Association Between Metformin Use and Mortality Among Patients with Type 2 Diabetes Mellitus Hospitalized for COVID-19 Infection
et al., Journal of the ASEAN Federation of Endocrine Societies, doi:10.15605/jafes.036.02.20, Oct 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 355 diabetic hospitalized COVID-19 patients in the Philippines, showing lower mortality with metformin use.
|
risk of death, 46.8% lower, RR 0.53, p = 0.02, treatment 33 of 186 (17.7%), control 57 of 169 (33.7%), NNT 6.3, adjusted per study, odds ratio converted to relative risk, combined pre-existing and in-hospital use.
|
|
risk of death, 23.9% lower, RR 0.76, p = 0.16, treatment 28 of 109 (25.7%), control 57 of 169 (33.7%), NNT 12, odds ratio converted to relative risk, pre-existing use, unadjusted.
|
|
risk of death, 85.2% lower, RR 0.15, p = 0.002, treatment 2 of 40 (5.0%), control 57 of 169 (33.7%), NNT 3.5, odds ratio converted to relative risk, in-hospital use, unadjusted.
|
|
risk of death, 76.0% lower, RR 0.24, p = 0.005, treatment 3 of 37 (8.1%), control 57 of 169 (33.7%), NNT 3.9, odds ratio converted to relative risk, mixed pre-existing/in-hospital use, unadjusted.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ong et al., 30 Oct 2021, retrospective, Philippines, peer-reviewed, 6 authors, study period 1 March, 2020 - 30 September, 2020.
Contact: anj0321ong@gmail.com.
Association Between Metformin Use and Mortality Among Patients with Type 2 Diabetes Mellitus Hospitalized for COVID-19 Infection
Journal of the ASEAN Federation of Endocrine Societies, doi:10.15605/jafes.036.02.20
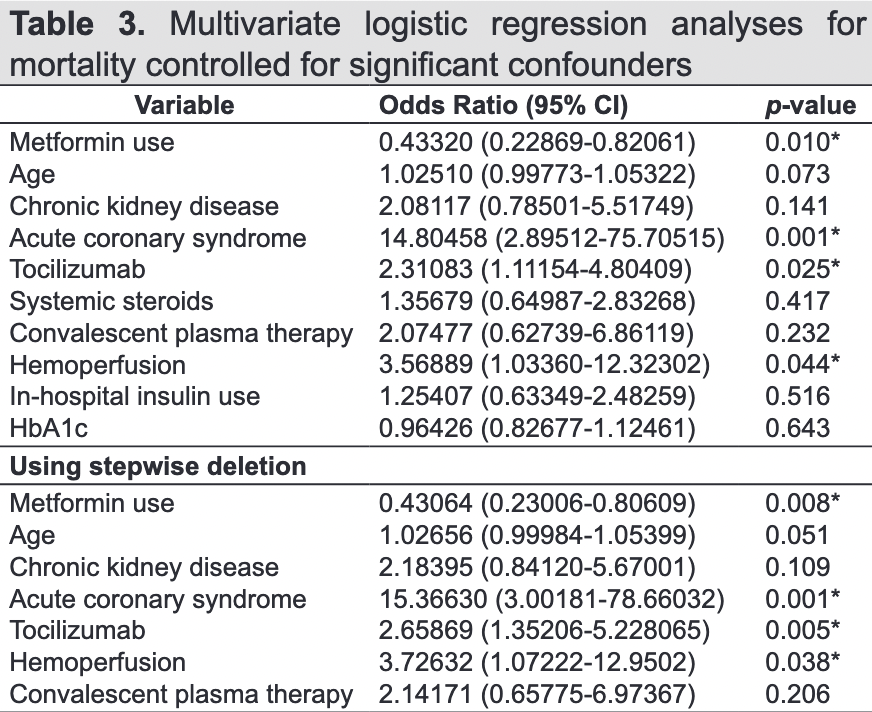
Introduction. Metformin has known mechanistic benefits on COVID-19 infection due to its anti-inflammatory effects and its action on the ACE2 receptor. However, some physicians are reluctant to use it in hypoxemic patients due to potential lactic acidosis. The primary purpose of the study was to determine whether metformin use is associated with survival. We also wanted to determine whether there is a difference in outcomes in subcategories of metformin use, whether at home, in-hospital, or mixed home/in-hospital use. Objectives. This study aimed to determine an association between metformin use and mortality among patients with type 2 diabetes mellitus hospitalized for COVID-19 infection. Methodology. This was a cross-sectional analysis of data acquired from the COVID-19 database of two tertiary hospitals in Cebu from March 1, 2020, to September 30, 2020. Hospitalized adult Filipino patients with type 2 diabetes mellitus who tested positive for COVID-19 via RT-PCR were included and categorized as either metformin users or metformin non-users. Results. We included 355 patients with type 2 diabetes mellitus in the study, 186 (52.4%) were metformin users. They were further categorized into home metformin users (n=109, 30.7%), in-hospital metformin users (n=40, 11.3%), and mixed home/in-hospital metformin users (n=37, 10.4%). Metformin use was associated with a lower risk for mortality compared to non-users (p=0.001; OR=0.424). In-hospital and mixed home/in-hospital metformin users were associated with lower mortality odds than non-users (p=0.002; OR=0.103 and p=0.005; OR 0.173, respectively). The lower risk for mortality was noted in metformin, regardless of dosage, from 500 mg to 2 g daily (p=0.002). Daily dose between ≥1000 mg to <2000 mg was associated with the greatest benefit on mortality (p≤0.001; OR=0.252). The survival distributions between metformin users and non-users were statistically different, showing inequality in survival (χ2=5.67, p=0.017).
Conclusion. Metformin was associated with a lower risk for mortality in persons with type 2 diabetes mellitus hospitalized for COVID-19 disease compared to non-users. Use of metformin in-hospital, and mixed home/in-hospital metformin use, was also associated with decreased risk for mortality. The greatest benefit seen was in those taking a daily dose of ≥1000 mg to <2000 mg.
Statement of Authorship All authors certified fulfillment of ICMJE authorship criteria.
Author Disclosure The authors declared no conflict of interest.
Funding Source None.
APPENDIX Vol. 36
JAFES Send your paper to the publication pathway. Instructions to Authors at www.ASEAN-endocrinejournal.org. Authors are required to accomplish, sign and submit scanned copies of the JAFES Author Form consisting of: (1) Authorship Certification, that authors contributed substantially to the work, that the manuscript has been read and approved by all authors, and that the requirements for authorship have been met by each author; (2) the Author Declaration, that the article represents original material that is not being considered for publication or has not been published or accepted for publication elsewhere, that the article does not infringe or violate any copyrights or intellectual property rights, and that no references have been made to predatory/suspected predatory journals; (3) the Author Contribution Disclosure, which lists the specific contributions of authors; (4) the Author Publishing Agreement which retains author copyright, grants publishing and distribution rights to JAFES, and allows JAFES to apply and enforce an Attribution-Non-Commercial Creative Commons user license; and (5) the Conversion to Visual Abstracts (*optional for original articles only) to improve dissemination to practitioners and lay readers Authors are also required to accomplish, sign, and submit..
References
Alqahtani, Aleanizy, Hadi Mohamed, Prevalence of comorbidities in cases of Middle East respiratory syndrome coronavirus: A retrospective study, Epidemiol Infect, doi:10.1017/S0950268818002923
Assiri, Al-Tawfiq, Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: A descriptive study, Lancet Infect Dis, doi:10.1016/S1473-3099
Bajgain, Badal, Bajgain, Santana, Prevalence of comorbidities among individuals with COVID-19: A rapid review of current literature, Am J Infect Control, doi:10.1016/j.ajic.2020.06.213
Bode, Garrett, Messler, Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States, J Diabetes Sci Technol, doi:10.1177/1932296820924469
Bornstein, Rubino, Khunti, Practical recommendations for the management of diabetes in patients with COVID-19, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587
Bramante, Ingraham, Murray, Metformin and risk of mortality in patients hospitalized with COVID-19: A retrospective cohort analysis, Lancet Healthy Longev, doi:10.1016/S2666-7568(20)30033-7
Cameron, Morrison, Levin, Anti-inflammatory effects of metformin irrespective of diabetes status, Circ Res, doi:10.1161/CIRCRESAHA.116.308445
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of in-patients with COVID-19 and diabetes: The CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Chan, Ng, Chan, Short-term outcome and risk factors for adverse clinical outcomes in adults with severe respiratory syndrome (SARS), Thorax, doi:10.1136/thorax.58.8.686
Cheng, Liu, Li, Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and preexisting type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.08.013
Crouse, Grimes, Li, Might, Ovalle et al., Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes, medRxiv, doi:10.1101/2020.07.29.20164020
Dalan, Metformin, neutrophils, and COVID-19 infection, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108230
Gupta, Ghosh, Singh, Misra, Clinical considerations for patients with diabetes in times of COVID-19 epidemic, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.03.002
Hoffman, Weber-Kleine, Schroeder, SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor, Cell, doi:10.1016/j.cell.2020.02.052
Hojyo, Uchida, Tanaka, How COVID-19 induces cytokine storm with high mortality, Inflamm Regen, doi:10.1186/s41232-020-00146-3
Hong, Zhang, Lai, Effects of metformin versus glipizide on cardiovascular outcomes in patients with type 2 diabetes and coronary artery disease, Diabetes Care, doi:10.2337/dc12-0719
Hyun, Shin, Lee, Metformin down-regulates TNF-alpha secretion via suppression of scavenger receptors in macrophages, Immune Netw, doi:10.4110/in.2013.13.4.123
Kumar, Arora, Sharma, Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.044
Lalau, Al-Salameh, Hadjadj, Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalized for COVID-19, Diabetes Metab, doi:10.1016/j.diabet.2020.101216
Lally, Tsoukas, Halladay, Neill, Gravenstein et al., Metformin is associated with decreased 30-day mortality among nursing home residents infected with SARS-CoV2, J AM Med Dir Assoc, doi:10.1016/j.jamda.2020.10.031
Liu, Li, Lu, AMPK: A balancer of the renin-angiotensin system, Biosci Rep, doi:10.1042/BSR20181994
Luo, Qiu, Liu, Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am J Trop Med Hyg, doi:10.4269/ajtmh.20-0375
Maiese, The mechanistic target of Rapamycin (mTOR): Novel considerations as an antiviral treatment, Curr Neurovasc Res, doi:10.2174/1567202617666200425205122
Plattner, Bibb, Elsevier, Serine and Threonine Phosphorylation, Basic Neurochemistry, doi:10.1016/B978-0-12-374947-5.00025-0
Raz, Guideline approach to therapy in patients with newly diagnosed type 2 diabetes, Diabetes Care, doi:10.2337/dcS13-2035
Shang, Wang, Zhang, The relationship between diabetes mellitus and COVID-19 prognosis: A retrospective cohort study in Wuhan, China, Am J Med, doi:10.1016/j.amjmed.2020.05.033
Shi, Zhang, Jiang, Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: A two-center, retrospective study, Diabetes Care, doi:10.2337/dc20-0598
Silvestre, Carvalho, Mendes, Metformin-induced lactic acidosis: A case series, J Med Case Rep, doi:10.1186/1752-1947
Targher, Mantovani, Wang, Patients with diabetes are at higher risk for severe illness from COVID-19, Diabetes Metab, doi:10.1016/j.diabet.2020.05.001
Wargny, Potier, Gourdy, Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: Updated results from the nationwide CORONADO study, Diabetologia, doi:10.1007/s00125-020-05351-w
Worldometer, Reported cases and deaths by country or territory, Worldometer
Yang, Zheng, Gou, Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis, Int J Infect Dis, doi:10.1016/j.ijid.2020.03.017
Zhou, Yang, Wang, A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature, doi:10.1038/s41586-020-2012-7
Zou, Chen, Zou, Han, Hao et al., The single-cell RNAseq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to Wuhan 2019-nCoV infection, Front Med, doi:10.1007/s11684-020-0754-0
DOI record:
{
"DOI": "10.15605/jafes.036.02.20",
"ISSN": [
"0857-1074",
"2308-118X"
],
"URL": "http://dx.doi.org/10.15605/jafes.036.02.20",
"author": [
{
"affiliation": [],
"family": "Ong",
"given": "Angeli Nicole",
"sequence": "first"
},
{
"affiliation": [],
"name": "Chong Hua Hospital, Cebu City, Philippines",
"sequence": "first"
},
{
"affiliation": [],
"family": "Tan",
"given": "Ceryl Cindy",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cañete",
"given": "Maria Teresa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lim",
"given": "Bryan Albert",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Robles",
"given": "Jeremyjones",
"sequence": "additional"
}
],
"container-title": [
"Journal of the ASEAN Federation of Endocrine Societies"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
11,
26
]
],
"date-time": "2021-11-26T08:25:48Z",
"timestamp": 1637915148000
},
"deposited": {
"date-parts": [
[
2021,
11,
26
]
],
"date-time": "2021-11-26T08:25:51Z",
"timestamp": 1637915151000
},
"indexed": {
"date-parts": [
[
2021,
12,
10
]
],
"date-time": "2021-12-10T21:59:06Z",
"timestamp": 1639173546732
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "0857-1074"
},
{
"type": "electronic",
"value": "2308-118X"
}
],
"issue": "2",
"issued": {
"date-parts": [
[
2021,
10,
30
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2021,
11,
26
]
]
},
"published-print": {
"date-parts": [
[
2021,
11,
26
]
]
}
},
"link": [
{
"URL": "https://asean-endocrinejournal.org/index.php/JAFES/article/view/1155",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "6244",
"original-title": [],
"page": "133-141",
"prefix": "10.15605",
"published": {
"date-parts": [
[
2021,
10,
30
]
]
},
"published-online": {
"date-parts": [
[
2021,
10,
30
]
]
},
"published-print": {
"date-parts": [
[
2021,
11,
26
]
]
},
"publisher": "Journal of the ASEAN Federation of Endocrine Societies (JAFES)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"score": 1,
"short-container-title": [
"JAFES"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": [
"Association Between Metformin Use and Mortality Among Patients with Type 2 Diabetes Mellitus Hospitalized for COVID-19 Infection"
],
"type": "journal-article",
"volume": "36"
}
