Metformin is associated with favorable outcomes in patients with COVID-19 and type 2 diabetes mellitus
et al., Scientific Reports, doi:10.1038/s41598-022-09639-2, Apr 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
PSM/IPTW retrospective 1,356 hospitalized COVID-19 patients with type 2 diabetes in China, showing lower mortality/hospice with metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 74.2% lower, RR 0.26, p = 0.03, treatment 3 of 361 (0.8%), control 40 of 995 (4.0%), NNT 31, odds ratio converted to relative risk, in-hospital death or hospice, propensity score weighting.
|
|
risk of mechanical ventilation, 25.0% lower, RR 0.75, p = 0.44, treatment 12 of 360 (3.3%), control 16 of 360 (4.4%), NNT 90, propensity score matching.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ma et al., 1 Apr 2022, retrospective, USA, peer-reviewed, 4 authors, study period 16 March, 2020 - 15 February, 2021.
Contact: mahesh.krishnamurthy@sluhn.org.
Metformin is associated with favorable outcomes in patients with COVID-19 and type 2 diabetes mellitus
Scientific Reports, doi:10.1038/s41598-022-09639-2
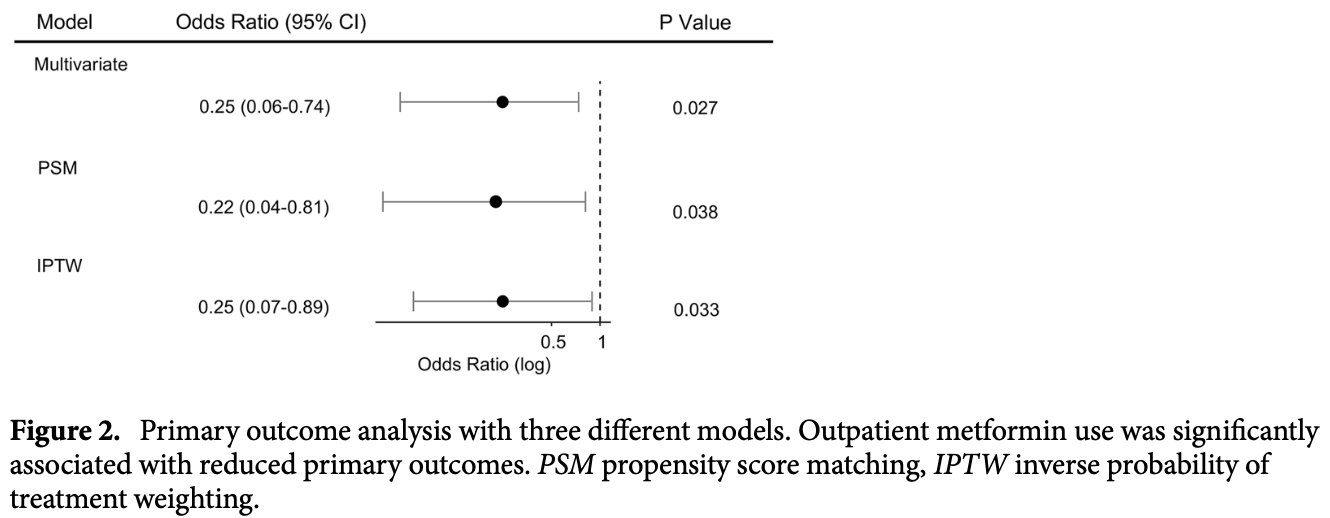
Coronavirus disease 2019 (COVID-19 ) is a new pandemic the entire world is facing since December of 2019. Several risk factors are identified in developing severe disease and one of which is preexisting type 2 diabetes mellitus. Metformin is known to have host-directed anti-viral and anti-inflammatory properties. However, whether these effects offer lower mortality remains unclear. In this retrospective study, we aim to address whether metformin use prior to admission decreases mortality in patients with COVID-19 and pre-existing type 2 diabetes mellitus. A total of 1356 hospitalized patients with COVID-19 and pre-existing type 2 diabetes mellitus was analyzed by multivariable regression. Covariates that potentially confound the association were further adjusted using propensity score matching or inverse probability of treatment weighting. We found that metformin therapy prior to admission in patients with COVID-19 and type 2 diabetes mellitus was significantly associated with less primary outcome events including in-hospital mortality and hospice care enrollment with an odds ratio (OR) of 0.25 (95% CI 0.06-0.74) and less in-hospital length of stay, compared to the nonmetformin group. Our results provide supporting evidence that metformin may confer increased survival in patients with COVID-19 and type 2 diabetes mellitus treated with metformin prior to hospitalization. Rapid outbreak and spread of coronavirus disease 2019 (COVID-19), caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), leads to a global health crisis [1] [2] [3] [4] [5] . Risk factors and comorbidities linked to worse outcomes for COVID-19 patients have been identified. These include old age 5 , chronic pulmonary disease and smoking 6 , cardiovascular disease 6 , hypertension 7 , diabetes mellitus and obesity 8 . Patients with pre-existing diabetes mellitus, depending on nations and patient cohorts, have been reported to account for patients with COVID-19 from 5 to 20% in China, 17% in Lombardy in Italy to 33% in the US 1-5 . Diabetic patients hospitalized with COVID-19 are two-to three-fold more likely to be admitted into intensive care units than that of non-diabetics and the mortality rate is at least doubled 6,9-11 , suggesting urgent need for effective treatments in patients with COVID-19 and diabetes mellitus. Metformin is widely used as the first-line therapy for type 2 diabetes mellitus 12 . Metformin is effective, safe, and inexpensive and may reduce the risk for cardiovascular events and death in type 2 diabetes mellitus 13 . Historically, because of its host-directed anti-viral properties, metformin was used during the treatment of influenza outbreak 14 . Likewise, based on the pathogenesis of SARS-CoV-2, several mechanisms have been speculated about the possible beneficial effects of metformin in COVID-19 patients with pre-existing type 2 diabetes mellitus, such as anti-inflammatory effects 15 , reduction in neutrophils 16 , increasing..
Author contributions Z.M. and M.K. designed the study and wrote the manuscript. Z.M., N.P., and P.V. collected the data. Z.M. performed and analyzed data. M.K. reviewed data. All authors reviewed the results and approved the final version of the manuscript.
Competing interests The authors declare no competing interests.
References
Bramante, Metformin and risk of mortality in patients hospitalised with COVID-19: A retrospective cohort analysis, Lancet Healthy Longev, doi:10.1016/S2666-7568(20)30033-7
Bramante, Outpatient metformin use is associated with reduced severity of COVID-19 disease in adults with overweight or obesity, J. Med. Virol, doi:10.1002/jmv.26873
Cameron, Anti-inflammatory effects of metformin irrespective of diabetes status, Circ. Res, doi:10.1161/CIRCRESAHA.116.308445
Cariou, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: The CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Chen, Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care, doi:10.2337/dc20-0660
Cheng, Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and pre-existing type 2 diabetes, Cell. Metab, doi:10.1016/j.cmet.2020.08.013
Crouse, Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes, Front Endocrinol, doi:10.3389/fendo.2020.600439
Cummings, Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study, Lancet, doi:10.1016/S0140-6736(20)31189-2
Dalan, Metformin, neutrophils and COVID-19 infection, Diabetes Res. Clin. Pract, doi:10.1016/j.diabres.2020.108230
Diabetes, Promoting health and reducing disparities in populations, Diabetes Care, doi:10.2337/dc17-S004
Esam, A proposed mechanism for the possible therapeutic potential of Metformin in COVID-19, Diabetes Res. Clin. Pract, doi:10.1016/j.diabres.2020.108282
Garcia, Flumamine, a new synthetic analgesic and anti-flu drug, J. Philipp. Med. Assoc
Grasselli, Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, JAMA, doi:10.1001/jama.2020.5394
Guan, Clinical characteristics of coronavirus disease 2019 in China, N. Engl. J. Med, doi:10.1056/NEJMoa2002032
Guan, Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis, Eur. Respir. J, doi:10.1183/13993003.00547-2020
Holman, Paul, Bethel, Matthews, Neil, 10-year follow-up of intensive glucose control in type 2 diabetes, N. Engl. J. Med, doi:10.1056/NEJMoa0806470
Huang, Lim, Pranata, Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia: A systematic review, meta-analysis, and meta-regression, Diabetes Metab. Syndr, doi:10.1016/j.dsx.2020.04.018
Lighter, Obesity in patients younger than 60 years is a risk factor for COVID-19 hospital admission, Clin. Infect. Dis, doi:10.1093/cid/ciaa415
Luo, Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am. J. Trop. Med. Hyg, doi:10.4269/ajtmh.20-0375
Roncon, Zuin, Rigatelli, Zuliani, Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome, J. Clin. Virol, doi:10.1016/j.jcv.2020.104354
Siddiqi, Mehra, COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal, J. Heart Lung. Transplant, doi:10.1016/j.healun.2020.03.012
Ursini, Ciaffi, Landini, Meliconi, COVID-19 and diabetes: Is metformin a friend or foe?, Diabetes Res. Clin. Pract, doi:10.1016/j.diabres.2020.108167
Ursini, Metformin and autoimmunity: A "new deal" of an old drug, Front Immunol, doi:10.3389/fimmu.2018.01236
Wu, Mcgoogan, Characteristics of and important lessons from the coronavirus disease, doi:10.1001/jama.2020.2648
Yang, Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A singlecentered, retrospective, observational study, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30079-5
Yang, Effect of hypertension on outcomes of adult inpatients with COVID-19 in Wuhan, China: A propensity scorematching analysis, Respir. Res, doi:10.1186/s12931-020-01435-8
Zhou, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
DOI record:
{
"DOI": "10.1038/s41598-022-09639-2",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-022-09639-2",
"abstract": "<jats:title>Abstract</jats:title><jats:p>Coronavirus disease 2019 (COVID-19) is a new pandemic the entire world is facing since December of 2019. Several risk factors are identified in developing severe disease and one of which is preexisting type 2 diabetes mellitus. Metformin is known to have host-directed anti-viral and anti-inflammatory properties. However, whether these effects offer lower mortality remains unclear. In this retrospective study, we aim to address whether metformin use prior to admission decreases mortality in patients with COVID-19 and pre-existing type 2 diabetes mellitus. A total of 1356 hospitalized patients with COVID-19 and pre-existing type 2 diabetes mellitus was analyzed by multivariable regression. Covariates that potentially confound the association were further adjusted using propensity score matching or inverse probability of treatment weighting. We found that metformin therapy prior to admission in patients with COVID-19 and type 2 diabetes mellitus was significantly associated with less primary outcome events including in-hospital mortality and hospice care enrollment with an odds ratio (OR) of 0.25 (95% CI 0.06–0.74) and less in-hospital length of stay, compared to the non-metformin group. Our results provide supporting evidence that metformin may confer increased survival in patients with COVID-19 and type 2 diabetes mellitus treated with metformin prior to hospitalization.</jats:p>",
"alternative-id": [
"9639"
],
"article-number": "5553",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "21 September 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "25 March 2022"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "1 April 2022"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Ma",
"given": "Zhiyuan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Patel",
"given": "Nishit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vemparala",
"given": "Pranathi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Krishnamurthy",
"given": "Mahesh",
"sequence": "additional"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2022,
4,
1
]
],
"date-time": "2022-04-01T14:26:56Z",
"timestamp": 1648823216000
},
"deposited": {
"date-parts": [
[
2022,
4,
1
]
],
"date-time": "2022-04-01T14:45:29Z",
"timestamp": 1648824329000
},
"indexed": {
"date-parts": [
[
2022,
8,
10
]
],
"date-time": "2022-08-10T09:05:49Z",
"timestamp": 1660122349922
},
"is-referenced-by-count": 2,
"issue": "1",
"issued": {
"date-parts": [
[
2022,
4,
1
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2022,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
4,
1
]
],
"date-time": "2022-04-01T00:00:00Z",
"timestamp": 1648771200000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
4,
1
]
],
"date-time": "2022-04-01T00:00:00Z",
"timestamp": 1648771200000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-022-09639-2.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-022-09639-2",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-022-09639-2.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2022,
4,
1
]
]
},
"published-online": {
"date-parts": [
[
2022,
4,
1
]
]
},
"published-print": {
"date-parts": [
[
2022,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1056/NEJMoa2002032",
"author": "WJ Guan",
"doi-asserted-by": "publisher",
"first-page": "1708",
"journal-title": "N. Engl. J. Med.",
"key": "9639_CR1",
"unstructured": "Guan, W. J. et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 382, 1708–1720. https://doi.org/10.1056/NEJMoa2002032 (2020).",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.2648",
"author": "Z Wu",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "9639_CR2",
"unstructured": "Wu, Z. & McGoogan, J. M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA https://doi.org/10.1001/jama.2020.2648 (2020).",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"author": "X Yang",
"doi-asserted-by": "publisher",
"first-page": "475",
"journal-title": "Lancet Respir. Med.",
"key": "9639_CR3",
"unstructured": "Yang, X. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 8, 475–481. https://doi.org/10.1016/S2213-2600(20)30079-5 (2020).",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)31189-2",
"author": "MJ Cummings",
"doi-asserted-by": "publisher",
"first-page": "1763",
"journal-title": "Lancet",
"key": "9639_CR4",
"unstructured": "Cummings, M. J. et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 395, 1763–1770. https://doi.org/10.1016/S0140-6736(20)31189-2 (2020).",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.5394",
"author": "G Grasselli",
"doi-asserted-by": "publisher",
"journal-title": "JAMA",
"key": "9639_CR5",
"unstructured": "Grasselli, G. et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA https://doi.org/10.1001/jama.2020.5394 (2020).",
"year": "2020"
},
{
"DOI": "10.1183/13993003.00547-2020",
"author": "WJ Guan",
"doi-asserted-by": "publisher",
"journal-title": "Eur. Respir. J.",
"key": "9639_CR6",
"unstructured": "Guan, W. J. et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur. Respir. J. https://doi.org/10.1183/13993003.00547-2020 (2020).",
"year": "2020"
},
{
"DOI": "10.1186/s12931-020-01435-8",
"author": "Q Yang",
"doi-asserted-by": "publisher",
"first-page": "172",
"journal-title": "Respir. Res.",
"key": "9639_CR7",
"unstructured": "Yang, Q. et al. Effect of hypertension on outcomes of adult inpatients with COVID-19 in Wuhan, China: A propensity score-matching analysis. Respir. Res. 21, 172. https://doi.org/10.1186/s12931-020-01435-8 (2020).",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa415",
"author": "J Lighter",
"doi-asserted-by": "publisher",
"first-page": "896",
"journal-title": "Clin. Infect. Dis.",
"key": "9639_CR8",
"unstructured": "Lighter, J. et al. Obesity in patients younger than 60 years is a risk factor for COVID-19 hospital admission. Clin. Infect. Dis. 71, 896–897. https://doi.org/10.1093/cid/ciaa415 (2020).",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"author": "F Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"journal-title": "Lancet",
"key": "9639_CR9",
"unstructured": "Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 395, 1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3 (2020).",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1016/j.jcv.2020.104354",
"author": "L Roncon",
"doi-asserted-by": "publisher",
"journal-title": "J. Clin. Virol.",
"key": "9639_CR10",
"unstructured": "Roncon, L., Zuin, M., Rigatelli, G. & Zuliani, G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J. Clin. Virol. 127, 104354. https://doi.org/10.1016/j.jcv.2020.104354 (2020).",
"volume": "127",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2020.04.018",
"author": "I Huang",
"doi-asserted-by": "publisher",
"first-page": "395",
"journal-title": "Diabetes Metab. Syndr.",
"key": "9639_CR11",
"unstructured": "Huang, I., Lim, M. A. & Pranata, R. Diabetes mellitus is associated with increased mortality and severity of disease in COVID-19 pneumonia: A systematic review, meta-analysis, and meta-regression. Diabetes Metab. Syndr. 14, 395–403. https://doi.org/10.1016/j.dsx.2020.04.018 (2020).",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.2337/dc17-S004",
"author": "American Diabetes",
"doi-asserted-by": "publisher",
"first-page": "6",
"journal-title": "Diabetes Care",
"key": "9639_CR12",
"unstructured": "American Diabetes. Promoting health and reducing disparities in populations. Diabetes Care 40, 6–10. https://doi.org/10.2337/dc17-S004 (2017).",
"volume": "40",
"year": "2017"
},
{
"DOI": "10.1056/NEJMoa0806470",
"author": "RR Holman",
"doi-asserted-by": "publisher",
"first-page": "1577",
"journal-title": "N. Engl. J. Med.",
"key": "9639_CR13",
"unstructured": "Holman, R. R., Paul, S. K., Bethel, M. A., Matthews, D. R. & Neil, H. A. 10-year follow-up of intensive glucose control in type 2 diabetes. N. Engl. J. Med. 359, 1577–1589. https://doi.org/10.1056/NEJMoa0806470 (2008).",
"volume": "359",
"year": "2008"
},
{
"author": "EY Garcia",
"first-page": "287",
"journal-title": "J. Philipp. Med. Assoc.",
"key": "9639_CR14",
"unstructured": "Garcia, E. Y. Flumamine, a new synthetic analgesic and anti-flu drug. J. Philipp. Med. Assoc. 26, 287–293 (1950).",
"volume": "26",
"year": "1950"
},
{
"DOI": "10.1161/CIRCRESAHA.116.308445",
"author": "AR Cameron",
"doi-asserted-by": "publisher",
"first-page": "652",
"journal-title": "Circ. Res.",
"key": "9639_CR15",
"unstructured": "Cameron, A. R. et al. Anti-inflammatory effects of metformin irrespective of diabetes status. Circ. Res. 119, 652–665. https://doi.org/10.1161/CIRCRESAHA.116.308445 (2016).",
"volume": "119",
"year": "2016"
},
{
"DOI": "10.1016/j.diabres.2020.108230",
"author": "R Dalan",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Res. Clin. Pract.",
"key": "9639_CR16",
"unstructured": "Dalan, R. Metformin, neutrophils and COVID-19 infection. Diabetes Res. Clin. Pract. 164, 108230. https://doi.org/10.1016/j.diabres.2020.108230 (2020).",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108282",
"doi-asserted-by": "publisher",
"key": "9639_CR17",
"unstructured": "Esam, Z. A proposed mechanism for the possible therapeutic potential of Metformin in COVID-19. Diabetes Res. Clin. Pract. 108282. doi:https://doi.org/10.1016/j.diabres.2020.108282 (2020)."
},
{
"DOI": "10.1016/j.diabres.2020.108167",
"author": "F Ursini",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Res. Clin. Pract.",
"key": "9639_CR18",
"unstructured": "Ursini, F., Ciaffi, J., Landini, M. P. & Meliconi, R. COVID-19 and diabetes: Is metformin a friend or foe?. Diabetes Res. Clin. Pract. 164, 108167. https://doi.org/10.1016/j.diabres.2020.108167 (2020).",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"author": "B Cariou",
"doi-asserted-by": "publisher",
"first-page": "1500",
"journal-title": "Diabetologia",
"key": "9639_CR19",
"unstructured": "Cariou, B. et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: The CORONADO study. Diabetologia 63, 1500–1515. https://doi.org/10.1007/s00125-020-05180-x (2020).",
"volume": "63",
"year": "2020"
},
{
"DOI": "10.2337/dc20-0660",
"author": "Y Chen",
"doi-asserted-by": "publisher",
"first-page": "1399",
"journal-title": "Diabetes Care",
"key": "9639_CR20",
"unstructured": "Chen, Y. et al. Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care 43, 1399–1407. https://doi.org/10.2337/dc20-0660 (2020).",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.3389/fendo.2020.600439",
"author": "AB Crouse",
"doi-asserted-by": "publisher",
"first-page": "600439",
"journal-title": "Front. Endocrinol.",
"key": "9639_CR21",
"unstructured": "Crouse, A. B. et al. (2020). Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes. Front Endocrinol 11, 600439, https://doi.org/10.3389/fendo.2020.600439",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/S2666-7568(20)30033-7",
"author": "CT Bramante",
"doi-asserted-by": "publisher",
"first-page": "e34",
"journal-title": "Lancet Healthy Longev.",
"key": "9639_CR22",
"unstructured": "Bramante, C. T. et al. Metformin and risk of mortality in patients hospitalised with COVID-19: A retrospective cohort analysis. Lancet Healthy Longev. 2, e34–e41. https://doi.org/10.1016/S2666-7568(20)30033-7 (2021).",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1002/jmv.26873",
"author": "CT Bramante",
"doi-asserted-by": "publisher",
"journal-title": "J. Med. Virol.",
"key": "9639_CR23",
"unstructured": "Bramante, C. T. et al. Outpatient metformin use is associated with reduced severity of COVID-19 disease in adults with overweight or obesity. J. Med. Virol. https://doi.org/10.1002/jmv.26873 (2021).",
"year": "2021"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"author": "P Luo",
"doi-asserted-by": "publisher",
"first-page": "69",
"journal-title": "Am. J. Trop. Med. Hyg.",
"key": "9639_CR24",
"unstructured": "Luo, P. et al. Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis. Am. J. Trop. Med. Hyg. 103, 69–72. https://doi.org/10.4269/ajtmh.20-0375 (2020).",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.08.013",
"author": "X Cheng",
"doi-asserted-by": "publisher",
"first-page": "537",
"journal-title": "Cell. Metab.",
"key": "9639_CR25",
"unstructured": "Cheng, X. et al. Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and pre-existing type 2 diabetes. Cell. Metab. 32, 537–547. https://doi.org/10.1016/j.cmet.2020.08.013 (2020).",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.1016/j.healun.2020.03.012",
"author": "HK Siddiqi",
"doi-asserted-by": "publisher",
"first-page": "405",
"journal-title": "J. Heart Lung. Transplant.",
"key": "9639_CR26",
"unstructured": "Siddiqi, H. K. & Mehra, M. R. COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal. J. Heart Lung. Transplant. 39, 405–407. https://doi.org/10.1016/j.healun.2020.03.012 (2020).",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.3389/fimmu.2018.01236",
"author": "F Ursini",
"doi-asserted-by": "publisher",
"first-page": "1236",
"journal-title": "Front Immunol.",
"key": "9639_CR27",
"unstructured": "Ursini, F. et al. Metformin and autoimmunity: A “new deal” of an old drug. Front Immunol. 9, 1236. https://doi.org/10.3389/fimmu.2018.01236 (2018).",
"volume": "9",
"year": "2018"
}
],
"reference-count": 27,
"references-count": 27,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-022-09639-2"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": "Metformin is associated with favorable outcomes in patients with COVID-19 and type 2 diabetes mellitus",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "12"
}
