Metformin Is Associated with Higher Incidence of Acidosis, but Not Mortality, in Individuals with COVID-19 and Pre-existing Type 2 Diabetes
et al., Cell Metabolism, doi:10.1016/j.cmet.2020.08.013, Aug 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
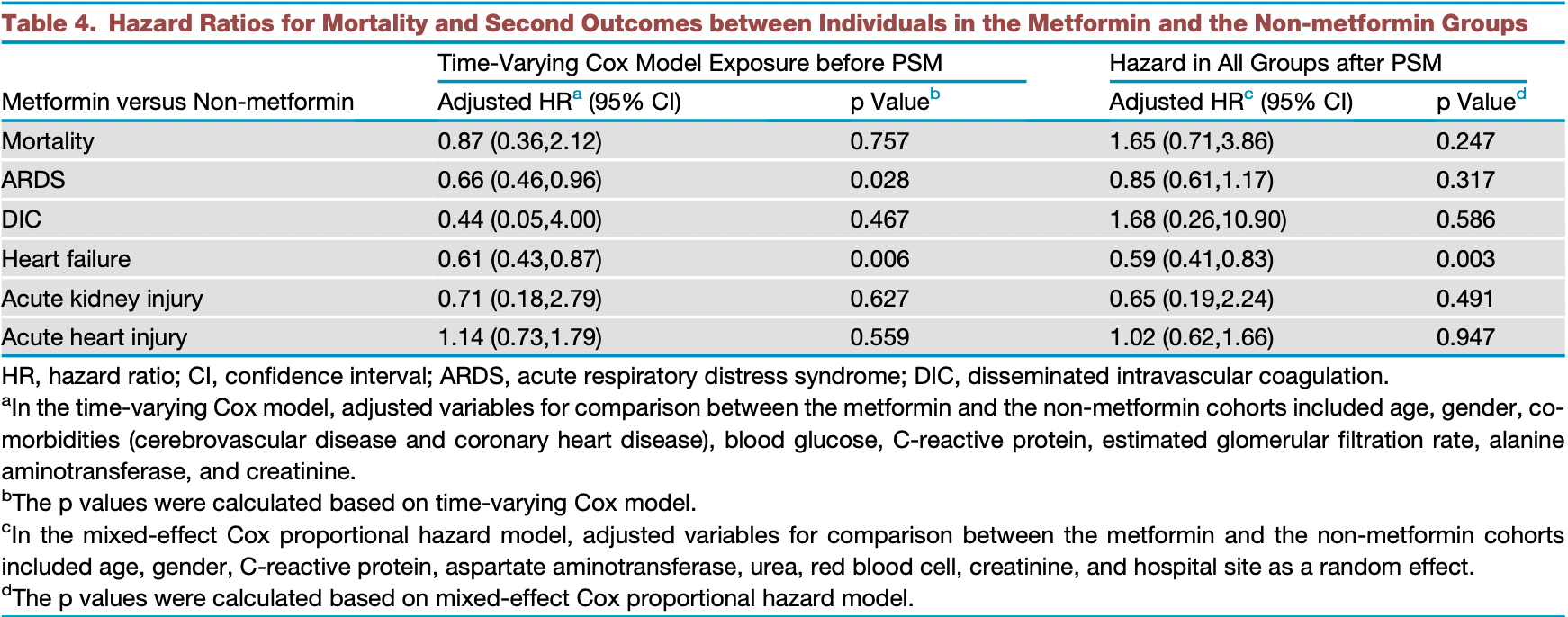
Retrospective 1,213 hospitalized diabetic COVID-19 patients in China, showing no significant difference in mortality with pre-existing metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
risk of death, 65.0% higher, HR 1.65, p = 0.25, treatment 678, control 535, after PSM.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Cheng et al., 20 Aug 2021, retrospective, propensity score matching, China, peer-reviewed, 35 authors.
Metformin Is Associated with Higher Incidence of Acidosis, but Not Mortality, in Individuals with COVID-19 and Pre-existing Type 2 Diabetes
Cell Metabolism, doi:10.1016/j.cmet.2020.08.013
Highlights d A retrospective study of 1,213 patients on metformin with COVID-19 was performed d Metformin was associated with increased incidence of acidosis in such patients d Metformin was not associated with increased 28-day allcause mortality in the patients d Metformin was significantly associated with reduced heart failure and inflammation
AUTHOR CONTRIBUTIONS X.C., Y.-M.L., Haomiao Li, X.Z., and F.L. designed the study, collected and analyzed data, and wrote the manuscript. Z.C., K.-Q.D., L.L., M.-M.C., X.S., M.X., Xuewei Huang, W.L., P.Z., P.Y., W.M., Xiaodong Huang, J.X., B.-H.Z., J.G., L.Z., and Z.L. collected, reviewed, interpreted, and checked clinical, laboratory, and radiological data. J.-J.Q. and F.Z. performed the statistical analysis. J.C., X.-J.Z., Y.W., X.M., Q.X., X.Z., and J.Y. wrote and edited the manuscript and provided valuable suggestions for study design and data analysis. Y.Y., X.W., Z.-G.S., Y.-X.J., and Hongliang Li contributed equally, designed the project, edited manuscript, and supervised the study. All authors have approved the final version of this paper.
DECLARATION OF INTERESTS We have no competing interests to declare.
Supplementary Information
Metformin Is Associated with Higher Incidence of Acidosis, but not Mortality, in Individuals Abbreviation: SBP, systolic blood pressure; DBP, Diastolic blood pressure; SpO2, oxygen saturation; RBC, red blood cells; ALT, alanine aminotransferase; eGFR, estimated glomerular filtration rate; LDL-c, low density lipoprotein cholesterol; IQR, interquartile range; SD, standardized difference. a Upper limit of normal (ULN) was defined according to criteria in each hospital. b Individuals with T2D taking Metformin during hospitalization were enrolled in the Metformin cohort. Individuals discontinued treatment of diabetes due to inability to..
References
Acc/Aha, /HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America, Circulation
Amin, Lux, 'callaghan, The journey of metformin from glycaemic control to mTOR inhibition and the suppression of tumour growth, Br. J. Clin. Pharmacol
Bailey, Metformin: historical overview, Diabetologia
Bakker, Coffernils, Leon, Gris, Vincent, Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock, Chest
Bates, Matrix-1
Bodmer, Meier, Kr€ Ahenb€ Uhl, Jick, Meier, None
Bornstein, Rubino, Khunti, Mingrone, Hopkins et al., Metformin, sulfonylureas, or other antidiabetes drugs and the risk of lactic acidosis or hypoglycemia: a nested case-control analysis, Lancet Diabetes Endocrinol
Bowker, Yasui, Veugelers, Johnson, Glucoselowering agents and cancer mortality rates in type 2 diabetes: assessing effects of time-varying exposure, Diabetologia
Cameron, Morrison, Levin, Mohan, Forteath et al., Lactic acidosis and severe septic shock in metformin users: a cohort study
Daniel, None
Dbp, Diastolic blood pressure; SpO2, oxygen saturation; RBC, red blood cells
Foretz, Guigas, Bertrand, Pollak, Viollet, Metformin: from mechanisms of action to therapies, Cell Metab
Fox, None
Gando, Wada, Thachil, Haneuse, Vanderweele et al., Differentiating disseminated intravascular coagulation (DIC) with the fibrinolytic phenotype from coagulopathy of trauma and acute coagulopathy of trauma-shock (COT/ACOTS), J. Thromb. Haemost
Harrell, Jr, Califf, Pryor, Lee et al., Evaluating the yield of medical tests, JAMA
Harrell, None
Harrell, Rms-6
Hoffmann, Kleine-Weber, Schroeder, Kr€ Uger, Herrler et al., None
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Imai, Kuba, Rao, Huan, Guo et al., Angiotensin-converting enzyme 2 protects from severe acute lung failure, Nature
Inzucchi, Lipska, Mayo, Bailey, Mcguire, Metformin in patients with type 2 diabetes and kidney disease: a systematic review, JAMA
Kellum, Lameire, Aspelin, Barsoum, Burdmann et al., Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury, Kidney Int. Suppl
Kraut, Madias, Metabolic acidosis: pathophysiology, diagnosis and management, Nat. Rev. Nephrol
Lalau, Lactic acidosis induced by metformin: incidence, management and prevention, Drug Saf
Lexis, Van Der Horst, Lipsic, Wieringa, De Boer et al., Effect of metformin on left ventricular function after acute myocardial infarction in patients without diabetes: the GIPS-III randomized clinical trial, JAMA
Liu, Liu, Xiang, Pu, Xiong et al., Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am. J. Trop. Med. Hyg
Mathur, Ding, Riddell, Vanderweele, Web site and R package for computing E-values, Epidemiology
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock, Crit. Care Med
Misbin, Green, Stadel, Gueriguian, Gubbi et al., Lactic acidosis in patients with diabetes treated with metformin, N. Engl. J. Med
Monteil, Kwon, Prado, Hagelkr€ Uys, Wimmer et al., Prior metformin therapy and 30-day mortality in patients with acute respiratory distress syndrome: a nationwide cohort study
Overbeek, Heintjes, Prieto-Alhambra, Blin, Lassalle et al., Type 2 diabetes mellitus treatment patterns across Europe: a population-based multi-database study, Clin. Ther
Pollak, The effects of metformin on gut microbiota and the immune system as research frontiers, Diabetologia
Rena, Hardie, Pearson, The mechanisms of action of metformin, Diabetologia
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, JAMA
Shirani, Zhao, Karim, Evans, Kingwell et al., Association between use of interferon beta and progression of disability in patients with relapsing-remitting multiple sclerosis, JAMA
Stricker, Stijnen, Analysis of individual drug use as a timevarying determinant of exposure in prospective population-based cohort studies, Eur. J. Epidemiol
Suetrong, Walley, Lactic acidosis in sepsis: it's not all anaerobic: implications for diagnosis and management, Chest
Therneau, None
Tomczynska, Bijak, Saluk, Metformin -the drug for the treatment of autoimmune diseases; a new use of a known anti-diabetic drug, Curr. Top. Med. Chem
Tsai, Chang, Sun, Chan, Wu et al., Metformin activates type I interferon signaling against HCV via activation of adenosine monophosphate-activated protein kinase, Oncotarget
Tzanavari, Varela, Theocharis, Ninou, Kapelouzou et al., Metformin protects against infection-induced myocardial dysfunction, Metabolism
Ursini, Russo, Pellino, D'angelo, Chiaravalloti et al., Metformin and autoimmunity: a ''New Deal'' of an old drug, Front. Immunol
Vanderweele, Ding, Sensitivity analysis in observational research: introducing the E-value, Ann. Intern. Med
Waljee, Mukherjee, Singal, Zhang, Warren et al., Comparison of imputation methods for missing laboratory data in medicine
Yancy, Jessup, Bozkurt, Butler, Casey et al., None
Zhang, Dong, Martin, He, Gongol et al., AMP-activated protein kinase phosphorylation of angiotensin-converting enzyme 2 in endothelium mitigates pulmonary hypertension, Am. J. Respir. Crit. Care Med
Zhang, Reinikainen, Adeleke, Pieterse, Groothuis-Oudshoorn et al., Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19, Ann. Transl. Med
Zhu, She, Cheng, Qin, Zhang et al., Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab
DOI record:
{
"DOI": "10.1016/j.cmet.2020.08.013",
"ISSN": [
"1550-4131"
],
"URL": "http://dx.doi.org/10.1016/j.cmet.2020.08.013",
"alternative-id": [
"S1550413120304265"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Metformin Is Associated with Higher Incidence of Acidosis, but Not Mortality, in Individuals with COVID-19 and Pre-existing Type 2 Diabetes"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Cell Metabolism"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.cmet.2020.08.013"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2020 Elsevier Inc."
}
],
"author": [
{
"affiliation": [],
"family": "Cheng",
"given": "Xu",
"sequence": "first"
},
{
"affiliation": [],
"family": "Liu",
"given": "Ye-Mao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Haomiao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Xin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lei",
"given": "Fang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Qin",
"given": "Juan-Juan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Ze",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Deng",
"given": "Ke-Qiong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lin",
"given": "Lijin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Ming-Ming",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Song",
"given": "Xiaohui",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xia",
"given": "Meng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huang",
"given": "Xuewei",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Liu",
"given": "Weifang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cai",
"given": "Jingjing",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Xiao-Jing",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhou",
"given": "Feng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Peng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wang",
"given": "Yibin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ma",
"given": "Xinliang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xu",
"given": "Qingbo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yang",
"given": "Juan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ye",
"given": "Ping",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mao",
"given": "Weiming",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Huang",
"given": "Xiaodong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xia",
"given": "Jiahong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Bing-Hong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guo",
"given": "Jiao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhu",
"given": "Lihua",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lu",
"given": "Zhibing",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yuan",
"given": "Yufeng",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wei",
"given": "Xiang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "She",
"given": "Zhi-Gang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ji",
"given": "Yan-Xiao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Hongliang",
"sequence": "additional"
}
],
"container-title": [
"Cell Metabolism"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"cell.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2020,
8,
20
]
],
"date-time": "2020-08-20T16:24:27Z",
"timestamp": 1597940667000
},
"deposited": {
"date-parts": [
[
2021,
11,
4
]
],
"date-time": "2021-11-04T17:32:31Z",
"timestamp": 1636047151000
},
"funder": [
{
"DOI": "10.13039/501100001809",
"doi-asserted-by": "publisher",
"name": "National Natural Science Foundation of China"
}
],
"indexed": {
"date-parts": [
[
2021,
12,
23
]
],
"date-time": "2021-12-23T23:06:44Z",
"timestamp": 1640300804040
},
"is-referenced-by-count": 61,
"issn-type": [
{
"type": "print",
"value": "1550-4131"
}
],
"issue": "4",
"issued": {
"date-parts": [
[
2020,
10
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2020,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
10,
1
]
],
"date-time": "2020-10-01T00:00:00Z",
"timestamp": 1601510400000
}
},
{
"URL": "http://www.elsevier.com/open-access/userlicense/1.0/",
"content-version": "vor",
"delay-in-days": 370,
"start": {
"date-parts": [
[
2021,
10,
6
]
],
"date-time": "2021-10-06T00:00:00Z",
"timestamp": 1633478400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S1550413120304265?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S1550413120304265?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "537-547.e3",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2020,
10
]
]
},
"published-print": {
"date-parts": [
[
2020,
10
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"article-title": "9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2019",
"first-page": "S90",
"issue": "Suppl 1",
"journal-title": "Diabetes Care",
"key": "10.1016/j.cmet.2020.08.013_bib1",
"volume": "42",
"year": "2019"
},
{
"DOI": "10.1111/bcp.13780",
"article-title": "The journey of metformin from glycaemic control to mTOR inhibition and the suppression of tumour growth",
"author": "Amin",
"doi-asserted-by": "crossref",
"first-page": "37",
"journal-title": "Br. J. Clin. Pharmacol.",
"key": "10.1016/j.cmet.2020.08.013_bib2",
"volume": "85",
"year": "2019"
},
{
"DOI": "10.1007/s00125-017-4318-z",
"article-title": "Metformin: historical overview",
"author": "Bailey",
"doi-asserted-by": "crossref",
"first-page": "1566",
"journal-title": "Diabetologia",
"key": "10.1016/j.cmet.2020.08.013_bib3",
"volume": "60",
"year": "2017"
},
{
"DOI": "10.1378/chest.99.4.956",
"article-title": "Blood lactate levels are superior to oxygen-derived variables in predicting outcome in human septic shock",
"author": "Bakker",
"doi-asserted-by": "crossref",
"first-page": "956",
"journal-title": "Chest",
"key": "10.1016/j.cmet.2020.08.013_bib4",
"volume": "99",
"year": "1991"
},
{
"DOI": "10.2337/dc08-1171",
"article-title": "Metformin, sulfonylureas, or other antidiabetes drugs and the risk of lactic acidosis or hypoglycemia: a nested case-control analysis",
"author": "Bodmer",
"doi-asserted-by": "crossref",
"first-page": "2086",
"journal-title": "Diabetes Care",
"key": "10.1016/j.cmet.2020.08.013_bib5",
"volume": "31",
"year": "2008"
},
{
"DOI": "10.1016/S2213-8587(20)30152-2",
"article-title": "Practical recommendations for the management of diabetes in patients with COVID-19",
"author": "Bornstein",
"doi-asserted-by": "crossref",
"first-page": "546",
"journal-title": "Lancet Diabetes Endocrinol.",
"key": "10.1016/j.cmet.2020.08.013_bib6",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1007/s00125-010-1750-8",
"article-title": "Glucose-lowering agents and cancer mortality rates in type 2 diabetes: assessing effects of time-varying exposure",
"author": "Bowker",
"doi-asserted-by": "crossref",
"first-page": "1631",
"journal-title": "Diabetologia",
"key": "10.1016/j.cmet.2020.08.013_bib7",
"volume": "53",
"year": "2010"
},
{
"DOI": "10.1161/CIRCRESAHA.116.308445",
"article-title": "Anti-inflammatory effects of metformin irrespective of diabetes status",
"author": "Cameron",
"doi-asserted-by": "crossref",
"first-page": "652",
"journal-title": "Circ. Res.",
"key": "10.1016/j.cmet.2020.08.013_bib8",
"volume": "119",
"year": "2016"
},
{
"article-title": "Guidelines for the prevention and control of type 2 diabetes in China (2017 Edition)",
"first-page": "53",
"journal-title": "Zhongguo Shiyong Neike Zazhi",
"key": "10.1016/j.cmet.2020.08.013_bib9",
"volume": "38",
"year": "2018"
},
{
"DOI": "10.1186/s13054-015-1180-6",
"article-title": "Lactic acidosis and severe septic shock in metformin users: a cohort study",
"author": "Doenyas-Barak",
"doi-asserted-by": "crossref",
"first-page": "10",
"journal-title": "Crit. Care",
"key": "10.1016/j.cmet.2020.08.013_bib10",
"volume": "20",
"year": "2016"
},
{
"DOI": "10.3390/ijms19102869",
"article-title": "Metabolic effects of metformin in the failing heart",
"author": "Dziubak",
"doi-asserted-by": "crossref",
"first-page": "E2869",
"journal-title": "Int. J. Mol. Sci.",
"key": "10.1016/j.cmet.2020.08.013_bib11",
"volume": "19",
"year": "2018"
},
{
"DOI": "10.1016/j.cmet.2014.09.018",
"article-title": "Metformin: from mechanisms of action to therapies",
"author": "Foretz",
"doi-asserted-by": "crossref",
"first-page": "953",
"journal-title": "Cell Metab.",
"key": "10.1016/j.cmet.2020.08.013_bib12",
"volume": "20",
"year": "2014"
},
{
"DOI": "10.1111/jth.12190",
"article-title": "Differentiating disseminated intravascular coagulation (DIC) with the fibrinolytic phenotype from coagulopathy of trauma and acute coagulopathy of trauma-shock (COT/ACOTS)",
"author": "Gando",
"doi-asserted-by": "crossref",
"first-page": "826",
"journal-title": "J. Thromb. Haemost.",
"key": "10.1016/j.cmet.2020.08.013_bib13",
"volume": "11",
"year": "2013"
},
{
"DOI": "10.1001/jama.2018.21554",
"article-title": "Using the E-value to assess the potential effect of unmeasured confounding in observational studies",
"author": "Haneuse",
"doi-asserted-by": "crossref",
"first-page": "602",
"journal-title": "JAMA",
"key": "10.1016/j.cmet.2020.08.013_bib49",
"volume": "321",
"year": "2019"
},
{
"DOI": "10.1001/jama.1982.03320430047030",
"article-title": "Evaluating the yield of medical tests",
"author": "Harrell",
"doi-asserted-by": "crossref",
"first-page": "2543",
"journal-title": "JAMA",
"key": "10.1016/j.cmet.2020.08.013_bib14",
"volume": "247",
"year": "1982"
},
{
"DOI": "10.1016/j.cell.2020.02.052",
"article-title": "SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor",
"author": "Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "271",
"journal-title": "Cell",
"key": "10.1016/j.cmet.2020.08.013_bib15",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "10.1016/j.cmet.2020.08.013_bib16",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1038/nature03712",
"article-title": "Angiotensin-converting enzyme 2 protects from severe acute lung failure",
"author": "Imai",
"doi-asserted-by": "crossref",
"first-page": "112",
"journal-title": "Nature",
"key": "10.1016/j.cmet.2020.08.013_bib17",
"volume": "436",
"year": "2005"
},
{
"DOI": "10.1001/jama.2014.15298",
"article-title": "Metformin in patients with type 2 diabetes and kidney disease: a systematic review",
"author": "Inzucchi",
"doi-asserted-by": "crossref",
"first-page": "2668",
"journal-title": "JAMA",
"key": "10.1016/j.cmet.2020.08.013_bib18",
"volume": "312",
"year": "2014"
},
{
"article-title": "Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury",
"author": "Kellum",
"first-page": "1",
"journal-title": "Kidney Int. Suppl.",
"key": "10.1016/j.cmet.2020.08.013_bib19",
"volume": "2",
"year": "2012"
},
{
"DOI": "10.1038/nrneph.2010.33",
"article-title": "Metabolic acidosis: pathophysiology, diagnosis and management",
"author": "Kraut",
"doi-asserted-by": "crossref",
"first-page": "274",
"journal-title": "Nat. Rev. Nephrol.",
"key": "10.1016/j.cmet.2020.08.013_bib20",
"volume": "6",
"year": "2010"
},
{
"DOI": "10.2165/11536790-000000000-00000",
"article-title": "Lactic acidosis induced by metformin: incidence, management and prevention",
"author": "Lalau",
"doi-asserted-by": "crossref",
"first-page": "727",
"journal-title": "Drug Saf.",
"key": "10.1016/j.cmet.2020.08.013_bib21",
"volume": "33",
"year": "2010"
},
{
"DOI": "10.1001/jama.2014.3315",
"article-title": "Effect of metformin on left ventricular function after acute myocardial infarction in patients without diabetes: the GIPS-III randomized clinical trial",
"author": "Lexis",
"doi-asserted-by": "crossref",
"first-page": "1526",
"journal-title": "JAMA",
"key": "10.1016/j.cmet.2020.08.013_bib22",
"volume": "311",
"year": "2014"
},
{
"DOI": "10.1186/s12967-020-02374-0",
"article-title": "Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "206",
"journal-title": "J. Transl. Med.",
"key": "10.1016/j.cmet.2020.08.013_bib23",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"article-title": "Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "69",
"journal-title": "Am. J. Trop. Med. Hyg.",
"key": "10.1016/j.cmet.2020.08.013_bib24",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.1097/EDE.0000000000000864",
"article-title": "Web site and R package for computing E-values",
"author": "Mathur",
"doi-asserted-by": "crossref",
"first-page": "e45",
"journal-title": "Epidemiology",
"key": "10.1016/j.cmet.2020.08.013_bib50",
"volume": "29",
"year": "2018"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"article-title": "COVID-19: consider cytokine storm syndromes and immunosuppression",
"author": "Mehta",
"doi-asserted-by": "crossref",
"first-page": "1033",
"journal-title": "Lancet",
"key": "10.1016/j.cmet.2020.08.013_bib25",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1097/CCM.0b013e31819fcf68",
"article-title": "Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock",
"author": "Mikkelsen",
"doi-asserted-by": "crossref",
"first-page": "1670",
"journal-title": "Crit. Care Med.",
"key": "10.1016/j.cmet.2020.08.013_bib26",
"volume": "37",
"year": "2009"
},
{
"DOI": "10.1056/NEJM199801223380415",
"article-title": "Lactic acidosis in patients with diabetes treated with metformin",
"author": "Misbin",
"doi-asserted-by": "crossref",
"first-page": "265",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.cmet.2020.08.013_bib27",
"volume": "338",
"year": "1998"
},
{
"DOI": "10.1016/j.cell.2020.04.004",
"article-title": "Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2",
"author": "Monteil",
"doi-asserted-by": "crossref",
"first-page": "905",
"journal-title": "Cell",
"key": "10.1016/j.cmet.2020.08.013_bib28",
"volume": "181",
"year": "2020"
},
{
"DOI": "10.21037/apm.2020.04.25",
"article-title": "Prior metformin therapy and 30-day mortality in patients with acute respiratory distress syndrome: a nationwide cohort study",
"author": "Oh",
"doi-asserted-by": "crossref",
"first-page": "903",
"journal-title": "Ann. Palliat. Med.",
"key": "10.1016/j.cmet.2020.08.013_bib30",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/j.clinthera.2017.02.008",
"article-title": "Type 2 diabetes mellitus treatment patterns across Europe: a population-based multi-database study",
"author": "Overbeek",
"doi-asserted-by": "crossref",
"first-page": "759",
"journal-title": "Clin. Ther.",
"key": "10.1016/j.cmet.2020.08.013_bib31",
"volume": "39",
"year": "2017"
},
{
"DOI": "10.1007/s00125-017-4352-x",
"article-title": "The effects of metformin on gut microbiota and the immune system as research frontiers",
"author": "Pollak",
"doi-asserted-by": "crossref",
"first-page": "1662",
"journal-title": "Diabetologia",
"key": "10.1016/j.cmet.2020.08.013_bib32",
"volume": "60",
"year": "2017"
},
{
"DOI": "10.1007/s00125-017-4342-z",
"article-title": "The mechanisms of action of metformin",
"author": "Rena",
"doi-asserted-by": "crossref",
"first-page": "1577",
"journal-title": "Diabetologia",
"key": "10.1016/j.cmet.2020.08.013_bib33",
"volume": "60",
"year": "2017"
},
{
"DOI": "10.1001/jama.2020.6775",
"article-title": "Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area",
"author": "Richardson",
"doi-asserted-by": "crossref",
"first-page": "2052",
"journal-title": "JAMA",
"key": "10.1016/j.cmet.2020.08.013_bib34",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1001/jama.2012.7625",
"article-title": "Association between use of interferon beta and progression of disability in patients with relapsing-remitting multiple sclerosis",
"author": "Shirani",
"doi-asserted-by": "crossref",
"first-page": "247",
"journal-title": "JAMA",
"key": "10.1016/j.cmet.2020.08.013_bib35",
"volume": "308",
"year": "2012"
},
{
"DOI": "10.1007/s10654-010-9451-7",
"article-title": "Analysis of individual drug use as a time-varying determinant of exposure in prospective population-based cohort studies",
"author": "Stricker",
"doi-asserted-by": "crossref",
"first-page": "245",
"journal-title": "Eur. J. Epidemiol.",
"key": "10.1016/j.cmet.2020.08.013_bib36",
"volume": "25",
"year": "2010"
},
{
"DOI": "10.1378/chest.15-1703",
"article-title": "Lactic acidosis in sepsis: it’s not all anaerobic: implications for diagnosis and management",
"author": "Suetrong",
"doi-asserted-by": "crossref",
"first-page": "252",
"journal-title": "Chest",
"key": "10.1016/j.cmet.2020.08.013_bib37",
"volume": "149",
"year": "2016"
},
{
"DOI": "10.2174/1568026616666160216152324",
"article-title": "Metformin - the drug for the treatment of autoimmune diseases; a new use of a known anti-diabetic drug",
"author": "Tomczynska",
"doi-asserted-by": "crossref",
"first-page": "2223",
"journal-title": "Curr. Top. Med. Chem.",
"key": "10.1016/j.cmet.2020.08.013_bib38",
"volume": "16",
"year": "2016"
},
{
"DOI": "10.18632/oncotarget.20248",
"article-title": "Metformin activates type I interferon signaling against HCV via activation of adenosine monophosphate-activated protein kinase",
"author": "Tsai",
"doi-asserted-by": "crossref",
"first-page": "91928",
"journal-title": "Oncotarget",
"key": "10.1016/j.cmet.2020.08.013_bib39",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1016/j.metabol.2016.06.012",
"article-title": "Metformin protects against infection-induced myocardial dysfunction",
"author": "Tzanavari",
"doi-asserted-by": "crossref",
"first-page": "1447",
"journal-title": "Metabolism",
"key": "10.1016/j.cmet.2020.08.013_bib40",
"volume": "65",
"year": "2016"
},
{
"DOI": "10.3389/fimmu.2018.01236",
"article-title": "Metformin and autoimmunity: a “New Deal” of an old drug",
"author": "Ursini",
"doi-asserted-by": "crossref",
"first-page": "1236",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.cmet.2020.08.013_bib41",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.7326/M16-2607",
"article-title": "Sensitivity analysis in observational research: introducing the E-value",
"author": "VanderWeele",
"doi-asserted-by": "crossref",
"first-page": "268",
"journal-title": "Ann. Intern. Med.",
"key": "10.1016/j.cmet.2020.08.013_bib51",
"volume": "167",
"year": "2017"
},
{
"DOI": "10.1136/bmjopen-2013-002847",
"article-title": "Comparison of imputation methods for missing laboratory data in medicine",
"author": "Waljee",
"doi-asserted-by": "crossref",
"first-page": "e002847",
"journal-title": "BMJ Open",
"key": "10.1016/j.cmet.2020.08.013_bib42",
"volume": "3",
"year": "2013"
},
{
"key": "10.1016/j.cmet.2020.08.013_bib43",
"series-title": "Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases interim guidance",
"year": "2020"
},
{
"DOI": "10.1161/CIR.0000000000000509",
"author": "Yancy",
"doi-asserted-by": "crossref",
"first-page": "e137",
"journal-title": "Circulation",
"key": "10.1016/j.cmet.2020.08.013_bib44",
"volume": "136",
"year": "2017"
},
{
"DOI": "10.1164/rccm.201712-2570OC",
"article-title": "AMP-activated protein kinase phosphorylation of angiotensin-converting enzyme 2 in endothelium mitigates pulmonary hypertension",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "509",
"journal-title": "Am. J. Respir. Crit. Care Med.",
"key": "10.1016/j.cmet.2020.08.013_bib45",
"volume": "198",
"year": "2018"
},
{
"DOI": "10.21037/atm.2018.02.12",
"article-title": "Time-varying covariates and coefficients in Cox regression models",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "121",
"journal-title": "Ann. Transl. Med.",
"key": "10.1016/j.cmet.2020.08.013_bib46",
"volume": "6",
"year": "2018"
},
{
"DOI": "10.1161/CIRCRESAHA.120.317134",
"article-title": "Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "1671",
"journal-title": "Circ. Res.",
"key": "10.1016/j.cmet.2020.08.013_bib47",
"volume": "126",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"article-title": "Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "1068",
"journal-title": "Cell Metab.",
"key": "10.1016/j.cmet.2020.08.013_bib48",
"volume": "31",
"year": "2020"
}
],
"reference-count": 50,
"references-count": 50,
"relation": {},
"score": 1,
"short-container-title": [
"Cell Metabolism"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Cell Biology",
"Molecular Biology",
"Physiology"
],
"subtitle": [],
"title": [
"Metformin Is Associated with Higher Incidence of Acidosis, but Not Mortality, in Individuals with COVID-19 and Pre-existing Type 2 Diabetes"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "32"
}
