Impact of overlapping risks of type 2 diabetes and obesity on coronavirus disease severity in the United States
et al., Scientific Reports, doi:10.1038/s41598-021-96720-x, Sep 2021
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 28,093 COVID+ patients in the USA, showing lower risk of hospitalization with metformin use.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
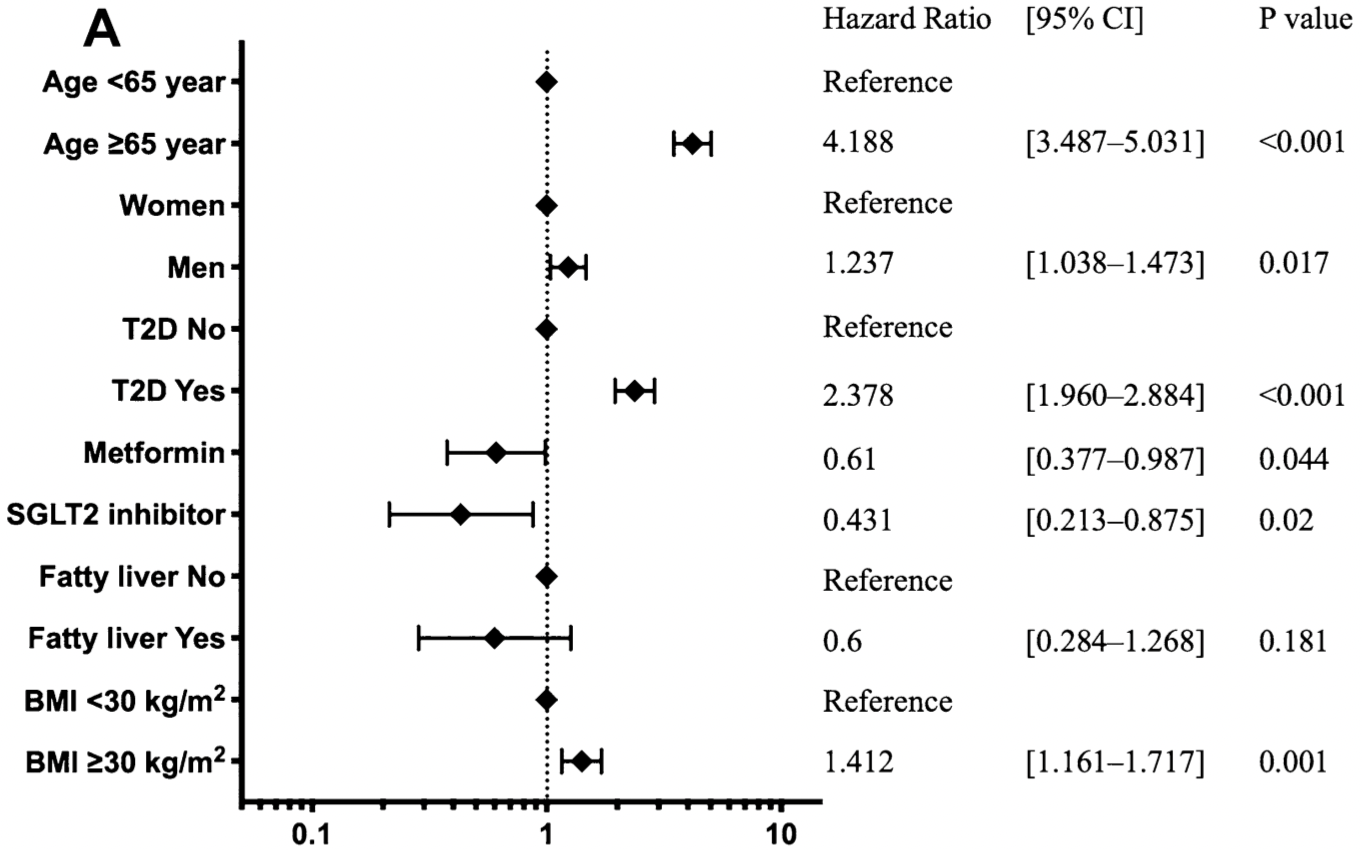
risk of hospitalization, 39.0% lower, HR 0.61, p = 0.04, treatment 19 of 663 (2.9%), control 1,056 of 27,430 (3.8%), adjusted per study, multivariable, Cox proportional hazards.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ando et al., 9 Sep 2021, retrospective, USA, peer-reviewed, 6 authors, study period 1 January, 2020 - 30 November, 2020.
Impact of overlapping risks of type 2 diabetes and obesity on coronavirus disease severity in the United States
Scientific Reports, doi:10.1038/s41598-021-96720-x
The impact of overlapping risk factors on coronavirus disease (COVID-19) severity is unclear. To evaluate the impact of type 2 diabetes (T2D) and obesity on COVID-19 severity, we conducted a cohort study with 28,095 anonymized COVID-19 patients using data from the COVID-19 Research Database from January 1, 2020 to November 30, 2020. The mean age was 50.8 ± 17.5 years, and 11,802 (42%) patients were male. Data on age, race, sex, T2D complications, antidiabetic medication prescription, and body mass index ≥ 30 kg/m 2 (obesity) were analysed using Cox proportional hazard models, with hospitalization risk and critical care within 30 days of COVID-19 diagnosis as the main outcomes. The risk scores were 0-4 for age ≥ 65 years, male sex, T2D, and obesity. Among the participants, 11,294 (61.9%) had obesity, and 4445 (15.8%) had T2D. T2D, obesity, and male sex were significantly associated with COVID-19 hospitalization risk. Regarding hospitalization risk scores, compared with those for hospitalization risk score 0 and critical care risk score 0, hazard ratios [95% confidence intervals] were 19.
www.nature.com/scientificreports/ patients. Therefore, further studies are required to evaluate the effects of blood glucose control and obesity on COVID-19. The BMI data comprise values measured up to 6 months prior to this study and may not accurately reflect the values immediately before the diagnosis of COVID-19. Because of the small number of cases of fatty liver and the exclusive availability of Non-alcoholic fatty liver disease (NAFLD) in CPT4 codes, the risk of COVID-19 severity in patients with fatty liver should be studied in detail in a larger population. Confounding factors for hospitalization and critical care risks should consider non-diabetic complications such as cardiovascular events. We hypothesized that there would be a period in the early phase of the epidemic (in the first half of 2020) when the high number of patients would overwhelm the health care system, and treatment of the most critically ill patients would be prioritized. Therefore, we attempted to examine the risk in early 2020. However, because of limited data in the early phase of the epidemic and concerns about accuracy, this database is not considered to have adequately accounted for the relative risks of outcomes related to diabetes, age, and BMI. Therefore, we hope that this issue will be clarified in the future as the risk of severe disease was unevenly distributed during the acute phase of the pandemic. In examining the risk score, we considered the weight of the patients; however, it was..
References
Aggarwal, Association of cardiovascular disease with coronavirus disease 2019 (COVID-19) severity: A meta-analysis, Curr. Probl. Cardiol, doi:10.1016/j.cpcardiol.2020.100617
Ali, Achievement of goals in U.S. diabetes care, 1999-2010, N. Engl. J. Med, doi:10.1056/NEJMsa1213829
Best, Baseline demographics and clinical characteristics among 3471 US patients hospitalized with COVID-19 and pulmonary involvement: A retrospective study, Adv. Ther, doi:10.1007/s12325-020-01510-y
Bossi, Forloni, Colombelli, Lack of efficacy of SGLT2-i in severe pneumonia related to novel coronavirus (nCoV) infection: No little help from our friends, Diabetes Ther, doi:10.1007/s13300-020-00844-8
Cases, COVID-19 Hospitalization and Death by Age
Cheng, Secular changes in the age-specific prevalence of diabetes among U.S. adults: 1988-2010, Diabetes Care, doi:10.2337/dc12-2074
Cowie, Fisher, SGLT2 inhibitors: Mechanisms of cardiovascular benefit beyond glycaemic control, Nat. Rev. Cardiol, doi:10.1038/s41569-020-0406-8
Flegal, Carroll, Ogden, Curtin, Prevalence and trends in obesity among US adults, 1999-2008, JAMA, doi:10.1001/jama.2009.2014
Fox, Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: A scientific statement from the American Heart Association and the American Diabetes Association, Diabetes Care, doi:10.2337/dci15-0012
Fried, Patient characteristics and outcomes of 11,721 patients with COVID19 hospitalized across the United States, Clin. Infect. Dis, doi:10.1093/cid/ciaa1268
Gold, Race, ethnicity, and age trends in persons who died from COVID-19: United States, MMWR Morb. Mortal. Wkly. Rep, doi:10.15585/mmwr.mm6942e1
Goodman, Impact of sex and metabolic comorbidities on COVID-19 mortality risk across age groups: 66,646 inpatients across 613, Clin. Infect. Dis, doi:10.1093/cid/ciaa1787
Grasselli, Pathophysiology of COVID-19-associated acute respiratory distress syndrome: A multicentre prospective observational study, Lancet Respir. Med, doi:10.1016/S2213-2600(20)30370-2
Hamer, Gale, Kivimaki, Batty, Overweight, obesity, and risk of hospitalization for COVID-19: A communitybased cohort study of adults in the United Kingdom, Proc. Natl. Acad. Sci. U. S. A, doi:10.1073/pnas.2011086117
Holman, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: A populationbased cohort study, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30271-0
Izurieta, Natural history of COVID-19: Risk factors for hospitalizations and deaths among > 26 million U.S. Medicare beneficiaries, J. Infect. Dis, doi:10.1093/infdis/jiaa767
Kosiborod, Effects of dapagliflozin on prevention of major clinical events and recovery in patients with respiratory failure because of COVID-19: Design and rationale for the DARE-19 study, Diabetes Obes. Metab, doi:10.1111/dom.14296
Kow, Hasan, Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis, J. Med. Virol, doi:10.1002/jmv.26498
Lalau, Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19, Diabetes Metab, doi:10.1016/j.diabet.2020.101216
Liang, Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19, JAMA Intern. Med, doi:10.1001/jamainternmed.2020.2033
Lundon, Social determinants predict outcomes in data from a multi-ethnic cohort of 20,899 patients investigated for COVID-19, Front. Public Health, doi:10.3389/fpubh.2020.571364
Moazzami, Metabolic risk factors and risk of Covid-19: A systematic review and meta-analysis, PLoS ONE, doi:10.1371/journal.pone.0243600
Nishiga, Wang, Han, Lewis, Wu, COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives, Nat. Rev. Cardiol, doi:10.1038/s41569-020-0413-9
O'driscoll, Age-specific mortality and immunity patterns of SARS-CoV-2, Nature, doi:10.1038/s41586-020-2918-0
Patoulias, Papadopoulos, Katsimardou, Toumpourleka, Doumas, Sodium-glucose cotransporter 2 inhibitors and major COVID-19 outcomes: Promising mechanisms, conflicting data, and intriguing clinical decisions, Diabetes Ther, doi:10.1007/s13300-020-00942-7
Perez-Belmonte, Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: A nationwide cohort study, BMC Med, doi:10.1186/s12916-020-01832-2
Perkin, Deaths in people from Black, Asian and minority ethnic communities from both COVID-19 and non-COVID causes in the first weeks of the pandemic in London: A hospital case note review, BMJ Open, doi:10.1136/bmjopen-2020-040638
Popkin, Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships, Obes. Rev, doi:10.1111/obr.13128
Raisi-Estabragh, Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: Study of 1326 cases from the UK Biobank, J. Public Health (Oxf.), doi:10.1093/pubmed/fdaa095
Ssentongo, Ssentongo, Heilbrunn, Ba, Chinchilli, Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis, PLoS ONE, doi:10.1371/journal.pone.0238215
Wang, Type 2 diabetes mellitus is associated with increased risks of sarcopenia and pre-sarcopenia in Chinese elderly, Sci. Rep, doi:10.1038/srep38937
Wikner, Gigante, Hellenius, De Faire, Leander, The risk of type 2 diabetes in men is synergistically affected by parental history of diabetes and overweight, PLoS ONE, doi:10.1371/journal.pone.0061763
DOI record:
{
"DOI": "10.1038/s41598-021-96720-x",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-021-96720-x",
"abstract": "<jats:title>Abstract</jats:title><jats:p>The impact of overlapping risk factors on coronavirus disease (COVID-19) severity is unclear. To evaluate the impact of type 2 diabetes (T2D) and obesity on COVID-19 severity, we conducted a cohort study with 28,095 anonymized COVID-19 patients using data from the COVID-19 Research Database from January 1, 2020 to November 30, 2020. The mean age was 50.8 ± 17.5 years, and 11,802 (42%) patients were male. Data on age, race, sex, T2D complications, antidiabetic medication prescription, and body mass index ≥ 30 kg/m<jats:sup>2</jats:sup> (obesity) were analysed using Cox proportional hazard models, with hospitalization risk and critical care within 30 days of COVID-19 diagnosis as the main outcomes. The risk scores were 0–4 for age ≥ 65 years, male sex, T2D, and obesity. Among the participants, 11,294 (61.9%) had obesity, and 4445 (15.8%) had T2D. T2D, obesity, and male sex were significantly associated with COVID-19 hospitalization risk. Regarding hospitalization risk scores, compared with those for hospitalization risk score 0 and critical care risk score 0, hazard ratios [95% confidence intervals] were 19.034 [10.470–34.600] and 55.803 [12.761–244.015] (<jats:italic>P</jats:italic> < 0.001) (<jats:italic>P</jats:italic> < 0.001), respectively, for risk score 4. Complications from diabetes and obesity increased hospitalization and critical care risks for COVID-19 patients.</jats:p>",
"alternative-id": [
"96720"
],
"article-number": "17968",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "9 February 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "12 August 2021"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "9 September 2021"
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Ando",
"given": "Wataru",
"sequence": "first"
},
{
"affiliation": [],
"family": "Horii",
"given": "Takeshi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Uematsu",
"given": "Takayuki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hanaki",
"given": "Hideaki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Atsuda",
"given": "Koichiro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Otori",
"given": "Katsuya",
"sequence": "additional"
}
],
"container-title": [
"Scientific Reports"
],
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2021,
9,
9
]
],
"date-time": "2021-09-09T10:06:24Z",
"timestamp": 1631181984000
},
"deposited": {
"date-parts": [
[
2021,
9,
9
]
],
"date-time": "2021-09-09T10:35:13Z",
"timestamp": 1631183713000
},
"indexed": {
"date-parts": [
[
2021,
12,
11
]
],
"date-time": "2021-12-11T23:26:47Z",
"timestamp": 1639265207258
},
"is-referenced-by-count": 1,
"issn-type": [
{
"type": "electronic",
"value": "2045-2322"
}
],
"issue": "1",
"issued": {
"date-parts": [
[
2021,
9,
9
]
]
},
"journal-issue": {
"issue": "1",
"published-print": {
"date-parts": [
[
2021,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
9
]
],
"date-time": "2021-09-09T00:00:00Z",
"timestamp": 1631145600000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
9,
9
]
],
"date-time": "2021-09-09T00:00:00Z",
"timestamp": 1631145600000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-021-96720-x.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-021-96720-x",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-021-96720-x.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2021,
9,
9
]
]
},
"published-online": {
"date-parts": [
[
2021,
9,
9
]
]
},
"published-print": {
"date-parts": [
[
2021,
12
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1038/s41586-020-2918-0",
"author": "M O'Driscoll",
"doi-asserted-by": "publisher",
"first-page": "140",
"journal-title": "Nature",
"key": "96720_CR1",
"unstructured": "O’Driscoll, M. et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature 590, 140–145. https://doi.org/10.1038/s41586-020-2918-0 (2021).",
"volume": "590",
"year": "2021"
},
{
"DOI": "10.15585/mmwr.mm6942e1",
"author": "JAW Gold",
"doi-asserted-by": "publisher",
"first-page": "1517",
"journal-title": "MMWR Morb. Mortal. Wkly. Rep.",
"key": "96720_CR2",
"unstructured": "Gold, J. A. W. et al. Race, ethnicity, and age trends in persons who died from COVID-19: United States, May–August 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 1517–1521. https://doi.org/10.15585/mmwr.mm6942e1 (2020).",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/S2213-2600(20)30370-2",
"author": "G Grasselli",
"doi-asserted-by": "publisher",
"first-page": "1201",
"journal-title": "Lancet Respir. Med.",
"key": "96720_CR3",
"unstructured": "Grasselli, G. et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: A multicentre prospective observational study. Lancet Respir. Med. 8, 1201–1208. https://doi.org/10.1016/S2213-2600(20)30370-2 (2020).",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1111/obr.13128",
"author": "BM Popkin",
"doi-asserted-by": "publisher",
"journal-title": "Obes. Rev.",
"key": "96720_CR4",
"unstructured": "Popkin, B. M. et al. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 21, e13128. https://doi.org/10.1111/obr.13128 (2020).",
"volume": "21",
"year": "2020"
},
{
"key": "96720_CR5",
"unstructured": "CASES, D. S. COVID-19 Hospitalization and Death by Age (Updated Aug. 18, 2020), https://www.cdc.gov/coronavirus/2019-ncov/covid-data/ (2020)."
},
{
"DOI": "10.1038/s41569-020-0413-9",
"author": "M Nishiga",
"doi-asserted-by": "publisher",
"first-page": "543",
"journal-title": "Nat. Rev. Cardiol.",
"key": "96720_CR6",
"unstructured": "Nishiga, M., Wang, D. W., Han, Y., Lewis, D. B. & Wu, J. C. COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives. Nat. Rev. Cardiol. 17, 543–558. https://doi.org/10.1038/s41569-020-0413-9 (2020).",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30271-0",
"author": "N Holman",
"doi-asserted-by": "publisher",
"first-page": "823",
"journal-title": "Lancet Diabetes Endocrinol.",
"key": "96720_CR7",
"unstructured": "Holman, N. et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: A population-based cohort study. Lancet Diabetes Endocrinol. 8, 823–833. https://doi.org/10.1016/S2213-8587(20)30271-0 (2020).",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.2337/dci15-0012",
"author": "CS Fox",
"doi-asserted-by": "publisher",
"first-page": "1777",
"journal-title": "Diabetes Care",
"key": "96720_CR8",
"unstructured": "Fox, C. S. et al. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: A scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care 38, 1777–1803. https://doi.org/10.2337/dci15-0012 (2015).",
"volume": "38",
"year": "2015"
},
{
"DOI": "10.2337/dc12-2074",
"author": "YJ Cheng",
"doi-asserted-by": "publisher",
"first-page": "2690",
"journal-title": "Diabetes Care",
"key": "96720_CR9",
"unstructured": "Cheng, Y. J. et al. Secular changes in the age-specific prevalence of diabetes among U.S. adults: 1988–2010. Diabetes Care 36, 2690–2696. https://doi.org/10.2337/dc12-2074 (2013).",
"volume": "36",
"year": "2013"
},
{
"DOI": "10.1056/NEJMsa1213829",
"author": "MK Ali",
"doi-asserted-by": "publisher",
"first-page": "1613",
"journal-title": "N. Engl. J. Med.",
"key": "96720_CR10",
"unstructured": "Ali, M. K. et al. Achievement of goals in U.S. diabetes care, 1999–2010. N. Engl. J. Med. 368, 1613–1624. https://doi.org/10.1056/NEJMsa1213829 (2013).",
"volume": "368",
"year": "2013"
},
{
"DOI": "10.1038/srep38937",
"author": "T Wang",
"doi-asserted-by": "publisher",
"first-page": "38937",
"journal-title": "Sci. Rep.",
"key": "96720_CR11",
"unstructured": "Wang, T. et al. Type 2 diabetes mellitus is associated with increased risks of sarcopenia and pre-sarcopenia in Chinese elderly. Sci. Rep. 6, 38937. https://doi.org/10.1038/srep38937 (2016).",
"volume": "6",
"year": "2016"
},
{
"DOI": "10.1371/journal.pone.0061763",
"author": "C Wikner",
"doi-asserted-by": "publisher",
"journal-title": "PLoS ONE",
"key": "96720_CR12",
"unstructured": "Wikner, C., Gigante, B., Hellenius, M. L., de Faire, U. & Leander, K. The risk of type 2 diabetes in men is synergistically affected by parental history of diabetes and overweight. PLoS ONE 8, e61763. https://doi.org/10.1371/journal.pone.0061763 (2013).",
"volume": "8",
"year": "2013"
},
{
"DOI": "10.1093/cid/ciaa1268",
"author": "MW Fried",
"doi-asserted-by": "publisher",
"journal-title": "Clin. Infect. Dis.",
"key": "96720_CR13",
"unstructured": "Fried, M. W. et al. Patient characteristics and outcomes of 11,721 patients with COVID19 hospitalized across the United States. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciaa1268 (2020).",
"year": "2020"
},
{
"DOI": "10.1007/s12325-020-01510-y",
"author": "JH Best",
"doi-asserted-by": "publisher",
"first-page": "4981",
"journal-title": "Adv. Ther.",
"key": "96720_CR14",
"unstructured": "Best, J. H. et al. Baseline demographics and clinical characteristics among 3471 US patients hospitalized with COVID-19 and pulmonary involvement: A retrospective study. Adv. Ther. 37, 4981–4995. https://doi.org/10.1007/s12325-020-01510-y (2020).",
"volume": "37",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0243600",
"author": "B Moazzami",
"doi-asserted-by": "publisher",
"journal-title": "PLoS ONE",
"key": "96720_CR15",
"unstructured": "Moazzami, B. et al. Metabolic risk factors and risk of Covid-19: A systematic review and meta-analysis. PLoS ONE 15, e0243600. https://doi.org/10.1371/journal.pone.0243600 (2020).",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1093/cid/ciaa1787",
"author": "KE Goodman",
"doi-asserted-by": "publisher",
"journal-title": "Clin. Infect. Dis.",
"key": "96720_CR16",
"unstructured": "Goodman, K. E. et al. Impact of sex and metabolic comorbidities on COVID-19 mortality risk across age groups: 66,646 inpatients across 613 U.S. hospitals. Clin. Infect. Dis. https://doi.org/10.1093/cid/ciaa1787 (2020).",
"year": "2020"
},
{
"DOI": "10.1073/pnas.2011086117",
"author": "M Hamer",
"doi-asserted-by": "publisher",
"first-page": "21011",
"journal-title": "Proc. Natl. Acad. Sci. U. S. A.",
"key": "96720_CR17",
"unstructured": "Hamer, M., Gale, C. R., Kivimaki, M. & Batty, G. D. Overweight, obesity, and risk of hospitalization for COVID-19: A community-based cohort study of adults in the United Kingdom. Proc. Natl. Acad. Sci. U. S. A. 117, 21011–21013. https://doi.org/10.1073/pnas.2011086117 (2020).",
"volume": "117",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.101216",
"author": "JD Lalau",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Metab.",
"key": "96720_CR18",
"unstructured": "Lalau, J. D. et al. Metformin use is associated with a reduced risk of mortality in patients with diabetes hospitalised for COVID-19. Diabetes Metab. https://doi.org/10.1016/j.diabet.2020.101216 (2020).",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26498",
"author": "CS Kow",
"doi-asserted-by": "publisher",
"first-page": "695",
"journal-title": "J. Med. Virol.",
"key": "96720_CR19",
"unstructured": "Kow, C. S. & Hasan, S. S. Mortality risk with preadmission metformin use in patients with COVID-19 and diabetes: A meta-analysis. J. Med. Virol. 93, 695–697. https://doi.org/10.1002/jmv.26498 (2021).",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.1007/s13300-020-00942-7",
"author": "D Patoulias",
"doi-asserted-by": "publisher",
"first-page": "3003",
"journal-title": "Diabetes Ther.",
"key": "96720_CR20",
"unstructured": "Patoulias, D., Papadopoulos, C., Katsimardou, A., Toumpourleka, M. & Doumas, M. Sodium-glucose cotransporter 2 inhibitors and major COVID-19 outcomes: Promising mechanisms, conflicting data, and intriguing clinical decisions. Diabetes Ther. 11, 3003–3005. https://doi.org/10.1007/s13300-020-00942-7 (2020).",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1038/s41569-020-0406-8",
"author": "MR Cowie",
"doi-asserted-by": "publisher",
"first-page": "761",
"journal-title": "Nat. Rev. Cardiol.",
"key": "96720_CR21",
"unstructured": "Cowie, M. R. & Fisher, M. SGLT2 inhibitors: Mechanisms of cardiovascular benefit beyond glycaemic control. Nat. Rev. Cardiol. 17, 761–772. https://doi.org/10.1038/s41569-020-0406-8 (2020).",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1007/s13300-020-00844-8",
"author": "AC Bossi",
"doi-asserted-by": "publisher",
"first-page": "1605",
"journal-title": "Diabetes Ther.",
"key": "96720_CR22",
"unstructured": "Bossi, A. C., Forloni, F. & Colombelli, P. L. Lack of efficacy of SGLT2-i in severe pneumonia related to novel coronavirus (nCoV) infection: No little help from our friends. Diabetes Ther. 11, 1605–1606. https://doi.org/10.1007/s13300-020-00844-8 (2020).",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0238215",
"author": "P Ssentongo",
"doi-asserted-by": "publisher",
"journal-title": "PLoS ONE",
"key": "96720_CR23",
"unstructured": "Ssentongo, P., Ssentongo, A. E., Heilbrunn, E. S., Ba, D. M. & Chinchilli, V. M. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis. PLoS ONE 15, e0238215. https://doi.org/10.1371/journal.pone.0238215 (2020).",
"volume": "15",
"year": "2020"
},
{
"DOI": "10.1111/dom.14296",
"author": "M Kosiborod",
"doi-asserted-by": "publisher",
"journal-title": "Diabetes Obes. Metab.",
"key": "96720_CR24",
"unstructured": "Kosiborod, M. et al. Effects of dapagliflozin on prevention of major clinical events and recovery in patients with respiratory failure because of COVID-19: Design and rationale for the DARE-19 study. Diabetes Obes. Metab. https://doi.org/10.1111/dom.14296 (2020).",
"year": "2020"
},
{
"DOI": "10.1186/s12916-020-01832-2",
"author": "LM Perez-Belmonte",
"doi-asserted-by": "publisher",
"first-page": "359",
"journal-title": "BMC Med.",
"key": "96720_CR25",
"unstructured": "Perez-Belmonte, L. M. et al. Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: A nationwide cohort study. BMC Med. 18, 359. https://doi.org/10.1186/s12916-020-01832-2 (2020).",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1001/jamainternmed.2020.2033",
"author": "W Liang",
"doi-asserted-by": "publisher",
"first-page": "1081",
"journal-title": "JAMA Intern. Med.",
"key": "96720_CR26",
"unstructured": "Liang, W. et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern. Med. 180, 1081–1089. https://doi.org/10.1001/jamainternmed.2020.2033 (2020).",
"volume": "180",
"year": "2020"
},
{
"DOI": "10.1093/pubmed/fdaa095",
"author": "Z Raisi-Estabragh",
"doi-asserted-by": "publisher",
"first-page": "451",
"journal-title": "J. Public Health (Oxf.)",
"key": "96720_CR27",
"unstructured": "Raisi-Estabragh, Z. et al. Greater risk of severe COVID-19 in Black, Asian and Minority Ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25(OH)-vitamin D status: Study of 1326 cases from the UK Biobank. J. Public Health (Oxf.) 42, 451–460. https://doi.org/10.1093/pubmed/fdaa095 (2020).",
"volume": "42",
"year": "2020"
},
{
"DOI": "10.1016/j.cpcardiol.2020.100617",
"author": "G Aggarwal",
"doi-asserted-by": "publisher",
"journal-title": "Curr. Probl. Cardiol.",
"key": "96720_CR28",
"unstructured": "Aggarwal, G. et al. Association of cardiovascular disease with coronavirus disease 2019 (COVID-19) severity: A meta-analysis. Curr. Probl. Cardiol. 45, 100617. https://doi.org/10.1016/j.cpcardiol.2020.100617 (2020).",
"volume": "45",
"year": "2020"
},
{
"DOI": "10.1136/bmjopen-2020-040638",
"author": "MR Perkin",
"doi-asserted-by": "publisher",
"journal-title": "BMJ Open",
"key": "96720_CR29",
"unstructured": "Perkin, M. R. et al. Deaths in people from Black, Asian and minority ethnic communities from both COVID-19 and non-COVID causes in the first weeks of the pandemic in London: A hospital case note review. BMJ Open 10, e040638. https://doi.org/10.1136/bmjopen-2020-040638 (2020).",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1093/infdis/jiaa767",
"author": "HS Izurieta",
"doi-asserted-by": "publisher",
"journal-title": "J. Infect. Dis.",
"key": "96720_CR30",
"unstructured": "Izurieta, H. S. et al. Natural history of COVID-19: Risk factors for hospitalizations and deaths among > 26 million U.S. Medicare beneficiaries. J. Infect. Dis. https://doi.org/10.1093/infdis/jiaa767 (2020).",
"year": "2020"
},
{
"DOI": "10.3389/fpubh.2020.571364",
"author": "DJ Lundon",
"doi-asserted-by": "publisher",
"journal-title": "Front. Public Health",
"key": "96720_CR31",
"unstructured": "Lundon, D. J. et al. Social determinants predict outcomes in data from a multi-ethnic cohort of 20,899 patients investigated for COVID-19. Front. Public Health 8, 571364. https://doi.org/10.3389/fpubh.2020.571364 (2020).",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1001/jama.2009.2014",
"author": "KM Flegal",
"doi-asserted-by": "publisher",
"first-page": "235",
"journal-title": "JAMA",
"key": "96720_CR32",
"unstructured": "Flegal, K. M., Carroll, M. D., Ogden, C. L. & Curtin, L. R. Prevalence and trends in obesity among US adults, 1999–2008. JAMA 303, 235–241. https://doi.org/10.1001/jama.2009.2014 (2010).",
"volume": "303",
"year": "2010"
}
],
"reference-count": 32,
"references-count": 32,
"relation": {},
"score": 1,
"short-container-title": [
"Sci Rep"
],
"short-title": [],
"source": "Crossref",
"subject": [
"Multidisciplinary"
],
"subtitle": [],
"title": [
"Impact of overlapping risks of type 2 diabetes and obesity on coronavirus disease severity in the United States"
],
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "11"
}
