Evaluation and management of COVID-19-related severity in people with type 2 diabetes
et al., BMJ Open Diabetes Research & Care, doi:10.1136/bmjdrc-2021-002299, Sep 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 16,504 COVID-19 type 2 diabetes patients, showing lower risk of ICU admission with existing metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of ICU admission, 12.0% lower, RR 0.88, p = 0.005, treatment 6,504, control 10,000, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Wang et al., 7 Sep 2021, retrospective, USA, peer-reviewed, 4 authors.
Evaluation and management of COVID-19-related severity in people with type 2 diabetes
BMJ Open Diabetes Research & Care, doi:10.1136/bmjdrc-2021-002299
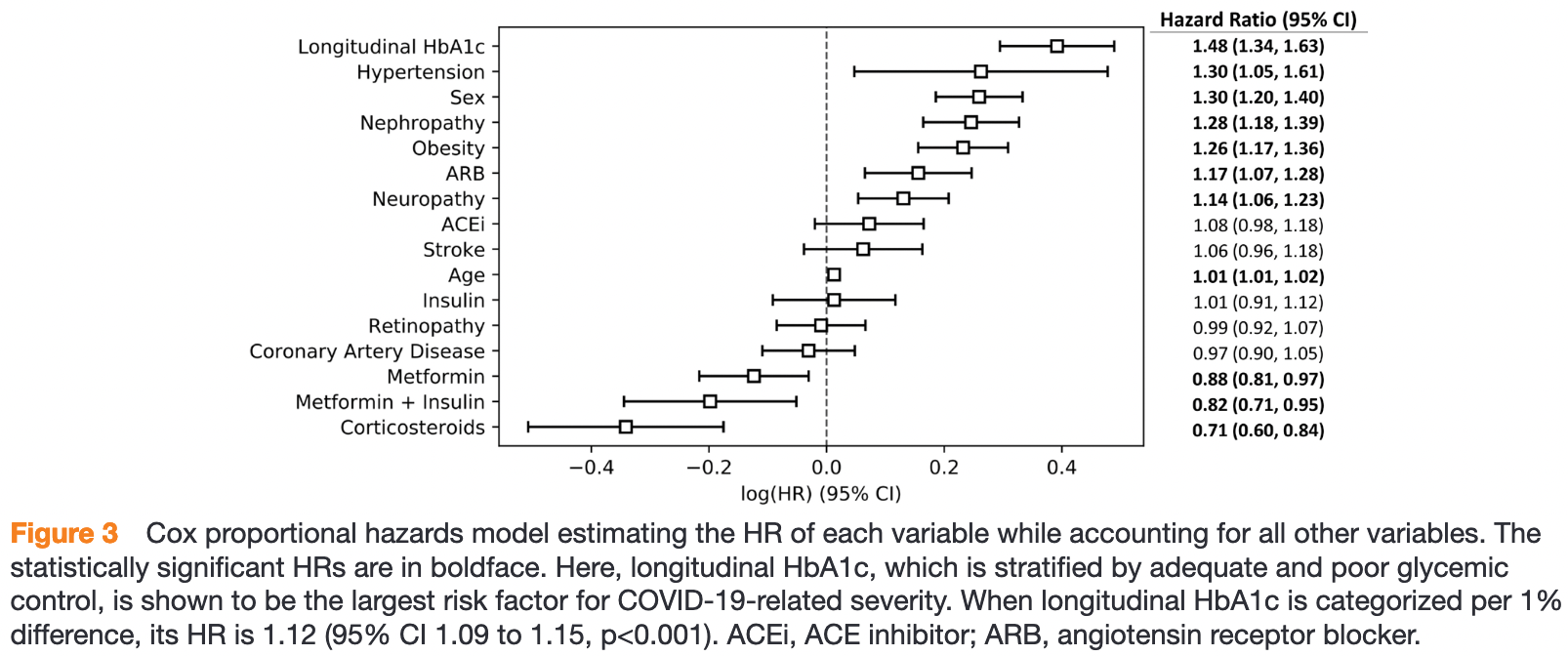
Introduction People with type 2 diabetes (T2D) have an increased rate of hospitalization and mortality related to COVID-19. To identify ahead of time those who are at risk of developing severe diseases and potentially in need of intensive care, we investigated the independent associations between longitudinal glycated hemoglobin (HbA1c), the impact of common medications (metformin, insulin, ACE inhibitors (ACEIs), angiotensin receptor blockers (ARBs), and corticosteroids) and COVID-19 severity in people with T2D. Research design and methods Retrospective cohort study was conducted using deidentified claims and electronic health record data from the OptumLabs Data Warehouse across the USA between January 2017 and November 2020, including 16 504 individuals with T2D and COVID-19. A univariate model and a multivariate model were applied to evaluate the association between 2 and 3-year HbA1c average, medication use between COVID-19 diagnosis and intensive care unit admission (if applicable), and risk of intensive care related to COVID-19. Results With covariates adjusted, the HR of longitudinal HbA1c for risk of intensive care was 1.12 (per 1% increase, p<0.001) and 1.48 (comparing group with poor (HbA1c ≥9%) and adequate glycemic control (HbA1c 6%-9%), p<0.001). The use of corticosteroids and the combined use of insulin and metformin were associated with significant reduction of intensive care risk, while ACEIs and ARBs were not associated with reduced risk of intensive care. Conclusions Two to three-year longitudinal glycemic level is independently associated with COVID-19-related severity in people with T2D. Here, we present a potential method to use HbA1c history, which presented a stronger association with COVID-19 severity than single-point HbA1c, to identify in advance those more at risk of intensive care due to COVID-19 in the T2D population. The combined use of metformin and insulin and the use of corticosteroids might be significant to prevent patients with T2D from becoming critically ill from COVID-19.
How might these results change the focus of research or clinical practice? ► The study emphasizes the importance of proper management glycemic level over longer period in reducing the risk of developing severe diseases from COVID-19. The method using HbA1c history could allow for personalized assessment and management of subsequent care related to COVID-19 in advance. copyright.
Competing interests None declared.
Patient consent for publication Not required. Ethics approval This study involves human participants, but the Institutional Review Board at Rensselaer Polytechnic Institute exempted this study. Patient identifiers have been coded or removed prior to its release to the study investigators, such that it is compliant with HIPAA and exempt from Institutional Review Board review. Provenance and peer review Not commissioned; externally peer reviewed. Data availability statement Data may be obtained from a third party and are not publicly available. The data that support the findings of this study are available from OptumLabs Data Warehouse. Restrictions apply to the availability of these data, which were used under license for this study. Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Open..
References
Apicella, Campopiano, Mantuano, COVID-19 in people with diabetes: understanding the reasons for worse outcomes, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30238-2
Ardigo, Valtuena, Zavaroni, Pulmonary complications in diabetes mellitus: the role of glycemic control, Curr Drug Targets Inflamm Allergy, doi:10.2174/1568010042634488
Bernal, Andrews, Gower, Effectiveness of Covid-19 vaccines against the B.1.617.2 (delta) variant, N Engl J Med, doi:10.1056/NEJMoa2108891
Bouhanick, Cracowski, Diabetes, And COVID-19, Therapies
Cano, Fuentes, Campioli, Impact of corticosteroids in coronavirus disease 2019 outcomes: systematic review and meta-analysis, Chest, doi:10.1016/j.chest.2020.10.054
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Chen, Yang, Cheng, Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care, doi:10.2337/dc20-0660
Chiang, Bai, Lin, The influence of diabetes, glycemic control, and diabetes-related comorbidities on pulmonary tuberculosis, PLoS One, doi:10.1371/journal.pone.0121698
Conlen, Keefe, Leatherby, How full are hospital I.C.U.s near you? The
Crouse, Grimes, Li, Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes, medRxiv, doi:10.1101/2020.07.29.20164020
Diabetes, Diagnosis and classification of diabetes mellitus, Diabetes Care, doi:10.2337/dc12-s064
Egbuonu, Antonio, Edavalath, Effect of inhaled corticosteroids on glycemic status, Open Respir Med J, doi:10.2174/1874306401408010101
Feldman, Cohen-Stavi, Leibowitz, Defining the role of medication adherence in poor glycemic control among a general adult population with diabetes, PLoS One, doi:10.1371/journal.pone.0108145
Ferlita, Yegiazaryan, Noori, Type 2 Diabetes Mellitus and Altered Immune System Leading to Susceptibility to Pathogens, Especially Mycobacterium tuberculosis, J Clin Med, doi:10.3390/jcm8122219
Hang, Panther user guide: data overview and use in applied research
Hayek, Ben-Shlomo, Balicer, Preinfection glycaemic control and disease severity among patients with type 2 diabetes and COVID-19: a retrospective, cohort study, Diabetes Obes Metab, doi:10.1111/dom.14393
Holman, Knighton, Kar, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30271-0
Jin, Bai, He, Gender differences in patients with COVID-19: focus on severity and mortality, Front Public Health, doi:10.3389/fpubh.2020.00152
Juarez, Sentell, Tokumaru, Factors associated with poor glycemic control or wide glycemic variability among diabetes patients in Hawaii, 2006-2009, Prev Chronic Dis, doi:10.5888/pcd9.120065
Liang, Xu, The association of diabetes with COVID-19 disease severity: evidence from adjusted effect estimates, Hormones, doi:10.1007/s42000-020-00259-x
Luo, Lim, Tan, Longitudinal trends in HbA1c and associations with comorbidity and all-cause mortality in Asian patients with type 2 diabetes: a cohort study, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2017.08.013
Onweni, Zhang, Caulfield, ACEI/ARB therapy in COVID-19: the double-edged sword of ACE2 and SARS-CoV-2 viral docking, Crit Care, doi:10.1186/s13054-020-03195-9
Papadokostaki, Tentolouris, Liberopoulos, COVID-19 and diabetes: what does the clinician need to know?, Prim Care Diabetes, doi:10.1016/j.pcd.2020.06.010
Pradhan, Olsson, Sex differences in severity and mortality from COVID-19: are males more vulnerable?, Biol Sex Differ, doi:10.1186/s13293-020-00330-7
Ritchie, Ortiz-Ospina, Beltekian, Coronavirus pandemic (COVID-19)
Scheen, Metformin, Metformin and COVID-19: from cellular mechanisms to reduced mortality, Diabetes Metab, doi:10.1016/j.diabet.2020.07.006
Sterne, Diaz, Villar, Corticosteroid therapy for critically ill patients with COVID-19: a structured summary of a study protocol for a prospective meta-analysis of randomized trials, Trials, doi:10.1186/s13063-020-04641-3
Sterne, Murthy, Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis, JAMA, doi:10.1001/jama.2020.17023
Wang, Wang, Poundarik, Fracture risk in type 2 diabetes: longitudinal glycemic control based prediction and the efficacy of medications, Journal of Bone and Mineral Research
Who, WHO coronavirus (COVID-19) dashboard
Xu, Liu, Zhang, Does hereditary angioedema make COVID-19 worse?, World Allergy Organ J, doi:10.1016/j.waojou.2020.100454
Yang, Yu, Xu, Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a singlecentered, retrospective, observational study, Lancet Respir Med, doi:10.1016/S2213-2600(20)30079-5
Zhang, Dong, Cao, Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China, Allergy, doi:10.1111/all.14238
Zhang, Zhu, Cai, Peng, Lihua et al., Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19, Circ Res, doi:10.1161/CIRCRESAHA.120.317134
Zhu, She, Cheng, Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.04.021
DOI record:
{
"DOI": "10.1136/bmjdrc-2021-002299",
"ISSN": [
"2052-4897"
],
"URL": "http://dx.doi.org/10.1136/bmjdrc-2021-002299",
"abstract": "<jats:sec><jats:title>Introduction</jats:title><jats:p>People with type 2 diabetes (T2D) have an increased rate of hospitalization and mortality related to COVID-19. To identify ahead of time those who are at risk of developing severe diseases and potentially in need of intensive care, we investigated the independent associations between longitudinal glycated hemoglobin (HbA1c), the impact of common medications (metformin, insulin, ACE inhibitors (ACEIs), angiotensin receptor blockers (ARBs), and corticosteroids) and COVID-19 severity in people with T2D.</jats:p></jats:sec><jats:sec><jats:title>Research design and methods</jats:title><jats:p>Retrospective cohort study was conducted using deidentified claims and electronic health record data from the OptumLabs Data Warehouse across the USA between January 2017 and November 2020, including 16 504 individuals with T2D and COVID-19. A univariate model and a multivariate model were applied to evaluate the association between 2 and 3-year HbA1c average, medication use between COVID-19 diagnosis and intensive care unit admission (if applicable), and risk of intensive care related to COVID-19.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>With covariates adjusted, the HR of longitudinal HbA1c for risk of intensive care was 1.12 (per 1% increase, p<0.001) and 1.48 (comparing group with poor (HbA1c ≥9%) and adequate glycemic control (HbA1c 6%–9%), p<0.001). The use of corticosteroids and the combined use of insulin and metformin were associated with significant reduction of intensive care risk, while ACEIs and ARBs were not associated with reduced risk of intensive care.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>Two to three-year longitudinal glycemic level is independently associated with COVID-19-related severity in people with T2D. Here, we present a potential method to use HbA1c history, which presented a stronger association with COVID-19 severity than single-point HbA1c, to identify in advance those more at risk of intensive care due to COVID-19 in the T2D population. The combined use of metformin and insulin and the use of corticosteroids might be significant to prevent patients with T2D from becoming critically ill from COVID-19.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjdrc-2021-002299"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-0049-1623",
"affiliation": [],
"authenticated-orcid": false,
"family": "Wang",
"given": "Bowen",
"sequence": "first"
},
{
"affiliation": [],
"family": "Glicksberg",
"given": "Benjamin S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Nadkarni",
"given": "Girish N",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Vashishth",
"given": "Deepak",
"sequence": "additional"
}
],
"container-title": [
"BMJ Open Diabetes Research & Care"
],
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2021,
9,
7
]
],
"date-time": "2021-09-07T16:35:13Z",
"timestamp": 1631032513000
},
"deposited": {
"date-parts": [
[
2021,
9,
7
]
],
"date-time": "2021-09-07T16:35:44Z",
"timestamp": 1631032544000
},
"funder": [
{
"DOI": "10.13039/100000069",
"award": [
"R21AR071681"
],
"doi-asserted-by": "crossref",
"name": "National Institute of Arthritis and Musculoskeletal and Skin Diseases"
}
],
"indexed": {
"date-parts": [
[
2021,
12,
12
]
],
"date-time": "2021-12-12T02:21:16Z",
"timestamp": 1639275676791
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "electronic",
"value": "2052-4897"
}
],
"issue": "1",
"issued": {
"date-parts": [
[
2021,
9
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2021,
9,
7
]
]
},
"published-print": {
"date-parts": [
[
2021,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 6,
"start": {
"date-parts": [
[
2021,
9,
7
]
],
"date-time": "2021-09-07T00:00:00Z",
"timestamp": 1630972800000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjdrc-2021-002299",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e002299",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2021,
9
]
]
},
"published-online": {
"date-parts": [
[
2021,
9,
7
]
]
},
"published-print": {
"date-parts": [
[
2021,
9
]
]
},
"publisher": "BMJ",
"reference": [
{
"key": "2021090709350734000_9.1.e002299.1",
"unstructured": "WHO . WHO coronavirus (COVID-19) dashboard, 2021. Available: https://covid19.who.int"
},
{
"key": "2021090709350734000_9.1.e002299.2",
"unstructured": "Ritchie H , Ortiz-Ospina E , Beltekian D . Coronavirus pandemic (COVID-19). Our World Data, 2020. Available: https://ourworldindata.org/covid-vaccinations"
},
{
"DOI": "10.1056/NEJMoa2108891",
"article-title": "Effectiveness of Covid-19 vaccines against the B.1.617.2 (delta) variant",
"author": "Lopez Bernal",
"doi-asserted-by": "crossref",
"first-page": "585",
"journal-title": "N Engl J Med",
"key": "2021090709350734000_9.1.e002299.3",
"volume": "385",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(20)30238-2",
"article-title": "COVID-19 in people with diabetes: understanding the reasons for worse outcomes",
"author": "Apicella",
"doi-asserted-by": "crossref",
"first-page": "782",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2021090709350734000_9.1.e002299.4",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30079-5",
"article-title": "Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "475",
"journal-title": "Lancet Respir Med",
"key": "2021090709350734000_9.1.e002299.5",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1111/all.14238",
"doi-asserted-by": "publisher",
"key": "2021090709350734000_9.1.e002299.6"
},
{
"DOI": "10.1007/s42000-020-00259-x",
"article-title": "The association of diabetes with COVID-19 disease severity: evidence from adjusted effect estimates",
"author": "Liang",
"doi-asserted-by": "crossref",
"journal-title": "Hormones",
"key": "2021090709350734000_9.1.e002299.7",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"article-title": "Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study",
"author": "Holman",
"doi-asserted-by": "crossref",
"first-page": "823",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2021090709350734000_9.1.e002299.8",
"volume": "8",
"year": "2020"
},
{
"key": "2021090709350734000_9.1.e002299.9",
"unstructured": "Conlen M , Keefe J , Leatherby L , et al . How full are hospital I.C.U.s near you? The New York Times, 2020. Available: https://www.nytimes.com/interactive/2020/us/covid-hospitals-near-you.html"
},
{
"DOI": "10.3390/jcm8122219",
"article-title": "Type 2 Diabetes Mellitus and Altered Immune System Leading to Susceptibility to Pathogens, Especially Mycobacterium tuberculosis",
"author": "Ferlita",
"doi-asserted-by": "crossref",
"journal-title": "J Clin Med",
"key": "2021090709350734000_9.1.e002299.10",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.2174/1568010042634488",
"doi-asserted-by": "publisher",
"key": "2021090709350734000_9.1.e002299.11"
},
{
"article-title": "Diagnosis and classification of diabetes mellitus",
"first-page": "S64",
"journal-title": "Diabetes Care",
"key": "2021090709350734000_9.1.e002299.12",
"volume": "35 Suppl 1",
"year": "2012"
},
{
"article-title": "Fracture risk in type 2 diabetes: longitudinal glycemic control based prediction and the efficacy of medications",
"author": "Wang",
"first-page": "30",
"journal-title": "Journal of Bone and Mineral Research",
"key": "2021090709350734000_9.1.e002299.13",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1016/j.pcd.2020.06.010",
"article-title": "COVID-19 and diabetes: what does the clinician need to know?",
"author": "Papadokostaki",
"doi-asserted-by": "crossref",
"first-page": "558",
"journal-title": "Prim Care Diabetes",
"key": "2021090709350734000_9.1.e002299.14",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1016/j.therap.2020.05.006",
"article-title": "And COVID-19",
"author": "Bouhanick",
"doi-asserted-by": "crossref",
"first-page": "327",
"journal-title": "Therapies",
"key": "2021090709350734000_9.1.e002299.15",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.07.006",
"article-title": "Metformin and COVID-19: from cellular mechanisms to reduced mortality",
"author": "Scheen",
"doi-asserted-by": "crossref",
"first-page": "423-426",
"journal-title": "Diabetes Metab",
"key": "2021090709350734000_9.1.e002299.16",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.chest.2020.10.054",
"article-title": "Impact of corticosteroids in coronavirus disease 2019 outcomes: systematic review and meta-analysis",
"author": "Cano",
"doi-asserted-by": "crossref",
"first-page": "1019",
"journal-title": "Chest",
"key": "2021090709350734000_9.1.e002299.17",
"volume": "159",
"year": "2021"
},
{
"DOI": "10.1186/s13063-020-04641-3",
"article-title": "Corticosteroid therapy for critically ill patients with COVID-19: a structured summary of a study protocol for a prospective meta-analysis of randomized trials",
"author": "Sterne",
"doi-asserted-by": "crossref",
"journal-title": "Trials",
"key": "2021090709350734000_9.1.e002299.18",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.2174/1874306401408010101",
"article-title": "Effect of inhaled corticosteroids on glycemic status",
"author": "Egbuonu",
"doi-asserted-by": "crossref",
"first-page": "101",
"journal-title": "Open Respir Med J",
"key": "2021090709350734000_9.1.e002299.19",
"volume": "8",
"year": "2014"
},
{
"DOI": "10.1186/s13054-020-03195-9",
"article-title": "ACEI/ARB therapy in COVID-19: the double-edged sword of ACE2 and SARS-CoV-2 viral docking",
"author": "Onweni",
"doi-asserted-by": "crossref",
"first-page": "475",
"journal-title": "Crit Care",
"key": "2021090709350734000_9.1.e002299.20",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.2337/dc20-0660",
"doi-asserted-by": "publisher",
"key": "2021090709350734000_9.1.e002299.21"
},
{
"DOI": "10.1161/CIRCRESAHA.120.317134",
"article-title": "Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "1671",
"journal-title": "Circ Res",
"key": "2021090709350734000_9.1.e002299.22",
"volume": "126",
"year": "2020"
},
{
"key": "2021090709350734000_9.1.e002299.23",
"unstructured": "OptumLabs . OptumLabs and OptumLabs data warehouse (OLDW) descriptions and citation. PDF. Reproduced with permission from OptumLabs. Eden prairie, MN: OptumLabs, 2020."
},
{
"key": "2021090709350734000_9.1.e002299.24",
"unstructured": "Hang L . Panther user guide: data overview and use in applied research. n.p.. PDF. Reproduced with permission from OptumLabs. Cambridge, MA: OptumLabs, 2021."
},
{
"DOI": "10.5888/pcd9.120065",
"doi-asserted-by": "publisher",
"key": "2021090709350734000_9.1.e002299.25"
},
{
"DOI": "10.1371/journal.pone.0108145",
"article-title": "Defining the role of medication adherence in poor glycemic control among a general adult population with diabetes",
"author": "Feldman",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One",
"key": "2021090709350734000_9.1.e002299.26",
"volume": "9",
"year": "2014"
},
{
"DOI": "10.1371/journal.pone.0121698",
"doi-asserted-by": "publisher",
"key": "2021090709350734000_9.1.e002299.27"
},
{
"DOI": "10.1016/j.diabres.2017.08.013",
"article-title": "Longitudinal trends in HbA1c and associations with comorbidity and all-cause mortality in Asian patients with type 2 diabetes: a cohort study",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "69",
"journal-title": "Diabetes Res Clin Pract",
"key": "2021090709350734000_9.1.e002299.28",
"volume": "133",
"year": "2017"
},
{
"DOI": "10.1186/s13293-020-00330-7",
"article-title": "Sex differences in severity and mortality from COVID-19: are males more vulnerable?",
"author": "Pradhan",
"doi-asserted-by": "crossref",
"journal-title": "Biol Sex Differ",
"key": "2021090709350734000_9.1.e002299.29",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2020.00152",
"doi-asserted-by": "crossref",
"key": "2021090709350734000_9.1.e002299.30",
"unstructured": "Jin J-M , Bai P , He W , et al . Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health 2020;8.doi:10.3389/fpubh.2020.00152"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"doi-asserted-by": "publisher",
"key": "2021090709350734000_9.1.e002299.31"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"doi-asserted-by": "publisher",
"key": "2021090709350734000_9.1.e002299.32"
},
{
"DOI": "10.1111/dom.14393",
"article-title": "Preinfection glycaemic control and disease severity among patients with type 2 diabetes and COVID-19: a retrospective, cohort study",
"author": "Hayek",
"doi-asserted-by": "crossref",
"first-page": "1995",
"journal-title": "Diabetes Obes Metab",
"key": "2021090709350734000_9.1.e002299.33",
"volume": "23",
"year": "2021"
},
{
"article-title": "Metformin use is associated with reduced mortality in a diverse population with COVID-19 and diabetes",
"author": "Crouse",
"journal-title": "medRxiv",
"key": "2021090709350734000_9.1.e002299.34",
"year": "2020"
},
{
"DOI": "10.1016/j.waojou.2020.100454",
"article-title": "Does hereditary angioedema make COVID-19 worse?",
"author": "Xu",
"doi-asserted-by": "crossref",
"first-page": "100454",
"journal-title": "World Allergy Organ J",
"key": "2021090709350734000_9.1.e002299.35",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.17023",
"doi-asserted-by": "publisher",
"key": "2021090709350734000_9.1.e002299.36"
}
],
"reference-count": 36,
"references-count": 36,
"relation": {},
"score": 1,
"short-container-title": [
"BMJ Open Diab Res Care"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": [
"Evaluation and management of COVID-19-related severity in people with type 2 diabetes"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "9"
}
