Infection Rates and Impact of Glucose Lowering Medications on the Clinical Course of COVID-19 in People with Type 2 Diabetes: A Retrospective Observational Study
et al., Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, doi:10.2147/DMSO.S385646, Oct 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 54,009 diabetes patients in Italy, showing lower mortality with metformin use.
|
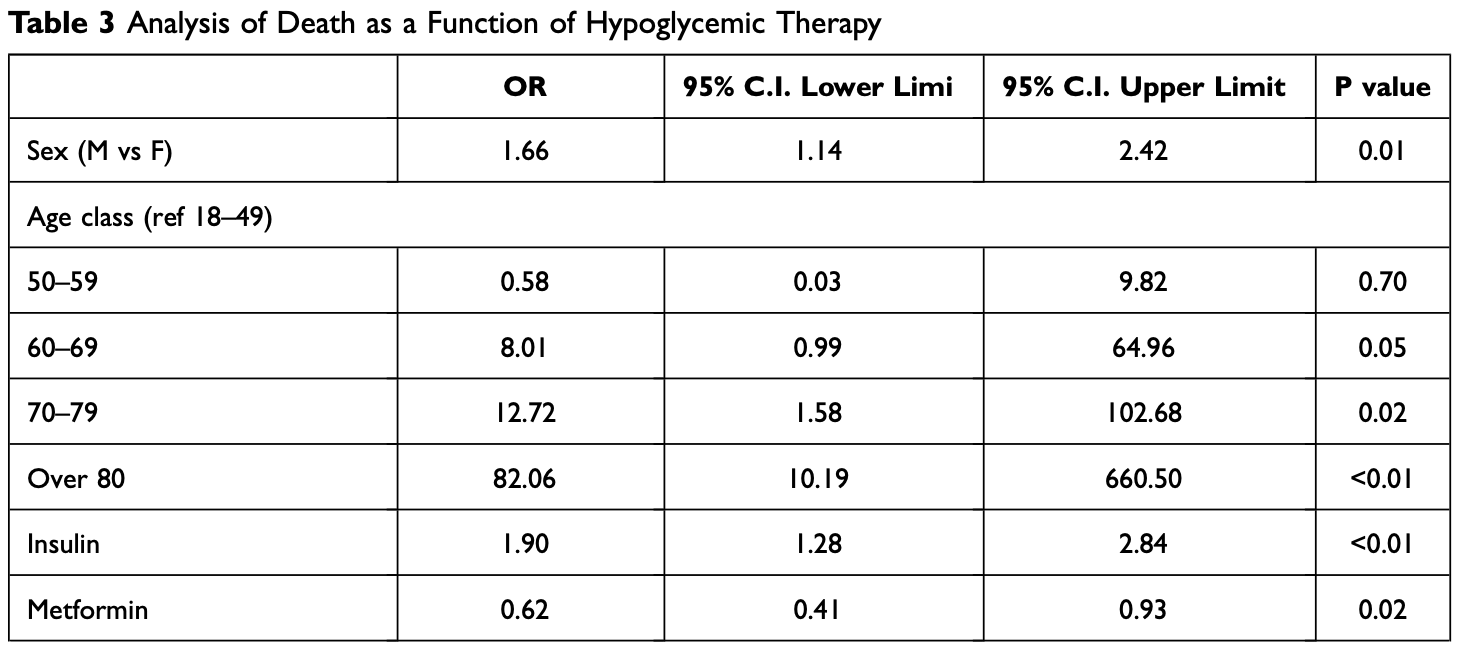
risk of death, 38.0% lower, OR 0.62, p = 0.02, RR approximated with OR.
|
|
risk of hospitalization, 15.0% lower, OR 0.85, p = 0.25, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Mannucci et al., 31 Oct 2022, retrospective, Italy, peer-reviewed, 10 authors, study period 1 March, 2020 - 31 December, 2020.
Contact: gianpaolo.fadini@unipd.it.
Infection Rates and Impact of Glucose Lowering Medications on the Clinical Course of COVID-19 in People with Type 2 Diabetes: A Retrospective Observational Study
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, doi:10.2147/dmso.s385646
Diabetes is a risk factor for COVID-19 severity, but the role played by glucose lowering medications (GLM) is still unclear. The aim of this study was to assess infection rates and outcomes of COVID-19 (hospitalization and mortality) in adults with diabetes assisted by the Local Health Unit of Padua (North-East Italy) according to the ongoing GLM. Patients and Methods: People with diabetes were identified using administrative claims, while those with SARS-CoV-2 infection were detected by cross referencing with the local COVID-19 surveillance registry. A multivariate logistic regression model was used to verify the association between GLM classes and the outcome. Results: SARS-CoV-2 infection rates were marginally but significantly higher in individuals with diabetes as compared to those without diabetes (RR 1.04, p = 0.043), though such relative 4% increase may be irrelevant from a clinical and epidemiological perspective. 1923 individuals with GLM-treated diabetes were diagnosed with COVID-19; 456 patients were hospitalized and 167 died. Those treated with insulin had a significantly higher risk of hospitalizations for COVID-19 (OR 1.48 p < 0.01) as were those treated with sulphonylureas/glinides (OR 1.34, p = 0.02). Insulin use was also significantly associated with higher mortality (OR 1.90, p < 0.01). Use of metformin was significantly associated with lower death rates (OR 0.62, p = 0.02). The association of other GLM classes with the outcome was not significant. Conclusion: Diabetes does not appear to modify the risk of SARS-CoV-2 infection in a clinically meaningful way, but strongly increases the rates of hospitalization and death. Insulin use was associated with worse outcomes, whereas metformin use was associated with lower mortality.
References
Bonora, Fedeli, Schievano, SARS-CoV-2 and COVID-19 in diabetes mellitus. Population-based study on ascertained infections, hospital admissions and mortality in an Italian region with ~5 million inhabitants and~250,000 diabetic people, Nutr Metab Cardiovasc Dis, doi:10.1016/j.numecd.2021.06.010
Boye, Erdemir, Zimmerman, Risk factors associated with COVID-19 hospitalization and mortality: a large claims-based analysis among people with type 2 diabetes mellitus in the United States, Diabetes Ther, doi:10.1007/s13300-021-01110-1
Bramante, Huling, Tignanelli, Randomized trial of metformin, ivermectin, and fluvoxamine for Covid-19, N Engl J Med, doi:10.1056/NEJMoa2201662
Cui, Li, Shi, Origin and evolution of pathogenic coronaviruses, Nat Rev Microbiol, doi:10.1038/s41579-018-0118-9
Diabetes, None, Metabolic Syndrome and Obesity: Targets and Therapy
Fadini, Morieri, Longato, Avogaro, Prevalence and impact of diabetes among people infected with SARS-CoV-2, J Endocrinol Invest, doi:10.1007/s40618-020-01236-2
Fadini, Morieri, Longato, Exposure to dipeptidyl-peptidase-4 inhibitors and COVID -19 among people with type 2 diabetes: a casecontrol study, Diabetes Obes Metab, doi:10.1111/dom.14097
Goldstein, Lee, Demographic perspectives on the mortality of COVID-19 and other epidemics, Proc Natl Acad Sci U S A, doi:10.1073/pnas.2006392117
Harrison, Lin, Wang, Mechanisms of SARS-CoV-2 transmission and pathogenesis, Trends Immunol, doi:10.1016/j.it.2020.10.004
Hui, Azhar, Madani, The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health -the latest 2019 novel coronavirus outbreak in Wuhan, China, Int J Infect Dis, doi:10.1016/j.ijid.2020.01.009
Jafar, Edriss, Nugent, The effect of short-term hyperglycemia on the innate immune system, Am J Med Sci, doi:10.1016/j.amjms.2015.11.011
Khunti, Knighton, Zaccardi, Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00050-4
Kumar, Arora, Sharma, Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.04.044
Lukito, Pranata, Henrina, Lim, Lawrensia et al., The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.11.006
Montopoli, Zumerle, Vettor, Androgen-deprivation therapies for prostate cancer and risk of infection by SARS-CoV-2: a population-based study (N = 4532), Ann Oncol, doi:10.1016/j.annonc.2020.04.479
Pollard, Morran, Al, The COVID-19 pandemic: a global health crisis, Physiol Genomics, doi:10.1152/physiolgenomics.00089.2020
Schlesinger, Neuenschwander, Lang, Risk phenotypes of diabetes and association with COVID-19 severity and death: a living systematic review and meta-analysis, Diabetologia, doi:10.1007/s00125-021-05458-8
Solerte, 'addio, Trevisan, Sitagliptin treatment at the time of hospitalization was associated with reduced mortality in patients with type 2 diabetes and COVID-19: a multicenter, case-control, retrospective, observational study, Dia Care, doi:10.2337/dc20-1521
Sun, Huang, Zhou, Perspectives of antidiabetic drugs in diabetes with coronavirus infections, Front Pharmacol, doi:10.3389/fphar.2020.592439
Varikasuvu, Dutt, Thangappazham, Varshney, Diabetes and COVID-19: a pooled analysis related to disease severity and mortality, Prim Care Diabetes, doi:10.1016/j.pcd.2020.08.015
Webster, COVID-19 timeline of events, Nat Med, doi:10.1038/s41591-021-01618-w
Wiersinga, Rhodes, Cheng, Peacock, Prescott, Pathophysiology, transmission, diagnosis, and treatment of coronavirus disease 2019 (COVID-19): a review, JAMA, doi:10.1001/jama.2020.12839
Yu, Li, Sun, Wang, Insulin treatment is associated with increased mortality in patients with COVID-19 and type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.11.014
DOI record:
{
"DOI": "10.2147/dmso.s385646",
"ISSN": [
"1178-7007"
],
"URL": "http://dx.doi.org/10.2147/DMSO.S385646",
"author": [
{
"affiliation": [],
"family": "Mannucci",
"given": "Francesca",
"sequence": "first"
},
{
"affiliation": [],
"family": "Vitturi",
"given": "Giacomo",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Benacchio",
"given": "Luca",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sbrogiò",
"given": "Luca Gino",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bano",
"given": "Francesca",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lapolla",
"given": "Annunziata",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Piarulli",
"given": "Francesco",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Giron",
"given": "Maria Cecilia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1177-0516",
"affiliation": [],
"authenticated-orcid": true,
"family": "Avogaro",
"given": "Angelo",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6510-2097",
"affiliation": [],
"authenticated-orcid": true,
"family": "Fadini",
"given": "Gian Paolo",
"sequence": "additional"
}
],
"container-title": "Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy",
"container-title-short": "DMSO",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
10,
10
]
],
"date-time": "2022-10-10T05:55:10Z",
"timestamp": 1665381310000
},
"deposited": {
"date-parts": [
[
2022,
10,
10
]
],
"date-time": "2022-10-10T05:55:12Z",
"timestamp": 1665381312000
},
"indexed": {
"date-parts": [
[
2022,
10,
10
]
],
"date-time": "2022-10-10T06:12:27Z",
"timestamp": 1665382347448
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
10
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/3.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
10,
1
]
],
"date-time": "2022-10-01T00:00:00Z",
"timestamp": 1664582400000
}
}
],
"link": [
{
"URL": "https://www.dovepress.com/getfile.php?fileID=84551",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.dovepress.com/getfile.php?fileID=84551",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "3093-3101",
"prefix": "10.2147",
"published": {
"date-parts": [
[
2022,
10
]
]
},
"published-online": {
"date-parts": [
[
2022,
10
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1016/j.ijid.2020.01.009",
"author": "Hui",
"doi-asserted-by": "publisher",
"first-page": "264",
"journal-title": "Int J Infect Dis",
"key": "ref1",
"volume": "91",
"year": "2020"
},
{
"DOI": "10.1038/s41579-018-0118-9",
"author": "Cui",
"doi-asserted-by": "publisher",
"first-page": "181",
"journal-title": "Nat Rev Microbiol",
"key": "ref2",
"volume": "17",
"year": "2019"
},
{
"DOI": "10.1001/jama.2020.12839",
"author": "Wiersinga",
"doi-asserted-by": "publisher",
"first-page": "782",
"journal-title": "JAMA",
"key": "ref3",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/j.it.2020.10.004",
"author": "Harrison",
"doi-asserted-by": "publisher",
"first-page": "1100",
"journal-title": "Trends Immunol",
"key": "ref4",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1152/physiolgenomics.00089.2020",
"author": "Pollard",
"doi-asserted-by": "publisher",
"first-page": "549",
"journal-title": "Physiol Genomics",
"key": "ref5",
"volume": "52",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2006392117",
"author": "Goldstein",
"doi-asserted-by": "publisher",
"first-page": "22035",
"journal-title": "Proc Natl Acad Sci U S A",
"key": "ref6",
"volume": "117",
"year": "2020"
},
{
"DOI": "10.1007/s40618-020-01236-2",
"author": "Fadini",
"doi-asserted-by": "publisher",
"first-page": "867",
"journal-title": "J Endocrinol Invest",
"key": "ref7",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1016/j.pcd.2020.08.015",
"author": "Varikasuvu",
"doi-asserted-by": "publisher",
"first-page": "24",
"journal-title": "Prim Care Diabetes",
"key": "ref8",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.3389/fphar.2020.592439",
"author": "Sun",
"doi-asserted-by": "publisher",
"first-page": "11",
"journal-title": "Front Pharmacol",
"key": "ref9",
"year": "2021"
},
{
"DOI": "10.1016/j.amjms.2015.11.011",
"author": "Jafar",
"doi-asserted-by": "publisher",
"first-page": "201",
"journal-title": "Am J Med Sci",
"key": "ref10",
"volume": "351",
"year": "2016"
},
{
"DOI": "10.1016/j.dsx.2020.11.006",
"author": "Lukito",
"doi-asserted-by": "publisher",
"first-page": "2177",
"journal-title": "Diabetes Metab Syndr",
"key": "ref11",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.2337/dc20-1521",
"author": "Solerte",
"doi-asserted-by": "publisher",
"first-page": "2999",
"journal-title": "Dia Care",
"key": "ref12",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1111/dom.14097",
"author": "Fadini",
"doi-asserted-by": "publisher",
"first-page": "1946",
"journal-title": "Diabetes Obes Metab",
"key": "ref13",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.1007/s00125-021-05458-8",
"author": "Schlesinger",
"doi-asserted-by": "publisher",
"first-page": "1480",
"journal-title": "Diabetologia",
"key": "ref14",
"volume": "64",
"year": "2021"
},
{
"DOI": "10.1016/j.numecd.2021.06.010",
"author": "Bonora",
"doi-asserted-by": "publisher",
"first-page": "2612",
"journal-title": "Nutr Metab Cardiovasc Dis",
"key": "ref15",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1038/s41591-021-01618-w",
"author": "Webster",
"doi-asserted-by": "publisher",
"first-page": "2054",
"journal-title": "Nat Med",
"key": "ref16",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.04.044",
"author": "Kumar",
"doi-asserted-by": "publisher",
"first-page": "535",
"journal-title": "Diabetes Metab Syndr",
"key": "ref17",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.11.014",
"author": "Yu",
"doi-asserted-by": "publisher",
"first-page": "65",
"journal-title": "Cell Metab",
"key": "ref18",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.1007/s13300-021-01110-1",
"author": "Boye",
"doi-asserted-by": "publisher",
"first-page": "2223",
"journal-title": "Diabetes Ther",
"key": "ref19",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"author": "Khunti",
"doi-asserted-by": "publisher",
"first-page": "293",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "ref20",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2201662",
"author": "Bramante",
"doi-asserted-by": "publisher",
"first-page": "599",
"journal-title": "N Engl J Med",
"key": "ref21",
"volume": "387",
"year": "2022"
},
{
"DOI": "10.1016/j.annonc.2020.04.479",
"author": "Montopoli",
"doi-asserted-by": "publisher",
"first-page": "1040",
"journal-title": "Ann Oncol",
"key": "ref22",
"volume": "31",
"year": "2020"
}
],
"reference-count": 22,
"references-count": 22,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.dovepress.com/infection-rates-and-impact-of-glucose-lowering-medications-on-the-clin-peer-reviewed-fulltext-article-DMSO"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology",
"Internal Medicine"
],
"subtitle": [],
"title": "Infection Rates and Impact of Glucose Lowering Medications on the Clinical Course of COVID-19 in People with Type 2 Diabetes: A Retrospective Observational Study",
"type": "journal-article",
"volume": "Volume 15"
}
