Risk factors for severe disease in patients admitted with COVID-19 to a hospital in London, England: a retrospective cohort study
et al., Epidemiology and Infection, doi:10.1017/S0950268820002472, Oct 2020
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 981 hospitalized patients in the UK, showing no significant difference with metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
the United Kingdom, is very poor with very low average efficacy for approved treatments1.
The United Kingdom focused on expensive high-profit treatments, approving only one low-cost early treatment, which required a prescription and had limited adoption. The high-cost prescription treatment strategy reduces the probability of early treatment due to access and cost barriers, and eliminates complementary and synergistic benefits seen with many low-cost treatments.
This may explain in part the very high mortality seen in this study.
Results may differ in countries with improved SOC.
|
risk of death, 3.0% lower, HR 0.97, p = 0.81, treatment 74 of 210 (35.2%), control 280 of 771 (36.3%), NNT 93.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Goodall et al., 13 Oct 2020, retrospective, United Kingdom, peer-reviewed, 7 authors, study period 12 March, 2020 - 15 April, 2020.
Risk factors for severe disease in patients admitted with COVID-19 to a hospital in London, England: a retrospective cohort study
Epidemiology and Infection, doi:10.1017/s0950268820002472
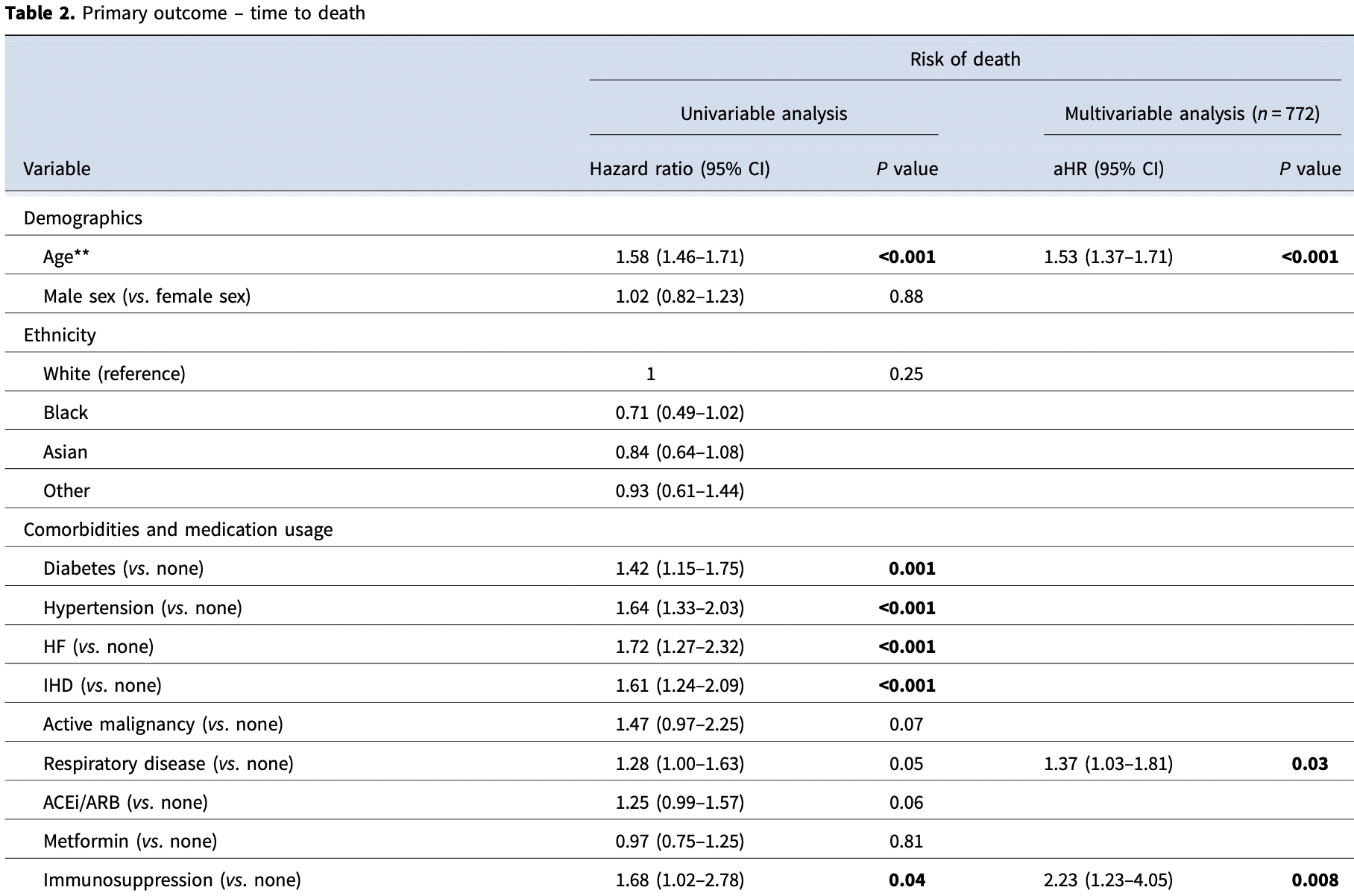
COVID-19 has caused a major global pandemic and necessitated unprecedented public health restrictions in almost every country. Understanding risk factors for severe disease in hospitalised patients is critical as the pandemic progresses. This observational cohort study aimed to characterise the independent associations between the clinical outcomes of hospitalised patients and their demographics, comorbidities, blood tests and bedside observations. All patients admitted to Northwick Park Hospital, London, UK between 12 March and 15 April 2020 with COVID-19 were retrospectively identified. The primary outcome was death. Associations were explored using Cox proportional hazards modelling. The study included 981 patients. The mortality rate was 36.0%. Age (adjusted hazard ratio (aHR) 1.53), respiratory disease (aHR 1.37), immunosuppression (aHR 2.23), respiratory rate (aHR 1.28), hypoxia (aHR 1.36), Glasgow Coma Scale <15 (aHR 1.92), urea (aHR 2.67), alkaline phosphatase (aHR 2.53), C-reactive protein (aHR 1.15), lactate (aHR 2.67), platelet count (aHR 0.77) and infiltrates on chest radiograph (aHR 1.89) were all associated with mortality. These important data will aid clinical risk stratification and provide direction for further research.
Author contributions. NV, DLC and TANR designed the study. MA, JWG and TANR collected the data with assistance from those acknowledged below. PB and JWG conducted the data analysis. JWG wrote the first draft of the article and conducted the literature search. TANR, MA, PB, AMW, DLC and NV all reviewed and approved the final report. Conflict of interest. All authors declare no conflict of interest.
References
Bhargava, Predictors for severe COVID-19 infection, Clinical Infectious Diseases, doi:10.1093/cid/ciaa674
Borghesi, Chest X-ray severity index as a predictor of in-hospital mortality in coronavirus disease 2019: a study of 302 patients from Italy, International Journal of Infectious Diseases
Cao, Clinical features and short-term outcomes of 102 patients with coronavirus disease 2019 in Wuhan, China, Clinical Infectious Diseases, doi:10.1093/cid/ciaa243
Chen, Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study, BMJ
Chen, Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China, Chest
Cummings, Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study, Lancet
Docherty, Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study, The BMJ
Du, Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study, European Respiratory Journal
Garrido, Liberal, Macedo, Review article: COVID-19 and liver disease-what we know on 1st May 2020, Alimentary Pharmacology & Therapeutics, doi:10.1111/apt.15813
Giacomelli, 30-day mortality in patients hospitalized with COVID-19 during the first wave of the Italian epidemic: a prospective cohort study, Pharmacological Research
Gold, Characteristics and clinical outcomes of adult patients hospitalized with COVID-19 -Georgia, MMWR. Morbidity and Mortality Weekly Report
Huang, Pranata, Lymphopenia in severe coronavirus disease-2019 (COVID-19): systematic review and meta-analysis, Journal of Intensive Care
Hwang, Serum alkaline phosphatase levels predict infection-related mortality and hospitalization in peritoneal dialysis patients. Aguilera AI, PLoS ONE
Li, Clinical characteristics of 25 death cases with COVID-19: a retrospective review of medical records in a single medical center, Wuhan, China, International Journal of Infectious Diseases
Li, Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors and outcomes, Journal of Medical Virology, doi:10.1002/jmv.26424
Liang, Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19, JAMA Internal Medicine
Luo, Prognostic value of C-reactive protein in patients with COVID-19, Clinical Infectious Diseases, doi:10.1093/cid/ciaa641
Parohan, Risk factors for mortality in patients with coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies, The Aging Male, doi:10.1080/13685538.2020.1774748
Petrilli, Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York city: prospective cohort study, BMJ
Qiu, Clinical characteristics, laboratory outcome characteristics, comorbidities, and complications of related COVID-19 deceased: a systematic review and meta-analysis, Aging Clinical and Experimental Research, doi:10.1007/s40520-020-01664-3
Sanchez-Ramirez, Mackey, Underlying respiratory diseases, specifically COPD, and smoking are associated with severe COVID-19 outcomes: a systematic review and meta-analysis, Respiratory Medicine
Toussie, Clinical and chest radiography features determine patient outcomes in young and middle age adults with COVID-19, Radiology, doi:10.1148/radiol.2020201754
Vaid, Clinical characteristics and outcomes of immunosuppressed patients hospitalized with COVID-19: experience from London, Journal of Internal Medicine, doi:10.1111/joim.13172
Wang, C-reactive protein levels in the early stage of COVID-19, Médecine et Maladies Infectieuses
Williamson, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Zhang, Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China, Journal of Clinical Virology
Zhang, Liver impairment in COVID-19 patients: a retrospective analysis of 115 cases from a single centre in Wuhan city, China, Liver International
Zhang, Predictive factors for disease progression in hospitalized patients with coronavirus disease 2019 in Wuhan, China, Journal of Clinical Virology
Zhou, Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: a systematic review and meta-analysis, International Journal of Infectious Diseases
DOI record:
{
"DOI": "10.1017/s0950268820002472",
"ISSN": [
"0950-2688",
"1469-4409"
],
"URL": "http://dx.doi.org/10.1017/s0950268820002472",
"abstract": "<jats:title>Abstract</jats:title>\n\t <jats:p>COVID-19 has caused a major global pandemic and necessitated unprecedented public health restrictions in almost every country. Understanding risk factors for severe disease in hospitalised patients is critical as the pandemic progresses. This observational cohort study aimed to characterise the independent associations between the clinical outcomes of hospitalised patients and their demographics, comorbidities, blood tests and bedside observations. All patients admitted to Northwick Park Hospital, London, UK between 12 March and 15 April 2020 with COVID-19 were retrospectively identified. The primary outcome was death. Associations were explored using Cox proportional hazards modelling. The study included 981 patients. The mortality rate was 36.0%. Age (adjusted hazard ratio (aHR) 1.53), respiratory disease (aHR 1.37), immunosuppression (aHR 2.23), respiratory rate (aHR 1.28), hypoxia (aHR 1.36), Glasgow Coma Scale <15 (aHR 1.92), urea (aHR 2.67), alkaline phosphatase (aHR 2.53), C-reactive protein (aHR 1.15), lactate (aHR 2.67), platelet count (aHR 0.77) and infiltrates on chest radiograph (aHR 1.89) were all associated with mortality. These important data will aid clinical risk stratification and provide direction for further research.</jats:p>",
"alternative-id": [
"S0950268820002472"
],
"article-number": "e251",
"assertion": [
{
"group": {
"label": "Copyright and Licensing",
"name": "copyright_and_licensing"
},
"label": "Copyright",
"name": "copyright",
"value": "Copyright © The Author(s), 2020. Published by Cambridge University Press"
},
{
"group": {
"label": "Copyright and Licensing",
"name": "copyright_and_licensing"
},
"label": "License",
"name": "license",
"value": "This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-0997-5528",
"affiliation": [],
"authenticated-orcid": false,
"family": "Goodall",
"given": "J. W.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Reed",
"given": "T. A. N.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ardissino",
"given": "M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bassett",
"given": "P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Whittington",
"given": "A. M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cohen",
"given": "D. L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vaid",
"given": "N.",
"sequence": "additional"
}
],
"container-title": [
"Epidemiology and Infection"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"cambridge.org"
]
},
"created": {
"date-parts": [
[
2020,
10,
13
]
],
"date-time": "2020-10-13T04:51:01Z",
"timestamp": 1602564661000
},
"deposited": {
"date-parts": [
[
2020,
10,
26
]
],
"date-time": "2020-10-26T03:32:51Z",
"timestamp": 1603683171000
},
"indexed": {
"date-parts": [
[
2021,
12,
31
]
],
"date-time": "2021-12-31T21:27:58Z",
"timestamp": 1640986078525
},
"is-referenced-by-count": 11,
"issn-type": [
{
"type": "print",
"value": "0950-2688"
},
{
"type": "electronic",
"value": "1469-4409"
}
],
"issued": {
"date-parts": [
[
2020
]
]
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 286,
"start": {
"date-parts": [
[
2020,
10,
13
]
],
"date-time": "2020-10-13T00:00:00Z",
"timestamp": 1602547200000
}
}
],
"link": [
{
"URL": "https://www.cambridge.org/core/services/aop-cambridge-core/content/view/S0950268820002472",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "56",
"original-title": [],
"prefix": "10.1017",
"published": {
"date-parts": [
[
2020
]
]
},
"published-online": {
"date-parts": [
[
2020,
10,
13
]
]
},
"published-print": {
"date-parts": [
[
2020
]
]
},
"publisher": "Cambridge University Press (CUP)",
"reference": [
{
"DOI": "10.1016/j.ijid.2020.05.021",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref28"
},
{
"DOI": "10.1016/j.jcv.2020.104364",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref2"
},
{
"DOI": "10.1016/j.jcv.2020.104392",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref3"
},
{
"article-title": "Prognostic value of C-reactive protein in patients with COVID-19",
"author": "Luo",
"journal-title": "Clinical Infectious Diseases",
"key": "S0950268820002472_ref18",
"year": "2020"
},
{
"key": "S0950268820002472_ref24",
"unstructured": "24. Public Health England (2020) Beyond the data: Understanding the impact of COVID-19 on BAME groups About Public Health England; Published online: 2020."
},
{
"DOI": "10.15585/mmwr.mm6918e1",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref22"
},
{
"DOI": "10.1136/bmj.m1091",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref31"
},
{
"DOI": "10.1080/13685538.2020.1774748",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref5"
},
{
"DOI": "10.1016/j.medmal.2020.03.007",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref17"
},
{
"DOI": "10.1016/j.ijid.2020.03.053",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref33"
},
{
"key": "S0950268820002472_ref15",
"unstructured": "15. The London Data Store (Great London Authority) (2020) London Area Profiles. https://data.london.gov.uk/london-area-profiles/ (Accessed 21 June 2020)."
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref13"
},
{
"DOI": "10.1148/radiol.2020201754",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref27"
},
{
"DOI": "10.1183/13993003.00524-2020",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref4"
},
{
"DOI": "10.1111/apt.15813",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref29"
},
{
"article-title": "Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO clinical characterisation protocol: prospective observational cohort study",
"author": "Docherty",
"first-page": "1",
"journal-title": "The BMJ",
"key": "S0950268820002472_ref14",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1016/j.rmed.2020.106096",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref20"
},
{
"DOI": "10.1016/j.chest.2020.04.010",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref6"
},
{
"article-title": "Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors and outcomes",
"author": "Li",
"journal-title": "Journal of Medical Virology",
"key": "S0950268820002472_ref10",
"year": "2020"
},
{
"DOI": "10.1111/liv.14455",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref30"
},
{
"DOI": "10.1093/cid/ciaa674",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref9"
},
{
"DOI": "10.1136/bmj.m1966",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref8"
},
{
"DOI": "10.1007/s40520-020-01664-3",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref11"
},
{
"DOI": "10.1186/s40560-020-00453-4",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref12"
},
{
"DOI": "10.1016/S0140-6736(20)31189-2",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref25"
},
{
"DOI": "10.1111/joim.13172",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref21"
},
{
"DOI": "10.1093/cid/ciaa243",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref1"
},
{
"key": "S0950268820002472_ref16",
"unstructured": "16. Public Health England (PHE) (2020) Guidance COVID-19: investigation and initial clinical management of possible cases (Updated 12 March 2020)."
},
{
"DOI": "10.1016/j.phrs.2020.104931",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref7"
},
{
"DOI": "10.1016/j.ijid.2020.07.029",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref19"
},
{
"DOI": "10.1001/jamainternmed.2020.2033",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref26"
},
{
"DOI": "10.1371/journal.pone.0157361",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref32"
},
{
"DOI": "10.1056/NEJMsa2011686",
"doi-asserted-by": "publisher",
"key": "S0950268820002472_ref23"
}
],
"reference-count": 33,
"references-count": 33,
"relation": {
"has-preprint": [
{
"asserted-by": "object",
"id": "10.1101/2020.09.24.20200337",
"id-type": "doi"
}
]
},
"score": 1,
"short-container-title": [
"Epidemiol. Infect."
],
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Epidemiology"
],
"subtitle": [],
"title": [
"Risk factors for severe disease in patients admitted with COVID-19 to a hospital in London, England: a retrospective cohort study"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1017/policypage",
"volume": "148"
}
