Risk Factors Associated with COVID-19 Hospitalization and Mortality: A Large Claims-Based Analysis Among People with Type 2 Diabetes Mellitus in the United States
et al., Diabetes Therapy, doi:10.1007/s13300-021-01110-1, Jul 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
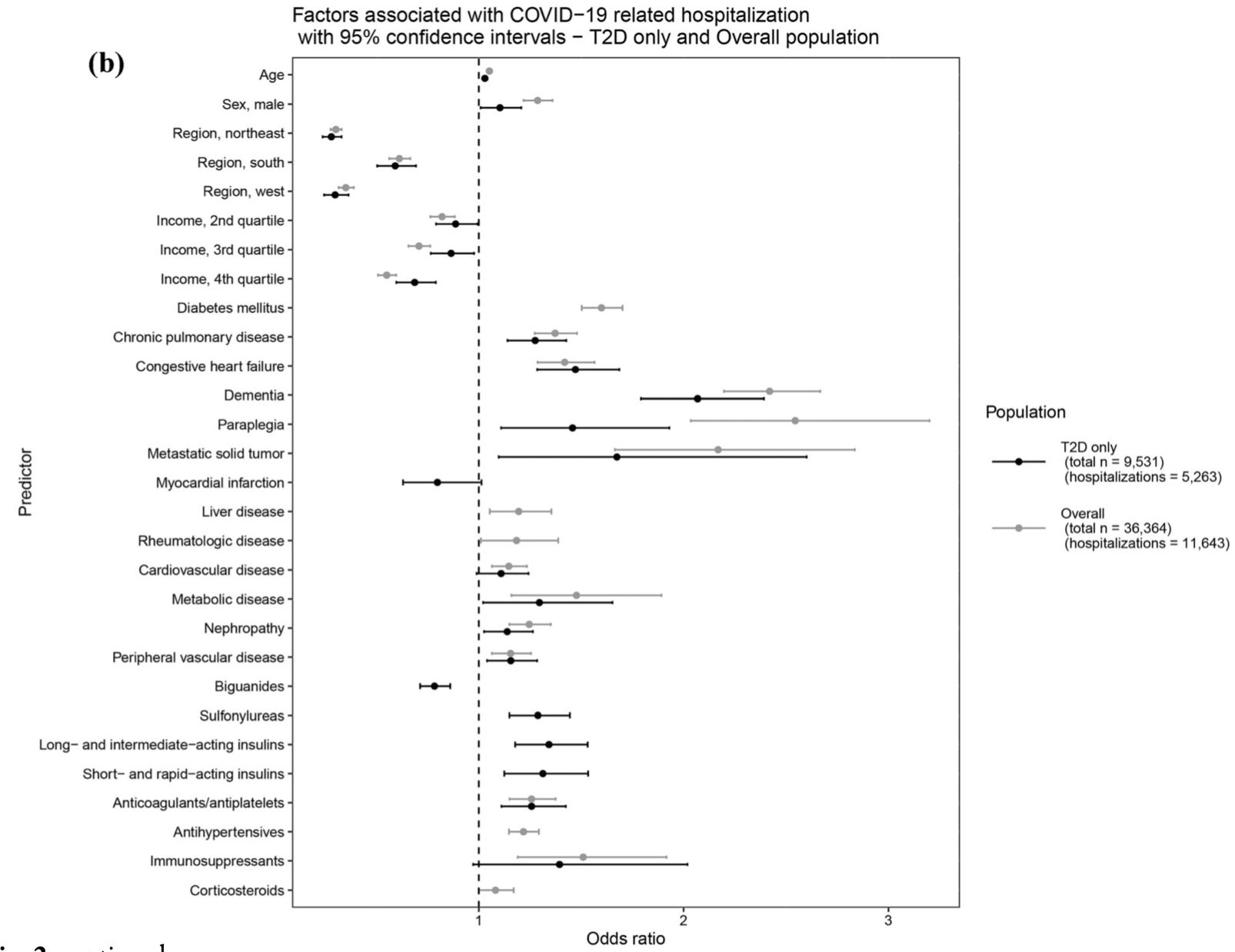
Retrospective 9531 COVID+ diabetes patients in the USA, showing lower risk of hospitalization with existing biguanides treatment (defined as mainly metformin in the abstract and entirely metformin in the text).
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of hospitalization, 10.0% lower, RR 0.90, p < 0.001, treatment 2,067 of 4,250 (48.6%), control 3,196 of 5,281 (60.5%), NNT 8.4, odds ratio converted to relative risk.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Boye et al., 18 Jul 2021, retrospective, USA, peer-reviewed, 14 authors.
Risk Factors Associated with COVID-19 Hospitalization and Mortality: A Large Claims-Based Analysis Among People with Type 2 Diabetes Mellitus in the United States
Diabetes Therapy, doi:10.1007/s13300-021-01110-1
Introduction: Diabetes has been identified as a high-risk comorbidity for COVID-19 hospitalization. We evaluated additional risk factors for COVID-19 hospitalization and in-hospital mortality in a nationwide US database. Methods: This retrospective study utilized the UnitedHealth Group Clinical Discovery Database (January 1, 2019-July 15, 2020) containing de-identified nationwide administrative claims, SARS-CoV-2 laboratory test results, and COVID-19 inpatient admissions data. Logistic regression was used to understand risk factors for hospitalization and in-hospital mortality among people with type 2 diabetes (T2D) and in the overall population. Robustness of associations was further confirmed by subgroup and sensitivity analyses in the T2D population. Results: A total of 36,364 people were identified who were either SARS-CoV-2 ? or hospitalized for COVID-19. T2D was associated with increased COVID-19-related hospitalization and mortality. Factors associated with increased hospitalization risk were largely consistent in the overall population and the T2D subgroup, including age, male sex, and these top five comorbidities: dementia, metastatic tumor, congestive heart failure, paraplegia, and metabolic disease. Biguanides (mainly metformin) were consistently associated with lower odds of hospitalization, whereas sulfonylureas and insulins were associated with greater odds of hospitalization among people with T2D. Conclusion: In this nationwide US analysis, T2D was identified as an independent risk factor for COVID-19 complications. Many factors conferred similar risk of hospitalization across both populations; however, particular diabetes medications may be markers for differential risk. The insights on comorbidities and medications may inform population health initiatives, including prevention efforts for high-risk patient populations such as those with T2D.
References
Baral, Tsampasian, Debski, Moran, Garg et al., Association between reninangiotensin-aldosterone system inhibitors and clinical outcomes in patients with COVID-19: a systematic review and meta-analysis, JAMA Netw Open
Bode, Garrett, Messler, Glycemic characteristics and clinical outcomes of COVID-19 hospitalized in the United States, J Diabetes Sci Technol
Bornstein, Rubino, Khunti, Practical recommendations for the management of diabetes in patients with COVID-19, Lancet Diabetes Endocrinol
Cdc Covid-, 19 Response Team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019-United States, February 12, MMWR Morb Mortal Wkly Rep
Chang, Weiner, Richards, Bleich, Segal, Validating the adapted Diabetes Complications Severity Index in claims data, Am J Manag Care
Chen, Yang, Cheng, Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care
Chen, Zhou, Dong, Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet
Cugno, Gualtierotti, Casazza, Tafuri, Ghigliazza et al., Mortality in PATIENTS with COVID-19 on renin angiotensin system inhibitor long-term treatment: an observational study showing that things are not always as they seem, Adv Ther
Deyo, Cherkin, Ciol, Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases, J Clin Epidemiol
Drucker, Coronavirus infections and type 2 diabetes-shared pathways with therapeutic implications, Endocr Rev
Glasheen, Dong, Diabetes Complications Severity Index (DCSI)-update and ICD-10 translation, J Diabetes Complicat
Grasselli, Zangrillo, Zanella, Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy, JAMA
Hastie, Tibshirani, Friedman, The elements of statistical learning: data mining, inference, and prediction
Holman, Knighton, Kar, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet
Jordan, Adab, Cheng, Covid-19: risk factors for severe disease and death, BMJ
Klabunde, Potosky, Legler, Warren, Development of a comorbidity index using physician claims data, J Clin Epidemiol
Li, Liu, Yu, Tang, Tang, Coronavirus disease 2019 (COVID-19): current status and future perspectives, Int J Antimicrob Agents
Liu, Fang, Deng, Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province, Chin Med J (Engl)
Onder, Rezza, Brusaferro, Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy, JAMA
Petrilli, Jones, Yang, Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study, BMJ
Quan, Sundararajan, Halfon, Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data, Med Care
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area, JAMA
Seiglie, Platt, Cromer, Diabetes as a risk factor for poor early outcomes in patients hospitalized with COVID-19, Diabetes Care
Sharma, Ray, Sadasivam, Metformin in COVID-19: a possible role beyond diabetes, Diabetes Res Clin Pract
Singh, Singh, Is metformin ahead in the race as a repurposed host-directed therapy for patients with diabetes and COVID-19?, Diabetes Res Clin Pract
Ursini, Russo, Pellino, Metformin and autoimmunity: a ''New Deal'' of an old drug, Front Immunol
Wu, Chen, Cai, Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China JAMA Intern Med
Xu, Teng, Shang, Gu, Fan et al., The effect of prior ACEI/ARB treatment on COVID-19 susceptibility and outcome: a systematic review and meta-analysis, Clin Infect Dis
Yang, Zheng, Gou, Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and metaanalysis, Int J Infect Dis
Young, Korff, Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization, Am J Manag Care
Yu, Li, Sun, Wang, Insulin treatment is associated with increased mortality in patients with COVID-19 and type 2 diabetes, Cell Metab
Zhang, Shang, Ahn, How to best protect people with diabetes from the impact of SARS-CoV-2: report of the international COVID-19 and diabetes summit, J Diabetes Sci Technol, doi:10.1177/1932296820978399
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, Lancet
Zhu, She, Cheng, Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab
DOI record:
{
"DOI": "10.1007/s13300-021-01110-1",
"ISSN": [
"1869-6953",
"1869-6961"
],
"URL": "http://dx.doi.org/10.1007/s13300-021-01110-1",
"alternative-id": [
"1110"
],
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "28 April 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "28 June 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "18 July 2021"
}
],
"author": [
{
"affiliation": [],
"family": "Boye",
"given": "Kristina S.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Tokar Erdemir",
"given": "Elif",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Zimmerman",
"given": "Nathan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Reddy",
"given": "Abraham",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Benneyworth",
"given": "Brian D.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dabora",
"given": "Matan C.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hankosky",
"given": "Emily R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bethel",
"given": "M. Angelyn",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Clark",
"given": "Callahan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lensing",
"given": "Cody J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sailer",
"given": "Scott",
"sequence": "additional"
},
{
"affiliation": [],
"family": "San Juan",
"given": "Ramira",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Heine",
"given": "Robert J.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Etemad",
"given": "Lida",
"sequence": "additional"
}
],
"container-title": [
"Diabetes Therapy"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
7,
18
]
],
"date-time": "2021-07-18T07:02:32Z",
"timestamp": 1626591752000
},
"deposited": {
"date-parts": [
[
2021,
8,
5
]
],
"date-time": "2021-08-05T10:02:14Z",
"timestamp": 1628157734000
},
"funder": [
{
"DOI": "10.13039/100004312",
"doi-asserted-by": "publisher",
"name": "Eli Lilly and Company"
},
{
"DOI": "10.13039/100018368",
"doi-asserted-by": "crossref",
"name": "UnitedHealth Group Inc"
}
],
"indexed": {
"date-parts": [
[
2021,
12,
15
]
],
"date-time": "2021-12-15T18:27:42Z",
"timestamp": 1639592862755
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "1869-6953"
},
{
"type": "electronic",
"value": "1869-6961"
}
],
"issue": "8",
"issued": {
"date-parts": [
[
2021,
7,
18
]
]
},
"journal-issue": {
"issue": "8",
"published-print": {
"date-parts": [
[
2021,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
18
]
],
"date-time": "2021-07-18T00:00:00Z",
"timestamp": 1626566400000
}
},
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
18
]
],
"date-time": "2021-07-18T00:00:00Z",
"timestamp": 1626566400000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1007/s13300-021-01110-1.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1007/s13300-021-01110-1/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1007/s13300-021-01110-1.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "2223-2239",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2021,
7,
18
]
]
},
"published-online": {
"date-parts": [
[
2021,
7,
18
]
]
},
"published-print": {
"date-parts": [
[
2021,
8
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1016/j.ijantimicag.2020.105951",
"author": "H Li",
"doi-asserted-by": "publisher",
"first-page": "105951",
"issue": "5",
"journal-title": "Int J Antimicrob Agents",
"key": "1110_CR1",
"unstructured": "Li H, Liu SM, Yu XH, Tang SL, Tang CK. Coronavirus disease 2019 (COVID-19): current status and future perspectives. Int J Antimicrob Agents. 2020;55(5):105951.",
"volume": "55",
"year": "2020"
},
{
"key": "1110_CR2",
"unstructured": "WHO Director-General’s opening remarks at the media briefing on COVID19. 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed 20 Apr 2020."
},
{
"key": "1110_CR3",
"unstructured": "World Health Organization. Coronavirus disease (COVID-2019) situation reports-90. 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update---2-february-2021. Accessed 05 Feb 2021."
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"author": "C Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"issue": "10223",
"journal-title": "Lancet",
"key": "1110_CR4",
"unstructured": "Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.2337/dc20-0660",
"author": "Y Chen",
"doi-asserted-by": "publisher",
"first-page": "1399",
"issue": "7",
"journal-title": "Diabetes Care",
"key": "1110_CR5",
"unstructured": "Chen Y, Yang D, Cheng B, et al. Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication. Diabetes Care. 2020;43(7):1399–407.",
"volume": "43",
"year": "2020"
},
{
"key": "1110_CR6",
"unstructured": "Centers for Disease Control and Prevention. Evidence used to update the list of underlying medical conditions that increase a person’s risk of severe illness from COVID-19. 2020. https://stacks.cdc.gov/view/cdc/89840. Accessed 30 Aug 2020."
},
{
"DOI": "10.15585/mmwr.mm6913e2",
"author": "CDC COVID-19 Response Team",
"doi-asserted-by": "publisher",
"first-page": "382",
"issue": "13",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "1110_CR7",
"unstructured": "CDC COVID-19 Response Team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019-United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):382–6.",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30211-7",
"author": "N Chen",
"doi-asserted-by": "publisher",
"first-page": "507",
"issue": "10223",
"journal-title": "Lancet",
"key": "1110_CR8",
"unstructured": "Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.0994",
"author": "C Wu",
"doi-asserted-by": "publisher",
"first-page": "934",
"issue": "7",
"journal-title": "China JAMA Intern Med",
"key": "1110_CR9",
"unstructured": "Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan. China JAMA Intern Med. 2020;180(7):934–43.",
"volume": "180",
"year": "2020"
},
{
"author": "G Onder",
"first-page": "1775",
"issue": "18",
"journal-title": "JAMA",
"key": "1110_CR10",
"unstructured": "Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323(18):1775–6.",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1966",
"author": "CM Petrilli",
"doi-asserted-by": "publisher",
"first-page": "m1966",
"journal-title": "BMJ",
"key": "1110_CR11",
"unstructured": "Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966.",
"volume": "369",
"year": "2020"
},
{
"DOI": "10.1097/CM9.0000000000000744",
"author": "K Liu",
"doi-asserted-by": "publisher",
"first-page": "1025",
"issue": "9",
"journal-title": "Chin Med J (Engl)",
"key": "1110_CR12",
"unstructured": "Liu K, Fang YY, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl). 2020;133(9):1025–31.",
"volume": "133",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.5394",
"author": "G Grasselli",
"doi-asserted-by": "publisher",
"first-page": "1574",
"issue": "16",
"journal-title": "JAMA",
"key": "1110_CR13",
"unstructured": "Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574–81.",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.6775",
"author": "S Richardson",
"doi-asserted-by": "publisher",
"first-page": "2052",
"issue": "20",
"journal-title": "JAMA",
"key": "1110_CR14",
"unstructured": "Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–9.",
"volume": "323",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"author": "F Zhou",
"doi-asserted-by": "publisher",
"first-page": "1054",
"issue": "10229",
"journal-title": "Lancet",
"key": "1110_CR15",
"unstructured": "Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62.",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1177/1932296820978399",
"author": "JY Zhang",
"doi-asserted-by": "publisher",
"journal-title": "J Diabetes Sci Technol",
"key": "1110_CR16",
"unstructured": "Zhang JY, Shang T, Ahn D, et al. How to best protect people with diabetes from the impact of SARS-CoV-2: report of the international COVID-19 and diabetes summit. J Diabetes Sci Technol. 2021. https://doi.org/10.1177/1932296820978399.",
"year": "2021"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"author": "L Zhu",
"doi-asserted-by": "publisher",
"first-page": "1068",
"issue": "6",
"journal-title": "Cell Metab",
"key": "1110_CR17",
"unstructured": "Zhu L, She ZG, Cheng X, et al. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;31(6):1068-1077.e3.",
"volume": "31",
"year": "2020"
},
{
"DOI": "10.1177/1932296820924469",
"author": "B Bode",
"doi-asserted-by": "publisher",
"first-page": "813",
"issue": "4",
"journal-title": "J Diabetes Sci Technol",
"key": "1110_CR18",
"unstructured": "Bode B, Garrett V, Messler J, et al. Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States. J Diabetes Sci Technol. 2020;14(4):813–21.",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.2337/dc20-1506",
"author": "J Seiglie",
"doi-asserted-by": "publisher",
"first-page": "2938",
"issue": "12",
"journal-title": "Diabetes Care",
"key": "1110_CR19",
"unstructured": "Seiglie J, Platt J, Cromer SJ, et al. Diabetes as a risk factor for poor early outcomes in patients hospitalized with COVID-19. Diabetes Care. 2020;43(12):2938–44.",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1210/endrev/bnaa011",
"author": "DJ Drucker",
"doi-asserted-by": "publisher",
"first-page": "bnaa011",
"issue": "3",
"journal-title": "Endocr Rev",
"key": "1110_CR20",
"unstructured": "Drucker DJ. Coronavirus infections and type 2 diabetes-shared pathways with therapeutic implications. Endocr Rev. 2020;41(3):bnaa011.",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30152-2",
"author": "SR Bornstein",
"doi-asserted-by": "publisher",
"first-page": "546",
"issue": "6",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "1110_CR21",
"unstructured": "Bornstein SR, Rubino F, Khunti K, et al. Practical recommendations for the management of diabetes in patients with COVID-19. Lancet Diabetes Endocrinol. 2020;8(6):546–50.",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/0895-4356(92)90133-8",
"author": "RA Deyo",
"doi-asserted-by": "publisher",
"first-page": "613",
"issue": "6",
"journal-title": "J Clin Epidemiol",
"key": "1110_CR22",
"unstructured": "Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9.",
"volume": "45",
"year": "1992"
},
{
"DOI": "10.1097/01.mlr.0000182534.19832.83",
"author": "H Quan",
"doi-asserted-by": "publisher",
"first-page": "1130",
"issue": "11",
"journal-title": "Med Care",
"key": "1110_CR23",
"unstructured": "Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.",
"volume": "43",
"year": "2005"
},
{
"DOI": "10.1016/S0895-4356(00)00256-0",
"author": "CN Klabunde",
"doi-asserted-by": "publisher",
"first-page": "1258",
"issue": "12",
"journal-title": "J Clin Epidemiol",
"key": "1110_CR24",
"unstructured": "Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53(12):1258–67.",
"volume": "53",
"year": "2000"
},
{
"author": "HY Chang",
"first-page": "721",
"issue": "11",
"journal-title": "Am J Manag Care",
"key": "1110_CR25",
"unstructured": "Chang HY, Weiner JP, Richards TM, Bleich SN, Segal JB. Validating the adapted Diabetes Complications Severity Index in claims data. Am J Manag Care. 2012;18(11):721–6.",
"volume": "18",
"year": "2012"
},
{
"DOI": "10.1016/j.jdiacomp.2017.02.018",
"author": "WP Glasheen",
"doi-asserted-by": "publisher",
"first-page": "1007",
"issue": "6",
"journal-title": "J Diabetes Complicat",
"key": "1110_CR26",
"unstructured": "Glasheen WP, Renda A, Dong Y. Diabetes Complications Severity Index (DCSI)-update and ICD-10 translation. J Diabetes Complicat. 2017;31(6):1007–13.",
"volume": "31",
"year": "2017"
},
{
"author": "BA Young",
"first-page": "15",
"issue": "1",
"journal-title": "Am J Manag Care",
"key": "1110_CR27",
"unstructured": "Young BA, Lin E, Von Korff M, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care. 2008;14(1):15–23.",
"volume": "14",
"year": "2008"
},
{
"DOI": "10.1007/978-0-387-84858-7",
"author": "T Hastie",
"doi-asserted-by": "publisher",
"edition": "2",
"key": "1110_CR28",
"unstructured": "Hastie T, Tibshirani R, Friedman JH. The elements of statistical learning: data mining, inference, and prediction. 2nd ed. New York: Pringer; 2009.",
"volume-title": "The elements of statistical learning: data mining, inference, and prediction",
"year": "2009"
},
{
"DOI": "10.1016/j.ijid.2020.03.017",
"author": "J Yang",
"doi-asserted-by": "publisher",
"first-page": "91",
"journal-title": "Int J Infect Dis",
"key": "1110_CR29",
"unstructured": "Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5.",
"volume": "94",
"year": "2020"
},
{
"DOI": "10.1136/bmj.m1198",
"author": "RE Jordan",
"doi-asserted-by": "publisher",
"first-page": "m1198",
"journal-title": "BMJ",
"key": "1110_CR30",
"unstructured": "Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198.",
"volume": "368",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"author": "N Holman",
"doi-asserted-by": "publisher",
"first-page": "823",
"issue": "10",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "1110_CR31",
"unstructured": "Holman N, Knighton P, Kar P, et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8(10):823–33.",
"volume": "8",
"year": "2020"
},
{
"key": "1110_CR32",
"unstructured": "Centers for Disease Control and Prevention (CDC). People with certain medical conditions. 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed 13 Jan 2021."
},
{
"DOI": "10.1016/j.diabres.2020.108268",
"author": "AK Singh",
"doi-asserted-by": "publisher",
"first-page": "108268",
"journal-title": "Diabetes Res Clin Pract",
"key": "1110_CR33",
"unstructured": "Singh AK, Singh R. Is metformin ahead in the race as a repurposed host-directed therapy for patients with diabetes and COVID-19? Diabetes Res Clin Pract. 2020;165:108268.",
"volume": "165",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.11.014",
"author": "B Yu",
"doi-asserted-by": "publisher",
"first-page": "65",
"issue": "1",
"journal-title": "Cell Metab",
"key": "1110_CR34",
"unstructured": "Yu B, Li C, Sun Y, Wang DW. Insulin treatment is associated with increased mortality in patients with COVID-19 and type 2 diabetes. Cell Metab. 2021;33(1):65-77.e2.",
"volume": "33",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2018.01236",
"author": "F Ursini",
"doi-asserted-by": "publisher",
"first-page": "1236",
"journal-title": "Front Immunol",
"key": "1110_CR35",
"unstructured": "Ursini F, Russo E, Pellino G, et al. Metformin and autoimmunity: a “New Deal” of an old drug. Front Immunol. 2018;9:1236.",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1016/j.diabres.2020.108183",
"author": "S Sharma",
"doi-asserted-by": "publisher",
"first-page": "108183",
"journal-title": "Diabetes Res Clin Pract",
"key": "1110_CR36",
"unstructured": "Sharma S, Ray A, Sadasivam B. Metformin in COVID-19: a possible role beyond diabetes. Diabetes Res Clin Pract. 2020;164:108183.",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa1592",
"author": "J Xu",
"doi-asserted-by": "publisher",
"first-page": "e901",
"issue": "11",
"journal-title": "Clin Infect Dis",
"key": "1110_CR37",
"unstructured": "Xu J, Teng Y, Shang L, Gu X, Fan G, Chen Y, Tian R, Zhang S, Cao B. The effect of prior ACEI/ARB treatment on COVID-19 susceptibility and outcome: a systematic review and meta-analysis. Clin Infect Dis. 2021;72(11):e901–13.",
"volume": "72",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.3594",
"author": "R Baral",
"doi-asserted-by": "publisher",
"first-page": "e213594",
"issue": "3",
"journal-title": "JAMA Netw Open",
"key": "1110_CR38",
"unstructured": "Baral R, Tsampasian V, Debski M, Moran B, Garg P, Clark A, Vassiliou VS. Association between renin-angiotensin-aldosterone system inhibitors and clinical outcomes in patients with COVID-19: a systematic review and meta-analysis. JAMA Netw Open. 2021;4(3):e213594.",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1007/s12325-021-01704-y",
"author": "M Cugno",
"doi-asserted-by": "publisher",
"first-page": "2709",
"issue": "5",
"journal-title": "Adv Ther",
"key": "1110_CR39",
"unstructured": "Cugno M, Gualtierotti R, Casazza G, Tafuri F, Ghigliazza G, Torri A, et al. Mortality in PATIENTS with COVID-19 on renin angiotensin system inhibitor long-term treatment: an observational study showing that things are not always as they seem. Adv Ther. 2021;38(5):2709–16.",
"volume": "38",
"year": "2021"
}
],
"reference-count": 39,
"references-count": 39,
"relation": {},
"score": 1,
"short-container-title": [
"Diabetes Ther"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": [
"Risk Factors Associated with COVID-19 Hospitalization and Mortality: A Large Claims-Based Analysis Among People with Type 2 Diabetes Mellitus in the United States"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "12"
}
