Prognostic Factors for COVID-19 Hospitalized Patients with Preexisting Type 2 Diabetes
et al., International Journal of Endocrinology, doi:10.1155/2022/9322332, Jan 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
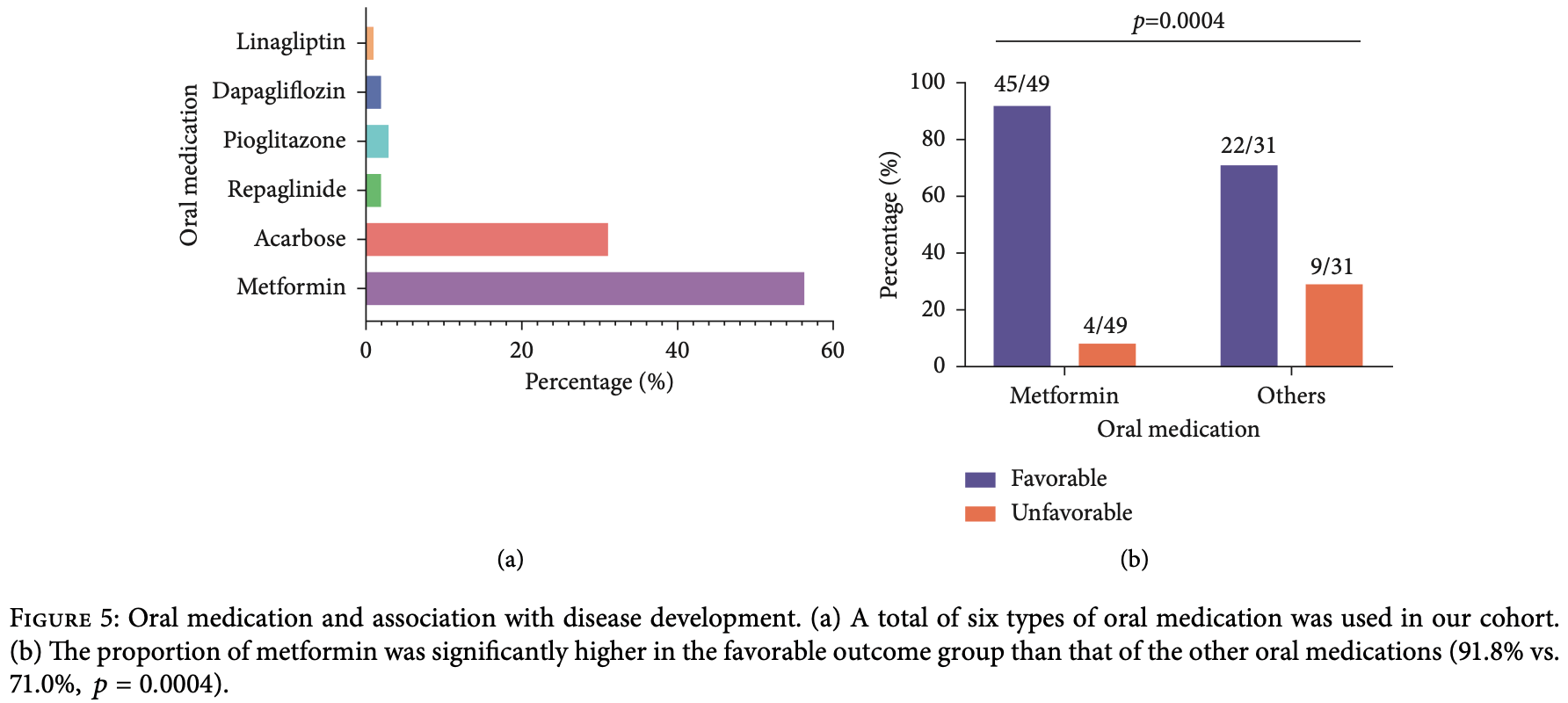
Retrospective 108 T2D patients hospitalized with COVID-19, showing lower risk of unfavorable outcomes with metformin use vs. other diabetic medications.
Standard of Care (SOC) for COVID-19 in the study country,
China, is average with moderate efficacy for approved treatments1.
|
risk of unfavorable outcome, 71.9% lower, RR 0.28, p = 0.03, treatment 4 of 49 (8.2%), control 9 of 31 (29.0%), NNT 4.8, unfavorable outcome, metformin vs. other treatments.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Fu et al., 17 Jan 2022, retrospective, China, peer-reviewed, median age 63.0, 14 authors, study period 8 January, 2020 - 7 March, 2020, this trial compares with another treatment - results may be better when compared to placebo.
Contact: dengy@hawaii.edu.
Prognostic Factors for COVID-19 Hospitalized Patients with Preexisting Type 2 Diabetes
International Journal of Endocrinology, doi:10.1155/2022/9322332
Background. Type 2 diabetes (T2D) as a worldwide chronic disease combined with the COVID-19 pandemic prompts the need for improving the management of hospitalized COVID-19 patients with preexisting T2D to reduce complications and the risk of death. is study aimed to identify clinical factors associated with COVID-19 outcomes specifically targeted at T2D patients and build an individualized risk prediction nomogram for risk stratification and early clinical intervention to reduce mortality. Methods. In this retrospective study, the clinical characteristics of 382 confirmed COVID-19 patients, consisting of 108 with and 274 without preexisting T2D, from January 8 to March 7, 2020, in Tianyou Hospital in Wuhan, China, were collected and analyzed. Univariate and multivariate Cox regression models were performed to identify specific clinical factors associated with mortality of COVID-19 patients with T2D. An individualized risk prediction nomogram was developed and evaluated by discrimination and calibration. Results. Nearly 15% (16/108) of hospitalized COVID-19 patients with T2D died. Twelve risk factors predictive of mortality were identified. Older age (HR � 1.076, 95% CI � 1.014-1.143, p � 0.016), elevated glucose level (HR � 1.153, 95% CI � 1.038-1.28, p � 0.0079), increased serum amyloid A (SAA) (HR � 1.007, 95% CI � 1.001-1.014, p � 0.022), diabetes treatment with only oral diabetes medication (HR � 0.152, 95%CI � 0.032-0.73, p � 0.0036), and oral medication plus insulin (HR � 0.095, 95%CI � 0.019-0.462, p � 0.019) were independent prognostic factors. A nomogram based on these prognostic factors was built for early prediction of 7-day, 14-day, and 21-day survival of diabetes patients. High concordance index (C-index) was achieved, and the calibration curves showed the model had good prediction ability within three weeks of COVID-19 onset. Conclusions. By incorporating specific prognostic factors, this study provided a user-friendly graphical risk prediction tool for clinicians to quickly identify high-risk T2D patients hospitalized for COVID-19.
Conflicts of Interest e authors declare no conflicts of interest.
Authors' Contributions YD and LH conceived and supervised the study. LH, QSZ, CS, YM, LW, JJH, and CZW collected the epidemiological and clinical data. LH, YZ, SC, and HWR contributed to radiological figure interpretation. YF and ZW processed and conducted statistical data analyses. YF, ZW, and RY drafted the manuscript. All the authors reviewed and approved the final version for publication. YD and YF are responsible for the integrity of the data and the accuracy of the analyzed data.
Supplementary Materials Supplementary table S1 : clinical characteristics of COVID-19 patients with and without T2D. Supplementary table S2 : clinical characteristics between survivors and nonsurvivors in COVID-19 patients with T2D. Fig. S1 : representative dynamic changes in chest computer tomography (CT) scans between admission and discharge for the three diabetes treatment groups. Fig. S2 : survival analysis for the three diabetes treatment groups. Fig. S3 : blood glucose levels of the three diabetes treatment groups. (Supplementary Materials)
References
-H. Haroun, Osman, Eessa, Interferonc-induced protein 10 (IP-10) and serum amyloid A (SAA) are excellent biomarkers for the prediction of COVID-19 progression and severity, Life Sciences
Abuissa, Jones, Marso, O'keefe, Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for prevention of type 2 diabetes, Journal of the American College of Cardiology
Al-Salameh, Bennis, Cariou, Lalau, e association between metformin treatment and COVID-19 outcomes according to metformin continuation during hospitalisation, Diabetes & Metabolism
Batlle, Soler, Ye, ACE2 and diabetes: ACE of ACEs?, Diabetes
Bell, Patil, O'keefe, Divergent effects of various diabetes drugs on cardiovascular prognosis, Reviews in Cardiovascular Medicine
Benfield, Jensen, Nordestgaard, Influence of diabetes and hyperglycaemia on infectious disease hospitalisation and outcome, Diabetologia
Bornstein, Rubino, Khunti, Practical recommendations for the management of diabetes in patients with COVID-19, Lancet Diabetes & Endocrinology
Boye, Tokar Erdemir, Zimmerman, Risk factors associated with COVID-19 hospitalization and mortality: a large claims-based analysis among people with type 2 diabetes mellitus in the United States, Diabetes erapy
Dennis, Mateen, Sonabend, Type 2 diabetes and COVID-19-related mortality in the critical care setting: a national cohort study in England, march-july 2020, Diabetes Care
Donoghue, Hsieh, Baronas, A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9, Circulation Research
Farshbafnadi, Kamali, Zonouzi, Sabahi, Dolatshahi et al., Aging & COVID-19 susceptibility, disease severity, and clinical outcomes: the role of entangled risk factors, Experimental Gerontology
Guo, Diabetes is a risk factor for the progression and prognosis of COVID-19, Diabetes/Metabolism Research and Reviews
Hamming, Timens, Bulthuis, Lely, Navis et al., Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis, e Journal of Pathology
Harrell, Evaluating the yield of medical tests, JAMA: e Journal of the American Medical Association
Harrell, Lee, Califf, Pryor, Rosati, Regression modelling strategies for improved prognostic prediction, Statistics in Medicine
Heagerty, Lumley, Pepe, Time-dependent ROC curves for censored survival data and a diagnostic marker, Biometrics
Heagerty, Zheng, Survival model predictive accuracy and ROC curves, Biometrics
Herman, O'keefe, Bell, Schwartz, Insulin therapy increases cardiovascular risk in type 2 diabetes, Progress in Cardiovascular Diseases
Holman, Knighton, Kar, Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study, Lancet Diabetes & Endocrinology
Hu, Risk factors associated with clinical outcomes in 323 COVID-19 hospitalized patients in wuhan, China, Clinical Infectious Diseases
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, e Lancet
Hundal, Krssak, Dufour, Mechanism by which metformin reduces glucose production in type 2 diabetes, Diabetes
Jana, Greenwood, Hansmann, Presence of a SARS-CoV-2 protein enhances amyloid formation of serum amyloid A, e Journal of Physical Chemistry B
Kamyshnyi, Matskevych, Lenchuk, Strilbytska, Storey et al., Metformin to decrease COVID-19 severity and mortality: molecular mechanisms and therapeutic potential, Biomedicine & Pharmacotherapy
Kifle, Woldeyohanis, Demeke, A review on protective roles and potential mechanisms of metformin in diabetic patients diagnosed with COVID-19, Metabolism Open
Li, Zhai, Song, Genome-Wide association study identifies a new locus at 7q21.13 associated with hepatitis B virus-related hepatocellular carcinoma, Clinical Cancer Research
Lindström, Jorfeldt, Tegler, Arnqvist, Hypoglycaemia and cardiac arrhythmias in patients with type 2 diabetes mellitus, Diabetic Medicine
Liu, Chen, Chen, Peng, Lin et al., Vascular and metabolic effects of metformin added to insulin therapy in patients with type 1 diabetes: a systematic review and meta-analysis, Diabetes/metabolism research and reviews
Logette, Lorin, Favreau, A machine-generated view of the role of blood glucose levels in the severity of COVID-19, Frontiers in Public Health
Luk, Yip, Zhang, Glucose-lowering drugs and outcome from COVID-19 among patients with type 2 diabetes mellitus: a population-wide analysis in Hong Kong, BMJ Open
Pieri, Ciotti, Nuccetelli, Serum Amyloid A Protein as a useful biomarker to predict COVID-19 patients severity and prognosis, International Immunopharmacology
Qin, Zhou, Hu, Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in wuhan, China, Clinical Infectious Diseases
Roy, Mazumder, Banik, e association of cardiovascular diseases and diabetes mellitus with COVID-19 (SARS-CoV-2) and their possible mechanisms, SN comprehensive clinical medicine
Sharma, Ray, Sadasivam, Metformin in COVID-19: a possible role beyond diabetes, Diabetes Research and Clinical Practice
Shen, Zhang, Wang, MDM2-Mediated ubiquitination of angiotensin-converting enzyme 2 contributes to the development of pulmonary arterial hypertension, Circulation
Tikellis, Bialkowski, Pete, ACE2 deficiency modifies renoprotection afforded by ACE inhibition in experimental diabetes, Diabetes
Tipnis, Hooper, Hyde, Karran, Christie et al., A human homolog of angiotensin-converting enzyme, Journal of Biological Chemistry
Tripathi, Srivastava, Diabetes mellitus: complications and therapeutics, Medical Science Monitor: International Medical Journal of Experimental and Clinical Research
Wander, Prior glucose-lowering medication use and 30-day outcomes among 64,892 veterans with diabetes and COVID-19, Diabetes Care
Wang, Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, china, JAMA
Wang, Shen, Tao, Elevated glucose level leads to rapid COVID-19 progression and high fatality, BMC Pulmonary Medicine
Weng, Ji, Jia, Standards of care for type 2 diabetes in China, Diabetes
Williamson, Walker, Bhaskaran, Factors associated with COVID-19-related death using Open-SAFELY, Nature
Yeoh, Zuo, Lui, Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19, Gut
Ygesen, Alpert, Jaffe, ird universal definition of myocardial infarction, Journal of the American College of Cardiology
Yip, Chan, Cho, Protein chip array profiling analysis in patients with severe acute respiratory 12 International Journal of Endocrinology syndrome identified serum amyloid a protein as a biomarker potentially useful in monitoring the extent of pneumonia, Clinical Chemistry
Zhang, Dong, Martin, AMP-activated protein kinase phosphorylation of angiotensin-converting enzyme 2 in Endothelium mitigates pulmonary hypertension, American Journal of Respiratory and Critical Care Medicine
Zhang, Huang, Lan, Association between serum amyloid A levels and predicting disase severity in COVID-19 patients: a systematic review and meta-analysis, European Review for Medical and Pharmacological Sciences
Zheng, Ley, Hu, Global aetiology and epidemiology of type 2 diabetes mellitus and its complications, Nature Reviews Endocrinology
Zhou, Yu, Du, Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study, e Lancet
Zhu, Zhang, Wang, A novel coronavirus from patients with pneumonia in China, 2019, New England Journal of Medicine
Zinellu, Paliogiannis, Carru, Mangoni, Serum amyloid A concentrations, COVID-19 severity and mortality: an updated systematic review and meta-analysis, International Journal of Infectious Diseases
Zou, Chen, Zou, Han, Hao et al., Singlecell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection, Frontiers of Medicine
DOI record:
{
"DOI": "10.1155/2022/9322332",
"ISSN": [
"1687-8345",
"1687-8337"
],
"URL": "http://dx.doi.org/10.1155/2022/9322332",
"abstract": "<jats:p>Background. Type 2 diabetes (T2D) as a worldwide chronic disease combined with the COVID-19 pandemic prompts the need for improving the management of hospitalized COVID-19 patients with preexisting T2D to reduce complications and the risk of death. This study aimed to identify clinical factors associated with COVID-19 outcomes specifically targeted at T2D patients and build an individualized risk prediction nomogram for risk stratification and early clinical intervention to reduce mortality. Methods. In this retrospective study, the clinical characteristics of 382 confirmed COVID-19 patients, consisting of 108 with and 274 without preexisting T2D, from January 8 to March 7, 2020, in Tianyou Hospital in Wuhan, China, were collected and analyzed. Univariate and multivariate Cox regression models were performed to identify specific clinical factors associated with mortality of COVID-19 patients with T2D. An individualized risk prediction nomogram was developed and evaluated by discrimination and calibration. Results. Nearly 15% (16/108) of hospitalized COVID-19 patients with T2D died. Twelve risk factors predictive of mortality were identified. Older age (HR = 1.076, 95% CI = 1.014–1.143,<jats:inline-formula><math xmlns=\"http://www.w3.org/1998/Math/MathML\" id=\"M1\"><mi>p</mi><mo>=</mo><mn>0.016</mn></math></jats:inline-formula>), elevated glucose level (HR = 1.153, 95% CI = 1.038–1.28,<jats:inline-formula><math xmlns=\"http://www.w3.org/1998/Math/MathML\" id=\"M2\"><mi>p</mi><mo>=</mo><mn>0.0079</mn></math></jats:inline-formula>), increased serum amyloid A (SAA) (HR = 1.007, 95% CI = 1.001–1.014,<jats:inline-formula><math xmlns=\"http://www.w3.org/1998/Math/MathML\" id=\"M3\"><mi>p</mi><mo>=</mo><mn>0.022</mn></math></jats:inline-formula>), diabetes treatment with only oral diabetes medication (HR = 0.152, 95%CI = 0.032–0.73,<jats:inline-formula><math xmlns=\"http://www.w3.org/1998/Math/MathML\" id=\"M4\"><mi>p</mi><mo>=</mo><mn>0.0036</mn></math></jats:inline-formula>), and oral medication plus insulin (HR = 0.095, 95%CI = 0.019–0.462,<jats:inline-formula><math xmlns=\"http://www.w3.org/1998/Math/MathML\" id=\"M5\"><mi>p</mi><mo>=</mo><mn>0.019</mn></math></jats:inline-formula>) were independent prognostic factors. A nomogram based on these prognostic factors was built for early prediction of 7-day, 14-day, and 21-day survival of diabetes patients. High concordance index (C-index) was achieved, and the calibration curves showed the model had good prediction ability within three weeks of COVID-19 onset. Conclusions. By incorporating specific prognostic factors, this study provided a user-friendly graphical risk prediction tool for clinicians to quickly identify high-risk T2D patients hospitalized for COVID-19.</jats:p>",
"alternative-id": [
"9322332",
"9322332"
],
"author": [
{
"affiliation": [
{
"name": "Department of Quantitative Health Sciences, John A. Burns School of Medicine, University of Hawaii at Manoa, Honolulu, HI, USA"
}
],
"family": "Fu",
"given": "Yuanyuan",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Tianyou Hospital, Affiliated to Wuhan University of Science and Technology, Wuhan, Hubei, China"
}
],
"family": "Hu",
"given": "Ling",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tianyou Hospital, Affiliated to Wuhan University of Science and Technology, Wuhan, Hubei, China"
}
],
"family": "Ren",
"given": "Hong-Wei",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Quantitative Health Sciences, John A. Burns School of Medicine, University of Hawaii at Manoa, Honolulu, HI, USA"
},
{
"name": "Tianyou Hospital, Affiliated to Wuhan University of Science and Technology, Wuhan, Hubei, China"
}
],
"family": "Zuo",
"given": "Yi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Quantitative Health Sciences, John A. Burns School of Medicine, University of Hawaii at Manoa, Honolulu, HI, USA"
}
],
"family": "Chen",
"given": "Shaoqiu",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tianyou Hospital, Affiliated to Wuhan University of Science and Technology, Wuhan, Hubei, China"
}
],
"family": "Zhang",
"given": "Qiu-Shi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tianyou Hospital, Affiliated to Wuhan University of Science and Technology, Wuhan, Hubei, China"
}
],
"family": "Shao",
"given": "Chen",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tianyou Hospital, Affiliated to Wuhan University of Science and Technology, Wuhan, Hubei, China"
}
],
"family": "Ma",
"given": "Yao",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tianyou Hospital, Affiliated to Wuhan University of Science and Technology, Wuhan, Hubei, China"
}
],
"family": "Wu",
"given": "Lin",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tianyou Hospital, Affiliated to Wuhan University of Science and Technology, Wuhan, Hubei, China"
}
],
"family": "Hao",
"given": "Jun-Jie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Tianyou Hospital, Affiliated to Wuhan University of Science and Technology, Wuhan, Hubei, China"
}
],
"family": "Wang",
"given": "Chuan-Zhen",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Cancer Epidemiology Program, University of Hawaii Cancer Center, University of Hawaii at Manoa, Honolulu, HI, USA"
}
],
"family": "Wang",
"given": "Zhanwei",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Pediatrics, John A. Burns School of Medicine, University of Hawaii at Manoa, Honolulu, HI, USA"
}
],
"family": "Yanagihara",
"given": "Richard",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5951-8213",
"affiliation": [
{
"name": "Department of Quantitative Health Sciences, John A. Burns School of Medicine, University of Hawaii at Manoa, Honolulu, HI, USA"
}
],
"authenticated-orcid": true,
"family": "Deng",
"given": "Youping",
"sequence": "additional"
}
],
"container-title": "International Journal of Endocrinology",
"container-title-short": "International Journal of Endocrinology",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
1,
17
]
],
"date-time": "2022-01-17T23:50:10Z",
"timestamp": 1642463410000
},
"deposited": {
"date-parts": [
[
2023,
1,
23
]
],
"date-time": "2023-01-23T08:36:49Z",
"timestamp": 1674463009000
},
"editor": [
{
"affiliation": [],
"family": "Merlotti",
"given": "Daniela",
"sequence": "additional"
}
],
"indexed": {
"date-parts": [
[
2023,
1,
24
]
],
"date-time": "2023-01-24T05:59:08Z",
"timestamp": 1674539948119
},
"is-referenced-by-count": 2,
"issued": {
"date-parts": [
[
2022,
1,
17
]
]
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
17
]
],
"date-time": "2022-01-17T00:00:00Z",
"timestamp": 1642377600000
}
}
],
"link": [
{
"URL": "http://downloads.hindawi.com/journals/ije/2022/9322332.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://downloads.hindawi.com/journals/ije/2022/9322332.xml",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://downloads.hindawi.com/journals/ije/2022/9322332.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "98",
"original-title": [],
"page": "1-13",
"prefix": "10.1155",
"published": {
"date-parts": [
[
2022,
1,
17
]
]
},
"published-print": {
"date-parts": [
[
2022,
1,
17
]
]
},
"publisher": "Hindawi Limited",
"reference": [
{
"DOI": "10.1056/nejmoa2001017",
"doi-asserted-by": "publisher",
"key": "1"
},
{
"DOI": "10.1016/s0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "2"
},
{
"DOI": "10.1016/s2213-8587(20)30152-2",
"doi-asserted-by": "publisher",
"key": "3"
},
{
"DOI": "10.1016/s0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "4"
},
{
"article-title": "Risk factors associated with clinical outcomes in 323 COVID-19 hospitalized patients in wuhan, China",
"author": "L. Hu",
"journal-title": "Clinical Infectious Diseases",
"key": "5",
"volume": "71",
"year": "2020"
},
{
"DOI": "10.1001/jama.2020.1585",
"article-title": "Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, china",
"author": "D. Wang",
"doi-asserted-by": "crossref",
"journal-title": "JAMA",
"key": "6",
"volume": "323",
"year": "2020"
},
{
"article-title": "Diabetes is a risk factor for the progression and prognosis of COVID-19",
"author": "W. Guo",
"journal-title": "Diabetes/Metabolism Research and Reviews",
"key": "7",
"volume": "36",
"year": "2020"
},
{
"DOI": "10.1038/nrendo.2017.151",
"doi-asserted-by": "publisher",
"key": "8"
},
{
"author": "International Diabetes Federation",
"edition": "9th",
"key": "9",
"volume-title": "IDF Diabetes Atlas",
"year": "2019"
},
{
"article-title": "Diabetes mellitus: complications and therapeutics",
"author": "B. K. Tripathi",
"first-page": "RA130",
"issue": "7",
"journal-title": "Medical Science Monitor: International Medical Journal of Experimental and Clinical Research",
"key": "10",
"volume": "12",
"year": "2006"
},
{
"DOI": "10.1007/s42399-020-00376-z",
"doi-asserted-by": "publisher",
"key": "11"
},
{
"DOI": "10.1158/1078-0432.ccr-17-2537",
"doi-asserted-by": "publisher",
"key": "12"
},
{
"key": "13",
"volume-title": "Coronavirus Disease 2019 (COVID-19) Treatment Guidelines",
"year": "2021"
},
{
"DOI": "10.1002/dmrr.2827",
"doi-asserted-by": "publisher",
"key": "14"
},
{
"DOI": "10.1016/j.jacc.2012.08.001",
"doi-asserted-by": "publisher",
"key": "15"
},
{
"DOI": "10.1111/j.0006-341x.2000.00337.x",
"doi-asserted-by": "publisher",
"key": "16"
},
{
"DOI": "10.1111/j.0006-341x.2005.030814.x",
"doi-asserted-by": "publisher",
"key": "17"
},
{
"DOI": "10.1002/sim.4780030207",
"doi-asserted-by": "publisher",
"key": "18"
},
{
"DOI": "10.1001/jama.1982.03320430047030",
"doi-asserted-by": "publisher",
"key": "19"
},
{
"DOI": "10.1016/j.exger.2021.111507",
"doi-asserted-by": "publisher",
"key": "20"
},
{
"DOI": "10.1016/s2213-8587(20)30271-0",
"doi-asserted-by": "publisher",
"key": "21"
},
{
"DOI": "10.1007/s13300-021-01110-1",
"doi-asserted-by": "publisher",
"key": "22"
},
{
"DOI": "10.2337/dc20-1444",
"doi-asserted-by": "publisher",
"key": "23"
},
{
"DOI": "10.1038/s41586-020-2521-4",
"doi-asserted-by": "publisher",
"key": "24"
},
{
"DOI": "10.1186/s12890-021-01413-w",
"doi-asserted-by": "publisher",
"key": "25"
},
{
"DOI": "10.1007/s00125-006-0570-3",
"doi-asserted-by": "publisher",
"key": "26"
},
{
"DOI": "10.3389/fpubh.2021.695139",
"doi-asserted-by": "publisher",
"key": "27"
},
{
"DOI": "10.1074/jbc.m002615200",
"doi-asserted-by": "publisher",
"key": "28"
},
{
"DOI": "10.1161/01.res.87.5.e1",
"doi-asserted-by": "publisher",
"key": "29"
},
{
"DOI": "10.1002/path.1570",
"doi-asserted-by": "publisher",
"key": "30"
},
{
"DOI": "10.1007/s11684-020-0754-0",
"doi-asserted-by": "publisher",
"key": "31"
},
{
"DOI": "10.2337/db10-1205",
"doi-asserted-by": "publisher",
"key": "32"
},
{
"DOI": "10.2337/db07-1212",
"doi-asserted-by": "publisher",
"key": "33"
},
{
"DOI": "10.1016/j.jacc.2005.05.051",
"doi-asserted-by": "publisher",
"key": "34"
},
{
"DOI": "10.1002/dmrr.3334",
"doi-asserted-by": "publisher",
"key": "35"
},
{
"DOI": "10.2337/diabetes.49.12.2063",
"doi-asserted-by": "publisher",
"key": "36"
},
{
"DOI": "10.1164/rccm.201712-2570oc",
"doi-asserted-by": "publisher",
"key": "37"
},
{
"DOI": "10.1161/circulationaha.120.048191",
"doi-asserted-by": "publisher",
"key": "38"
},
{
"DOI": "10.1016/j.diabres.2020.108183",
"doi-asserted-by": "publisher",
"key": "39"
},
{
"DOI": "10.1016/j.metop.2021.100137",
"doi-asserted-by": "publisher",
"key": "40"
},
{
"DOI": "10.1016/j.biopha.2021.112230",
"doi-asserted-by": "publisher",
"key": "41"
},
{
"DOI": "10.1136/gutjnl-2020-323020",
"doi-asserted-by": "publisher",
"key": "42"
},
{
"DOI": "10.1136/bmjopen-2021-052310",
"doi-asserted-by": "publisher",
"key": "43"
},
{
"DOI": "10.1016/j.diabet.2021.101297",
"doi-asserted-by": "publisher",
"key": "44"
},
{
"DOI": "10.1016/j.pcad.2017.09.001",
"doi-asserted-by": "publisher",
"key": "45"
},
{
"DOI": "10.2337/dc21-1351",
"article-title": "Prior glucose-lowering medication use and 30-day outcomes among 64,892 veterans with diabetes and COVID-19",
"author": "P. L. Wander",
"doi-asserted-by": "crossref",
"journal-title": "Diabetes Care",
"key": "46",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1111/j.1464-5491.1992.tb01834.x",
"doi-asserted-by": "publisher",
"key": "47"
},
{
"DOI": "10.3909/ricm0671",
"article-title": "Divergent effects of various diabetes drugs on cardiovascular prognosis",
"author": "D. S. Bell",
"doi-asserted-by": "crossref",
"first-page": "e107",
"issue": "2-4",
"journal-title": "Reviews in Cardiovascular Medicine",
"key": "48",
"volume": "14",
"year": "2013"
},
{
"DOI": "10.1093/cid/ciaa248",
"doi-asserted-by": "publisher",
"key": "49"
},
{
"DOI": "10.1021/acs.jpcb.1c04871",
"doi-asserted-by": "publisher",
"key": "50"
},
{
"DOI": "10.1373/clinchem.2004.031229",
"doi-asserted-by": "publisher",
"key": "51"
},
{
"DOI": "10.1016/j.intimp.2021.107512",
"doi-asserted-by": "publisher",
"key": "52"
},
{
"DOI": "10.1016/j.lfs.2021.119019",
"doi-asserted-by": "publisher",
"key": "53"
},
{
"DOI": "10.26355/eurrev_202107_26255",
"doi-asserted-by": "publisher",
"key": "54"
},
{
"DOI": "10.1016/j.ijid.2021.03.025",
"doi-asserted-by": "publisher",
"key": "55"
}
],
"reference-count": 55,
"references-count": 55,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.hindawi.com/journals/ije/2022/9322332/"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Endocrine and Autonomic Systems",
"Endocrinology",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Prognostic Factors for COVID-19 Hospitalized Patients with Preexisting Type 2 Diabetes",
"type": "journal-article",
"volume": "2022"
}
