Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication
et al., Diabetes Care, doi:10.2337/dc20-0660, Jul 2020
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 120 COVID-19 diabetes patients, showing non-statistically significantly lower mortality with existing metformin treatment.
Although the 33% lower mortality is not statistically significant, it is consistent with the significant 36% lower mortality [32‑40%] from meta-analysis of the 74 mortality results to date.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
risk of death, 33.0% lower, RR 0.67, p = 0.46, treatment 4 of 43 (9.3%), control 15 of 77 (19.5%), NNT 9.8, adjusted per study, odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Chen et al., 31 Jul 2020, retrospective, China, peer-reviewed, 12 authors.
Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication
Diabetes Care, doi:10.2337/dc20-0660
Diabetes is one of the most distinct comorbidities of COVID-19. Here, we describe the clinical characteristics of and outcomes in patients with diabetes in whom COVID-19 was confirmed or clinically diagnosed (with typical features on lung imaging and symptoms) and their association with glucose-lowering or blood pressure-lowering medications.
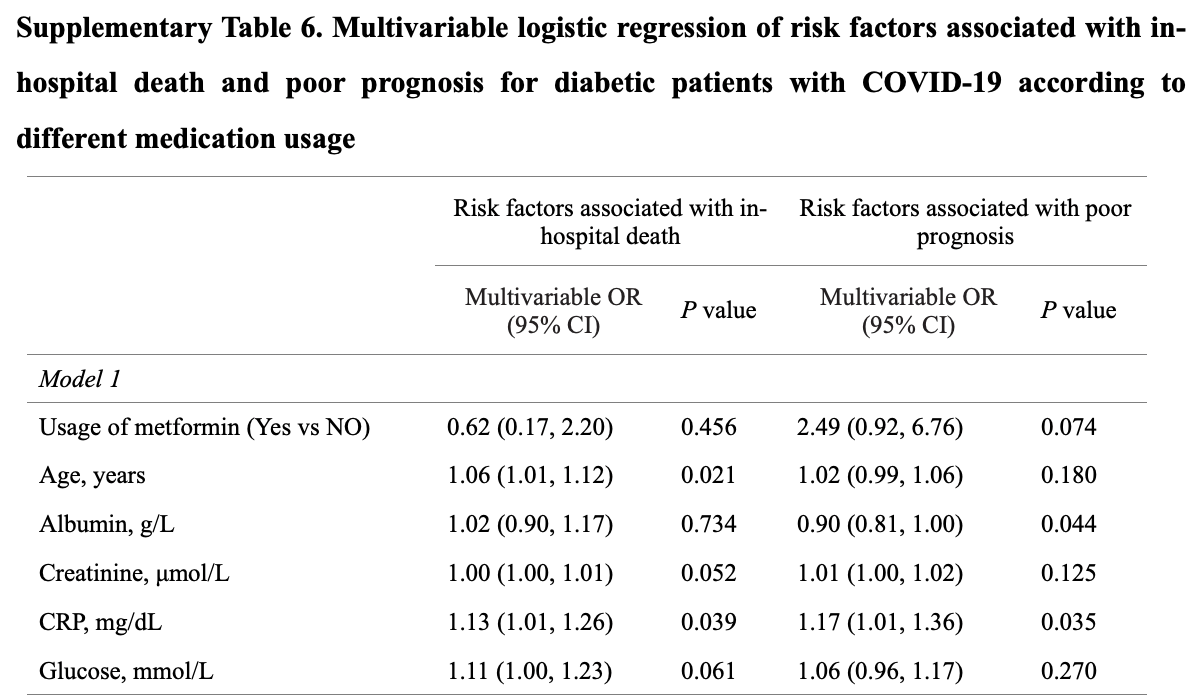
RESEARCH DESIGN AND METHODS In this retrospective study involving 904 patients with COVID-19 (136 with diabetes, mostly type 2 diabetes), clinical and laboratory characteristics were collected and compared between the group with diabetes and the group without diabetes, and between groups taking different medications. Logistic regression was used to explore risk factors associated with mortality or poor prognosis.
RESULTS The proportion of comorbid diabetes is similar between cases of confirmed and of clinically diagnosed COVID-19. Risk factors for higher mortality of patients with diabetes and COVID-19 were older age (adjusted odds ratio [aOR] 1.09 [95% CI 1.04, 1.15] per year increase; P 5 0.001) and elevated C-reactive protein (aOR 1.12 [95% CI 1.00, 1.24]; P 5 0.043). Insulin usage (aOR 3.58 [95% CI 1.37, 9.35]; P 5 0.009) was associated with poor prognosis. Clinical outcomes of those who use an ACE inhibitor (ACEI) or angiotensin II type-I receptor blocker (ARB) were comparable with those of patients who do not use ACEI/ARB among COVID-19 patients with diabetes and hypertension.
CONCLUSIONS C-reactive protein may help to identify patients with diabetes who are at greater risk of dying during hospitalization. Older patients with diabetes were prone to death related to COVID-19. Attention needs to be paid to patients with diabetes and COVID-19 who use insulin. ACEI/ARB use showed no significant impact on patients with diabetes and hypertension who have COVID-19.
References
Adhikari, Meng, Wu, Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review, Infect Dis Poverty
Chan-Yeung, Xu, SARS: epidemiology, Respirology
Chen, Liu, Cheng, Zheng, Huang, Effects of apelin peptides on diabetic complications, Curr Protein Pept Sci
Chen, Zhang, Yang, Fangcang shelter hospitals: a novel concept for responding to public health emergencies [published correction appears in Lancet 2020, Lancet
Fang, Karakiulakis, Roth, Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?, Lancet Respir Med
Garbati, Fagbo, Fang, A comparative study of clinical presentation and risk factors for adverse outcome in patients hospitalised with acute respiratory disease due to MERS coronavirus or other causes, PLoS One
Giovannelli, Trouiller, Hulo, Low-grade systemic inflammation: a partial mediator of the relationship between diabetes and lung function, Ann Epidemiol
Guan, Ni, Hu, China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med
Gupta, Ghosh, Singh, Misra, Clinical considerations for patients with diabetes in times of COVID-19 epidemic, Diabetes Metab Syndr
Harding, Pavkov, Magliano, Shaw, Gregg, Global trends in diabetes complications: a review of current evidence, Diabetologia
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Kulcsar, Coleman, Beck, Frieman, Gupta et al., Comorbid diabetes results in immune dysregulation and enhanced disease severity following MERS-CoV infection, Front Immunol
Li, Guan, Wu, Early transmission dynamics in Wuhan, China, of novel coronavirusinfected pneumonia, N Engl J Med
Li, Yao, Li, Stability issues of RT-PCR testing of SARS-CoV-2 for hospitalized patients clinically diagnosed with COVID-19, J Med Virol, doi:10.1002/jmv.25786
Li, Yi, Luo, Development and clinical application of a rapid IgM-IgG combined antibody test for SARS-CoV-2 infection diagnosis, J Med Virol, doi:10.1002/jmv.25727
Li, Zhang, Zhuo, The vasoprotective axes of the renin-angiotensin system: physiological relevance and therapeutic implications in cardiovascular, hypertensive and kidney diseases, Pharmacol Res
Pan, Liu, Wang, Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China, JAMA, doi:10.1001/jama.2020.6130
Pearson-Stuttard, Blundell, Harris, Cook, Critchley, Diabetes and infection: assessing the association with glycaemic control in population-based studies, Lancet Diabetes Endocrinol
Teeter, Riese, Cross-sectional and prospective study of lung function in adults with type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) study: response to Yeh et al, Diabetes Care
Wan, Shang, Graham, Baric, Li, Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus, J Virol
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention, JAMA
Yang, Feng, Yuan, Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS, Diabet Med
Yeh, Punjabi, Wang, Crosssectional and prospective study of lung function in adults with type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) study, Diabetes Care
Zhao, Yao, Wang, A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias, Clin Infect Dis, doi:10.1093/cid/ciaa247
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
DOI record:
{
"DOI": "10.2337/dc20-0660",
"ISSN": [
"0149-5992",
"1935-5548"
],
"URL": "http://dx.doi.org/10.2337/dc20-0660",
"abstract": "<jats:sec>\n <jats:title>OBJECTIVE</jats:title>\n <jats:p>Diabetes is one of the most distinct comorbidities of COVID-19. Here, we describe the clinical characteristics of and outcomes in patients with diabetes in whom COVID-19 was confirmed or clinically diagnosed (with typical features on lung imaging and symptoms) and their association with glucose-lowering or blood pressure–lowering medications.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>RESEARCH DESIGN AND METHODS</jats:title>\n <jats:p>In this retrospective study involving 904 patients with COVID-19 (136 with diabetes, mostly type 2 diabetes), clinical and laboratory characteristics were collected and compared between the group with diabetes and the group without diabetes, and between groups taking different medications. Logistic regression was used to explore risk factors associated with mortality or poor prognosis.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>RESULTS</jats:title>\n <jats:p>The proportion of comorbid diabetes is similar between cases of confirmed and of clinically diagnosed COVID-19. Risk factors for higher mortality of patients with diabetes and COVID-19 were older age (adjusted odds ratio [aOR] 1.09 [95% CI 1.04, 1.15] per year increase; P = 0.001) and elevated C-reactive protein (aOR 1.12 [95% CI 1.00, 1.24]; P = 0.043). Insulin usage (aOR 3.58 [95% CI 1.37, 9.35]; P = 0.009) was associated with poor prognosis. Clinical outcomes of those who use an ACE inhibitor (ACEI) or angiotensin II type-I receptor blocker (ARB) were comparable with those of patients who do not use ACEI/ARB among COVID-19 patients with diabetes and hypertension.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>CONCLUSIONS</jats:title>\n <jats:p>C-reactive protein may help to identify patients with diabetes who are at greater risk of dying during hospitalization. Older patients with diabetes were prone to death related to COVID-19. Attention needs to be paid to patients with diabetes and COVID-19 who use insulin. ACEI/ARB use showed no significant impact on patients with diabetes and hypertension who have COVID-19.</jats:p>\n </jats:sec>",
"author": [
{
"affiliation": [
{
"name": "Tongji School of Pharmacy, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China"
}
],
"family": "Chen",
"given": "Yuchen",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Tongji School of Pharmacy, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China"
}
],
"family": "Yang",
"given": "Dong",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy and the Center of Information, The Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China"
}
],
"family": "Cheng",
"given": "Biao",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy and the Center of Information, The Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China"
}
],
"family": "Chen",
"given": "Jian",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, The Third Hospital of Wuhan, Wuhan, China"
}
],
"family": "Peng",
"given": "Anlin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tongji School of Pharmacy, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China"
}
],
"family": "Yang",
"given": "Chen",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hubei Key Laboratory of Cell Homeostasis, College of Life Sciences, Wuhan University, Wuhan, China"
}
],
"family": "Liu",
"given": "Chong",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tongji School of Pharmacy, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China"
}
],
"family": "Xiong",
"given": "Mingrui",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy and the Center of Information, The Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China"
}
],
"family": "Deng",
"given": "Aiping",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tongji School of Pharmacy, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China"
}
],
"family": "Zhang",
"given": "Yu",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7918-6682",
"affiliation": [
{
"name": "Hubei Key Laboratory of Cell Homeostasis, College of Life Sciences, Wuhan University, Wuhan, China"
}
],
"authenticated-orcid": false,
"family": "Zheng",
"given": "Ling",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0808-2325",
"affiliation": [
{
"name": "Tongji School of Pharmacy, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China"
}
],
"authenticated-orcid": false,
"family": "Huang",
"given": "Kun",
"sequence": "additional"
}
],
"container-title": "Diabetes Care",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"diabetesjournals.org"
]
},
"created": {
"date-parts": [
[
2020,
5,
14
]
],
"date-time": "2020-05-14T18:16:51Z",
"timestamp": 1589480211000
},
"deposited": {
"date-parts": [
[
2022,
3,
13
]
],
"date-time": "2022-03-13T03:42:45Z",
"timestamp": 1647142965000
},
"funder": [
{
"DOI": "10.13039/501100012166",
"award": [
"2019YFA0802701",
"2018YFA0800700"
],
"doi-asserted-by": "crossref",
"name": "National Key R&D Program of China"
},
{
"DOI": "10.13039/501100001809",
"award": [
"91957114",
"31971066",
"31871381",
"31671195"
],
"doi-asserted-by": "publisher",
"name": "National Natural Science Foundation of China"
},
{
"award": [
"WX18M02"
],
"name": "Family Planning Commission of Wuhan"
}
],
"indexed": {
"date-parts": [
[
2024,
3,
29
]
],
"date-time": "2024-03-29T14:33:45Z",
"timestamp": 1711722825870
},
"is-referenced-by-count": 295,
"issue": "7",
"issued": {
"date-parts": [
[
2020,
5,
14
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2020,
5,
14
]
]
},
"published-print": {
"date-parts": [
[
2020,
7,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.diabetesjournals.org/content/license",
"content-version": "vor",
"delay-in-days": 36,
"start": {
"date-parts": [
[
2020,
6,
19
]
],
"date-time": "2020-06-19T00:00:00Z",
"timestamp": 1592524800000
}
}
],
"link": [
{
"URL": "http://care.diabetesjournals.org/syndication/doi/10.2337/dc20-0660",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://diabetesjournals.org/care/article-pdf/43/7/1399/630050/dc200660.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://diabetesjournals.org/care/article-pdf/43/7/1399/630050/dc200660.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1167",
"original-title": [],
"page": "1399-1407",
"prefix": "10.2337",
"published": {
"date-parts": [
[
2020,
5,
14
]
]
},
"published-online": {
"date-parts": [
[
2020,
5,
14
]
]
},
"published-print": {
"date-parts": [
[
2020,
7,
1
]
]
},
"publisher": "American Diabetes Association",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "2022031300271909000_B1",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"article-title": "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "1054",
"journal-title": "Lancet",
"key": "2022031300271909000_B2",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical characteristics of coronavirus disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"journal-title": "N Engl J Med",
"key": "2022031300271909000_B3",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2001316",
"article-title": "Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "1199",
"journal-title": "N Engl J Med",
"key": "2022031300271909000_B4",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1186/s40249-020-00646-x",
"article-title": "Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review",
"author": "Adhikari",
"doi-asserted-by": "crossref",
"first-page": "29",
"journal-title": "Infect Dis Poverty",
"key": "2022031300271909000_B5",
"volume": "9",
"year": "2020"
},
{
"article-title": "Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention",
"author": "Wu",
"journal-title": "JAMA",
"key": "2022031300271909000_B6"
},
{
"article-title": "A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias",
"author": "Zhao",
"journal-title": "Clin Infect Dis",
"key": "2022031300271909000_B7"
},
{
"article-title": "Development and clinical application of a rapid IgM-IgG combined antibody test for SARS-CoV-2 infection diagnosis",
"author": "Li",
"journal-title": "J Med Virol",
"key": "2022031300271909000_B8"
},
{
"author": "Li",
"key": "2022031300271909000_B9"
},
{
"key": "2022031300271909000_B10",
"unstructured": "National Health Commission of China. Diagnosis and treatment plan for COVID-19, 5th edition (in Chinese) [Internet], 2020. Available from http://www.nhc.gov.cn/xcs/zhengcwj/202002/3b09b894ac9b4204a79db5b8912d4440/files/7260301a393845fc87fcf6dd52965ecb.pdf. Accessed 27 March 2020"
},
{
"key": "2022031300271909000_B11",
"unstructured": "National Health Commission of China. Diagnosis and treatment plan for COVID-19, 6th edition (in Chinese) [Internet], 2020. Available from http://www.nhc.gov.cn/xcs/zhengcwj/202002/8334a8326dd94d329df351d7da8aefc2/files/b218cfeb1bc54639af227f922bf6b817.pdf. Accessed 27 March 2020"
},
{
"DOI": "10.1016/S0140-6736(20)30744-3",
"article-title": "Fangcang shelter hospitals: a novel concept for responding to public health emergencies [published correction appears in Lancet 2020]",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "1305",
"journal-title": "Lancet",
"key": "2022031300271909000_B12",
"volume": "395",
"year": "2020"
},
{
"article-title": "Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China",
"author": "Pan",
"journal-title": "JAMA",
"key": "2022031300271909000_B13"
},
{
"DOI": "10.1016/j.phrs.2017.06.005",
"article-title": "The vasoprotective axes of the renin-angiotensin system: physiological relevance and therapeutic implications in cardiovascular, hypertensive and kidney diseases",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "21",
"journal-title": "Pharmacol Res",
"key": "2022031300271909000_B14",
"volume": "125",
"year": "2017"
},
{
"DOI": "10.1128/JVI.00127-20",
"article-title": "Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus",
"author": "Wan",
"doi-asserted-by": "crossref",
"first-page": "e00127",
"journal-title": "J Virol",
"key": "2022031300271909000_B15",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(15)00379-4",
"article-title": "Diabetes and infection: assessing the association with glycaemic control in population-based studies",
"author": "Pearson-Stuttard",
"doi-asserted-by": "crossref",
"first-page": "148",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2022031300271909000_B16",
"volume": "4",
"year": "2016"
},
{
"DOI": "10.1007/s00125-018-4711-2",
"article-title": "Global trends in diabetes complications: a review of current evidence",
"author": "Harding",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "Diabetologia",
"key": "2022031300271909000_B17",
"volume": "62",
"year": "2019"
},
{
"DOI": "10.1046/j.1440-1843.2003.00518.x",
"article-title": "SARS: epidemiology",
"author": "Chan-Yeung",
"doi-asserted-by": "crossref",
"first-page": "S9",
"journal-title": "Respirology",
"key": "2022031300271909000_B18",
"volume": "8",
"year": "2003"
},
{
"DOI": "10.1111/j.1464-5491.2006.01861.x",
"article-title": "Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "623",
"journal-title": "Diabet Med",
"key": "2022031300271909000_B19",
"volume": "23",
"year": "2006"
},
{
"DOI": "10.1371/journal.pone.0165978",
"article-title": "A comparative study of clinical presentation and risk factors for adverse outcome in patients hospitalised with acute respiratory disease due to MERS coronavirus or other causes",
"author": "Garbati",
"doi-asserted-by": "crossref",
"first-page": "e0165978",
"journal-title": "PLoS One",
"key": "2022031300271909000_B20",
"volume": "11",
"year": "2016"
},
{
"DOI": "10.1172/jci.insight.131774",
"article-title": "Comorbid diabetes results in immune dysregulation and enhanced disease severity following MERS-CoV infection",
"author": "Kulcsar",
"doi-asserted-by": "crossref",
"first-page": "e131774",
"journal-title": "JCI Insight",
"key": "2022031300271909000_B21",
"volume": "4",
"year": "2019"
},
{
"DOI": "10.3389/fimmu.2018.02160",
"article-title": "Inflammation, a double-edge sword for cancer and other age-related diseases",
"author": "Gupta",
"doi-asserted-by": "crossref",
"first-page": "2160",
"journal-title": "Front Immunol",
"key": "2022031300271909000_B22",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.2337/dc08-1090",
"article-title": "Cross-sectional and prospective study of lung function in adults with type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) study: response to Yeh et al",
"author": "Teeter",
"doi-asserted-by": "crossref",
"first-page": "e82",
"journal-title": "Diabetes Care",
"key": "2022031300271909000_B23",
"volume": "31",
"year": "2008"
},
{
"DOI": "10.2337/dc07-1464",
"article-title": "Cross-sectional and prospective study of lung function in adults with type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) study",
"author": "Yeh",
"doi-asserted-by": "crossref",
"first-page": "741",
"journal-title": "Diabetes Care",
"key": "2022031300271909000_B24",
"volume": "31",
"year": "2008"
},
{
"DOI": "10.1016/j.annepidem.2017.11.004",
"article-title": "Low-grade systemic inflammation: a partial mediator of the relationship between diabetes and lung function",
"author": "Giovannelli",
"doi-asserted-by": "crossref",
"first-page": "26",
"journal-title": "Ann Epidemiol",
"key": "2022031300271909000_B25",
"volume": "28",
"year": "2018"
},
{
"article-title": "Effects of apelin peptides on diabetic complications",
"author": "Chen",
"first-page": "179",
"journal-title": "Curr Protein Pept Sci",
"key": "2022031300271909000_B26",
"volume": "19",
"year": "2018"
},
{
"DOI": "10.1016/j.dsx.2020.03.002",
"article-title": "Clinical considerations for patients with diabetes in times of COVID-19 epidemic",
"author": "Gupta",
"doi-asserted-by": "crossref",
"first-page": "211",
"journal-title": "Diabetes Metab Syndr",
"key": "2022031300271909000_B27",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30116-8",
"article-title": "Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection",
"author": "Fang",
"doi-asserted-by": "crossref",
"first-page": "e21",
"journal-title": "Lancet Respir Med",
"key": "2022031300271909000_B28",
"volume": "8",
"year": "2020"
}
],
"reference-count": 28,
"references-count": 28,
"relation": {},
"resource": {
"primary": {
"URL": "https://diabetesjournals.org/care/article/43/7/1399/35532/Clinical-Characteristics-and-Outcomes-of-Patients"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Advanced and Specialized Nursing",
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": "Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.2337/ada-journal-policies",
"volume": "43"
}
