Metformin Treatment Was Associated with Decreased Mortality in COVID-19 Patients with Diabetes in a Retrospective Analysis
et al., The American Journal of Tropical Medicine and Hygiene, doi:10.4269/ajtmh.20-0375, May 2020
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
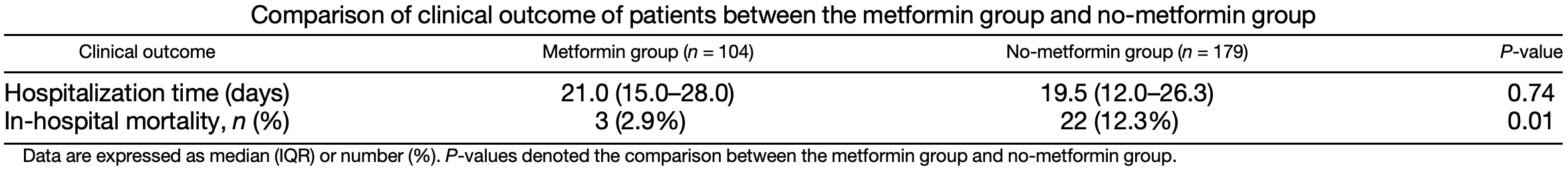
Retrospective 283 COVID-19+ diabetes patients in China, showing lower mortality with existing metformin treatment.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
Study covers HCQ and metformin.
|
risk of death, 74.7% lower, RR 0.25, p = 0.02, treatment 3 of 104 (2.9%), control 22 of 179 (12.3%), NNT 11, adjusted per study, inverted to make RR<1 favor treatment, odds ratio converted to relative risk, multivariate.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Luo et al., 21 May 2020, retrospective, China, peer-reviewed, 9 authors.
Metformin Treatment Was Associated with Decreased Mortality in COVID-19 Patients with Diabetes in a Retrospective Analysis
The American Journal of Tropical Medicine and Hygiene, doi:10.4269/ajtmh.20-0375
Metformin was proposed to be a candidate for host-directed therapy for COVID-19. However, its efficacy remains to be validated. In this study, we compared the outcome of metformin users and nonusers in hospitalized COVID-19 patients with diabetes. Hospitalized diabetic patients with confirmed COVID-19 in the Tongji Hospital of Wuhan, China, from January 27, 2020 to March 24, 2020, were grouped into metformin and no-metformin groups according to the diabetic medications used. The demographics, characteristics, laboratory parameters, treatments, and clinical outcome in these patients were retrospectively assessed. A total of 283 patients (104 in the metformin and 179 in the no-metformin group) were included in this study. There were no significant differences between the two groups in gender, age, underlying diseases, clinical severity, and oxygen-support category at admission. The fasting blood glucose level of the metformin group was higher than that of the no-metformin group at admission and was under effective control in both groups after admission. Other laboratory parameters at admission and treatments after admission were not different between the two groups. The length of hospital stay did not differ between the two groups (21.0 days for metformin versus 19.5 days for no metformin, P = 0.74). However, in-hospital mortality was significantly lower in the metformin group (3/104 (2.9%) versus 22/179 (12.3%), P = 0.01). Antidiabetic treatment with metformin was associated with decreased mortality compared with diabetics not receiving metformin. This retrospective analysis suggests that metformin may offer benefits in patients with COVID-19 and that further study is indicated.
References
Ahmed, Raqib, Guethmundsson, Bergman, Agerberth et al., Host-directed therapy as a novel treatment strategy to overcome tuberculosis: targeting immune modulation, Antibiotics
Ba, Xu, Yin, Yang, Wang et al., Metformin inhibits pro-inflammatory responses via targeting nuclear factor-kappaB in HaCaT cells, Cell Biochem Funct
Burgos-Moron, Relationship between oxidative stress, ER stress, and inflammation in type 2 diabetes: the battle continues, J Clin Med
Chen, Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet
Hill, Mantzoros, Sowers, Commentary: COVID-19 in patients with diabetes, Metabolism
Huang, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Ouyang, Isnard, Lin, Fombuena, Marette et al., Metformin effect on gut microbiota: insights for HIV-related inflammation, AIDS Res Ther
Prompetchara, Ketloy, Palaga, Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic, Asian Pac J Allergy Immunol
Schuiveling, Vazirpanah, Radstake, Zimmermann, Broen, Metformin, a new era for an old drug in the treatment of immune mediated disease?, Curr Drug Targets
Shi, Wang, Shao, Huang, Gan et al., COVID-19 infection: the perspectives on immune responses, Cell Death Differ
Vilela, Peixoto, Teixeira, Baptista, Caixeta et al., The role of metformin in controlling oxidative stress in muscle of diabetic rats, Oxid Med Cell Longev
Yew, Chang, Chan, Zhang, Metformin as a host-directed therapeutic in tuberculosis: is there a promise?, Tuberculosis
Zhang, Wang, Ni, Di, Ma et al., COVID-19: melatonin as a potential adjuvant treatment, Life Sci
Zumla, Hui, Azhar, Memish, Maeurer, Reducing mortality from 2019-nCoV: host-directed therapies should be an option, Lancet
DOI record:
{
"DOI": "10.4269/ajtmh.20-0375",
"ISSN": [
"0002-9637",
"1476-1645"
],
"URL": "http://dx.doi.org/10.4269/ajtmh.20-0375",
"author": [
{
"affiliation": [
{
"name": "Department of Pharmacy, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China;"
}
],
"family": "Luo",
"given": "Pan",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China;"
}
],
"family": "Qiu",
"given": "Lin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China;"
}
],
"family": "Liu",
"given": "Yi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China;"
}
],
"family": "Liu",
"given": "Xiu-lan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China;"
}
],
"family": "Zheng",
"given": "Jian-ling",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China;"
}
],
"family": "Xue",
"given": "Hui-ying",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Clinical Research Center, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China"
}
],
"family": "Liu",
"given": "Wen-hua",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China;"
}
],
"family": "Liu",
"given": "Dong",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pharmacy, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China;"
}
],
"family": "Li",
"given": "Juan",
"sequence": "additional"
}
],
"container-title": "The American Journal of Tropical Medicine and Hygiene",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
5,
22
]
],
"date-time": "2020-05-22T07:00:46Z",
"timestamp": 1590130846000
},
"deposited": {
"date-parts": [
[
2021,
1,
27
]
],
"date-time": "2021-01-27T17:40:32Z",
"timestamp": 1611769232000
},
"indexed": {
"date-parts": [
[
2024,
4,
8
]
],
"date-time": "2024-04-08T07:56:59Z",
"timestamp": 1712563019748
},
"is-referenced-by-count": 199,
"issue": "1",
"issued": {
"date-parts": [
[
2020,
7,
8
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2020,
7,
8
]
]
}
},
"language": "en",
"member": "2795",
"original-title": [],
"page": "69-72",
"prefix": "10.4269",
"published": {
"date-parts": [
[
2020,
7,
8
]
]
},
"published-print": {
"date-parts": [
[
2020,
7,
8
]
]
},
"publisher": "American Society of Tropical Medicine and Hygiene",
"reference": [
{
"article-title": "Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic",
"author": "Prompetchara",
"first-page": "1",
"journal-title": "Asian Pac J Allergy Immunol",
"key": "b1",
"volume": "38",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "497",
"journal-title": "Lancet",
"key": "b2",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1038/s41418-020-0530-3",
"article-title": "COVID-19 infection: the perspectives on immune responses",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "1451",
"journal-title": "Cell Death Differ",
"key": "b3",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.3390/antibiotics9010021",
"article-title": "Host-directed therapy as a novel treatment strategy to overcome tuberculosis: targeting immune modulation",
"author": "Ahmed",
"doi-asserted-by": "crossref",
"first-page": "E21",
"journal-title": "Antibiotics (Basel)",
"key": "b4",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30305-6",
"article-title": "Reducing mortality from 2019-nCoV: host-directed therapies should be an option",
"author": "Zumla",
"doi-asserted-by": "crossref",
"first-page": "e35",
"journal-title": "Lancet",
"key": "b5",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.metabol.2020.154217",
"article-title": "Commentary: COVID-19 in patients with diabetes",
"author": "Hill",
"doi-asserted-by": "crossref",
"first-page": "154217",
"journal-title": "Metabolism",
"key": "b6",
"volume": "107",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30211-7",
"article-title": "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "507",
"journal-title": "Lancet",
"key": "b7",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.lfs.2020.117583",
"article-title": "COVID-19: melatonin as a potential adjuvant treatment",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "117583",
"journal-title": "Life Sci",
"key": "b8",
"volume": "253",
"year": "2020"
},
{
"DOI": "10.3390/jcm8091385",
"article-title": "Relationship between oxidative stress, ER stress, and inflammation in type 2 diabetes: the battle continues",
"author": "Burgos-Moron",
"doi-asserted-by": "crossref",
"first-page": "E1385",
"journal-title": "J Clin Med",
"key": "b9",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.2174/1389450118666170613081730",
"article-title": "Metformin, a new era for an old drug in the treatment of immune mediated disease?",
"author": "Schuiveling",
"doi-asserted-by": "crossref",
"first-page": "945",
"journal-title": "Curr Drug Targets",
"key": "b10",
"volume": "19",
"year": "2018"
},
{
"DOI": "10.1002/cbf.3367",
"article-title": "Metformin inhibits pro-inflammatory responses via targeting nuclear factor-kappaB in HaCaT cells",
"author": "Ba",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "Cell Biochem Funct",
"key": "b11",
"volume": "37",
"year": "2019"
},
{
"DOI": "10.1186/s12981-020-00267-2",
"article-title": "Metformin effect on gut microbiota: insights for HIV-related inflammation",
"author": "Ouyang",
"doi-asserted-by": "crossref",
"first-page": "10",
"journal-title": "AIDS Res Ther",
"key": "b12",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.tube.2019.02.004",
"article-title": "Metformin as a host-directed therapeutic in tuberculosis: is there a promise?",
"author": "Yew",
"doi-asserted-by": "crossref",
"first-page": "76",
"journal-title": "Tuberculosis (Edinb)",
"key": "b13",
"volume": "115",
"year": "2019"
},
{
"DOI": "10.1038/ncomms3192",
"article-title": "Metformin improves healthspan and lifespan in mice",
"author": "Martin-Montalvo",
"doi-asserted-by": "crossref",
"first-page": "2192",
"journal-title": "Nat Commun",
"key": "b14",
"volume": "4",
"year": "2013"
},
{
"DOI": "10.1155/2016/6978625",
"article-title": "The role of metformin in controlling oxidative stress in muscle of diabetic rats",
"author": "Diniz Vilela",
"doi-asserted-by": "crossref",
"first-page": "6978625",
"journal-title": "Oxid Med Cell Longev",
"key": "b15",
"volume": "2016",
"year": "2016"
}
],
"reference-count": 15,
"references-count": 15,
"relation": {
"has-review": [
{
"asserted-by": "object",
"id": "10.3410/f.738014105.793574896",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://ajtmh.org/doi/10.4269/ajtmh.20-0375"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Virology",
"Infectious Diseases",
"Parasitology"
],
"subtitle": [],
"title": "Metformin Treatment Was Associated with Decreased Mortality in COVID-19 Patients with Diabetes in a Retrospective Analysis",
"type": "journal-article",
"volume": "103"
}
