Impact of diabetes status and related factors on COVID-19-associated hospitalization: A nationwide retrospective cohort study of 116,370 adults with SARS-CoV-2 infection
et al., Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2022.110156, Nov 2022
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 136 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 116,370 COVID+ patients in the USA, showing higher risk of hospitalization with vitamin D deficiency/insufficiency.
This is the 150th of 228 COVID-19 sufficiency studies for vitamin D, which collectively show higher levels reduce risk with p<0.0000000001.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of hospitalization, 41.5% lower, OR 0.58, p < 0.001, high D levels (≥30ng/mL) 113,143, low D levels (<30ng/mL) 3,227, adjusted per study, inverted to make OR<1 favor high D levels (≥30ng/mL), RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Tallon et al., 15 Nov 2022, retrospective, USA, peer-reviewed, 17 authors.
Contact: erin.tallon@mail.missouri.edu.
Impact of diabetes status and related factors on COVID-19-associated hospitalization: A nationwide retrospective cohort study of 116,370 adults with SARS-CoV-2 infection
Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2022.110156
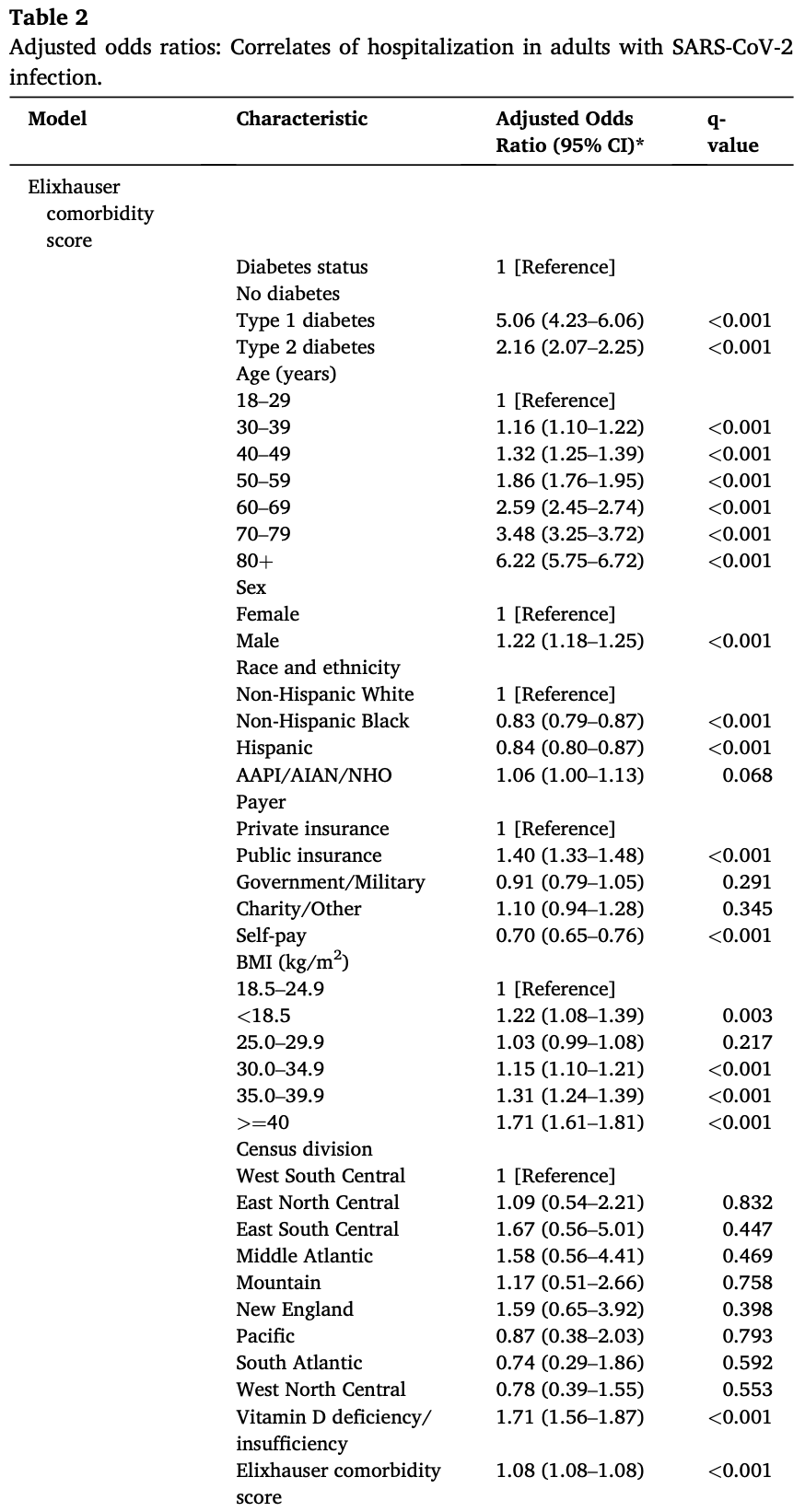
We examined diabetes status (no diabetes; type 1 diabetes [T1D]; type 2 diabetes [T2D]) and other demographic and clinical factors as correlates of coronavirus disease 2019 (COVID-19)-related hospitalization. Further, we evaluated predictors of COVID-19-related hospitalization in T1D and T2D. Methods: We analyzed electronic health record data from the de-identified COVID-19 database (December 2019 through mid-September 2020; 87 US health systems). Logistic mixed models were used to examine predictors of hospitalization at index encounters associated with confirmed SARS-CoV-2 infection. Results: In 116,370 adults (>=18 years old) with COVID-19 (93,098 no diabetes; 802 T1D; 22,470 T2D), factors that independently increased risk for hospitalization included diabetes, male sex, public health insurance, decreased body mass index (BMI; <25.0-29.9 kg/m 2 ), increased BMI (>25.0-29.9 kg/m 2 ), vitamin D deficiency/ insufficiency, and Elixhauser comorbidity score. After further adjustment for concurrent hyperglycemia and acidosis in those with diabetes, hospitalization risk was substantially higher in T1D than T2D and in those with low vitamin D and elevated hemoglobin A1c (HbA1c). Conclusions: The higher hospitalization risk in T1D versus T2D warrants further investigation. Modifiable risk factors such as vitamin D deficiency/insufficiency, BMI, and elevated HbA1c may serve as prognostic indicators for COVID-19-related hospitalization in adults with diabetes.
responsibility of the authors and does not necessarily represent the official views of the NIH.
CRediT authorship contribution statement
Appendix A. Supplementary data Supplementary data to this article can be found online at https://doi. org/10.1016/j.diabres.2022.110156.
References
Ahmed, Alotaibi, Aldubayan, Alhowail, Al-Najjar et al., Factors affecting the incidence, progression, and severity of COVID-19 in type 1 diabetes mellitus, BioMed Res Int
Barron, Bakhai, Kar, Type 1 and type 2 diabetes and COVID-19 related mortality in England: A whole population study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30272-2
Barron, Bakhai, Kar, Weaver, Bradley et al., Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: A wholepopulation study, Lancet Diabetes Endocrinol
Bellini, Cresci, Cosentino, Profili, Bartolacci et al., Obesity as a risk factor for hospitalization in COronaVirus Disease-19 (COVID-19) patients: Analysis of the Tuscany regional database, Nutrition, Metabolism and Cardiovascular Diseases
Bhatti, Raza, Shahid, Akhtar, Ahmed et al., Association between glycemic control and the outcome in hospitalized patients with COVID-19, Endocrine
Boye, Erdemir, Zimmerman, Reddy, Benneyworth et al., Risk factors associated with COVID-19 hospitalization and mortality: A large claims-based analysis among people with type 2 diabetes mellitus in the United States, Diabetes Ther
Clausen, Leo-Hansen, Faurholt-Jepsen, Krogh-Madsen, Ritz et al., Glucometabolic changes influence hospitalization and outcome in patients with COVID-19: An observational cohort study, Diabetes Res Clin Pract
Dissanayake, Silva, Sumanatilleke, Prognostic and therapeutic role of vitamin D in COVID-19: Systematic review and meta-analysis, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab892
Ehwerhemuepha, Carlson, Moog, Bondurant, Akridge et al., Cerner real-world data (CRWD) -A de-identified multicenter electronic health records database, Data Brief
Ehwerhemuepha, Gasperino, Bischoff, Taraman, Chang et al., HealtheDataLab -a cloud computing solution for data science and advanced analytics in healthcare with application to predicting multi-center pediatric readmissions, BMC Med Inform Decis Mak, doi:10.1186/s12911-020-01153-7
Elixhauser, Steiner, Harris, Coffey, Comorbidity measures for use with administrative data, Med Care
Filippo, Allora, Doga, Vitamin D levels are associated with blood glucose and bmi in COVID-19 patients, predicting disease severity, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab599
Fresán, Guevara, Elía, Albéniz, Burgui et al., Independent role of severe obesity as a risk factor for COVID-19 hospitalization: A Spanish population-based cohort study, Obesity
Ghasemian, Shamshirian, Heydari, Malekan, Alizadeh-Navaei et al., The role of vitamin D in the age of COVID-19: A systematic review and meta-analysis, Int J Clin Pract, doi:10.1111/ijcp.14675
Halpin, Rabe, Loke, Grieve, Daniele et al., Epidemiology, healthcare resource utilization, and mortality of asthma and COPD in COVID-19: A systematic literature review and meta-analyses, Journal of Asthma and Allergy
Heald, Jenkins, Williams, Sperrin, Fachim et al., The risk factors potentially influencing hospital admission in people with diabetes, following SARS-CoV-2 infection: A population-level analysis, Diabetes Ther
Holman, Knighton, Kar, 'keefe, Curley et al., Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: A population-based cohort study, Lancet Diabetes Endocrinol
Hough, Sonn, Jo, Birge, Avioli, Vitamin D metabolism in the chronic streptozotocin-induced diabetic rat, Endocrinology
Jordan, Siuka, Rotovnik, COVID-19 and Vitamin D -A systematic review, Zdr Varst, doi:10.2478/sjph-2022-0017
Khanijahani, Iezadi, Gholipour, Azami-Aghdash, Naghibi, A systematic review of racial/ethnic and socioeconomic disparities in COVID-19, Int J Equity Health, doi:10.1186/s12939-021-01582-4
Klompas, Eggleston, Mcvetta, Li, Platt, Automated detection and classification of type 1 versus type 2 diabetes using electronic health record data, Diabetes Care
Kompaniyets, Pennington, Goodman, Rosenblum, Belay et al., Underlying medical conditions and severe illness among 540,667 adults hospitalized with COVID-19, March 2020, Prev Chronic Dis, doi:10.5888/pcd18.210123
Kristófi, Bodegard, Norhammar, Thuresson, Nathanson et al., Cardiovascular and renal disease burden in type 1 compared with type 2 diabetes: A two-country nationwide observational study, Diabetes Care
Mackey, Ayers, Kondo, Saha, Advani et al., Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: A systematic review, Ann Intern Med
Magesh, John, Li, Li, Mattingly-App et al., Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status, JAMA Netw Open
Mude, Oguoma, Nyanhanda, Mwanri, Njue, Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: A systematic review and meta-analysis, J Glob Health, doi:10.7189/jogh.11.05015
Must, Anderson, Body mass index in children and adolescents: Considerations for population-based applications, Int J Obes (Lond), doi:10.1038/sj.ijo.0803300
Newton, Zollinger, Freeman, Moran, Helfand et al., Factors associated with clinical severity in emergency department patients presenting with symptomatic SARS-CoV-2 infection, J Am Coll Emerg Physicians Open, doi:10.1002/emp2.12453
Nichols, Desai, Elston, Lawrence, Connor et al., Construction of a multisite DataLink using electronic health records for the identification, surveillance, prevention, and management of diabetes mellitus: The SUPREME-DM project, Prev Chronic Dis, doi:10.5888/pcd9.110311
O'hearn, Liu, Cudhea, Coronavirus Disease, hospitalizations attributable to cardiometabolic conditions in the United States: A comparative risk assessment analysis, J Am Heart Assoc, doi:10.1161/jaha.120.019259
O'malley, Ebekozien, Desimone, COVID-19 hospitalization in adults with type 1 diabetes: Results from the T1D Exchange Multicenter Surveillance Study, J Clin Endocrinol Metab, doi:10.1210/clinem/dgaa825
Patel, Klek, Peragallo-Dittko, Goldstein, Burdge et al., Correlation of hemoglobin A1c and outcomes in patients hospitalized with COVID-19, Endocr Pract
Pereira, Damascena, Azevedo, De Almeida Oliveira, Da et al., Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis, Crit Rev Food Sci Nutr
Pietschmann, Schernthaner, Woloszczuk, Serum osteocalcin levels in diabetes mellitus: Analysis of the type of diabetes and microvascular complications, Diabetologia, doi:10.1007/bf00265373
Pinheiro, Bates, Approximations to the log-likelihood function in the nonlinear mixed-effects model, J Comput Graph Stat, doi:10.1080/10618600.1995.10474663
Quan, Sundararajan, Halfon, Fong, Burnand et al., Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data, Med Care
Raebel, Schroeder, Goodrich, Mini-Sentinel statistical methods: Validating type 1 and type 2 diabetes mellitus in the Mini-Sentinel Distributed Database
Raharja, Tamara, Kok, Association between ethnicity and severe COVID-19 disease: A systematic review and meta-analysis, J Racial Ethn Health Disparities, doi:10.1007/s40615-020-00921-5
Roncon, Zuin, Rigatelli, Zuliani, Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome, J Clin Virol
Rubin, Multiple imputation for nonresponse in surveys, doi:10.1002/9780470316696
Sathish, Cao, What is the role of admission HbA1c in managing COVID-19 patients?, J Diabetes, doi:10.1111/1753-0407.13140
Sattar, Mcinnes, Mcmurray, Obesity is a risk factor for severe COVID-19 infection, Circulation, doi:10.1161/circulationaha.120.047659
Storey, The positive false discovery rate: A Bayesian interpretation and the qvalue, Ann Stat, doi:10.2307/3448445
Sze, Pan, Nevill, Gray, Martin et al., Ethnicity and clinical outcomes in COVID-19: A systematic review and meta-analysis, EClinicalMedicine
Van Buuren, Groothuis-Oudshoorn, mice: Multivariate imputation by chained equations in R, J Stat Softw, doi:10.18637/jss.v045.i03
Van Walraven, Austin, Jennings, Quan, Forster, A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data, Med Care
DOI record:
{
"DOI": "10.1016/j.diabres.2022.110156",
"ISSN": [
"0168-8227"
],
"URL": "http://dx.doi.org/10.1016/j.diabres.2022.110156",
"alternative-id": [
"S0168822722009706"
],
"article-number": "110156",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Impact of diabetes status and related factors on COVID-19-associated hospitalization: A nationwide retrospective cohort study of 116,370 adults with SARS-CoV-2 infection"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Diabetes Research and Clinical Practice"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.diabres.2022.110156"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2022 The Authors. Published by Elsevier B.V."
}
],
"author": [
{
"affiliation": [],
"family": "Tallon",
"given": "Erin M.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ebekozien",
"given": "Osagie",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sanchez",
"given": "Janine",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Staggs",
"given": "Vincent S.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ferro",
"given": "Diana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McDonough",
"given": "Ryan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Demeterco-Berggren",
"given": "Carla",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Polsky",
"given": "Sarit",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gomez",
"given": "Patricia",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Patel",
"given": "Neha",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prahalad",
"given": "Priya",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Odugbesan",
"given": "Ori",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mathias",
"given": "Priyanka",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lee",
"given": "Joyce M.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Smith",
"given": "Chelsey",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Shyu",
"given": "Chi-Ren",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Clements",
"given": "Mark A.",
"sequence": "additional"
}
],
"container-title": "Diabetes Research and Clinical Practice",
"container-title-short": "Diabetes Research and Clinical Practice",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"diabetesresearchclinicalpractice.com",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2022,
11,
15
]
],
"date-time": "2022-11-15T07:22:50Z",
"timestamp": 1668496970000
},
"deposited": {
"date-parts": [
[
2022,
12,
3
]
],
"date-time": "2022-12-03T00:56:40Z",
"timestamp": 1670029000000
},
"indexed": {
"date-parts": [
[
2022,
12,
3
]
],
"date-time": "2022-12-03T05:46:44Z",
"timestamp": 1670046404316
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
12
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
12,
1
]
],
"date-time": "2022-12-01T00:00:00Z",
"timestamp": 1669852800000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
11,
28
]
],
"date-time": "2022-11-28T00:00:00Z",
"timestamp": 1669593600000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0168822722009706?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0168822722009706?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "110156",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
12
]
]
},
"published-print": {
"date-parts": [
[
2022,
12
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"key": "10.1016/j.diabres.2022.110156_b0005",
"unstructured": "Johns Hopkins University & Medicine. Coronavirus resource center. Available from: https://coronavirus.jhu.edu/ [Accessed: August 9, 2022]."
},
{
"key": "10.1016/j.diabres.2022.110156_b0010",
"unstructured": "Centers for Disease Control and Prevention. Underlying medical conditions associated with higher risk for severe COVID-19: Information for healthcare professionals. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html [Accessed: August 9, 2022]."
},
{
"DOI": "10.1016/j.jcv.2020.104354",
"article-title": "Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome",
"author": "Roncon",
"doi-asserted-by": "crossref",
"first-page": "104354",
"journal-title": "J Clin Virol",
"key": "10.1016/j.diabres.2022.110156_b0015",
"volume": "127",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30272-2",
"article-title": "Type 1 and type 2 diabetes and COVID-19 related mortality in England: A whole population study",
"author": "Barron",
"doi-asserted-by": "crossref",
"first-page": "813",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.1016/j.diabres.2022.110156_b0020",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1007/s13300-021-01110-1",
"article-title": "Risk factors associated with COVID-19 hospitalization and mortality: A large claims-based analysis among people with type 2 diabetes mellitus in the United States",
"author": "Boye",
"doi-asserted-by": "crossref",
"first-page": "2223",
"issue": "8",
"journal-title": "Diabetes Ther",
"key": "10.1016/j.diabres.2022.110156_b0025",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.5888/pcd18.210123",
"article-title": "Underlying medical conditions and severe illness among 540,667 adults hospitalized with COVID-19, March 2020-March 2021",
"author": "Kompaniyets",
"doi-asserted-by": "crossref",
"journal-title": "Prev Chronic Dis",
"key": "10.1016/j.diabres.2022.110156_b0030",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgab892",
"doi-asserted-by": "crossref",
"key": "10.1016/j.diabres.2022.110156_b0035",
"unstructured": "Dissanayake HA, De Silva NL, Sumanatilleke M, et al. Prognostic and therapeutic role of vitamin D in COVID-19: Systematic review and meta-analysis. J Clin Endocrinol Metab 2022; 107:1484-1502. DOI: 10.1210/clinem/dgab892."
},
{
"DOI": "10.1016/j.eclinm.2020.100630",
"article-title": "Ethnicity and clinical outcomes in COVID-19: A systematic review and meta-analysis",
"author": "Sze",
"doi-asserted-by": "crossref",
"first-page": "100630",
"journal-title": "EClinicalMedicine",
"key": "10.1016/j.diabres.2022.110156_b0040",
"volume": "29-30",
"year": "2020"
},
{
"DOI": "10.7326/M20-6306",
"article-title": "Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: A systematic review",
"author": "Mackey",
"doi-asserted-by": "crossref",
"first-page": "362",
"issue": "3",
"journal-title": "Ann Intern Med",
"key": "10.1016/j.diabres.2022.110156_b0045",
"volume": "174",
"year": "2021"
},
{
"DOI": "10.7189/jogh.11.05015",
"article-title": "Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: A systematic review and meta-analysis",
"author": "Mude",
"doi-asserted-by": "crossref",
"journal-title": "J Glob Health",
"key": "10.1016/j.diabres.2022.110156_b0050",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2021.34147",
"article-title": "Disparities in COVID-19 outcomes by race, ethnicity, and socioeconomic status",
"author": "Magesh",
"doi-asserted-by": "crossref",
"first-page": "e2134147",
"issue": "11",
"journal-title": "JAMA Netw Open",
"key": "10.1016/j.diabres.2022.110156_b0055",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1186/s12939-021-01582-4",
"article-title": "A systematic review of racial/ethnic and socioeconomic disparities in COVID-19",
"author": "Khanijahani",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "Int J Equity Health",
"key": "10.1016/j.diabres.2022.110156_b0060",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1007/s40615-020-00921-5",
"article-title": "Association between ethnicity and severe COVID-19 disease: A systematic review and meta-analysis",
"author": "Raharja",
"doi-asserted-by": "crossref",
"first-page": "1563",
"journal-title": "J Racial Ethn Health Disparities",
"key": "10.1016/j.diabres.2022.110156_b0065",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/j.dib.2022.108120",
"article-title": "Cerner real-world data (CRWD) - A de-identified multicenter electronic health records database",
"author": "Ehwerhemuepha",
"doi-asserted-by": "crossref",
"first-page": "108120",
"journal-title": "Data Brief",
"key": "10.1016/j.diabres.2022.110156_b0070",
"volume": "42",
"year": "2022"
},
{
"key": "10.1016/j.diabres.2022.110156_b0075",
"unstructured": "Cerner Corporation. Cerner Real-World Data (CRWD) 2020Q3 COVID database data dictionary. 2020."
},
{
"DOI": "10.5888/pcd9.110311",
"article-title": "Construction of a multisite DataLink using electronic health records for the identification, surveillance, prevention, and management of diabetes mellitus: The SUPREME-DM project",
"author": "Nichols",
"doi-asserted-by": "crossref",
"journal-title": "Prev Chronic Dis",
"key": "10.1016/j.diabres.2022.110156_b0080",
"year": "2012"
},
{
"key": "10.1016/j.diabres.2022.110156_b0085",
"unstructured": "Raebel MA, Schroeder EB, Goodrich G, et al. Mini-Sentinel statistical methods: Validating type 1 and type 2 diabetes mellitus in the Mini-Sentinel Distributed Database using the SUrveillance, PREvention, and ManagEment of Diabetes Mellitus (SUPREME-DM) DataLink. Available from: https://www.sentinelinitiative.org/sites/default/files/Methods/Mini-Sentinel_Methods_Validating-Diabetes-Mellitus_MSDD_Using-SUPREME-DM-DataLink.pdf [Accessed: August 9, 2022]."
},
{
"DOI": "10.2337/dc12-0964",
"article-title": "Automated detection and classification of type 1 versus type 2 diabetes using electronic health record data",
"author": "Klompas",
"doi-asserted-by": "crossref",
"first-page": "914",
"issue": "4",
"journal-title": "Diabetes Care",
"key": "10.1016/j.diabres.2022.110156_b0090",
"volume": "36",
"year": "2013"
},
{
"DOI": "10.1038/sj.ijo.0803300",
"doi-asserted-by": "crossref",
"key": "10.1016/j.diabres.2022.110156_b0095",
"unstructured": "Must A, Anderson SE. Body mass index in children and adolescents: Considerations for population-based applications. Int J Obes (Lond) 2006; 30:590-4. DOI: 10.1038/sj.ijo.0803300."
},
{
"DOI": "10.1097/MLR.0b013e31819432e5",
"article-title": "A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data",
"author": "van Walraven",
"doi-asserted-by": "crossref",
"first-page": "626",
"issue": "6",
"journal-title": "Med Care",
"key": "10.1016/j.diabres.2022.110156_b0100",
"volume": "47",
"year": "2009"
},
{
"DOI": "10.1097/01.mlr.0000182534.19832.83",
"article-title": "Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data",
"author": "Quan",
"doi-asserted-by": "crossref",
"first-page": "1130",
"issue": "11",
"journal-title": "Med Care",
"key": "10.1016/j.diabres.2022.110156_b0105",
"volume": "43",
"year": "2005"
},
{
"DOI": "10.1097/00005650-199801000-00004",
"article-title": "Comorbidity measures for use with administrative data",
"author": "Elixhauser",
"doi-asserted-by": "crossref",
"first-page": "8",
"issue": "1",
"journal-title": "Med Care",
"key": "10.1016/j.diabres.2022.110156_b0110",
"volume": "36",
"year": "1998"
},
{
"DOI": "10.1186/s12911-020-01153-7",
"article-title": "HealtheDataLab – a cloud computing solution for data science and advanced analytics in healthcare with application to predicting multi-center pediatric readmissions",
"author": "Ehwerhemuepha",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "BMC Med Inform Decis Mak",
"key": "10.1016/j.diabres.2022.110156_b0115",
"volume": "20",
"year": "2020"
},
{
"article-title": "mice: Multivariate imputation by chained equations in R",
"author": "van Buuren",
"first-page": "1",
"journal-title": "J Stat Softw",
"key": "10.1016/j.diabres.2022.110156_b0120",
"volume": "45",
"year": "2011"
},
{
"article-title": "Approximations to the log-likelihood function in the nonlinear mixed-effects model",
"author": "Pinheiro",
"first-page": "12",
"journal-title": "J Comput Graph Stat",
"key": "10.1016/j.diabres.2022.110156_b0125",
"volume": "4",
"year": "1995"
},
{
"DOI": "10.1002/9780470316696",
"doi-asserted-by": "crossref",
"key": "10.1016/j.diabres.2022.110156_b0130",
"unstructured": "Rubin D. Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons, Inc.; 1987. Accessed August 9, 2022. Available from: https://onlinelibrary.wiley.com/doi/book/10.1002/9780470316696. DOI: 10.1002/9780470316696."
},
{
"DOI": "10.1214/aos/1074290335",
"doi-asserted-by": "crossref",
"key": "10.1016/j.diabres.2022.110156_b0135",
"unstructured": "Storey J. The positive false discovery rate: A Bayesian interpretation and the q-value. Ann Stat 2003; 31:2013-35. DOI: https://doi.org/10.2307/3448445."
},
{
"DOI": "10.1007/s13300-022-01230-2",
"article-title": "The risk factors potentially influencing hospital admission in people with diabetes, following SARS-CoV-2 infection: A population-level analysis",
"author": "Heald",
"doi-asserted-by": "crossref",
"first-page": "1007",
"issue": "5",
"journal-title": "Diabetes Ther",
"key": "10.1016/j.diabres.2022.110156_b0140",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/S2213-8587(20)30272-2",
"article-title": "Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: A whole-population study",
"author": "Barron",
"doi-asserted-by": "crossref",
"first-page": "813",
"issue": "10",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.1016/j.diabres.2022.110156_b0145",
"volume": "8",
"year": "2020"
},
{
"article-title": "hospitalizations attributable to cardiometabolic conditions in the United States: A comparative risk assessment analysis",
"author": "O’Hearn",
"first-page": "10",
"journal-title": "J Am Heart Assoc",
"key": "10.1016/j.diabres.2022.110156_b0150",
"volume": "2021",
"year": "2019"
},
{
"DOI": "10.2337/dc20-2839",
"article-title": "Cardiovascular and renal disease burden in type 1 compared with type 2 diabetes: A two-country nationwide observational study",
"author": "Kristófi",
"doi-asserted-by": "crossref",
"first-page": "1211",
"issue": "5",
"journal-title": "Diabetes Care",
"key": "10.1016/j.diabres.2022.110156_b0155",
"volume": "44",
"year": "2021"
},
{
"article-title": "Factors associated with clinical severity in emergency department patients presenting with symptomatic SARS-CoV-2 infection",
"author": "Newton",
"issue": "4",
"journal-title": "J Am Coll Emerg Physicians Open",
"key": "10.1016/j.diabres.2022.110156_b0160",
"volume": "2",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgaa825",
"doi-asserted-by": "crossref",
"key": "10.1016/j.diabres.2022.110156_b0165",
"unstructured": "O’Malley G, Ebekozien O, Desimone M, et al. COVID-19 hospitalization in adults with type 1 diabetes: Results from the T1D Exchange Multicenter Surveillance Study. J Clin Endocrinol Metab 2021; 106:e936-e942. DOI: https://doi.org/10.1210/clinem/dgaa825."
},
{
"DOI": "10.1002/oby.23029",
"article-title": "Independent role of severe obesity as a risk factor for COVID-19 hospitalization: A Spanish population-based cohort study",
"author": "Fresán",
"doi-asserted-by": "crossref",
"first-page": "29",
"issue": "1",
"journal-title": "Obesity",
"key": "10.1016/j.diabres.2022.110156_b0170",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1016/j.numecd.2020.11.030",
"article-title": "Obesity as a risk factor for hospitalization in COronaVirus Disease-19 (COVID-19) patients: Analysis of the Tuscany regional database",
"author": "Bellini",
"doi-asserted-by": "crossref",
"first-page": "769",
"issue": "3",
"journal-title": "Nutrition, Metabolism and Cardiovascular Diseases",
"key": "10.1016/j.diabres.2022.110156_b0175",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.1080/10408398.2020.1841090",
"article-title": "Vitamin D deficiency aggravates COVID-19: Systematic review and meta-analysis",
"author": "Pereira",
"doi-asserted-by": "crossref",
"first-page": "1308",
"issue": "5",
"journal-title": "Crit Rev Food Sci Nutr",
"key": "10.1016/j.diabres.2022.110156_b0180",
"volume": "62",
"year": "2022"
},
{
"DOI": "10.1111/ijcp.14675",
"article-title": "The role of vitamin D in the age of COVID-19: A systematic review and meta-analysis",
"author": "Ghasemian",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "Int J Clin Pract",
"key": "10.1016/j.diabres.2022.110156_b0185",
"volume": "75",
"year": "2021"
},
{
"DOI": "10.2478/sjph-2022-0017",
"doi-asserted-by": "crossref",
"key": "10.1016/j.diabres.2022.110156_b0190",
"unstructured": "Jordan T, Siuka D, Rotovnik NK, et al. COVID-19 and Vitamin D – A systematic review. Zdr Varst 2022; 61:124-132. DOI: https://doi.org/10.2478/sjph-2022-0017."
},
{
"article-title": "Factors affecting the incidence, progression, and severity of COVID-19 in type 1 diabetes mellitus",
"author": "Ahmed",
"first-page": "1",
"journal-title": "BioMed Res Int",
"key": "10.1016/j.diabres.2022.110156_b0195",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1007/s12020-022-03078-9",
"article-title": "Association between glycemic control and the outcome in hospitalized patients with COVID-19",
"author": "Bhatti",
"doi-asserted-by": "crossref",
"first-page": "213",
"issue": "2",
"journal-title": "Endocrine",
"key": "10.1016/j.diabres.2022.110156_b0200",
"volume": "77",
"year": "2022"
},
{
"DOI": "10.1016/j.diabres.2022.109880",
"article-title": "Glucometabolic changes influence hospitalization and outcome in patients with COVID-19: An observational cohort study",
"author": "Clausen",
"doi-asserted-by": "crossref",
"first-page": "109880",
"journal-title": "Diabetes Res Clin Pract",
"key": "10.1016/j.diabres.2022.110156_b0205",
"volume": "187",
"year": "2022"
},
{
"DOI": "10.1111/1753-0407.13140",
"article-title": "What is the role of admission HbA1c in managing COVID-19 patients?",
"author": "Sathish",
"doi-asserted-by": "crossref",
"first-page": "273",
"journal-title": "J Diabetes",
"key": "10.1016/j.diabres.2022.110156_b0210",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/j.eprac.2021.07.008",
"article-title": "Correlation of hemoglobin A1c and outcomes in patients hospitalized with COVID-19",
"author": "Patel",
"doi-asserted-by": "crossref",
"first-page": "1046",
"issue": "10",
"journal-title": "Endocr Pract",
"key": "10.1016/j.diabres.2022.110156_b0215",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgab599",
"doi-asserted-by": "crossref",
"key": "10.1016/j.diabres.2022.110156_b0220",
"unstructured": "Di Filippo L, Allora A, Doga M, et al. Vitamin D levels are associated with blood glucose and bmi in COVID-19 patients, predicting disease severity. J Clin Endocrinol Metab 2022; 107:e348-e360. DOI: https://doi.org/10.1210/clinem/dgab599."
},
{
"DOI": "10.1007/BF00265373",
"doi-asserted-by": "crossref",
"key": "10.1016/j.diabres.2022.110156_b0225",
"unstructured": "Pietschmann P, Schernthaner G, Woloszczuk W. Serum osteocalcin levels in diabetes mellitus: Analysis of the type of diabetes and microvascular complications. Diabetologia 1988; 31:892-5. DOI: https://doi.org/10.1007/bf00265373."
},
{
"DOI": "10.1210/endo-113-2-790",
"article-title": "Vitamin D metabolism in the chronic streptozotocin-induced diabetic rat",
"author": "Hough",
"doi-asserted-by": "crossref",
"first-page": "790",
"issue": "2",
"journal-title": "Endocrinology",
"key": "10.1016/j.diabres.2022.110156_b0230",
"volume": "113",
"year": "1983"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"article-title": "Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: A population-based cohort study",
"author": "Holman",
"doi-asserted-by": "crossref",
"first-page": "823",
"issue": "10",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "10.1016/j.diabres.2022.110156_b0235",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047659",
"article-title": "Obesity is a risk factor for severe COVID-19 infection",
"author": "Sattar",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "Circulation",
"key": "10.1016/j.diabres.2022.110156_b0240",
"volume": "142",
"year": "2020"
},
{
"DOI": "10.2147/JAA.S360985",
"article-title": "Epidemiology, healthcare resource utilization, and mortality of asthma and COPD in COVID-19: A systematic literature review and meta-analyses",
"author": "Halpin",
"doi-asserted-by": "crossref",
"first-page": "811",
"journal-title": "Journal of Asthma and Allergy",
"key": "10.1016/j.diabres.2022.110156_b0245",
"volume": "Volume 15",
"year": "2022"
}
],
"reference-count": 49,
"references-count": 49,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0168822722009706"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology",
"General Medicine",
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": "Impact of diabetes status and related factors on COVID-19-associated hospitalization: A nationwide retrospective cohort study of 116,370 adults with SARS-CoV-2 infection",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "194"
}
