Risk factors for COVID-19 case fatality rate in people with type 1 and type 2 diabetes mellitus: A nationwide retrospective cohort study of 235,248 patients in the Russian Federation
et al., Frontiers in Endocrinology, doi:10.3389/fendo.2022.909874, Aug 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 224,190 type 2 diabetes patients in Russia, showing lower mortality with metformin use.
|
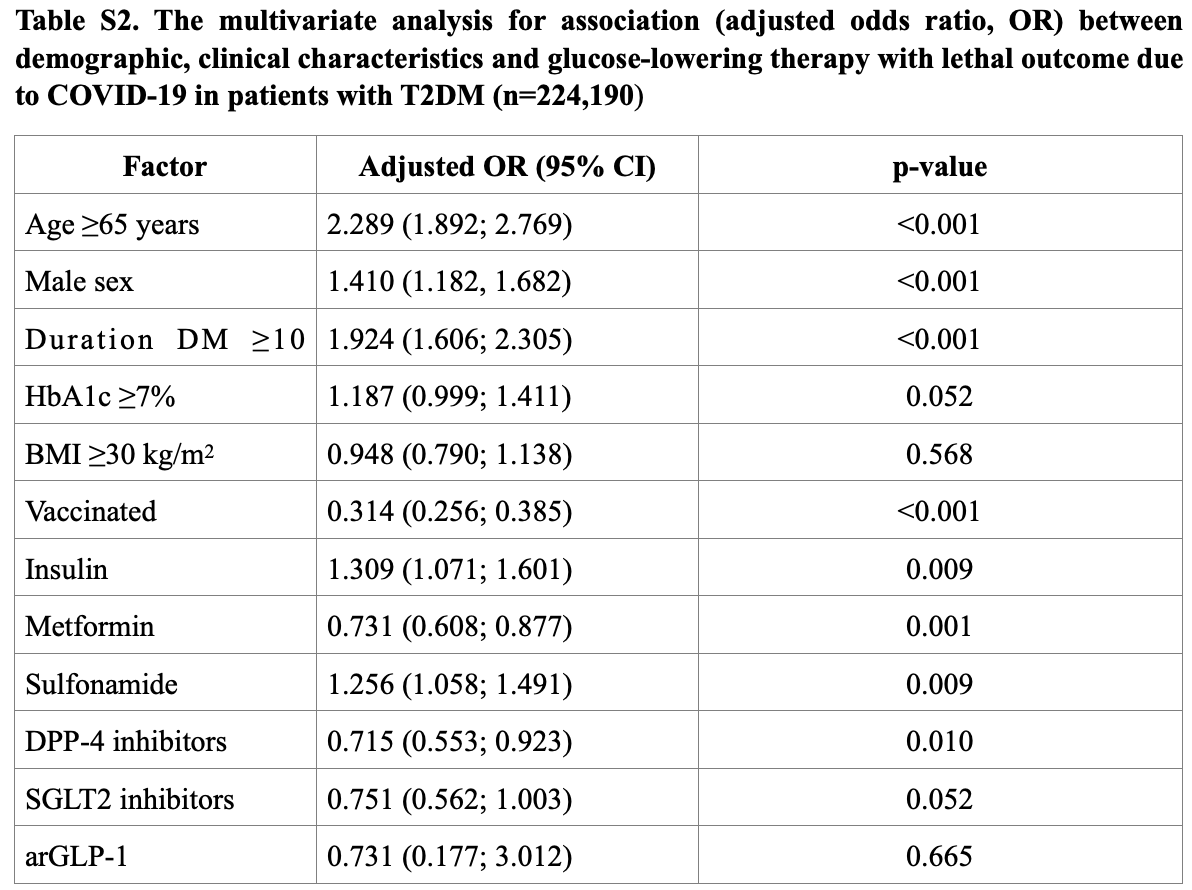
risk of death, 21.6% lower, RR 0.78, p = 0.001, treatment 21,471 of 139,637 (15.4%), control 12,721 of 50,361 (25.3%), adjusted per study, odds ratio converted to relative risk, Table S2, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Shestakova et al., 9 Aug 2022, retrospective, Russia, peer-reviewed, 6 authors, study period 20 March, 2020 - 25 November, 2021.
Contact: olga-vikulova-1973@yandex.ru.
Risk factors for COVID-19 case fatality rate in people with type 1 and type 2 diabetes mellitus: A nationwide retrospective cohort study of 235,248 patients in the Russian Federation
Frontiers in Endocrinology, doi:10.3389/fendo.2022.909874
The aim: To study the association of demographic, clinical, and laboratory factors and the use of glucose-lowering drugs and anti-coronavirus disease (COVID-19) vaccination with the COVID-19-related case fatality rate (CFR) in diabetes mellitus (DM) patients. Methods: This study is a nationwide observational cohort study based on the data from the National Diabetes Register (NDR) that is the database containing online clinical information about the population with DM. The outcomes (death or recovery) for COVID-19 were registered in 235,248 patients with DM [type 1 diabetes mellitus (T1DM), n = 11,058; type 2 diabetes mellitus (T2DM), n = 224,190] from March 20, 2020, until November 25, 2021. The unadjusted odds ratio (OR) and 95% confidence interval (CI) were used to estimate the risk factors for CFR. Then the ranging of significant factors was performed and the most vulnerable groups of factors for the lethal outcome were chosen.
Results: The CFR due to COVID-19 was 8.1% in T1DM and 15.3% in T2DM. Increased CFR was associated with the male population [OR = 1.25 (95% CI: 1.09-1.44) in T1DM and 1.18 (95% CI: 1.15-1.21) in T2DM], age ≥65 years [OR = 4.44 (95% CI: 3.75-5.24) in T1DM and 3.18 (95% CI: 3.09-3.26) in T2DM], DM duration ≥10 years [OR = 2.46 (95% CI: 2.06-2.95) in T1DM and 2.11 (95% CI: 2.06-2.16) in T2DM], body mass index (BMI) ≥30 kg/m 2 [OR = 1.95 (95% CI: 1.52-2.50)] in T1DM, HbA1c ≥7% [OR = 1.35 (95% CI: 1.29-1.43)] in T2DM. The atherosclerotic cardiovascular disease (ASCVD) and chronic kidney disease (CKD) were associated with higher CFR in T1DM but not in T2DM. The pre-COVID-19 glucose-lowering therapy in T2DM was differently associated with CFR (OR): 0.61 (95% CI: 0.59-0.62) for metformin, 0.59 (95% CI: 0.57-0.61) for dipeptidyl peptidase-4 inhibitors (DPP-4 inhibitors), 0.46 (95% CI: 0.44-0.49) for sodium-glucose co-transporter-2 (SGLT2) inhibitors, 0.38 (95% CI: 0.29-0.51) for glucagon-like peptide-1 receptor agonists (arGLP-1), 1.34 (95% CI: 1.31-1.37) for sulfonylurea (SU), and 1.47 (95% CI: 1.43-1.51) for insulin. Anti-Frontiers in Endocrinology frontiersin.org 01
Ethics statement The studies involving human participants (human data of register medical reports) were reviewed and approved by local ethics committee of Endocrinology Research Centre, Moscow, Russia. The patients/participants provided their written informed consent for use of medical data register records for the study.
Author contributions MS, OV, ID and NM conceived and designed the study. AE, AD, and OV analyzed the data. OV, AD, AE, MS wrote the paper. ID and NM have done final revision of article. All authors, reviewed, edited, and approved the manuscript.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/ fendo.2022.909874/full#supplementary-material
References
Ando, Horii, Uematsu, Hanaki, Atsuda et al., Impact of overlapping risks of type 2 diabetes and obesity on coronavirus disease severity in the united states, Sci Rep, doi:10.1038/s41598-021-96720-x
Barron, Bakhai, Kar, Weaver, Bradley et al., Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: A whole-population study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30272-2
Bermingham, Morgan, Nafilyan, Deaths involving COVID-19 by vaccination status
Bornstein, Rubino, Khunti, Mingrone, Hopkins et al., Practical recommendations for the management of diabetes in patients with COVID-19, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30152-2
Breland, Wong, Steers, Yuan, Haderlein et al., The effect of metformin consumption on mortality in hospitalized COVID-19 patients: A systematic review and meta-analysis, Diabetes Metab Syndr Clin Res Rev, doi:10.1016/j.dsx.2020.11.006
Chen, Yang, Cheng, Chen, Peng et al., Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care, doi:10.2337/dc20-0660
Corona, Pizzocaro, Vena, Rastrelli, Semeraro et al., Diabetes is most important cause for mortality in COVID-19 hospitalized patients: Systematic review and meta-analysis, Rev Endocr Metab Disord, doi:10.1007/s11154-021-09630-8
Daniels, Ren, Kumar, Bui, Zhang et al., Relation of prior statin and anti-hypertensive use to severity of disease among patients hospitalized with COVID-19: Findings from the American heart association's COVID-19 cardiovascular disease registry, PloS One, doi:10.1371/journal.pone.0254635
Dedov, Shestakova, Vikulova, Zheleznyakova, Isakov, Epidemiological characteristics of diabetes mellitus in the Russian federation: Clinical and statistical analysis according to the federal diabetes register data of 01.01, Diabetes Mellit, doi:10.14341/DM12759
Dispinseri, Lampasona, Secchi, Bazzigaluppi, Negri, Robust neutralizing antibodies to SARS-CoV-2 develop and persist in subjects with diabetes and COVID-19 pneumonia, J Clin Endocrinol Metab, doi:10.1210/clinem/dgab055
Douros, Dell'aniello, Yu, Filion, Azoulay et al., Sulfonylureas as second line drugs in type 2 diabetes and the risk of cardiovascular and hypoglycaemic events: Population based cohort study, BMJ, doi:10.1136/bmj.k2693
Gregg, Sophiea, Weldegiorgis, Diabetes and COVID-19: Population impact 18 months into the pandemic, Diabetes Care, doi:10.2337/dci21-0001
Han, Ma, Sun, Zhang, Qu et al., The association between anti-diabetic agents and clinical outcomes of COVID-19 in patients with diabetes: A systematic review and meta-analysis, Arch Med Res, doi:10.1101/2021.01.26.21250506
Hariyanto, Intan, Hananto, Putri, Kurniawan, Pre-admission glucagon-like peptide-1 receptor agonist (GLP-1RA) and mortality from coronavirus disease 2019 (Covid-19): A systematic review, meta-analysis, and meta-regression, Diabetes Res Clin Pract, doi:10.1016/j.diabres.2021.109031
Holden, Currie, Schramm, Tk, Gislason et al., Mortality and cardiovascular risk associated with different insulin secretagogues compared with metformin in type 2 diabetes, with or without a previous myocardial infarction: a nationwide study, Diabetes Obes Metab, doi:10.1093/eurheartj/ehr077
Holman, Knighton, Kar, 'keefe, Curley et al., Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30271-0
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Hussain, Mahawar, Xia, Yang, El-Hasani, Retraction notice to obesity a nd mortality of COVID-19. Meta-analysis, Obesity Res Clin Pract, doi:10.1016/j.orcp.2020.12.008
Iheanacho, Odili, Eze, Risk of SARS-CoV-2 infection and COVID-19 prognosis with the use of renin-angiotensin-aldosterone system (RAAS) inhibitors: A systematic review, Futur J Pharm Sci, doi:10.1186/s43094-021-00224-4
Kan, Zhang, Han, Xu, Ye et al., Mortality risk of antidiabetic agents for type 2 diabetes with COVID-19: A systematic review and meta-analysis, Front Endocrinol, doi:10.3389/fendo.2021.708494/full
Kazakou, Lambadiari, Ikonomidis, Kountouri, Panagopoulos et al., Diabetes and COVID-19; A bidirectional interplay, Front Endocrinol, doi:10.3389/fendo.2022.780663/full
Khunti, Knighton, Zaccardi, Bakhai, Barron et al., Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: A nationwide observational study in England, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00244-8
Kosiborod, Esterline, Furtado, Oscarsson, Gasparyan et al., Dapagliflozin in patients with cardiometabolic risk factors hospitalised with COVID-19 (DARE-19): A randomised, double-blind, placebocontrolled, phase 3 trial, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(21)00180-7
Kung, Doppen, Black, Braithwaite, Kearns et al., Underestimation of COVID-19 mortality during the pandemic, ERJ Open Res, doi:10.1183/23120541.00766-2020
Li, Yang, Yan, Sun, Zeng et al., Metformin in patients with COVID-19: A systematic review and meta-analysis, Front Med, doi:10.3389/fmed.2021.704666
Logunov, Dolzhikova, Shcheblyakov, Tukhvatulin, Zubkova et al., Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: An interim analysis of a randomised controlled phase 3 trial in Russia, Lancet, doi:10.1016/S0140-6736(21)00234-8
Mcallister, Risks of and risk factors for COVID-19 disease in people with diabetes: A cohort study of the total population of Scotland, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30405-8
Mcgurnaghan, Weir, Bishop, Kennedy, Blackbourn, None
Meijer, Hoekstra, Van Den Oever, Simsek, Van Den Bergh et al., Treatment with a DPP-4 inhibitor at time of hospital admission for COVID-19 is not associated with improved clinical outcomes: Data from the COVID-PREDICT cohort study in the Netherlands, J Diabetes Metab Disord, doi:10.1007/s40200-021-00833-z
Nauck, Quast, Wefers, Meier, GLP-1 receptor agonists in the treatment of type 2 diabetes -state-of-the-art, Mol Metab, doi:10.1016/j.molmet.2020.101102
Patel, Strong, Fontes, Carvalho, Santos-Ferreira et al., Protective effects of SGLT-2 inhibitors across the cardiorenal continuum: two faces of the same coin, Diabetes Ther Res Treat Educ Diabetes Relat Disord, doi:10.1093/eurjpc/zwab034
Prattichizzo, De Candia, Nicolucci, Ceriello, Elevated HbA1c levels in pre-Covid-19 infection increases the risk of mortality: A sistematic review and meta-analysis, Diabetes Metab Res Rev, doi:10.1002/DMRR.3476/v2/response1
Rakhmat, Kusmala, Handayani, Juliastuti, Nawangsih et al., Dipeptidyl peptidase-4 (DPP-4) inhibitor and mortality in coronavirus disease 2019 (COVID-19) -a systematic review, meta-analysis, and meta-regression, Diabetes Metab Syndr, doi:10.1016/j.dsx.2021.03.027
Rawshani, Kjölhede, Rawshani, Sattar, Eeg-Olofsson et al., Severe COVID-19 in people with type 1 and type 2 diabetes in Sweden: A nationwide retrospective cohort study, Lancet Reg Heal -Eur, doi:10.1016/j.lanepe.2021.100105
Santoro, Nuñez-Gil, Vitale, Viana-Llamas, Martinez et al., Antiplatelet therapy and outcome in COVID-19: The health outcome predictive evaluation registry, Heart, doi:10.1136/heartjnl-2021-319552
Sharma, Ray, Sadasivam, Krejner, Bienias et al., DPP4 inhibitors and COVID-19-Holy grail or another dead end?, Arch Immunol Ther Exp (Warsz), doi:10.1007/s00005-020-00602-5
Shestakova, Vikulova, Isakov, Dedov, Diabetes and COVID-19: Analysis of the clinical outcomes according to the data of the Russian diabetes registry, Probl Endokrinol (Mosk), doi:10.14341/probl12458
Williamson, Walker, Bhaskaran, Bacon, Bates et al., Factors associated with COVID-19-related death using OpenSAFELY, Nature, doi:10.1038/s41586-020-2521-4
Yang, Cai, Zhang, DPP-4 inhibitors may improve the mortality of coronavirus disease 2019: A meta-analysis, PloS One, doi:10.1371/journal.pone.0251916
Yang, Cai, Zhang, Insulin treatment may increase adverse outcomes in patients with COVID-19 and diabetes: A systematic review and meta-analysis, Front Endocrinol, doi:10.3389/fendo.2021.696087/full
Zhang, Lewis, Moley, Brestoff, A systematic review and metaanalysis of obesity and COVID-19 outcomes, Sci Rep, doi:10.1038/s41598-021-86694-1
DOI record:
{
"DOI": "10.3389/fendo.2022.909874",
"ISSN": [
"1664-2392"
],
"URL": "http://dx.doi.org/10.3389/fendo.2022.909874",
"abstract": "<jats:sec><jats:title>The aim</jats:title><jats:p>To study the association of demographic, clinical, and laboratory factors and the use of glucose-lowering drugs and anti-coronavirus disease (COVID-19) vaccination with the COVID-19-related case fatality rate (CFR) in diabetes mellitus (DM) patients.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>This study is a nationwide observational cohort study based on the data from the National Diabetes Register (NDR) that is the database containing online clinical information about the population with DM. The outcomes (death or recovery) for COVID-19 were registered in 235,248 patients with DM [type 1 diabetes mellitus (T1DM), n = 11,058; type 2 diabetes mellitus (T2DM), n = 224,190] from March 20, 2020, until November 25, 2021. The unadjusted odds ratio (OR) and 95% confidence interval (CI) were used to estimate the risk factors for CFR. Then the ranging of significant factors was performed and the most vulnerable groups of factors for the lethal outcome were chosen.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>The CFR due to COVID-19 was 8.1% in T1DM and 15.3% in T2DM. Increased CFR was associated with the male population [OR = 1.25 (95% CI: 1.09–1.44) in T1DM and 1.18 (95% CI: 1.15–1.21) in T2DM], age ≥65 years [OR = 4.44 (95% CI: 3.75–5.24) in T1DM and 3.18 (95% CI: 3.09–3.26) in T2DM], DM duration ≥10 years [OR = 2.46 (95% CI: 2.06–2.95) in T1DM and 2.11 (95% CI: 2.06–2.16) in T2DM], body mass index (BMI) ≥30 kg/m<jats:sup>2</jats:sup> [OR = 1.95 (95% CI: 1.52–2.50)] in T1DM, HbA1c ≥7% [OR = 1.35 (95% CI: 1.29–1.43)] in T2DM. The atherosclerotic cardiovascular disease (ASCVD) and chronic kidney disease (CKD) were associated with higher CFR in T1DM but not in T2DM. The pre-COVID-19 glucose-lowering therapy in T2DM was differently associated with CFR (OR): 0.61 (95% CI: 0.59–0.62) for metformin, 0.59 (95% CI: 0.57–0.61) for dipeptidyl peptidase-4 inhibitors (DPP-4 inhibitors), 0.46 (95% CI: 0.44–0.49) for sodium-glucose co-transporter-2 (SGLT2) inhibitors, 0.38 (95% CI: 0.29–0.51) for glucagon-like peptide-1 receptor agonists (arGLP-1), 1.34 (95% CI: 1.31–1.37) for sulfonylurea (SU), and 1.47 (95% CI: 1.43–1.51) for insulin. Anti-COVID-19 vaccination was associated with a lower fatality risk in both DM types: OR = 0.07 (95% CI: 0.03–0.20) in T1DM and OR = 0.19 (95% CI: 0.17–0.22) in T2DM.</jats:p></jats:sec><jats:sec><jats:title>Conclusions</jats:title><jats:p>The results of our study suggest that increased COVID-19-related fatality risk in both T1DM and T2DM patients associated with the male population, older age, longer DM duration, and absence of anti-COVID-19 vaccination. In T2DM, pre-COVID-19 glucose-lowering therapy with metformin, DPP-4 inhibitors, SGLT2 inhibitors, and arGLP-1 had a positive effect on the risk of death. The most vulnerable combination of risk factors for lethal outcome in both DM types was vaccine absence + age ≥65 years + DM duration ≥10 years.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fendo.2022.909874"
],
"author": [
{
"affiliation": [],
"family": "Shestakova",
"given": "M. V.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Vikulova",
"given": "O. K.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Elfimova",
"given": "A. R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Deviatkin",
"given": "A. A.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Dedov",
"given": "I. I.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mokrysheva",
"given": "N. G.",
"sequence": "additional"
}
],
"container-title": "Frontiers in Endocrinology",
"container-title-short": "Front. Endocrinol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2022,
8,
9
]
],
"date-time": "2022-08-09T08:05:24Z",
"timestamp": 1660032324000
},
"deposited": {
"date-parts": [
[
2022,
8,
9
]
],
"date-time": "2022-08-09T08:05:31Z",
"timestamp": 1660032331000
},
"funder": [
{
"DOI": "10.13039/501100012190",
"doi-asserted-by": "publisher",
"name": "Ministry of Science and Higher Education of the Russian Federation"
}
],
"indexed": {
"date-parts": [
[
2022,
8,
9
]
],
"date-time": "2022-08-09T08:42:40Z",
"timestamp": 1660034560412
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
8,
9
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
9
]
],
"date-time": "2022-08-09T00:00:00Z",
"timestamp": 1660003200000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fendo.2022.909874/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2022,
8,
9
]
]
},
"published-online": {
"date-parts": [
[
2022,
8,
9
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"article-title": "Clinical features of patients infected with 2019 novel coronavirus in wuhan, China",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"journal-title": "Lancet",
"key": "B1",
"volume": "395",
"year": "2020"
},
{
"first-page": "1",
"key": "B2",
"volume-title": "Weekly operational update on COVID-19",
"year": "2021"
},
{
"key": "B3",
"unstructured": "Russian Nationwide statistical data about covid-19"
},
{
"DOI": "10.1183/23120541.00766-2020",
"article-title": "Underestimation of COVID-19 mortality during the pandemic",
"author": "Kung",
"doi-asserted-by": "publisher",
"journal-title": "ERJ Open Res",
"key": "B4",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(20)30152-2",
"article-title": "Practical recommendations for the management of diabetes in patients with COVID-19",
"author": "Bornstein",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "B5",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"article-title": "Factors associated with COVID-19-related death using OpenSAFELY",
"author": "Williamson",
"doi-asserted-by": "publisher",
"journal-title": "Nature",
"key": "B6",
"volume": "584",
"year": "2020"
},
{
"DOI": "10.1016/j.lanepe.2021.100105",
"article-title": "Severe COVID-19 in people with type 1 and type 2 diabetes in Sweden: A nationwide retrospective cohort study",
"author": "Rawshani",
"doi-asserted-by": "publisher",
"first-page": "100105",
"journal-title": "Lancet Reg Heal - Eur",
"key": "B7",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(20)30272-2",
"article-title": "Associations of type 1 and type 2 diabetes with COVID-19-related mortality in England: A whole-population study",
"author": "Barron",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "B8",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"article-title": "Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study",
"author": "Holman",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "B9",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-96720-x",
"article-title": "Impact of overlapping risks of type 2 diabetes and obesity on coronavirus disease severity in the united states",
"author": "Ando",
"doi-asserted-by": "publisher",
"first-page": "17968",
"journal-title": "Sci Rep",
"key": "B10",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2022.780663/full",
"article-title": "Diabetes and COVID-19; A bidirectional interplay",
"author": "Kazakou",
"doi-asserted-by": "publisher",
"journal-title": "Front Endocrinol (Lausanne)",
"key": "B11",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/S2213-8587(21)00050-4",
"article-title": "Prescription of glucose-lowering therapies and risk of COVID-19 mortality in people with type 2 diabetes: A nationwide observational study in England",
"author": "Khunti",
"doi-asserted-by": "publisher",
"first-page": "293",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "B12",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1152/ajpendo.00244.2021",
"article-title": "CHM, guimarães JCW, sampaio NS, Silva l de ML, de mascarenhas LP, et al. diabetic ketoacidosis and COVID-19: What have we learned so far",
"author": "de Sá-Ferreira",
"doi-asserted-by": "publisher",
"journal-title": "Am J Physiol Metab",
"key": "B13",
"volume": "322",
"year": "2022"
},
{
"DOI": "10.1016/S2213-8587(21)00244-8",
"article-title": "COVID-19 and metabolic disease: Mechanisms and clinical management",
"author": "Steenblock",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "B14",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.14341/probl12458",
"article-title": "Diabetes and COVID-19: Analysis of the clinical outcomes according to the data of the Russian diabetes registry",
"author": "Shestakova",
"doi-asserted-by": "publisher",
"first-page": "35",
"journal-title": "Probl Endokrinol (Mosk)",
"key": "B15",
"volume": "66",
"year": "2020"
},
{
"DOI": "10.2337/dci21-0001",
"article-title": "Diabetes and COVID-19: Population impact 18 months into the pandemic",
"author": "Gregg",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Care",
"key": "B16",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1007/s11154-021-09630-8",
"article-title": "Diabetes is most important cause for mortality in COVID-19 hospitalized patients: Systematic review and meta-analysis",
"author": "Corona",
"doi-asserted-by": "publisher",
"journal-title": "Rev Endocr Metab Disord",
"key": "B17",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(20)30405-8",
"article-title": "Risks of and risk factors for COVID-19 disease in people with diabetes: A cohort study of the total population of Scotland",
"author": "McGurnaghan",
"doi-asserted-by": "publisher",
"first-page": "82",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "B18",
"volume": "9",
"year": "2021"
},
{
"key": "B19",
"unstructured": "Oficial information about COVID-19 in Russia"
},
{
"DOI": "10.1371/journal.pone.0254635",
"article-title": "Relation of prior statin and anti-hypertensive use to severity of disease among patients hospitalized with COVID-19: Findings from the American heart association’s COVID-19 cardiovascular disease registry",
"author": "Daniels",
"doi-asserted-by": "publisher",
"first-page": "e0254635",
"journal-title": "PloS One",
"key": "B20",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1186/s43094-021-00224-4",
"article-title": "Risk of SARS-CoV-2 infection and COVID-19 prognosis with the use of renin-angiotensin-aldosterone system (RAAS) inhibitors: A systematic review",
"author": "Iheanacho",
"doi-asserted-by": "publisher",
"first-page": "73",
"journal-title": "Futur J Pharm Sci",
"key": "B21",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1136/heartjnl-2021-319552",
"article-title": "Antiplatelet therapy and outcome in COVID-19: The health outcome predictive evaluation registry",
"author": "Santoro",
"doi-asserted-by": "publisher",
"journal-title": "Heart",
"key": "B22",
"volume": "108",
"year": "2021"
},
{
"DOI": "10.1002/DMRR.3476/v2/response1",
"article-title": "Elevated HbA1c levels in pre-Covid-19 infection increases the risk of mortality: A sistematic review and meta-analysis",
"author": "Prattichizzo",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab Res Rev",
"key": "B23",
"volume": "38",
"year": "2021"
},
{
"DOI": "10.1016/j.orcp.2020.12.008",
"article-title": "Retraction notice to obesity a nd mortality of COVID-19",
"author": "Hussain",
"doi-asserted-by": "publisher",
"first-page": "100",
"journal-title": "Meta-analysis Obesity Res Clin Pract",
"key": "B24",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1038/s41598-021-86694-1",
"article-title": "A systematic review and meta-analysis of obesity and COVID-19 outcomes",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "7193",
"journal-title": "Sci Rep",
"key": "B25",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1002/oby.23121",
"article-title": "BMI and risk for severe COVID-19 among veterans health administration patients",
"author": "Breland",
"doi-asserted-by": "publisher",
"journal-title": "Obesity",
"key": "B26",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2020.11.006",
"article-title": "The effect of metformin consumption on mortality in hospitalized COVID-19 patients: A systematic review and meta-analysis",
"author": "Lukito",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab Syndr Clin Res Rev",
"key": "B27",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2021.704666",
"article-title": "Metformin in patients with COVID-19: A systematic review and meta-analysis",
"author": "Li",
"doi-asserted-by": "publisher",
"journal-title": "Front Med",
"key": "B28",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2021.708494/full",
"article-title": "Mortality risk of antidiabetic agents for type 2 diabetes with COVID-19: A systematic review and meta-analysis",
"author": "Kan",
"doi-asserted-by": "publisher",
"journal-title": "Front Endocrinol (Lausanne)",
"key": "B29",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.diabres.2020.108183",
"article-title": "Metformin in COVID-19: A possible role beyond diabetes",
"author": "Sharma",
"doi-asserted-by": "publisher",
"first-page": "108183",
"journal-title": "Diabetes Res Clin Pract",
"key": "B30",
"volume": "164",
"year": "2020"
},
{
"DOI": "10.1007/s00005-020-00602-5",
"article-title": "DPP4 inhibitors and COVID-19-Holy grail or another dead end",
"author": "Krejner-Bienias",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Arch Immunol Ther Exp (Warsz)",
"key": "B31",
"volume": "69",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0251916",
"article-title": "DPP-4 inhibitors may improve the mortality of coronavirus disease 2019: A meta-analysis",
"author": "Yang",
"doi-asserted-by": "publisher",
"first-page": "e0251916",
"journal-title": "PloS One",
"key": "B32",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2021.03.027",
"article-title": "Dipeptidyl peptidase-4 (DPP-4) inhibitor and mortality in coronavirus disease 2019 (COVID-19) - a systematic review, meta-analysis, and meta-regression",
"author": "Rakhmat",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab Syndr",
"key": "B33",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1016/S2213-8587(21)00180-7",
"article-title": "Dapagliflozin in patients with cardiometabolic risk factors hospitalised with COVID-19 (DARE-19): A randomised, double-blind, placebo-controlled, phase 3 trial",
"author": "Kosiborod",
"doi-asserted-by": "publisher",
"journal-title": "Lancet Diabetes Endocrinol",
"key": "B34",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1007/s40200-021-00833-z",
"article-title": "Treatment with a DPP-4 inhibitor at time of hospital admission for COVID-19 is not associated with improved clinical outcomes: Data from the COVID-PREDICT cohort study in the Netherlands",
"author": "Meijer",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Diabetes Metab Disord",
"key": "B35",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1007/s13300-019-00686-z",
"article-title": "The pleiotropic effects of sodium-glucose cotransporter-2 inhibitors: Beyond the glycemic benefit",
"author": "Patel",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Ther Res Treat Educ Diabetes Relat Disord",
"key": "B36",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1093/eurjpc/zwab034",
"article-title": "Protective effects of SGLT-2 inhibitors across the cardiorenal continuum: two faces of the same coin",
"author": "Fontes-Carvalho",
"doi-asserted-by": "publisher",
"journal-title": "Eur J Prev Cardiol",
"key": "B37",
"year": "2021"
},
{
"DOI": "10.1016/j.diabres.2021.109031",
"article-title": "Pre-admission glucagon-like peptide-1 receptor agonist (GLP-1RA) and mortality from coronavirus disease 2019 (Covid-19): A systematic review, meta-analysis, and meta-regression",
"author": "Hariyanto",
"doi-asserted-by": "publisher",
"first-page": "109031",
"journal-title": "Diabetes Res Clin Pract",
"key": "B38",
"volume": "179",
"year": "2021"
},
{
"DOI": "10.1016/j.molmet.2020.101102",
"article-title": "GLP-1 receptor agonists in the treatment of type 2 diabetes - state-of-the-art",
"author": "Nauck",
"doi-asserted-by": "publisher",
"first-page": "101102",
"journal-title": "Mol Metab",
"key": "B39",
"volume": "46",
"year": "2021"
},
{
"DOI": "10.2337/dc20-0660",
"article-title": "Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication",
"author": "Chen",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Care",
"key": "B40",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.3389/fendo.2021.696087/full",
"article-title": "Insulin treatment may increase adverse outcomes in patients with COVID-19 and diabetes: A systematic review and meta-analysis",
"author": "Yang",
"doi-asserted-by": "publisher",
"journal-title": "Front Endocrinol (Lausanne)",
"key": "B41",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1101/2021.01.26.21250506",
"article-title": "The association between anti-diabetic agents and clinical outcomes of COVID-19 in patients with diabetes: A systematic review and meta-analysis",
"author": "Han",
"doi-asserted-by": "publisher",
"journal-title": "Arch Med Res",
"key": "B42",
"volume": "53",
"year": "2021"
},
{
"DOI": "10.14341/DM12759",
"article-title": "Epidemiological characteristics of diabetes mellitus in the Russian federation: Clinical and statistical analysis according to the federal diabetes register data of 01.01.2021",
"author": "Dedov",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Mellit",
"key": "B43",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1111/dom.12280",
"article-title": "Mortality risk with sulphonylureas compared to metformin",
"author": "Holden",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Obes Metab",
"key": "B44",
"volume": "16",
"year": "2014"
},
{
"DOI": "10.1093/eurheartj/ehr077",
"article-title": "Mortality and cardiovascular risk associated with different insulin secretagogues compared with metformin in type 2 diabetes, with or without a previous myocardial infarction: a nationwide study",
"author": "Schramm",
"doi-asserted-by": "publisher",
"journal-title": "Eur Heart J",
"key": "B45",
"volume": "32",
"year": "2011"
},
{
"DOI": "10.1136/bmj.k2693",
"article-title": "Sulfonylureas as second line drugs in type 2 diabetes and the risk of cardiovascular and hypoglycaemic events: Population based cohort study",
"author": "Douros",
"doi-asserted-by": "publisher",
"first-page": "k2693",
"journal-title": "BMJ",
"key": "B46",
"volume": "362",
"year": "2018"
},
{
"DOI": "10.1016/S0140-6736(21)00234-8",
"article-title": "Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: An interim analysis of a randomised controlled phase 3 trial in Russia",
"author": "Logunov",
"doi-asserted-by": "publisher",
"journal-title": "Lancet",
"key": "B47",
"volume": "397",
"year": "2021"
},
{
"DOI": "10.1210/clinem/dgab055",
"article-title": "Robust neutralizing antibodies to SARS-CoV-2 develop and persist in subjects with diabetes and COVID-19 pneumonia",
"author": "Dispinseri",
"doi-asserted-by": "publisher",
"journal-title": "J Clin Endocrinol Metab",
"key": "B48",
"volume": "106",
"year": "2021"
},
{
"article-title": "Deaths involving COVID-19 by vaccination status, England: deaths occurring between 2 January and 24 September 2021",
"author": "Bermingham",
"key": "B49",
"volume-title": "Deaths involving COVID-19 by vaccination status, England: deaths occurring between 2 January and 24 September 2021",
"year": ""
}
],
"reference-count": 49,
"references-count": 49,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fendo.2022.909874/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Risk factors for COVID-19 case fatality rate in people with type 1 and type 2 diabetes mellitus: A nationwide retrospective cohort study of 235,248 patients in the Russian Federation",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "13"
}
