Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study
et al., Diabetologia, doi:10.1007/s00125-020-05351-w, CORONADO, NCT04324736, Feb 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 2,796 hospitalized diabetes patients with COVID-19 in France, showing lower mortality with metformin use.
|
risk of death, 28.3% lower, RR 0.72, p = 0.03, treatment 247 of 1,553 (15.9%), control 330 of 1,241 (26.6%), NNT 9.4, adjusted per study, odds ratio converted to relative risk, multivariable, day 28.
|
|
risk of no hospital discharge, 14.8% lower, RR 0.85, p = 0.02, treatment 690 of 1,553 (44.4%), control 702 of 1,241 (56.6%), NNT 8.2, adjusted per study, inverted to make RR<1 favor treatment, odds ratio converted to relative risk, multivariable, day 28.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Wargny et al., 17 Feb 2021, retrospective, France, peer-reviewed, 43 authors, study period 10 March, 2020 - 10 April, 2020, trial NCT04324736 (history) (CORONADO).
Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study
Diabetologia, doi:10.1007/s00125-020-05351-w
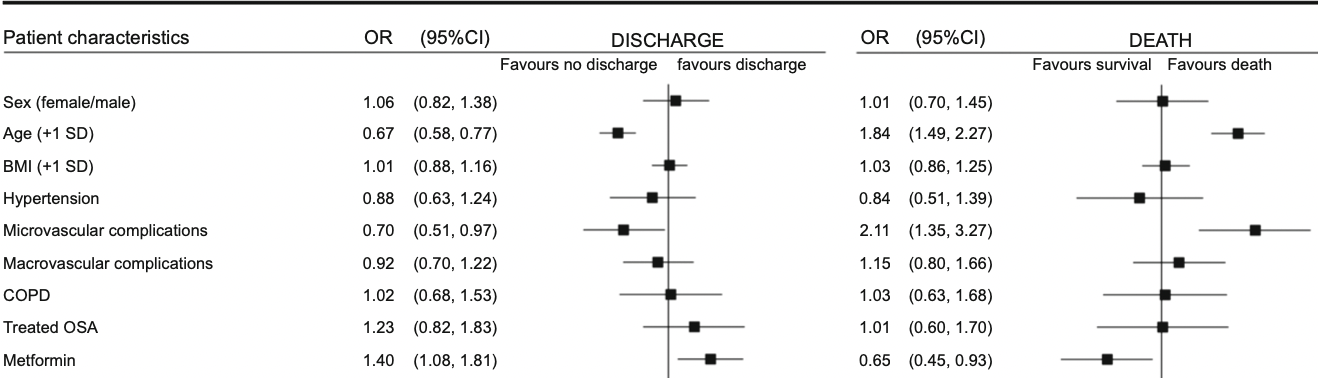
Aims/hypothesis This is an update of the results from the previous report of the CORONADO (Coronavirus SARS-CoV-2 and Diabetes Outcomes) study, which aims to describe the outcomes and prognostic factors in patients with diabetes hospitalised for coronavirus disease-2019 (COVID-19). Methods The CORONADO initiative is a French nationwide multicentre study of patients with diabetes hospitalised for COVID-19 with a 28-day follow-up. The patients were screened after hospital admission from 10 March to 10 April 2020. We mainly focused on hospital discharge and death within 28 days. Results We included 2796 participants: 63.7% men, mean age 69.7 ± 13.2 years, median BMI (25th-75th percentile) 28.4 (25.0-32.4) kg/m 2 . Microvascular and macrovascular diabetic complications were found in 44.2% and 38.6% of participants, respectively. Within 28 days, 1404 (50.2%; 95% CI 48.3%, 52.1%) were discharged from hospital with a median duration of hospital stay of 9 (5-14) days, while 577 participants died (20.6%; 95% CI 19.2%, 22.2%). In multivariable models, younger age, routine metformin therapy and longer symptom duration on admission were positively associated with discharge. History of microvascular complications, anticoagulant routine therapy, dyspnoea on admission, and higher aspartate aminotransferase, white cell count and C-reactive protein levels were associated with a reduced chance of discharge. Factors associated with death within 28 days mirrored those associated with discharge, and also included routine treatment by insulin and statin as deleterious factors. Conclusions/interpretation In patients with diabetes hospitalised for COVID-19, we established prognostic factors for hospital discharge and death that could help clinicians in this pandemic period. Trial registration Clinicaltrials.gov identifier: NCT04324736
Supplementary Information The online version contains peer-reviewed but unedited supplementary material available at https://doi.org/10.1007/ s00125-020-05351-w. Authors' relationships and activities BC reports grants and personal fees from Amgen, AstraZeneca, Akcea, Genfit, Gilead, Eli Lilly, Novo Nordisk, and MSD, and grants and personal fees from Sanofi and Regeneron. PD reports personal fees from Novo Nordisk, Sanofi, Eli Lilly, MSD, Novartis, Abbott, AstraZeneca, Boehringer Ingelheim and Mundipharma. J-FG reports personal fees and non-financial support from Eli Lilly, Novo Nordisk and AstraZeneca, personal fees from Bristol-Myers Squibb, Gilead and Bayer; all disclosures above unrelated to this presentation. PG reports personal fees from Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, MSD, Mundipharma, Sanofi and Servier, and grants and personal fees from Novo Nordisk. SH reports personal fees and nonfinancial support from AstraZeneca, grants and personal fees from Bayer, personal fees from Boehringer Ingelheim, grants from Dinno Santé, personal fees from Eli Lilly, non-financial support from LVL, personal fees and non-financial support from MSD, personal fees from Novartis, grants from Pierre Fabre Santé, personal fees and non-financial support from Sanofi, personal fees and non-financial support from Servier, and personal fees from Valbiotis. MP reports personal fees and non-financial support from Novo Nordisk, and non-financial support from Sanofi and..
References
Agarwal, Schechter, Southern, Crandall, Tomer, Preadmission diabetes-specific risk factors for mortality in hospitalized patients with diabetes and coronavirus disease 2019, Diabetes Care, doi:10.2337/dc20-1543
Alqahtani, Aleanizy, Hadi Mohamed, Prevalence of comorbidities in cases of Middle East respiratory syndrome coronavirus: a retrospective study, Epidemiol Infect, doi:10.1017/S0950268818002923
Argenziano, Bruce, Slater, Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series, BMJ, doi:10.1136/bmj.m1996
Ben Zadok, Kornowski, Goldenberg, Admission blood glucose and 10-year mortality among patients with or without pre-existing diabetes mellitus hospitalized with heart failure, Cardiovasc Diabetol, doi:10.1186/s12933-017-0582-y
Bhatraju, Ghassemieh, Nichols, Covid-19 in critically ill patients in the Seattle region -case series, N Engl J Med, doi:10.1056/NEJMoa2004500
C2vn, 21 Service d'Endocrinologie, Diabétologie et Maladies Métaboliques, Centre Hospitalier d'Aix-en-Provence, Aix-en-Provence, France 22 Service Endocrinologie-Diabétologie
Capes, Hunt, Malmberg, Gerstein, Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview, Lancet, doi:10.1016/S0140-6736(99)08415-9
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Coppelli, Giannarelli, Aragona, Hyperglycemia at hospital admission is associated with severity of the prognosis in patients hospitalized for COVID-19: the Pisa COVID-19 Study, Diabetes Care, doi:10.2337/dc20-1380
Docherty, Harrison, Green, Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study, BMJ, doi:10.1136/bmj.m1985
Gencer, Rigamonti, Nanchen, Prognostic values of fasting hyperglycaemia in non-diabetic patients with acute coronary syndrome: a prospective cohort study, Eur Heart J Acute Cardiovasc Care, doi:10.1177/2048872618777819
Grasselli, Zangrillo, Zanella, Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy, JAMA, doi:10.1001/jama.2020.5394
Holman, Knighton, Kar, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30271-0
Joensen, Madsen, Holm, Diabetes and COVID-19: psychosocial consequences of the COVID-19 pandemic in people with diabetes in Denmark-what characterizes people with high levels of COVID-19-related worries?, Diabet Med, doi:10.1111/dme.14319
Knight, Ho, Pius, Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score, BMJ, doi:10.1136/bmj.m3339
Lepper, Bals, Jüni, Von Eynatten, Blood glucose, diabetes and metabolic control in patients with communityacquired pneumonia, Diabetologia, doi:10.1007/s00125-020-05225-1
Mantovani, Byrne, Zheng, Targher, Diabetes as a risk factor for greater COVID-19 severity and in-hospital death: a meta-analysis of observational studies, Nutr Metab Cardiovasc Dis, doi:10.1016/j.numecd.2020.05.014
Mukhtar, Mukhtar, Letter to the editor: mental health and psychological distress in people with diabetes during COVID-19, Metabolism, doi:10.1016/j.metabol.2020.154248
Onder, Rezza, Brusaferro, Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy, JAMA, doi:10.1001/jama.2020.4683
Pan, Cai, Jing, Stress hyperglycemia and prognosis of minor ischemic stroke and transient ischemic attack: the CHANCE study (clopidogrel in high-risk patients with acute nondisabling cerebrovascular events), Stroke, doi:10.1161/STROKEAHA.117.019081
Roncon, Zuin, Rigatelli, Zuliani, Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome, J Clin Virol, doi:10.1016/j.jcv.2020.104354
Sardu, Onofrio, Balestrieri, Hyperglycaemia on admission to hospital and COVID-19, Diabetologia, doi:10.1007/s00125-020-05216-2
Selvin, Juraschek, Diabetes epidemiology in the COVID-19 pandemic, Diabetes Care, doi:10.2337/dc20-1295
Sy, Munshi, Caring for older adults with diabetes during the COVID-19 pandemic, JAMA Intern Med, doi:10.1001/jamainternmed.2020.2492
Wang, Ma, Zhang, Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: a multi-centre retrospective study, Diabetologia, doi:10.1007/s00125-020-05209-1
Wargny, Pierre, Benhamou, Bonnet, Bordier, Pierre-Antoine Gourraud 2 & Ronan Roussel 3,4 & Bertrand Cariou 1 & Samy Hadjadj 1 & for the CORONADO investigators Institut des Maladies Métaboliques et Cardiovasculaires
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Wu, Chen, Cai, Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China, JAMA Intern Med, doi:10.1001/jamainternmed.2020.0994
Xu, Wang, Wang, The impact of type 2 diabetes and its management on the prognosis of patients with severe COVID-19, J Diabetes, doi:10.1111/1753-0407.13084
Yang, Feng, Yuan, Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS, Diabet Med, doi:10.1111/j.1464-5491.2006.01861.x
Zhang, Liu, Zhang, Dong, Zhang, Admission fasting blood glucose predicts 30-day poor outcome in patients hospitalized for COVID-19 pneumonia, Diabetes Obes Metab, doi:10.1111/dom.14132
Zhang, Qin, Cheng, In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19, Cell Metab, doi:10.1016/j.cmet.2020.06.015
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
Zhu, She, Cheng, Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.04.021
DOI record:
{
"DOI": "10.1007/s00125-020-05351-w",
"ISSN": [
"0012-186X",
"1432-0428"
],
"URL": "http://dx.doi.org/10.1007/s00125-020-05351-w",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Aims/hypothesis</jats:title>\n <jats:p>This is an update of the results from the previous report of the CORONADO (Coronavirus SARS-CoV-2 and Diabetes Outcomes) study, which aims to describe the outcomes and prognostic factors in patients with diabetes hospitalised for coronavirus disease-2019 (COVID-19).</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>The CORONADO initiative is a French nationwide multicentre study of patients with diabetes hospitalised for COVID-19 with a 28-day follow-up. The patients were screened after hospital admission from 10 March to 10 April 2020. We mainly focused on hospital discharge and death within 28 days.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>We included 2796 participants: 63.7% men, mean age 69.7 ± 13.2 years, median BMI (25th–75th percentile) 28.4 (25.0–32.4) kg/m<jats:sup>2</jats:sup>. Microvascular and macrovascular diabetic complications were found in 44.2% and 38.6% of participants, respectively. Within 28 days, 1404 (50.2%; 95% CI 48.3%, 52.1%) were discharged from hospital with a median duration of hospital stay of 9 (5–14) days, while 577 participants died (20.6%; 95% CI 19.2%, 22.2%). In multivariable models, younger age, routine metformin therapy and longer symptom duration on admission were positively associated with discharge. History of microvascular complications, anticoagulant routine therapy, dyspnoea on admission, and higher aspartate aminotransferase, white cell count and C-reactive protein levels were associated with a reduced chance of discharge. Factors associated with death within 28 days mirrored those associated with discharge, and also included routine treatment by insulin and statin as deleterious factors.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusions/interpretation</jats:title>\n <jats:p>In patients with diabetes hospitalised for COVID-19, we established prognostic factors for hospital discharge and death that could help clinicians in this pandemic period.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Trial registration</jats:title>\n <jats:p><jats:ext-link xmlns:xlink=\"http://www.w3.org/1999/xlink\" ext-link-type=\"uri\" xlink:href=\"http://clinicaltrials.gov\">Clinicaltrials.gov</jats:ext-link> identifier: NCT04324736</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Graphical abstract</jats:title>\n \n </jats:sec>",
"alternative-id": [
"5351"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "2 September 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "10 November 2020"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "17 February 2021"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-6027-9486",
"affiliation": [],
"authenticated-orcid": false,
"family": "Wargny",
"given": "Matthieu",
"sequence": "first"
},
{
"affiliation": [],
"name": "for the CORONADO investigators",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-6268-7360",
"affiliation": [],
"authenticated-orcid": false,
"family": "Potier",
"given": "Louis",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5362-3813",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gourdy",
"given": "Pierre",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6822-6132",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pichelin",
"given": "Matthieu",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0581-7592",
"affiliation": [],
"authenticated-orcid": false,
"family": "Amadou",
"given": "Coralie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Benhamou",
"given": "Pierre-Yves",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bonnet",
"given": "Jean-Baptiste",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bordier",
"given": "Lyse",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7348-7161",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bourron",
"given": "Olivier",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chaumeil",
"given": "Claude",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7160-4301",
"affiliation": [],
"authenticated-orcid": false,
"family": "Chevalier",
"given": "Nicolas",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1726-2296",
"affiliation": [],
"authenticated-orcid": false,
"family": "Darmon",
"given": "Patrice",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Delenne",
"given": "Blandine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Demarsy",
"given": "Delphine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dumas",
"given": "Marie",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8731-3242",
"affiliation": [],
"authenticated-orcid": false,
"family": "Dupuy",
"given": "Olivier",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Flaus-Furmaniuk",
"given": "Anna",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6458-2001",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gautier",
"given": "Jean-François",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Guedj",
"given": "Anne-Marie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jeandidier",
"given": "Nathalie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Larger",
"given": "Etienne",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Le Berre",
"given": "Jean-Philippe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lungo",
"given": "Myriam",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Montanier",
"given": "Nathanaëlle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Moulin",
"given": "Philippe",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Plat",
"given": "Françoise",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Rigalleau",
"given": "Vincent",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5989-5409",
"affiliation": [],
"authenticated-orcid": false,
"family": "Robert",
"given": "René",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Seret-Bégué",
"given": "Dominique",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sérusclat",
"given": "Pierre",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Smati",
"given": "Sarra",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4926-9943",
"affiliation": [],
"authenticated-orcid": false,
"family": "Thébaut",
"given": "Jean-François",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Tramunt",
"given": "Blandine",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8342-1596",
"affiliation": [],
"authenticated-orcid": false,
"family": "Vatier",
"given": "Camille",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Velayoudom",
"given": "Fritz-Line",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vergès",
"given": "Bruno",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Winiszewski",
"given": "Patrice",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zabulon",
"given": "Audrey",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1131-9554",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gourraud",
"given": "Pierre-Antoine",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2292-8363",
"affiliation": [],
"authenticated-orcid": false,
"family": "Roussel",
"given": "Ronan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cariou",
"given": "Bertrand",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7110-6994",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hadjadj",
"given": "Samy",
"sequence": "additional"
}
],
"container-title": [
"Diabetologia"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
2,
19
]
],
"date-time": "2021-02-19T15:07:09Z",
"timestamp": 1613747229000
},
"deposited": {
"date-parts": [
[
2021,
3,
8
]
],
"date-time": "2021-03-08T11:11:13Z",
"timestamp": 1615201873000
},
"funder": [
{
"DOI": "10.13039/100009947",
"doi-asserted-by": "publisher",
"name": "Merck Sharp and Dohme"
},
{
"name": "Fonds de dotation du CHU de Nantes"
},
{
"name": "Fondation Francophone de Recherche sur le Diabète"
},
{
"DOI": "10.13039/501100008966",
"doi-asserted-by": "publisher",
"name": "Société Francophone du Diabète"
},
{
"DOI": "10.13039/100004312",
"doi-asserted-by": "publisher",
"name": "Eli Lilly and Company"
},
{
"DOI": "10.13039/100004325",
"doi-asserted-by": "publisher",
"name": "AstraZeneca"
},
{
"DOI": "10.13039/501100004191",
"doi-asserted-by": "publisher",
"name": "Novo Nordisk"
},
{
"name": "Fédération Française des Diabétiques"
},
{
"DOI": "10.13039/100000046",
"doi-asserted-by": "publisher",
"name": "Abbott Fund"
}
],
"indexed": {
"date-parts": [
[
2022,
2,
16
]
],
"date-time": "2022-02-16T06:46:51Z",
"timestamp": 1644994011664
},
"is-referenced-by-count": 42,
"issn-type": [
{
"type": "print",
"value": "0012-186X"
},
{
"type": "electronic",
"value": "1432-0428"
}
],
"issue": "4",
"issued": {
"date-parts": [
[
2021,
2,
17
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2021,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
2,
17
]
],
"date-time": "2021-02-17T00:00:00Z",
"timestamp": 1613520000000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
2,
17
]
],
"date-time": "2021-02-17T00:00:00Z",
"timestamp": 1613520000000
}
}
],
"link": [
{
"URL": "http://link.springer.com/content/pdf/10.1007/s00125-020-05351-w.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://link.springer.com/article/10.1007/s00125-020-05351-w/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://link.springer.com/content/pdf/10.1007/s00125-020-05351-w.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "778-794",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2021,
2,
17
]
]
},
"published-online": {
"date-parts": [
[
2021,
2,
17
]
]
},
"published-print": {
"date-parts": [
[
2021,
4
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1001/jama.2020.4683",
"author": "G Onder",
"doi-asserted-by": "publisher",
"first-page": "1775",
"issue": "18",
"journal-title": "JAMA.",
"key": "5351_CR1",
"unstructured": "Onder G, Rezza G, Brusaferro S (2020) Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 323(18):1775–1776. https://doi.org/10.1001/jama.2020.4683",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"author": "F Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"issue": "10229",
"journal-title": "Lancet",
"key": "5351_CR2",
"unstructured": "Zhou F, Yu T, Du R et al (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229):1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1017/S0950268818002923",
"doi-asserted-by": "publisher",
"key": "5351_CR3",
"unstructured": "Alqahtani FY, Aleanizy FS, Ali El Hadi Mohamed R et al (2018) Prevalence of comorbidities in cases of Middle East respiratory syndrome coronavirus: a retrospective study. Epidemiol Infect:1–5. https://doi.org/10.1017/S0950268818002923"
},
{
"DOI": "10.1111/j.1464-5491.2006.01861.x",
"author": "JK Yang",
"doi-asserted-by": "publisher",
"first-page": "623",
"issue": "6",
"journal-title": "Diabet Med",
"key": "5351_CR4",
"unstructured": "Yang JK, Feng Y, Yuan MY et al (2006) Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet Med 23(6):623–628. https://doi.org/10.1111/j.1464-5491.2006.01861.x",
"volume": "23",
"year": "2006"
},
{
"DOI": "10.1001/jama.2020.5394",
"author": "G Grasselli",
"doi-asserted-by": "publisher",
"first-page": "1574",
"issue": "16",
"journal-title": "JAMA",
"key": "5351_CR5",
"unstructured": "Grasselli G, Zangrillo A, Zanella A et al (2020) Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 323(16):1574–1581. https://doi.org/10.1001/jama.2020.5394",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.2337/dc20-1295",
"author": "E Selvin",
"doi-asserted-by": "publisher",
"first-page": "1690",
"issue": "8",
"journal-title": "Diabetes Care",
"key": "5351_CR6",
"unstructured": "Selvin E, Juraschek SP (2020) Diabetes epidemiology in the COVID-19 pandemic. Diabetes Care 43(8):1690–1694. https://doi.org/10.2337/dc20-1295",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1996",
"author": "MG Argenziano",
"doi-asserted-by": "publisher",
"first-page": "m1996",
"journal-title": "BMJ",
"key": "5351_CR7",
"unstructured": "Argenziano MG, Bruce SL, Slater CL et al (2020) Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ 369:m1996. https://doi.org/10.1136/bmj.m1996",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2004500",
"author": "PK Bhatraju",
"doi-asserted-by": "publisher",
"first-page": "2012",
"issue": "21",
"journal-title": "N Engl J Med",
"key": "5351_CR8",
"unstructured": "Bhatraju PK, Ghassemieh BJ, Nichols M et al (2020) Covid-19 in critically ill patients in the Seattle region - case series. N Engl J Med 382(21):2012–2022. https://doi.org/10.1056/NEJMoa2004500",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/j.jcv.2020.104354",
"author": "L Roncon",
"doi-asserted-by": "publisher",
"first-page": "104354",
"journal-title": "J Clin Virol",
"key": "5351_CR9",
"unstructured": "Roncon L, Zuin M, Rigatelli G, Zuliani G (2020) Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J Clin Virol 127:104354. https://doi.org/10.1016/j.jcv.2020.104354",
"volume": "127",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"author": "C Wu",
"doi-asserted-by": "publisher",
"first-page": "934",
"issue": "7",
"journal-title": "JAMA Intern Med",
"key": "5351_CR10",
"unstructured": "Wu C, Chen X, Cai Y et al (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 180(7):934–943. https://doi.org/10.1001/jamainternmed.2020.0994",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1111/dme.14319",
"author": "LE Joensen",
"doi-asserted-by": "publisher",
"first-page": "1146",
"issue": "7",
"journal-title": "Diabet Med",
"key": "5351_CR11",
"unstructured": "Joensen LE, Madsen KP, Holm L et al (2020) Diabetes and COVID-19: psychosocial consequences of the COVID-19 pandemic in people with diabetes in Denmark-what characterizes people with high levels of COVID-19-related worries? Diabet Med 37(7):1146–1154. https://doi.org/10.1111/dme.14319",
"volume": "37",
"year": "2020"
},
{
"DOI": "10.1016/j.metabol.2020.154248",
"author": "S Mukhtar",
"doi-asserted-by": "publisher",
"first-page": "154248",
"journal-title": "Metabolism",
"key": "5351_CR12",
"unstructured": "Mukhtar S, Mukhtar S (2020) Letter to the editor: mental health and psychological distress in people with diabetes during COVID-19. Metabolism 108:154248. https://doi.org/10.1016/j.metabol.2020.154248",
"volume": "108",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.2492",
"author": "SL Sy",
"doi-asserted-by": "publisher",
"first-page": "1147",
"issue": "9",
"journal-title": "JAMA Intern Med",
"key": "5351_CR13",
"unstructured": "Sy SL, Munshi MN (2020) Caring for older adults with diabetes during the COVID-19 pandemic. JAMA Intern Med 180(9):1147–1148. https://doi.org/10.1001/jamainternmed.2020.2492",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"author": "B Cariou",
"doi-asserted-by": "publisher",
"first-page": "1500",
"issue": "8",
"journal-title": "Diabetologia",
"key": "5351_CR14",
"unstructured": "Cariou B, Hadjadj S, Wargny M et al (2020) Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia 63(8):1500–1151. https://doi.org/10.1007/s00125-020-05180-x",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1016/j.numecd.2020.05.014",
"author": "A Mantovani",
"doi-asserted-by": "publisher",
"first-page": "1236",
"issue": "8",
"journal-title": "Nutr Metab Cardiovasc Dis",
"key": "5351_CR15",
"unstructured": "Mantovani A, Byrne CD, Zheng MH, Targher G (2020) Diabetes as a risk factor for greater COVID-19 severity and in-hospital death: a meta-analysis of observational studies. Nutr Metab Cardiovasc Dis 30(8):1236–1248. https://doi.org/10.1016/j.numecd.2020.05.014",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.2337/dc20-1543",
"author": "S Agarwal",
"doi-asserted-by": "publisher",
"first-page": "2339",
"issue": "10",
"journal-title": "Diabetes Care",
"key": "5351_CR16",
"unstructured": "Agarwal S, Schechter C, Southern W, Crandall JP, Tomer Y (2020) Preadmission diabetes-specific risk factors for mortality in hospitalized patients with diabetes and coronavirus disease 2019. Diabetes Care 43(10):2339–2344. https://doi.org/10.2337/dc20-1543",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1985",
"author": "AB Docherty",
"doi-asserted-by": "publisher",
"first-page": "m1985",
"journal-title": "BMJ",
"key": "5351_CR17",
"unstructured": "Docherty AB, Harrison EM, Green CA et al (2020) Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study. BMJ 369:m1985. https://doi.org/10.1136/bmj.m1985",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"author": "N Holman",
"doi-asserted-by": "publisher",
"first-page": "823",
"issue": "10",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "5351_CR18",
"unstructured": "Holman N, Knighton P, Kar P et al (2020) Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol 8(10):823–833. https://doi.org/10.1016/S2213-8587(20)30271-0",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"author": "E Williamson",
"doi-asserted-by": "publisher",
"first-page": "430",
"issue": "7821",
"journal-title": "Nature",
"key": "5351_CR19",
"unstructured": "Williamson E, Walker A, Bhaskaran K et al (2020) Factors associated with COVID-19-related death using OpenSAFELY. Nature 584(7821):430–436. https://doi.org/10.1038/s41586-020-2521-4",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m3339",
"author": "S Knight",
"doi-asserted-by": "publisher",
"first-page": "m3339",
"journal-title": "BMJ",
"key": "5351_CR20",
"unstructured": "Knight S, Ho A, Pius R et al (2020) Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. BMJ 370:m3339. https://doi.org/10.1136/bmj.m3339",
"volume": "370",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05216-2",
"author": "C Sardu",
"doi-asserted-by": "publisher",
"first-page": "2486",
"issue": "11",
"journal-title": "Diabetologia",
"key": "5351_CR21",
"unstructured": "Sardu C, D’Onofrio N, Balestrieri ML et al (2020) Hyperglycaemia on admission to hospital and COVID-19. Diabetologia 63(11):2486–2487. https://doi.org/10.1007/s00125-020-05216-2",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05225-1",
"author": "PM Lepper",
"doi-asserted-by": "publisher",
"first-page": "2488",
"issue": "11",
"journal-title": "Diabetologia",
"key": "5351_CR22",
"unstructured": "Lepper PM, Bals R, Jüni P, von Eynatten M (2020) Blood glucose, diabetes and metabolic control in patients with community-acquired pneumonia. Diabetologia 63(11):2488–2490. https://doi.org/10.1007/s00125-020-05225-1",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05209-1",
"author": "S Wang",
"doi-asserted-by": "publisher",
"first-page": "2102",
"issue": "10",
"journal-title": "Diabetologia",
"key": "5351_CR23",
"unstructured": "Wang S, Ma P, Zhang S et al (2020) Fasting blood glucose at admission is an independent predictor for 28-day mortality in patients with COVID-19 without previous diagnosis of diabetes: a multi-centre retrospective study. Diabetologia 63(10):2102–2111. https://doi.org/10.1007/s00125-020-05209-1",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.1111/dom.14132",
"doi-asserted-by": "publisher",
"key": "5351_CR24",
"unstructured": "Zhang B, Liu S, Zhang L, Dong Y, Zhang S (2020) Admission fasting blood glucose predicts 30-day poor outcome in patients hospitalized for COVID-19 pneumonia. Diabetes Obes Metab. https://doi.org/10.1111/dom.14132"
},
{
"DOI": "10.2337/dc20-1380",
"author": "A Coppelli",
"doi-asserted-by": "publisher",
"first-page": "2345",
"issue": "10",
"journal-title": "Diabetes Care",
"key": "5351_CR25",
"unstructured": "Coppelli A, Giannarelli R, Aragona M et al (2020) Hyperglycemia at hospital admission is associated with severity of the prognosis in patients hospitalized for COVID-19: the Pisa COVID-19 Study. Diabetes Care 43(10):2345–2348. https://doi.org/10.2337/dc20-1380",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1111/1753-0407.13084",
"doi-asserted-by": "publisher",
"key": "5351_CR26",
"unstructured": "Xu Z, Wang Z, Wang S et al (2020) The impact of type 2 diabetes and its management on the prognosis of patients with severe COVID-19. J Diabetes. https://doi.org/10.1111/1753-0407.13084"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"author": "L Zhu",
"doi-asserted-by": "publisher",
"first-page": "1068",
"issue": "6",
"journal-title": "Cell Metab",
"key": "5351_CR27",
"unstructured": "Zhu L, She ZG, Cheng X et al (2020) Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab 31(6):1068–1077 e1063. https://doi.org/10.1016/j.cmet.2020.04.021",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(99)08415-9",
"author": "SE Capes",
"doi-asserted-by": "publisher",
"first-page": "773",
"issue": "9206",
"journal-title": "Lancet",
"key": "5351_CR28",
"unstructured": "Capes SE, Hunt D, Malmberg K, Gerstein HC (2000) Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet 355(9206):773–778. https://doi.org/10.1016/S0140-6736(99)08415-9",
"volume": "355",
"year": "2000"
},
{
"DOI": "10.1177/2048872618777819",
"doi-asserted-by": "publisher",
"key": "5351_CR29",
"unstructured": "Gencer B, Rigamonti F, Nanchen D et al (2018) Prognostic values of fasting hyperglycaemia in non-diabetic patients with acute coronary syndrome: a prospective cohort study. Eur Heart J Acute Cardiovasc Care:2048872618777819. https://doi.org/10.1177/2048872618777819"
},
{
"DOI": "10.1186/s12933-017-0582-y",
"author": "O Itzhaki Ben Zadok",
"doi-asserted-by": "publisher",
"first-page": "102",
"issue": "1",
"journal-title": "Cardiovasc Diabetol",
"key": "5351_CR30",
"unstructured": "Itzhaki Ben Zadok O, Kornowski R, Goldenberg I et al (2017) Admission blood glucose and 10-year mortality among patients with or without pre-existing diabetes mellitus hospitalized with heart failure. Cardiovasc Diabetol 16(1):102. https://doi.org/10.1186/s12933-017-0582-y",
"volume": "16",
"year": "2017"
},
{
"DOI": "10.1161/STROKEAHA.117.019081",
"author": "Y Pan",
"doi-asserted-by": "publisher",
"first-page": "3006",
"issue": "11",
"journal-title": "Stroke",
"key": "5351_CR31",
"unstructured": "Pan Y, Cai X, Jing J et al (2017) Stress hyperglycemia and prognosis of minor ischemic stroke and transient ischemic attack: the CHANCE study (clopidogrel in high-risk patients with acute nondisabling cerebrovascular events). Stroke 48(11):3006–3011. https://doi.org/10.1161/STROKEAHA.117.019081",
"volume": "48",
"year": "2017"
},
{
"DOI": "10.1016/j.cmet.2020.06.015",
"doi-asserted-by": "publisher",
"key": "5351_CR32",
"unstructured": "Zhang XJ, Qin JJ, Cheng X et al (2020) In-hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19. Cell Metab 32(2):176–187.e4. https://doi.org/10.1016/j.cmet.2020.06.015"
}
],
"reference-count": 32,
"references-count": 32,
"relation": {},
"score": 1,
"short-container-title": [
"Diabetologia"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": [
"Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "64"
}
