Folate Levels in Patients Hospitalized with Coronavirus Disease 2019
et al., Nutrients, doi:10.3390/nu13030812, Mar 2021
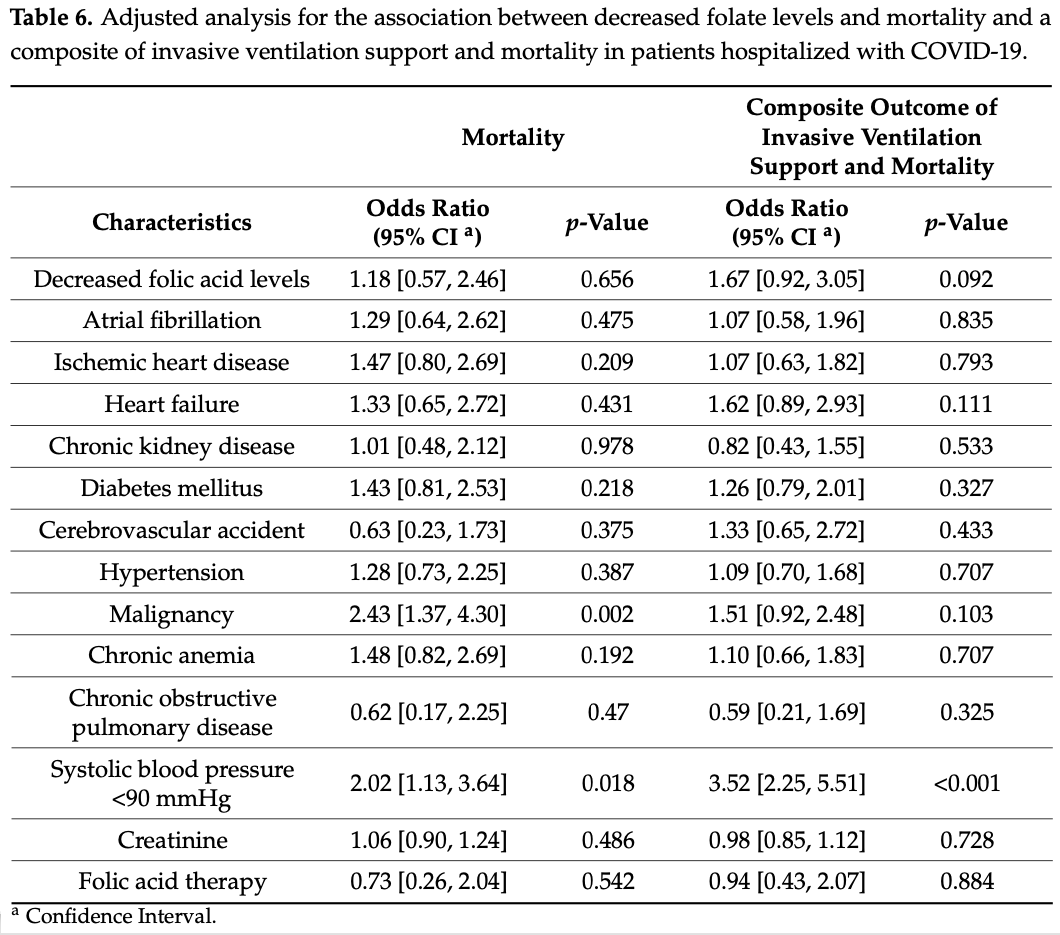
Retrospective 333 hospitalized patients in Israel, showing no significant difference in outcomes with low folate levels or with folic acid supplementation.
|
risk of death, 27.0% lower, OR 0.73, p = 0.54, treatment 23, control 310, RR approximated with OR.
|
|
risk of death/intubation, 6.0% lower, OR 0.94, p = 0.88, treatment 23, control 310, RR approximated with OR.
|
|
risk of death, 15.3% lower, OR 0.85, p = 0.66, high vitamin B9 levels (≥5.9ng/mL) 296, low vitamin B9 levels (<5.9ng/mL) 38, inverted to make OR<1 favor high vitamin B9 levels (≥5.9ng/mL), RR approximated with OR, outcome based on serum levels.
|
|
risk of death/intubation, 40.1% lower, OR 0.60, p = 0.09, high vitamin B9 levels (≥5.9ng/mL) 296, low vitamin B9 levels (<5.9ng/mL) 38, inverted to make OR<1 favor high vitamin B9 levels (≥5.9ng/mL), RR approximated with OR, outcome based on serum levels.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Meisel et al., 2 Mar 2021, retrospective, Israel, peer-reviewed, 8 authors, study period 27 January, 2020 - 23 November, 2020.
Contact: eshcarme@gmail.com (corresponding author), orlyefros@gmail.com, jobleier@gmail.com, talbh142@gmail.com, avshalom.leibowitz@sheba.health.gov.il, gad.segal@sheba.health.gov.il, galia.rahav@sheba.health.gov.il, ehud.grossman@sheba.health.gov.il.
Folate Levels in Patients Hospitalized with Coronavirus Disease 2019
Nutrients, doi:10.3390/nu13030812
We aimed to investigate the prevalence of decreased folate levels in patients hospitalized with Coronavirus Disease 2019 (COVID-19) and evaluate their outcome and the prognostic significance associated with its different levels. In this retrospective cohort study, data were obtained from the electronic medical records at the Sheba Medical Center. Folic acid levels were available in 333 out of 1020 consecutive patients diagnosed with COVID-19 infection hospitalized from January 2020 to November 2020. Thirty-eight (11.4%) of the 333 patients comprising the present study population had low folate levels. No significant difference was found in the incidence of acute kidney injury, hypoxemia, invasive ventilation, length of hospital stay, and mortality be-tween patients with decreased and normal-range folate levels. When sub-dividing the study population according to quartiles of folate levels, similar findings were observed. In conclusion, decreased serum folate levels are common among hospitalized patients with COVID-19, but there was no association between serum folate levels and clinical outcomes. Due to the important role of folate in cell metabolism and the potential pathologic impact when deficient, a follow-up of folate levels or possible supplementation should be encouraged in hospitalized COVID-19 patients. Fur-ther studies are required to assess the prevalence and consequences of folate deficiency in COVID-19 patients.
References
Acosta-Elias, Espinosa-Tanguma, The Folate Concentration and/or Folic Acid Metabolites in Plasma as Factor for COVID-19 Infection, Front. Pharmacol, doi:10.3389/fphar.2020.01062
Annweiler, Corvaisier, Gautier, Dubée, Legrand et al., Vitamin D Supplementation Associated to Better Survival in Hospitalized Frail Elderly COVID-19 Patients: The GERIA-COVID Quasi-Experimental Study, Nutrients, doi:10.3390/nu12113377
Baj, Karakuła-Juchnowicz, Teresi Ński, Buszewicz, Ciesielka et al., COVID-19: Specific and Non-Specific Clinical Manifestations and Symptoms: The Current State of Knowledge, J. Clin. Med, doi:10.3390/jcm9061753
Bamonti-Catena, Buccianti, Porcella, Valenti, Como et al., Folate measurements in patients on regular hemodialysis treatment, Am. J. Kidney Dis, doi:10.1016/S0272-6386(99)70186-1
Benskin, A Basic Review of the Preliminary Evidence That COVID-19 Risk and Severity Is Increased in Vitamin D Deficiency, Front. Public Health, doi:10.3389/fpubh.2020.00513
Berlin, Gulick, Martinez, Severe Covid-19, N. Engl. J. Med, doi:10.1056/NEJMcp2009575
Breu, Theisen-Toupal, Feldman, Serum and red blood cell folate testing on hospitalized patients, J. Hosp. Med, doi:10.1002/jhm.2385
Calder, Carr, Gombart, Eggersdorfer, Optimal Nutritional Status for a Well-Functioning Immune System Is an Important Factor to Protect against Viral Infections, Nutrients, doi:10.3390/nu12041181
Calder, Nutrition, immunity and COVID-19, BMJ Nutr. Prev. Health, doi:10.1136/bmjnph-2020-000085
Choumenkovitch, Selhub, Wilson, Rader, Rosenberg et al., Folic Acid Intake from Fortification in United States Exceeds Predictions, J. Nutr, doi:10.1093/jn/132.9.2792
Ducker, Rabinowitz, One-Carbon Metabolism in Health and Disease, Cell Metab, doi:10.1016/j.cmet.2016.08.009
Eloranta, Zaïr, Hiller, Häusler, Stieger et al., Vitamin D3 and its nuclear receptor increase the expression and activity of the human proton-coupled folate transporter, Mol. Pharmacol, doi:10.1124/mol.109.055392
Gombart, Pierre, Maggini, A Review of Micronutrients and the Immune System-Working in Harmony to Reduce the Risk of Infection, Nutrients, doi:10.3390/nu12010236
Grant, Lahore, Mcdonnell, Baggerly, French et al., Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths, Nutrients, doi:10.3390/nu12040988
Green, Indicators for assessing folate and vitamin B-12 status and for monitoring the efficacy of intervention strategies, Am. J. Clin. Nutr, doi:10.3945/ajcn.110.009613
Gropper, Smith, Advanced Nutrition and Human Metabolism
Han, Huang, Jiang, Dong, Peng et al., Early Clinical and CT Manifestations of Coronavirus Disease 2019 (COVID-19) Pneumonia, Am. J. Roentgenol, doi:10.2214/AJR.20.22961
Ikizler, A Patient with CKD and Poor Nutritional Status, Clin. J. Am. Soc. Nephrol, doi:10.2215/CJN.04630513
Ilie, Stefanescu, Smith, The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality, Aging Clin. Exp. Res, doi:10.1007/s40520-020-01570-8
Im, Je, Baek, Chung, Kwon et al., Nutritional status of patients with COVID-19, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.08.018
Itelman, Wasserstrum, Segev, Avaky, Negru et al., Clinical Characterization of 162 COVID-19 patients in Israel: Preliminary Report from a Large Tertiary Center, Isr. Med. Assoc. J
Jacobson, Wreghitt, Saich, Nagington, Serum folate in viral and mycoplasmal infections, J. Infect
Katz, Yue, Xue, Increased risk for COVID-19 in patients with vitamin D deficiency, Nutrition, doi:10.1016/j.nut.2020.111106
Keskin, Turk Kardiyol, Iron Deficiency and Hematinic Changes in Atrial Fibrillation; A New Insight, Dern. Arsivi-Arch. Turk. Soc. Cardiol, doi:10.5543/tkda.2018.51001
Khwaja, KDIGO Clinical Practice Guidelines for Acute Kidney Injury, Nephron, doi:10.1159/000339789
Kumar, Jena, In silico virtual screening-based study of nutraceuticals predicts the therapeutic potentials of folic acid and its derivatives against COVID-19, Res. Sq, doi:10.21203/rs.3.rs-31775/v1
Li, Ma, Acute respiratory failure in COVID-19: Is it "typical" ARDS?, Crit. Care, doi:10.1186/s13054-020-02911-9
Lucock, Folic Acid: Nutritional Biochemistry, Molecular Biology, and Role in Disease Processes, Mol. Genet. Metab, doi:10.1006/mgme.2000.3027
Mao, Xing, Xu, Gong, He et al., Folic Acid and Vitamins D and B12 Correlate with Homocysteine in Chinese Patients with Type-2 Diabetes Mellitus, Hypertension, or Cardiovascular Disease, Medicine, doi:10.1097/MD.0000000000002652
Mercola, Grant, Wagner, Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity, Nutrients, doi:10.3390/nu12113361
Quinlivan, Gregory, Effect of food fortification on folic acid intake in the United States, Am. J. Clin. Nutr, doi:10.1093/ajcn/77.1.221
Rahman, Al-Taiar, Shaban, Al-Sabah, Mojiminiyi, Plasma 25-hydroxyvitamin D is positively associated with folate and vitamin B12 levels in adolescents, Nutr. Res, doi:10.1016/j.nutres.2020.06.003
Santaolalla, Beckmann, Kibaru, Josephs, Van Hemelrijck et al., Association Between Vitamin D and Novel SARS-CoV-2 Respiratory Dysfunction-A Scoping Review of Current Evidence and Its Implication for COVID-19 Pandemic, Front. Physiol, doi:10.3389/fphys.2020.564387
Scaglione, Panzavolta, Folate, folic acid and 5-methyltetrahydrofolate are not the same thing, Xenobiotica, doi:10.3109/00498254.2013.845705
Serseg, Benarous, Yousfi, Hispidin, Lepidine, Two Natural Compounds and Folic acid as Potential Inhibitors of 2019-novel coronavirus Main Protease (2019-nCoVMpro), molecular docking and SAR study, Curr. Comput. Aided. Drug Des, doi:10.2174/1573409916666200422075440
Shakoor, Feehan, Mikkelsen, Al Dhaheri, Ali et al., Be well: A potential role for vitamin B in COVID-19, Maturitas, doi:10.1016/j.maturitas.2020.08.007
Sheybani, Dokoohaki, Negahdaripour, Dehdashti, Zolghadr et al., The Role of Folic Acid in the Management of Respiratory Disease Caused by COVID-19, ChemRxiv, doi:10.26434/chemrxiv.12034980.v1
Singh, Gupta, Kazmi, Al-Abbasi, Negi et al., SARS CoV-2 aggravates cellular metabolism mediated complications in COVID-19 infection, Dermatol. Ther, doi:10.1111/dth.13871
Snow, Laboratory diagnosis of vitamin B12 and folate deficiency: A guide for the primary care physician, Arch. Intern. Med, doi:10.1001/archinte.159.12.1289
Strand, Taneja, Bhandari, Refsum, Ueland et al., Folate, but not vitamin B-12 status, predicts respiratory morbidity in north Indian children, Am. J. Clin. Nutr
Von Elm, Altman, Egger, Pocock, Gøtzsche et al., Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies, BMJ, doi:10.1136/bmj.39335.541782.AD
Wiltshire, Peña, Mackenzie, Shaw, Couper, High dose folic acid is a potential treatment for pulmonary hypertension, including when associated with COVID-19 pneumonia, Med. Hypotheses, doi:10.1016/j.mehy.2020.110142
DOI record:
{
"DOI": "10.3390/nu13030812",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu13030812",
"abstract": "<jats:p>We aimed to investigate the prevalence of decreased folate levels in patients hospitalized with Coronavirus Disease 2019 (COVID-19) and evaluate their outcome and the prognostic signifi-cance associated with its different levels. In this retrospective cohort study, data were obtained from the electronic medical records at the Sheba Medical Center. Folic acid levels were available in 333 out of 1020 consecutive patients diagnosed with COVID-19 infection hospitalized from January 2020 to November 2020. Thirty-eight (11.4%) of the 333 patients comprising the present study population had low folate levels. No significant difference was found in the incidence of acute kidney injury, hypoxemia, invasive ventilation, length of hospital stay, and mortality be-tween patients with decreased and normal-range folate levels. When sub-dividing the study population according to quartiles of folate levels, similar findings were observed. In conclusion, decreased serum folate levels are common among hospitalized patients with COVID-19, but there was no association between serum folate levels and clinical outcomes. Due to the important role of folate in cell metabolism and the potential pathologic impact when deficient, a follow-up of folate levels or possible supplementation should be encouraged in hospitalized COVID-19 patients. Fur-ther studies are required to assess the prevalence and consequences of folate deficiency in COVID-19 patients.</jats:p>",
"alternative-id": [
"nu13030812"
],
"author": [
{
"affiliation": [],
"family": "Meisel",
"given": "Eshcar",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-6024-9110",
"affiliation": [],
"authenticated-orcid": false,
"family": "Efros",
"given": "Orly",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0828-4867",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bleier",
"given": "Jonathan",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3798-8684",
"affiliation": [],
"authenticated-orcid": false,
"family": "Beit Halevi",
"given": "Tal",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3851-3245",
"affiliation": [],
"authenticated-orcid": false,
"family": "Segal",
"given": "Gad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rahav",
"given": "Galia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Leibowitz",
"given": "Avshalom",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Grossman",
"given": "Ehud",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
3,
2
]
],
"date-time": "2021-03-02T06:49:44Z",
"timestamp": 1614667784000
},
"deposited": {
"date-parts": [
[
2021,
3,
2
]
],
"date-time": "2021-03-02T07:07:16Z",
"timestamp": 1614668836000
},
"indexed": {
"date-parts": [
[
2023,
3,
15
]
],
"date-time": "2023-03-15T14:13:33Z",
"timestamp": 1678889613709
},
"is-referenced-by-count": 16,
"issue": "3",
"issued": {
"date-parts": [
[
2021,
3,
2
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2021,
3
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
3,
2
]
],
"date-time": "2021-03-02T00:00:00Z",
"timestamp": 1614643200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/13/3/812/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "812",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
3,
2
]
]
},
"published-online": {
"date-parts": [
[
2021,
3,
2
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"author": "Gropper",
"key": "ref1",
"series-title": "Advanced Nutrition and Human Metabolism",
"year": "2017"
},
{
"DOI": "10.3109/00498254.2013.845705",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1016/j.cmet.2016.08.009",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1001/archinte.159.12.1289",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.3945/ajcn.110.009613",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1006/mgme.2000.3027",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1016/S0163-4453(87)91827-5",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1093/ajcn/86.1.139",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.3390/nu12041181",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1136/bmjnph-2020-000085",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.3390/nu12010236",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1186/s13054-020-02911-9",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.2214/AJR.20.22961",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1056/NEJMcp2009575",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.3390/jcm9061753",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"article-title": "Clinical Characterization of 162 COVID-19 patients in Israel: Preliminary Report from a Large Tertiary Center",
"author": "Itelman",
"first-page": "271",
"journal-title": "Isr. Med. Assoc. J.",
"key": "ref16",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.3389/fphar.2020.01062",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1016/j.ijid.2020.08.018",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1124/mol.109.055392",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1016/j.nut.2020.111106",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.3389/fpubh.2020.00513",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.3390/nu12113361",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.3389/fphys.2020.564387",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1007/s40520-020-01570-8",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1159/000339789",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1136/bmj.39335.541782.AD",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1002/jhm.2385",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1093/ajcn/77.1.221",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1093/jn/132.9.2792",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1016/S0272-6386(99)70186-1",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.5543/tkda.2018.51001",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.2215/CJN.04630513",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.26434/chemrxiv.12034980.v1",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1016/j.maturitas.2020.08.007",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.21203/rs.3.rs-31775/v1",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.2174/1573409916666200422075440",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1111/dth.13871",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1016/j.mehy.2020.110142",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1097/MD.0000000000002652",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1016/j.nutres.2020.06.003",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.3390/nu12040988",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.3390/nu12113377",
"doi-asserted-by": "publisher",
"key": "ref42"
}
],
"reference-count": 42,
"references-count": 42,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/13/3/812"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Folate Levels in Patients Hospitalized with Coronavirus Disease 2019",
"type": "journal-article",
"volume": "13"
}