Prior Glucose-Lowering Medication Use and 30-Day Outcomes Among 64,892 Veterans With Diabetes and COVID-19
et al., Diabetes Care, doi:10.2337/dc21-1351, Oct 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 64,892 veterans with diabetes in the USA, showing lower mortality with existing metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
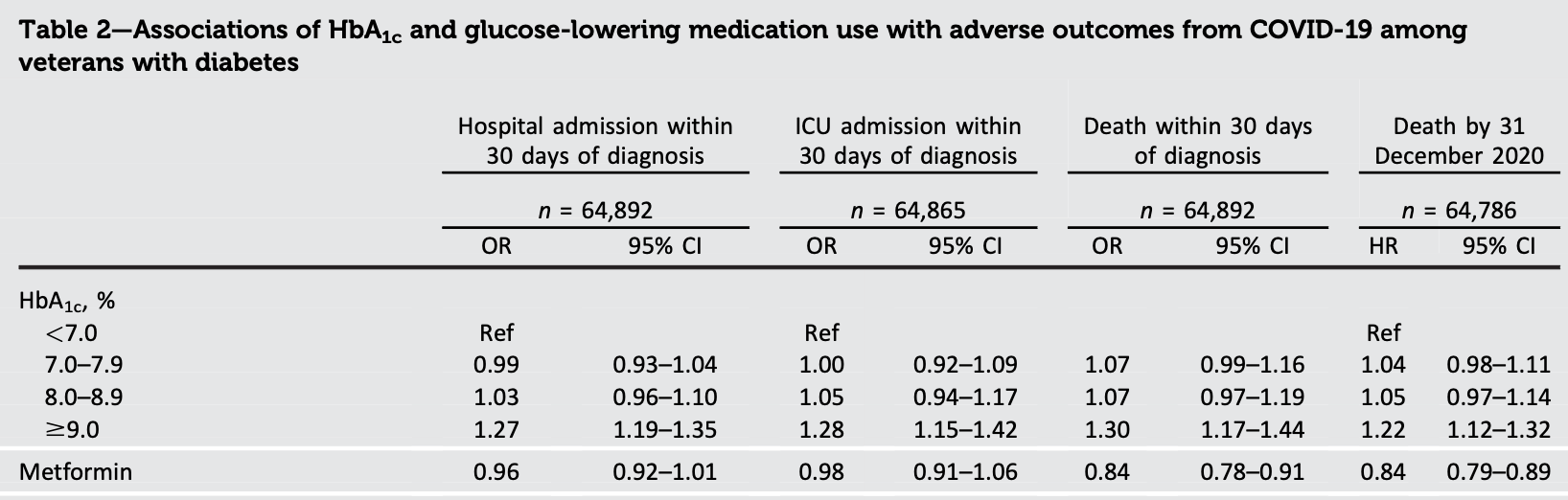
risk of death, 15.0% lower, RR 0.85, p < 0.001, treatment 29,685, control 35,207, odds ratio converted to relative risk, logistic regression, within 30 days of diagnosis, control prevalance approximated with overall prevalence.
|
|
risk of ICU admission, 1.9% lower, RR 0.98, p = 0.62, treatment 29,685, control 35,207, odds ratio converted to relative risk, logistic regression, within 30 days of diagnosis, control prevalance approximated with overall prevalence.
|
|
risk of hospitalization, 3.2% lower, RR 0.97, p = 0.09, treatment 29,685, control 35,207, odds ratio converted to relative risk, logistic regression, within 30 days of diagnosis, control prevalance approximated with overall prevalence.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Wander et al., 6 Oct 2021, retrospective, database analysis, USA, peer-reviewed, 8 authors.
Prior Glucose-Lowering Medication Use and 30-Day Outcomes Among 64,892 Veterans With Diabetes and COVID-19
Diabetes Care, doi:10.2337/dc21-1351
To identify preinfection risk factors for adverse outcomes among veterans with diabetes and coronavirus disease 2019 (COVID-19) infection.
RESEARCH DESIGN AND METHODS We identified all Veterans Health Administration patients with diabetes and one or more positive nasal swab(s) for severe acute respiratory syndrome coronavirus 2 (1 March 2020-10 March 2021) (n = 64,892). We examined associations of HbA 1c and glucose-lowering medication use with hospitalization, intensive care unit (ICU) admission, and mortality at 30 days using logistic regression models and during 4.4 months of follow-up (range <1-13.1) using proportional hazards models.
RESULTS Compared with HbA 1c <7.0%, HbA 1c ‡9.0% was associated with higher odds of hospitalization, ICU admission, and death at 30 days (odds ratio [
Continued on p. 5 Author Contributions. P.L.W. conceived the project, designed the overall research plan, and wrote the first draft of the manuscript. E.L. analyzed the data and reviewed and edited the manuscript. L.A.B. reviewed and edited the manuscript. L.T.-P. reviewed and edited the manuscript. A.K. contributed to design and interpretation of the analyses and reviewed and edited the manuscript. A.C.P. contributed to the design and interpretation of the analyses and reviewed and edited the manuscript. S.E.K. contributed to the design of the analyses and reviewed and edited the manuscript. E.J.B. conceived the project, designed the overall research plan, and reviewed and edited the manuscript. P.L.W. and E.J.B. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
Apicella, Campopiano, Mantuano, Mazoni, Coppelli et al., COVID-19 in people with diabetes: understanding the reasons for worse outcomes, Lancet Diabetes Endocrinol
Bangi, Barve, Qamar, Protective effects of CVD and DM medications in SARS-CoV-2 Infection, SN Compr Clin Med
Dennis, Mcgovern, Vollmer, Mateen, Improving survival of critical care patients with coronavirus disease 2019 in England: a national cohort study, March to June 2020, Crit Care Med
Holman, Knighton, Kar, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a populationbased cohort study, Lancet Diabetes Endocrinol
Kahkoska, Abrahamsen, Alexander, N3C Consortium. Association between glucagon-like peptide 1 receptor agonist and sodium-glucose cotransporter 2 inhibitor use and COVID-19 Outcomes, Diabetes Care
Khunti, Knighton, Zaccardi, Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England, Lancet Diabetes Endocrinol
Wander, Lowy, Beste, Risk factors for adverse outcomes among 35 879 veterans with and without diabetes after diagnosis with COVID-19, BMJ Open Diabetes Res Care
DOI record:
{
"DOI": "10.2337/dc21-1351",
"ISSN": [
"0149-5992",
"1935-5548"
],
"URL": "http://dx.doi.org/10.2337/dc21-1351",
"abstract": "<jats:sec>\n <jats:title>OBJECTIVE</jats:title>\n <jats:p>To identify preinfection risk factors for adverse outcomes among veterans with diabetes and coronavirus disease 2019 (COVID-19) infection.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>RESEARCH DESIGN AND METHODS</jats:title>\n <jats:p>We identified all Veterans Health Administration patients with diabetes and one or more positive nasal swab(s) for severe acute respiratory syndrome coronavirus 2 (1 March 2020–10 March 2021) (n = 64,892). We examined associations of HbA1c and glucose-lowering medication use with hospitalization, intensive care unit (ICU) admission, and mortality at 30 days using logistic regression models and during 4.4 months of follow-up (range &lt;1–13.1) using proportional hazards models.</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>RESULTS</jats:title>\n <jats:p>Compared with HbA1c &lt;7.0%, HbA1c ≥9.0% was associated with higher odds of hospitalization, ICU admission, and death at 30 days (odds ratio [OR] 1.27 [95% CI 1.19–1.35], 1.28 [95% CI 1.15–1.42], 1.30 [95% CI 1.17–1.44], respectively) as well as higher risk of death over 4.4 months (hazard ratio [HR] 1.22 [95% CI 1.12–1.32]). Insulin use was associated with higher odds of hospitalization, ICU admission, and death (OR 1.12 [95% CI 1.07–1.18], 1.12 [95% CI 1.04–1.22], and 1.18 [95% CI 1.09–1.27], respectively) and higher risk of death (HR 1.12 [95% CI 1.07–1.18]). Sodium–glucose cotransporter 2 inhibitor (SGLT2i), glucagon-like peptide-1 receptor agonist (GLP1-RA), or angiotensin receptor blocker use were associated with lower odds of hospitalization (OR 0.92 [95% CI 0.85–0.99], 0.88 [95% CI 0.81–0.96], and 0.94 [95% CI 0.89–0.99], respectively). Metformin and SGLT2i use were associated with lower odds (OR 0.84 [95% CI 0.78–0.91], 0.82 [95% CI 0.72–0.94], respectively) and risk of death (HR 0.84 [95% CI 0.79–0.89], 0.82 [95% CI 0.74–0.92], respectively).</jats:p>\n </jats:sec>\n <jats:sec>\n <jats:title>CONCLUSIONS</jats:title>\n <jats:p>Among veterans with diabetes and COVID-19, higher HbA1c and insulin use were directly associated with adverse outcomes, while use of a GLP1-RA, metformin, and SGLT2i was inversely associated.</jats:p>\n </jats:sec>",
"author": [
{
"ORCID": "http://orcid.org/0000-0003-3671-1464",
"affiliation": [
{
"name": "Veterans Affairs Puget Sound Health Care System, Seattle, WA"
},
{
"name": "Department of Medicine, University of Washington, Seattle, WA"
}
],
"authenticated-orcid": false,
"family": "Wander",
"given": "Pandora L.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Veterans Affairs Puget Sound Health Care System, Seattle, WA"
},
{
"name": "Department of Health Systems and Population Health, University of Washington, Seattle, WA"
}
],
"family": "Lowy",
"given": "Elliott",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Veterans Affairs Puget Sound Health Care System, Seattle, WA"
},
{
"name": "Department of Medicine, University of Washington, Seattle, WA"
}
],
"family": "Beste",
"given": "Lauren A.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Veterans Affairs Puget Sound Health Care System, Seattle, WA"
},
{
"name": "Department of Medicine, University of Washington, Seattle, WA"
}
],
"family": "Tulloch-Palomino",
"given": "Luis",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Veterans Affairs Puget Sound Health Care System, Seattle, WA"
}
],
"family": "Korpak",
"given": "Anna",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Veterans Affairs Puget Sound Health Care System, Seattle, WA"
}
],
"family": "Peterson",
"given": "Alexander C.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Veterans Affairs Puget Sound Health Care System, Seattle, WA"
},
{
"name": "Department of Medicine, University of Washington, Seattle, WA"
}
],
"family": "Kahn",
"given": "Steven E.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Veterans Affairs Puget Sound Health Care System, Seattle, WA"
},
{
"name": "Department of Medicine, University of Washington, Seattle, WA"
}
],
"family": "Boyko",
"given": "Edward J.",
"sequence": "additional"
}
],
"container-title": "Diabetes Care",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"diabetesjournals.org"
]
},
"created": {
"date-parts": [
[
2021,
10,
6
]
],
"date-time": "2021-10-06T18:25:52Z",
"timestamp": 1633544752000
},
"deposited": {
"date-parts": [
[
2022,
3,
13
]
],
"date-time": "2022-03-13T10:43:20Z",
"timestamp": 1647168200000
},
"indexed": {
"date-parts": [
[
2024,
3,
27
]
],
"date-time": "2024-03-27T07:48:11Z",
"timestamp": 1711525691583
},
"is-referenced-by-count": 19,
"issue": "12",
"issued": {
"date-parts": [
[
2021,
10,
6
]
]
},
"journal-issue": {
"issue": "12",
"published-online": {
"date-parts": [
[
2021,
10,
6
]
]
},
"published-print": {
"date-parts": [
[
2021,
12,
1
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://www.diabetesjournals.org/content/license",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
10,
6
]
],
"date-time": "2021-10-06T00:00:00Z",
"timestamp": 1633478400000
}
}
],
"link": [
{
"URL": "https://diabetesjournals.org/care/article-pdf/44/12/2708/631623/dc211351.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "syndication"
},
{
"URL": "https://diabetesjournals.org/care/article-pdf/44/12/2708/631623/dc211351.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1167",
"original-title": [],
"page": "2708-2713",
"prefix": "10.2337",
"published": {
"date-parts": [
[
2021,
10,
6
]
]
},
"published-online": {
"date-parts": [
[
2021,
10,
6
]
]
},
"published-print": {
"date-parts": [
[
2021,
12,
1
]
]
},
"publisher": "American Diabetes Association",
"reference": [
{
"DOI": "10.1016/S2213-8587(20)30238-2",
"article-title": "COVID-19 in people with diabetes: understanding the reasons for worse outcomes",
"author": "Apicella",
"doi-asserted-by": "crossref",
"first-page": "782",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2022031309331775900_B1",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1136/bmjdrc-2021-002252",
"article-title": "Risk factors for adverse outcomes among 35 879 veterans with and without diabetes after diagnosis with COVID-19",
"author": "Wander",
"doi-asserted-by": "crossref",
"first-page": "e002252",
"journal-title": "BMJ Open Diabetes Res Care",
"key": "2022031309331775900_B2",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1097/CCM.0000000000004747",
"article-title": "Improving survival of critical care patients with coronavirus disease 2019 in England: a national cohort study, March to June 2020",
"author": "Dennis",
"doi-asserted-by": "crossref",
"first-page": "209",
"journal-title": "Crit Care Med",
"key": "2022031309331775900_B3",
"volume": "49",
"year": "2021"
},
{
"key": "2022031309331775900_B4",
"unstructured": "U.S. Department of Veterans Affairs\n . Veterans Health Administration. 2020 Accessed 28 September 2020. Available from https://www.va.gov/health/"
},
{
"key": "2022031309331775900_B5",
"unstructured": "Corporate Data Warehouse (CDW)\n . VA COVID-19 Shared Data Resource. Accessed 2 October 2021. https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/3810-notes.pdf"
},
{
"DOI": "10.2337/dc20-S002",
"article-title": "2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2020",
"author": "American Diabetes Association",
"doi-asserted-by": "crossref",
"first-page": "S14",
"journal-title": "Diabetes Care",
"key": "2022031309331775900_B6",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"article-title": "Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study",
"author": "Holman",
"doi-asserted-by": "crossref",
"first-page": "823",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2022031309331775900_B7",
"volume": "8",
"year": "2020"
},
{
"article-title": "Protective effects of CVD and DM medications in SARS-CoV-2 Infection",
"author": "Bangi",
"first-page": "1",
"journal-title": "SN Compr Clin Med",
"key": "2022031309331775900_B8",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"article-title": "Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: a nationwide observational study in England",
"author": "Khunti",
"doi-asserted-by": "crossref",
"first-page": "293",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "2022031309331775900_B9",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.2337/dc21-0065",
"article-title": "Association between glucagon-like peptide 1 receptor agonist and sodium-glucose cotransporter 2 inhibitor use and COVID-19 Outcomes",
"author": "Kahkoska",
"doi-asserted-by": "crossref",
"first-page": "1564",
"journal-title": "Diabetes Care",
"key": "2022031309331775900_B10",
"volume": "44",
"year": "2021"
}
],
"reference-count": 10,
"references-count": 10,
"relation": {
"has-preprint": [
{
"asserted-by": "object",
"id": "10.2337/figshare.16629652",
"id-type": "doi"
},
{
"asserted-by": "object",
"id": "10.2337/figshare.16629652.v1",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://diabetesjournals.org/care/article/44/12/2708/138488/Prior-Glucose-Lowering-Medication-Use-and-30-Day"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Advanced and Specialized Nursing",
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine"
],
"subtitle": [],
"title": "Prior Glucose-Lowering Medication Use and 30-Day Outcomes Among 64,892 Veterans With Diabetes and COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.2337/ada-journal-policies",
"volume": "44"
}
