Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis
et al., Frontiers in Medicine, doi:10.3389/fmed.2021.704666, Aug 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
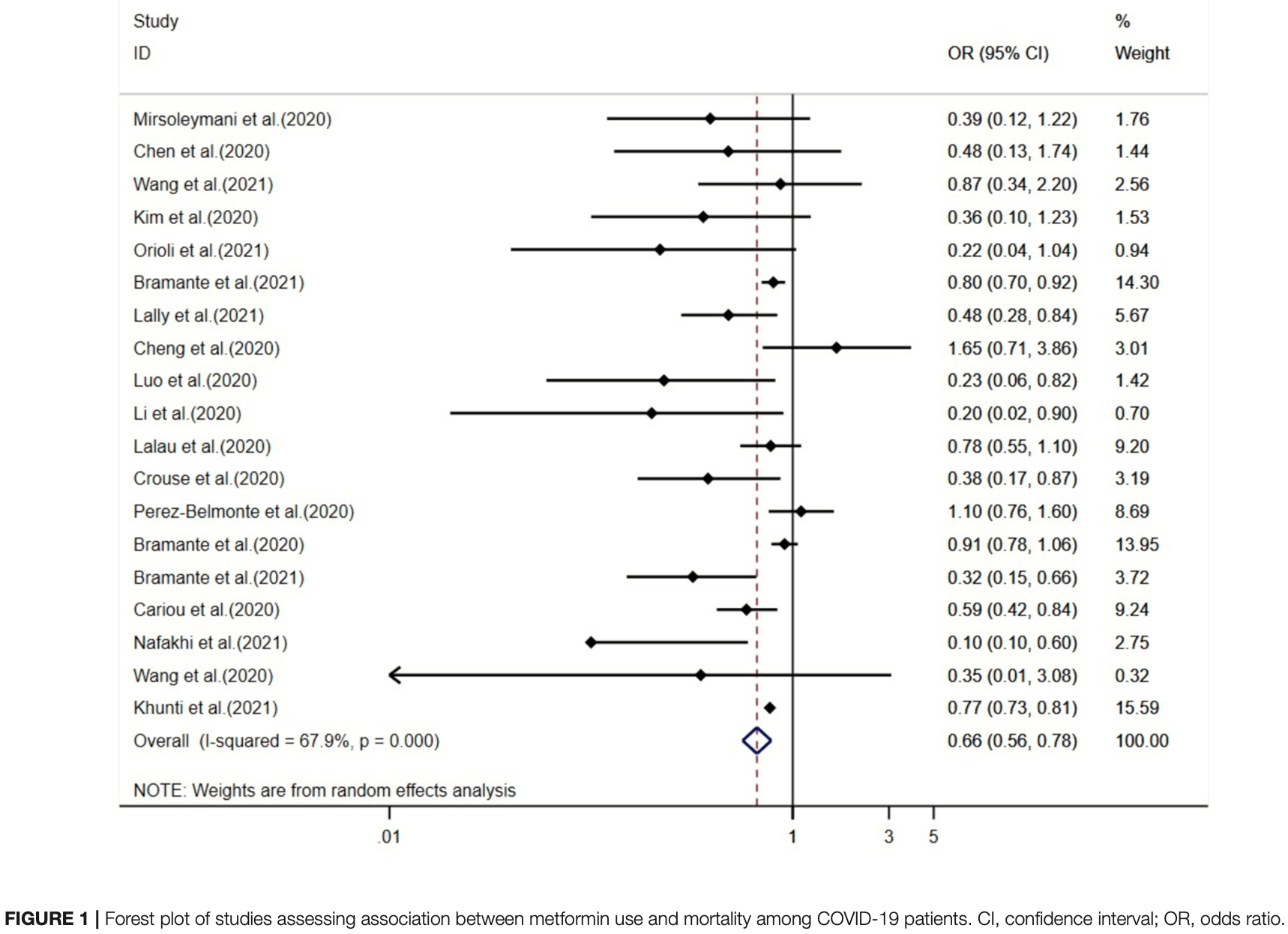
Meta analysis of 19 studies showing metformin use associated with lower COVID-19 mortality and hospitalization.
24 meta-analyses show significant improvements with metformin for mortality1-23,
hospitalization7,13,23 ,
progression1, and
severity8,9,13 .
Currently there are 110 metformin for COVID-19 studies, showing 36% lower mortality [32‑40%], 29% lower ventilation [12‑43%], 19% lower ICU admission [8‑28%], 17% lower hospitalization [11‑23%], and 5% fewer cases [-4‑13%].
|
risk of death, 34.0% lower, OR 0.66, p < 0.001, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Yang et al., The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus, Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2021.108977.
2.
Lukito et al., The Effect of Metformin Consumption on Mortality in Hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2020.11.006.
3.
Kow et al., Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis, Journal of Medical Virology, doi:10.1002/jmv.26498.
4.
Hariyanto et al., Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection, Obesity Medicine, doi:10.1016/j.obmed.2020.100290.
5.
Ma et al., Is metformin use associated with low mortality in patients with type 2 diabetes mellitus hospitalized for COVID-19? a multivariable and propensity score-adjusted meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0282210.
6.
Parveen et al., Association of Metformin with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis, Annals of the National Academy of Medical Sciences (India), doi:10.1055/s-0042-1760353.
7.
Li et al., Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Medicine, doi:10.3389/fmed.2021.704666.
8.
Schlesinger et al., Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis, Diabetologia, doi:10.1007/s00125-023-05928-1.
9.
Petrelli et al., Metformin and Covid-19: a systematic review of systematic reviews with meta-analysis, Acta Biomedica Atenei Parmensis, doi:10.23750/abm.v94iS3.14405.
10.
Oscanoa et al., Metformin therapy and severity and mortality of SARS-CoV-2 infection: a meta-analysis, Clinical Diabetology, doi:10.5603/DK.a2021.0035.
11.
Kan et al., Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2021.708494.
12.
Poly et al., Metformin Use Is Associated with Decreased Mortality in COVID-19 Patients with Diabetes: Evidence from Retrospective Studies and Biological Mechanism, Journal of Clinical Medicine, doi:10.3390/jcm10163507.
13.
Song et al., The Effect of Antihyperglycemic Medications on COVID-19: A Meta-analysis and Systematic Review from Observational Studies, Therapeutic Innovation & Regulatory Science, doi:10.1007/s43441-024-00633-6.
14.
Ganesh et al., Does metformin affect outcomes in COVID‐19 patients with new or pre‐existing diabetes mellitus? A systematic review and meta‐analysis, British Journal of Clinical Pharmacology, doi:10.1111/bcp.15258.
15.
Nassar et al., Noninsulin‐based antihyperglycemic medications in patients with diabetes and COVID‐19: A systematic review and meta‐analysis, Journal of Diabetes, doi:10.1111/1753-0407.13359.
16.
Zhan et al., Effect of Antidiabetic Therapy on Clinical Outcomes of COVID-19 Patients With Type 2 Diabetes: A Systematic Review and Meta-Analysis, Annals of Pharmacotherapy, doi:10.1177/10600280221133577.
17.
Nguyen et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196.
18.
Han et al., Association Between Anti-diabetic Agents and Clinical Outcomes of COVID-19 in Patients with Diabetes: A Systematic Review and Meta-Analysis, Archives of Medical Research, doi:10.1016/j.arcmed.2021.08.002.
19.
Chen et al., The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2022.895458.
20.
Scheen, A., Metformin and COVID-19: From cellular mechanisms to reduced mortality, Diabetes & Metabolism, doi:10.1016/j.diabet.2020.07.006.
21.
Sun et al., Is Metformin Use Associated With a Decreased Mortality for COVID-19 Diabetic Patients? A Meta-Analysis, Journal of the Endocrine Society, doi:10.1210/jendso/bvab048.709.
Li et al., 19 Aug 2021, peer-reviewed, 6 authors.
Contact: zhizeng_scu@yeaah.net, lisheyu@gmail.com.
Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis
Frontiers in Medicine, doi:10.3389/fmed.2021.704666
Importance/Background: The coronavirus disease (COVID-19) pandemic is a critical public health issue. Evidence has shown that metformin favorably influences COVID-19 outcomes. This study aimed to assess the benefits and risks of metformin in COVID-19 patients.
Methods: We searched the PubMed, Embase, Cochrane Library, and Chinese Biomedical Literature Database from inception to February 18, 2021. Observational studies assessing the association between metformin use and the outcomes of COVID-19 patients were included. The primary outcome was mortality, and the secondary outcomes included intubation, deterioration, and hospitalization. Random-effects weighted models were used to pool the specific effect sizes. Subgroup analyses were conducted by stratifying the meta-analysis by region, diabetic status, the adoption of multivariate model, age, risk of bias, and timing for adding metformin.
Results: We identified 28 studies with 2,910,462 participants. Meta-analysis of 19 studies showed that metformin is associated with 34% lower COVID-19 mortality [odds ratio (OR), 0.66; 95% confidence interval (CI), 0.56-0.78; I 2 = 67.9%] and 27% lower hospitalization rate (pooled OR, 0.73; 95% CI, 0.53-1.00; I 2 = 16.8%). However, we did not identify any subgroup effects. The meta-analysis did not identify statistically significant association between metformin and intubation and deterioration of COVID-19 (OR, 0.94; 95% CI, 0.77-1.16; I 2 = 0.0% for intubation and OR, 2.04; 95% CI, 0.65-6.34; I 2 = 79.4% for deterioration of COVID-19), respectively.
Conclusions: Metformin use among COVID-19 patients was associated with a reduced risk of mortality and hospitalization. Our findings suggest a relative benefit for metformin use in nursing home and hospitalized COVID-19 patients. However, randomized controlled trials are warranted to confirm the association between metformin use and COVID-19 outcomes.
AUTHOR CONTRIBUTIONS YL, ZZ, and SL: conception or design. YL, XY, PY, and TS: acquisition, analysis, or interpretation. YL, XY, PY, TS, ZZ, and SL: drafting the work or revision and final approval of the manuscript. All authors contributed to the article and approved the submitted version.
SUPPLEMENTARY MATERIAL The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed. 2021.704666/full#supplementary-material
Conflict of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Publisher's Note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Bonnet, Scheen, Understanding, and overcoming metformin gastrointestinal intolerance, Diabetes Obes Metab, doi:10.1111/dom.12854
Bramante, Buse, Tamaritz, Palacio, Cohen et al., Outpatient metformin use is associated with reduced severity of COVID-19 disease in adults with overweight or obesity, J Med Virol, doi:10.1002/jmv.26873
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis, Lancet Healthy Longev, doi:10.1016/S2666-7568(20)30033-7
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Observational study of metformin and risk of mortality in patients hospitalized with COVID-19, doi:10.1101/2020.06.19.20135095
Bramante, Tignanelli, Dutta, Jones, Tamariz et al., Non-alcoholic fatty liver disease (NAFLD) and risk of hospitalization for COVID-19, doi:10.1101/2020.09.01.20185850
Buse, Wexler, Tsapas, Rossing, Mingrone et al., update to: management of hyperglycemia in type 2 diabetes, 2018. a consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD), Diabetes Care, doi:10.2337/dci19-0066
Cancer, Fitzmaurice, Abate, Abbasi, Abbastabar et al., Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disabilityadjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the global burden of disease study, JAMA Oncol, doi:10.1001/jamaoncol.2019.2996
Cariou, Hadjadj, Wargny, Pichelin, Al-Salameh et al., Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Cheng, Liu, Zhang, Lei, Qin et al., Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.08.013
Choi, Ahn, Ryu, Kim, Jang et al., Clinical characteristics and disease progression in early-stage COVID-19 patients in South Korea, J Clin Med, doi:10.3390/jcm9061959
Clark, Jit, Warren-Gash, Guthrie, Wang et al., Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study, Lancet Global Health, doi:10.1016/S2214-109X(20)30264-3
Crouse, Grimes, Li, Might, Ovalle et al., Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes, Front Endocrinol, doi:10.3389/fendo.2020.600439
Do, Kim, Park, Cho, Kang, Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19?, Diabetes Metab, doi:10.1016/j.diabet.2020.10.006
Gao, Liu, Zhong, Liu, Zhou et al., Risk of metformin in patients with type 2 diabetes with COVID-19: a preliminary retrospective report, Clin Transl Sci, doi:10.1111/cts.12897
Garber, Handelsman, Grunberger, Einhorn, Abrahamson et al., Consensus statement by the American association of clinical endocrinologists and American college of endocrinology on the comprehensive ttype 2 diabetes management algorithm -2020 executive summary, Endocr Pract, doi:10.4158/cs-2019-0472
Griffin, Leaver, Irving, Impact of metformin on cardiovascular disease: a meta-analysis of randomised trials among people with type 2 diabetes, Diabetologia, doi:10.1007/s00125-017-4337-9
Guan, Ni, Hu, Liang, Ou et al., Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032
Hayek, Robert, Matar, Algarni, Alkubedan et al., Risk factors for hospital admission among COVID-19 patients with diabetes a study from Saudi Arabia, Saudi Med J, doi:10.15537/smj.2020.10.25419
Hoffmann, Kleine-Weber, Schroeder, Krüger, Herrler et al., SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Huang, Lim, Pranata, Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia -a systematic review, meta-analysis, and meta-regression, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.018
Izzi-Engbeaya, Distaso, Amin, Yang, Idowu et al., Adverse outcomes in COVID-19 and diabetes: a retrospective cohort study from three London teaching hospitals, BMJ Open Diabetes Res Care, doi:10.1136/bmjdrc-2020-001858
Jiang, Chen, Yin, Liu, Yang et al., Association of metformin with mortality or ARDS in patients with COVID-19 and type 2 diabetes: a retrospective cohort study, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108619
Khunti, Knighton, Zaccardi, Bakhai, Barron et al., Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00050-4
Kichloo, Albosta, Dettloff, Wani, El-Amir et al., Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA, Fam Med Community Health, doi:10.1136/fmch-2020-000530
Kim, Jeon, Moon, Cho, Han et al., The clinical characteristics and outcomes of patients with moderate-to-severe coronavirus disease 2019 infection and diabetes in daegu, South Korea, Diabetes Metab J, doi:10.4093/dmj.2020.0146
Kow, Hasan, Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: a meta-analysis, J Med Virol, doi:10.1002/jmv.26498
Lalau, Al-Salameh, Hadjadj, Goronflot, Wiernsperger et al., Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19, Diabetes Metab, doi:10.1016/j.diabet.2020.101216
Lalau, Kajbaf, Protti, Christensen, Broe, Metforminassociated lactic acidosis (MALA): moving towards a new paradigm, Diabetes Obes Metab, doi:10.1111/dom.12974
Lally, Tsoukas, Halladay, Neill, Gravenstein et al., Metformin is associated with decreased 30-day mortality among nursing home residents infected with SARS-CoV2, J Am Med Dir Assoc, doi:10.1016/j.jamda.2020.10.031
Li, Nemeth, Donnelly, Hapca, Zhou et al., Visit-to-visit HbA1c variability is associated with cardiovascular disease and microvascular complications in patients with newly diagnosed type 2 diabetes, Diabetes Care, doi:10.2337/dc19-0823
Li, Wei, Li, Mccowen, Xiong et al., Metformin use in diabetes prior to hospitalization: effects on mortality in COVID-19, Endocr Pract, doi:10.4158/EP-2020-0466
Li, Zong, Sun, Li, New evidence-based clinical practice guideline timely supports hospital infection control of coronavirus disease 2019, Precis Clin Med, doi:10.1093/pcmedi/pbaa008
Liu, Bai, Han, Jiang, Qiu et al., The association of diabetes and the prognosis of COVID-19 patients: a retrospective study, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108386
Liu, Li, Quan, Li, Vitamin B12 status in metformin treated patients: systematic review, PLoS ONE, doi:10.1371/journal.pone.0100379
Lukito, Pranata, Henrina, Lim, Lawrensia et al., The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.11.006
Luo, Qiu, Liu, Liu, Zheng et al., Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am J Trop Med Hyg, doi:10.4269/ajtmh.20-0375
Matsiukevich, Piraino, Lahni, Hake, Wolfe et al., Metformin ameliorates gender-and age-dependent hemodynamic instability and myocardial injury in murine hemorrhagic shock, Biochim Biophys Acta Mol Basis Dis, doi:10.1016/j.bbadis.2017.05.027
Mccreight, Bailey, Pearson, Metformin, and the gastrointestinal tract, Diabetologia, doi:10.1007/s00125-015-3844-9
Mirsoleymani, Nekooghadam, Marzaleh, Peyravi, Soltani et al., Assessment of risk factors for severe coronavirus disease 2019 among Iranian patients, Iran Red Crescent Med J, doi:10.32592/ircmj.2020.22.9.72
Moher, Liberati, Tetzlaff, Altman, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, PLoS Med, doi:10.1371/journal.pmed.1000097
Nafakhi, Alareedh, Al-Buthabhak, Shaghee, Nafakhi et al., Predictors of adverse in-hospital outcome and recovery in patients with diabetes mellitus and COVID-19 pneumonia in Iraq, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.12.014
Orioli, Servais, Belkhir, Laterre, Thissen et al., Clinical characteristics and short-term prognosis of in-patients with diabetes and COVID-19: a retrospective study from an academic center in Belgium, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.12.020
Palmer, Tendal, Mustafa, Vandvik, Li et al., Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials, BMJ, doi:10.1136/bmj.m4573
Park, Lee, Park, Park, Cheon et al., Sex-dependent difference in the effect of metformin on colorectal cancer-specific mortality of diabetic colorectal cancer patients, World J Gastroenterol, doi:10.3748/wjg.v23.i28.5196
Perez-Belmonte, Torres-Pena, Lopez-Carmona, Ayala-Gutierrez, Fuentes-Jimenez et al., Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: a nationwide cohort study, BMC Med, doi:10.1186/s12916-020-01832-2
Petrie, Rossing, Campbell, Metformin, and cardiorenal outcomes in diabetes: a reappraisal, Diabetes Obes Metab, doi:10.1111/dom.13984
Simonnet, Chetboun, Poissy, Raverdy, Noulette et al., High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation, Obesity, doi:10.1002/oby.22831
Stang, Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses, Eur J Epidemiol, doi:10.1007/s10654-010-9491-z
Tan, Wang, Liu, Shi, Zhou et al., Long-acting metformin vs. Metformin immediate release in patients with type 2 diabetes: a systematic review, Front Pharmacol, doi:10.3389/fphar.2021.669814
Ursini, Ciaffi, Landini, Meliconi, COVID-19, and diabetes: Is metformin a friend or foe?, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108167
Vj, Illescas-Montes, Puerta-Puerta, Ruiz, Melguizo-Rodríguez, SARS-CoV-2 infection: the role of cytokines in COVID-19 disease, Cytokine Growth Factor Rev, doi:10.1016/j.cytogfr.2020.06.001
Wang, Cooper, Gokhale, Acosta-Mena, Dhalla et al., Association of metformin with susceptibility to COVID-19 in people with type 2 diabetes, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab067
Wang, Gao, Zhang, Huang, Zhang et al., Prevalence ethnic pattern of diabetes prediabetes in China in 2013, JAMA, doi:10.1001/jama.2017.7596
Wang, Van Oekelen, Mouhieddine, Valle, Richter et al., A tertiary center experience of multiple myeloma patients with COVID-19: lessons learned and the path forward, J Hematol Oncol, doi:10.1186/s13045-020-00934-x
Yang, Tao, Peng, Zhao, Li et al., High-sensitivity C-reactive protein and risk of type 2 diabetes: a nationwide cohort study and updated meta-analysis, Diabetes Metab Res Rev, doi:10.1002/dmrr.3446
Yitao, Mu, Ling, Shiyao, Jiaojie et al., Predictors of clinical deterioration in non-severe patients with COVID-19: a retrospective cohort study, Curr Med Res Opin, doi:10.1080/03007995.2021.1876005
Zhang, Dong, Martin, He, Gongol et al., AMPactivated protein kinase phosphorylation of angiotensin-converting enzyme 2 in endothelium mitigates pulmonary hypertension, Am J Respir Crit Care Med, doi:10.1164/rccm.201712-2570OC
Zhang, Li, Li, Li, Ren et al., Metformin treatment and homocysteine: a systematic review and meta-analysis of randomized controlled trials, Nutrients, doi:10.3390/nu8120798
Zhang, Wang, Zhu, Mao, Bai et al., Risk factors for poor outcomes of diabetes patients with COVID-19: a single-center, retrospective study in early outbreak in China, Front Endocrinol, doi:10.3389/fendo.2020.571037
Zhou, Zhang, Zhang, Zhou, Li et al., Population diversity of cardiovascular outcome trials and real-world patients with diabetes in a Chinese tertiary hospital, Chin Med J, doi:10.1097/CM9.0000000000001407
Zhu, Zhong, Li, Li, Pang, Clinicopathological characteristics of 8697 patients with COVID-19 in China: a meta-analysis, Fam Med Community Health, doi:10.1136/fmch-2020-000406
DOI record:
{
"DOI": "10.3389/fmed.2021.704666",
"ISSN": [
"2296-858X"
],
"URL": "http://dx.doi.org/10.3389/fmed.2021.704666",
"abstract": "<jats:p><jats:bold>Importance/Background:</jats:bold> The coronavirus disease (COVID-19) pandemic is a critical public health issue. Evidence has shown that metformin favorably influences COVID-19 outcomes. This study aimed to assess the benefits and risks of metformin in COVID-19 patients.</jats:p><jats:p><jats:bold>Methods:</jats:bold> We searched the PubMed, Embase, Cochrane Library, and Chinese Biomedical Literature Database from inception to February 18, 2021. Observational studies assessing the association between metformin use and the outcomes of COVID-19 patients were included. The primary outcome was mortality, and the secondary outcomes included intubation, deterioration, and hospitalization. Random-effects weighted models were used to pool the specific effect sizes. Subgroup analyses were conducted by stratifying the meta-analysis by region, diabetic status, the adoption of multivariate model, age, risk of bias, and timing for adding metformin.</jats:p><jats:p><jats:bold>Results:</jats:bold> We identified 28 studies with 2,910,462 participants. Meta-analysis of 19 studies showed that metformin is associated with 34% lower COVID-19 mortality [odds ratio (OR), 0.66; 95% confidence interval (CI), 0.56–0.78; <jats:italic>I</jats:italic><jats:sup>2</jats:sup> = 67.9%] and 27% lower hospitalization rate (pooled OR, 0.73; 95% CI, 0.53–1.00; <jats:italic>I</jats:italic><jats:sup>2</jats:sup> = 16.8%). However, we did not identify any subgroup effects. The meta-analysis did not identify statistically significant association between metformin and intubation and deterioration of COVID-19 (OR, 0.94; 95% CI, 0.77–1.16; <jats:italic>I</jats:italic><jats:sup>2</jats:sup> = 0.0% for intubation and OR, 2.04; 95% CI, 0.65–6.34; <jats:italic>I</jats:italic><jats:sup>2</jats:sup> = 79.4% for deterioration of COVID-19), respectively.</jats:p><jats:p><jats:bold>Conclusions:</jats:bold> Metformin use among COVID-19 patients was associated with a reduced risk of mortality and hospitalization. Our findings suggest a relative benefit for metformin use in nursing home and hospitalized COVID-19 patients. However, randomized controlled trials are warranted to confirm the association between metformin use and COVID-19 outcomes.</jats:p><jats:p><jats:bold>Study Registration:</jats:bold> The study was registered on the PROSPERO on Feb 23, 2021 (CRD42021238722).</jats:p>",
"alternative-id": [
"10.3389/fmed.2021.704666"
],
"author": [
{
"affiliation": [],
"family": "Li",
"given": "Yin",
"sequence": "first"
},
{
"affiliation": [],
"family": "Yang",
"given": "Xue",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yan",
"given": "Peijing",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sun",
"given": "Tong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zeng",
"given": "Zhi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Sheyu",
"sequence": "additional"
}
],
"container-title": "Frontiers in Medicine",
"container-title-short": "Front. Med.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2021,
8,
19
]
],
"date-time": "2021-08-19T08:30:04Z",
"timestamp": 1629361804000
},
"deposited": {
"date-parts": [
[
2021,
8,
19
]
],
"date-time": "2021-08-19T08:30:08Z",
"timestamp": 1629361808000
},
"funder": [
{
"DOI": "10.13039/501100004829",
"doi-asserted-by": "publisher",
"name": "Department of Science and Technology of Sichuan Province"
},
{
"DOI": "10.13039/501100013365",
"doi-asserted-by": "publisher",
"name": "West China Hospital, Sichuan University"
}
],
"indexed": {
"date-parts": [
[
2023,
4,
25
]
],
"date-time": "2023-04-25T18:02:49Z",
"timestamp": 1682445769071
},
"is-referenced-by-count": 22,
"issued": {
"date-parts": [
[
2021,
8,
19
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
19
]
],
"date-time": "2021-08-19T00:00:00Z",
"timestamp": 1629331200000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2021.704666/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2021,
8,
19
]
]
},
"published-online": {
"date-parts": [
[
2021,
8,
19
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"key": "B1",
"unstructured": "COVID-19 Coronavirus Pandemic"
},
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical characteristics of coronavirus disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "publisher",
"first-page": "1708",
"journal-title": "N Engl J Med.",
"key": "B2",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1136/fmch-2020-000406",
"article-title": "Clinicopathological characteristics of 8697 patients with COVID-19 in China: a meta-analysis",
"author": "Zhu",
"doi-asserted-by": "publisher",
"first-page": "e000406",
"journal-title": "Fam Med Community Health.",
"key": "B3",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1136/fmch-2020-000530",
"article-title": "Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA",
"author": "Kichloo",
"doi-asserted-by": "publisher",
"first-page": "e000530",
"journal-title": "Fam Med Community Health.",
"key": "B4",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1093/pcmedi/pbaa008",
"article-title": "New evidence-based clinical practice guideline timely supports hospital infection control of coronavirus disease 2019",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Precis Clin Med.",
"key": "B5",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1001/jama.2017.7596",
"article-title": "Prevalence ethnic pattern of diabetes prediabetes in China in 2013",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "2515",
"journal-title": "JAMA.",
"key": "B6",
"volume": "317",
"year": "2017"
},
{
"DOI": "10.1001/jamaoncol.2019.2996",
"article-title": "Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the global burden of disease study",
"doi-asserted-by": "publisher",
"first-page": "1749",
"journal-title": "JAMA Oncol.",
"key": "B7",
"volume": "5",
"year": "2019"
},
{
"DOI": "10.1097/CM9.0000000000001407",
"article-title": "Population diversity of cardiovascular outcome trials and real-world patients with diabetes in a Chinese tertiary hospital",
"author": "Zhou",
"doi-asserted-by": "publisher",
"first-page": "1317",
"journal-title": "Chin Med J.",
"key": "B8",
"volume": "134",
"year": "2021"
},
{
"DOI": "10.1016/S2214-109X(20)30264-3",
"article-title": "Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study",
"author": "Clark",
"doi-asserted-by": "publisher",
"first-page": "e1003",
"journal-title": "Lancet Global Health.",
"key": "B9",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.2337/dc19-0823",
"article-title": "Visit-to-visit HbA1c variability is associated with cardiovascular disease and microvascular complications in patients with newly diagnosed type 2 diabetes",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "426",
"journal-title": "Diabetes Care.",
"key": "B10",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1002/oby.22831",
"article-title": "High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation",
"author": "Simonnet",
"doi-asserted-by": "publisher",
"first-page": "1195",
"journal-title": "Obesity.",
"key": "B11",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.018",
"article-title": "Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia - a systematic review, meta-analysis, and meta-regression",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "395",
"journal-title": "Diabetes Metab Syndr.",
"key": "B12",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m4573",
"article-title": "Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials",
"author": "Palmer",
"doi-asserted-by": "publisher",
"first-page": "m4573",
"journal-title": "BMJ.",
"key": "B13",
"volume": "372",
"year": "2021"
},
{
"DOI": "10.4158/cs-2019-0472",
"article-title": "Consensus statement by the American association of clinical endocrinologists and American college of endocrinology on the comprehensive ttype 2 diabetes management algorithm – 2020 executive summary",
"author": "Garber",
"doi-asserted-by": "publisher",
"first-page": "107",
"journal-title": "Endocr Pract.",
"key": "B14",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.2337/dci19-0066",
"article-title": "2019 update to: management of hyperglycemia in type 2 diabetes, 2018. a consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD)",
"author": "Buse",
"doi-asserted-by": "publisher",
"first-page": "487",
"journal-title": "Diabetes Care",
"key": "B15",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1007/s00125-017-4337-9",
"article-title": "Impact of metformin on cardiovascular disease: a meta-analysis of randomised trials among people with type 2 diabetes",
"author": "Griffin",
"doi-asserted-by": "publisher",
"first-page": "1620",
"journal-title": "Diabetologia.",
"key": "B16",
"volume": "60",
"year": "2017"
},
{
"DOI": "10.1111/dom.13984",
"article-title": "Metformin, and cardiorenal outcomes in diabetes: a reappraisal",
"author": "Petrie",
"doi-asserted-by": "publisher",
"first-page": "904",
"journal-title": "Diabetes Obes Metab.",
"key": "B17",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"article-title": "Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England",
"author": "Khunti",
"doi-asserted-by": "publisher",
"first-page": "293",
"journal-title": "Lancet Diabetes Endocrinol.",
"key": "B18",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.11.006",
"article-title": "The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis",
"author": "Lukito",
"doi-asserted-by": "publisher",
"first-page": "2177",
"journal-title": "Diabetes Metab Syndr.",
"key": "B19",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26498",
"article-title": "Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: a meta-analysis",
"author": "Kow",
"doi-asserted-by": "publisher",
"first-page": "695",
"journal-title": "J Med Virol.",
"key": "B20",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1371/journal.pmed.1000097",
"article-title": "Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement",
"author": "Moher",
"doi-asserted-by": "publisher",
"first-page": "e1000097",
"journal-title": "PLoS Med.",
"key": "B21",
"volume": "6",
"year": "2009"
},
{
"DOI": "10.1007/s10654-010-9491-z",
"article-title": "Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses",
"doi-asserted-by": "publisher",
"first-page": "603",
"journal-title": "Eur J Epidemiol.",
"key": "B22",
"volume": "25",
"year": "2010"
},
{
"DOI": "10.1002/dmrr.3446",
"article-title": "High-sensitivity C-reactive protein and risk of type 2 diabetes: a nationwide cohort study and updated meta-analysis",
"author": "Yang",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab Res Rev.",
"key": "B23",
"year": "2021"
},
{
"DOI": "10.1016/S2666-7568(20)30033-7",
"article-title": "Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis",
"author": "Bramante",
"doi-asserted-by": "publisher",
"first-page": "e34",
"journal-title": "Lancet Healthy Longev.",
"key": "B24",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1016/j.jamda.2020.10.031",
"article-title": "Metformin is associated with decreased 30-day mortality among nursing home residents infected with SARS-CoV2",
"author": "Lally",
"doi-asserted-by": "publisher",
"first-page": "193",
"journal-title": "J Am Med Dir Assoc.",
"key": "B25",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.12.014",
"article-title": "Predictors of adverse in-hospital outcome and recovery in patients with diabetes mellitus and COVID-19 pneumonia in Iraq",
"author": "Nafakhi",
"doi-asserted-by": "publisher",
"first-page": "33",
"journal-title": "Diabetes Metab Syndr.",
"key": "B26",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.12.020",
"article-title": "Clinical characteristics and short-term prognosis of in-patients with diabetes and COVID-19: a retrospective study from an academic center in Belgium",
"author": "Orioli",
"doi-asserted-by": "publisher",
"first-page": "149",
"journal-title": "Diabetes Metab Syndr.",
"key": "B27",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgab067",
"article-title": "Association of metformin with susceptibility to COVID-19 in people with type 2 diabetes",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "dgab067",
"journal-title": "J Clin Endocrinol Metab.",
"key": "B28",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.15537/smj.2020.10.25419",
"article-title": "Risk factors for hospital admission among COVID-19 patients with diabetes a study from Saudi Arabia",
"author": "Al Hayek",
"doi-asserted-by": "publisher",
"first-page": "1090",
"journal-title": "Saudi Med J.",
"key": "B29",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1101/2020.09.01.20185850",
"article-title": "Non-alcoholic fatty liver disease (NAFLD) and risk of hospitalization for COVID-19",
"author": "Bramante",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv [Preprint].",
"key": "B30",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26873",
"article-title": "Outpatient metformin use is associated with reduced severity of COVID-19 disease in adults with overweight or obesity",
"author": "Bramante",
"doi-asserted-by": "publisher",
"first-page": "4273",
"journal-title": "J Med Virol.",
"key": "B31",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1101/2020.06.19.20135095",
"article-title": "Observational study of metformin and risk of mortality in patients hospitalized with COVID-19",
"author": "Bramante",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv [Preprint].",
"key": "B32",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"article-title": "Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study",
"author": "Cariou",
"doi-asserted-by": "publisher",
"first-page": "1500",
"journal-title": "Diabetologia.",
"key": "B33",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.08.013",
"article-title": "Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and pre-existing type 2 diabetes",
"author": "Cheng",
"doi-asserted-by": "publisher",
"first-page": "537",
"journal-title": "Cell Metab.",
"key": "B34",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.3390/jcm9061959",
"article-title": "Clinical characteristics and disease progression in early-stage COVID-19 patients in South Korea",
"author": "Choi",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Clin Med.",
"key": "B35",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3389/fendo.2020.600439",
"article-title": "Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes",
"author": "Crouse",
"doi-asserted-by": "publisher",
"first-page": "600439",
"journal-title": "Front Endocrinol.",
"key": "B36",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.10.006",
"article-title": "Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19?",
"author": "Do",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab.",
"key": "B37",
"year": "2020"
},
{
"DOI": "10.1111/cts.12897",
"article-title": "Risk of metformin in patients with type 2 diabetes with COVID-19: a preliminary retrospective report",
"author": "Gao",
"doi-asserted-by": "publisher",
"first-page": "1055",
"journal-title": "Clin Transl Sci.",
"key": "B38",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1136/bmjdrc-2020-001858",
"article-title": "Adverse outcomes in COVID-19 and diabetes: a retrospective cohort study from three London teaching hospitals",
"author": "Izzi-Engbeaya",
"doi-asserted-by": "publisher",
"first-page": "e001858",
"journal-title": "BMJ Open Diabetes Res Care.",
"key": "B39",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.diabres.2020.108619",
"article-title": "Association of metformin with mortality or ARDS in patients with COVID-19 and type 2 diabetes: a retrospective cohort study",
"author": "Jiang",
"doi-asserted-by": "publisher",
"first-page": "108619",
"journal-title": "Diabetes Res Clin Pract.",
"key": "B40",
"volume": "173",
"year": "2021"
},
{
"DOI": "10.4093/dmj.2020.0146",
"article-title": "The clinical characteristics and outcomes of patients with moderate-to-severe coronavirus disease 2019 infection and diabetes in daegu, South Korea",
"author": "Kim",
"doi-asserted-by": "publisher",
"first-page": "602",
"journal-title": "Diabetes Metab J.",
"key": "B41",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.4158/EP-2020-0466",
"article-title": "Metformin use in diabetes prior to hospitalization: effects on mortality in COVID-19",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "1166",
"journal-title": "Endocr Pract.",
"key": "B42",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108386",
"article-title": "The association of diabetes and the prognosis of COVID-19 patients: a retrospective study",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "108386",
"journal-title": "Diabetes Res Clin Pract.",
"key": "B43",
"volume": "169",
"year": "2020"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"article-title": "Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis",
"author": "Luo",
"doi-asserted-by": "publisher",
"first-page": "69",
"journal-title": "Am J Trop Med Hyg.",
"key": "B44",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.32592/ircmj.2020.22.9.72",
"article-title": "Assessment of risk factors for severe coronavirus disease 2019 among Iranian patients",
"author": "Mirsoleymani",
"doi-asserted-by": "publisher",
"first-page": "e72",
"journal-title": "Iran Red Crescent Med J.",
"key": "B45",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1186/s12916-020-01832-2",
"article-title": "Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: a nationwide cohort study",
"author": "Perez-Belmonte",
"doi-asserted-by": "publisher",
"first-page": "359",
"journal-title": "BMC Med.",
"key": "B46",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1186/s13045-020-00934-x",
"article-title": "A tertiary center experience of multiple myeloma patients with COVID-19: lessons learned and the path forward",
"author": "Wang",
"doi-asserted-by": "publisher",
"first-page": "94",
"journal-title": "J Hematol Oncol.",
"key": "B47",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1080/03007995.2021.1876005",
"article-title": "Predictors of clinical deterioration in non-severe patients with COVID-19: a retrospective cohort study",
"author": "Yitao",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Curr Med Res Opin.",
"key": "B48",
"volume": "37",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2020.571037",
"article-title": "Risk factors for poor outcomes of diabetes patients with COVID-19: a single-center, retrospective study in early outbreak in China",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "571037",
"journal-title": "Front Endocrinol.",
"key": "B49",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1111/dom.12854",
"article-title": "Understanding, and overcoming metformin gastrointestinal intolerance",
"author": "Bonnet",
"doi-asserted-by": "publisher",
"first-page": "473",
"journal-title": "Diabetes Obes Metab.",
"key": "B50",
"volume": "19",
"year": "2017"
},
{
"DOI": "10.1016/j.diabet.2020.101216",
"article-title": "Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19",
"author": "Lalau",
"doi-asserted-by": "publisher",
"first-page": "101216",
"journal-title": "Diabetes Metab.",
"key": "B51",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1111/dom.12974",
"article-title": "Metformin-associated lactic acidosis (MALA): moving towards a new paradigm",
"author": "Lalau",
"doi-asserted-by": "publisher",
"first-page": "1502",
"journal-title": "Diabetes Obes Metab.",
"key": "B52",
"volume": "19",
"year": "2017"
},
{
"DOI": "10.1007/s00125-015-3844-9",
"article-title": "Metformin, and the gastrointestinal tract",
"author": "McCreight",
"doi-asserted-by": "publisher",
"first-page": "426",
"journal-title": "Diabetologia.",
"key": "B53",
"volume": "59",
"year": "2016"
},
{
"DOI": "10.1371/journal.pone.0100379",
"article-title": "Vitamin B12 status in metformin treated patients: systematic review",
"author": "Liu",
"doi-asserted-by": "publisher",
"first-page": "e100379",
"journal-title": "PLoS ONE.",
"key": "B54",
"volume": "9",
"year": "2014"
},
{
"DOI": "10.3390/nu8120798",
"article-title": "Metformin treatment and homocysteine: a systematic review and meta-analysis of randomized controlled trials",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "798",
"journal-title": "Nutrients.",
"key": "B55",
"volume": "8",
"year": "2016"
},
{
"DOI": "10.3389/fphar.2021.669814",
"article-title": "Long-acting metformin vs. Metformin immediate release in patients with type 2 diabetes: a systematic review",
"author": "Tan",
"doi-asserted-by": "publisher",
"first-page": "669814",
"journal-title": "Front Pharmacol.",
"key": "B56",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "publisher",
"first-page": "271",
"journal-title": "Cell.",
"key": "B57",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1164/rccm.201712-2570OC",
"article-title": "AMP-activated protein kinase phosphorylation of angiotensin-converting enzyme 2 in endothelium mitigates pulmonary hypertension",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "509",
"journal-title": "Am J Respir Crit Care Med.",
"key": "B58",
"volume": "198",
"year": "2018"
},
{
"DOI": "10.1016/j.diabres.2020.108167",
"article-title": "COVID-19, and diabetes: Is metformin a friend or foe?",
"author": "Ursini",
"doi-asserted-by": "publisher",
"first-page": "108167",
"journal-title": "Diabetes Res Clin Pract.",
"key": "B59",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.1016/j.cytogfr.2020.06.001",
"article-title": "SARS-CoV-2 infection: the role of cytokines in COVID-19 disease",
"author": "Costela-Ruiz",
"doi-asserted-by": "publisher",
"first-page": "62",
"journal-title": "Cytokine Growth Factor Rev.",
"key": "B60",
"volume": "54",
"year": "2020"
},
{
"DOI": "10.1016/j.bbadis.2017.05.027",
"article-title": "Metformin ameliorates gender-and age-dependent hemodynamic instability and myocardial injury in murine hemorrhagic shock",
"author": "Matsiukevich",
"doi-asserted-by": "publisher",
"first-page": "2680",
"journal-title": "Biochim Biophys Acta Mol Basis Dis.",
"key": "B61",
"volume": "1863",
"year": "2017"
},
{
"DOI": "10.3748/wjg.v23.i28.5196",
"article-title": "Sex-dependent difference in the effect of metformin on colorectal cancer-specific mortality of diabetic colorectal cancer patients",
"author": "Park",
"doi-asserted-by": "publisher",
"first-page": "5196",
"journal-title": "World J Gastroenterol.",
"key": "B62",
"volume": "23",
"year": "2017"
}
],
"reference-count": 62,
"references-count": 62,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fmed.2021.704666/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": "Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "8"
}
