Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis
et al., Frontiers in Endocrinology, doi:10.3389/fendo.2021.708494, PROSPERO CRD42021242898, Sep 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
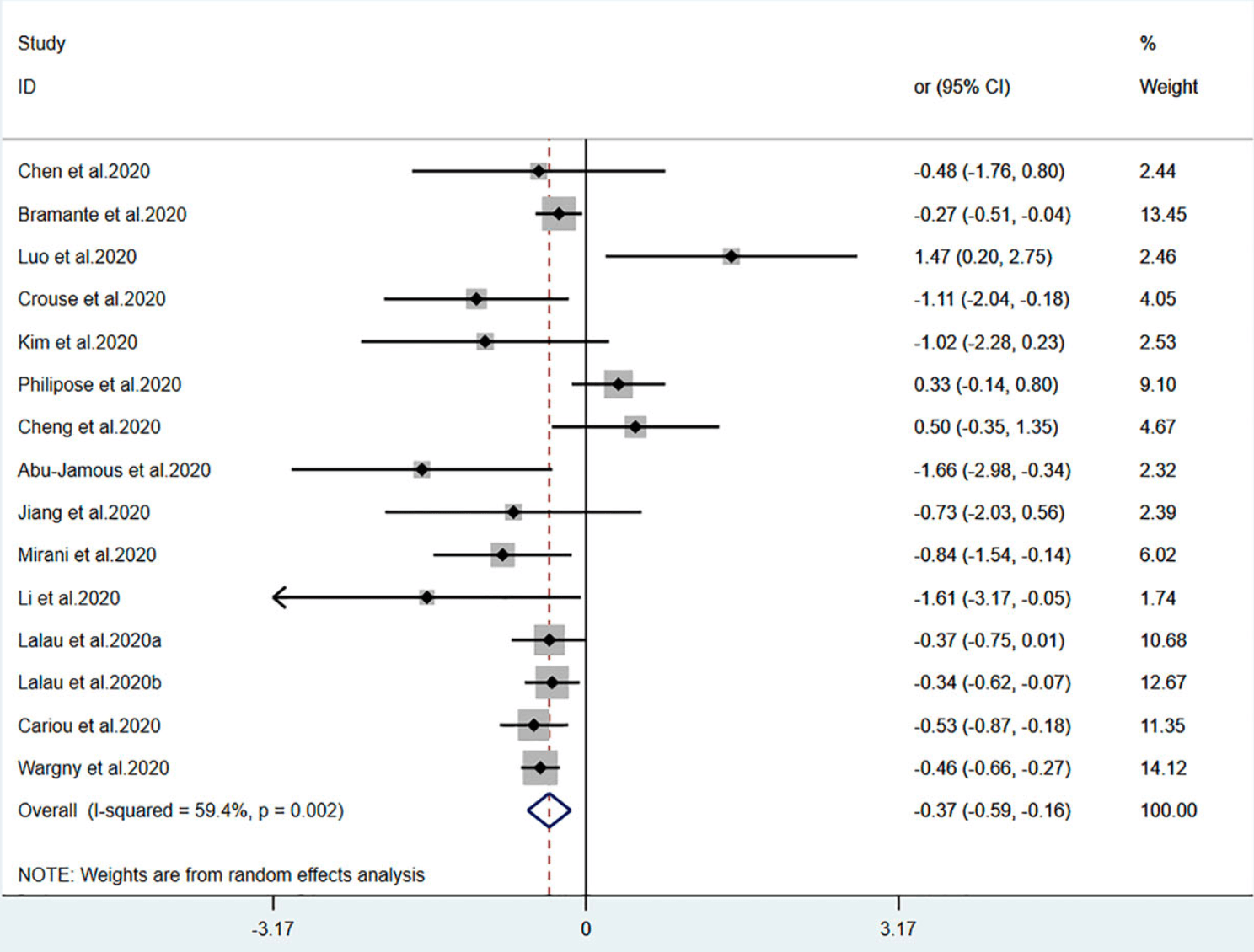
Meta analysis of 14 studies showing significantly lower COVID-19 mortality with metformin use.
24 meta-analyses show significant improvements with metformin for mortality1-23,
hospitalization7,13,23 ,
progression1, and
severity8,9,13 .
Currently there are 110 metformin for COVID-19 studies, showing 36% lower mortality [32‑40%], 29% lower ventilation [12‑43%], 19% lower ICU admission [8‑28%], 17% lower hospitalization [11‑23%], and 5% fewer cases [-4‑13%].
|
risk of death, 31.0% lower, OR 0.69, p = 0.001, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Yang et al., The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus, Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2021.108977.
2.
Lukito et al., The Effect of Metformin Consumption on Mortality in Hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2020.11.006.
3.
Kow et al., Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis, Journal of Medical Virology, doi:10.1002/jmv.26498.
4.
Hariyanto et al., Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection, Obesity Medicine, doi:10.1016/j.obmed.2020.100290.
5.
Ma et al., Is metformin use associated with low mortality in patients with type 2 diabetes mellitus hospitalized for COVID-19? a multivariable and propensity score-adjusted meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0282210.
6.
Parveen et al., Association of Metformin with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis, Annals of the National Academy of Medical Sciences (India), doi:10.1055/s-0042-1760353.
7.
Li et al., Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Medicine, doi:10.3389/fmed.2021.704666.
8.
Schlesinger et al., Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis, Diabetologia, doi:10.1007/s00125-023-05928-1.
9.
Petrelli et al., Metformin and Covid-19: a systematic review of systematic reviews with meta-analysis, Acta Biomedica Atenei Parmensis, doi:10.23750/abm.v94iS3.14405.
10.
Oscanoa et al., Metformin therapy and severity and mortality of SARS-CoV-2 infection: a meta-analysis, Clinical Diabetology, doi:10.5603/DK.a2021.0035.
11.
Kan et al., Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2021.708494.
12.
Poly et al., Metformin Use Is Associated with Decreased Mortality in COVID-19 Patients with Diabetes: Evidence from Retrospective Studies and Biological Mechanism, Journal of Clinical Medicine, doi:10.3390/jcm10163507.
13.
Song et al., The Effect of Antihyperglycemic Medications on COVID-19: A Meta-analysis and Systematic Review from Observational Studies, Therapeutic Innovation & Regulatory Science, doi:10.1007/s43441-024-00633-6.
14.
Ganesh et al., Does metformin affect outcomes in COVID‐19 patients with new or pre‐existing diabetes mellitus? A systematic review and meta‐analysis, British Journal of Clinical Pharmacology, doi:10.1111/bcp.15258.
15.
Nassar et al., Noninsulin‐based antihyperglycemic medications in patients with diabetes and COVID‐19: A systematic review and meta‐analysis, Journal of Diabetes, doi:10.1111/1753-0407.13359.
16.
Zhan et al., Effect of Antidiabetic Therapy on Clinical Outcomes of COVID-19 Patients With Type 2 Diabetes: A Systematic Review and Meta-Analysis, Annals of Pharmacotherapy, doi:10.1177/10600280221133577.
17.
Nguyen et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196.
18.
Han et al., Association Between Anti-diabetic Agents and Clinical Outcomes of COVID-19 in Patients with Diabetes: A Systematic Review and Meta-Analysis, Archives of Medical Research, doi:10.1016/j.arcmed.2021.08.002.
19.
Chen et al., The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2022.895458.
20.
Scheen, A., Metformin and COVID-19: From cellular mechanisms to reduced mortality, Diabetes & Metabolism, doi:10.1016/j.diabet.2020.07.006.
21.
Sun et al., Is Metformin Use Associated With a Decreased Mortality for COVID-19 Diabetic Patients? A Meta-Analysis, Journal of the Endocrine Society, doi:10.1210/jendso/bvab048.709.
Kan et al., 16 Sep 2021, peer-reviewed, 7 authors, trial PROSPERO CRD42021242898.
Contact: xiaodong.sun@wfmc.edu.cn, ningning.hou@wfmc.edu.cn.
Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis
Frontiers in Endocrinology, doi:10.3389/fendo.2021.708494
Aims: We conducted a systematic review and meta-analysis to assess various antidiabetic agents' association with mortality in patients with type 2 diabetes (T2DM) who have coronavirus disease 2019 . Methods: We performed comprehensive literature retrieval from the date of inception until February 2, 2021, in medical databases (PubMed, Web of Science, Embase, and Cochrane Library), regarding mortality outcomes in patients with T2DM who have COVID-19. Pooled OR and 95% CI data were used to assess relationships between antidiabetic agents and mortality. Results: Eighteen studies with 17,338 patients were included in the meta-analysis. Metformin (pooled OR, 0.69; P=0.001) and sulfonylurea (pooled OR, 0.80; P=0.016) were associated with lower mortality risk in patients with T2DM who had COVID-19. However, patients with T2DM who had COVID-19 and received insulin exhibited greater mortality (pooled OR, 2.20; P=0.002). Mortality did not significantly differ (pooled OR, 0.72; P=0.057) between DPP-4 inhibitor users and non-users. Conclusions: Metformin and sulfonylurea could be associated with reduced mortality risk in patients with T2DM who have COVID-19. Furthermore, insulin use could be associated with greater mortality, while DPP-4 inhibitor use could not be. The effects of antidiabetic agents in patients with T2DM who have COVID-19 require further exploration. Systematic Review Registration: PROSPERO (identifier, CRD42021242898).
AUTHOR CONTRIBUTIONS CK, YZ, and FH: Conceptualization, methodology, and writingoriginal draft preparation. TY and QX: Data curation and investigation. XS and NH: Supervision, writingreviewing and editing, and funding acquisition. All authors contributed to the article and approved the submitted version.
Conflict of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Publisher's Note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abu-Jamous, Anisimovich, Baxter, Mackillop, Vizcaychipi et al., Associations of Comorbidities and Medications With COVID-19 Outcome: A Retrospective Analysis of Real-World Evidence Data, medRxiv, doi:10.1101/2020.08.20.20174169
Banik, Alqahtani, Booy, Rashid, Risk Factors for Severity and Mortality in Patients With MERS-CoV: Analysis of Publicly Available Data From Saudi Arabia, Virol Sin, doi:10.1007/s12250-015-3679-z
Bloomgarden, Diabetes and COVID-19, J Diabetes, doi:10.1111/1753-0407.13027
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Observational Study of Metformin and Risk of Mortality in Patients Hospitalized With Covid-19, medRxiv, doi:10.1101/2020.06.19.20135095
Cariou, Hadjadj, Wargny, Pichelin, Al-Salameh et al., Phenotypic Characteristics and Prognosis of Inpatients With COVID-19 and Diabetes: The CORONADO Study, Diabetologia, doi:10.1007/s00125-020-05180-x
Chen, Yang, Cheng, Chen, Peng et al., Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication, Diabetes Care, doi:10.2337/dc20-0660
Cheng, Liu, Li, Zhang, Lei et al., Metformin Is Associated With Higher Incidence of Acidosis, But Not Mortality, doi:10.1016/j.cmet.2020.08.013
Crouse, Grimes, Li, Might, Ovalle et al., Metformin Use Is Associated With Reduced Mortality in a Diverse Population With COVID-19 and Diabetes, Front Endocrinol (Lausanne), doi:10.3389/fendo.2020.600439
Davis, Xie, Viollet, Zou, Activation of the AMP-Activated Kinase by Antidiabetes Drug Metformin Stimulates Nitric Oxide Synthesis In Vivo by Promoting the Association of Heat Shock Protein 90 and Endothelial Nitric Oxide Synthase, Diabetes, doi:10.2337/diabetes.55.02.06.db05-1064
Egger, Smith, Schneider, Minder, Bias in Meta-Analysis Detected by a Simple, Graphical Test, BMJ, doi:10.1136/bmj.315.7109.629
Fadini, Morieri, Longato, Bonora, Pinelli et al., Exposure to Dipeptidyl-Peptidase-4 Inhibitors and COVID-19 Among People With Type 2 Diabetes: A Case-Control Study, Diabetes Obes Metab, doi:10.1111/dom.14097
Finfer, Chittock, Su, Blair, Foster et al., Intensive Versus Conventional Glucose Control in Critically Ill Patients, N Engl J Med, doi:10.1056/NEJMoa0810625
Guan, Ni, Hu, Liang, Ou et al., Clinical Characteristics of Coronavirus Disease 2019 in China, N Engl J Med, doi:10.1056/NEJMoa2002032
Gupta, Ghosh, Singh, Misra, Clinical Considerations for Patients With Diabetes in Times of COVID-19 Epidemic, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.03.002
Haltmeier, Benjamin, Beale, Inaba, Demetriades, Insulin-Treated Patients With Diabetes Mellitus Undergoing Emergency Abdominal Surgery Have Worse Outcomes Than Patients Treated With Oral Agents, World J Surg, doi:10.1007/s00268-016-3469-2
Hariyanto, Kurniawan, Dipeptidyl Peptidase 4 (DPP4) Inhibitor and Outcome From Coronavirus Disease 2019 (COVID-19) in Diabetic Patients: A Systematic Review, Meta-Analysis, and Meta-Regression, J Diabetes Metab Disord, doi:10.1007/s40200-021-00777-4
Hariyanto, Kurniawan, Metformin Use is Associated With Reduced Mortality Rate From Coronavirus Disease 2019 (COVID-19) Infection, Obes Med, doi:10.1016/j.obmed.2020.100290
Hariyanto, Putri, Situmeang, Kurniawan, Dementia is a Predictor for Mortality Outcome From Coronavirus Disease 2019 (COVID-19) Infection, Eur Arch Psychiatry Clin Neurosci, doi:10.1007/s00406-020-01205-z
Hattori, Suzuki, Hattori, Kasai, Metformin Inhibits Cytokine-Induced Nuclear Factor kappaB Activation via AMP-Activated Protein Kinase Activation in Vascular Endothelial Cells, Hypertension, doi:10.1161/01.HYP.0000221429.94591.72
Huang, Lim, Pranata, Diabetes Mellitus Is Associated With Increased Mortality and Severity of Disease in COVID-19 Pneumonia -A Systematic Review, Meta-Analysis, and Meta-Regression, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.018
Iacobellis, COVID-19 and Diabetes: Can DPP4 Inhibition Play a Role, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108125
Jiang, Chen, Yin, Liu, Yang et al., Association of Metformin With Mortality or ARDS in Patients With COVID-19 and Type 2 Diabetes: A Retrospective Cohort Study, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108619
Kim, Jeon, Kim, Moon, Cho et al., The Clinical Characteristics and Outcomes of Patients With Moderate-To-Severe Coronavirus Disease 2019 Infection and Diabetes in Daegu, South Korea, Diabetes Metab J, doi:10.4093/dmj.2020.0146
Kow, Hasan, Mortality Risk With Preadmission Metformin Use in Patients With COVID-19 and Diabetes: A Meta-Analysis, J Med Virol, doi:10.1002/jmv.26498
Lalau, Al-Salameh, Hadjadj, Goronflot, Wiernsperger et al., Metformin Use is Associated With a Reduced Risk of Mortality in Patients With Diabetes Hospitalised for COVID-19, Diabetes Metab, doi:10.1016/j.diabet.2020.101216
Li, Wei, Li, Mccowen, Xiong et al., Metformin Use in Diabetes Prior to Hospitalization: Effects on Mortality in Covid-19, Endocr Pract, doi:10.4158/EP-2020-0466
Lukito, Pranata, Henrina, Lim, Lawrensia et al., The Effect of Metformin Consumption on Mortality in Hospitalized COVID-19 Patients: A Systematic Review and Meta-Analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.11.006
Luo, Qiu, Liu, Liu, Zheng et al., Metformin Treatment Was Associated With Decreased Mortality in COVID-19 Patients With Diabetes in a Retrospective Analysis, Am J Trop Med Hyg, doi:10.4269/ajtmh.20-0375
Martini, Piccinni, Pedrini, Maggioni, CoViD-19 and Chronic Diseases: Current Knowledge, Future Steps and the MaCroScopio Project
Mirani, Favacchio, Carrone, Betella, Biamonte et al., Impact of Comorbidities and Glycemia at Admission and Dipeptidyl Peptidase 4 Inhibitors in Patients With Type 2 Diabetes With COVID-19: A Case Series From an Academic Hospital in Lombardy, Italy. Diabetes Care, doi:10.2337/dc20-1340
Mishra, Dingli, Metformin Inhibits IL-6 Signaling by Decreasing IL-6R Expression on Multiple Myeloma Cells, Leukemia, doi:10.1038/s41375-019-0470-4
Moher, Liberati, Tetzlaff, Altman, Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement, PloS Med, doi:10.1371/journal.pmed.1000097
Nauck, Meier, Reduced COVID-19 Mortality With Sitagliptin Treatment? Weighing the Dissemination of Potentially Lifesaving Findings Against the Assurance of High Scientific Standards, Diabetes Care, doi:10.2337/dci20-0062
Onder, Rezza, Brusaferro, Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy, JAMA, doi:10.1001/jama.2020.4683
Pearson-Stuttard, Blundell, Harris, Cook, Critchley, Diabetes and Infection: Assessing the Association With Glycaemic Control in Population-Based Studies, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(15)00379-4
Philipose, Smati, Wong, Aspey, Mendall, Obesity, Old Age and Frailty are the True Risk Factors for COVID-19 Mortality and Not Chronic Disease or, Ethnicity in Croydon. medRxiv, doi:10.1101/2020.08.12.20156257
Putri, Hariyanto, Hananto, Christian, Situmeang et al., Parkinson's Disease may Worsen Outcomes From Coronavirus Disease 2019 (COVID-19) Pneumonia in Hospitalized Patients: A Systematic Review, Meta-Analysis, and Meta-Regression, Parkinsonism Relat Disord, doi:10.1016/j.parkreldis.2021.04.019
Rangarajan, Bone, Zmijewska, Jiang, Park et al., Metformin Reverses Established Lung Fibrosis in a Bleomycin Model, Nat Med, doi:10.1038/s41591-018-0087-6
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area, JAMA, doi:10.1001/jama.2020.6775
Scheen, Metformin and COVID-19: From Cellular Mechanisms to Reduced Mortality, Diabetes Metab, doi:10.1016/j.diabet.2020.07.006
Schlesinger, Neuenschwander, Lang, Pafili, Kuss et al., Risk Phenotypes of Diabetes and Association With COVID-19 Severity and Death: A Living Systematic Review and Meta-Analysis, Diabetologia, doi:10.1007/s00125-021-05458-8
Schoen, Horvat, Guerreiro, De Castro, De Giassi, Spectrum of Clinical and Radiographic Findings in Patients With Diagnosis of H1N1 and Correlation With Clinical Severity, BMC Infect Dis, doi:10.1186/s12879-019-4592-0
Soberanes, Misharin, Jairaman, Morales-Nebreda, Pimentel et al., Metformin Targets Mitochondrial Electron Transport to Reduce Air-Pollution-Induced Thrombosis, Cell Metab, doi:10.1016/j.cmet.2018.09.019
Solerte, ' Addio, Trevisan, Lovati, Rossi et al., Sitagliptin Treatment at the Time of Hospitalization Was Associated With Reduced Mortality in Patients With Type 2 Diabetes and COVID-19: A Multicenter, Case-Control, Retrospective, Observational Study, Diabetes Care, doi:10.2337/dc20-1521
Sourij, Aziz, Bräuer, Ciardi, Clodi et al., COVID-19 Fatality Prediction in People With Diabetes and Prediabetes Using a Simple Score Upon Hospital Admission, Diabetes Obes Metab, doi:10.1111/dom.14256
Stang, Critical Evaluation of the Newcastle-Ottawa Scale for the Assessment of the Quality of Nonrandomized Studies in Meta-Analyses, Eur J Epidemiol, doi:10.1007/s10654-010-9491-z
Strollo, Maddaloni, Dauriz, Pedone, Buzzetti et al., Use of DPP4 Inhibitors in Italy Does Not Correlate With Diabetes Prevalence Among COVID-19 Deaths, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108444
Wargny, Potier, Gourdy, Pichelin, Amadou et al., Predictors of Hospital Discharge and Mortality in Patients With Diabetes and COVID-19: Updated Results From the Nationwide CORONADO Study, Diabetologia, doi:10.1007/s00125-020-05351-w
Wilder-Smith, Chiew, Lee, Can We Contain the COVID-19 Outbreak With the Same Measures as for SARS, Lancet Infect Dis, doi:10.1016/S1473-3099(20)30129-8
Wu, Mcgoogan, Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention, JAMA, doi:10.1001/jama.2020.2648
Xu, Du, Zheng, Peng, Sun, Effect of Metformin on Serum Interleukin-6 Levels in Polycystic Ovary Syndrome: A Systematic Review, BMC Womens Health, doi:10.1186/1472-6874-14-93
Yang, Feng, Yuan, Yuan, Fu et al., Plasma Glucose Levels and Diabetes are Independent Predictors for Mortality and Morbidity in Patients With SARS, Diabetes Med, doi:10.1111/j.1464-5491.2006.01861.x
Yang, Yu, Xu, Shu, Xia et al., Clinical Course and Outcomes of Critically Ill Patients With SARS-CoV-2 Pneumonia in Wuhan, China: A Single-Centered, Retrospective, Observational Study, Lancet Respir Med, doi:10.1016/S2213-2600(20)30079-5
Yu, Li, Sun, Wang, Insulin Treatment Is Associated With Increased Mortality in Patients With COVID-19 and Type 2 Diabetes, Cell Metab, doi:10.1016/j.cmet.2020.11.014
Zhou, Wu, Wang, Lei, Cheng et al., No Significant Association Between Dipeptidyl Peptidase-4 Inhibitors and Adverse Outcomes of COVID-19, World J Clin cases, doi:10.12998/wjcc.v8.i22.5576
DOI record:
{
"DOI": "10.3389/fendo.2021.708494",
"ISSN": [
"1664-2392"
],
"URL": "http://dx.doi.org/10.3389/fendo.2021.708494",
"abstract": "<jats:sec><jats:title>Aims</jats:title><jats:p>We conducted a systematic review and meta-analysis to assess various antidiabetic agents’ association with mortality in patients with type 2 diabetes (T2DM) who have coronavirus disease 2019 (COVID-19).</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We performed comprehensive literature retrieval from the date of inception until February 2, 2021, in medical databases (PubMed, Web of Science, Embase, and Cochrane Library), regarding mortality outcomes in patients with T2DM who have COVID-19. Pooled OR and 95% CI data were used to assess relationships between antidiabetic agents and mortality.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Eighteen studies with 17,338 patients were included in the meta-analysis. Metformin (pooled OR, 0.69; <jats:italic>P</jats:italic>=0.001) and sulfonylurea (pooled OR, 0.80; <jats:italic>P</jats:italic>=0.016) were associated with lower mortality risk in patients with T2DM who had COVID-19. However, patients with T2DM who had COVID-19 and received insulin exhibited greater mortality (pooled OR, 2.20; <jats:italic>P</jats:italic>=0.002). Mortality did not significantly differ (pooled OR, 0.72; <jats:italic>P</jats:italic>=0.057) between DPP-4 inhibitor users and non-users.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>Metformin and sulfonylurea could be associated with reduced mortality risk in patients with T2DM who have COVID-19. Furthermore, insulin use could be associated with greater mortality, while DPP-4 inhibitor use could not be. The effects of antidiabetic agents in patients with T2DM who have COVID-19 require further exploration.</jats:p></jats:sec><jats:sec><jats:title>Systematic Review Registration</jats:title><jats:p>PROSPERO (identifier, CRD42021242898).</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fendo.2021.708494"
],
"author": [
{
"affiliation": [],
"family": "Kan",
"given": "Chengxia",
"sequence": "first"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Yang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Han",
"given": "Fang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Xu",
"given": "Qian",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ye",
"given": "Tongtong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hou",
"given": "Ningning",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sun",
"given": "Xiaodong",
"sequence": "additional"
}
],
"container-title": "Frontiers in Endocrinology",
"container-title-short": "Front. Endocrinol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2021,
9,
16
]
],
"date-time": "2021-09-16T04:47:46Z",
"timestamp": 1631767666000
},
"deposited": {
"date-parts": [
[
2021,
9,
16
]
],
"date-time": "2021-09-16T04:47:50Z",
"timestamp": 1631767670000
},
"indexed": {
"date-parts": [
[
2023,
8,
23
]
],
"date-time": "2023-08-23T20:54:56Z",
"timestamp": 1692824096616
},
"is-referenced-by-count": 29,
"issued": {
"date-parts": [
[
2021,
9,
16
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
16
]
],
"date-time": "2021-09-16T00:00:00Z",
"timestamp": 1631750400000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fendo.2021.708494/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2021,
9,
16
]
]
},
"published-online": {
"date-parts": [
[
2021,
9,
16
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1016/S1473-3099(20)30129-8",
"article-title": "Can We Contain the COVID-19 Outbreak With the Same Measures as for SARS",
"author": "Wilder-Smith",
"doi-asserted-by": "publisher",
"first-page": "e102",
"journal-title": "Lancet Infect Dis",
"key": "B1",
"volume": "20",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"article-title": "Clinical Course and Outcomes of Critically Ill Patients With SARS-CoV-2 Pneumonia in Wuhan, China: A Single-Centered, Retrospective, Observational Study",
"author": "Yang",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Respir Med",
"key": "B2",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1701/3347.33180",
"article-title": "[CoViD-19 and Chronic Diseases: Current Knowledge, Future Steps and the MaCroScopio Project.]",
"author": "Martini",
"doi-asserted-by": "publisher",
"first-page": "198",
"journal-title": "Recenti Prog Med",
"key": "B3",
"volume": "111",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6775",
"article-title": "Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area",
"author": "Richardson",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "B4",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2002032",
"article-title": "Clinical Characteristics of Coronavirus Disease 2019 in China",
"author": "Guan",
"doi-asserted-by": "publisher",
"journal-title": "N Engl J Med",
"key": "B5",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.2648",
"article-title": "Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention",
"author": "Wu",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "B6",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.3389/fendo.2020.600439",
"article-title": "Metformin Use Is Associated With Reduced Mortality in a Diverse Population With COVID-19 and Diabetes",
"author": "Crouse",
"doi-asserted-by": "publisher",
"journal-title": "Front Endocrinol (Lausanne)",
"key": "B7",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1111/dom.14256",
"article-title": "COVID-19 Fatality Prediction in People With Diabetes and Prediabetes Using a Simple Score Upon Hospital Admission",
"author": "Sourij",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Obes Metab",
"key": "B8",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.1016/j.obmed.2020.100290",
"article-title": "Metformin Use is Associated With Reduced Mortality Rate From Coronavirus Disease 2019 (COVID-19) Infection",
"author": "Hariyanto",
"doi-asserted-by": "publisher",
"journal-title": "Obes Med",
"key": "B9",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1371/journal.pmed.1000097",
"article-title": "Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement",
"author": "Moher",
"doi-asserted-by": "publisher",
"first-page": "e1000097",
"journal-title": "PloS Med",
"key": "B10",
"volume": "6",
"year": "2009"
},
{
"DOI": "10.1007/s10654-010-9491-z",
"article-title": "Critical Evaluation of the Newcastle-Ottawa Scale for the Assessment of the Quality of Nonrandomized Studies in Meta-Analyses",
"author": "Stang",
"doi-asserted-by": "publisher",
"journal-title": "Eur J Epidemiol",
"key": "B11",
"volume": "25",
"year": "2010"
},
{
"DOI": "10.1136/bmj.315.7109.629",
"article-title": "Bias in Meta-Analysis Detected by a Simple, Graphical Test",
"author": "Egger",
"doi-asserted-by": "publisher",
"journal-title": "BMJ",
"key": "B12",
"volume": "315",
"year": "1997"
},
{
"DOI": "10.2337/dc20-0660",
"article-title": "Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication",
"author": "Chen",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Care",
"key": "B13",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1101/2020.06.19.20135095",
"article-title": "Observational Study of Metformin and Risk of Mortality in Patients Hospitalized With Covid-19",
"author": "Bramante",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "B14",
"year": "2020"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"article-title": "Metformin Treatment Was Associated With Decreased Mortality in COVID-19 Patients With Diabetes in a Retrospective Analysis",
"author": "Luo",
"doi-asserted-by": "publisher",
"first-page": "69",
"journal-title": "Am J Trop Med Hyg",
"key": "B15",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.4093/dmj.2020.0146",
"article-title": "The Clinical Characteristics and Outcomes of Patients With Moderate-To-Severe Coronavirus Disease 2019 Infection and Diabetes in Daegu, South Korea",
"author": "Kim",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab J",
"key": "B16",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.1101/2020.08.12.20156257",
"article-title": "Obesity, Old Age and Frailty are the True Risk Factors for COVID-19 Mortality and Not Chronic Disease or Ethnicity in Croydon",
"author": "Philipose",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "B17",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.08.013",
"article-title": "Metformin Is Associated With Higher Incidence of Acidosis, But Not Mortality, in Individuals With COVID-19 and Pre-Existing Type 2 Diabetes",
"author": "Cheng",
"doi-asserted-by": "publisher",
"first-page": "537",
"journal-title": "Cell Metab",
"key": "B18",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1101/2020.08.20.20174169",
"article-title": "Associations of Comorbidities and Medications With COVID-19 Outcome: A Retrospective Analysis of Real-World Evidence Data",
"author": "Abu-Jamous",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "B19",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108619",
"article-title": "Association of Metformin With Mortality or ARDS in Patients With COVID-19 and Type 2 Diabetes: A Retrospective Cohort Study",
"author": "Jiang",
"doi-asserted-by": "publisher",
"first-page": "108619",
"journal-title": "Diabetes Res Clin Pract",
"key": "B20",
"volume": "173",
"year": "2020"
},
{
"DOI": "10.2337/dc20-1340",
"article-title": "Impact of Comorbidities and Glycemia at Admission and Dipeptidyl Peptidase 4 Inhibitors in Patients With Type 2 Diabetes With COVID-19: A Case Series From an Academic Hospital in Lombardy, Italy",
"author": "Mirani",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Care",
"key": "B21",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.4158/EP-2020-0466",
"article-title": "Metformin Use in Diabetes Prior to Hospitalization: Effects on Mortality in Covid-19",
"author": "Li",
"doi-asserted-by": "publisher",
"journal-title": "Endocr Pract",
"key": "B22",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.101216",
"article-title": "Metformin Use is Associated With a Reduced Risk of Mortality in Patients With Diabetes Hospitalised for COVID-19",
"author": "Lalau",
"doi-asserted-by": "publisher",
"first-page": "101216",
"journal-title": "Diabetes Metab",
"key": "B23",
"volume": "47",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"article-title": "Phenotypic Characteristics and Prognosis of Inpatients With COVID-19 and Diabetes: The CORONADO Study",
"author": "Cariou",
"doi-asserted-by": "publisher",
"journal-title": "Diabetologia",
"key": "B24",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05351-w",
"article-title": "Predictors of Hospital Discharge and Mortality in Patients With Diabetes and COVID-19: Updated Results From the Nationwide CORONADO Study",
"author": "Wargny",
"doi-asserted-by": "publisher",
"journal-title": "Diabetologia",
"key": "B25",
"volume": "64",
"year": "2021"
},
{
"DOI": "10.2337/dc20-1521",
"article-title": "Sitagliptin Treatment at the Time of Hospitalization Was Associated With Reduced Mortality in Patients With Type 2 Diabetes and COVID-19: A Multicenter, Case-Control, Retrospective, Observational Study",
"author": "Solerte",
"doi-asserted-by": "publisher",
"first-page": "2999",
"journal-title": "Diabetes Care",
"key": "B26",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1111/dom.14097",
"article-title": "Exposure to Dipeptidyl-Peptidase-4 Inhibitors and COVID-19 Among People With Type 2 Diabetes: A Case-Control Study",
"author": "Fadini",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Obes Metab",
"key": "B27",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.12998/wjcc.v8.i22.5576",
"article-title": "No Significant Association Between Dipeptidyl Peptidase-4 Inhibitors and Adverse Outcomes of COVID-19",
"author": "Zhou",
"doi-asserted-by": "publisher",
"journal-title": "World J Clin cases",
"key": "B28",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.11.014",
"article-title": "Insulin Treatment Is Associated With Increased Mortality in Patients With COVID-19 and Type 2 Diabetes",
"author": "Yu",
"doi-asserted-by": "publisher",
"first-page": "65",
"journal-title": "Cell Metab",
"key": "B29",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.04.018",
"article-title": "Diabetes Mellitus Is Associated With Increased Mortality and Severity of Disease in COVID-19 Pneumonia - A Systematic Review, Meta-Analysis, and Meta-Regression",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "395",
"journal-title": "Diabetes Metab Syndr",
"key": "B30",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(15)00379-4",
"article-title": "Diabetes and Infection: Assessing the Association With Glycaemic Control in Population-Based Studies",
"author": "Pearson-Stuttard",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "B31",
"volume": "4",
"year": "2016"
},
{
"DOI": "10.1186/s12879-019-4592-0",
"article-title": "Spectrum of Clinical and Radiographic Findings in Patients With Diagnosis of H1N1 and Correlation With Clinical Severity",
"author": "Schoen",
"doi-asserted-by": "publisher",
"first-page": "964",
"journal-title": "BMC Infect Dis",
"key": "B32",
"volume": "19",
"year": "2019"
},
{
"DOI": "10.1111/j.1464-5491.2006.01861.x",
"article-title": "Plasma Glucose Levels and Diabetes are Independent Predictors for Mortality and Morbidity in Patients With SARS",
"author": "Yang",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Med",
"key": "B33",
"volume": "23",
"year": "2006"
},
{
"DOI": "10.1007/s12250-015-3679-z",
"article-title": "Risk Factors for Severity and Mortality in Patients With MERS-CoV: Analysis of Publicly Available Data From Saudi Arabia",
"author": "Banik",
"doi-asserted-by": "publisher",
"journal-title": "Virol Sin",
"key": "B34",
"volume": "31",
"year": "2016"
},
{
"DOI": "10.1001/jama.2020.4683",
"article-title": "Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy",
"author": "Onder",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "B35",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1007/s00125-021-05458-8",
"article-title": "Risk Phenotypes of Diabetes and Association With COVID-19 Severity and Death: A Living Systematic Review and Meta-Analysis",
"author": "Schlesinger",
"doi-asserted-by": "publisher",
"journal-title": "Diabetologia",
"key": "B36",
"volume": "64",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26498",
"article-title": "Mortality Risk With Preadmission Metformin Use in Patients With COVID-19 and Diabetes: A Meta-Analysis",
"author": "Kow",
"doi-asserted-by": "publisher",
"journal-title": "J Med Virol",
"key": "B37",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1016/j.diabet.2020.07.006",
"article-title": "Metformin and COVID-19: From Cellular Mechanisms to Reduced Mortality",
"author": "Scheen",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab",
"key": "B38",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.11.006",
"article-title": "The Effect of Metformin Consumption on Mortality in Hospitalized COVID-19 Patients: A Systematic Review and Meta-Analysis",
"author": "Lukito",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab Syndr",
"key": "B39",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.2337/diabetes.55.02.06.db05-1064",
"article-title": "Activation of the AMP-Activated Kinase by Antidiabetes Drug Metformin Stimulates Nitric Oxide Synthesis In Vivo by Promoting the Association of Heat Shock Protein 90 and Endothelial Nitric Oxide Synthase",
"author": "Davis",
"doi-asserted-by": "publisher",
"first-page": "496",
"journal-title": "Diabetes",
"key": "B40",
"volume": "55",
"year": "2006"
},
{
"DOI": "10.1161/01.HYP.0000221429.94591.72",
"article-title": "Metformin Inhibits Cytokine-Induced Nuclear Factor kappaB Activation via AMP-Activated Protein Kinase Activation in Vascular Endothelial Cells",
"author": "Hattori",
"doi-asserted-by": "publisher",
"journal-title": "Hypertension",
"key": "B41",
"volume": "47",
"year": "2006"
},
{
"DOI": "10.1038/s41591-018-0087-6",
"article-title": "Metformin Reverses Established Lung Fibrosis in a Bleomycin Model",
"author": "Rangarajan",
"doi-asserted-by": "publisher",
"journal-title": "Nat Med",
"key": "B42",
"volume": "24",
"year": "2018"
},
{
"DOI": "10.1038/s41375-019-0470-4",
"article-title": "Metformin Inhibits IL-6 Signaling by Decreasing IL-6R Expression on Multiple Myeloma Cells",
"author": "Mishra",
"doi-asserted-by": "publisher",
"journal-title": "Leukemia",
"key": "B43",
"volume": "33",
"year": "2019"
},
{
"DOI": "10.1186/1472-6874-14-93",
"article-title": "Effect of Metformin on Serum Interleukin-6 Levels in Polycystic Ovary Syndrome: A Systematic Review",
"author": "Xu",
"doi-asserted-by": "publisher",
"first-page": "93",
"journal-title": "BMC Womens Health",
"key": "B44",
"volume": "14",
"year": "2014"
},
{
"DOI": "10.1016/j.cmet.2018.09.019",
"article-title": "Metformin Targets Mitochondrial Electron Transport to Reduce Air-Pollution-Induced Thrombosis",
"author": "Soberanes",
"doi-asserted-by": "publisher",
"first-page": "335",
"journal-title": "Cell Metab",
"key": "B45",
"volume": "29",
"year": "2019"
},
{
"DOI": "10.1007/s40200-021-00777-4",
"article-title": "Dipeptidyl Peptidase 4 (DPP4) Inhibitor and Outcome From Coronavirus Disease 2019 (COVID-19) in Diabetic Patients: A Systematic Review, Meta-Analysis, and Meta-Regression",
"author": "Hariyanto",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Diabetes Metab Disord",
"key": "B46",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1016/j.diabres.2020.108444",
"article-title": "Use of DPP4 Inhibitors in Italy Does Not Correlate With Diabetes Prevalence Among COVID-19 Deaths",
"author": "Strollo",
"doi-asserted-by": "publisher",
"first-page": "108444",
"journal-title": "Diabetes Res Clin Pract",
"key": "B47",
"volume": "171",
"year": "2021"
},
{
"DOI": "10.2337/dci20-0062",
"article-title": "Reduced COVID-19 Mortality With Sitagliptin Treatment? Weighing the Dissemination of Potentially Lifesaving Findings Against the Assurance of High Scientific Standards",
"author": "Nauck",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Care",
"key": "B48",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108125",
"article-title": "COVID-19 and Diabetes: Can DPP4 Inhibition Play a Role",
"author": "Iacobellis",
"doi-asserted-by": "publisher",
"first-page": "108125",
"journal-title": "Diabetes Res Clin Pract",
"key": "B49",
"volume": "162",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.03.002",
"article-title": "Clinical Considerations for Patients With Diabetes in Times of COVID-19 Epidemic",
"author": "Gupta",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab Syndr",
"key": "B50",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1111/1753-0407.13027",
"article-title": "Diabetes and COVID-19",
"author": "Bloomgarden",
"doi-asserted-by": "publisher",
"journal-title": "J Diabetes",
"key": "B51",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1007/s00268-016-3469-2",
"article-title": "Insulin-Treated Patients With Diabetes Mellitus Undergoing Emergency Abdominal Surgery Have Worse Outcomes Than Patients Treated With Oral Agents",
"author": "Haltmeier",
"doi-asserted-by": "publisher",
"journal-title": "World J Surg",
"key": "B52",
"volume": "40",
"year": "2016"
},
{
"DOI": "10.1056/NEJMoa0810625",
"article-title": "Intensive Versus Conventional Glucose Control in Critically Ill Patients",
"author": "Finfer",
"doi-asserted-by": "publisher",
"journal-title": "N Engl J Med",
"key": "B53",
"volume": "360",
"year": "2009"
},
{
"DOI": "10.1007/s00406-020-01205-z",
"article-title": "Dementia is a Predictor for Mortality Outcome From Coronavirus Disease 2019 (COVID-19) Infection",
"author": "Hariyanto",
"doi-asserted-by": "publisher",
"journal-title": "Eur Arch Psychiatry Clin Neurosci",
"key": "B54",
"volume": "271",
"year": "2021"
},
{
"DOI": "10.1016/j.parkreldis.2021.04.019",
"article-title": "Parkinson’s Disease may Worsen Outcomes From Coronavirus Disease 2019 (COVID-19) Pneumonia in Hospitalized Patients: A Systematic Review, Meta-Analysis, and Meta-Regression",
"author": "Putri",
"doi-asserted-by": "publisher",
"journal-title": "Parkinsonism Relat Disord",
"key": "B55",
"volume": "87",
"year": "2021"
}
],
"reference-count": 55,
"references-count": 55,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fendo.2021.708494/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "12"
}
