Outpatient metformin use is associated with reduced severity of COVID‐19 disease in adults with overweight or obesity
et al., Journal of Medical Virology, doi:10.1002/jmv.26873, Mar 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 17,396 PCR+ patients in the USA, showing lower mortality with metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
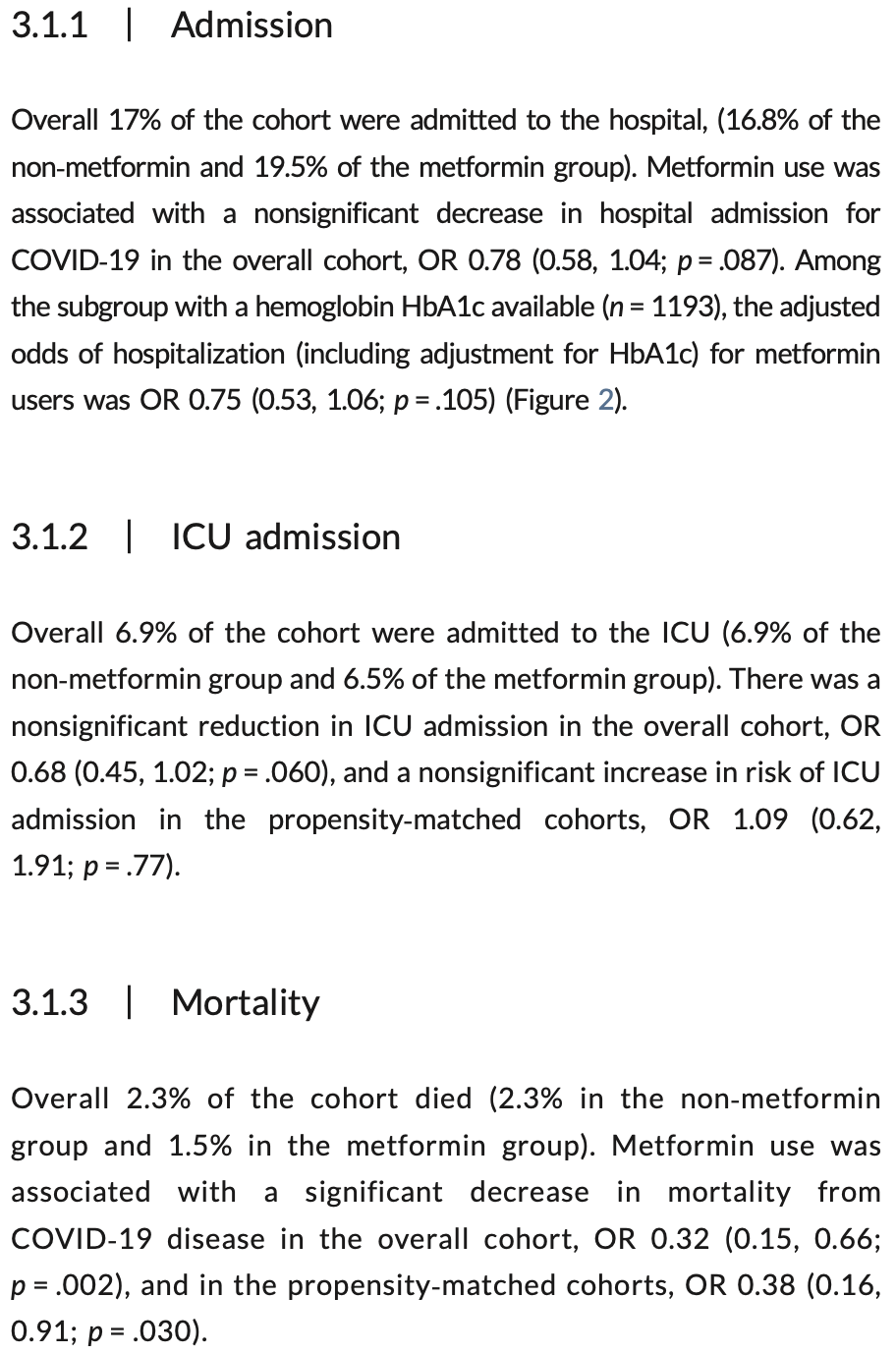
risk of death, 62.0% lower, OR 0.38, p = 0.03, treatment 342, control 342, propensity score matching, RR approximated with OR.
|
|
risk of death, 68.0% lower, OR 0.32, p = 0.003, treatment 676, control 8,879, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of ICU admission, 9.0% higher, OR 1.09, p = 0.78, treatment 342, control 342, propensity score matching, RR approximated with OR.
|
|
risk of ICU admission, 32.0% lower, OR 0.68, p = 0.06, treatment 676, control 8,879, adjusted per study, multivariable, RR approximated with OR.
|
|
risk of hospitalization, 22.0% lower, OR 0.78, p = 0.10, treatment 676, control 8,879, adjusted per study, multivariable, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Bramante et al., 23 Mar 2021, retrospective, USA, peer-reviewed, 18 authors, study period 4 March, 2020 - 4 December, 2020.
Contact: bramante@umn.edu.
Outpatient metformin use is associated with reduced severity of COVID‐19 disease in adults with overweight or obesity
Journal of Medical Virology, doi:10.1002/jmv.26873
Observational studies suggest outpatient metformin use is associated with reduced mortality from coronavirus disease-2019 (COVID-19). Metformin is known to decrease interleukin-6 and tumor-necrosis factor-α, which appear to contribute to morbidity in COVID-19. We sought to understand whether outpatient metformin use was associated with reduced odds of severe COVID-19 disease in a large US healthcare data set. Retrospective cohort analysis of electronic health record (EHR) data that was pooled across This is an open access article under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs License, which permits use and distribution in any medium, provided the original work is properly cited, the use is non-commercial and no modifications or adaptations are made.
AUTHOR CONTRIBUTIONS Dr. Tignanelli is the guarantor with responsibility for the work as a whole given his full access to the data. Carolyn T. Bramante Michael Usher contributed to design and analysis. Ryan Demmer contributed to design, analysis, and critical review. Genevieve B. Melton contributed to design and analysis and writing. Nicholas Ingraham contributed to analysis and writing. Christopher J. Tignanelli contributed to study design, analysis, interpretation, and critical review.
SUPPORTING INFORMATION Additional Supporting Information may be found online in the supporting information tab for this article.
References
Afshari, Haddadi, Anti-inflammatory effects of metformin improve the neuropathic pain and locomotor activity in spinal cord injured rats: introduction of an alternative therapy, Spinal Cord
Alwarawrah, Nichols, Green, Targeting T-cell oxidative metabolism to improve influenza survival in a mouse model of obesity, Int J Obes
Atzeni, Gerratana, Giallanza, The effect of drugs used in rheumatology for treating SARS-CoV2 infection, Expert Opin Biol Ther
Babinski, Giermaziak, Influenza epidemic in 1971 in diabetics treated with 1-butyl-biguanidine hydrochloride (Silubin retard) and 1-phenylethyl-biguanidine hydrochloride (Phenformin), Pol Tyg Lek
Bailey, Metformin: historical overview, Diabetologia
Barbaro, Hoffman, The Vaccine Trust Problem [Internet
Berlin, Gulick, Martinez, Severe COVID-19, N Engl J Med
Bramante, Ingraham, Murray, Observational study of metformin and risk of mortality in patients hospitalized with COVID-19
Bramante, Tignanelli, Dutta, Non-alcoholic fatty liver disease (NAFLD) and risk of hospitalization for COVID-19, doi:10.1101/2020.09.01.20185850v1
Brookhart, Schneeweiss, Rothman, Glynn, Avorn et al., Variable selection for propensity score models, Am J Epidemiol
Cameron, Morrison, Levin, Anti-inflammatory effects of metformin irrespective of diabetes status, Circ Res
Campo, García-Valdecasas, Simvastatin and metformin inhibit cell growth in hepatitis C virus infected cells via mTOR increasing PTEN and autophagy, PLOS One
Campo, García-Valdecasas, Simvastatin and metformin inhibit cell growth in hepatitis C virus infected cells via mTOR increasing PTEN and autophagy, PLOS One
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia
Chen, Sang, Jiang, Longitudinal hematologic and immunologic variations associated with the progression of COVID-19 patients in China, J Allergy Clin Immunol
Crouse, Grimes, Peng, Might, Ovalle et al., Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes
De Macedo, Brazil and COVID-19-A fleeting glimpse of what is to come, JAMA Health Forum
Dehkordi, Abbaszadeh, Mir, Hasanvand, Metformin and its anti-inflammatory and anti-oxidative effects; new concepts, J Renal Inj Prev
Flory, Lipska, Metformin in 2019, JAMA
Gordon, Jang, Bouhaddou, A SARS-CoV-2-human protein-protein interaction map reveals drug targets and potential drug-repurposing, bioRxiv
Hyun, Shin, Lee, Metformin down-regulates TNF-α secretion via suppression of scavenger receptors in macrophages, Immune Netw
Ingraham, Lotfi-Emran, Thielen, Immunomodulation in COVID-19, Lancet Respir Med
Karam, Morris, Bramante, mTOR inhibition in COVID-19: A commentary and review of efficacy in RNA viruses, J Med Virol
Krysiak, Gdula-Dymek, Okopień, Monocyte-suppressing effect of high-dose metformin in fenofibrate-treated patients with impaired glucose tolerance, Pharmacol Rep
Kuo, Pilling, Atkins, COVID-19 severity is predicted by earlier evidence of accelerated aging, medRxiv
Little, Agostino, Cohen, The prevention and treatment of missing data in clinical trials, N Engl J Med
Lunt, Selecting an appropriate caliper can be essential for achieving good balance with propensity score matching, Am J Epidemiol
Luo, Qiu, Liu, Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am J Trop Med Hyg
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., COVID-19: consider cytokine storm syndromes and immunosuppression, Lancet
Mishra, Dingli, Metformin inhibits IL-6 signaling by decreasing IL-6R expression on multiple myeloma cells, Leukemia
Nakashima, Takeuchi, Chihara, Hotta, Sada, Inhibition of hepatitis C virus replication through adenosine monophosphateactivated protein kinase-dependent and -independent pathways, Microbiol Immunol
Rangarajan, Bone, Zmijewska, Metformin reverses established lung fibrosis in a bleomycin model, Nat Med
Salber, Wang, Lynch, Metformin use in practice: compliance with guidelines for patients with diabetes and preserved renal function, Clinical Diabetes
Salpeter, Greyber, Pasternak, Posthumous, Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus, Cochrane Database Syst Rev
Singh, Singh, Suhail, AMP-activated protein kinase restricts zika virus replication in endothelial cells by potentiating innate antiviral responses and inhibiting glycolysis, J Immunol
Ursini, Russo, Pellino, Metformin and autoimmunity: a "new deal" of an old drug, Front Immunol
Vanderweele, Ding, Sensitivity analysis in observational research: introducing the E-value, Ann Intern Med
Verdura, Cuyàs, Martin-Castillo, Menendez, Metformin as an archetype immuno-metabolic adjuvant for cancer immunotherapy, Oncoimmunology
Wang, Li, Chen, Gu, Ye, Neutrophil extracellular trap mitochondrial DNA and its autoantibody in systemic lupus erythematosus and a proof-of-concept trial of metformin, Arthritis Rheumatol
Warnakulasuriya, Fernando, Adikaram, Metformin in the management of childhood obesity: a randomized control trial, Childhood Obesity
DOI record:
{
"DOI": "10.1002/jmv.26873",
"ISSN": [
"0146-6615",
"1096-9071"
],
"URL": "http://dx.doi.org/10.1002/jmv.26873",
"alternative-id": [
"10.1002/jmv.26873"
],
"assertion": [
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2020-12-22"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 1,
"value": "2021-02-10"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 2,
"value": "2021-03-23"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5858-2080",
"affiliation": [
{
"name": "Department of Medicine, Division of General Internal Medicine University of Minnesota Minneapolis Minnesota USA"
}
],
"authenticated-orcid": false,
"family": "Bramante",
"given": "Carolyn T.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Medicine, Division of Endocrinology University of North Carolina Chapel Hill North Carolina USA"
}
],
"family": "Buse",
"given": "John",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Humana Health Services Research Center, Miami University Miami Florida USA"
}
],
"family": "Tamaritz",
"given": "Leonardo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Humana Health Services Research Center, Miami University Miami Florida USA"
}
],
"family": "Palacio",
"given": "Ana",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "UnitedHealth Group Research and Development Minnetonka Minnesota USA"
}
],
"family": "Cohen",
"given": "Ken",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "UnitedHealth Group Research and Development Minnetonka Minnesota USA"
}
],
"family": "Vojta",
"given": "Deneen",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Northwestern University Feinberg School of Medicine Chicago Illinois USA"
}
],
"family": "Liebovitz",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Duke University School of Medicine Durham North Carolina USA"
}
],
"family": "Mitchell",
"given": "Nia",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Division of General Internal Medicine University of Colorado School of Medicine Aurora Colorado USA"
}
],
"family": "Nicklas",
"given": "Jacinda",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine/Endocrinology UT Southwestern Medical Center Dallas Texas USA"
},
{
"name": "Department of Population and Data Sciences UT Southwestern Medical Center Dallas Texas USA"
}
],
"family": "Lingvay",
"given": "Ildiko",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Division of General Internal Medicine John Hopkins Baltimore Maryland USA"
}
],
"family": "Clark",
"given": "Jeanne M.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine Weill Cornell Medicine New York New York USA"
}
],
"family": "Aronne",
"given": "Louis J.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Emergency Medicine Alameda County Oakland California USA"
}
],
"family": "Anderson",
"given": "Erik",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Division of General Internal Medicine University of Minnesota Minneapolis Minnesota USA"
}
],
"family": "Usher",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Epidemiology, Division of Epidemiology and Community Health University of Minnesota School of Public Health Minneapolis Minnesota USA"
}
],
"family": "Demmer",
"given": "Ryan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Division of Pulmonary Medicine University of Minnesota Minneapolis Minnesota USA"
}
],
"family": "Melton",
"given": "Genevieve B.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0292-0594",
"affiliation": [
{
"name": "Department of Surgery, Division of Surgical Oncology University of Minnesota Minneapolis Minnesota USA"
}
],
"authenticated-orcid": false,
"family": "Ingraham",
"given": "Nicholas",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Medicine, Division of Pulmonary Medicine University of Minnesota Minneapolis Minnesota USA"
}
],
"family": "Tignanelli",
"given": "Christopher J.",
"sequence": "additional"
}
],
"container-title": "Journal of Medical Virology",
"container-title-short": "Journal of Medical Virology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"onlinelibrary.wiley.com"
]
},
"created": {
"date-parts": [
[
2021,
2,
14
]
],
"date-time": "2021-02-14T15:45:32Z",
"timestamp": 1613317532000
},
"deposited": {
"date-parts": [
[
2022,
1,
25
]
],
"date-time": "2022-01-25T06:22:54Z",
"timestamp": 1643091774000
},
"funder": [
{
"DOI": "10.13039/100000133",
"award": [
"K12HS026379"
],
"doi-asserted-by": "publisher",
"name": "Agency for Healthcare Research and Quality"
},
{
"DOI": "10.13039/100000050",
"award": [
"1K23HL133604",
"T32HL07741"
],
"doi-asserted-by": "publisher",
"name": "National Heart, Lung, and Blood Institute"
},
{
"DOI": "10.13039/100006108",
"award": [
"KL2TR002492",
"UL1TR002489",
"UL1TR002494"
],
"doi-asserted-by": "publisher",
"name": "National Center for Advancing Translational Sciences"
}
],
"indexed": {
"date-parts": [
[
2023,
2,
16
]
],
"date-time": "2023-02-16T10:53:25Z",
"timestamp": 1676544805365
},
"is-referenced-by-count": 31,
"issue": "7",
"issued": {
"date-parts": [
[
2021,
3,
23
]
]
},
"journal-issue": {
"issue": "7",
"published-print": {
"date-parts": [
[
2021,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
3,
23
]
],
"date-time": "2021-03-23T00:00:00Z",
"timestamp": 1616457600000
}
},
{
"URL": "http://doi.wiley.com/10.1002/tdm_license_1.1",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
3,
23
]
],
"date-time": "2021-03-23T00:00:00Z",
"timestamp": 1616457600000
}
}
],
"link": [
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/jmv.26873",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/full-xml/10.1002/jmv.26873",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://onlinelibrary.wiley.com/doi/pdf/10.1002/jmv.26873",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "311",
"original-title": [],
"page": "4273-4279",
"prefix": "10.1002",
"published": {
"date-parts": [
[
2021,
3,
23
]
]
},
"published-online": {
"date-parts": [
[
2021,
3,
23
]
]
},
"published-print": {
"date-parts": [
[
2021,
7
]
]
},
"publisher": "Wiley",
"reference": [
{
"DOI": "10.1001/jamahealthforum.2020.1061",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_2_1"
},
{
"key": "e_1_2_10_3_1",
"unstructured": "BarbaroM HoffmanJ.The Vaccine Trust Problem [Internet]: National Public Radio 2020 July 21 2020. Podcast. https://www.nytimes.com/2020/07/21/podcasts/the-daily/coronavirus-vaccine.html"
},
{
"DOI": "10.1101/2020.06.19.20135095",
"doi-asserted-by": "crossref",
"key": "e_1_2_10_4_1",
"unstructured": "BramanteC IngrahamN MurrayT et al.Observational study of metformin and risk of mortality in patients hospitalized with COVID‐19.medRxiv.2020."
},
{
"DOI": "10.1101/2020.09.01.20185850",
"doi-asserted-by": "crossref",
"key": "e_1_2_10_5_1",
"unstructured": "BramanteCT TignanelliCJ DuttaN et al. Non‐alcoholic fatty liver disease (NAFLD) and risk of hospitalization for COVID‐19.https://www.medrxiv.org/content/10.1101/2020.09.01.20185850v1. Accessed 2020."
},
{
"DOI": "10.1007/s00125-020-05180-x",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_6_1"
},
{
"DOI": "10.1101/2020.07.29.20164020",
"doi-asserted-by": "crossref",
"key": "e_1_2_10_7_1",
"unstructured": "CrouseA GrimesT PengL MightM OvalleF ShalevA.Metformin use is associated with reduced mortality in a diverse population with COVID‐19 and diabetes.medRxiv. 2020."
},
{
"DOI": "10.4269/ajtmh.20-0375",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_8_1"
},
{
"DOI": "10.1161/CIRCRESAHA.116.308445",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_9_1"
},
{
"DOI": "10.3389/fimmu.2018.01236",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_10_1"
},
{
"DOI": "10.15171/jrip.2019.11",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_11_1"
},
{
"DOI": "10.1038/s41393-018-0168-x",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_12_1"
},
{
"DOI": "10.1080/14712598.2020.1817372",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_13_1"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_14_1"
},
{
"DOI": "10.1016/S2213-2600(20)30226-5",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_15_1"
},
{
"DOI": "10.1056/NEJMcp2009575",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_16_1"
},
{
"DOI": "10.1016/j.jaci.2020.05.003",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_17_1"
},
{
"article-title": "A SARS‐CoV‐2‐human protein‐protein interaction map reveals drug targets and potential drug‐repurposing",
"author": "Gordon DE",
"journal-title": "bioRxiv",
"key": "e_1_2_10_18_1",
"year": "2020"
},
{
"DOI": "10.4049/jimmunol.1901310",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_19_1"
},
{
"DOI": "10.1007/s00125-017-4318-z",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_20_1"
},
{
"DOI": "10.1001/jama.2019.3805",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_21_1"
},
{
"article-title": "Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus",
"author": "Salpeter SR",
"first-page": "Cd002967",
"journal-title": "Cochrane Database Syst Rev",
"key": "e_1_2_10_22_1",
"volume": "1",
"year": "2010"
},
{
"DOI": "10.1056/NEJMsr1203730",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_23_1"
},
{
"key": "e_1_2_10_24_1",
"unstructured": "Health MDo. Weekly COVID‐19 Report.https://www.health.state.mn.us/diseases/coronavirus/stats/covidweekly30.pdf. Accessed July 23 2020."
},
{
"key": "e_1_2_10_25_1",
"unstructured": "MN. Health Information Exchange. 2020. www.health.state.mn.us/facilities/ehealth/hie/certified/index.html. Accessed September 1 2020."
},
{
"DOI": "10.1101/2020.07.10.20147777",
"doi-asserted-by": "crossref",
"key": "e_1_2_10_26_1",
"unstructured": "KuoC‐L PillingLC AtkinsJC et al. COVID‐19 severity is predicted by earlier evidence of accelerated aging.medRxiv.2020:2020.2007.2010.20147777."
},
{
"DOI": "10.1093/aje/kwt212",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_27_1"
},
{
"DOI": "10.1093/aje/kwj149",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_28_1"
},
{
"DOI": "10.7326/M16-2607",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_29_1"
},
{
"DOI": "10.1038/s41591-018-0087-6",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_30_1"
},
{
"DOI": "10.4110/in.2013.13.4.123",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_31_1"
},
{
"DOI": "10.1016/S1734-1140(13)71489-0",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_32_1"
},
{
"DOI": "10.1038/s41375-019-0470-4",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_33_1"
},
{
"DOI": "10.2337/diacare.28.10.2472",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_34_1"
},
{
"DOI": "10.1089/chi.2018.0043",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_35_1"
},
{
"DOI": "10.1002/art.39296",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_36_1"
},
{
"DOI": "10.1080/2162402X.2019.1633235",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_37_1"
},
{
"DOI": "10.1038/s41366-020-00692-3",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_38_1"
},
{
"article-title": "mTOR inhibition in COVID‐19: A commentary and review of efficacy in RNA viruses",
"author": "Karam BS",
"journal-title": "J Med Virol",
"key": "e_1_2_10_39_1"
},
{
"DOI": "10.1371/journal.pone.0191805",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_40_1"
},
{
"DOI": "10.1371/journal.pone.0191805",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_41_1"
},
{
"DOI": "10.1111/j.1348-0421.2011.00382.x",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_42_1"
},
{
"article-title": "Influenza epidemic in 1971 in diabetics treated with 1‐butyl‐biguanidine hydrochloride (Silubin retard) and 1‐phenylethyl‐biguanidine hydrochloride (Phenformin)",
"author": "Babinski S",
"first-page": "1815",
"issue": "46",
"journal-title": "Pol Tyg Lek",
"key": "e_1_2_10_43_1",
"volume": "28",
"year": "1973"
},
{
"DOI": "10.2337/cd15-0045",
"doi-asserted-by": "publisher",
"key": "e_1_2_10_44_1"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "https://onlinelibrary.wiley.com/doi/10.1002/jmv.26873"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Virology"
],
"subtitle": [],
"title": "Outpatient metformin use is associated with reduced severity of COVID‐19 disease in adults with overweight or obesity",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1002/crossmark_policy",
"volume": "93"
}
