The Clinical Characteristics and Outcomes of Patients with Moderate-to-Severe Coronavirus Disease 2019 Infection and Diabetes in Daegu, South Korea
et al., Diabetes & Metabolism Journal, doi:10.4093/dmj.2020.0146, Aug 2020
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
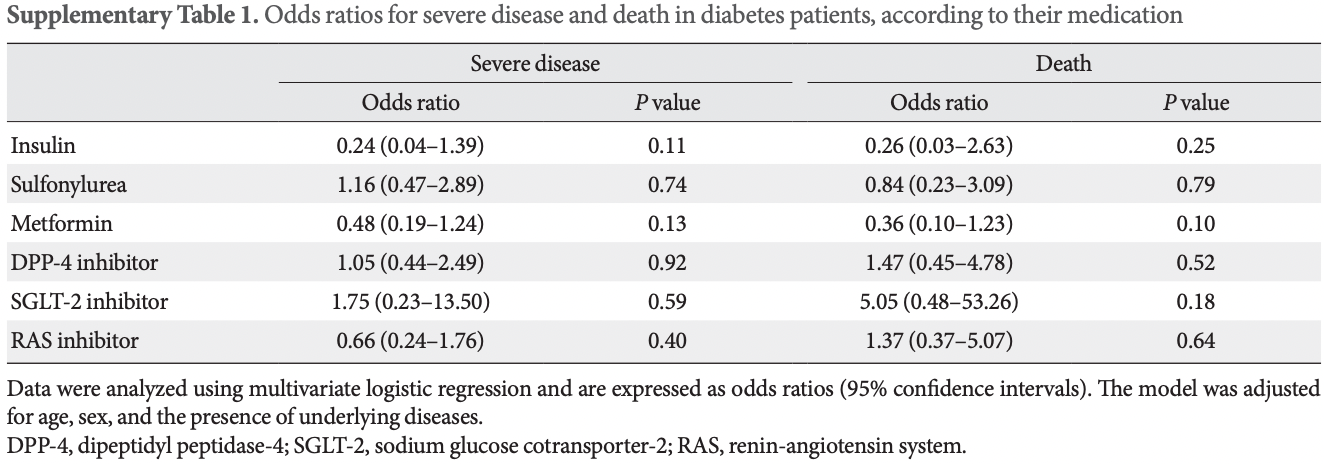
Retrospective 235 hospitalized diabetes patients in South Korea, showing lower mortality and lower progression to severe disease with metformin.
|
risk of death, 64.0% lower, OR 0.36, p = 0.10, treatment 113, control 122, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of progression, 52.0% lower, OR 0.48, p = 0.13, treatment 113, control 122, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Kim et al., 12 Aug 2020, retrospective, South Korea, peer-reviewed, 32 authors.
The Clinical Characteristics and Outcomes of Patients with Moderate-to-Severe Coronavirus Disease 2019 Infection and Diabetes in Daegu, South Korea
Diabetes & Metabolism Journal, doi:10.4093/dmj.2020.0146
Background: Coronavirus disease 2019 (COVID-19) is a global pandemic that had affected more than eight million people worldwide by June 2020. Given the importance of the presence of diabetes mellitus (DM) for host immunity, we retrospectively evaluated the clinical characteristics and outcomes of moderate-to-severe COVID-19 in patients with diabetes. Methods: We conducted a multi-center observational study of 1,082 adult inpatients (aged ≥18 years) who were admitted to one of five university hospitals in Daegu because of the severity of their COVID-19-related disease. The demographic, laboratory, and radiologic findings, and the mortality, prevalence of severe disease, and duration of quarantine were compared between patients with and without DM. In addition, 1:1 propensity score (PS)-matching was conducted with the DM group. Results: Compared with the non-DM group (n=847), patients with DM (n=235) were older, exhibited higher mortality, and required more intensive care. Even after PS-matching, patients with DM exhibited more severe disease, and DM remained a prognostic factor for higher mortality (hazard ratio, 2.40; 95% confidence interval, 1.38 to 4.15). Subgroup analysis revealed that the presence of DM was associated with higher mortality, especially in older people (≥70 years old). Prior use of a dipeptidyl peptidase-4 inhibitor or a renin-angiotensin system inhibitor did not affect mortality or the clinical severity of the disease. Conclusion: DM is a significant risk factor for COVID-19 severity and mortality. Our findings imply that COVID-19 patients with DM, especially if elderly, require special attention and prompt intensive care.
SUPPLEMENTARY MATERIALS Supplementary materials related to this article can be found online at https://doi.org/10.4093/dmj.2020.0146.
CONFLICTS OF INTEREST No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
References
Bassendine, Bridge, Mccaughan, Gorrell, COVID-19 and comorbidities: a role for dipeptidyl peptidase 4 (DPP4) in disease severity?, J Diabetes
Bornstein, Rubino, Khunti, Mingrone, Hopkins et al., Practical recommendations for the management of diabetes in patients with COVID-19, Lancet Diabetes Endocrinol
Brufsky, Hyperglycemia, hydroxychloroquine, and the CO-VID-19 pandemic, J Med Virol
Cariou, Hadjadj, Wargny, Pichelin, Al-Salameh et al., Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia
Chatterjee, SGLT-2 inhibitors for COVID-19: a miracle waiting to happen or just another beat around the bush?, Prim Care Diabetes, doi:10.1016/j.pcd.2020.05.013
Chung, Lee, Ha, Yoon, Won et al., The risk of diabetes on clinical outcomes in patients with coronavirus disease 2019: a retrospective cohort study, Diabetes Metab J
Cristelo, Azevedo, Marques, Nunes, Sarmento, SARS-CoV-2 and diabetes: new challenges for the disease, Diabetes Res Clin Pract
Docherty, Harrison, Green, Hardwick, Pius et al., Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study, Dun-Diabetes Metab J
Fadini, Morieri, Longato, Bonora, Pinelli et al., Exposure to dipeptidyl-peptidase-4 inhibitors and COVID-19 among people with type 2 diabetes: a case-control study, Diabetes Obes Metab, doi:10.1111/dom.14097
Guan, Liang, Zhao, Liang, Chen et al., China Medical Treatment Expert Group for COVID-19. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis, Eur Respir J
Guan, Ni, Hu, Liang, Ou et al., None
Guo, Li, Dong, Zhou, Zhang et al., Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabe, tes Metab Res Rev, doi:10.1002/dmrr.3319
Hoffmann, Kleine-Weber, Pohlmann, A multibasic cleavage site in the spike protein of SARS-CoV-2 is essential for infection of human lung cells, Mol Cell
Jafar, Edriss, Nugent, The effect of short-term hyperglycemia on the innate immune system, Am J Med Sci
Katulanda, Dissanayake, Ranathunga, Ratnasamy, Wijewickrama et al., Prevention and management of COVID-19 among patients with diabetes: an appraisal of the literature, Diabetologia
Kim, Ko, Kim, Kang, Noh et al., Committee of Clinical Practice Guidelines, Korean Diabetes Association. 2019 Clinical practice guidelines for type 2 diabetes mellitus in Korea, Diabetes Metab J
Kim, Lee, Kim, Lee, Kim et al., A brief telephone severity scoring system and therapeutic living centers solved acute hospital-bed shortage during the COVID-19 outbreak in Daegu, Korea, J Korean Med Sci
Kumar, Arora, Sharma, Anikhindi, Bansal et al., Is diabetes mellitus associated with mortality and severity of COVID-19?: a meta-analysis, Diabetes Metab Syndr
Luo, Qiu, Liu, Liu, Zheng et al., Metformin treatment was associated with decreased mor-Diabetes Metab J, Am J Trop Med Hyg
Memish, Perlman, Van Kerkhove, Zumla, Middle East respiratory syndrome, Lancet
Pal, Bhadada, Should anti-diabetic medications be reconsidered amid COVID-19 pandemic?, Diabetes Res Clin Pract
Raj, Mou, Smits, Dekkers, Muller et al., Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC, Nature
Turina, Fry, Polk, Acute hyperglycemia and the innate immune system: clinical, cellular, and molecular aspects, Crit Care Med
Ursini, Ciaffi, Landini, Meliconi, COVID-19 and diabetes: is metformin a friend or foe?, Diabetes Res Clin Pract
Zhu, She, Cheng, Qin, Zhang et al., Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab
DOI record:
{
"DOI": "10.4093/dmj.2020.0146",
"ISSN": [
"2233-6079",
"2233-6087"
],
"URL": "http://dx.doi.org/10.4093/dmj.2020.0146",
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"value": "2020-06-26"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"value": "2020-07-02"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published online",
"name": "published_online",
"value": "2020-08-12"
},
{
"group": {
"label": "Copyright and Licensing",
"name": "Copyright_and_licensing"
},
"label": "Copyright",
"name": "copyright",
"value": "Copyright © 2020 Korean Diabetes Association"
},
{
"explanation": {
"URL": "http://creativecommons.org/licenses/by-nc/4.0/"
},
"group": {
"label": "Copyright and Licensing",
"name": "Copyright_and_licensing"
},
"label": "License",
"name": "license",
"value": "This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5750-3598",
"affiliation": [
{
"name": "Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea."
}
],
"authenticated-orcid": false,
"family": "Kim",
"given": "Mi Kyung",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-9217-968X",
"affiliation": [
{
"name": "Department of Internal Medicine, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea."
}
],
"authenticated-orcid": false,
"family": "Jeon",
"given": "Jae-Han",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Daegu Catholic University Hospital, Daegu Catholic University School of Medicine, Daegu, Korea."
}
],
"family": "Kim",
"given": "Sung-Woo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Yeungnam University Hospital, Yeungnam University College of Medicine, Daegu, Korea."
}
],
"family": "Moon",
"given": "Jun Sung",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea."
}
],
"family": "Cho",
"given": "Nan Hee",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea."
}
],
"family": "Han",
"given": "Eugene",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea."
}
],
"family": "You",
"given": "Ji Hong",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea."
}
],
"family": "Lee",
"given": "Ji Yeon",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea."
}
],
"family": "Hyun",
"given": "Miri",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea."
}
],
"family": "Park",
"given": "Jae Seok",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea."
}
],
"family": "Kwon",
"given": "Yong Shik",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea."
}
],
"family": "Choi",
"given": "Yeon-Kyung",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea."
}
],
"family": "Kwon",
"given": "Ki Tae",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea."
}
],
"family": "Lee",
"given": "Shin Yup",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Daegu Catholic University Hospital, Daegu Catholic University School of Medicine, Daegu, Korea."
}
],
"family": "Jeon",
"given": "Eon Ju",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Daegu Catholic University Hospital, Daegu Catholic University School of Medicine, Daegu, Korea."
}
],
"family": "Kim",
"given": "Jin-Woo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Daegu Catholic University Hospital, Daegu Catholic University School of Medicine, Daegu, Korea."
}
],
"family": "Hong",
"given": "Hyo-Lim",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Daegu Catholic University Hospital, Daegu Catholic University School of Medicine, Daegu, Korea."
}
],
"family": "Kwon",
"given": "Hyun Hee",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Daegu Catholic University Hospital, Daegu Catholic University School of Medicine, Daegu, Korea."
}
],
"family": "Jung",
"given": "Chi Young",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Yeungnam University Hospital, Yeungnam University College of Medicine, Daegu, Korea."
}
],
"family": "Lee",
"given": "Yin Young",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Yeungnam University Hospital, Yeungnam University College of Medicine, Daegu, Korea."
}
],
"family": "Ha",
"given": "Eunyeoung",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Yeungnam University Hospital, Yeungnam University College of Medicine, Daegu, Korea."
}
],
"family": "Chung",
"given": "Seung Min",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Yeungnam University Hospital, Yeungnam University College of Medicine, Daegu, Korea."
}
],
"family": "Hur",
"given": "Jian",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Yeungnam University Hospital, Yeungnam University College of Medicine, Daegu, Korea."
}
],
"family": "Ahn",
"given": "June Hong",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea."
}
],
"family": "Kim",
"given": "Na-young",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea."
}
],
"family": "Kim",
"given": "Shin-Woo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea."
}
],
"family": "Chang",
"given": "Hyun Ha",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea."
}
],
"family": "Lee",
"given": "Yong Hoon",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea."
}
],
"family": "Lee",
"given": "Jaehee",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea."
}
],
"family": "Park",
"given": "Keun-Gyu",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9125-7156",
"affiliation": [
{
"name": "Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea."
}
],
"authenticated-orcid": false,
"family": "Kim",
"given": "Hyun Ah",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5671-0875",
"affiliation": [
{
"name": "Department of Internal Medicine, Daegu Catholic University Hospital, Daegu Catholic University School of Medicine, Daegu, Korea."
}
],
"authenticated-orcid": false,
"family": "Lee",
"given": "Ji-Hyun",
"sequence": "additional"
}
],
"container-title": [
"Diabetes & Metabolism Journal"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"e-dmj.org"
]
},
"created": {
"date-parts": [
[
2020,
8,
12
]
],
"date-time": "2020-08-12T07:23:37Z",
"timestamp": 1597217017000
},
"deposited": {
"date-parts": [
[
2020,
10,
21
]
],
"date-time": "2020-10-21T09:52:13Z",
"timestamp": 1603273933000
},
"funder": [
{
"name": "Daegu Medical Association COVID-19 Scientific Committee"
}
],
"indexed": {
"date-parts": [
[
2022,
2,
15
]
],
"date-time": "2022-02-15T13:07:38Z",
"timestamp": 1644930458165
},
"is-referenced-by-count": 54,
"issn-type": [
{
"type": "print",
"value": "2233-6079"
},
{
"type": "electronic",
"value": "2233-6087"
}
],
"issue": "4",
"issued": {
"date-parts": [
[
2020
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2020
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
1,
1
]
],
"date-time": "2020-01-01T00:00:00Z",
"timestamp": 1577836800000
}
}
],
"link": [
{
"URL": "https://e-dmj.org/pdf/10.4093/dmj.2020.0146",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://e-dmj.org/DOIx.php?id=10.4093/dmj.2020.0146",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://e-dmj.org/DOIx.php?id=10.4093/dmj.2020.0146",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "2567",
"original-title": [],
"page": "602",
"prefix": "10.4093",
"published": {
"date-parts": [
[
2020
]
]
},
"published-print": {
"date-parts": [
[
2020
]
]
},
"publisher": "Korean Diabetes Association",
"reference": [
{
"DOI": "10.24171/j.phrp.2020.11.2.04",
"author": "COVID-19 National Emergency Response Center",
"doi-asserted-by": "crossref",
"first-page": "81",
"journal-title": "Osong Public Health Res Perspect",
"key": "10.4093/dmj.2020.0146_ref1",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.24171/j.phrp.2020.11.2.05",
"author": "COVID-19 National Emergency Response Center",
"doi-asserted-by": "crossref",
"first-page": "85",
"journal-title": "Osong Public Health Res Perspect",
"key": "10.4093/dmj.2020.0146_ref2",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3346/jkms.2020.35.e152",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "e152",
"journal-title": "J Korean Med Sci",
"key": "10.4093/dmj.2020.0146_ref3",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1016/j.amjms.2015.11.011",
"author": "Jafar",
"doi-asserted-by": "crossref",
"first-page": "201",
"journal-title": "Am J Med Sci",
"key": "10.4093/dmj.2020.0146_ref4",
"volume": "351",
"year": "2016"
},
{
"DOI": "10.1097/01.CCM.0000170106.61978.D8",
"author": "Turina",
"doi-asserted-by": "crossref",
"first-page": "1624",
"journal-title": "Crit Care Med",
"key": "10.4093/dmj.2020.0146_ref5",
"volume": "33",
"year": "2005"
},
{
"DOI": "10.1016/j.diabres.2020.108228",
"author": "Cristelo",
"doi-asserted-by": "crossref",
"first-page": "108228",
"journal-title": "Diabetes Res Clin Pract",
"key": "10.4093/dmj.2020.0146_ref6",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(19)33221-0",
"author": "Memish",
"doi-asserted-by": "crossref",
"first-page": "1063",
"journal-title": "Lancet",
"key": "10.4093/dmj.2020.0146_ref7",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1183/13993003.00547-2020",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "2000547",
"journal-title": "Eur Respir J",
"key": "10.4093/dmj.2020.0146_ref8",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.044",
"author": "Kumar",
"doi-asserted-by": "crossref",
"first-page": "535",
"journal-title": "Diabetes Metab Syndr",
"key": "10.4093/dmj.2020.0146_ref9",
"volume": "14",
"year": "2020"
},
{
"author": "Guo",
"journal-title": "Diabetes Metab Res Rev",
"key": "10.4093/dmj.2020.0146_ref10",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1985",
"author": "Docherty",
"doi-asserted-by": "crossref",
"first-page": "m1985",
"journal-title": "BMJ",
"key": "10.4093/dmj.2020.0146_ref11",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.4093/dmj.2019.0137",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "398",
"journal-title": "Diabetes Metab J",
"key": "10.4093/dmj.2020.0146_ref12",
"volume": "43",
"year": "2019"
},
{
"key": "10.4093/dmj.2020.0146_ref13",
"unstructured": "Ministry of Health and Welfare. Central Disaster Management Headquarters. cited 2020 Jul 8. Available from: http://ncov.mohw.go.kr"
},
{
"DOI": "10.1016/j.molcel.2020.04.022",
"author": "Hoffmann",
"doi-asserted-by": "crossref",
"first-page": "779",
"journal-title": "Mol Cell",
"key": "10.4093/dmj.2020.0146_ref14",
"volume": "78",
"year": "2020"
},
{
"DOI": "10.1038/nature12005",
"author": "Raj",
"doi-asserted-by": "crossref",
"first-page": "251",
"journal-title": "Nature",
"key": "10.4093/dmj.2020.0146_ref15",
"volume": "495",
"year": "2013"
},
{
"DOI": "10.1016/S2213-8587(20)30152-2",
"author": "Bornstein",
"doi-asserted-by": "crossref",
"first-page": "546",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.4093/dmj.2020.0146_ref16",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2002032",
"author": "Guan",
"doi-asserted-by": "crossref",
"first-page": "1708",
"journal-title": "N Engl J Med",
"key": "10.4093/dmj.2020.0146_ref17",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "1068",
"journal-title": "Cell Metab",
"key": "10.4093/dmj.2020.0146_ref18",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.3346/jkms.2020.35.e112",
"author": "Korean Society of Infectious Diseases",
"doi-asserted-by": "crossref",
"first-page": "e112",
"journal-title": "J Korean Med Sci",
"key": "10.4093/dmj.2020.0146_ref19",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05164-x",
"author": "Katulanda",
"doi-asserted-by": "crossref",
"first-page": "1440",
"journal-title": "Diabetologia",
"key": "10.4093/dmj.2020.0146_ref20",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.4093/dmj.2020.0105",
"author": "Chung",
"doi-asserted-by": "crossref",
"first-page": "405",
"journal-title": "Diabetes Metab J",
"key": "10.4093/dmj.2020.0146_ref21",
"volume": "44",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"author": "Cariou",
"doi-asserted-by": "crossref",
"first-page": "1500",
"journal-title": "Diabetologia",
"key": "10.4093/dmj.2020.0146_ref22",
"volume": "63",
"year": "2020"
},
{
"author": "Fadini",
"journal-title": "Diabetes Obes Metab",
"key": "10.4093/dmj.2020.0146_ref23",
"year": "2020"
},
{
"DOI": "10.1111/1753-0407.13052",
"author": "Bassendine",
"doi-asserted-by": "crossref",
"first-page": "649",
"journal-title": "J Diabetes",
"key": "10.4093/dmj.2020.0146_ref24",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1002/jmv.25887",
"author": "Brufsky",
"doi-asserted-by": "crossref",
"first-page": "770",
"journal-title": "J Med Virol",
"key": "10.4093/dmj.2020.0146_ref25",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108167",
"author": "Ursini",
"doi-asserted-by": "crossref",
"first-page": "108167",
"journal-title": "Diabetes Res Clin Pract",
"key": "10.4093/dmj.2020.0146_ref26",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "69",
"journal-title": "Am J Trop Med Hyg",
"key": "10.4093/dmj.2020.0146_ref27",
"volume": "103",
"year": "2020"
},
{
"author": "Chatterjee",
"journal-title": "Prim Care Diabetes",
"key": "10.4093/dmj.2020.0146_ref28",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108146",
"author": "Pal",
"doi-asserted-by": "crossref",
"first-page": "108146",
"journal-title": "Diabetes Res Clin Pract",
"key": "10.4093/dmj.2020.0146_ref29",
"volume": "163",
"year": "2020"
}
],
"reference-count": 29,
"references-count": 29,
"relation": {},
"score": 1,
"short-container-title": [
"Diabetes Metab J"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": [
"The Clinical Characteristics and Outcomes of Patients with Moderate-to-Severe Coronavirus Disease 2019 Infection and Diabetes in Daegu, South Korea"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.4093/crossmark_policy",
"volume": "44"
}
