Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis
et al., Diabetologia, doi:10.1007/s00125-023-05928-1, May 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Systematic review and meta analysis showing significantly lower COVID-19 mortality and severity with metformin use. Authors analyze 169 studies of diabetes patients, with 23 reporting mortality results and 34 reporting severity results for metformin.
24 meta-analyses show significant improvements with metformin for mortality1-23,
hospitalization7,13,23 ,
progression1, and
severity8,9,13 .
Currently there are 110 metformin for COVID-19 studies, showing 36% lower mortality [32‑40%], 29% lower ventilation [12‑43%], 19% lower ICU admission [8‑28%], 17% lower hospitalization [11‑23%], and 5% fewer cases [-4‑13%].
|
risk of death, 31.0% lower, RR 0.69, p < 0.001.
|
|
risk of severe case, 22.0% lower, RR 0.78, p < 0.001.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Yang et al., The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus, Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2021.108977.
2.
Lukito et al., The Effect of Metformin Consumption on Mortality in Hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2020.11.006.
3.
Kow et al., Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis, Journal of Medical Virology, doi:10.1002/jmv.26498.
4.
Hariyanto et al., Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection, Obesity Medicine, doi:10.1016/j.obmed.2020.100290.
5.
Ma et al., Is metformin use associated with low mortality in patients with type 2 diabetes mellitus hospitalized for COVID-19? a multivariable and propensity score-adjusted meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0282210.
6.
Parveen et al., Association of Metformin with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis, Annals of the National Academy of Medical Sciences (India), doi:10.1055/s-0042-1760353.
7.
Li et al., Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Medicine, doi:10.3389/fmed.2021.704666.
8.
Schlesinger et al., Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis, Diabetologia, doi:10.1007/s00125-023-05928-1.
9.
Petrelli et al., Metformin and Covid-19: a systematic review of systematic reviews with meta-analysis, Acta Biomedica Atenei Parmensis, doi:10.23750/abm.v94iS3.14405.
10.
Oscanoa et al., Metformin therapy and severity and mortality of SARS-CoV-2 infection: a meta-analysis, Clinical Diabetology, doi:10.5603/DK.a2021.0035.
11.
Kan et al., Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2021.708494.
12.
Poly et al., Metformin Use Is Associated with Decreased Mortality in COVID-19 Patients with Diabetes: Evidence from Retrospective Studies and Biological Mechanism, Journal of Clinical Medicine, doi:10.3390/jcm10163507.
13.
Song et al., The Effect of Antihyperglycemic Medications on COVID-19: A Meta-analysis and Systematic Review from Observational Studies, Therapeutic Innovation & Regulatory Science, doi:10.1007/s43441-024-00633-6.
14.
Ganesh et al., Does metformin affect outcomes in COVID‐19 patients with new or pre‐existing diabetes mellitus? A systematic review and meta‐analysis, British Journal of Clinical Pharmacology, doi:10.1111/bcp.15258.
15.
Nassar et al., Noninsulin‐based antihyperglycemic medications in patients with diabetes and COVID‐19: A systematic review and meta‐analysis, Journal of Diabetes, doi:10.1111/1753-0407.13359.
16.
Zhan et al., Effect of Antidiabetic Therapy on Clinical Outcomes of COVID-19 Patients With Type 2 Diabetes: A Systematic Review and Meta-Analysis, Annals of Pharmacotherapy, doi:10.1177/10600280221133577.
17.
Nguyen et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196.
18.
Han et al., Association Between Anti-diabetic Agents and Clinical Outcomes of COVID-19 in Patients with Diabetes: A Systematic Review and Meta-Analysis, Archives of Medical Research, doi:10.1016/j.arcmed.2021.08.002.
19.
Chen et al., The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2022.895458.
20.
Scheen, A., Metformin and COVID-19: From cellular mechanisms to reduced mortality, Diabetes & Metabolism, doi:10.1016/j.diabet.2020.07.006.
21.
Sun et al., Is Metformin Use Associated With a Decreased Mortality for COVID-19 Diabetic Patients? A Meta-Analysis, Journal of the Endocrine Society, doi:10.1210/jendso/bvab048.709.
Schlesinger et al., 19 May 2023, peer-reviewed, 10 authors.
Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis
Diabetologia, doi:10.1007/s00125-023-05928-1
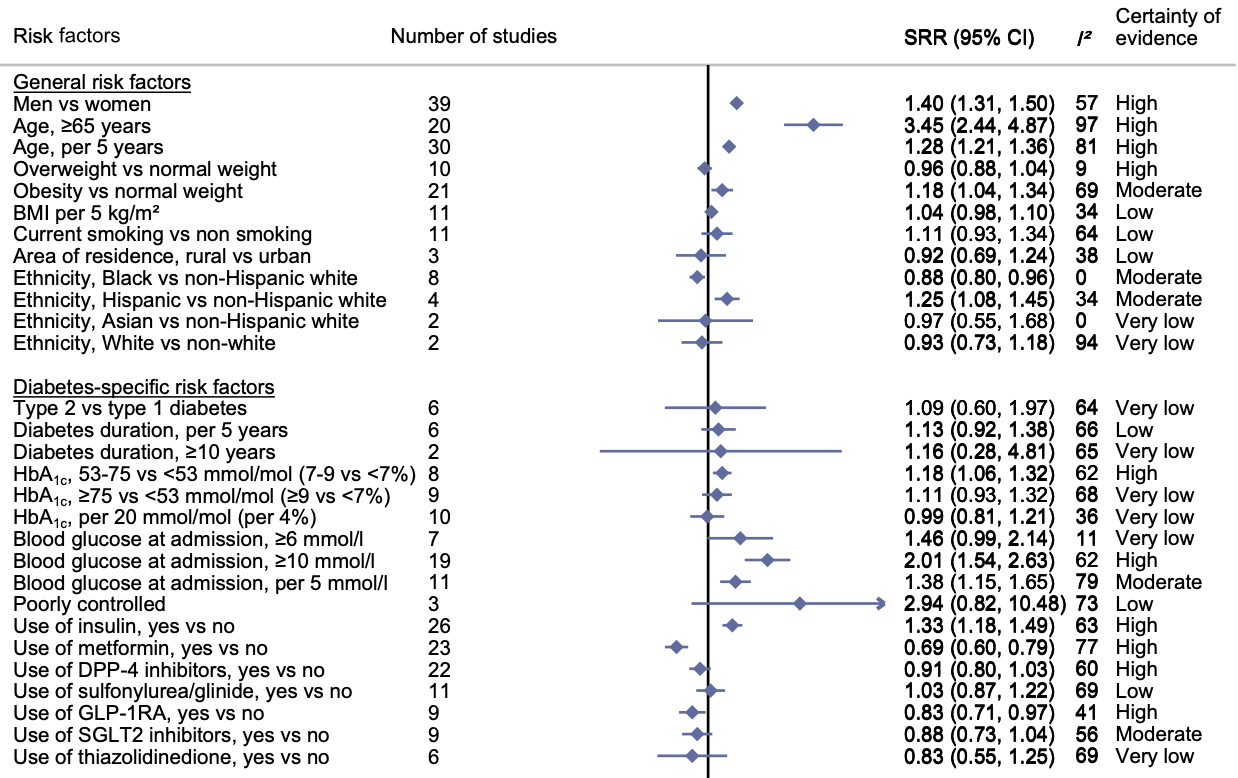
Aims/hypothesis To provide a systematic overview of the current body of evidence on high-risk phenotypes of diabetes associated with COVID-19 severity and death. Methods This is the first update of our recently published living systematic review and meta-analysis. Observational studies investigating phenotypes in individuals with diabetes and confirmed SARS-CoV-2 infection with regard to COVID-19-related death and severity were included. The literature search was conducted from inception up to 14 February 2022 in PubMed, Epistemonikos, Web of Science and the COVID-19 Research Database and updated using PubMed alert to 1 December 2022. A random-effects meta-analysis was used to calculate summary relative risks (SRRs) with 95% CIs. The risk of bias was evaluated using the Quality in Prognosis Studies (QUIPS) tool and the certainty of evidence using the GRADE approach. Results A total of 169 articles (147 new studies) based on approximately 900,000 individuals were included. We conducted 177 meta-analyses (83 on COVID-19-related death and 94 on COVID-19 severity). Certainty of evidence was strengthened for associations between male sex, older age, blood glucose level at admission, chronic insulin use, chronic metformin use (inversely) and pre-existing comorbidities (CVD, chronic kidney disease, chronic obstructive pulmonary disease) and COVID-19-related death. New evidence with moderate to high certainty emerged for the association between obesity (SRR [95% CI] 1.18 [1.04, 1.34], n=21 studies), HbA 1c (53-75 mmol/mol [7-9%]: 1.18 [1.06, 1.32], n=8), chronic glucagon-like peptide-1 receptor agonist use (0.83 [0.71, 0.97], n=9), pre-existing heart failure (1.33 [1.21, 1.47], n=14), pre-existing liver disease (1.40 [1.17, 1.67], n=6), the Charlson index (per 1 unit increase: 1.33 [1.13, 1.57], n=2), high levels of C-reactive protein (per 5 mg/l increase: 1.07 [1.02, 1.12], n=10), aspartate aminotransferase level (per 5 U/l increase: 1.28 [1.06, 1.54], n=5), eGFR (per 10 ml/min per 1.73 m 2 increase: 0.80 [0.71, 0.90], n=6), lactate dehydrogenase level (per 10 U/l increase: 1.03 [1.01, 1.04], n=7) and lymphocyte count (per 1×10 9 /l increase: 0.59 [0.40, 0.86], n=6) and COVID-19-related death. Similar associations were observed between risk phenotypes of diabetes and severity of COVID-19, with some new evidence on existing 0.38], n=3), pre-existing hypertension (1.23 [1.14, 1.33], n=49), neuropathy and cancer, and high IL-6 levels. A limitation of this study is that the included studies are observational in nature and residual or unmeasured confounding cannot be ruled out. Conclusions/interpretation Individuals with a more severe course of diabetes and pre-existing comorbidities had a poorer prognosis of COVID-19 than individuals with a milder course of the disease. Registration PROSPERO registration no. CRD42020193692. Previous version This is a living systematic review and meta-analysis. The previous version can be found at https:// link. sprin ger...
Supplementary Information The online version contains peer-reviewed but unedited supplementary material available at https:// doi. org/ 10. 1007/ s00125-023-05928-1.
Authors' relationships and activities CH is a member of the editorial board of Diabetologia. MR received personal fees from Boehringer Ingelheim Pharma, Eli Lilly, Fishawack Group, Novo Nordisk, Sanofi US, Target NASH and Terra Firma, and investigator-initiated research support from Boehringer Ingelheim, Nutricia/Danone and Sanofi-Aventis. All other authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work. Contribution statement MR and SS designed the study and wrote the first draft of the manuscript. AL, NC, PL, MN, JB and SS performed the literature search and literature screening. CH assisted in the selection of eligible studies. AL, NC, PL and MN extracted data and KP assisted with extraction of data on treatment. AL, NC, PL, MN and SS assessed the risk of bias of the studies and JB, MN and SS assessed the certainty of evidence of the associations. SS performed the statistical analysis and OK assisted with the statistical analysis. All authors contributed to data acquisition, data interpretation and revision of manuscript drafts and read and approved the final manuscript. SS is the guarantor of this work.
Authors and Affiliations
Sabrina
References
Abe, Egbuche, Igwe, Cardiovascular complications in COVID-19 patients with or without diabetes mellitus, Endocrinol Diabetes Metab, doi:10.1002/edm2.218
Acharya, Lee, Lee, Lee, Moon, Mortality rate and predictors of mortality in hospitalized COVID-19 Patients with diabetes, Healthcare (Basel), doi:10.3390/healthcare8030338
Agarwal, Schechter, Southern, Crandall, Tomer, Preadmission diabetes-specific risk factors for mortality in hospitalized patients with diabetes and coronavirus disease, Diabetes Care, doi:10.2337/dc20-1543
Aghaaliakbari, Abbasi, Ranjbar, Angiotensin converting enzyme inhibitors, a risk factor of poor outcome in diabetic patients with COVID-19 infection, Iran J Kidney Dis
Ahmed, Kirresh, Robinson, A retrospective study assessing the effect of diabetes on mortality in patients with COVID-19 at a teaching hospital in the United Kingdom, Cureus, doi:10.7759/cureus.13902
Alhakak, Butt, Gerds, Glycated haemoglobin levels among 3295 hospitalized COVID-19 patients, with and without diabetes, and risk of severe infection, admission to an intensive care unit and all-cause mortality, Diabetes Obes Metab, doi:10.1111/dom.14604
Alrashed, Khan, Alhusseini, Severity of COVID-19 infection in ACEI/ARB users in specialty hospitals: a retrospective cohort study, J Infect Public Health, doi:10.1016/j.jiph.2021.03.004
Aon, Alsaeedi, Alzafiri, Stress hyperglycemia ratio as a prognostic marker in diabetic patients hospitalized with COVID-19, Infect Dis Rep, doi:10.3390/idr14050073
Assaad, Hekmat-Joo, Hosry, Insulin use in type 2 diabetic patients: a predictive of mortality in covid-19 infection, Diabetol Metab Syndr, doi:10.1186/s13098-022-00857-2
Bae, Kim, Kim, Shim, Park, Impact of cardiovascular disease and risk factors on fatal outcomes in patients with COVID-19 according to age: a systematic review and meta-analysis, Heart, doi:10.1136/heartjnl-2020-317901
Baral, Tsampasian, Debski, Association between renin-angiotensin-aldosterone system inhibitors and clinical outcomes in patients with COVID-19: a systematic review and metaanalysis, JAMA Netw Open, doi:10.1001/jamanetworkopen.2021.3594
Barrett, Park, Kompaniyets, Intensive care unit admission, mechanical ventilation, and mortality among patients with type 1 diabetes hospitalized for COVID-19 in the U.S, Diabetes Care, doi:10.2337/dc21-060410.2337/dc21-0604
Barron, Bakhai, Kar, Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30272-2
Bello-Chavolla, Bahena-Lopez, Ne, Predicting mortality due to SARS-CoV-2: a mechanistic score relating obesity and diabetes to COVID-19 outcomes in Mexico, J Clin Endocrinol Metab, doi:10.1210/clinem/dgaa346
Borzouei, Mohammadian-Khoshnoud, Omidi, Predictors of COVID-19 related death in diabetes patients: a case-control study in Iran, Diabetes Metab Syndr, doi:10.1016/j.dsx.2021.05.022
Boye, Erdemir, Zimmerman, Risk factors associated with COVID-19 hospitalization and mortality: a large claims-based analysis among people with type 2 diabetes mellitus in the United States, Diabetes Ther, doi:10.1007/s13300-021-01110-1
Butler-Laporte, Nakanishi, Mooser, The effect of angiotensin-converting enzyme levels on COVID-19 susceptibility and severity: a Mendelian randomization study, Int J Epidemiol, doi:10.1093/ije/dyaa229
Calapod, Marin, Onisai, Tribus, Pop CS, Fierbinteanu-Braticevici C (2021) The impact of increased Fib-4 score in patients with type II diabetes mellitus on Covid-19 disease prognosis, Medicina (Kaunas), doi:10.3390/medicina57050434
Cao, Song, Zhuang, Obesity and COVID-19 in adult patients with diabetes, Diabetes, doi:10.2337/db20-0671
Cariou, Goronflot, Rimbert, Routine use of statins and increased COVID-19 related mortality in inpatients with type 2 diabetes: results from the CORONADO study, Diabetes Metab, doi:10.1016/j.diabet.2020.10.001
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Chai, Chen, Li, Effect of elevated fasting blood glucose level on the 1-year mortality and sequelae in hospitalized COVID-19 patients: a bidirectional cohort study, J Med Virol, doi:10.1002/jmv.27737
Charoenngam, Alexanian, Apovian, Holick, Association between hyperglycemia at hospital presentation and hospital outcomes in COVID-19 patients with and without type 2 diabetes: a retrospective cohort study of hospitalized innercity COVID-19 patients, Nutrients, doi:10.3390/nu13072199
Chen, Chen, Wu, Coagulopathy is a major extrapulmonary risk factor for mortality in hospitalized patients with COVID-19 with type 2 diabetes, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2020-001851
Chen, Yang, Cheng, Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care, doi:10.2337/dc20-0660
Chen, Zhao, Huang, Malnutrition predicts poor outcomes in diabetic COVID-19 patients in Huangshi, Hubei. J Biomed Res, doi:10.7555/JBR.35.20210083
Cheng, Yue, Wang, Zhang, Xiang, Hyperglycemia associated with lymphopenia and disease severity of COVID-19 in type 2 diabetes mellitus, J Diabetes Complications, doi:10.1016/j.jdiacomp.2020.107809
Choi, Koo, Seok, ARB/ACEI use and severe COVID-19: a nationwide case-control study. medRxiv: 2020, doi:10.1101/2020.06.12.20129916
Chung, Lee, Ha, The risk of diabetes on clinical outcomes in patients with coronavirus disease 2019: a retrospective cohort study, Diabetes Metab J, doi:10.4093/dmj.2020.0105
Corcillo, Cohen, Li, Crane, Kariyawasam et al., Diabetic retinopathy is independently associated with increased risk of intubation: a single centre cohort study of patients with diabetes hospitalised with COVID-19, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108529
Crouse, Grimes, Li, Might, Ovalle et al., Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes, Front Endocrinol (Lausanne), doi:10.3389/fendo.2020.600439
Dalan, Ang, Tan, The association of hypertension and diabetes pharmacotherapy with COVID-19 severity and immune signatures: an observational study, Eur Heart J Cardiovasc Pharmacother, doi:10.1093/ehjcvp/pvaa098
De Abajo, Rodriguez-Martin, Lerma, Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study, Lancet, doi:10.1016/S0140-6736(20)31030-8
De Miguel-Yanes, Jimenez-Garcia, De, Diez, Impact of type 2 diabetes mellitus on the incidence and outcomes of COVID-19 needing hospital admission according to sex: retrospective cohort study using hospital discharge data in Spain, year 2020, J Clin Med, doi:10.3390/jcm11092654
Demirci, Haymana, Tasci, Higher rate of COVID-19 mortality in patients with type 1 than type 2 diabetes: a nationwide study, Endokrynol Pol, doi:10.5603/EP.a2022.0008
Djuric, Ottone, Vicentini, Diabetes and COVID-19 testing, positivity, and mortality: a population-wide study in Northern Italy, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2022.110051
Do, Kim, Park, Cho, Kang, Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19?, Diabetes Metab, doi:10.1016/j.diabet.2020.10.006
Duan, Li, Li, Association of blood glucose level and prognosis of inpatients with coexistent diabetes and COVID-19, Endocrine, doi:10.1007/s12020-021-02923-7
Elibol, Eren, Erdogan, Factors influencing on development of COVID-19 pneumonia and association with oral anti-diabetic drugs in hospitalized patients with diabetes mellitus, Prim Care Diabetes, doi:10.1016/j.pcd.2021.08.001
Emami, Akbari, Basirat, The role of comorbidities on mortality of COVID-19 in patients with diabetes, Obes Med, doi:10.1016/j.obmed.2021.100352
Emral, Haymana, Demirci, Lower COVID-19 mortality in patients with type 2 diabetes mellitus taking dipeptidyl peptidase-4 inhibitors: results from a Turkish nationwide study, Diabetes Ther, doi:10.1007/s13300-021-01133-8
Erol, Sen, Ozturk, Does DPP-4 inhibitor treatment affect the clinical outcomes of COVID-19 in type 2 diabetes mellitus patients?, North Clin Istanb, doi:10.14744/nci.2022.34341
Fernández-Pombo, Santamaria-Nieto, Rodríguez-Carnero, Factores predictores de formas graves de COVID-19 que requieren hospitalización en pacientes con diabetes mellitus, Galicia Clínica, doi:10.22546/62/2561
Ferrannini, Lund, Benson, Association between use of novel glucose-lowering drugs and COVID-19 hospitalization and death in patients with type 2 diabetes: a nationwide registry analysis, Eur Heart J Cardiovasc Pharmacother, doi:10.1093/ehjcvp/pvac044
Fox, Ruddiman, Lo, The relationship between diabetes and clinical outcomes in COVID-19: a single-center retrospective analysis, Acta Diabetol, doi:10.1007/s00592-020-01592-8
Fu, Hu, Ren, Prognostic factors for COVID-19 hospitalized patients with preexisting type 2 diabetes, Int J Endocrinol, doi:10.1155/2022/9322332
Fukushima, Chubachi, Namkoong, Clinical significance of prediabetes, undiagnosed diabetes and diagnosed diabetes on critical outcomes in COVID-19: integrative analysis from the Japan COVID-19 task force, Diabetes Obes Metab, doi:10.1111/dom.14857
Ghany, Palacio, Dawkins, Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA, Diabetes Metab Syndr, doi:10.1016/j.dsx.2021.02.022
Giorda, Picariello, Tartaglino, From swab testing to health outcomes within the T2DM population: impact of diabetes background on COVID19 progression, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2021.109021
Gregory, Slaughter, Duffus, COVID-19 severity is tripled in the diabetes community: a prospective analysis of the pandemic's impact in type 1 and type 2 diabetes, Diabetes Care, doi:10.2337/dc20-2260
Hadjadj, Saulnier, Ruan, Associations of microvascular complications with all-cause death in patients with diabetes and COVID-19: the CORONADO, ABCD COVID-19 UK national audit and AMERICADO study groups, Diabetes Obes Metab, doi:10.1111/dom.14845
Hammad, Alseoudy, The sex-related discrepancy in laboratory parameters of severe COVID-19 patients with diabetes: a retrospective cohort study, Prim Care Diabetes, doi:10.1016/j.pcd.2021.05.002
Harding, Oviedo, Ali, The bidirectional association between diabetes and long-COVID-19 -a systematic review, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2022.110202
Harris, Ruan, Wild, Association of statin and/ or renin-angiotensin-aldosterone system modulating therapy with mortality in adults with diabetes admitted to hospital with COVID-19: a retrospective multicentre European study, Diabetes Metab Syndr, doi:10.1016/j.dsx.2022.102484
Hayden, Van Der Windt, Cartwright, Cote, Bombardier, Assessing bias in studies of prognostic factors, Ann Intern Med, doi:10.7326/0003-4819-158-4-201302190-00009
Hayek, Robert, Matar, Risk factors for hospital admission among COVID-19 patients with diabetes. A study from Saudi Arabia, Saudi Med J, doi:10.15537/smj.2020.10.25419
Heald, Jenkins, Williams, The risk factors potentially influencing hospital admission in people with diabetes, following SARS-CoV-2 infection: a population-level analysis, Diabetes Ther, doi:10.1007/s13300-022-01230-2
Holman, Knighton, Kar, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30271-0
Huang, Chen, Association of lipid-lowering drugs with COVID-19 outcomes from a Mendelian randomization study, Elife, doi:10.7554/eLife.73873
Huang, Zhu, Bai, Multidimensional analysis of risk factors for the severity and mortality of patients with COVID-19 and diabetes, Infect Dis Ther, doi:10.1007/s40121-020-00359-6
Hui, Li, Tong, The risk factors for mortality of diabetic patients with severe COVID-19: a retrospective study of 167 severe COVID-19 cases in Wuhan, PLoS One, doi:10.1371/journal.pone.0243602
Ikram, Pillay, Hyperglycaemia, diabetes mellitus and COVID-19 in a tertiary hospital in KwaZulu-Natal, J Endocrinol Metab Diabetes South Africa, doi:10.1080/16089677.2021.1997427
Iqbal, Greig, Arshad, Julian, Tan et al., Higher admission activated partial thromboplastin time, neutrophil-lymphocyte ratio, serum sodium, and anticoagulant use predict in-hospital COVID-19 mortality in people with diabetes: findings from two university hospitals in the U.K, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2021.108955
Izzi-Engbeaya, Distaso, Amin, Adverse outcomes in COVID-19 and diabetes: a retrospective cohort study from three London teaching hospitals, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2020-001858
Jayaswal, Singh, Malik, Detrimental effect of diabetes and hypertension on the severity and mortality of COVID-19 infection: a multi-center case-control study from India, Diabetes Metab Syndr, doi:10.1016/j.dsx.2021.102248
Junqueira, Crespo, Ranjbar, FγgammaR-mediated SARS-CoV-2 infection of monocytes activates inflammation, Nature, doi:10.1038/s41586-022-04702-4
Kabootari, Tirtashi, Hasheminia, Clinical features, risk factors and a prediction model for in-hospital mortality among diabetic patients infected with COVID-19: data from a referral centre in Iran, Public Health, doi:10.1016/j.puhe.2021.11.007
Kang, Kong, Body mass index and severity/fatality from coronavirus disease 2019: a nationwide epidemiological study in Korea, PLoS One, doi:10.1371/journal.pone.0253640
Khalili, Moradi, Kharazmi, Raoufi, Sistanizad et al., Comparison of mortality rate and severity of pulmonary involvement in coronavirus disease-2019 adult patients with and without type 2 diabetes: a cohort study, Can J Diabetes, doi:10.1016/j.jcjd.2020.10.014
Khalili, Sabaghian, Sedaghat, Soroureddin, Askari et al., Prevalence, risk factors and outcomes associated with acute kidney injury in patients hospitalized for COVID-19: a comparative study between diabetic and nondiabetic patients, J Diabetes Res, doi:10.1155/2021/6666086
Khunti, Knighton, Zaccardi, Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00050-4
Khunti, Ruan, Davies, Association between SGLT2 inhibitor treatment and diabetic ketoacidosis and mortality in people with type 2 diabetes admitted to hospital with COVID-19, Diabetes Care, doi:10.2337/dc22-0357
Kim, Jeon, Kim, The clinical characteristics and outcomes of patients with moderate-to-severe coronavirus disease 2019 infection and diabetes in Daegu, South Korea, Diabetes Metab J, doi:10.4093/dmj.2020.0146
Kollias, Kyriakoulis, Kyriakoulis, Statin use and mortality in COVID-19 patients: updated systematic review and meta-analysis, Atherosclerosis, doi:10.1016/j.atherosclerosis.2021.06.911
Kristan, Kim, Nelson, Predictors of severe COVID-19 in patients with diabetes: a multicenter review, Endocr Pract, doi:10.1016/j.eprac.2021.05.011
Lalau, Al-Salameh, Hadjadj, Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19, Diabetes Metab, doi:10.1016/j.diabet.2020.101216
Lampasona, Secchi, Scavini, Antibody response to multiple antigens of SARS-CoV-2 in patients with diabetes: an observational cohort study, Diabetologia, doi:10.1007/s00125-020-05284-4
Laurenzi, Caretto, Molinari, Pre-existing diabetes and COVID-associated hyperglycaemia in patients with COVID-19 pneumonia, Biology (Basel), doi:10.3390/biology10080754
Lazarus, Wangsaputra, Tahapary, High admission blood glucose independently predicts poor prognosis in COVID-19 patients: a systematic review and doseresponse meta-analysis, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108561
Lee, Ahn, Park, Beneficial effect of statins in COVID-19-related outcomes-brief report: a national populationbased cohort study, Arterioscler Thromb Vasc Biol, doi:10.1161/ATVBAHA.120.315551
Lei, Lin, Pi, Clinical features and risk factors of ICU admission for COVID-19 patients with diabetes, J Diabetes Res, doi:10.1155/2020/5237840
Leon-Pedroza, Rodriguez-Cortes, Flores-Mejia, Gaona-Aguas, Gonzalez-Chavez, Impact of metabolic syndrome in the clinical outcome of disease by SARS-COV-2, Arch Med Res, doi:10.1016/j.arcmed.2021.04.001
Leong, Cole, Brenner, Meigs, Florez et al., Cardiometabolic risk factors for COVID-19 susceptibility and severity: a Mendelian randomization analysis, PLoS Med, doi:10.1371/journal.pmed.1003553
Li, Han, Alwalid, Baseline characteristics and risk factors for short-term outcomes in 132 COVID-19 patients with diabetes in Wuhan China: a retrospective study, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108299
Li, Wei, Li, Metformin use in diabetes prior to hospitalization: effects on mortality in Covid-19, Endocr Pract, doi:10.4158/EP-2020-0466
Liu, Bai, Han, The association of diabetes and the prognosis of COVID-19 patients: a retrospective study, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108386
Liu, Ni, Mental and neurological disorders and risk of COVID-19 susceptibility, illness severity and mortality: a systematic review, meta-analysis and call for action, EClinicalMedicine, doi:10.1016/j.eclinm.2021.101111
Liu, Zhang, Hu, Liu, Huang, The role of neutrophil-lymphocyte ratio and lymphocyte-monocyte ratio in the prognosis of type 2 diabetics with COVID-19, Scott Med J, doi:10.1177/0036933020953516
Llanera, Wilmington, Shoo, Clinical characteristics of COVID-19 patients in a regional population with diabetes mellitus: the ACCREDIT study, Front Endocrinol (Lausanne), doi:10.3389/fendo.2021.777130
Llaurado, Vlacho, Wargny, The association between macrovascular complications and intensive care admission, invasive mechanical ventilation, and mortality in people with diabetes hospitalized for coronavirus disease-2019 (COVID-19), Cardiovasc Diabetol, doi:10.1186/s12933-022-01657-8
Lombardi, Agarwal, Schechter, Tomer, In-hospital hyperglycemia is associated with worse outcomes in patients admitted with COVID-19, Diabetes Care, doi:10.2337/dc22-0708
Longmore, Miller, Bekkering, Diabetes and overweight/obesity are independent, nonadditive risk factors for in-hospital severity of COVID-19: an international, multicenter retrospective meta-analysis, Diabetes Care, doi:10.2337/dc20-2676
Lopez-Huamanrayme, Garate-Chirinos, Espinoza-Morales, Association between hyperglycemia treatment and mortality in patients with diabetes and COVID-19 in a Peruvian hospital: a retrospective cohort study, J Clin Transl Endocrinol, doi:10.1016/j.jcte.2021.100265
Luk, Yip, Zhang, Glucose-lowering drugs and outcome from COVID-19 among patients with type 2 diabetes mellitus: a population-wide analysis in Hong Kong, BMJ Open, doi:10.1136/bmjopen-2021-052310
Ma, Patel, Vemparala, Krishnamurthy, Metformin is associated with favorable outcomes in patients with COVID-19 and type 2 diabetes mellitus, Sci Rep, doi:10.1038/s41598-022-09639-2
Madaschi, Resmini, Bonfadini, Predictive markers for clinical outcomes in a cohort of diabetic patients hospitalized for COVID-19, Diabetol Metab Syndr, doi:10.1186/s13098-022-00941-7
Mahamat-Saleh, Fiolet, Rebeaud, Diabetes, hypertension, body mass index, smoking and COVID-19-related mortality: a systematic review and meta-analysis of observational studies, BMJ Open, doi:10.1136/bmjopen-2021-052777
Mannucci, Vitturi, Benacchio, Infection rates and impact of glucose lowering medications on the clinical course of COVID-19 in people with type 2 diabetes: a retrospective observational study, Diabetes Metab Syndr Obes, doi:10.2147/DMSO.S385646
Marimuthu, Kunnavil, Satyanarayana, Clinical presentation and mortality risk factors for COVID-19 among diabetic patients in a tertiary care center in South India, Indian J Tuberc, doi:10.1016/j.ijtb.2021.08.015
Mcgurnaghan, Weir, Bishop, Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30405-8
Mehta, Kohn, Koliwad, Rushakoff, Lack of association between either outpatient or inpatient glycemic control and COVID-19 illness severity or mortality in patients with diabetes, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2021-002203
Meijer, Hoekstra, Van Den Oever, Treatment with a DPP-4 inhibitor at time of hospital admission for COVID-19 is not associated with improved clinical outcomes: data from the COVID-PREDICT cohort study in The Netherlands, J Diabetes Metab Disord, doi:10.1007/s40200-021-00833-z
Merzon, Green, Shpigelman, Haemoglobin A1c is a predictor of COVID-19 severity in patients with diabetes, Diabetes Metab Res Rev, doi:10.1002/dmrr.3398
Mirani, Favacchio, Carrone, Impact of comorbidities and glycemia at admission and dipeptidyl peptidase 4 inhibitors in patients with type 2 diabetes with COVID-19: a case series from an academic hospital in Lombardy, Italy, Diabetes Care, doi:10.2337/dc20-1340
Mohamed, Gouda, Hanafy, Clinical, laboratory and radiological predictors of unfavorable hospital admission course for diabetic patients with COVID-19, Egypt J Hosp Med, doi:10.21608/ejhm.2021.165528
Mondal, Dasgupta, Lodh, Predictors of new-onset diabetic ketoacidosis in patients with moderate to severe COVID-19 receiving parenteral glucocorticoids: a prospective single-centre study among Indian type 2 diabetes patients, Diabetes Metab Syndr, doi:10.1016/j.dsx.2021.03.022
Mondal, Dasgupta, Lodh, Stress hyperglycemia ratio, rather than admission blood glucose, predicts inhospital mortality and adverse outcomes in moderate-to severe COVID-19 patients, irrespective of pre-existing glycemic status, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2022.109974
Morsali, Rezazadeh-Gavgani, Oladghaffari, Effects of underlying heart failure on outcomes of COVID-19; a systematic review and meta-analysis, Rom J Intern Med, doi:10.2478/rjim-2022-0021
Morse, Gay, Korwek, Hyperglycaemia increases mortality risk in non-diabetic patients with COVID-19 even more than in diabetic patients, Endocrinol Diabetes Metab, doi:10.1002/edm2.291
Myers, Kim, Zhu, Liu, Qiu et al., Predictors of mortality in a multiracial urban cohort of persons with type 2 diabetes and novel coronavirus 19, J Diabetes, doi:10.1111/1753-0407.13158
Nagarajan, Krishnamoorthy, Rajaa, Hariharan, COVID-19 severity and mortality among chronic liver disease patients: a systematic review and meta-analysis, doi:10.5888/pcd19.210228
Nguyen, Ho, Nguyen, Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: a meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196
Nikniaz, Somi, Dinevari, Taghizadieh, Mokhtari, Diabesity associates with poor COVID-19 outcomes among hospitalized patients, J Obes Metab Syndr, doi:10.7570/jomes20121
Numaguchi, Kurajoh, Hiura, Glycated hemoglobin level on admission associated with progression to severe disease in hospitalized patients with non-severe coronavirus disease 2019, J Diabetes Investig, doi:10.1111/jdi.13845
Nyland, Raja-Khan, Bettermann, Diabetes, drug treatment, and mortality in COVID-19: a multinational retrospective cohort study, Diabetes, doi:10.2337/db21-0385
O'malley, Ebekozien, Desimone, COVID-19 Hospitalization in adults with type 1 diabetes: results from the T1D Exchange Multicenter Surveillance Study, J Clin Endocrinol Metab, doi:10.1210/clinem/dgaa825
Oh, Song, Metformin use and risk of COVID-19 among patients with type II diabetes mellitus: an NHIS-COVID-19 database cohort study, Acta Diabetol, doi:10.1007/s00592-020-01666-7
Ojeda-Fernandez, Foresta, Macaluso, Metformin use is associated with a decrease in the risk of hospitalization and mortality in COVID-19 patients with diabetes: a population-based study in Lombardy, Diabetes Obes Metab, doi:10.1111/dom.14648
Orioli, Servais, Belkhir, Clinical characteristics and short-term prognosis of in-patients with diabetes and COVID-19: a retrospective study from an academic center in Belgium, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.12.020
Ortega, Corcoy, Gratacos, Risk factors for severe outcomes in people with diabetes hospitalised for COVID-19: a cross-sectional database study, BMJ Open, doi:10.1136/bmjopen-2021-051237
Ouchi, Vilaplana-Carnerero, De Dios, Giner-Soriano, Morros, Antidiabetic treatment and COVID-19 Outcomes: a population-based cohort study in primary health care in Catalonia during the first wave of the pandemic, Prim Care Diabetes, doi:10.1016/j.pcd.2022.10.001
Page, Mckenzie, Bossuyt, The PRISMA 2020 statement: an updated guideline for reporting systematic reviews, BMJ, doi:10.1136/bmj.n71
Palazzuoli, Mancone, Ferrari, Antecedent administration of angiotensin-converting enzyme inhibitors or angiotensin II receptor antagonists and survival after hospitalization for COVID-19 syndrome, J Am Heart Assoc, doi:10.1161/JAHA.120.017364
Patel, Klek, Peragallo-Dittko, Correlation of hemoglobin A1C and outcomes in patients hospitalized with COVID-19, Endocr Pract, doi:10.1016/j.eprac.2021.07.008
Pazoki, Chichagi, Hadadi, Association of clinical characteristics, antidiabetic and cardiovascular agents with diabetes mellitus and COVID-19: a 7-month follow-up cohort study, J Diabetes Metab Disord, doi:10.1007/s40200-021-00901-4
Pazoki, Keykhaei, Kafan, Risk indicators associated with in-hospital mortality and severity in patients with diabetes mellitus and confirmed or clinically suspected COVID-19, J Diabetes Metab Disord, doi:10.1007/s40200-020-00701-2
Perez-Belmonte, Torres-Pena, Lopez-Carmona, Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: a nationwide cohort study, BMC Med, doi:10.1186/s12916-020-01832-2
Petrakis, Panagopoulos, Trypsianis, Papazoglou, Papanas, Glucose on admission: unfavourable effects on hospitalisation and outcomes in type 2 diabetes mellitus patients with COVID-19 pneumonia, Exp Clin Endocrinol Diabetes, doi:10.1055/a-1686-8738
Pettrone, Burnett, Link-Gelles, Characteristics and risk factors of hospitalized and nonhospitalized COVID-19 patients, Emerg Infect Dis, doi:10.3201/eid2704.204709
Phan, Boussouar, Lucidarme, Cardiac adipose tissue volume and IL-6 level at admission are complementary predictors of severity and short-term mortality in COVID-19 diabetic patients, Cardiovasc Diabetol, doi:10.1186/s12933-021-01327-1
Pulido-Perez, Angeles, Hernandez-Hernandez, Torres-Rasgado, Romero, Renal function, serum magnesium levels and mortality in COVID-19 patients with type 2 diabetes, Magnes Res, doi:10.1684/mrh.2021.0481
Ramesh, Rajesh, Varghese, Reddy, Calculated plasma osmolality at hospital admission correlates well with eGFR and D-Dimer, a simple outcome predictor and guiding tool for management of severe COVID-19 patients, Diabetes Metab Syndr, doi:10.1016/j.dsx.2021.102240
Ramos-Rincon, Perez-Belmonte, Carrasco-Sanchez, Cardiometabolic therapy and mortality in very old patients with diabetes hospitalized due to COVID-19, J Gerontol A Biol Sci Med Sci, doi:10.1093/gerona/glab124
Rastad, Ejtahed, Mahdavi-Ghorabi, Factors associated with the poor outcomes in diabetic patients with
Rastad, Karim, Ejtahed, Risk and predictors of in-hospital mortality from COVID-19 in patients with diabetes and cardiovascular disease, Diabetol Metab Syndr, doi:10.1186/s13098-020-00565-9
Reyes, Hache-Marliere, Karamanis, Assessment of the association of COPD and asthma with in-hospital mortality in patients with COVID-19. A Systematic review, meta-analysis, and meta-regression analysis, J Clin Med, doi:10.3390/jcm10102087
Rezaei, Montazeri, Malekpour, COVID-19 in patients with diabetes: factors associated with worse outcomes, J Diabetes Metab Disord, doi:10.1007/s40200-021-00910-3
Rhee, Lee, Nam, Kyoung, Shin et al., Effects of a DPP-4 Inhibitor and RAS blockade on clinical outcomes of patients with diabetes and COVID-19, Diabetes Metab J, doi:10.4093/dmj.2020.0206
Riahi, Sombra, Lo, Insulin use, diabetes control, and outcomes in patients with COVID-19, Endocr Res, doi:10.1080/07435800.2020.1856865
Rosoff, Yoo, Lohoff, Smoking is significantly associated with increased risk of COVID-19 and other respiratory infections, Commun Biol, doi:10.1038/s42003-021-02685-y
Roussel, Darmon, Pichelin, Use of dipeptidyl peptidase-4 inhibitors and prognosis of COVID-19 in hospitalized patients with type 2 diabetes: a propensity score analysis from the CORONADO study, Diabetes Obes Metab, doi:10.1111/dom.14324
Ruan, Ryder, De, A UK nationwide study of people with type 1 diabetes admitted to hospital with COVID-19 infection, Diabetologia, doi:10.1007/s00125-021-05463-x
Sadidi, Zare, Nasrollahzadehsabet, Dastan, Khah et al., The roles of dipeptidyl peptidase-4 inhibitors in prognosis of COVID-19 infection in patients with type 2 diabetes mellitus, J Res Med Sci, doi:10.4103/jrms.jrms_71_22
Sarigumba, Aragon, Kanapi, Baseline glycemic status and outcome of persons with type 2 diabetes with COVID-19 infections: a single-center retrospective study, J ASEAN Fed Endocr Soc, doi:10.15605/jafes.036.01.06
Sathish, Kapoor, Cao, Tapp, Zimmet, Proportion of newly diagnosed diabetes in COVID-19 patients: a systematic review and meta-analysis, Diabetes Obes Metab, doi:10.1111/dom.14269
Satman, Demirci, Haymana, Unexpectedly lower mortality rates in COVID-19 patients with and without type 2 diabetes in Istanbul, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2021.108753
Savarese, Benson, Sundstrom, Lund, Association between renin-angiotensin-aldosterone system inhibitor use and COVID-19 hospitalization and death: a 1.4 million patient nationwide registry analysis, Eur J Heart Fail, doi:10.1002/ejhf.206010.1002/ejhf.2060
Saygili, Karakilic, Mert, Sener, Mirci, Preadmission usage of metformin and mortality in COVID-19 patients including the post-discharge period, Ir J Med Sci, doi:10.1007/s11845-021-02823-9
Schlesinger, Neuenschwander, Risk phenotypes of diabetes and association with COVID-19 severity and death: a living systematic review and metaanalysis, Diabetologia, doi:10.1007/s00125-021-05458-8
Schunemann, Cuello, Akl, GRADE guidelines: 18. How ROBINS-I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence, J Clin Epidemiol, doi:10.1016/j.jclinepi.2018.01.012
Seiglie, Platt, Cromer, Diabetes as a risk factor for poor early outcomes in patients hospitalized with COVID-19, Diabetes Care, doi:10.2337/dc20-1506
Shah, Owens, Franklin, Jani, Kumar et al., Baseline use of angiotensin-converting enzyme inhibitor/AT1 blocker and outcomes in hospitalized coronavirus disease 2019 African-American patients, J Hypertens, doi:10.1097/HJH.0000000000002584
Shang, Liu, Ni, Evaluation of prognostic indicators for COVID•19 patients with diabetes, Med J Wuhan Univ
Shang, Wang, Zhang, The relationship between diabetes mellitus and COVID-19 prognosis: a retrospective cohort study in Wuhan. China, Am J Med, doi:10.1016/j.amjmed.2020.05.033
Shauly-Aharonov, Shafrir, Paltiel, Both high and low pre-infection glucose levels associated with increased risk for severe COVID-19: new insights from a population-based study, PLoS One, doi:10.1371/journal.pone.0254847
Shestakova, Vikulova, Elfimova, Deviatkin, Dedov et al., Risk factors for COVID-19 case fatality rate in people with type 1 and type 2 diabetes mellitus: a nationwide retrospective cohort study of 235,248 patients in the Russian Federation, Front Endocrinol (Lausanne), doi:10.3389/fendo.2022.909874
Shi, Zhang, Jiang, Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: a two-center, retrospective study, Diabetes Care, doi:10.2337/dc20-0598
Shukla, Tchang, Lam, Preadmission predictors of severe COVID-19 in patients with diabetes mellitus, J Diabetes Complications, doi:10.1016/j.jdiacomp.2021.107967
Silverii, Monami, Cernigliaro, Are diabetes and its medications risk factors for the development of COVID-19? Data from a population-based study in Sicily, Nutr Metab Cardiovasc Dis, doi:10.1016/j.numecd.2020.09.028
Singh, Gillies, Singh, Prevalence of co-morbidities and their association with mortality in patients with COVID-19: a systematic review and meta-analysis, Diabetes Obes Metab, doi:10.1111/dom.14124
Singh, Malik, Patel, Kidney disease and COVID-19 disease severity-systematic review and meta-analysis, Clin Exp Med, doi:10.1007/s10238-021-00715-x
Smati, Tramunt, Wargny, Relationship between obesity and severe COVID-19 outcomes in patients with type 2 diabetes: results from the CORONADO study, Diabetes Obes Metab, doi:10.1111/dom.14228
Solerte, 'addio, Trevisan, Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and COVID-19: a multicenter, case-control, retrospective, observational study, Diabetes Care, doi:10.2337/dc20-1521
Soliman, Abdelaziz, Fathy, Impact of vitamin D therapy on the progress COVID-19: six weeks follow-up study of vitamin D deficient elderly diabetes patients, Proc Singapore Healthc, doi:10.1177/20101058211041405
Sonmez, Demirci, Haymana, Clinical characteristics and outcomes of COVID-19 in patients with type 2 diabetes in Turkey: a nationwide study (TurCoviDia), J Diabetes, doi:10.1111/1753-0407.13171
Souza, Quintao, Soares, Survival of patients with diabetes mellitus hospitalized for acute respiratory syndrome due to COVID-19, Rev Inst Med Trop Sao Paulo, doi:10.1590/S1678-9946202264074
Stevens, Bogun, Mcmahon, Diabetic ketoacidosis and mortality in COVID-19 infection, Diabetes Metab, doi:10.1016/j.diabet.2021.101267
Strollo, Maddaloni, Dauriz, Pedone, Buzzetti et al., Use of DPP4 inhibitors in Italy does not correlate with diabetes prevalence among COVID-19 deaths, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108444
Tallon, Ebekozien, Sanchez, Impact of diabetes status and related factors on COVID-19-associated hospitalization: a nationwide retrospective cohort study of 116,370 adults with SARS-CoV-2 infection, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2022.110156
Tamura, Said, De Freitas, Rubio, Outcome and death risk of diabetes patients with Covid-19 receiving prehospital and in-hospital metformin therapies, Diabetol Metab Syndr, doi:10.1186/s13098-021-00695-8
Tian, Heald, Stedman, Age of people with type 2 diabetes and the risk of dying following SARS-CoV-2 infection, Int J Clin Pract, doi:10.1111/ijcp.14053
Tramunt, Smati, Coudol, Sex disparities in COVID-19 outcomes of inpatients with diabetes: insights from the CORO-NADO study, Eur J Endocrinol, doi:10.1530/EJE-21-0068
Tuan, Lennon, Zhang, Macherla, Zgierska, Risks of severe COVID-19 outcomes among patients with diabetic polyneuropathy in the United States, J Public Health Manag Pract, doi:10.1097/PHH.0000000000001587
Valle, Rodriguez, Camina, Martinez-Olmos, Ortola et al., At-admission HbA(1c) levels in hospitalized COVID-19 participants with and without known diabetes, Clin Chim Acta, doi:10.1016/j.cca.2022.05.027
Vargas-Vazquez, Bello-Chavolla, Ortiz-Brizuela, Impact of undiagnosed type 2 diabetes and pre-diabetes on severity and mortality for SARS-CoV-2 infection, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2020-002026
Vasbinder, Anderson, Shadid, Inflammation, hyperglycemia, and adverse outcomes in individuals with diabetes mellitus hospitalized for COVID-19, Diabetes Care, doi:10.2337/dc21-2102
Venkatesulu, Chandrasekar, Girdhar, A systematic review and meta-analysis of cancer patients affected by a novel coronavirus, JNCI Cancer Spectr, doi:10.1093/jncics/pkaa102
Wander, Lowy, Beste, Prior glucose-lowering medication use and 30-day outcomes among 64,892 veterans with diabetes and COVID-19, Diabetes Care, doi:10.2337/dc21-1351
Wang, Glicksberg, Nadkarni, Vashishth, Evaluation and management of COVID-19-related severity in people with type 2 diabetes, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2021-002299
Wang, Liu, Li, Impacts of type 2 diabetes on disease severity, therapeutic effect, and mortality of patients with
Wang, Zhang, Li, Prognostic value of leucocyte to high-density lipoprotein-cholesterol ratios in COVID-19 patients and the diabetes subgroup, Front Endocrinol (Lausanne), doi:10.3389/fendo.2021.727419
Wargny, Potier, Gourdy, Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study, Diabetologia, doi:10.1007/s00125-020-05351-w
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wong, Hall, Vaddavalli, Glycemic control and clinical outcomes in U.S. patients with COVID-19: data from the National COVID Cohort Collaborative (N3C) Database, Diabetes Care, doi:10.2337/dc21-218610.2337/dc21-2186
Wong, Lui, Lui, Metformin use in relation to clinical outcomes and hyperinflammatory syndrome among COVID-19 patients with type 2 diabetes: a propensity score analysis of a territory-wide cohort, Front Endocrinol (Lausanne), doi:10.3389/fendo.2022.810914
Wong, Lui, Lui, Use of DPP4i reduced odds of clinical deterioration and hyperinflammatory syndrome in COVID-19 patients with type 2 diabetes: propensity score analysis of a territory-wide cohort in Hong Kong, Diabetes Metab, doi:10.1016/j.diabet.2021.101307
Wong, Tan, Zheng, A systematic review and meta-analysis of the COVID-19 associated liver injury, Ann Hepatol, doi:10.1016/j.aohep.2020.08.064
Wu, Zhou, Wang, Association analysis of hyperlipidemia with the 28-day all-cause mortality of COVID-19 in hospitalized patients, Chin Med Sci J, doi:10.24920/003866
Xiao, He, Xu, Major characteristics of severity and mortality in diabetic patients with COVID-19 and establishment of severity risk score, Front Med (Lausanne), doi:10.3389/fmed.2021.655604
Xu, Wang, Wang, The impact of type 2 diabetes and its management on the prognosis of patients with severe COVID-19, J Diabetes, doi:10.1111/1753-0407.13084
Yan, Valdes, Vijay, Role of drugs used for chronic disease management on susceptibility and severity of COVID-19: a large case-control study, Clin Pharmacol Ther, doi:10.1002/cpt.2047
Yeh, Kraschnewski, Kong, Hospitalization and mortality in patients with COVID-19 with or at risk of type 2 diabetes: data from five health systems in Pennsylvania and Maryland, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2022-002774
Yeung, Zhao, Schooling, Evaluation of glycemic traits in susceptibility to COVID-19 risk: a Mendelian randomization study, BMC Med, doi:10.1186/s12916-021-01944-3
Yoo, Choi, Park, Seo, Ahn et al., Glycated albumin and glycated albumin/HbA1c predict the progression of coronavirus disease 2019 from mild to severe disease in Korean patients with type 2 diabetes, J Clin Med, doi:10.3390/jcm11092327
You, Lee, Sy, Clinical outcomes of COVID-19 patients with type 2 diabetes: a population-based study in Korea, Endocrinol Metab (Seoul), doi:10.3803/EnM.2020.787
Zeltyn-Abramov, Lysenko, Frolova, Risk factors of adverse outcome of COVID-19 and experience of tocilizumab administration in patients on maintenance hemodialysis due to diabetic kidney disease, Diabetes Mellitus, doi:10.14341/dm12688
Zhan, Zhang, Wang, Short-and long-term prognosis of glycemic control in COVID-19 patients with type 2 diabetes, QJM, doi:10.1093/qjmed/hcac020
Zhang, Wang, Zhu, Risk factors for poor outcomes of diabetes patients with COVID-19: a single-center, retrospective study in early outbreak in China, Front Endocrinol (Lausanne), doi:10.3389/fendo.2020.571037
Zhang, Wei, Chen, Wan, Chen, Clinical analysis of risk factors for severe COVID-19 patients with type 2 diabetes, J Diabetes Complications, doi:10.1016/j.jdiacomp.2020.107666
Zhu, She, Cheng, Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.04.021
