The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus
et al., Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2021.108977, Aug 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
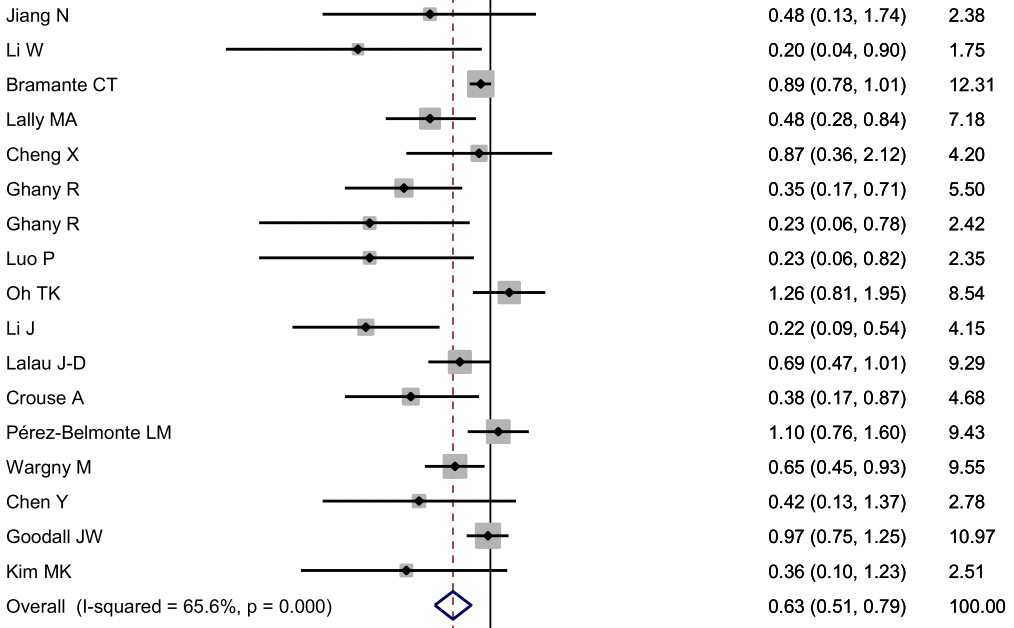
Meta analysis of 17 studies including 20,719 COVID-19 patients with diabetes, showing lower risk of mortality and severity with metformin.
24 meta-analyses show significant improvements with metformin for mortality1-23,
hospitalization7,13,23 ,
progression1, and
severity8,9,13 .
Currently there are 110 metformin for COVID-19 studies, showing 36% lower mortality [32‑40%], 29% lower ventilation [12‑43%], 19% lower ICU admission [8‑28%], 17% lower hospitalization [11‑23%], and 5% fewer cases [-4‑13%].
|
risk of death, 36.0% lower, OR 0.64, p < 0.001, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Yang et al., The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus, Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2021.108977.
2.
Lukito et al., The Effect of Metformin Consumption on Mortality in Hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes & Metabolic Syndrome: Clinical Research & Reviews, doi:10.1016/j.dsx.2020.11.006.
3.
Kow et al., Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis, Journal of Medical Virology, doi:10.1002/jmv.26498.
4.
Hariyanto et al., Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection, Obesity Medicine, doi:10.1016/j.obmed.2020.100290.
5.
Ma et al., Is metformin use associated with low mortality in patients with type 2 diabetes mellitus hospitalized for COVID-19? a multivariable and propensity score-adjusted meta-analysis, PLOS ONE, doi:10.1371/journal.pone.0282210.
6.
Parveen et al., Association of Metformin with Mortality in COVID-19 Patients: A Systematic Review and Meta-Analysis, Annals of the National Academy of Medical Sciences (India), doi:10.1055/s-0042-1760353.
7.
Li et al., Metformin in Patients With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Medicine, doi:10.3389/fmed.2021.704666.
8.
Schlesinger et al., Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis, Diabetologia, doi:10.1007/s00125-023-05928-1.
9.
Petrelli et al., Metformin and Covid-19: a systematic review of systematic reviews with meta-analysis, Acta Biomedica Atenei Parmensis, doi:10.23750/abm.v94iS3.14405.
10.
Oscanoa et al., Metformin therapy and severity and mortality of SARS-CoV-2 infection: a meta-analysis, Clinical Diabetology, doi:10.5603/DK.a2021.0035.
11.
Kan et al., Mortality Risk of Antidiabetic Agents for Type 2 Diabetes With COVID-19: A Systematic Review and Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2021.708494.
12.
Poly et al., Metformin Use Is Associated with Decreased Mortality in COVID-19 Patients with Diabetes: Evidence from Retrospective Studies and Biological Mechanism, Journal of Clinical Medicine, doi:10.3390/jcm10163507.
13.
Song et al., The Effect of Antihyperglycemic Medications on COVID-19: A Meta-analysis and Systematic Review from Observational Studies, Therapeutic Innovation & Regulatory Science, doi:10.1007/s43441-024-00633-6.
14.
Ganesh et al., Does metformin affect outcomes in COVID‐19 patients with new or pre‐existing diabetes mellitus? A systematic review and meta‐analysis, British Journal of Clinical Pharmacology, doi:10.1111/bcp.15258.
15.
Nassar et al., Noninsulin‐based antihyperglycemic medications in patients with diabetes and COVID‐19: A systematic review and meta‐analysis, Journal of Diabetes, doi:10.1111/1753-0407.13359.
16.
Zhan et al., Effect of Antidiabetic Therapy on Clinical Outcomes of COVID-19 Patients With Type 2 Diabetes: A Systematic Review and Meta-Analysis, Annals of Pharmacotherapy, doi:10.1177/10600280221133577.
17.
Nguyen et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: A meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196.
18.
Han et al., Association Between Anti-diabetic Agents and Clinical Outcomes of COVID-19 in Patients with Diabetes: A Systematic Review and Meta-Analysis, Archives of Medical Research, doi:10.1016/j.arcmed.2021.08.002.
19.
Chen et al., The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis, Frontiers in Endocrinology, doi:10.3389/fendo.2022.895458.
20.
Scheen, A., Metformin and COVID-19: From cellular mechanisms to reduced mortality, Diabetes & Metabolism, doi:10.1016/j.diabet.2020.07.006.
21.
Sun et al., Is Metformin Use Associated With a Decreased Mortality for COVID-19 Diabetic Patients? A Meta-Analysis, Journal of the Endocrine Society, doi:10.1210/jendso/bvab048.709.
Yang et al., 31 Aug 2021, peer-reviewed, 4 authors.
The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus
Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2021.108977
Aim: COVID-19 has spread globally with heavy impact on most countries and our therapeutic strategies in COVID-19 patients with diabetes are still limited. Recently, some new information was added to this field. We performed this updated meta-analysis to reveal the underlying effect of metformin on COVID-19 patients with diabetes. Methods: We searched the PubMed, Embase and CNKI (China National Knowledge Infrastructure) databases for all articles. The odds ratio (OR) corresponding to the 95% confidence interval (95% CI) was used to assess the effect of metformin on COVID-19 patients with diabetes. The statistical heterogeneity among studies was assessed with the Q-test and I 2 statistics. Results: We collected 17 studies including 20,719 COVID-19 patients with diabetes. Our results found that metformin was associated with significantly decreased mortality and severity in COVID-19 patients with diabetes (OR = 0.64, 95% CI = 0.51-0.79 for mortality, and OR = 0.81, 95% CI = 0.66-0.99 for severity). Conclusions: Our meta-analysis indicated that following metformin treatment might benefit the patients with T2DM, both the mortality and severity. However, patients with severe COVID-19 should be monitored closely for the development of lactic acidosis, acidosis, and decreased kidney function.
References
Begg, Mazumdar, Operating characteristics of a rank correlation test for publication bias, Biometrics, doi:10.2307/2533446
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis, Lancet Healthy Longev
Bramante, Ingraham, Murray, Marmor, Hovertsen et al., Observational Study of Metformin and Risk of Mortality in Patients Hospitalized with Covid-19, medRxiv
Cariou, Hadjadj, Wargny, Pichelin, Al-Salameh et al., Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia
Chen, Ou, Li, Hu, Shao et al., Metformin extends C. elegans lifespan through lysosomal pathway, Elife
Chen, Yang, Cheng, Chen, Peng et al., Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care
Crouse, Grimes, Li, Might, Ovalle et al., metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes
Dalan, Metformin, neutrophils and COVID-19 infection, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108230
Dersimonian, Laird, Meta-analysis in clinical trials, Control Clin Trials
Erener, Diabetes, infection risk and COVID-19, Mol Metab, doi:10.1016/j.molmet.2020.101044
Gao, Liu, Zhong, Liu, Zhou et al., Risk of metformin in patients with type 2 diabetes with COVID-19: a preliminary retrospective report, Clin Transl Sci
Ghany, Palacio, Dawkins, Chen, Mccarter et al., Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA, Diabetes Metab Syndr
Goodall, Reed, Ardissino, Bassett, Whittington et al., Risk factors for severe disease in patients admitted with COVID-19 to a hospital in London, England: a retrospective cohort study, Epidemiol Infect, doi:10.1017/S0950268820002472
Haes, Frooninckx, Van Assche, Smolders, Depuydt et al., Metformin promotes lifespan through mitohormesis via the peroxiredoxin PRDX-2, Proc Natl Acad Sci U S A
Hahn, Ejaz, Kanbay, Lanaspa, Johnson, Acute kidney injury from SGLT2 inhibitors: potential mechanisms, Nat Rev Nephrol
Higgins, Thompson, Quantifying heterogeneity in a meta-analysis, Stat Med
Holman, Knighton, Kar, 'keefe, Curley et al., Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a populationbased cohort study, Lancet Diabetes Endocrinol
Inzucchi, Bergenstal, Buse, Diamant, Ferrannini et al., Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes, Diabetes Care
Jiang, Chen, Li, Yin, Yang et al., Association of metformin with mortality or ARDS in patients with COVID-19 and type 2 diabetes: a retrospective cohort study, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108619
Kim, Jeon, Kim, Moon, Cho et al., The clinical characteristics and outcomes of patients with moderate-to-severe coronavirus disease 2019 infection and diabetes in Daegu, South Korea, Diabetes Metab J, doi:10.4093/dmj.2020.0146
Lalau, Al-Salameh, Hadjadj, Goronflot, Wiernsperger et al., Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19, Diabetes Metab
Lally, Tsoukas, Halladay, Neill, Gravenstein et al., Metformin is associated with decreased 30-day mortality among nursing home residents infected with SARS-CoV2, J Am Med Dir Assoc
Lazarus, Suhardi, Wiyarta, Rasyidah, Barliana, Is there a need to reconsider the use of metformin in COVID-19 patients with type 2 diabetes mellitus?, Int J Diabetes Dev Ctries
Li, Deng, Sheng, Zuo, Metformin attenuates Alzheimer's disease-like neuropathology in obese, leptinresistant mice, Pharmacol Biochem Behav
Li, Li, Wei, Mccowen, Xiong et al., Inpatient use of metformin and acarbose is associated with reduced mortality of COVID-19 patients with type 2 diabetes mellitus, Res Sq
Li, Qi, Li, Mccowen, Xiong et al., Metformin use in diabetes prior to hospitalization: effects on mortality in Covid-19, Endocr Pract
Lim, Bae, Kwon, Nauck, COVID-19 and diabetes mellitus: from pathophysiology to clinical management, Nat Rev Endocrinol
Lukito, Pranata, Henrina, Lim, Lawrensia et al., The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr
Luo, Qiu, Liu, Liu, Zheng et al., Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am J Trop Med Hyg
Mantel, Haenszel, Statistical aspects of the analysis of data from retrospective studies of disease, J Natl Cancer Inst
Moher, Liberati, Tetzlaff, Altman, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement, BMJ
Nauck, Meier, Management of endocrine disease: are all GLP-1 agonists equal in the treatment of type 2 diabetes?, Eur J Endocrinol
Oh, Song, Metformin use and risk of COVID-19 among patients with type II diabetes mellitus: an NHIS-COVID-19 database cohort study, Acta Diabetol
Pe ´rez-Belmonte, Torres-Pen ˜a, Lo ´pez-Carmona, Ayala-Gutie ´rrez, Fuentes-Jime ´nez et al., Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: a nationwide cohort study, BMC Med, doi:10.1186/s12916-020-01832-2
Pryor, Norvaisas, Marinos, Best, Thingholm et al., Host-microbe-drug-nutrient screen identifies bacterial effectors of metformin therapy, Cell
Rizos, Elisaf, Metformin and cancer, Eur J Pharmacol
Schuiveling, Vazirpanah, Radstake, Zimmermann, Broen, Metformin, a new era for an old drug in the treatment of immune mediated disease?, Curr Drug Targets
Valencia, Peiro, Lorenzo, Sa ´nchez-Ferrer, Eckel et al., DPP4 and ACE2 in diabetes and COVID-19: therapeutic targets for cardiovascular complications?, Front Pharmacol
Wargny, Potier, Gourdy, Pichelin, Amadou et al., Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study, Diabetologia
Wu, Esteve, Tremaroli, Khan, Caesar et al., Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug, Nat Med
Xu, Liu, Li, Zhang, Lei et al., Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and preexisting type 2 diabetes, Cell Metab
Zangrillo, Beretta, Scandroglio, Monti, Fominskiy et al., Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy, Crit Care Resusc
Zhang, Li, Ma, Zong, Cui et al., Metformin activates AMPK through the lysosomal pathway, Cell Metab
Zhu, She, Xu, Qin, Zhang et al., Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab
DOI record:
{
"DOI": "10.1016/j.diabres.2021.108977",
"ISSN": [
"0168-8227"
],
"URL": "http://dx.doi.org/10.1016/j.diabres.2021.108977",
"alternative-id": [
"S0168822721003363"
],
"article-number": "108977",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Diabetes Research and Clinical Practice"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.diabres.2021.108977"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2021 Elsevier B.V. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "Yang",
"given": "Wenxing",
"sequence": "first"
},
{
"affiliation": [],
"family": "Sun",
"given": "Xuehong",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Jun",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zhang",
"given": "Kui",
"sequence": "additional"
}
],
"container-title": [
"Diabetes Research and Clinical Practice"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"diabetesresearchclinicalpractice.com",
"clinicalkey.jp",
"clinicalkey.com",
"clinicalkey.es",
"clinicalkey.fr",
"clinicalkey.com.au",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2021,
7,
22
]
],
"date-time": "2021-07-22T06:03:50Z",
"timestamp": 1626933830000
},
"deposited": {
"date-parts": [
[
2021,
9,
4
]
],
"date-time": "2021-09-04T04:54:47Z",
"timestamp": 1630731287000
},
"indexed": {
"date-parts": [
[
2022,
2,
10
]
],
"date-time": "2022-02-10T09:04:57Z",
"timestamp": 1644483897995
},
"is-referenced-by-count": 7,
"issn-type": [
{
"type": "print",
"value": "0168-8227"
}
],
"issued": {
"date-parts": [
[
2021,
8
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
8,
1
]
],
"date-time": "2021-08-01T00:00:00Z",
"timestamp": 1627776000000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0168822721003363?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0168822721003363?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "108977",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2021,
8
]
]
},
"published-print": {
"date-parts": [
[
2021,
8
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"article-title": "Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study",
"author": "Holman",
"doi-asserted-by": "crossref",
"first-page": "823",
"issue": "10",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.1016/j.diabres.2021.108977_b0005",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"article-title": "Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "1068",
"issue": "6",
"journal-title": "Cell Metab",
"key": "10.1016/j.diabres.2021.108977_b0010",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1038/s41574-020-00435-4",
"article-title": "COVID-19 and diabetes mellitus: from pathophysiology to clinical management",
"author": "Lim",
"doi-asserted-by": "crossref",
"first-page": "11",
"issue": "1",
"journal-title": "Nat Rev Endocrinol",
"key": "10.1016/j.diabres.2021.108977_b0015",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.3389/fphar.2020.01161",
"article-title": "DPP4 and ACE2 in diabetes and COVID-19: therapeutic targets for cardiovascular complications?",
"author": "Valencia",
"doi-asserted-by": "crossref",
"first-page": "1161",
"journal-title": "Front Pharmacol",
"key": "10.1016/j.diabres.2021.108977_b0020",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1530/EJE-19-0566",
"article-title": "Management of endocrine disease: are all GLP-1 agonists equal in the treatment of type 2 diabetes?",
"author": "Nauck",
"doi-asserted-by": "crossref",
"first-page": "R211",
"journal-title": "Eur J Endocrinol",
"key": "10.1016/j.diabres.2021.108977_b0025",
"volume": "181",
"year": "2019"
},
{
"DOI": "10.1038/nrneph.2016.159",
"article-title": "Acute kidney injury from SGLT2 inhibitors: potential mechanisms",
"author": "Hahn",
"doi-asserted-by": "crossref",
"first-page": "711",
"issue": "12",
"journal-title": "Nat Rev Nephrol",
"key": "10.1016/j.diabres.2021.108977_b0030",
"volume": "12",
"year": "2016"
},
{
"DOI": "10.2337/dc14-2441",
"article-title": "Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes",
"author": "Inzucchi",
"doi-asserted-by": "crossref",
"first-page": "140",
"issue": "1",
"journal-title": "Diabetes Care",
"key": "10.1016/j.diabres.2021.108977_b0035",
"volume": "38",
"year": "2015"
},
{
"DOI": "10.1136/bmj.b2535",
"article-title": "Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement",
"author": "Moher",
"doi-asserted-by": "crossref",
"first-page": "b2535",
"journal-title": "BMJ",
"key": "10.1016/j.diabres.2021.108977_b0040",
"volume": "339",
"year": "2009"
},
{
"DOI": "10.1002/sim.1186",
"article-title": "Quantifying heterogeneity in a meta-analysis",
"author": "Higgins",
"doi-asserted-by": "crossref",
"first-page": "1539",
"issue": "11",
"journal-title": "Stat Med",
"key": "10.1016/j.diabres.2021.108977_b0045",
"volume": "21",
"year": "2002"
},
{
"article-title": "Statistical aspects of the analysis of data from retrospective studies of disease",
"author": "Mantel",
"first-page": "719",
"journal-title": "J Natl Cancer Inst",
"key": "10.1016/j.diabres.2021.108977_b0050",
"volume": "22",
"year": "1959"
},
{
"DOI": "10.1016/0197-2456(86)90046-2",
"article-title": "Meta-analysis in clinical trials",
"author": "DerSimonian",
"doi-asserted-by": "crossref",
"first-page": "177",
"issue": "3",
"journal-title": "Control Clin Trials",
"key": "10.1016/j.diabres.2021.108977_b0055",
"volume": "7",
"year": "1986"
},
{
"DOI": "10.2307/2533446",
"article-title": "Operating characteristics of a rank correlation test for publication bias",
"author": "Begg",
"doi-asserted-by": "crossref",
"first-page": "1088",
"issue": "4",
"journal-title": "Biometrics",
"key": "10.1016/j.diabres.2021.108977_b0060",
"volume": "50",
"year": "1994"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"article-title": "Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study",
"author": "Cariou",
"doi-asserted-by": "crossref",
"first-page": "1500",
"issue": "8",
"journal-title": "Diabetologia",
"key": "10.1016/j.diabres.2021.108977_b0065",
"volume": "63",
"year": "2020"
},
{
"article-title": "Observational Study of Metformin and Risk of Mortality in Patients Hospitalized with Covid-19",
"author": "Bramante",
"journal-title": "medRxiv",
"key": "10.1016/j.diabres.2021.108977_b0070",
"year": "2020"
},
{
"DOI": "10.1016/j.molmet.2020.101044",
"article-title": "Diabetes, infection risk and COVID-19",
"author": "Erener",
"doi-asserted-by": "crossref",
"first-page": "101044",
"journal-title": "Mol Metab",
"key": "10.1016/j.diabres.2021.108977_b0075",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.11.006",
"article-title": "The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis",
"author": "Lukito",
"doi-asserted-by": "crossref",
"first-page": "2177",
"issue": "6",
"journal-title": "Diabetes Metab Syndr",
"key": "10.1016/j.diabres.2021.108977_b0080",
"volume": "14",
"year": "2020"
},
{
"article-title": "Is there a need to reconsider the use of metformin in COVID-19 patients with type 2 diabetes mellitus?",
"author": "Lazarus",
"first-page": "1",
"journal-title": "Int J Diabetes Dev Ctries",
"key": "10.1016/j.diabres.2021.108977_b0085",
"year": "2021"
},
{
"DOI": "10.1016/S2666-7568(20)30033-7",
"article-title": "Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis",
"author": "Bramante",
"doi-asserted-by": "crossref",
"first-page": "e34",
"issue": "1",
"journal-title": "Lancet Healthy Longev",
"key": "10.1016/j.diabres.2021.108977_b0090",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2021.02.022",
"article-title": "Metformin is associated with lower hospitalizations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA",
"author": "Ghany",
"doi-asserted-by": "crossref",
"first-page": "513",
"issue": "2",
"journal-title": "Diabetes Metab Syndr",
"key": "10.1016/j.diabres.2021.108977_b0095",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1016/j.diabres.2020.108619",
"article-title": "Association of metformin with mortality or ARDS in patients with COVID-19 and type 2 diabetes: a retrospective cohort study",
"author": "Jiang",
"doi-asserted-by": "crossref",
"first-page": "108619",
"journal-title": "Diabetes Res Clin Pract",
"key": "10.1016/j.diabres.2021.108977_b0100",
"volume": "173",
"year": "2021"
},
{
"DOI": "10.1016/j.jamda.2020.10.031",
"article-title": "Metformin is associated with decreased 30-day mortality among nursing home residents infected with SARS-CoV2",
"author": "Lally",
"doi-asserted-by": "crossref",
"first-page": "193",
"issue": "1",
"journal-title": "J Am Med Dir Assoc",
"key": "10.1016/j.diabres.2021.108977_b0105",
"volume": "22",
"year": "2021"
},
{
"article-title": "Inpatient use of metformin and acarbose is associated with reduced mortality of COVID-19 patients with type 2 diabetes mellitus",
"author": "Li",
"journal-title": "Res Sq",
"key": "10.1016/j.diabres.2021.108977_b0110",
"year": "2021"
},
{
"DOI": "10.1007/s00592-020-01666-7",
"article-title": "Metformin use and risk of COVID-19 among patients with type II diabetes mellitus: an NHIS-COVID-19 database cohort study",
"author": "Oh",
"doi-asserted-by": "crossref",
"first-page": "771",
"issue": "6",
"journal-title": "Acta Diabetol",
"key": "10.1016/j.diabres.2021.108977_b0115",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.1007/s00125-020-05351-w",
"article-title": "Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study",
"author": "Wargny",
"doi-asserted-by": "crossref",
"first-page": "778",
"issue": "4",
"journal-title": "Diabetologia",
"key": "10.1016/j.diabres.2021.108977_b0120",
"volume": "64",
"year": "2021"
},
{
"DOI": "10.7554/eLife.31268",
"article-title": "Metformin extends C. elegans lifespan through lysosomal pathway",
"author": "Chen",
"doi-asserted-by": "crossref",
"journal-title": "Elife",
"key": "10.1016/j.diabres.2021.108977_b0125",
"volume": "6",
"year": "2017"
},
{
"DOI": "10.1016/j.ejphar.2013.02.038",
"article-title": "Metformin and cancer",
"author": "Rizos",
"doi-asserted-by": "crossref",
"first-page": "96",
"issue": "1-3",
"journal-title": "Eur J Pharmacol",
"key": "10.1016/j.diabres.2021.108977_b0130",
"volume": "705",
"year": "2013"
},
{
"DOI": "10.1016/j.pbb.2012.03.002",
"article-title": "Metformin attenuates Alzheimer's disease-like neuropathology in obese, leptin-resistant mice",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "564",
"issue": "4",
"journal-title": "Pharmacol Biochem Behav",
"key": "10.1016/j.diabres.2021.108977_b0135",
"volume": "101",
"year": "2012"
},
{
"DOI": "10.1073/pnas.1321776111",
"article-title": "Metformin promotes lifespan through mitohormesis via the peroxiredoxin PRDX-2",
"author": "De Haes",
"doi-asserted-by": "crossref",
"first-page": "E2501",
"issue": "24",
"journal-title": "Proc Natl Acad Sci U S A",
"key": "10.1016/j.diabres.2021.108977_b0140",
"volume": "111",
"year": "2014"
},
{
"DOI": "10.1016/j.cmet.2016.09.003",
"article-title": "Metformin activates AMPK through the lysosomal pathway",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "521",
"issue": "4",
"journal-title": "Cell Metab",
"key": "10.1016/j.diabres.2021.108977_b0145",
"volume": "24",
"year": "2016"
},
{
"DOI": "10.1038/nm.4345",
"article-title": "Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "850",
"issue": "7",
"journal-title": "Nat Med",
"key": "10.1016/j.diabres.2021.108977_b0150",
"volume": "23",
"year": "2017"
},
{
"DOI": "10.1016/j.cell.2019.08.003",
"article-title": "Host-microbe-drug-nutrient screen identifies bacterial effectors of metformin therapy",
"author": "Pryor",
"doi-asserted-by": "crossref",
"first-page": "1299",
"issue": "6",
"journal-title": "Cell",
"key": "10.1016/j.diabres.2021.108977_b0155",
"volume": "178",
"year": "2019"
},
{
"DOI": "10.2174/1389450118666170613081730",
"article-title": "Metformin, a new era for an old drug in the treatment of immune mediated disease?",
"author": "Schuiveling",
"doi-asserted-by": "crossref",
"first-page": "945",
"issue": "8",
"journal-title": "Curr Drug Targets",
"key": "10.1016/j.diabres.2021.108977_b0160",
"volume": "19",
"year": "2018"
},
{
"DOI": "10.1016/j.diabres.2020.108230",
"article-title": "Metformin, neutrophils and COVID-19 infection",
"author": "Dalan",
"doi-asserted-by": "crossref",
"first-page": "108230",
"journal-title": "Diabetes Res Clin Pract",
"key": "10.1016/j.diabres.2021.108977_b0165",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.2337/dc20-0660",
"article-title": "Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "1399",
"issue": "7",
"journal-title": "Diabetes Care",
"key": "10.1016/j.diabres.2021.108977_b0170",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.08.013",
"article-title": "Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and pre-existing type 2 diabetes",
"author": "Cheng",
"doi-asserted-by": "crossref",
"first-page": "537",
"issue": "4",
"journal-title": "Cell Metab",
"key": "10.1016/j.diabres.2021.108977_b0175",
"volume": "32",
"year": "2020"
},
{
"article-title": "Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19",
"author": "Lalau",
"journal-title": "Diabetes Metab",
"key": "10.1016/j.diabres.2021.108977_b0180",
"volume": "47",
"year": "2020"
},
{
"DOI": "10.4093/dmj.2020.0146",
"article-title": "The clinical characteristics and outcomes of patients with moderate-to-severe coronavirus disease 2019 infection and diabetes in Daegu, South Korea",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "602",
"issue": "4",
"journal-title": "Diabetes Metab J",
"key": "10.1016/j.diabres.2021.108977_b0185",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.1186/s12916-020-01832-2",
"article-title": "Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: a nationwide cohort study",
"author": "Pérez-Belmonte",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "BMC Med",
"key": "10.1016/j.diabres.2021.108977_b0190",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1017/S0950268820002472",
"article-title": "Risk factors for severe disease in patients admitted with COVID-19 to a hospital in London, England: a retrospective cohort study",
"author": "Goodall",
"doi-asserted-by": "crossref",
"journal-title": "Epidemiol Infect",
"key": "10.1016/j.diabres.2021.108977_b0195",
"volume": "148",
"year": "2020"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"article-title": "Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "69",
"journal-title": "Am J Trop Med Hyg",
"key": "10.1016/j.diabres.2021.108977_b0200",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.4158/EP-2020-0466",
"article-title": "Metformin use in diabetes prior to hospitalization: effects on mortality in Covid-19",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "1166",
"issue": "10",
"journal-title": "Endocr Pract",
"key": "10.1016/j.diabres.2021.108977_b0205",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1101/2020.07.29.20164020",
"doi-asserted-by": "crossref",
"key": "10.1016/j.diabres.2021.108977_b0210",
"unstructured": "Crouse A, Grimes T, Li P, Might M, Ovalle F, Shalev A. metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes. medRxiv. 2020."
},
{
"article-title": "Characteristics, treatment, outcomes and cause of death of invasively ventilated patients with COVID-19 ARDS in Milan, Italy",
"author": "Zangrillo",
"journal-title": "Crit Care Resusc",
"key": "10.1016/j.diabres.2021.108977_b0215",
"year": "2020"
},
{
"DOI": "10.1111/cts.12897",
"article-title": "Risk of metformin in patients with type 2 diabetes with COVID-19: a preliminary retrospective report",
"author": "Gao",
"doi-asserted-by": "crossref",
"first-page": "1055",
"issue": "6",
"journal-title": "Clin Transl Sci",
"key": "10.1016/j.diabres.2021.108977_b0220",
"volume": "13",
"year": "2020"
}
],
"reference-count": 44,
"references-count": 44,
"relation": {},
"score": 1,
"short-container-title": [
"Diabetes Research and Clinical Practice"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology",
"General Medicine",
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": [
"The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "178"
}
