 "Local control of TH action" (LocoTact, P17).
Institutional Review Board Statement: The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of JPH Ghent and UZ Gent (BC-07492, approved on 23 March 2020). Informed Consent Statement: Informed consent was obtained from all subjects involved in the study.
Conflicts of Interest: LS holds shares in selenOmed GmbH, a company involved in Se status assessment and supplementation. The other authors declare no competing interest.
References
Alexander, Tinkov, Strand, Alehagen, Skalny et al., Early Nutritional Interventions with Zinc, Selenium and Vitamin D for Raising Anti-Viral Resistance Against Progressive COVID-19, Nutrients, doi:10.3390/nu12082358
Alfthan, Eurola, Ekholm, Venalainen, Root et al., Effects of nationwide addition of selenium to fertilizers on foods, and animal and human health in Finland: From deficiency to optimal selenium status of the population, J. Trace Elem. Med. Biol, doi:10.1016/j.jtemb.2014.04.009
Beck, Handy, Levander, Host nutritional status: The neglected virulence factor, Trends Microbiol
Beck, Nelson, Shi, Van Dael, Schiffrin et al., Selenium deficiency increases the pathology of an influenza virus infection, FASEB J, doi:10.1096/fj.00-0721fje
Beck, Shi, Morris, Levander, Rapid genomic evolution of a non-virulent coxsackievirus B3 in seleniumdeficient mice results in selection of identical virulent isolates, Nat. Med, doi:10.1038/nm0595-433
Berger, Manzanares, Micronutrients early in critical illness, selective or generous, enteral or intravenous?, Curr. Opin. Clin. Nutr. Metab. Care, doi:10.1097/MCO.0000000000000724
Bermano, Meplan, Mercer, Hesketh, Selenium and viral infection: Are there lessons for COVID-19? Brit, J. Nutr, doi:10.1017/S0007114520003128
Braunstein, Kusmenkov, Zuck, Angstwurm, Becker et al., Selenium and Selenoprotein P Deficiency Correlates with Complications and Adverse Outcome After Major Trauma, Shock
Brodin, Hackler, Misra, Wendt, Sun et al., Selenoprotein P as Biomarker of Selenium Status in Clinical Trials with Therapeutic Dosages of Selenite, Nutrients, doi:10.3390/nu12041067
Buicu, Cernea, Benedek, Buicu, Benedek, Systemic Inflammation and COVID-19 Mortality in Patients with Major Noncommunicable Diseases: Chronic Coronary Syndromes, Diabetes and Obesity, J. Clin. Med, doi:10.3390/jcm10081545
Cabral, Kuxhaus, Eichelmann, Kopp, Alker et al., Trace element profile and incidence of type 2 diabetes, cardiovascular disease and colorectal cancer: Results from the EPIC-Potsdam cohort study, Eur. J. Nutr, doi:10.1007/s00394-021-02494-3
Calder, Bosco, Bourdet-Sicard, Capuron, Delzenne et al., Health relevance of the modification of low grade inflammation in ageing (inflammageing) and the role of nutrition, Ageing Res. Rev, doi:10.1016/j.arr.2017.09.001
Dettorre, Patel, Gennari, Pentheroudakis, Romano et al., The systemic pro-inflammatory response: Targeting the dangerous liaison between COVID-19 and cancer, ESMO Open, doi:10.1016/j.esmoop.2021.100123
Femiano, Gombos, Scully, Recurrent herpes labialis: A pilot study of the efficacy of zinc therapy, J. Oral Pathol. Med, doi:10.1111/j.1600-0714.2005.00327.x
Forceville, Vitoux, Gauzit, Combes, Lahilaire et al., Selenium, systemic immune response syndrome, sepsis, and outcome in critically ill patients, Crit. Care Med, doi:10.1097/00003246-199809000-00021
Gasmi, Tippairote, Mujawdiya, Peana, Menzel et al., Micronutrients as immunomodulatory tools for COVID-19 management, Clin. Immunol, doi:10.1016/j.clim.2020.108545
Gorji, Khaleghi Ghadiri, Potential roles of micronutrient deficiency and immune system dysfunction in the coronavirus disease 2019 (COVID-19) pandemic, Nutrition, doi:10.1016/j.nut.2020.111047
Guillin, Vindry, Ohlmann, Chavatte, Selenium, Selenoproteins and Viral Infection, Nutrients
Haase, Schomburg, You'd Better Zinc-Trace Element Homeostasis in Infection and Inflammation, Nutrients
Heller, Sun, Hackler, Seelig, Seibert et al., Prediction of survival odds in COVID-19 by zinc, age and selenoprotein P as composite biomarker, Redox Biol
Hoffmann, Berry, The influence of selenium on immune responses, Mol. Nutr. Food Res, doi:10.1002/mnfr.200700330
Huang, Rose, Hoffmann, The role of selenium in inflammation and immunity: From molecular mechanisms to therapeutic opportunities, Antioxid. Redox Signal, doi:10.1089/ars.2011.4145
Hughes, Fedirko, Jenab, Schomburg, Meplan et al., Selenium status is associated with colorectal cancer risk in the European prospective investigation of cancer and nutrition cohort, Int. J. Cancer, doi:10.1002/ijc.29071
Hulisz, Efficacy of zinc against common cold viruses: An overview, J. Am. Pharm. Assoc, doi:10.1331/1544-3191.44.5.594.Hulisz
Jaspers, Zhang, Brighton, Carson, Styblo et al., Selenium deficiency alters epithelial cell morphology and responses to influenza, Free Radic. Biol. Med, doi:10.1016/j.freeradbiomed.2007.03.017
Jothimani, Kailasam, Danielraj, Nallathambi, Ramachandran et al., COVID-19: Poor outcomes in patients with zinc deficiency, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.09.014
Kipp, Strohm, Brigelius-Flohe, Schomburg, Bechthold et al., Revised reference values for selenium intake, J. Trace Elem. Med. Biol, doi:10.1016/j.jtemb.2015.07.005
Labunskyy, Hatfield, Gladyshev, Selenoproteins: Molecular pathways and physiological roles, Physiol. Rev, doi:10.1152/physrev.00039.2013
Levander, The selenium-coxsackievirus connection: Chronicle of a collaboration, J. Nutr, doi:10.1093/jn/130.2.485S
Lossow, Kopp, Schwarz, Finke, Winkelbeiner et al., Aging affects sex-and organ-specific trace element profiles in mice, Aging, doi:10.18632/aging.103572
Maehira, Luyo, Miyagi, Oshiro, Yamane et al., Alterations of serum selenium concentrations in the acute phase of pathological conditions, Clin. Chim. Acta, doi:10.1016/S0009-8981(01)00744-6
Majeed, Nagabhushanam, Gowda, Mundkur, An exploratory study of selenium status in healthy individuals and in patients with COVID-19 in a south Indian population: The case for adequate selenium status, Nutrition, doi:10.1016/j.nut.2020.111053
Moghaddam, Heller, Sun, Seelig, Cherkezov et al., Selenium Deficiency Is Associated with Mortality Risk from COVID-19, Nutrients, doi:10.3390/nu12072098
Monsen, Dietary reference intakes for the antioxidant nutrients: Vitamin C, vitamin E, selenium, and carotenoids, J. Am. Diet. Assoc, doi:10.1016/S0002-8223(00)00189-9
Ng, Tipih, Makoah, Vermeulen, Goedhals et al., Comorbidities in SARS-CoV-2 Patients: A Systematic Review and Meta-Analysis, mBio, doi:10.1128/mBio.03647-20
Renko, Hofmann, Stoedter, Hollenbach, Behrends et al., Down-regulation of the hepatic selenoprotein biosynthesis machinery impairs selenium metabolism during the acute phase response in mice, FASEB J, doi:10.1096/fj.08-119370
Rolles, Maywald, Rink, Influence of zinc deficiency and supplementation on NK cell cytotoxicity, J. Funct. Foods, doi:10.1016/j.jff.2018.07.027
Salonen, Alfthan, Huttunen, Pikkarainen, Puska, Association between Cardiovascular Death and Myocardial-Infarction and Serum Selenium in a Matched-Pair Longitudinal-Study, Lancet, doi:10.1016/S0140-6736(82)91028-5
Samad, Sodunke, Abubakar, Jahan, Sharma et al., The Implications of Zinc Therapy in Combating the COVID-19 Global Pandemic, J. Inflamm. Res, doi:10.2147/JIR.S295377
Santos, Sinha, Obesity and aging: Molecular mechanisms and therapeutic approaches, Ageing Res. Rev
Schomburg, The other view: The trace element selenium as a micronutrient in thyroid disease, diabetes, and beyond, Hormones, doi:10.1007/s42000-019-00150-4
Sherlock, Sjostrom, Sian, Delaney, Tipple et al., Hepatic-Specific Decrease in the Expression of Selenoenzymes and Factors Essential for Selenium Processing After Endotoxemia, Front. Immunol, doi:10.3389/fimmu.2020.595282
Sies, Jones, Reactive oxygen species (ROS) as pleiotropic physiological signalling agents, Nat. Rev. Mol. Cell Biol, doi:10.1038/s41580-020-0230-3
Steinbrenner, Al-Quraishy, Dkhil, Wunderlich, Sies, Dietary selenium in adjuvant therapy of viral and bacterial infections, Adv. Nutr, doi:10.3945/an.114.007575
Steinman, Lum, Ho, Kaminski, Steinman, Reduced development of COVID-19 in children reveals molecular checkpoints gating pathogenesis illuminating potential therapeutics, Proc. Natl. Acad. Sci, doi:10.1073/pnas.2012358117
Stoedter, Renko, Hog, Schomburg, Selenium controls the sex-specific immune response and selenoprotein expression during the acute-phase response in mice, Biochem. J, doi:10.1042/BJ20091868
Stone, Kawai, Kupka, Fawzi, Role of selenium in HIV infection, Nutr. Rev, doi:10.1111/j.1753-4887.2010.00337.x
Suara, Crowe, Jr, Effect of zinc salts on respiratory syncytial virus replication, Antimicrob. Agents Chemother, doi:10.1128/AAC.48.3.783-790.2004
Subedi, Tchen, Gaire, Hu, Hu, Adjunctive Nutraceutical Therapies for COVID-19, Int. J. Mol. Sci, doi:10.3390/ijms22041963
Thomson, Assessment of requirements for selenium and adequacy of selenium status: A review, Eur. J. Clin. Nutr, doi:10.1038/sj.ejcn.1601800
Vogel-Gonzalez, Tallo-Parra, Herrera-Fernandez, Perez-Vilaro, Chilton et al., Low Zinc Levels at Admission Associates with Poor Clinical Outcomes in SARS-CoV-2 Infection, Nutrients, doi:10.3390/nu13020562
Wessels, Rolles, Rink, The Potential Impact of Zinc Supplementation on COVID-19 Pathogenesis, Front. Immunol, doi:10.3389/fimmu.2020.01712
Wiehe, Cremer, Wisniewska, Becker, Rijntjes et al., Selenium status in neonates with connatal infection, Br. J. Nutr, doi:10.1017/S0007114516002208
Yang, Zheng, Gou, Pu, Chen et al., Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.03.017
Zhang, Taylor, Bennett, Saad, Rayman, Association between regional selenium status and reported outcome of COVID-19 cases in China, Am. J. Clin. Nutr, doi:10.1093/ajcn/nqaa095
DOI record:
{
"DOI": "10.3390/nu13103304",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu13103304",
"abstract": "<jats:p>Selenium (Se) and zinc (Zn) are essential trace elements needed for appropriate immune system responses, cell signalling and anti-viral defence. A cross-sectional observational study was conducted at two hospitals in Ghent, Belgium, to investigate whether Se and/or Zn deficiency upon hospital admission correlates to disease severity and mortality risk in COVID-19 patients with or without co-morbidities. Trace element concentrations along with additional biomarkers were determined in serum or plasma and associated to disease severity and outcome. An insufficient Se and/or Zn status upon hospital admission was associated with a higher mortality rate and a more severe disease course in the entire study group, especially in the senior population. In comparison to healthy European adults, the patients displayed strongly depressed total Se (mean ± SD: 59.2 ± 20.6 vs. 84.4 ± 23.4 µg L−1) and SELENOP (mean ± SD: 2.2 ± 1.9 vs. 4.3 ± 1.0 mg L−1) concentrations at hospital admission. Particularly strong associations were observed for death risk of cancer, diabetes and chronic cardiac disease patients with low Se status, and of diabetes and obese patients with Zn deficiency. A composite biomarker based on serum or plasma Se, SELENOP and Zn at hospital admission proved to be a reliable tool to predict severe COVID-19 course and death, or mild disease course. We conclude that trace element assessment at hospital admission may contribute to a better stratification of patients with COVID-19 and other similar infectious diseases, support clinical care, therapeutic interventions and adjuvant supplementation needs, and may prove of particular relevance for patients with relevant comorbidities.</jats:p>",
"alternative-id": [
"nu13103304"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-6661-1312",
"affiliation": [],
"authenticated-orcid": false,
"family": "Du Laing",
"given": "Gijs",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-7506-8646",
"affiliation": [],
"authenticated-orcid": false,
"family": "Petrovic",
"given": "Mirko",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1389-8855",
"affiliation": [],
"authenticated-orcid": false,
"family": "Lachat",
"given": "Carl",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6151-5126",
"affiliation": [],
"authenticated-orcid": false,
"family": "De Boevre",
"given": "Marthe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Klingenberg",
"given": "Georg J.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4458-6555",
"affiliation": [],
"authenticated-orcid": false,
"family": "Sun",
"given": "Qian",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2160-7253",
"affiliation": [],
"authenticated-orcid": false,
"family": "De Saeger",
"given": "Sarah",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9291-0658",
"affiliation": [],
"authenticated-orcid": false,
"family": "De Clercq",
"given": "Jozefien",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ide",
"given": "Louis",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vandekerckhove",
"given": "Linos",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9445-1555",
"affiliation": [],
"authenticated-orcid": false,
"family": "Schomburg",
"given": "Lutz",
"sequence": "additional"
}
],
"container-title": [
"Nutrients"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
9,
27
]
],
"date-time": "2021-09-27T02:24:13Z",
"timestamp": 1632709453000
},
"deposited": {
"date-parts": [
[
2021,
9,
28
]
],
"date-time": "2021-09-28T02:20:19Z",
"timestamp": 1632795619000
},
"funder": [
{
"DOI": "10.13039/501100001659",
"award": [
"Scho 849/6-2",
"CRC/TR 296"
],
"doi-asserted-by": "publisher",
"name": "Deutsche Forschungsgemeinschaft"
}
],
"indexed": {
"date-parts": [
[
2022,
2,
12
]
],
"date-time": "2022-02-12T12:26:56Z",
"timestamp": 1644668816066
},
"is-referenced-by-count": 3,
"issn-type": [
{
"type": "electronic",
"value": "2072-6643"
}
],
"issue": "10",
"issued": {
"date-parts": [
[
2021,
9,
22
]
]
},
"journal-issue": {
"issue": "10",
"published-online": {
"date-parts": [
[
2021,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
22
]
],
"date-time": "2021-09-22T00:00:00Z",
"timestamp": 1632268800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/13/10/3304/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3304",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
9,
22
]
]
},
"published-online": {
"date-parts": [
[
2021,
9,
22
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1073/pnas.2012358117",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1128/mBio.03647-20",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1016/j.ijid.2020.03.017",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1016/j.arr.2021.101268",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1038/s41580-020-0230-3",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.18632/aging.103572",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1007/s00394-021-02494-3",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.3390/nu11092078",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1016/j.arr.2017.09.001",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.3390/ijms22041963",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.1017/S0007114520003128",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1016/j.clim.2020.108545",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.3389/fimmu.2020.01712",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1016/j.nut.2020.111047",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1152/physrev.00039.2013",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1002/mnfr.200700330",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.3945/an.114.007575",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1017/S0007114516002208",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1038/nm0595-433",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1096/fj.00-0721fje",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/j.freeradbiomed.2007.03.017",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1093/jn/130.2.485S",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1016/j.jtemb.2015.07.005",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1093/ajcn/nqaa095",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.3390/nu12072098",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1331/1544-3191.44.5.594.Hulisz",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1128/AAC.48.3.783-790.2004",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1111/j.1600-0714.2005.00327.x",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1016/j.jff.2018.07.027",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1016/j.redox.2020.101764",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.3390/nu13020562",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1002/ijc.29071",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1016/S0140-6736(82)91028-5",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.3390/nu12041067",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1016/S0002-8223(00)00189-9",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1016/j.nut.2020.111053",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.3390/nu11092101",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1089/ars.2011.4145",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1096/fj.08-119370",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1042/BJ20091868",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1016/S0009-8981(01)00744-6",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.3389/fimmu.2020.595282",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1097/00003246-199809000-00021",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1097/MCO.0000000000000724",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1111/j.1753-4887.2010.00337.x",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1016/j.tim.2004.07.007",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1097/SHK.0000000000001344",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.3390/nu12082358",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.2147/JIR.S295377",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1016/j.ijid.2020.09.014",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1038/sj.ejcn.1601800",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.1007/s42000-019-00150-4",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.1016/j.jtemb.2014.04.009",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1016/j.esmoop.2021.100123",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.3390/jcm10081545",
"doi-asserted-by": "publisher",
"key": "ref55"
}
],
"reference-count": 55,
"references-count": 55,
"relation": {},
"score": 1,
"short-container-title": [
"Nutrients"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": [
"Course and Survival of COVID-19 Patients with Comorbidities in Relation to the Trace Element Status at Hospital Admission"
],
"type": "journal-article",
"volume": "13"
}
