Is metformin use associated with low mortality in patients with type 2 diabetes mellitus hospitalized for COVID-19? a multivariable and propensity score-adjusted meta-analysis
et al., PLOS ONE, doi:10.1371/journal.pone.0282210, Feb 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Meta analysis of 22 metformin studies, showing significantly lower mortality with metformin use prior to hospitalization.
24 meta-analyses show significant improvements with metformin for mortality1-23,
hospitalization7,13,23 ,
progression1, and
severity8,9,13 .
Currently there are 110 metformin for COVID-19 studies, showing 36% lower mortality [32‑40%], 29% lower ventilation [12‑43%], 19% lower ICU admission [8‑28%], 17% lower hospitalization [11‑23%], and 5% fewer cases [-4‑13%].
1.
Yang et al., The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus, Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2021.108977.
2.
Lukito et al., The Effect of Metformin Consumption on Mortality in Hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2020.11.006.
3.
Kow et al., Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis, Journal of Medical Virology, doi:10.1002/jmv.26498.
4.
Hariyanto et al., Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection, Obesity Medicine, doi:10.1016/j.obmed.2020.100290.
5.
Ma et al., Is metformin use associated with low mortality in patients with type 2 diabetes mellitus hospitalized for COVID-19? a multivariable and propensity score-adjusted meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0282210.
6.
Parveen et al., Association of Metformin with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis, Annals of the National Academy of Medical Sciences (India), doi:10.1055/s-0042-1760353.
7.
Li et al., Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Medicine, doi:10.3389/fmed.2021.704666.
8.
Schlesinger et al., Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis, Diabetologia, doi:10.1007/s00125-023-05928-1.
9.
Petrelli et al., Metformin and Covid-19: a systematic review of systematic reviews with meta-analysis, Acta Biomedica Atenei Parmensis, doi:10.23750/abm.v94iS3.14405.
10.
Oscanoa et al., Metformin therapy and severity and mortality of SARS-CoV-2 infection: a meta-analysis, Clinical Diabetology, doi:10.5603/DK.a2021.0035.
11.
Kan et al., Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2021.708494.
12.
Poly et al., Metformin Use Is Associated with Decreased Mortality in COVID-19 Patients with Diabetes: Evidence from Retrospective Studies and Biological Mechanism, Journal of Clinical Medicine, doi:10.3390/jcm10163507.
13.
Song et al., The Effect of Antihyperglycemic Medications on COVID-19: A Meta-analysis and Systematic Review from Observational Studies, Therapeutic Innovation & Regulatory Science, doi:10.1007/s43441-024-00633-6.
14.
Ganesh et al., Does metformin affect outcomes in COVID‐19 patients with new or pre‐existing diabetes mellitus? A systematic review and meta‐analysis, British Journal of Clinical Pharmacology, doi:10.1111/bcp.15258.
15.
Nassar et al., Noninsulin‐based antihyperglycemic medications in patients with diabetes and COVID‐19: A systematic review and meta‐analysis, Journal of Diabetes, doi:10.1111/1753-0407.13359.
16.
Zhan et al., Effect of Antidiabetic Therapy on Clinical Outcomes of COVID-19 Patients With Type 2 Diabetes: A Systematic Review and Meta-Analysis, Annals of Pharmacotherapy, doi:10.1177/10600280221133577.
17.
Nguyen et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196.
18.
Han et al., Association Between Anti-diabetic Agents and Clinical Outcomes of COVID-19 in Patients with Diabetes: A Systematic Review and Meta-Analysis, Archives of Medical Research, doi:10.1016/j.arcmed.2021.08.002.
19.
Chen et al., The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2022.895458.
20.
Scheen, A., Metformin and COVID-19: From cellular mechanisms to reduced mortality, Diabetes & Metabolism, doi:10.1016/j.diabet.2020.07.006.
21.
Sun et al., Is Metformin Use Associated With a Decreased Mortality for COVID-19 Diabetic Patients? A Meta-Analysis, Journal of the Endocrine Society, doi:10.1210/jendso/bvab048.709.
Ma et al., 23 Feb 2023, peer-reviewed, 2 authors.
Contact: mahesh.krishnamurthy@sluhn.org.
Is metformin use associated with low mortality in patients with type 2 diabetes mellitus hospitalized for COVID-19? a multivariable and propensity score-adjusted meta-analysis
PLOS ONE, doi:10.1371/journal.pone.0282210
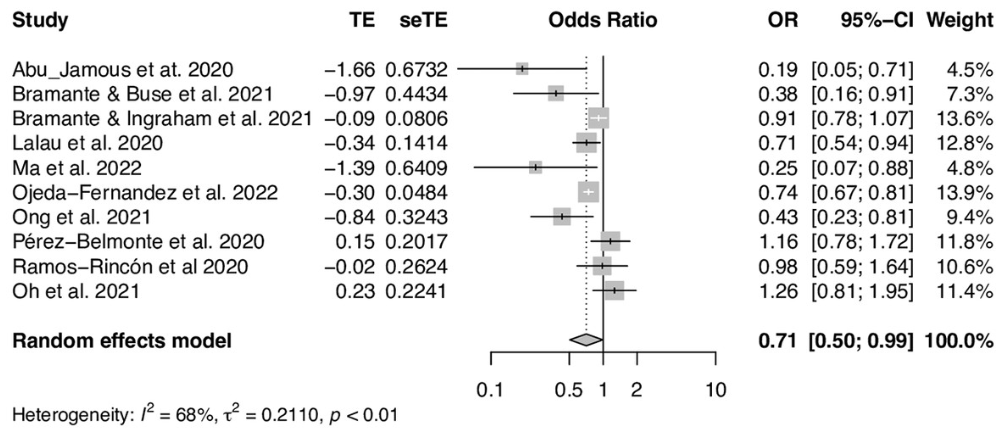
Background Coronavirus disease 2019 (COVID-19) is a new pandemic that the entire world is facing since December of 2019. Increasing evidence has shown that metformin is linked to favorable outcomes in patients with COVID-19. The aim of this study was to address whether outpatient or inpatient metformin therapy for type 2 diabetes mellitus is associated with low inhospital mortality in patients hospitalized for COVID-19.
Methods We searched studies published in PubMed, Embase, Google Scholar and Cochrane Library up to November 1, 2022. Raw event data extracted from individual study were pooled using the Mantel-Haenszel approach. Odds ratio (OR) or hazard ratio (HR) adjusted for covariates that potentially confound the association using multivariable regression or propensity score matching was pooled by the inverse-variance method. Random effect models were applied for meta-analysis due to variance among studies.
Results Twenty-two retrospective observational studies were selected. The pooled unadjusted OR for outpatient metformin therapy and in-hospital mortality was 0.48 (95% CI, 0.37-0.62) and the pooled OR adjusted with multivariable regression or propensity score matching was 0.71 (95% CI, 0.50-0.99). The pooled unadjusted OR for inpatient metformin therapy and in-hospital mortality was 0.18 (95% CI, 0.10-0.31), whereas the pooled adjusted HR was 1.10 (95% CI, 0.38-3.15).
References
Abu-Jamous, Anisimovich, Baxter, Mackillop, Vizcaychipi et al., Associations of comorbidities and medications with COVID-19 outcome: A retrospective analysis of real-world evidence data, medRxiv, doi:10.1101/2020.08.20.20174169
Bramante, Buse, Tamaritz, Palacio, Cohen et al., Outpatient metformin use is associated with reduced severity of COVID-19 disease in adults with overweight or obesity, J Med Virol, doi:10.1002/jmv.26873
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis, Lancet Healthy Longev, doi:10.1016/S2666-7568%2820%2930033-7
Cameron, Morrison, Levin, Mohan, Forteath et al., Anti-Inflammatory Effects of Metformin Irrespective of Diabetes Status, Circ Res, doi:10.1161/CIRCRESAHA.116.308445
Cariou, Hadjadj, Wargny, Pichelin, Al-Salameh et al., Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Chen, Yang, Cheng, Chen, Peng et al., Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication, Diabetes Care, doi:10.2337/dc20-0660
Cheng, Liu, Li, Zhang, Lei et al., Metformin Is Associated with Higher Incidence of Acidosis, but Not Mortality, in Individuals with COVID-19 and Pre-existing Type 2 Diabetes, Cell Metab, doi:10.1016/j.cmet.2020.08.013
Crouse, Grimes, Li, Might, Ovalle et al., Metformin Use Is Associated With Reduced Mortality in a Diverse Population With COVID-19 and Diabetes, Front Endocrinol, doi:10.3389/fendo.2020.600439
Cummings, Baldwin, Abrams, Jacobson, Meyer et al., Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study, Lancet, doi:10.1016/S0140-6736%2820%2931189-2
Dalan, Metformin, neutrophils and COVID-19 infection, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108230
Esam, A proposed mechanism for the possible therapeutic potential of Metformin in COVID-19, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108282
Garcia, Flumamine, a new synthetic analgesic and anti-flu drug, J Philipp Med Assoc
Ghany, Palacio, Dawkins, Chen, Mccarter et al., Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA, Diabetes Metab Syndr, doi:10.1016/j.dsx.2021.02.022
Grasselli, Zangrillo, Zanella, Antonelli, Cabrini et al., Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, JAMA, doi:10.1001/jama.2020.5394
Guan, Liang, Zhao, Liang, Chen et al., Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis, Eur Respir J, doi:10.1183/13993003.00547%26%23x2013%3B2020
Guan, Ni, Hu, Liang, Ou et al., Clinical Characteristics of Coronavirus Disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032
Huang, Lim, Pranata, Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia-A systematic review, meta-analysis, and meta-regression, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.018
Jiang, Chen, Liu, Yin, Yang et al., Association of metformin with mortality or ARDS in patients with COVID-19 and type 2 diabetes: A retrospective cohort study, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108619
Lalau, Al-Salameh, Hadjadj, Goronflot, Wiernsperger et al., Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19, Diabetes Metab, doi:10.1016/j.diabet.2020.101216
Li, Wei, Li, Mccowen, Xiong et al., Metformin Use in Diabetes Prior to Hospitalization: Effects on Mortality in Covid-19, Endocr Pract, doi:10.4158/EP-2020-0466
Li, Wei, Mccowen, Xiong, Liu et al., Inpatient use of metformin and acarbose is associated with reduced mortality of COVID-19 patients with type 2 diabetes mellitus, Endocrinol Diabetes Metab, doi:10.1002/edm2.301
Li, Yang, Yan, Sun, Zeng et al., Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis, Front Med, doi:10.3389/fmed.2021.704666
Lighter, Phillips, Hochman, Sterling, Johnson et al., Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission, Clin Infect Dis, doi:10.1093/cid/ciaa415
Luk, Yip, Zhang, Kong, Wong et al., Glucose-lowering drugs and outcome from COVID-19 among patients with type 2 diabetes mellitus: a population-wide analysis in Hong Kong, BMJ Open, doi:10.1136/bmjopen-2021-052310
Luo, Qiu, Liu, Liu, Zheng et al., Metformin Treatment Was Associated with Decreased Mortality in COVID-19 Patients with Diabetes in a Retrospective Analysis, Am J Trop Med Hyg, doi:10.4269/ajtmh.20-0375
Ma, Fan, Cheng, Does sleeve lobectomy concomitant with or without pulmonary artery reconstruction (double sleeve) have favorable results for non-small cell lung cancer compared with pneumonectomy? A meta-analysis, Eur J Cardiothorac Surg, doi:10.1016/j.ejcts.2007.03.018
Ma, Patel, Vemparala, Krishnamurthy, Metformin is associated with favorable outcomes in patients with COVID-19 and type 2 diabetes mellitus, Sci Rep, doi:10.1038/s41598-022-09639-2
Mirani, Favacchio, Carrone, Betella, Biamonte et al., Impact of Comorbidities and Glycemia at Admission and Dipeptidyl Peptidase 4 Inhibitors in Patients With Type 2 Diabetes With COVID-19: A Case Series From an Academic Hospital in Lombardy, Italy, Diabetes Care, doi:10.2337/dc20-1340
Oh, Song, Metformin use and risk of COVID-19 among patients with type II diabetes mellitus: an NHIS-COVID-19 database cohort study, Acta Diabetol, doi:10.1007/s00592-020-01666-7
Ojeda-Fernandez, Foresta, Macaluso, Colacioppo, Tettamanti et al., Metformin use is associated with a decrease in the risk of hospitalization and mortality in COVID-19 patients with diabetes: A population-based study in Lombardy, Diabetes Obes Metab, doi:10.1111/dom.14648
Ong, Tan, Canete, Lim, Robles, Association Between Metformin Use and Mortality among Patients with Type 2 Diabetes Mellitus Hospitalized for COVID-19 Infection, J ASEAN Fed Endocr Soc, doi:10.15605/jafes.036.02.20
Oscanoa, Amado, Vidal, Savarino, Romero-Ortuno, Metformin therapy, severity and mortality of SARS-CoV-2 infection: a meta-analysis, Clin Diabetol
Perez-Belmonte, Torres-Pena, Lopez-Carmona, Ayala-Gutierrez, Fuentes-Jimenez et al., Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: a nationwide cohort study, BMC Med, doi:10.1186/s12916-020-01832-2
Ramos-Rinco ´n, ´rez-Belmonte, ´nchez, Jansen-Chaparro, De-Sousa-Baena, type 2 diabetes mellitus hospitalized due to COVID-19. A nationwide observational study in Spain, doi:10.21203/rs.3.rs-133358/v1
Roncon, Zuin, Rigatelli, Zuliani, Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome, J Clin Virol, doi:10.1016/j.jcv.2020.104354
Siddiqi, Mehra, COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal, J Heart Lung Transplant, doi:10.1016/j.healun.2020.03.012
Stang, Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses, Eur J Epidemiol, doi:10.1007/s10654-010-9491-z
Tamura, Said, De Freitas, Rubio, Outcome and death risk of diabetes patients with Covid-19 receiving pre-hospital and in-hospital metformin therapies, Diabetol Metab Syndr, doi:10.1186/s13098-021-00695-8
Thomas, Li, Pencina, Overlap Weighting: A Propensity Score Method That Mimics Attributes of a Randomized Clinical Trial, JAMA, doi:10.1001/jama.2020.7819
Ursini, Ciaffi, Landini, Meliconi, COVID-19 and diabetes: Is metformin a friend or foe? Diabetes, Res Clin Pract, doi:10.1016/j.diabres.2020.108167
Ursini, Russo, Pellino, Angelo, Chiaravalloti et al., Metformin and Autoimmunity: A "New Deal" of an Old Drug, Front Immunol, doi:10.3389/fimmu.2018.01236
Wiernsperger, Al-Salameh, Cariou, Lalau, Protection by metformin against severe Covid-19: An in-depth mechanistic analysis, Diabetes Metab, doi:10.1016/j.diabet.2022.101359
Wu, Mcgoogan, Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention, JAMA, doi:10.1001/jama.2020.2648
Yang, Sun, Zhang, Zhang, The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2021.108977
Yang, Yu, Xu, Shu, Xia et al., Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lan, cet Respir Med, doi:10.1016/S2213-2600%2820%2930079-5
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736%2820%2930566-3
DOI record:
{
"DOI": "10.1371/journal.pone.0282210",
"ISSN": [
"1932-6203"
],
"URL": "http://dx.doi.org/10.1371/journal.pone.0282210",
"abstract": "<jats:sec id=\"sec001\">\n<jats:title>Background</jats:title>\n<jats:p>Coronavirus disease 2019 (COVID-19) is a new pandemic that the entire world is facing since December of 2019. Increasing evidence has shown that metformin is linked to favorable outcomes in patients with COVID-19. The aim of this study was to address whether outpatient or inpatient metformin therapy for type 2 diabetes mellitus is associated with low in-hospital mortality in patients hospitalized for COVID-19.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec002\">\n<jats:title>Methods</jats:title>\n<jats:p>We searched studies published in PubMed, Embase, Google Scholar and Cochrane Library up to November 1, 2022. Raw event data extracted from individual study were pooled using the Mantel-Haenszel approach. Odds ratio (OR) or hazard ratio (HR) adjusted for covariates that potentially confound the association using multivariable regression or propensity score matching was pooled by the inverse-variance method. Random effect models were applied for meta-analysis due to variance among studies.</jats:p>\n</jats:sec>\n<jats:sec id=\"sec003\">\n<jats:title>Results</jats:title>\n<jats:p>Twenty-two retrospective observational studies were selected. The pooled unadjusted OR for outpatient metformin therapy and in-hospital mortality was 0.48 (95% CI, 0.37–0.62) and the pooled OR adjusted with multivariable regression or propensity score matching was 0.71 (95% CI, 0.50–0.99). The pooled unadjusted OR for inpatient metformin therapy and in-hospital mortality was 0.18 (95% CI, 0.10–0.31), whereas the pooled adjusted HR was 1.10 (95% CI, 0.38–3.15).</jats:p>\n</jats:sec>\n<jats:sec id=\"sec004\">\n<jats:title>Conclusions</jats:title>\n<jats:p>Our results suggest that there is a significant association between the reduction of in-hospital mortality and outpatient metformin therapy for type 2 diabetes mellitus in patients hospitalized for COVID-19.</jats:p>\n</jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0002-0381-7804",
"affiliation": [],
"authenticated-orcid": true,
"family": "Ma",
"given": "Zhiyuan",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-1132-1788",
"affiliation": [],
"authenticated-orcid": true,
"family": "Krishnamurthy",
"given": "Mahesh",
"sequence": "additional"
}
],
"container-title": "PLOS ONE",
"container-title-short": "PLoS ONE",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.plosone.org"
]
},
"created": {
"date-parts": [
[
2023,
2,
23
]
],
"date-time": "2023-02-23T18:31:15Z",
"timestamp": 1677177075000
},
"deposited": {
"date-parts": [
[
2023,
2,
23
]
],
"date-time": "2023-02-23T18:31:42Z",
"timestamp": 1677177102000
},
"editor": [
{
"affiliation": [],
"family": "Hirst",
"given": "Jennifer A.",
"sequence": "first"
}
],
"indexed": {
"date-parts": [
[
2023,
2,
24
]
],
"date-time": "2023-02-24T05:21:00Z",
"timestamp": 1677216060751
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2023,
2,
23
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2023,
2,
23
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
2,
23
]
],
"date-time": "2023-02-23T00:00:00Z",
"timestamp": 1677110400000
}
}
],
"link": [
{
"URL": "https://dx.plos.org/10.1371/journal.pone.0282210",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "340",
"original-title": [],
"page": "e0282210",
"prefix": "10.1371",
"published": {
"date-parts": [
[
2023,
2,
23
]
]
},
"published-online": {
"date-parts": [
[
2023,
2,
23
]
]
},
"publisher": "Public Library of Science (PLoS)",
"reference": [
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical Characteristics of Coronavirus Disease 2019 in China",
"author": "WJ Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"issue": "18",
"journal-title": "N Engl J Med",
"key": "pone.0282210.ref001",
"volume": "382",
"year": "2020"
},
{
"article-title": "Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention.",
"author": "Z Wu",
"journal-title": "JAMA",
"key": "pone.0282210.ref002",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"article-title": "Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study",
"author": "X Yang",
"doi-asserted-by": "crossref",
"first-page": "475",
"issue": "5",
"journal-title": "Lancet Respir Med",
"key": "pone.0282210.ref003",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)31189-2",
"article-title": "Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study",
"author": "MJ Cummings",
"doi-asserted-by": "crossref",
"first-page": "1763",
"issue": "10239",
"journal-title": "Lancet",
"key": "pone.0282210.ref004",
"volume": "395",
"year": "2020"
},
{
"article-title": "Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy.",
"author": "G Grasselli",
"journal-title": "JAMA",
"key": "pone.0282210.ref005",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa415",
"article-title": "Obesity in Patients Younger Than 60 Years Is a Risk Factor for COVID-19 Hospital Admission",
"author": "J Lighter",
"doi-asserted-by": "crossref",
"first-page": "896",
"issue": "15",
"journal-title": "Clin Infect Dis",
"key": "pone.0282210.ref006",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study",
"author": "F Zhou",
"doi-asserted-by": "crossref",
"first-page": "1054",
"issue": "10229",
"journal-title": "Lancet",
"key": "pone.0282210.ref007",
"volume": "395",
"year": "2020"
},
{
"article-title": "Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis",
"author": "WJ Guan",
"issue": "5",
"journal-title": "Eur Respir J",
"key": "pone.0282210.ref008",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1016/j.jcv.2020.104354",
"article-title": "Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome.",
"author": "L Roncon",
"doi-asserted-by": "crossref",
"first-page": "104354",
"journal-title": "J Clin Virol",
"key": "pone.0282210.ref009",
"volume": "127",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.018",
"article-title": "Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia—A systematic review, meta-analysis, and meta-regression.",
"author": "I Huang",
"doi-asserted-by": "crossref",
"first-page": "395",
"issue": "4",
"journal-title": "Diabetes Metab Syndr.",
"key": "pone.0282210.ref010",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.healun.2020.03.012",
"article-title": "COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal",
"author": "HK Siddiqi",
"doi-asserted-by": "crossref",
"first-page": "405",
"issue": "5",
"journal-title": "J Heart Lung Transplant",
"key": "pone.0282210.ref011",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2018.01236",
"article-title": "Metformin and Autoimmunity: A \"New Deal\" of an Old Drug.",
"author": "F Ursini",
"doi-asserted-by": "crossref",
"first-page": "1236",
"journal-title": "Front Immunol.",
"key": "pone.0282210.ref012",
"volume": "9",
"year": "2018"
},
{
"article-title": "Flumamine, a new synthetic analgesic and anti-flu drug.",
"author": "EY Garcia",
"first-page": "287",
"issue": "7",
"journal-title": "J Philipp Med Assoc",
"key": "pone.0282210.ref013",
"volume": "26",
"year": "1950"
},
{
"DOI": "10.1161/CIRCRESAHA.116.308445",
"article-title": "Anti-Inflammatory Effects of Metformin Irrespective of Diabetes Status",
"author": "AR Cameron",
"doi-asserted-by": "crossref",
"first-page": "652",
"issue": "5",
"journal-title": "Circ Res",
"key": "pone.0282210.ref014",
"volume": "119",
"year": "2016"
},
{
"DOI": "10.1016/j.diabres.2020.108230",
"article-title": "Metformin, neutrophils and COVID-19 infection.",
"author": "R Dalan",
"doi-asserted-by": "crossref",
"first-page": "108230",
"journal-title": "Diabetes Res Clin Pract",
"key": "pone.0282210.ref015",
"volume": "164",
"year": "2020"
},
{
"article-title": "A proposed mechanism for the possible therapeutic potential of Metformin in COVID-19",
"author": "Z. Esam",
"first-page": "108282",
"journal-title": "Diabetes Res Clin Pract",
"key": "pone.0282210.ref016",
"volume": "2020"
},
{
"DOI": "10.1016/j.diabet.2022.101359",
"article-title": "Protection by metformin against severe Covid-19: An in-depth mechanistic analysis",
"author": "N Wiernsperger",
"doi-asserted-by": "crossref",
"first-page": "101359",
"issue": "4",
"journal-title": "Diabetes Metab",
"key": "pone.0282210.ref017",
"volume": "48",
"year": "2022"
},
{
"DOI": "10.1016/j.diabres.2020.108167",
"article-title": "COVID-19 and diabetes: Is metformin a friend or foe?",
"author": "F Ursini",
"doi-asserted-by": "crossref",
"first-page": "108167",
"journal-title": "Diabetes Res Clin Pract",
"key": "pone.0282210.ref018",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.1007/s10654-010-9491-z",
"article-title": "Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses",
"author": "A. Stang",
"doi-asserted-by": "crossref",
"first-page": "603",
"issue": "9",
"journal-title": "Eur J Epidemiol",
"key": "pone.0282210.ref019",
"volume": "25",
"year": "2010"
},
{
"DOI": "10.1016/j.ejcts.2007.03.018",
"article-title": "Does sleeve lobectomy concomitant with or without pulmonary artery reconstruction (double sleeve) have favorable results for non-small cell lung cancer compared with pneumonectomy? A meta-analysis.",
"author": "Z Ma",
"doi-asserted-by": "crossref",
"first-page": "20",
"issue": "1",
"journal-title": "Eur J Cardiothorac Surg.",
"key": "pone.0282210.ref020",
"volume": "32",
"year": "2007"
},
{
"article-title": "Associations of comorbidities and medications with COVID-19 outcome: A retrospective analysis of real-world evidence data.",
"author": "B Abu-Jamous",
"journal-title": "medRxiv",
"key": "pone.0282210.ref021",
"year": "2020"
},
{
"article-title": "Outpatient metformin use is associated with reduced severity of COVID-19 disease in adults with overweight or obesity",
"author": "CT Bramante",
"journal-title": "J Med Virol",
"key": "pone.0282210.ref022",
"year": "2021"
},
{
"DOI": "10.1016/S2666-7568(20)30033-7",
"article-title": "Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis",
"author": "CT Bramante",
"doi-asserted-by": "crossref",
"first-page": "e34",
"issue": "1",
"journal-title": "Lancet Healthy Longev",
"key": "pone.0282210.ref023",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"article-title": "Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study",
"author": "B Cariou",
"doi-asserted-by": "crossref",
"first-page": "1500",
"issue": "8",
"journal-title": "Diabetologia",
"key": "pone.0282210.ref024",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.2337/dc20-0660",
"article-title": "Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication",
"author": "Y Chen",
"doi-asserted-by": "crossref",
"first-page": "1399",
"issue": "7",
"journal-title": "Diabetes Care",
"key": "pone.0282210.ref025",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.3389/fendo.2020.600439",
"article-title": "Metformin Use Is Associated With Reduced Mortality in a Diverse Population With COVID-19 and Diabetes.",
"author": "AB Crouse",
"doi-asserted-by": "crossref",
"first-page": "600439",
"journal-title": "Front Endocrinol (Lausanne).",
"key": "pone.0282210.ref026",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2021.02.022",
"article-title": "Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA.",
"author": "R Ghany",
"doi-asserted-by": "crossref",
"first-page": "513",
"issue": "2",
"journal-title": "Diabetes Metab Syndr",
"key": "pone.0282210.ref027",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1016/j.diabet.2020.101216",
"article-title": "Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19.",
"author": "JD Lalau",
"doi-asserted-by": "crossref",
"first-page": "101216",
"issue": "5",
"journal-title": "Diabetes Metab.",
"key": "pone.0282210.ref028",
"volume": "47",
"year": "2020"
},
{
"DOI": "10.4158/EP-2020-0466",
"article-title": "Metformin Use in Diabetes Prior to Hospitalization: Effects on Mortality in Covid-19.",
"author": "J Li",
"doi-asserted-by": "crossref",
"first-page": "1166",
"issue": "10",
"journal-title": "Endocr Pract.",
"key": "pone.0282210.ref029",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1038/s41598-022-09639-2",
"article-title": "Metformin is associated with favorable outcomes in patients with COVID-19 and type 2 diabetes mellitus",
"author": "Z Ma",
"doi-asserted-by": "crossref",
"first-page": "5553",
"issue": "1",
"journal-title": "Sci Rep",
"key": "pone.0282210.ref030",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.2337/dc20-1340",
"article-title": "Impact of Comorbidities and Glycemia at Admission and Dipeptidyl Peptidase 4 Inhibitors in Patients With Type 2 Diabetes With COVID-19: A Case Series From an Academic Hospital in Lombardy, Italy.",
"author": "M Mirani",
"doi-asserted-by": "crossref",
"first-page": "3042",
"issue": "12",
"journal-title": "Diabetes Care",
"key": "pone.0282210.ref031",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1007/s00592-020-01666-7",
"article-title": "Metformin use and risk of COVID-19 among patients with type II diabetes mellitus: an NHIS-COVID-19 database cohort study.",
"author": "TK Oh",
"doi-asserted-by": "crossref",
"first-page": "771",
"issue": "6",
"journal-title": "Acta Diabetol.",
"key": "pone.0282210.ref032",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.1186/s12916-020-01832-2",
"article-title": "Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: a nationwide cohort study.",
"author": "LM Perez-Belmonte",
"doi-asserted-by": "crossref",
"first-page": "359",
"issue": "1",
"journal-title": "BMC Med.",
"key": "pone.0282210.ref033",
"volume": "18",
"year": "2020"
},
{
"article-title": "Association between prior cardiometabolic therapy and in-hospital mortality in very old patients with type 2 diabetes mellitus hospitalized due to COVID-19. A nationwide observational study in Spain.",
"author": "JM Ramos-Rincón",
"journal-title": "Research Square.",
"key": "pone.0282210.ref034",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2021-052310",
"article-title": "Glucose-lowering drugs and outcome from COVID-19 among patients with type 2 diabetes mellitus: a population-wide analysis in Hong Kong.",
"author": "AOY Luk",
"doi-asserted-by": "crossref",
"first-page": "e052310",
"issue": "10",
"journal-title": "BMJ Open",
"key": "pone.0282210.ref035",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1111/dom.14648",
"article-title": "Metformin use is associated with a decrease in the risk of hospitalization and mortality in COVID-19 patients with diabetes: A population-based study in Lombardy.",
"author": "L Ojeda-Fernandez",
"doi-asserted-by": "crossref",
"first-page": "891",
"issue": "5",
"journal-title": "Diabetes Obes Metab",
"key": "pone.0282210.ref036",
"volume": "24",
"year": "2022"
},
{
"DOI": "10.15605/jafes.036.02.20",
"article-title": "Association Between Metformin Use and Mortality among Patients with Type 2 Diabetes Mellitus Hospitalized for COVID-19 Infection.",
"author": "AN Ong",
"doi-asserted-by": "crossref",
"first-page": "133",
"issue": "2",
"journal-title": "J ASEAN Fed Endocr Soc.",
"key": "pone.0282210.ref037",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.1016/j.cmet.2020.08.013",
"article-title": "Metformin Is Associated with Higher Incidence of Acidosis, but Not Mortality, in Individuals with COVID-19 and Pre-existing Type 2 Diabetes.",
"author": "X Cheng",
"doi-asserted-by": "crossref",
"first-page": "537",
"issue": "4",
"journal-title": "Cell Metab",
"key": "pone.0282210.ref038",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108619",
"article-title": "Association of metformin with mortality or ARDS in patients with COVID-19 and type 2 diabetes: A retrospective cohort study",
"author": "N Jiang",
"doi-asserted-by": "crossref",
"first-page": "108619",
"journal-title": "Diabetes Res Clin Pract",
"key": "pone.0282210.ref039",
"volume": "173",
"year": "2021"
},
{
"article-title": "Inpatient use of metformin and acarbose is associated with reduced mortality of COVID-19 patients with type 2 diabetes mellitus",
"author": "J Li",
"first-page": "e00301",
"issue": "1",
"journal-title": "Endocrinol Diabetes Metab",
"key": "pone.0282210.ref040",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"article-title": "Metformin Treatment Was Associated with Decreased Mortality in COVID-19 Patients with Diabetes in a Retrospective Analysis",
"author": "P Luo",
"doi-asserted-by": "crossref",
"first-page": "69",
"issue": "1",
"journal-title": "Am J Trop Med Hyg",
"key": "pone.0282210.ref041",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.1186/s13098-021-00695-8",
"article-title": "Outcome and death risk of diabetes patients with Covid-19 receiving pre-hospital and in-hospital metformin therapies.",
"author": "RE Tamura",
"doi-asserted-by": "crossref",
"first-page": "76",
"issue": "1",
"journal-title": "Diabetol Metab Syndr.",
"key": "pone.0282210.ref042",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3389/fmed.2021.704666",
"article-title": "Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis.",
"author": "Y Li",
"doi-asserted-by": "crossref",
"first-page": "704666",
"journal-title": "Front Med (Lausanne).",
"key": "pone.0282210.ref043",
"volume": "8",
"year": "2021"
},
{
"article-title": "Metformin therapy, severity and mortality of SARS-CoV-2 infection: a meta-analysis.",
"author": "TJ Oscanoa",
"first-page": "317",
"issue": "4",
"journal-title": "Clin Diabetol",
"key": "pone.0282210.ref044",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1016/j.diabres.2021.108977",
"article-title": "The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus",
"author": "W Yang",
"doi-asserted-by": "crossref",
"first-page": "108977",
"journal-title": "Diabetes Res Clin Pract",
"key": "pone.0282210.ref045",
"volume": "178",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.7819",
"article-title": "Overlap Weighting: A Propensity Score Method That Mimics Attributes of a Randomized Clinical Trial",
"author": "LE Thomas",
"doi-asserted-by": "crossref",
"first-page": "2417",
"issue": "23",
"journal-title": "JAMA",
"key": "pone.0282210.ref046",
"volume": "323",
"year": "2020"
}
],
"reference-count": 46,
"references-count": 46,
"relation": {},
"resource": {
"primary": {
"URL": "https://dx.plos.org/10.1371/journal.pone.0282210"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Is metformin use associated with low mortality in patients with type 2 diabetes mellitus hospitalized for COVID-19? a multivariable and propensity score-adjusted meta-analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1371/journal.pone.corrections_policy",
"volume": "18"
}
