Association between prior cardiometabolic therapy and in-hospital mortality in very old patients with type 2 diabetes mellitus hospitalized due to COVID-19. A nationwide observational study in Spain
et al., Research Square, doi:10.21203/rs.3.rs-133358/v1, Dec 2020
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 790 hospitalized type 2 diabetes patients ≥80 years old in Spain, showing no significant difference in mortality with existing metformin use.
Study covers aspirin and metformin.
|
risk of death, 1.3% lower, RR 0.99, p = 0.78, treatment 206 of 420 (49.0%), control 179 of 370 (48.4%), adjusted per study, odds ratio converted to relative risk, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ramos-Rincón et al., 28 Dec 2020, retrospective, Spain, preprint, 25 authors, study period 1 March, 2020 - 29 May, 2020.
Contact: luismiguelpb1984@gmail.com.
Association between prior cardiometabolic therapy and in-hospital mortality in very old patients with type 2 diabetes mellitus hospitalized due to COVID-19. A nationwide observational study in Spain
doi:10.21203/rs.3.rs-133358/v1
Background Advanced age and diabetes are both associated with poor prognosis in COVID-19. However, the effects of cardiometabolic drugs on the prognosis of diabetic patients with COVID-19, especially very old patients, are not well-known. This work aims to analyze the association between preadmission cardiometabolic therapy (antidiabetic, antiaggregant, antihypertensive, and lipid-lowering drugs) and in-hospital mortality among patients ≥ 80 years with type 2 diabetes mellitus hospitalized for COVID-19.
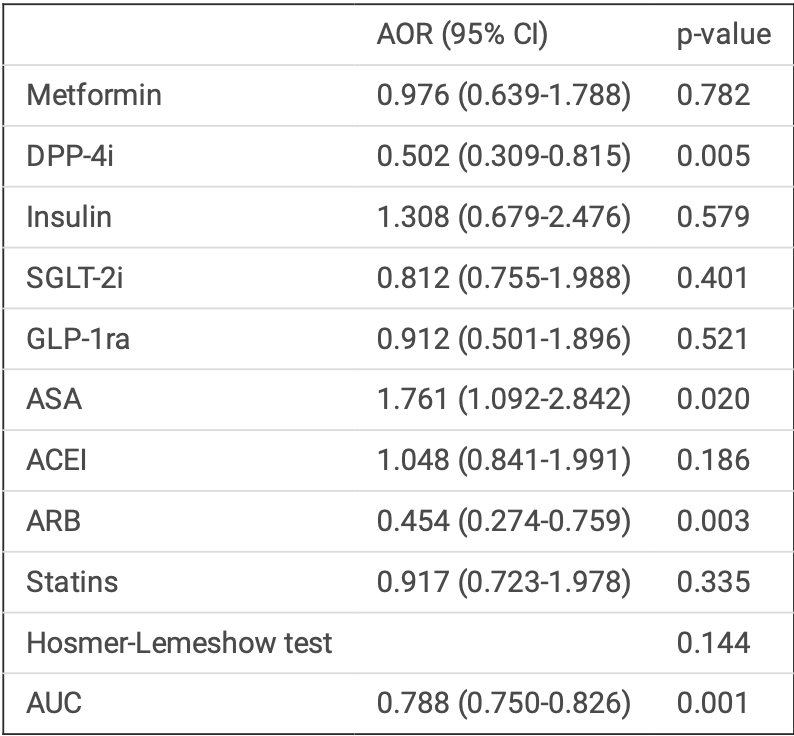
Methods We conducted a nationwide, multicenter, retrospective, observational study in patients ≥ 80 years with type 2 diabetes mellitus and COVID-19 hospitalized in 160 Spanish hospitals between March 1 and May 29, 2020 who were included in the SEMI-COVID-19 Registry. The primary outcome measure was inhospital mortality. A multivariate logistic regression analysis were performed to assess the association between preadmission cardiometabolic therapy and in-hospital mortality. The regression analysis values were expressed as adjusted odds ratios (AOR) with a 95% con dence interval (CI). In order to select the variables, the forward selection Wald statistic was used. Discrimination of the tted logistic model was assessed via a receiver operating characteristic (ROC) curve. The Hosmer-Lemeshow test for logistic regression was used to determine the model's goodness of t.
Declarations Ethics approval and consent to participate gave their informed consent. When there were biosafety concerns and/or when the patient had already been discharged, verbal informed consent was requested and noted on the medical record. Data con dentiality and patient anonymity were maintained at all times, in accordance with Spanish regulations on observational studies. This study was carried out in accordance with the Declaration of Helsinki and was approved by the Institutional Research Ethics Committee of Málaga on March 27, 2020 (Ethics Committe code: SEMI-COVID-19 27-03-20), as per the guidelines of the Spanish Agency of Medicines and Medical Products.
Consent for publication Not applicable.
Competing interest The authors declare that they have no competing interests. Authors' contributions JMRR contributed to the conception, design of the work the acquisition, interpretation of data, writingoriginal draft preparation, writing-review and editing, and supervision. FJCS, SJC, MDSB, JBF, MPA, CAC, MBC, MMB, IFM, AGG, FNR, CTA, GMN, AGN, AHM, GMGG, JNAP, VHG, LCG, PCC, HMM, and JMCR made contributions to the acquisition of data and revised the work. LMPB contributed to interpretation of data, writing-review and editing, and supervision. RGH was a major contributor in interpretation of data, writingoriginal draft preparation, writing-review and editing, and supervision. All authors read and approved the nal manuscript.
Supplementary Files This is a list of..
References
Alghatrif, Cingolani, Lakatta, The dilemma of coronavirus disease 2019, aging, and cardiovascular disease: insights from cardiovascular aging science, JAMA Cardiol
Apicella, Campopiano, Mantuano, Mazoni, Coppelli et al., COVID-19 in people with diabetes: understanding the reasons for worse outcomes, Lancet Diabetes Endocrinol
Baral, White, Vassiliou, Effect of Renin-Angiotensin-Aldosterone System inhibitors in patients with COVID-19: a systematic review and meta-analysis of 28,872 patients, Curr Atheroscler Rep
Baral, White, Vassiliou, Effect of renin-angiotensin-aldosterone system inhibitors in patients with COVID-19: a systematic review and meta-analysis of 28,872 patients, Curr Atheroscler Rep
Bornstein, Rubino, Khunti, Mingrone, Hopkins et al., Practical recommendations for the management of diabetes in patients with COVID-19, Lancet Diabetes Endocrinol
Bramante, Ingraham, Murray, Marmor, Hoversten et al., Observational study of metformin and risk of mortality in patients hospitalized with Covid-19, medRxiv
Casas Rojo, Santos, Núñez-Cortés, Lumbreras-Bermejo, Ramos-Rincón et al., Clinical characteristics of patients hospitalized with COVID-19 in Spain: results from the SEMI-COVID-19 Registry, Rev Clin Esp
Chen, Yang, Cheng, Chen, Peng et al., Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care
Chow, Khanna, Kethireddy, Yamane, Levine et al., Aspirin use is associated with decreased mechanical ventilation, ICU admission, and in-hospital mortality in hospitalized patients with COVID-19, Anesth Analg
Cunha, Perazzio, Azzi, Cravedi, Riella, Remodeling of the immune response with aging: immunosenescence and its potential impact on COVID-19 immune response, Front Immunol
Daniels, Sitapati, Zhang, Zou, Bui et al., Relation of statin use prior to admission to severity and recovery among COVID-19 inpatients, Am J Cardiol
Detel, Baticic, Varljen, The in uence of age on intestinal dipeptidyl peptidase IV (DPP IV/CD26), disaccharidases, and alkaline phosphatase enzyme activity in C57BL/6 mice, Exp Aging Res
Docherty, Harrison, Green, Hardwick, Pius et al., DPP-4i: dipeptidyl peptidase-4 inhibitors eGFR: estimated glomerular ltration rate GLP-1ra: glucagon-like peptide-1 receptor agonist IQR: interquartile ranges qSOFA: quick sequential organ failure assessment ROC: receiver operating characteristic RT-PCR: reverse transcription polymerase chain reaction SARS-CoV-2: severe acute respiratory syndrome coronavirus 2 SGLT-2i: sodium-glucose cotransporter 2 inhibitors SEMI (for its initials in Spanish): Spanish Society of Internal Medicine T2DM: type 2 diabetes mellitus References, BMJ
Drucker, Coronavirus infections and type 2 diabetes-shared pathways with therapeutic implications, Endocr Rev
Fadini, Morieri, Longato, Avogaro, Prevalence and impact of diabetes among people infected with SARS-CoV-2, J Endocrinol Invest
Fang, Karakiulakis, Roth, Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?, Lancet Respir Med
Fosbøl, Butt, Østergaard, Andersson, Selmer et al., Association of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with COVID-19 diagnosis and mortality, JAMA
Furuhashi, Moniwa, Mita, Fuseya, Ishimura et al., Urinary angiotensin-converting enzyme 2 in hypertensive patients may be increased by olmesartan, an angiotensin II receptor blocker, Am J Hypertens
Iaccarino, Grassi, Borghi, Ferri, Salvetti et al., Age and Multimorbidity Predict Death Among COVID-19 Patients: Results of the SARS-RAS Study of the Italian Society of Hypertension, Hypertension
Iacobellis, COVID-19 and diabetes: can DPP4 inhibition play a role?, Diabetes Res Clin Pract
Jia, Pulmonary angiotensin-converting enzyme 2 (ACE2) and in ammatory lung disease, Shock
Kim, Noh, Bodogai, Martindale, Yang et al., Identi cation of senescent cell surface targetable protein DPP4, Genes Dev
Kow, Hasan, Meta-analysis of effect of statins in patients with COVID-19, Am J Cardiol
Kow, Hasan, Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis, J Med Virol
Kuba, Imai, Rao, Gao, Guo et al., A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury, Nat Med
Lamontagne, Agoritsas, Macdonald, Leo, Diaz et al., A living WHO guideline on drugs for covid-19, BMJ
Lee, Sewa, Phua, Potential role of statins in COVID-19, Int J Infect Dis
Li, Zhang, Yang, Lian, Xie et al., The MERS-CoV receptor DPP4 as a candidate binding target of the SARS-CoV-2 spike, iScience
Loomans-Kropp, Pinsky, Cao, Chan, Umar, Association of aspirin use with mortality risk among older adult participants in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial, JAMA Netw Open
Makdissi, Ghanim, Vora, Green, Abuaysheh et al., Sitagliptin exerts an antin ammatory action, J Clin Endocrinol Metab
Mancia, Rea, Ludergnani, Apolone, Corrao, Renin-Angiotensin-Aldosterone System Blockers and the risk of Covid-19, N Engl J Med
Mcneil, Nelson, Woods, Lockery, Wolfe et al., Effect of aspirin on all-cause mortality in the healthy elderly, N Engl J Med
Omar, Vikman, Winzell, Voss, Ekblad et al., Enhanced beta cell function and anti-in ammatory effect after chronic treatment with the dipeptidyl peptidase-4 inhibitor vildagliptin in an advanced-aged diet-induced obesity mouse model, Diabetologia
Patel, Baliga, Role of aspirin for primary prevention in persons with diabetes mellitus and in the elderly, Cardiol Rep
Petrilli, Jones, Yang, Rajagopalan, Donnell et al., Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ
Pinheiro, Stoppa, Valduga, Okuyama, Gorjão et al., Sitagliptin inhibit human lymphocytes proliferation and Th1/Th17 differentiation in vitro, Eur J Pharm Sci
Pérez-Belmonte, Torres-Peña, López-Carmona, Ayala-Gutiérrez, Fuentes-Jiménez et al., -COVID-19 Network. Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: a nationwide cohort study, BMC Medicine
Ramos-Rincon, Buonaiuto, Ricci, Martín-Carmona, Paredes-Ruíz et al., Clinical characteristics and risk factors for mortality in very old patients hospitalized with COVID-19 in Spain, J Gerontol A Biol Sci Med Sci
Reiner, Hatamipour, Banach, Pirro, Rasadi et al., Statins and the COVID-19 main protease: in silico evidence on direct interaction, Arch Med Sci
Rhee, Lee, Nam, Kyoung, Kim, Effects of a DPP-4 inhibitor and RAS blockade on clinical outcomes of patients with diabetes and COVID-19, medRxiv
Rodilla, Saura, Jiménez, Mendizábal, Pineda-Cantero et al., Association of hypertension with all-cause mortality among hospitalized patients with COVID-19, J Clin Med
Saavedra, Angiotensin receptor blockers and COVID-19, Pharmacol Res
Saeed, Castagna, Agalliu, Xue, Patel et al., Statin Use and In-Hospital Mortality in Diabetics with COVID-19, J Am Heart Assoc
Solerte, 'addio, Trevisan, Lovati, Rossi et al., Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and COVID-19: a multicenter, case-control, retrospective, observational study, Diabetes Care
Solerte, Sabatino, Galli, Fiorina, Dipeptidyl peptidase-4 (DPP4) inhibition in COVID-19, Acta Diabetol
Strollo, Pozzilli, DPP4 inhibition: preventing SARS-CoV-2 infection and/or progression of COVID-19?, Diabetes Metab Res Rev
Yan, Zhang, Li, Xia, Guo et al., Structural basis for the recognition of SARS-CoV-2 by fulllength human ACE2, Science
Yang, Zheng, Gou, Pu, Chen et al., Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis, Int J Infect Dis
Yu, Li, Sun, Wang, Insulin treatment is associated with increased mortality in patients with COVID-19 and type 2 diabetes, Cell Metab
DOI record:
{
"DOI": "10.21203/rs.3.rs-133358/v1",
"URL": "http://dx.doi.org/10.21203/rs.3.rs-133358/v1",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p>Background\n\nAdvanced age and diabetes are both associated with poor prognosis in COVID-19. However, the effects of cardiometabolic drugs on the prognosis of diabetic patients with COVID-19, especially very old patients, are not well-known. This work aims to analyze the association between preadmission cardiometabolic therapy (antidiabetic, antiaggregant, antihypertensive, and lipid-lowering drugs) and in-hospital mortality among patients ≥ 80 years with type 2 diabetes mellitus hospitalized for COVID-19.\nMethods\n\nWe conducted a nationwide, multicenter, retrospective, observational study in patients ≥ 80 years with type 2 diabetes mellitus and COVID-19 hospitalized in 160 Spanish hospitals between March 1 and May 29, 2020 who were included in the SEMI-COVID-19 Registry. The primary outcome measure was in-hospital mortality. A multivariate logistic regression analysis were performed to assess the association between preadmission cardiometabolic therapy and in-hospital mortality. The regression analysis values were expressed as adjusted odds ratios (AOR) with a 95% confidence interval (CI). In order to select the variables, the forward selection Wald statistic was used. Discrimination of the fitted logistic model was assessed via a receiver operating characteristic (ROC) curve. The Hosmer-Lemeshow test for logistic regression was used to determine the model’s goodness of fit.\nResults\n\nOf the 2,763 patients ≥80 years old hospitalized due to COVID-19, 790 (28.6%) had T2DM. Of these patients, 385 (48.7%) died during admission. On the multivariate analysis, the use of dipeptidyl peptidase-4 inhibitors (AOR 0.502, 95% CI 0.309–0.815, p = 0.005) and angiotensin receptor blockers (AOR 0.454, 95% CI 0.274–0.759, p = 0.003) were independent protectors against in-hospital mortality whereas the use of acetylsalicylic acid was associated with higher in-hospital mortality (AOR 1.761, 95% CI 1.092–2.842, p = 0.020). Other antidiabetic drugs, angiotensin-converting enzyme inhibitors and statins showed neutral association with in-hospital mortality. The model showed an area under the curve of 0.788.\nConclusions\n\nWe found important differences between cardiometabolic drugs and in-hospital mortality in older patients with type 2 diabetes mellitus hospitalized for COVID-19. Preadmission treatment with dipeptidyl peptidase-4 inhibitors and angiotensin receptor blockers may reduce in-hospital mortality; other antidiabetic drugs, angiotensin-converting enzyme inhibitors and statins seem to have a neutral effect; and acetylsalicylic acid may be associated with excess mortality.</jats:p>",
"accepted": {
"date-parts": [
[
2020,
12,
21
]
]
},
"author": [
{
"affiliation": [
{
"name": "Miguel Hernandez University of Elche: Universidad Miguel Hernandez de Elche"
}
],
"family": "Ramos-Rincón",
"given": "Jose Manuel",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0001-9512-8274",
"affiliation": [
{
"name": "Hospital Regional Universitario de Málaga: Hospital Regional Universitario de Malaga"
}
],
"authenticated-orcid": false,
"family": "Pérez-Belmonte",
"given": "Luis M",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Juan Ramón Jiménez: Hospital Juan Ramon Jimenez"
}
],
"family": "Carrasco-Sánchez",
"given": "Francisco Javier",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Regional Universitario de Málaga: Hospital Regional Universitario de Malaga"
}
],
"family": "Jansen-Chaparro",
"given": "Sergio",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Juan Ramón Jiménez: Hospital Juan Ramon Jimenez"
}
],
"family": "De-Sousa-Baena",
"given": "Mercedes",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Regional Universitario de Málaga: Hospital Regional Universitario de Malaga"
}
],
"family": "Bueno-Fonseca",
"given": "José",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Juan Ramón Jiménez: Hospital Juan Ramon Jimenez"
}
],
"family": "Pérez-Aguilar",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital 12 de Octubre Servicio de Medicina Interna"
}
],
"family": "Cañas",
"given": "Coral Arévalo",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital General Universitario Gregorio Marañón: Hospital General Universitario Gregorio Maranon"
}
],
"family": "Cebrian",
"given": "Marta Bacete",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "San Carlos University Hospital Internal Medicine III Service: Hospital Clinico Universitario San Carlos Servicio de Medicina Interna III"
}
],
"family": "Méndez-Bailón",
"given": "Manuel",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Royo Villanova Hospital: Hospital Royo Villanova"
}
],
"family": "Mera",
"given": "Isabel Fiteni",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Ramon y Cajal: Hospital Universitario Ramon y Cajal"
}
],
"family": "García",
"given": "Andrés González",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Costa del Sol"
}
],
"family": "Romero",
"given": "Francisco Navarro",
"sequence": "additional"
},
{
"affiliation": [
{
"name": ": Complejo Asistencial de Zamora"
}
],
"family": "Almeida",
"given": "Carlota Tuñón de",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Virgen de la Salud"
}
],
"family": "Nicolás",
"given": "Gemma Muñiz",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Complejo Hospitalario de Orense: Complexo Hospitalario de Ourense"
}
],
"family": "Noya",
"given": "Amara González",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Universitario Son Espases: Hospital Universitari Son Espases"
}
],
"family": "Milian",
"given": "Almudena Hernández",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Complejo Hospitalario Universitario de Badajoz"
}
],
"family": "García",
"given": "Gema María García",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "VS Hospital"
}
],
"family": "Pedrajas",
"given": "José Nicolás Alcalá",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Doctor Jose Molina Orosa"
}
],
"family": "García",
"given": "Virginia Herrero",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Universitario Rio Hortega"
}
],
"family": "Corral-Gudino",
"given": "Luis",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital de Blanes"
}
],
"family": "Casanova",
"given": "Pere Comas",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital QuironSalud A Coruña"
}
],
"family": "Míguez",
"given": "Héctor Meijide",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Hospital Universitario Infanta Cristina"
}
],
"family": "Casas-Rojo",
"given": "José Manuel",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Regional University Hospital of Malaga: Hospital Regional Universitario de Malaga"
}
],
"family": "Gómez-Huelgas",
"given": "Ricardo",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
12,
28
]
],
"date-time": "2020-12-28T21:58:47Z",
"timestamp": 1609192727000
},
"deposited": {
"date-parts": [
[
2021,
3,
17
]
],
"date-time": "2021-03-17T17:11:49Z",
"timestamp": 1616001109000
},
"group-title": "In Review",
"indexed": {
"date-parts": [
[
2022,
4,
5
]
],
"date-time": "2022-04-05T14:34:08Z",
"timestamp": 1649169248491
},
"institution": [
{
"name": "Research Square"
}
],
"is-referenced-by-count": 1,
"issued": {
"date-parts": [
[
2020,
12,
28
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2020,
12,
28
]
],
"date-time": "2020-12-28T00:00:00Z",
"timestamp": 1609113600000
}
}
],
"link": [
{
"URL": "https://www.researchsquare.com/article/rs-133358/v1",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.researchsquare.com/article/rs-133358/v1.html",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "8761",
"original-title": [],
"posted": {
"date-parts": [
[
2020,
12,
28
]
]
},
"prefix": "10.21203",
"published": {
"date-parts": [
[
2020,
12,
28
]
]
},
"publisher": "Research Square Platform LLC",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.researchsquare.com/article/rs-133358/v1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Association between prior cardiometabolic therapy and in-hospital mortality in very old patients with type 2 diabetes mellitus hospitalized due to COVID-19. A nationwide observational study in Spain",
"type": "posted-content"
}
