Preadmission usage of metformin and mortality in COVID-19 patients including the post-discharge period
et al., Irish Journal of Medical Science, doi:10.1007/s11845-021-02823-9, Oct 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 586 diabetic hospitalized COVID-19 patients in Turkey, showing lower mortality with existing metformin use.
|
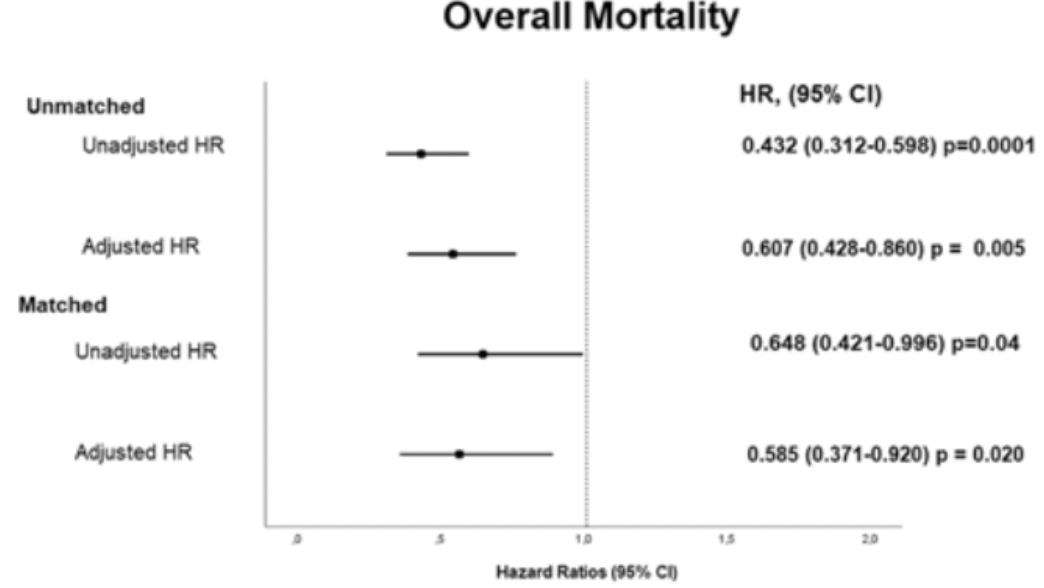
risk of death, 41.5% lower, RR 0.58, p = 0.02, treatment 120, control 120, overall mortality, Cox regression in matched group, propensity score matching.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Saygili et al., 29 Oct 2021, retrospective, Turkey, peer-reviewed, 5 authors.
Preadmission usage of metformin and mortality in COVID-19 patients including the post-discharge period
Irish Journal of Medical Science (1971 -), doi:10.1007/s11845-021-02823-9
Background The effect of preadmission metformin usage (PMU) on the mortality of coronavirus disease-2019 (COVID-19) patients with diabetes is conflicting. Most studies have focused on in-hospital mortality; however, mortality after discharge also increases in COVID-19 patients. Aims Examining the effect of PMU on all-cause mortality, including the post-discharge period. Methods Patients with diabetes who were hospitalised in 2020 due to COVID-19 were included in the study. They were divided into two groups: those with a history of metformin use (MF( +)) and those without such history (MF( −)). Propensity score matching (PSM) was performed at a ratio of 1:1 for age and sex. COX regression analyses were used to demonstrate risk factors for mortality.
Results We investigated 4103 patients hospitalised for COVID-19. After excluding those without diabetes or with chronic liver/kidney disease, we included the remaining 586 patients, constituting 293 women (50%) with an overall mean age of 66 ± 11.9 years. After PSM analysis, the in-hospital and post-discharge mortality rates were higher in the MF( −) group though not significantly different. However, overall mortality was higher in the MF( −) group (51 (42.5%) vs. 35 (29.2%), p = 0.031). For overall mortality, the adjusted HR was 0.585 (95% CI: 0.371 − 0.920, p = 0.020) in the MF( +) group. Conclusion PMU is associated with reducing all-cause mortality. This effect starts from the in-hospital period and becomes more significant with the post-discharge period. The main limitations were the inability to evaluate the compliance with metformin and the effects of other medications due to retrospective nature.
Declarations Ethics approval The study was approved by the Local Ethics Committee of the Canakkale Onsekiz Mart University Medical School (2011-KAEK-27/2021-E.2100041806).
Conflict of interest The authors declare no competing interests. Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Apicella, Campopiano, Mantuano, COVID-19 in people with diabetes: understanding the reasons for worse outcomes, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30238-2
Avogaro, Bonora, Fadini, Managing diabetes in diabetic patients with COVID: where do we start from? Acta Diabetol, doi:10.1007/s00592-021-01739-1
Ayoubkhani, Khunti, Nafilyan, Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study, BMJ, doi:10.1136/bmj.n693
Bailey, Metformin: historical overview, Diabetologia, doi:10.1007/s00125-017-4318-z
Barron, Bakhai, Kar, Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30272-2
Ceriello, Stoian, Rizzo, COVID-19 and diabetes management: what should be considered?, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2020.108151
Chen, Gu, Guan, Metformin might inhibit virus through increasing insulin sensitivity, Chin Med J (Engl), doi:10.4103/0366-6999.223856
Chen, Yang, Cheng, Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care, doi:10.2337/dc20-0660
Cheng, Liu, Li, Metformin is associated with higher incidence of acidosis, but not mortalitY, in individuals with COVID-19 and pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.08.013
Dave, Tamuhla, Tiffin, Risk factors for COVID-19 hospitalisation and death in people living with diabetes: a virtual cohort study from the Western Cape Province South Africa Diabetes, Res Clin Pract, doi:10.1016/j.diabres.2021.108925
Do, Kim, Park, Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19?, Diabetes Metab, doi:10.1016/j.diabet.2020.10.006
Donnelly, Wang, Iwashyna, Prescott, Readmission and death after initial hospital discharge among patients with COVID-19 in a large multihospital system, JAMA, doi:10.1001/jama.2020.21465
Ghany, Palacio, Dawkins, Metformin is associated with lower hospitalisations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA, Diabetes Metab Syndr Clin Res Rev, doi:10.1016/j.dsx.2021.02.022
Guo, Li, Dong, Diabetes is a risk factor for the progression and prognosis of COVID -19, Diabetes Metab Res Rev, doi:10.1002/dmrr.3319
Hariyanto, Kurniawan, Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection, Obes Med, doi:10.1016/j.obmed.2020.100290
Ho, Huang, Tsai, Metformin use mitigates the adverse prognostic effect of diabetes mellitus in chronic obstructive pulmonary disease, Respir Res, doi:10.1186/s12931-019-1035-9
Kajiwara, Kusaka, Kimura, Metformin mediates protection against Legionella pneumonia through activation of AMPK and mitochondrial reactive oxygen species, J Immunol, doi:10.4049/jimmunol.1700474
Khunti, Knighton, Zaccardi, Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00050-4
Kow, Hasan, Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: a metaanalysis, J Med Virol, doi:10.1002/jmv.26498
Levey, Stevens, Schmid, A new equation to estimate glomerular filtration rate, Ann Intern Med, doi:10.7326/0003-4819-150-9-200905050-00006
Liang, Ding, Li, Association of preadmission metformin use and mortality in patients with sepsis and diabetes mellitus: a systematic review and meta-analysis of cohort studies, Crit Care, doi:10.1186/s13054-019-2346-4
Lukito, Pranata, Henrina, The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr Clin Res Rev, doi:10.1016/j.dsx.2020.11.006
Luo, Qiu, Liu, Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am J Trop Med Hyg, doi:10.4269/ajtmh.20-0375
Medetalibeyoglu, Catma, Senkal, The effect of liver test abnormalities on the prognosis of COVID-19, Ann Hepatol, doi:10.1016/j.aohep.2020.08.068
Mendy, Gopal, Alcorn, Forno, Reduced mortality from lower respiratory tract disease in adult diabetic patients treated with metformin, Respirology, doi:10.1111/resp.13486
Mortensen, Anzueto, Association of metformin and mortality for patients with diabetes who are hospitalised with pneumonia
Salık, Uzundere, Bıçak, Liver function as a predictor of mortality in COVID-19 Retrospective study, Ann Hepatol, doi:10.1016/j.aohep.2021.100553
Wang, Cooper, Gokhale, Association of metformin with susceptibility to COVID-19 in people with type 2 diabetes, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab067
Wu, Keet, Fawzy, Association of metformin initiation and risk of asthma exacerbation A claims-based cohort study, Ann Am Thorac Soc, doi:10.1513/AnnalsATS.201812-897OC
Zangiabadian, Nejadghaderi, Zahmatkesh, The efficacy and potential mechanisms of metformin in the treatment of COVID-19 in the diabetics: a systematic review Front, Endocrinol, doi:10.3389/fendo.2021.645194
Zhang, He, Impacts of metformin on tuberculosis incidence and clinical outcomes in patients with diabetes: a systematic review and meta-analysis, Eur J Clin Pharmacol, doi:10.1007/s00228-019-02786-y
DOI record:
{
"DOI": "10.1007/s11845-021-02823-9",
"ISSN": [
"0021-1265",
"1863-4362"
],
"URL": "http://dx.doi.org/10.1007/s11845-021-02823-9",
"alternative-id": [
"2823"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "24 September 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "21 October 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "29 October 2021"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The study was approved by the Local Ethics Committee of the Canakkale Onsekiz Mart University Medical School (2011-KAEK-27/2021-E.2100041806)."
},
{
"group": {
"label": "Conflict of interest",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "The authors declare no competing interests."
},
{
"label": "Free to read",
"name": "free",
"value": "This content has been made available to all."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-0022-5704",
"affiliation": [],
"authenticated-orcid": false,
"family": "Saygili",
"given": "Emre Sedar",
"sequence": "first"
},
{
"affiliation": [],
"family": "Karakiliç",
"given": "Ersen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mert",
"given": "Erdal",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Şener",
"given": "Alper",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mirci",
"given": "Arzu",
"sequence": "additional"
}
],
"container-title": [
"Irish Journal of Medical Science (1971 -)"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
10,
29
]
],
"date-time": "2021-10-29T01:02:19Z",
"timestamp": 1635469339000
},
"deposited": {
"date-parts": [
[
2021,
10,
29
]
],
"date-time": "2021-10-29T02:12:11Z",
"timestamp": 1635473531000
},
"indexed": {
"date-parts": [
[
2021,
12,
15
]
],
"date-time": "2021-12-15T23:06:30Z",
"timestamp": 1639609590292
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "0021-1265"
},
{
"type": "electronic",
"value": "1863-4362"
}
],
"issued": {
"date-parts": [
[
2021,
10,
29
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
10,
29
]
],
"date-time": "2021-10-29T00:00:00Z",
"timestamp": 1635465600000
}
},
{
"URL": "https://www.springer.com/tdm",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
10,
29
]
],
"date-time": "2021-10-29T00:00:00Z",
"timestamp": 1635465600000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11845-021-02823-9.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s11845-021-02823-9/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s11845-021-02823-9.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1007",
"published": {
"date-parts": [
[
2021,
10,
29
]
]
},
"published-online": {
"date-parts": [
[
2021,
10,
29
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/S2213-8587(20)30238-2",
"author": "M Apicella",
"doi-asserted-by": "publisher",
"first-page": "782",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2823_CR1",
"unstructured": "Apicella M, Campopiano MC, Mantuano M et al (2020) COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol 8:782–792. https://doi.org/10.1016/S2213-8587(20)30238-2",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30272-2",
"author": "E Barron",
"doi-asserted-by": "publisher",
"first-page": "813",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2823_CR2",
"unstructured": "Barron E, Bakhai C, Kar P et al (2020) Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: a whole-population study. Lancet Diabetes Endocrinol 8:813–822. https://doi.org/10.1016/S2213-8587(20)30272-2",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1002/dmrr.3319",
"author": "W Guo",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab Res Rev",
"key": "2823_CR3",
"unstructured": "Guo W, Li M, Dong Y et al (2020) Diabetes is a risk factor for the progression and prognosis of COVID -19. Diabetes Metab Res Rev 36:e3319. https://doi.org/10.1002/dmrr.3319",
"volume": "36",
"year": "2020"
},
{
"DOI": "10.4049/jimmunol.1700474",
"author": "C Kajiwara",
"doi-asserted-by": "publisher",
"first-page": "623",
"journal-title": "J Immunol",
"key": "2823_CR4",
"unstructured": "Kajiwara C, Kusaka Y, Kimura S et al (2018) Metformin mediates protection against Legionella pneumonia through activation of AMPK and mitochondrial reactive oxygen species. J Immunol 200:623–631. https://doi.org/10.4049/jimmunol.1700474",
"volume": "200",
"year": "2018"
},
{
"DOI": "10.4103/0366-6999.223856",
"author": "Y Chen",
"doi-asserted-by": "publisher",
"first-page": "376",
"journal-title": "Chin Med J (Engl)",
"key": "2823_CR5",
"unstructured": "Chen Y, Gu F, Guan J-L (2018) Metformin might inhibit virus through increasing insulin sensitivity. Chin Med J (Engl) 131:376–377. https://doi.org/10.4103/0366-6999.223856",
"volume": "131",
"year": "2018"
},
{
"DOI": "10.1007/s00125-017-4318-z",
"author": "CJ Bailey",
"doi-asserted-by": "publisher",
"first-page": "1566",
"journal-title": "Diabetologia",
"key": "2823_CR6",
"unstructured": "Bailey CJ (2017) Metformin: historical overview. Diabetologia 60:1566–1576. https://doi.org/10.1007/s00125-017-4318-z",
"volume": "60",
"year": "2017"
},
{
"DOI": "10.1186/s12931-019-1035-9",
"doi-asserted-by": "publisher",
"key": "2823_CR7",
"unstructured": "Ho TW,Huang CT, Tsai YJ et al (2019) Metformin use mitigates the adverse prognostic effect of diabetes mellitus in chronic obstructive pulmonary disease Respir Res 20https://doi.org/10.1186/s12931-019-1035-9"
},
{
"DOI": "10.1513/AnnalsATS.201812-897OC",
"author": "TD Wu",
"doi-asserted-by": "publisher",
"first-page": "1527",
"journal-title": "Ann Am Thorac Soc",
"key": "2823_CR8",
"unstructured": "Wu TD, Keet CA, Fawzy A et al (2019) Association of metformin initiation and risk of asthma exacerbation A claims-based cohort study. Ann Am Thorac Soc 16:1527–1533. https://doi.org/10.1513/AnnalsATS.201812-897OC",
"volume": "16",
"year": "2019"
},
{
"DOI": "10.1183/13993003.congress-2018.PA2639",
"doi-asserted-by": "crossref",
"key": "2823_CR9",
"unstructured": "Mortensen E, Anzueto A (2018) Association of metformin and mortality for patients with diabetes who are hospitalised with pneumonia. In: Respiratory infections. European Respiratory Society, p PA2639"
},
{
"DOI": "10.1007/s00228-019-02786-y",
"author": "M Zhang",
"doi-asserted-by": "publisher",
"first-page": "149",
"journal-title": "Eur J Clin Pharmacol",
"key": "2823_CR10",
"unstructured": "Zhang M, He J (2020) Impacts of metformin on tuberculosis incidence and clinical outcomes in patients with diabetes: a systematic review and meta-analysis. Eur J Clin Pharmacol 76:149–159. https://doi.org/10.1007/s00228-019-02786-y",
"volume": "76",
"year": "2020"
},
{
"DOI": "10.1111/resp.13486",
"author": "A Mendy",
"doi-asserted-by": "publisher",
"first-page": "646",
"journal-title": "Respirology",
"key": "2823_CR11",
"unstructured": "Mendy A, Gopal R, Alcorn JF, Forno E (2019) Reduced mortality from lower respiratory tract disease in adult diabetic patients treated with metformin. Respirology 24:646–651. https://doi.org/10.1111/resp.13486",
"volume": "24",
"year": "2019"
},
{
"DOI": "10.1186/s13054-019-2346-4",
"author": "H Liang",
"doi-asserted-by": "publisher",
"first-page": "50",
"journal-title": "Crit Care",
"key": "2823_CR12",
"unstructured": "Liang H, Ding X, Li L et al (2019) Association of preadmission metformin use and mortality in patients with sepsis and diabetes mellitus: a systematic review and meta-analysis of cohort studies. Crit Care 23:50. https://doi.org/10.1186/s13054-019-2346-4",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"author": "K Khunti",
"doi-asserted-by": "publisher",
"first-page": "293",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2823_CR13",
"unstructured": "Khunti K, Knighton P, Zaccardi F et al (2021) Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England. Lancet Diabetes Endocrinol 9:293–303. https://doi.org/10.1016/S2213-8587(21)00050-4",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1016/j.obmed.2020.100290",
"author": "TI Hariyanto",
"doi-asserted-by": "publisher",
"journal-title": "Obes Med",
"key": "2823_CR14",
"unstructured": "Hariyanto TI, Kurniawan A (2020) Metformin use is associated with reduced mortality rate from coronavirus disease 2019 (COVID-19) infection. Obes Med 19:100290. https://doi.org/10.1016/j.obmed.2020.100290",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26498",
"author": "CS Kow",
"doi-asserted-by": "publisher",
"first-page": "695",
"journal-title": "J Med Virol",
"key": "2823_CR15",
"unstructured": "Kow CS, Hasan SS (2021) Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: a meta-analysis. J Med Virol 93:695–697. https://doi.org/10.1002/jmv.26498",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.21465",
"author": "JP Donnelly",
"doi-asserted-by": "publisher",
"first-page": "304",
"journal-title": "JAMA",
"key": "2823_CR16",
"unstructured": "Donnelly JP, Wang XQ, Iwashyna TJ, Prescott HC (2021) Readmission and death after initial hospital discharge among patients with COVID-19 in a large multihospital system. JAMA 325:304. https://doi.org/10.1001/jama.2020.21465",
"volume": "325",
"year": "2021"
},
{
"DOI": "10.1136/bmj.n693",
"doi-asserted-by": "publisher",
"key": "2823_CR17",
"unstructured": "Ayoubkhani D, Khunti K, Nafilyan V et al (2021) Post-covid syndrome in individuals admitted to hospital with covid-19: retrospective cohort study. BMJ 372 https://doi.org/10.1136/bmj.n693"
},
{
"DOI": "10.1016/j.diabet.2020.10.006",
"doi-asserted-by": "publisher",
"key": "2823_CR18",
"unstructured": "Do JY, Kim SW, Park JW et al (2020) Is there an association between metformin use and clinical outcomes in diabetes patients with COVID-19? Diabetes Metab 101208https://doi.org/10.1016/j.diabet.2020.10.006"
},
{
"DOI": "10.3389/fendo.2021.645194",
"doi-asserted-by": "publisher",
"key": "2823_CR19",
"unstructured": "Zangiabadian M, Nejadghaderi SA, Zahmatkesh MM et al (2021) The efficacy and potential mechanisms of metformin in the treatment of COVID-19 in the diabetics: a systematic review Front Endocrinol (Lausanne) 12 https://doi.org/10.3389/fendo.2021.645194"
},
{
"DOI": "10.1016/j.cmet.2020.08.013",
"author": "X Cheng",
"doi-asserted-by": "publisher",
"first-page": "537",
"journal-title": "Cell Metab",
"key": "2823_CR20",
"unstructured": "Cheng X, Liu Y-M, Li H et al (2020) Metformin is associated with higher incidence of acidosis, but not mortalitY, in individuals with COVID-19 and pre-existing type 2 diabetes. Cell Metab 32:537-547.e3. https://doi.org/10.1016/j.cmet.2020.08.013",
"volume": "32",
"year": "2020"
},
{
"DOI": "10.7326/0003-4819-150-9-200905050-00006",
"author": "AS Levey",
"doi-asserted-by": "publisher",
"first-page": "604",
"journal-title": "Ann Intern Med",
"key": "2823_CR21",
"unstructured": "Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612. https://doi.org/10.7326/0003-4819-150-9-200905050-00006",
"volume": "150",
"year": "2009"
},
{
"DOI": "10.1016/j.diabres.2020.108151",
"author": "A Ceriello",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Res Clin Pract",
"key": "2823_CR22",
"unstructured": "Ceriello A, Stoian AP, Rizzo M (2020) COVID-19 and diabetes management: what should be considered? Diabetes Res Clin Pract 163:108151. https://doi.org/10.1016/j.diabres.2020.108151",
"volume": "163",
"year": "2020"
},
{
"DOI": "10.1007/s00592-021-01739-1",
"author": "A Avogaro",
"doi-asserted-by": "publisher",
"journal-title": "Acta Diabetol",
"key": "2823_CR23",
"unstructured": "Avogaro A, Bonora B, Fadini GP (2021) Managing diabetes in diabetic patients with COVID: where do we start from? Acta Diabetol. https://doi.org/10.1007/s00592-021-01739-1",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.11.006",
"author": "AA Lukito",
"doi-asserted-by": "publisher",
"first-page": "2177",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "2823_CR24",
"unstructured": "Lukito AA, Pranata R, Henrina J et al (2020) The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis. Diabetes Metab Syndr Clin Res Rev 14:2177–2183. https://doi.org/10.1016/j.dsx.2020.11.006",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2021.108925",
"doi-asserted-by": "publisher",
"key": "2823_CR25",
"unstructured": "Dave JA, Tamuhla T, Tiffin N et al (2021) Risk factors for COVID-19 hospitalisation and death in people living with diabetes: a virtual cohort study from the Western Cape Province South Africa Diabetes Res Clin Pract 108925 https://doi.org/10.1016/j.diabres.2021.108925"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"author": "P Luo",
"doi-asserted-by": "publisher",
"first-page": "69",
"journal-title": "Am J Trop Med Hyg",
"key": "2823_CR26",
"unstructured": "Luo P, Qiu L, Liu Y et al (2020) Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis. Am J Trop Med Hyg 103:69–72. https://doi.org/10.4269/ajtmh.20-0375",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.1016/j.dsx.2021.02.022",
"author": "R Ghany",
"doi-asserted-by": "publisher",
"first-page": "513",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "2823_CR27",
"unstructured": "Ghany R, Palacio A, Dawkins E et al (2021) Metformin is associated with lower hospitalisations, mortality and severe coronavirus infection among elderly medicare minority patients in 8 states in USA. Diabetes Metab Syndr Clin Res Rev 15:513–518. https://doi.org/10.1016/j.dsx.2021.02.022",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.2337/dc20-0660",
"author": "Y Chen",
"doi-asserted-by": "publisher",
"first-page": "1399",
"journal-title": "Diabetes Care",
"key": "2823_CR28",
"unstructured": "Chen Y, Yang D, Cheng B et al (2020) Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care 43:1399–1407. https://doi.org/10.2337/dc20-0660",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1210/clinem/dgab067",
"author": "J Wang",
"doi-asserted-by": "publisher",
"first-page": "1255",
"journal-title": "J Clin Endocrinol Metab",
"key": "2823_CR29",
"unstructured": "Wang J, Cooper JM, Gokhale K et al (2021) Association of metformin with susceptibility to COVID-19 in people with type 2 diabetes. J Clin Endocrinol Metab 106:1255–1268. https://doi.org/10.1210/clinem/dgab067",
"volume": "106",
"year": "2021"
},
{
"DOI": "10.1016/j.aohep.2021.100553",
"doi-asserted-by": "publisher",
"key": "2823_CR30",
"unstructured": "Salık F, Uzundere O, Bıçak M et al (2021) Liver function as a predictor of mortality in COVID-19 Retrospective study Ann Hepatol 100553https://doi.org/10.1016/j.aohep.2021.100553"
},
{
"DOI": "10.1016/j.aohep.2020.08.068",
"doi-asserted-by": "publisher",
"key": "2823_CR31",
"unstructured": "Medetalibeyoglu A, Catma Y, Senkal N et al (2019) The effect of liver test abnormalities on the prognosis of COVID-19. Ann Hepatol 19:614–621. https://doi.org/10.1016/j.aohep.2020.08.068"
}
],
"reference-count": 31,
"references-count": 31,
"relation": {},
"score": 1,
"short-container-title": [
"Ir J Med Sci"
],
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine"
],
"subtitle": [],
"title": [
"Preadmission usage of metformin and mortality in COVID-19 patients including the post-discharge period"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy"
}
