Metformin and Covid-19: a systematic review of systematic reviews with meta-analysis
et al., Acta Biomedica Atenei Parmensis, doi:10.23750/abm.v94iS3.14405, Aug 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
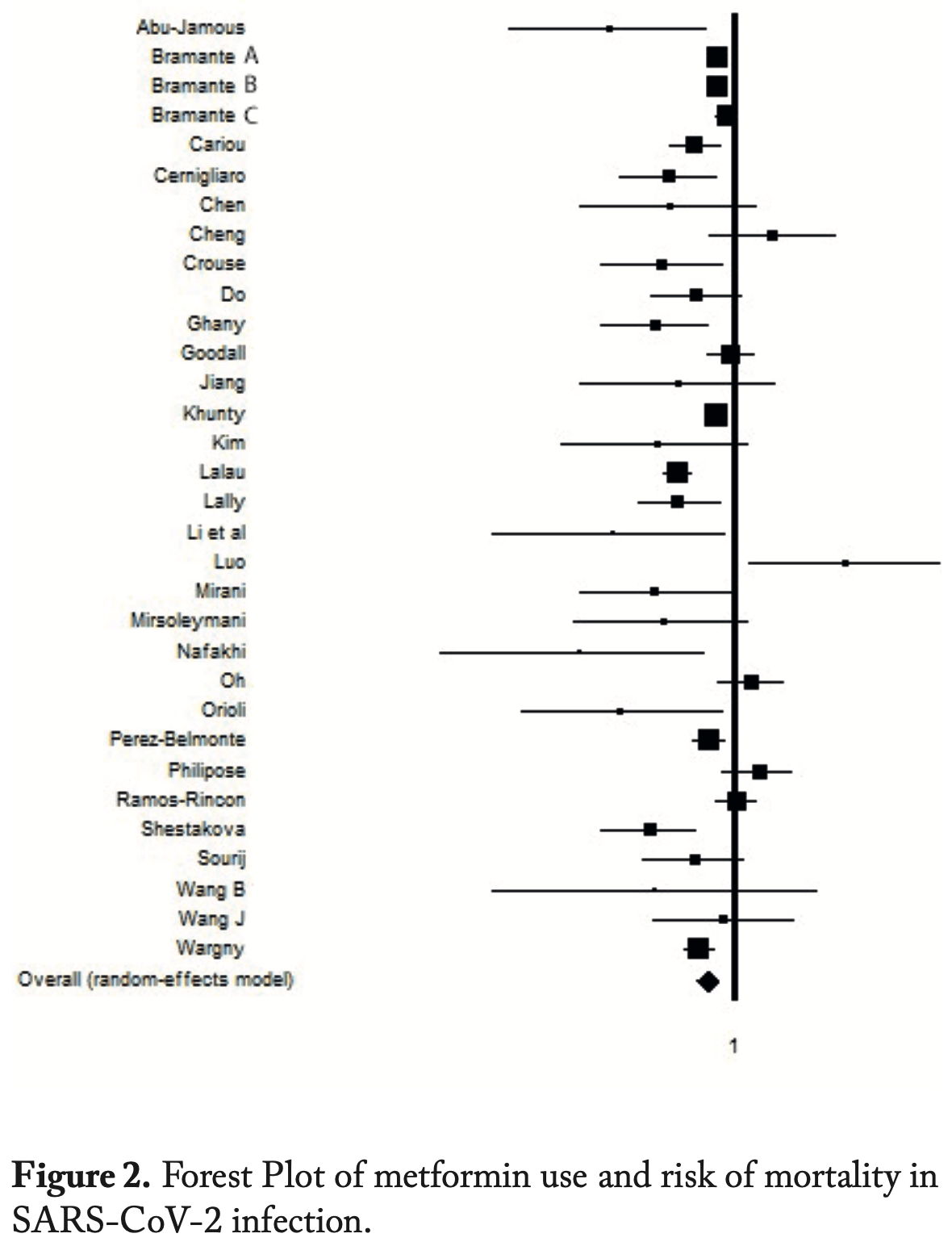
Systematic review and meta analysis of 36 studies showing significantly lower COVID-19 mortality and severity with metformin use.
24 meta-analyses show significant improvements with metformin for mortality1-23,
hospitalization7,13,23 ,
progression1, and
severity8,9,13 .
Currently there are 110 metformin for COVID-19 studies, showing 36% lower mortality [32‑40%], 29% lower ventilation [12‑43%], 19% lower ICU admission [8‑28%], 17% lower hospitalization [11‑23%], and 5% fewer cases [-4‑13%].
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments24.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 31.0% lower, OR 0.69, p < 0.001, RR approximated with OR.
|
|
risk of severe case, 20.0% lower, OR 0.80, p = 0.03, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Yang et al., The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus, Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2021.108977.
2.
Lukito et al., The Effect of Metformin Consumption on Mortality in Hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2020.11.006.
3.
Kow et al., Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis, Journal of Medical Virology, doi:10.1002/jmv.26498.
4.
Hariyanto et al., Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection, Obesity Medicine, doi:10.1016/j.obmed.2020.100290.
5.
Ma et al., Is metformin use associated with low mortality in patients with type 2 diabetes mellitus hospitalized for COVID-19? a multivariable and propensity score-adjusted meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0282210.
6.
Parveen et al., Association of Metformin with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis, Annals of the National Academy of Medical Sciences (India), doi:10.1055/s-0042-1760353.
7.
Li et al., Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Medicine, doi:10.3389/fmed.2021.704666.
8.
Schlesinger et al., Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis, Diabetologia, doi:10.1007/s00125-023-05928-1.
9.
Petrelli et al., Metformin and Covid-19: a systematic review of systematic reviews with meta-analysis, Acta Biomedica Atenei Parmensis, doi:10.23750/abm.v94iS3.14405.
10.
Oscanoa et al., Metformin therapy and severity and mortality of SARS-CoV-2 infection: a meta-analysis, Clinical Diabetology, doi:10.5603/DK.a2021.0035.
11.
Kan et al., Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2021.708494.
12.
Poly et al., Metformin Use Is Associated with Decreased Mortality in COVID-19 Patients with Diabetes: Evidence from Retrospective Studies and Biological Mechanism, Journal of Clinical Medicine, doi:10.3390/jcm10163507.
13.
Song et al., The Effect of Antihyperglycemic Medications on COVID-19: A Meta-analysis and Systematic Review from Observational Studies, Therapeutic Innovation & Regulatory Science, doi:10.1007/s43441-024-00633-6.
14.
Ganesh et al., Does metformin affect outcomes in COVID‐19 patients with new or pre‐existing diabetes mellitus? A systematic review and meta‐analysis, British Journal of Clinical Pharmacology, doi:10.1111/bcp.15258.
15.
Nassar et al., Noninsulin‐based antihyperglycemic medications in patients with diabetes and COVID‐19: A systematic review and meta‐analysis, Journal of Diabetes, doi:10.1111/1753-0407.13359.
16.
Zhan et al., Effect of Antidiabetic Therapy on Clinical Outcomes of COVID-19 Patients With Type 2 Diabetes: A Systematic Review and Meta-Analysis, Annals of Pharmacotherapy, doi:10.1177/10600280221133577.
17.
Nguyen et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196.
18.
Han et al., Association Between Anti-diabetic Agents and Clinical Outcomes of COVID-19 in Patients with Diabetes: A Systematic Review and Meta-Analysis, Archives of Medical Research, doi:10.1016/j.arcmed.2021.08.002.
19.
Chen et al., The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2022.895458.
20.
Scheen, A., Metformin and COVID-19: From cellular mechanisms to reduced mortality, Diabetes & Metabolism, doi:10.1016/j.diabet.2020.07.006.
21.
Sun et al., Is Metformin Use Associated With a Decreased Mortality for COVID-19 Diabetic Patients? A Meta-Analysis, Journal of the Endocrine Society, doi:10.1210/jendso/bvab048.709.
22.
Keels et al., Antidiabetic agent use and clinical outcomes in patients with diabetes hospitalized for COVID-19: a systematic review and meta-analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2024.1482853.
Petrelli et al., 30 Aug 2023, retrospective, USA, peer-reviewed, 7 authors.
Metformin and Covid-19: a systematic review of systematic reviews with meta-analysis
doi:10.23750/abm.v94iS3.14405
Introduction: the COVID-19 infection, caused by severe Coronavirus 2 syndrome (Sars-Cov-2), immediately appeared to be the most tragic global pandemic event of the twentieth century. Right from the start of the pandemic, diabetic patients treated with metformin experienced a reduction in mortality and complications from COVID-19 compared to those with different treatments or no treatment. Objective: The main objective of the study was to observe the effects of metformin in diabetic hospitalized subjects infected with COVID-19. Specifically, the outcomes of hospitalization in Intensive Care Units or death were examined. Materials and Methods: A specific research PICOS was developed and the Pubmed, Embase and Scopus databases were consulted down to April 30, 2022. To estimate the extent of the metformin effect and risk of severity in SARS-CoV-2 infection, the Odd Ratio (OR) with 95% Confidence Interval (CI) published by the authors of the selected systematic reviews was used. Results: from five systematic reviews 36 studies were selected. The final meta-analysis showed that thanks to treatment with metformin, Type II Diabetes (DM2) patients affected by COVID-19 had protection against risk of disease severity, complications (SE 0.80; CI 95%: 0.61 -0.78; I 2 : 70.5%) and mortality (SE 0.69; CI 95%: 0.65 -0.98; I 2 : 53,6%). Conclusions: More indepth studies on the use of metformin, compared to other molecules, may be required to understand the real protective potential of the drug against negative outcomes caused by
Conflict of Interest statement: Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
Ethics approval and consent to participate: Not applicable Consent for publication: All the authors have read the paper and agreed to submit the paper.
Competing interests: The authors declare no competing interests.
Funding: Not applicable Authors' contributions : FP and GC designed and conducted research, analyzed data and wrote the paper. All authors approved the final manuscript.
References
Abu-Jamous, Anisimovich, Baxter, Associations of comorbidities and medications with COVID-19 outcome: a retrospective analysis of real-world evidence data, doi:10.1101/2020.08.20.20174169
Acito, Bartolini, Ceccarini, Imbalance in the antioxidant defence system and pro-genotoxic status induced by high glucose concentrations: In vitro testing in human liver cells, Toxicol In Vitro, doi:10.1016/j.tiv.2020.105001
Alleva, Leigheb, Rinaldi, Achieving quadruple aim goals through clinical networks: A systematic review, Journal of Healthcare Quality Research, doi:10.1016/j.jhqr.2018.10.010
Altınbilek, Öztürk, Atasoy, Analysis of the Patients Who Admitted To A Turkish Emergency Department During COVID-19 Pandemic, Acta Biomed, doi:10.23750/abm.v91i4.10227
Bas, Metin, Sevinç, The Effect of Diabetes Mellitus on Mortality in Patients Hospitalized Intensive Care Unit in Covid-19 Pandemic, Acta Biomed, doi:10.23750/abm.v93i3.11880
Bramante, Ingraham, Murray, Metformin and risk of mortality in patients hospitalised with COV-ID19: a retrospective cohort analysis, The Lancet Healthy Longevity, doi:10.1016/s2666-7568
Bramante, Ingraham, Murray, Observational study of metformin and risk of mortality in patients hospitalized with covid-19, MedRxiv Prepr Serv Heal Sci, doi:10.1101/2020.06.19.20135095.2020.06.19.20135095
Bramante, Tignanelli, Dutta, Non-alcoholic fatty liver disease (NAFLD) and risk of hospitalization for COVID-19. medRxiv [Preprint], doi:10.1101/2020.09.01.20185850
Cangelosi, Grappasonni, Pantanetti, Nurse Case Manager Lifestyle Medicine (NCMLM) in the Type Two Diabetes patient concerning post COVID-19 Pandemic management: Integrated-Scoping literature review, Ann Ig, doi:10.7416/ai.2022.2500
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Cernigliaro, Allotta, Scondotto, Can diabetes and its related hypoglycemic drug treatment be considered risk factors for health outcomes in COVID-19 patients? The results of a study in the population residing in Sicily Region (Southern Italy), Epidemiol Prev, doi:10.19191/EP20.5-6.S2.132
Chen, Yang, Cheng, Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care, doi:10.2337/dc20-0660
Cheng, Liu, Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.08.013
Crouse, Grimes, Li, Metformin use IS associated with reduced mortality IN a diverse population with COVID-19 and diabetes, MedRxiv Prepr Serv Heal Sci, doi:10.1101/2020.07.29.20164020
Do, Kim, Park, Is there an association between metform-in use and clinical outcomes in diabetes patients with COVID-19?, Diabetes Metab
Gao, Liu, Zhong, Risk of metformin in patients with type 2 diabetes with COVID-19: a preliminary retrospective report, Clin Transl Sci, doi:10.1111/cts.12897
Ghany, Palacio, Dawkins, Correspondence: Received: 6 March 2023 Accepted: 1 April 2023 Prof Grappasonni Iolanda School of Medicinal and Health Products Sciences University of Camerino, Camerino, Italy E-mail: iolanda.grappasonni@unicam.it of incretins in diabetes and COVID-19 infection: a hypothesis worth exploring, Diabetes Metab Syndr, doi:10.1007/s11739-020-02389-x
Goodall, Reed, Ardissino, Risk factors for severe disease in patients admitted with COVID-19 to a hospital in London, England: a retrospective cohort study, Epidemiol Infect, doi:10.1017/S0950268820002472
Hariyanto, Kurniawan, Metformin Use is Associated With Reduced Mortality Rate From Coronavirus Disease 2019 (COVID-19) Infection, Obes Med, doi:10.1016/j.obmed.2020.100290
Higgins, Thompson, Quantifying heterogeneity in a meta-analysis, Statics in Medicine, doi:10.1002/sim.1186
Hippisley-Cox, Young, Coupland, Risk of severe COVID-19 disease with ACE inhibitors and angiotensin recep-tor blockers: cohort study including 8.3 million people, Heart, doi:10.1136/heartjnl-2020-317393
Inzucchi, Bergenstal, Buse, Management of Hyperglycemia in Type 2 Diabetes, 2015: A Patient-Centered Approach: Update to a Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes, Diabetes Care, doi:10.2337/dc14-2441
Jiang, Chen, Yin, Association of Metformin With Mortality or ARDS in Patients With COVID-19 and Type 2 Diabetes: A Retrospective Cohort Study, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108619
Kan, Zhang, Han, Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis, Front. Endocrinol. Sept, doi:10.3389/fendo.2021.708494
Khunti, Knighton, Zaccardi, Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00050-4
Kim, Jeon, Kim, The clinical characteristics and outcomes of patients with moderate-to-severe coronavirus disease 2019 infection and diabetes in Daegu, South Korea, Diabetes Metab J, doi:10.4093/dmj.2020.0146
Kumar, Arora, Sharma, Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.044
Lalau, Al-Salameh, Hadjadj, Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19, Diabetes Metab, doi:10.1016/j.diabet.2020.101216
Lally, Tsoukas, Halladay, Metformin is associated with decreased 30-day mortality among nursing home residents infected with SARS-CoV-2, J Am Med Dir Assoc, doi:10.1016/j.jamda.2020.10.031
Li, Wei, Li, Metformin use in diabetes prior to hospitalization: effects on mortality in covid-19, Endocr Pract, doi:10.4158/EP-2020-0466
Li, Yang, Yan, Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis
Liu, Xi, Han, The association of diabetes and the prognosis of COVID-19 patients: A retrospective study, Diabetes Res Clin Pract, doi:10.1016/j.dia-bres.2020.108386
Lukito, Pranata, Henrina, The effect of metformin consumption on mortality in hospitalized COV-ID-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.11.006
Luo, Qiu, Liu, Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am J Trop Med Hyg, doi:10.4269/ajtmh.20-0375
Mirani, Favacchio, Carrone, Impact of comorbidities and glycemia at admission and dipeptidyl peptidase 4 inhibitors in patients with type 2 diabetes with COVID-19: a Case series from an Academic Hospital in 53. Oh TK, Song IA. Metformin use and risk of COV-ID-19 among patients with type II diabetes mellitus: an NHIS-COVID-19 database cohort study, Acta Diabetol
Mirsoleymani, Nekooghadam, Marzaleh, Assessment of risk factors for severe coronavirus disease 2019 among Iranian patients, Iran Red Crescent Med J, doi:10.32592/ircmj.2020.22.9.72
Moher, Liberati, Tetzlaff, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, Ann Intern Med, doi:10.7326/0003-4819-151-4-200908180-00135
Nafakhi, Alareedh, Al-Buthabhak, Predictors of adverse in-hospital outcome and recovery in patients with diabetes mellitus and COVID-19 pneumonia in Iraq, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.12.014
Natalucci, Villarini, Emili, Special Attention to Physical Activity in Breast Cancer Patients during the First Wave of COVID-19 Pandemic in Italy: The Di-anaWeb Cohort, J. Pers. Med, doi:10.3390/jpm11050381
Orioli, Servais, Belkhir, Clinical characteristics and short-term prognosis of in-patients with diabetes and COVID-19: A retrospective study from an academic center in Belgium, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.12.020
Oscanoa, Amado, Vidal, Metformin therapy, severity and mortality of SARS-CoV-2 infection: a metaanalysis, Clinical Diabetology, doi:10.5603/DK.a2021.0035
Page, Mckenzie, Bossuyt, The PRISMA 2020 statement: an update guideline for reporting systematic reviews, BMJ, doi:10.1136/bmj.n71
Pantanetti, Cangelosi, None, doi:10.1016/j.diabet.2020.10.006
Petrelli, Cangelosi, Nittari, Chronic Care Model in Italy: a narrative review of the literature, Primary Health Care Research & Development, doi:10.1017/S1463423621000268
Petrelli, Cangelosi, Scuri, Conoscenze alimentari in pazienti afferenti ad un centro di diabetologia, Acta Biomed, doi:10.23750/abm.v91i3-S.9418
Petrelli, Cangelosi, Scuri, Diabetes and technology: A pilot study on the management of patients with insulin pumps during the COVID-19 pandemic, Diabetes Res Clin Pract, doi:10.1016/j.dia-bres.2020.108481
Philipose, Smati, Wong, Aspey, Mendall, Obesity, old age, and frailty are the true risk factors for COVID-19 mortality and not chronic disease or ethnicity. MedRxi, doi:10.1101/2020.08.12.20156257
Puig-Domingo, Marazuela, Giustina, COVID-19 and endocrine diseases. A statement from the, Endocrine, doi:10.1007/s12020-020-02294-5
Pérez-Belmonte, Torres-Peña, Md, Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COV-ID-19 in association with glucose-lowering drugs: a nationwide cohort study, BMC Med, doi:10.1186/s12916-020-01832-2
Ramos-Rincón, Pérez-Belmonte, Carrasco-Sánchez, Association between prior cardiometabolic therapy and in-hospital mortality in very old patients with type 2 diabetes mellitus hospitalized due to COVID-19. A nationwide observational study in Spain, Research Square, doi:10.21203/rs.3.rs-133358/v1
Saha, Rami, Sujata, Diabetes prevalence and mortality in COVID-19 patients: a systematic review, meta-analysis, and meta-regression, J Diabetes Metab Disord, doi:10.1007/s40200-021-00779-2
Sanctis, Soliman, Tzoulis, The use of oral glucose-lowering agents (GLAs) in β-thalassemia patients with diabetes: Preliminary data from a retrospective study of ICET-A Network, Acta Biomed, doi:10.23750/abm.v93i2.12056
Scuri, Tesauri, Petrelli, Use of an online platform to evaluate the impact of social distancing measures on psycho-physical well-being in the COVID-19 Era, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph19116805
Shestakova, Vikulova, Isakov, Diabetes and COV-ID-19: analysis of the clinical outcomes according to the data of the russian diabetes registry, Probl Endokrinol (Mosk), doi:10.14341/probl12458
Soliman, Nair, Masalamani, Prevalence, clinical manifestations, and biochemical data of type 2 diabetes mellitus versus nondiabetic symptomatic patients with COVID-19: A comparative study, Acta Biomed, doi:10.23750/abm.v91i3.10214
Sourij, Aziz, Bräuer, COVID-19 fatality prediction in people with diabetes and prediabetes using a simple score upon hospital admission, Diabetes Obes Metab, doi:10.1111/dom.14256
Wang, Cooper, Gokhale, Association of metformin with susceptibility to COVID-19 in people with type 2 diabetes, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab067
Wang, Van Oekelen, Mouhieddine, A tertiary center experience of multiple myeloma patients with COVID-19: lessons learned and the path forward, J Hematol Oncol, doi:10.1186/s13045-020-00934-x
Wargny, Potier, Gourdy, Predictors of Hospital Discharge and Mortality in Patients With Diabetes and COVID-19: Updated Results From the Nationwide CORONADO Study, Diabetologia, doi:10.1007/s00125-020-05351-w
Yan, Valdes, Vijay, Role of drugs used for chronic disease management on susceptibility and severity of COVID-19: a large case-control study. medRxiv, doi:10.1101/2020.04.24.20077875
Yang, Sun, Zhang, The effect of Metformin on Mortality and Severity in COVID-19 patients with Diabetes Mellitus, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2021.108977
DOI record:
{
"DOI": "10.23750/abm.v94iS3.14405",
"ISSN": "2531-6745, 0392-4203",
"URL": "https://doi.org/10.23750/abm.v94iS3.14405",
"abstract": "Abstract Introduction: the COVID-19 infection, caused by severe Coronavirus 2 syndrome (Sars-Cov-2), immediately appeared to be the most tragic global pandemic event of the twentieth century. Right from the start of the pandemic, diabetic patients treated with metformin experienced a reduction in mortality and complications from COVID-19 compared to those with different treatments or no treatment. Objective The main objective of the study was to observe the effects of metformin in hospitalized subjects infected with COVID-19. Specifically, the outcomes of hospitalization in Intensive Care Units or death were examined. Materials and Methods A specific research PICOS was developed and the Pubmed, Embase and Scopus databases were consulted down to April 30, 2022. To estimate the extent of the metformin effect and risk of severity in SARS-CoV-2 infection, the Odd Ratio (OR) with 95% Confidence Interval (CI) published by the authors of the selected systematic reviews was used. Results from five systematic reviews 36 studies were selected. The final meta-analysis showed that thanks to treatment with metformin, DM2 patients affected by COVID-19 had protection against risk of disease severity, complications (ES 0.80; 95% CI) and mortality (ES 0.69; 95% CI). Conclusions More in-depth studies on the use of metformin, compared to other molecules, may be required to understand the real protective potential of the drug against negative outcomes caused by COVID-19 infection in DM2 patients.",
"author": [
{
"family": "Petrelli",
"given": "Fabio"
},
{
"family": "Grappasonni",
"given": "Iolanda"
},
{
"family": "Nguyen",
"given": "Cuc Thi Thu"
},
{
"family": "Tesauro",
"given": "Marina"
},
{
"family": "Pantanetti",
"given": "Paola"
},
{
"family": "Xhafa",
"given": "Sonila"
},
{
"family": "Cangelosi",
"given": "Giovanni"
}
],
"container-title": "Acta Biomedica Atenei Parmensis",
"issue": "S3",
"issued": {
"date-parts": [
[
2023,
8,
30
]
]
},
"language": "eng",
"medium": "JB",
"page": "e2023138",
"page-first": "e2023138",
"publisher": "Mattioli 1885 srl",
"publisher-place": "IT",
"title": "Metformin and Covid-19: a systematic review of systematic reviews with meta-analysis",
"type": "article-journal",
"volume": "94"
}
