Hospitalization and mortality in patients with COVID-19 with or at risk of type 2 diabetes: data from five health systems in Pennsylvania and Maryland
et al., BMJ Open Diabetes Research & Care, doi:10.1136/bmjdrc-2022-002774, NCT02788903, Jun 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
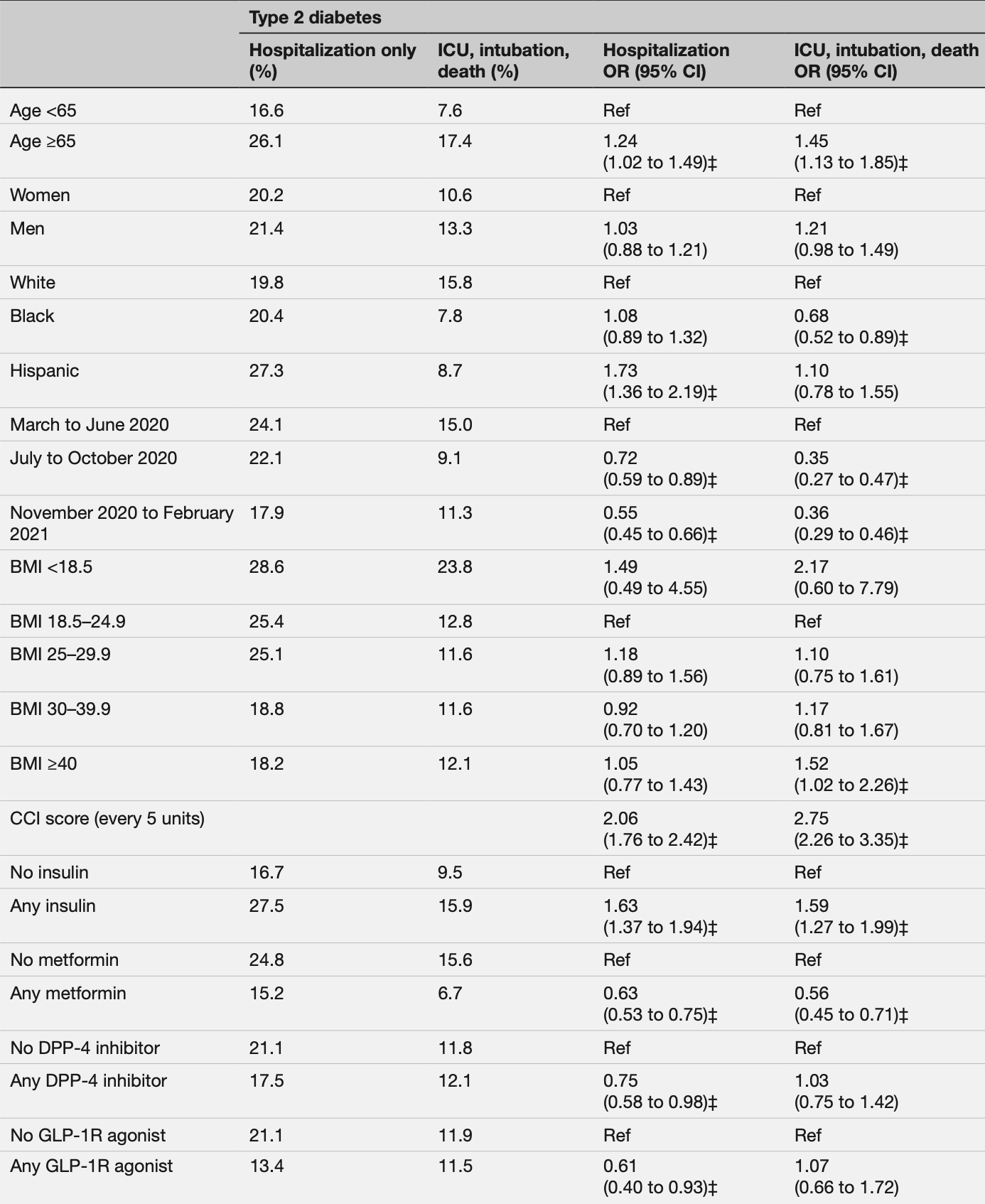
Retrospective 4,944 COVID-19 patients with type 2 diabetes in the USA, showing lower risk of hospitalization and combined ICU/intubation/death with metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
ICU/intubation/death, 44.0% lower, OR 0.56, p < 0.001, RR approximated with OR.
|
|
risk of hospitalization, 37.0% lower, OR 0.63, p < 0.001, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Yeh et al., 9 Jun 2022, retrospective, USA, peer-reviewed, mean age 62.3, 9 authors, study period 1 March, 2020 - 28 February, 2021, trial NCT02788903 (history).
Contact: hyeh1@jhmi.e.
Hospitalization and mortality in patients with COVID-19 with or at risk of type 2 diabetes: data from five health systems in Pennsylvania and Maryland
BMJ Open Diabetes Research & Care, doi:10.1136/bmjdrc-2022-002774
Objective To identify the demographic and clinical characteristics associated with adverse COVID-19 outcomes across a 12-month period in 2020 and 2021.
Research design and methods We conducted a retrospective cohort study using electronic health records from five academic health systems in Pennsylvania and Maryland, including patients with COVID-19 with type 2 diabetes or at risk of type 2 diabetes. Patients were classified based on 30-day outcomes: (1) no hospitalization; (2) hospitalization only; or (3) a composite measure including admission to the intensive care unit (ICU), intubation, or death. Analyses were conducted in patients with type 2 diabetes and patients at risk of type 2 diabetes separately. Results We included 15 725 patients with COVID-19 diagnoses between March 2020 and February 2021. Older age and higher Charlson Comorbidity Index scores were associated with higher odds of adverse outcomes, while COVID-19 diagnoses later in the study period were associated with lower odds of severe outcomes. In patients with type 2 diabetes, individuals on insulin treatment had higher odds for ICU/intubation/death (OR=1.59, 95% CI 1.27 to 1.99), whereas those on metformin had lower odds (OR=0.56, 95% CI 0.45 to 0.71). Compared with non-Hispanic White patients, Hispanic patients had higher odds of hospitalization in patients with type 2 diabetes (OR=1.73, 95% CI 1.36 to 2.19) or at risk of type 2 diabetes (OR=1.77, 95% CI 1.43 to 2.18.) Conclusions Adults who were older, in racial minority groups, had multiple chronic conditions or were on insulin treatment had higher risks for severe COVID-19 outcomes. This study reinforced the urgency of preventing COVID-19 and its complications in vulnerable populations. Trial registration number NCT02788903. ⇒ This study reinforced the urgency of prevent-
Competing interests None declared. Patient consent for publication Not required. Ethics approval This study was reviewed and approved by the Institutional Review Board (IRB) of Johns Hopkins School of Medicine, the central IRB for all participating institutions. Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement No data are available. The data sets generated and/ or analyzed during the current study are not publicly available due to data sharing agreements with electronic health record data. However, opportunities exist for collaborations with the PaTH Network. Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Open access This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others..
References
Ackermann, Verleden, Kuehnel, Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19, N Engl J Med, doi:10.1056/NEJMoa2015432
Bendib, De Chaisemartin, Granger, Neutrophil extracellular traps are elevated in patients with pneumonia-related acute respiratory distress syndrome, Anesthesiology, doi:10.1097/ALN.0000000000002619
Boye, Erdemir, Zimmerman, Risk factors associated with COVID-19 hospitalization and mortality: a large Claims-Based analysis among people with type 2 diabetes mellitus in the United States, Diabetes Ther, doi:10.1007/s13300-021-01110-1
Cameron, Morrison, Levin, Anti-Inflammatory effects of metformin irrespective of diabetes status, Circ Res, doi:10.1161/CIRCRESAHA.116.308445
Cariou, Hadjadj, Wargny, Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study, Diabetologia, doi:10.1007/s00125-020-05180-x
Charlson, Pompei, Ales, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis, doi:10.1016/0021-9681(87)90171-8
Garcia, Sharma, Ramaiah, Antiviral drug screen of kinase inhibitors identifies cellular signaling pathways critical for SARS-CoV-2 replication, bioRxiv
Glasheen, Cordier, Gumpina, Comorbidity Index: ICD-9 Update and ICD-10 Translation, Am Health Drug Benefits
Gregory, Slaughter, Duffus, COVID-19 severity is Tripled in the diabetes community: a prospective analysis of the pandemic's impact in type 1 and type 2 diabetes, Diabetes Care, doi:10.2337/dc20-2260
Griffith, Morris, Tudball, Collider bias undermines our understanding of COVID-19 disease risk and severity, Nat Commun, doi:10.1038/s41467-020-19478-2
Holman, Knighton, Kar, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30271-0
Khunti, Knighton, Zaccardi, Prescription of glucoselowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00050-4
Kindrachuk, Ork, Hart, Antiviral potential of ERK/ MAPK and PI3K/Akt/mTOR signaling modulation for middle East respiratory syndrome coronavirus infection as identified by temporal kinome analysis, Antimicrob Agents Chemother, doi:10.1128/AAC.03659-14
Kraschnewski, Kong, Francis, A patient-centered path to address diabetes: protocol for a study on the impact of obesity counseling, JMIR Res Protoc, doi:10.2196/12054
Mahamat-Saleh, Fiolet, Rebeaud, Diabetes, hypertension, body mass index, smoking and COVID-19-related mortality: a systematic review and meta-analysis of observational studies, BMJ Open, doi:10.1136/bmjopen-2021-052777
Merzon, Green, Shpigelman, Haemoglobin A1c is a predictor of COVID-19 severity in patients with diabetes, Diabetes Metab Res Rev, doi:10.1002/dmrr.3398
Muñoz-Price, Nattinger, Rivera, Racial disparities in incidence and outcomes among patients with COVID-19, JAMA Netw Open, doi:10.1001/jamanetworkopen.2020.21892
Nguyen, Ho, Nguyen, Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: a meta-analysis, Metabolism, doi:10.1016/j.metabol.2022.155196
Nyland, Raja-Khan, Bettermann, Diabetes, drug treatment, and mortality in COVID-19: a multinational retrospective cohort study, Diabetes, doi:10.2337/db21-0385
Pan, Khan, Meeks, Disparities in COVID-19 hospitalizations and mortality among black and Hispanic patients: cross-sectional analysis from the greater Houston metropolitan area, BMC Public Health, doi:10.1186/s12889-021-11431-2
Richardson, Hirsch, Narasimhan, Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area, JAMA, doi:10.1001/jama.2020.6775
Schlesinger, Neuenschwander, Lang, Risk phenotypes of diabetes and association with COVID-19 severity and death: a living systematic review and meta-analysis, Diabetologia, doi:10.1007/s00125-021-05458-8
Shukla, Tchang, Lam, Preadmission predictors of severe COVID-19 in patients with diabetes mellitus, J Diabetes Complications, doi:10.1016/j.jdiacomp.2021.107967
Smith, Boppana, Traupman, Impaired glucose metabolism in patients with diabetes, prediabetes, and obesity is associated with severe COVID-19, J Med Virol, doi:10.1002/jmv.26227
Tartof, Qian, Hong, Obesity and mortality among patients diagnosed with COVID-19: results from an integrated health care organization, Ann Intern Med, doi:10.7326/M20-3742
Vahidy, Drews, Masud, Characteristics and outcomes of COVID-19 patients during initial peak and resurgence in the Houston metropolitan area, JAMA, doi:10.1001/jama.2020.15301
Wander, Lowy, Beste, Prior glucose-lowering medication use and 30-day outcomes among 64,892 veterans with diabetes and COVID-19, Diabetes Care, doi:10.2337/dc21-1351
Wander, Lowy, Beste, Prior glucose-lowering medication use and 30-day outcomes among 64,892 veterans with diabetes and COVID-19, Diabetes Care, doi:10.2337/dc21-1351
Wang, Li, Wang, Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999-2018, JAMA, doi:10.1001/jama.2021.9883
Wang, Shah, Carnethon, Age at diagnosis of diabetes by race and ethnicity in the United States from 2011 to 2018, JAMA Intern Med, doi:10.1001/jamainternmed.2021.4945
Wargny, Potier, Gourdy, Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study, Diabetologia, doi:10.1007/s00125-020-05351-w
Wong, Hall, Vaddavalli, Glycemic control and clinical outcomes in US. patients with COVID-19: data from the National COVID cohort collaborative (N3C) database, Diabetes Care
Xin, Wei, Ji, Metformin uniquely prevents thrombosis by inhibiting platelet activation and mtDNA release, Sci Rep, doi:10.1038/srep36222
Yin, Rohli, Shen, The epidemiology, pathophysiological mechanisms, and management toward COVID-19 patients with type 2 diabetes: a systematic review, Prim Care Diabetes, doi:10.1016/j.pcd.2021.08.014
Zhu, She, Cheng, Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes, Cell Metab, doi:10.1016/j.cmet.2020.04.021
Zuo, Yalavarthi, Shi, Neutrophil extracellular traps in COVID-19, JCI Insight, doi:10.1172/jci.insight.138999
DOI record:
{
"DOI": "10.1136/bmjdrc-2022-002774",
"ISSN": [
"2052-4897"
],
"URL": "http://dx.doi.org/10.1136/bmjdrc-2022-002774",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p>To identify the demographic and clinical characteristics associated with adverse COVID-19 outcomes across a 12-month period in 2020 and 2021.</jats:p></jats:sec><jats:sec><jats:title>Research design and methods</jats:title><jats:p>We conducted a retrospective cohort study using electronic health records from five academic health systems in Pennsylvania and Maryland, including patients with COVID-19 with type 2 diabetes or at risk of type 2 diabetes. Patients were classified based on 30-day outcomes: (1) no hospitalization; (2) hospitalization only; or (3) a composite measure including admission to the intensive care unit (ICU), intubation, or death. Analyses were conducted in patients with type 2 diabetes and patients at risk of type 2 diabetes separately.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>We included 15 725 patients with COVID-19 diagnoses between March 2020 and February 2021. Older age and higher Charlson Comorbidity Index scores were associated with higher odds of adverse outcomes, while COVID-19 diagnoses later in the study period were associated with lower odds of severe outcomes. In patients with type 2 diabetes, individuals on insulin treatment had higher odds for ICU/intubation/death (OR=1.59, 95% CI 1.27 to 1.99), whereas those on metformin had lower odds (OR=0.56, 95% CI 0.45 to 0.71). Compared with non-Hispanic White patients, Hispanic patients had higher odds of hospitalization in patients with type 2 diabetes (OR=1.73, 95% CI 1.36 to 2.19) or at risk of type 2 diabetes (OR=1.77, 95% CI 1.43 to 2.18.)</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>Adults who were older, in racial minority groups, had multiple chronic conditions or were on insulin treatment had higher risks for severe COVID-19 outcomes. This study reinforced the urgency of preventing COVID-19 and its complications in vulnerable populations.</jats:p></jats:sec><jats:sec><jats:title>Trial registration number</jats:title><jats:p><jats:ext-link xmlns:xlink=\"http://www.w3.org/1999/xlink\" ext-link-type=\"clintrialgov\" xlink:href=\"NCT02788903\">NCT02788903</jats:ext-link>.</jats:p></jats:sec>",
"alternative-id": [
"10.1136/bmjdrc-2022-002774"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-5738-0652",
"affiliation": [],
"authenticated-orcid": false,
"family": "Yeh",
"given": "Hsin-Chieh",
"sequence": "first"
},
{
"affiliation": [],
"family": "Kraschnewski",
"given": "Jennifer L",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kong",
"given": "Lan",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lehman",
"given": "Erik B",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Heilbrunn",
"given": "Emily S",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Williams",
"given": "Pamela",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Poger",
"given": "Jennifer M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Francis",
"given": "Erica",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bryce",
"given": "Cindy L",
"sequence": "additional"
}
],
"clinical-trial-number": [
{
"clinical-trial-number": "nct02788903",
"registry": "10.18810/clinical-trials-gov"
}
],
"container-title": "BMJ Open Diabetes Research & Care",
"container-title-short": "BMJ Open Diab Res Care",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2022,
6,
9
]
],
"date-time": "2022-06-09T16:20:38Z",
"timestamp": 1654791638000
},
"deposited": {
"date-parts": [
[
2022,
6,
9
]
],
"date-time": "2022-06-09T16:21:03Z",
"timestamp": 1654791663000
},
"funder": [
{
"DOI": "10.13039/100006093",
"award": [
"NEN-1509-32304"
],
"doi-asserted-by": "crossref",
"name": "PCORI"
}
],
"indexed": {
"date-parts": [
[
2022,
12,
13
]
],
"date-time": "2022-12-13T23:27:32Z",
"timestamp": 1670974052493
},
"is-referenced-by-count": 3,
"issue": "3",
"issued": {
"date-parts": [
[
2022,
6
]
]
},
"journal-issue": {
"issue": "3",
"published-online": {
"date-parts": [
[
2022,
6,
9
]
]
},
"published-print": {
"date-parts": [
[
2022,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 8,
"start": {
"date-parts": [
[
2022,
6,
9
]
],
"date-time": "2022-06-09T00:00:00Z",
"timestamp": 1654732800000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/bmjdrc-2022-002774",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e002774",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2022,
6
]
]
},
"published-online": {
"date-parts": [
[
2022,
6,
9
]
]
},
"published-print": {
"date-parts": [
[
2022,
6
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1016/S2213-8587(20)30238-2",
"article-title": "COVID-19 in people with diabetes: understanding the reasons for worse outcomes",
"author": "Apicella",
"doi-asserted-by": "crossref",
"first-page": "782",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2022060909200758000_10.3.e002774.1",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.diabres.2020.108142",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.2"
},
{
"DOI": "10.1016/j.pcd.2021.08.014",
"article-title": "The epidemiology, pathophysiological mechanisms, and management toward COVID-19 patients with type 2 diabetes: a systematic review",
"author": "Yin",
"doi-asserted-by": "crossref",
"first-page": "899",
"journal-title": "Prim Care Diabetes",
"key": "2022060909200758000_10.3.e002774.3",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1007/s00125-021-05458-8",
"article-title": "Risk phenotypes of diabetes and association with COVID-19 severity and death: a living systematic review and meta-analysis",
"author": "Schlesinger",
"doi-asserted-by": "crossref",
"first-page": "1480",
"journal-title": "Diabetologia",
"key": "2022060909200758000_10.3.e002774.4",
"volume": "64",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.6775",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.5"
},
{
"DOI": "10.7326/M20-3742",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.6"
},
{
"DOI": "10.1016/j.jdiacomp.2021.107967",
"article-title": "Preadmission predictors of severe COVID-19 in patients with diabetes mellitus",
"author": "Shukla",
"doi-asserted-by": "crossref",
"journal-title": "J Diabetes Complications",
"key": "2022060909200758000_10.3.e002774.7",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1007/s00125-020-05180-x",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.8"
},
{
"DOI": "10.1007/s00125-020-05351-w",
"article-title": "Predictors of hospital discharge and mortality in patients with diabetes and COVID-19: updated results from the nationwide CORONADO study",
"author": "Wargny",
"doi-asserted-by": "crossref",
"first-page": "778",
"journal-title": "Diabetologia",
"key": "2022060909200758000_10.3.e002774.9",
"volume": "64",
"year": "2021"
},
{
"DOI": "10.1038/s41467-020-19478-2",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.10"
},
{
"key": "2022060909200758000_10.3.e002774.11",
"unstructured": "Common Data Model. Patient Centered Outcomes Research Institute . The National patient-centered clinical research network. accessed January 7, 2019. Available: http://www.pcornet.org/resource-center/pcornet-common-data-model/"
},
{
"DOI": "10.2196/12054",
"article-title": "A patient-centered path to address diabetes: protocol for a study on the impact of obesity counseling",
"author": "Kraschnewski",
"doi-asserted-by": "crossref",
"journal-title": "JMIR Res Protoc",
"key": "2022060909200758000_10.3.e002774.12",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.13"
},
{
"article-title": "Charlson Comorbidity Index: ICD-9 Update and ICD-10 Translation",
"author": "Glasheen",
"first-page": "188",
"journal-title": "Am Health Drug Benefits",
"key": "2022060909200758000_10.3.e002774.14",
"volume": "12",
"year": "2019"
},
{
"DOI": "10.2337/dc20-2260",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.15"
},
{
"DOI": "10.1002/jmv.26227",
"article-title": "Impaired glucose metabolism in patients with diabetes, prediabetes, and obesity is associated with severe COVID-19",
"author": "Smith",
"doi-asserted-by": "crossref",
"first-page": "409",
"journal-title": "J Med Virol",
"key": "2022060909200758000_10.3.e002774.16",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1001/jama.2020.15301",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.17"
},
{
"DOI": "10.1016/j.cmet.2020.04.021",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.18"
},
{
"DOI": "10.1001/jamainternmed.2021.4945",
"article-title": "Age at diagnosis of diabetes by race and ethnicity in the United States from 2011 to 2018",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "1537",
"journal-title": "JAMA Intern Med",
"key": "2022060909200758000_10.3.e002774.19",
"volume": "181",
"year": "2021"
},
{
"DOI": "10.1001/jama.2021.9883",
"article-title": "Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999-2018",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "704",
"journal-title": "JAMA",
"key": "2022060909200758000_10.3.e002774.20",
"volume": "326",
"year": "2021"
},
{
"DOI": "10.1001/jamanetworkopen.2020.21892",
"article-title": "Racial disparities in incidence and outcomes among patients with COVID-19",
"author": "Muñoz-Price",
"doi-asserted-by": "crossref",
"journal-title": "JAMA Netw Open",
"key": "2022060909200758000_10.3.e002774.21",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1186/s12889-021-11431-2",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.22"
},
{
"DOI": "10.1007/s13300-021-01110-1",
"article-title": "Risk factors associated with COVID-19 hospitalization and mortality: a large Claims-Based analysis among people with type 2 diabetes mellitus in the United States",
"author": "Boye",
"doi-asserted-by": "crossref",
"first-page": "2223",
"journal-title": "Diabetes Ther",
"key": "2022060909200758000_10.3.e002774.23",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"article-title": "Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England",
"author": "Khunti",
"doi-asserted-by": "crossref",
"first-page": "293",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2022060909200758000_10.3.e002774.24",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.2337/dc21-1351",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.25"
},
{
"DOI": "10.1016/j.metabol.2022.155196",
"article-title": "Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: a meta-analysis",
"author": "Nguyen",
"doi-asserted-by": "crossref",
"first-page": "155196",
"journal-title": "Metabolism",
"key": "2022060909200758000_10.3.e002774.26",
"volume": "131",
"year": "2022"
},
{
"DOI": "10.1056/NEJMoa2015432",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.27"
},
{
"DOI": "10.1038/srep36222",
"article-title": "Metformin uniquely prevents thrombosis by inhibiting platelet activation and mtDNA release",
"author": "Xin",
"doi-asserted-by": "crossref",
"journal-title": "Sci Rep",
"key": "2022060909200758000_10.3.e002774.28",
"volume": "6",
"year": "2016"
},
{
"DOI": "10.1161/CIRCRESAHA.116.308445",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.29"
},
{
"DOI": "10.1097/ALN.0000000000002619",
"article-title": "Neutrophil extracellular traps are elevated in patients with pneumonia-related acute respiratory distress syndrome",
"author": "Bendib",
"doi-asserted-by": "crossref",
"first-page": "581",
"journal-title": "Anesthesiology",
"key": "2022060909200758000_10.3.e002774.30",
"volume": "130",
"year": "2019"
},
{
"DOI": "10.1172/jci.insight.138999",
"doi-asserted-by": "crossref",
"key": "2022060909200758000_10.3.e002774.31",
"unstructured": "Zuo Y , Yalavarthi S , Shi H , et al . Neutrophil extracellular traps in COVID-19. JCI Insight 2020;5:e138999.doi:10.1172/jci.insight.138999"
},
{
"DOI": "10.1128/AAC.03659-14",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.32"
},
{
"DOI": "10.1101/2020.06.24.150326",
"doi-asserted-by": "crossref",
"key": "2022060909200758000_10.3.e002774.33",
"unstructured": "Garcia G , Sharma A , Ramaiah A . Antiviral drug screen of kinase inhibitors identifies cellular signaling pathways critical for SARS-CoV-2 replication. bioRxiv 2020."
},
{
"DOI": "10.2337/db21-0385",
"article-title": "Diabetes, drug treatment, and mortality in COVID-19: a multinational retrospective cohort study",
"author": "Nyland",
"doi-asserted-by": "crossref",
"journal-title": "Diabetes",
"key": "2022060909200758000_10.3.e002774.34",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.2337/dc21-1351",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.35"
},
{
"DOI": "10.2337/figshare.19119302",
"doi-asserted-by": "crossref",
"key": "2022060909200758000_10.3.e002774.36",
"unstructured": "Wong R , Hall M , Vaddavalli R . Glycemic control and clinical outcomes in US. patients with COVID-19: data from the National COVID cohort collaborative (N3C) database. Diabetes Care 2022;24:dc212186."
},
{
"DOI": "10.1002/dmrr.3398",
"article-title": "Haemoglobin A1c is a predictor of COVID-19 severity in patients with diabetes",
"author": "Merzon",
"doi-asserted-by": "crossref",
"journal-title": "Diabetes Metab Res Rev",
"key": "2022060909200758000_10.3.e002774.37",
"volume": "37",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"article-title": "Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study",
"author": "Holman",
"doi-asserted-by": "crossref",
"first-page": "823",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2022060909200758000_10.3.e002774.38",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2021-052777",
"doi-asserted-by": "publisher",
"key": "2022060909200758000_10.3.e002774.39"
}
],
"reference-count": 39,
"references-count": 39,
"relation": {},
"resource": {
"primary": {
"URL": "https://drc.bmj.com/lookup/doi/10.1136/bmjdrc-2022-002774"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Hospitalization and mortality in patients with COVID-19 with or at risk of type 2 diabetes: data from five health systems in Pennsylvania and Maryland",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "10"
}
