Antidiabetic treatment and COVID-19 Outcomes: A population-based cohort study in primary health care in Catalonia during the first wave of the pandemic
et al., Primary Care Diabetes, doi:10.1016/j.pcd.2022.10.001, Oct 2022
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
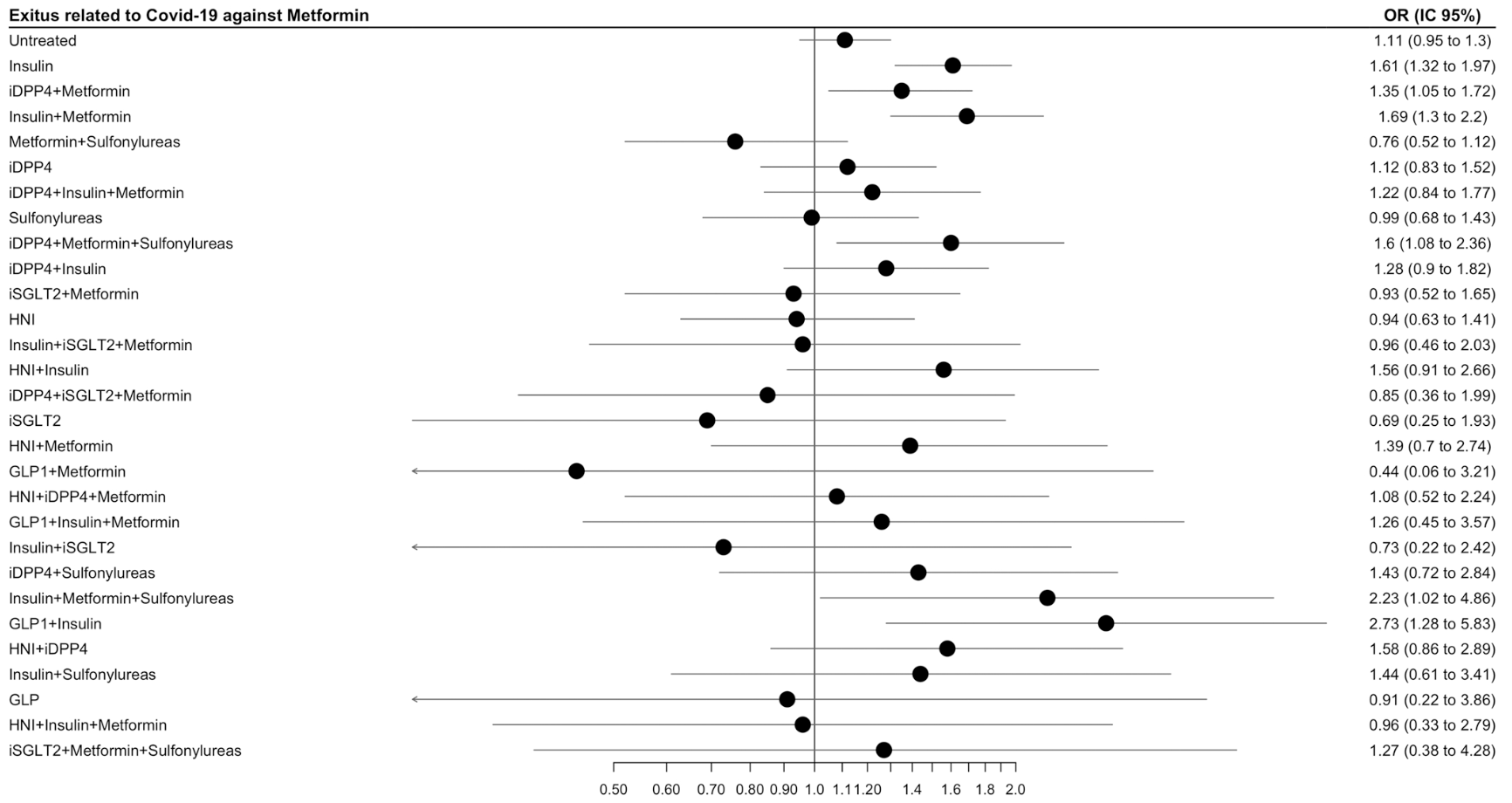
Retrospective 31,006 diabetic COVID-19 patients in Spain, showing lower mortality with metformin treatment, without statistical significance. Authors provide results for metformin compared with untreated patients rather than all non-metformin patients, which may increase confounding due to higher prevalence for treatment of patients with more severe disease.
|
risk of death, 9.9% lower, OR 0.90, p = 0.19, treatment 6,168, control 9,875, inverted to make OR<1 favor treatment, metformin monotherapy vs. untreated, RR approximated with OR.
|
|
risk of death/hospitalization, 8.3% lower, OR 0.92, p = 0.12, treatment 6,168, control 9,875, inverted to make OR<1 favor treatment, metformin monotherapy vs. untreated, RR approximated with OR.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ouchi et al., 4 Oct 2022, retrospective, Spain, peer-reviewed, mean age 71.5, 5 authors, study period March 2020 - June 2020.
Contact: mginer@idiapjgol.info.
Antidiabetic treatment and COVID-19 Outcomes: A population-based cohort study in primary health care in Catalonia during the first wave of the pandemic
Primary Care Diabetes, doi:10.1016/j.pcd.2022.10.001
To analyse if antidiabetic treatment was associated with better COVID-19 outcomes in type 2 diabetic patients, measured by hospital admission and mortality rates as severe outcomes. Methods: Cohort study including COVID-19 patients registered in the Primary Care electronic records, in March-June 2020, comparing exposed to metformin in monotherapy with exposed to any other antidiabetic. Data source: SIDIAP (Information System for Research in Primary Care), which captures clinical information of 5,8 million people from Catalonia, Spain. Results: We included 31,006 diabetic patients infected with COVID-19, 43.7% previously exposed to metformin, 45.5% of them in monotherapy. 16.4% were admitted to hospital and 15.1% died. Users of insulin in monotherapy (OR 1.29, 95% CI 1.11-1.50), combined with metformin (OR 1.38, 1.13-1.69) or IDPP4 alone (OR 1.29, 1.03-1.63) had higher risk of severe outcomes than those in metformin monotherapy. Users of any insulin (OR 1.61, 1.32-1.97) or combined with metformin (OR 1.69, 1.30-2.20) had a higher risk of mortality. Conclusions: Patients receiving metformin monotherapy in our study showed a lower risk of hospitalization and death in comparison to those treated with other frequent antidiabetic agents. We cannot distinguish if better outcomes are related with the antidiabetic therapy or with other factors, such as metabolic control or interventions applied during the hospital admission.
Conflict of interest The authors declare no conflict of interest.
References
Almalki, Qayyum, Irfan, Haider, Glowacz et al., A novel method for COVID-19 diagnosis using artificial intelligence in chest X-ray images, Healthc, doi:10.3390/healthcare9050522
Belančić, Kresović, Troskot Dijan, Glucagon-like peptide-1 receptor agonists in the era of COVID -19: Friend or foe?, Clin. Obes, doi:10.1111/cob.12439
Bornstein, Rubino, Khunti, Mingrone, Hopkins et al., Practical recommendations for the management of diabetes in patients with COVID-19, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30152-2
Catsalut, Servei Català de la Salut, Conjunt mínim bàsic de dades
Chen, Lv, Lin, Arshad, Dai, The association between antidiabetic agents and clinical outcomes of COVID-19 patients with diabetes: a bayesian network meta-analysis, Front. Endocrinol, doi:10.3389/FENDO.2022.895458
Chen, Yang, Cheng, Chen, Peng et al., Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication, Diabetes Care, doi:10.2337/DC20-0660
Drucker, Coronavirus infections and type 2 diabetes-shared pathways with therapeutic implications, Endocr. Rev, doi:10.1210/endrev/bnaa011
Fadini, Morieri, Longato, Avogaro, Prevalence and impact of diabetes among people infected with SARS-CoV-2, J. Endocrinol. Investig, doi:10.1007/s40618-020-01236-2
Kan, Zhang, Han, Xu, Ye et al., Mortality risk of antidiabetic agents for type 2 diabetes with COVID-19: a systematic review and meta-analysis, Front. Endocrinol, doi:10.3389/FENDO.2021.708494/BIBTEX
Katsiki, Ferrannini, Anti-inflammatory properties of antidiabetic drugs: a "promised land" in the COVID-19 era?, J. Diabetes Its Complicat, doi:10.1016/j.jdiacomp.2020.107723
Kieffer, Mc Intosh, Pederson, Degradation of glucose-dependent insulinotropic polypeptide and truncated glucagon-like peptide 1 in vitro and in vivo by dipeptidyl peptidase IV, Endocrinology, doi:10.1210/ENDO.136.8.7628397
Landstra, De Koning, COVID-19 and diabetes: understanding the interrelationship and risks for a severe course, Front. Endocrinol, doi:10.3389/fendo.2021.649525
Li, Zhang, Yang, Lian, Xie et al., The MERS-CoV Receptor DPP4 as a Candidate Binding Target of the SARS-CoV-2 Spike, IScience, doi:10.1016/J.ISCI.2020.101160
Lipsitch, Swerdlow, Finelli, Defining the epidemiology of Covid-19 -studies needed, N. Engl. J. Med, doi:10.1056/NEJMp2002125
Luo, Qiu, Liu, Liu, Zheng et al., Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis, Am. J. Trop. Med. Hyg, doi:10.4269/AJTMH.20-0375
Mcgurnaghan, Robertson, Murray Mscph, Mcmenamin Mbchb, Phd et al., Articles Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland, Www. Thelancet, Com. /Diabetes-Endocrinol, doi:10.1016/S2213-8587(20)30405-8
Nguyen, Ho, Nguyen, Ho, Li et al., Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: a meta-analysis, Metab.: Clin. Exp, doi:10.1016/J.METABOL.2022.155196
Orozco-Beltrán, Merino-Torres, Pérez, Cebrián-Cuenca, Párraga-Martínez et al., Diabetes does not increase the risk of hospitalization due to COVID-19 in patients aged 50 years or older in primary care-APHOSDIAB-COVID-19 multicenter study, J. Clin. Med, doi:10.3390/jcm11082092
Pal, Banerjee, Mukherjee, Bhogal, Kaur et al., Dipeptidyl peptidase-4 inhibitor use and mortality in COVID-19 patients with diabetes mellitus: an updated systematic review and meta-analysis, 204201882199648, Ther. Adv. Endocrinol. Metab, doi:10.1177/2042018821996482
Patoulias, Doumas, Dipeptidyl peptidase-4 inhibitors and COVID-19-related deaths among patients with type 2 diabetes mellitus: a meta-analysis of observational studies, Endocrinol. Metab, doi:10.3803/ENM.2021.1048
Qi, Qian, Zhang, Zhang, Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses, Biochem. Biophys. Res. Commun, doi:10.1016/j.bbrc.2020.03.044
Qu, Zheng, Wang, Li, Liu et al., The potential effects of clinical antidiabetic agents on SARS-CoV-2, J. Diabetes, doi:10.1111/1753-0407.13135
Recalde, Data resource profile: the information system for research in primary care (SIDIAP), Int. J. Epidemiol
Recalde, Rodríguez, Burn, Far, García et al., Data resource profile: the information system for research in primary care (SIDIAP, Int. J. Epidemiol, doi:10.1093/ije/dyac068
Reynolds, Adhikari, Pulgarin, Troxel, Iturrate et al., Renin-Angiotensin-Aldosterone system inhibitors and risk of Covid-19, N. Engl. J. Med, doi:10.1056/NEJMoa2008975
Roberts, Pritchard, Treweeke, Rossi, Brace et al., Why Is COVID-19 more severe in patients with diabetes? the role of angiotensin-converting enzyme 2, endothelial dysfunction and the immunoinflammatory system, Front. Cardiovasc. Med, doi:10.3389/fcvm.2020.629933
Samuel, Varghese, Büsselberg, Therapeutic potential of metformin in COVID-19: reasoning for its protective role, Trends Microbiol, doi:10.1016/j.tim.2021.03.004
Scheen, Metformin and COVID-19: from cellular mechanisms to reduced mortality, Diabetes Metab, doi:10.1016/j.diabet.2020.07.006
Solerte, Antonio, Galli, Fiorina, Dipeptidyl peptidase-4 (DPP4) inhibition in COVID-19, Acta Diabetol, doi:10.1007/s00592-020-01539-z
Who, Int. Stat. Classif. Dis. Relat. Health Probl. 10th Revis
Yan, Yang, Wang, Ren, Zhang et al., Clinical characteristics and outcomes of patients with severe covid-19 with diabetes, BMJ Open Diabetes Res. Care, doi:10.1136/BMJDRC-2020-001343
Yang, Cai, Zhangid, DPP-4 inhibitors may improve the mortality of coronavirus disease 2019: a meta-analysis, PLoS One, doi:10.1371/journal.pone.0251916
Yang, Sun, Zhang, Zhang, The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus, Diabetes Res. Clin. Pract, doi:10.1016/j.diabres.2021.108977
Yu, Li, Sun, Wang, Insulin treatment is associated with increased mortality in patients with COVID-19 and Type 2 diabetes, 65-77.e2, Cell Metab, doi:10.1016/J.CMET.2020.11.014
DOI record:
{
"DOI": "10.1016/j.pcd.2022.10.001",
"ISSN": [
"1751-9918"
],
"URL": "http://dx.doi.org/10.1016/j.pcd.2022.10.001",
"alternative-id": [
"S175199182200167X"
],
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "Antidiabetic treatment and COVID-19 Outcomes: A population-based cohort study in primary health care in Catalonia during the first wave of the pandemic"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Primary Care Diabetes"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.pcd.2022.10.001"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2022 Primary Care Diabetes Europe. Published by Elsevier Ltd. All rights reserved."
}
],
"author": [
{
"affiliation": [],
"family": "Ouchi",
"given": "Dan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Vilaplana-Carnerero",
"given": "Carles",
"sequence": "additional"
},
{
"affiliation": [],
"family": "de Dios",
"given": "Vanessa",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Giner-Soriano",
"given": "Maria",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Morros",
"given": "Rosa",
"sequence": "additional"
}
],
"container-title": "Primary Care Diabetes",
"container-title-short": "Primary Care Diabetes",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"primary-care-diabetes.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2022,
10,
4
]
],
"date-time": "2022-10-04T17:07:26Z",
"timestamp": 1664903246000
},
"deposited": {
"date-parts": [
[
2022,
10,
19
]
],
"date-time": "2022-10-19T23:10:11Z",
"timestamp": 1666221011000
},
"indexed": {
"date-parts": [
[
2022,
10,
20
]
],
"date-time": "2022-10-20T05:00:32Z",
"timestamp": 1666242032657
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
10
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
10,
1
]
],
"date-time": "2022-10-01T00:00:00Z",
"timestamp": 1664582400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S175199182200167X?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S175199182200167X?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
10
]
]
},
"published-print": {
"date-parts": [
[
2022,
10
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"key": "10.1016/j.pcd.2022.10.001_bib1",
"unstructured": "European Centre for Disease Prevention and Control (ECDC), COVID-19 situation updates, 2022."
},
{
"key": "10.1016/j.pcd.2022.10.001_bib2",
"unstructured": "World health organization (WHO), Coronavirus disease 2019, 2022."
},
{
"DOI": "10.1056/NEJMp2002125",
"article-title": "Defining the epidemiology of Covid-19 — studies needed",
"author": "Lipsitch",
"doi-asserted-by": "crossref",
"first-page": "1194",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.pcd.2022.10.001_bib3",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/S2213-8587(20)30152-2",
"article-title": "Practical recommendations for the management of diabetes in patients with COVID-19",
"author": "Bornstein",
"doi-asserted-by": "crossref",
"first-page": "546",
"journal-title": "Lancet Diabetes Endocrinol.",
"key": "10.1016/j.pcd.2022.10.001_bib4",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1016/j.jdiacomp.2020.107723",
"article-title": "Anti-inflammatory properties of antidiabetic drugs: a “promised land” in the COVID-19 era?",
"author": "Katsiki",
"doi-asserted-by": "crossref",
"journal-title": "J. Diabetes Its Complicat.",
"key": "10.1016/j.pcd.2022.10.001_bib5",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.3389/fcvm.2020.629933",
"article-title": "Why Is COVID-19 more severe in patients with diabetes? the role of angiotensin-converting enzyme 2, endothelial dysfunction and the immunoinflammatory system",
"author": "Roberts",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Front. Cardiovasc. Med.",
"key": "10.1016/j.pcd.2022.10.001_bib6",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2008975",
"article-title": "Renin–Angiotensin–Aldosterone system inhibitors and risk of Covid-19",
"author": "Reynolds",
"doi-asserted-by": "crossref",
"first-page": "2441",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.pcd.2022.10.001_bib7",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/j.isci.2020.101400",
"article-title": "The MERS-CoV Receptor DPP4 as a Candidate Binding Target of the SARS-CoV-2 Spike",
"author": "Li",
"doi-asserted-by": "crossref",
"journal-title": "IScience",
"key": "10.1016/j.pcd.2022.10.001_bib8",
"volume": "23",
"year": "2020"
},
{
"DOI": "10.1177/2042018821996482",
"article-title": "Dipeptidyl peptidase-4 inhibitor use and mortality in COVID-19 patients with diabetes mellitus: an updated systematic review and meta-analysis",
"author": "Pal",
"doi-asserted-by": "crossref",
"journal-title": "Ther. Adv. Endocrinol. Metab.",
"key": "10.1016/j.pcd.2022.10.001_bib9",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.bbrc.2020.03.044",
"article-title": "Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses",
"author": "Qi",
"doi-asserted-by": "crossref",
"first-page": "135",
"journal-title": "Biochem. Biophys. Res. Commun.",
"key": "10.1016/j.pcd.2022.10.001_bib10",
"volume": "526",
"year": "2020"
},
{
"DOI": "10.1210/endo.136.8.7628397",
"article-title": "Degradation of glucose-dependent insulinotropic polypeptide and truncated glucagon-like peptide 1 in vitro and in vivo by dipeptidyl peptidase IV",
"author": "Kieffer",
"doi-asserted-by": "crossref",
"first-page": "3585",
"journal-title": "Endocrinology",
"key": "10.1016/j.pcd.2022.10.001_bib11",
"volume": "136",
"year": "1995"
},
{
"DOI": "10.1007/s00592-020-01539-z",
"article-title": "Dipeptidyl peptidase-4 (DPP4) inhibition in COVID-19",
"author": "Solerte",
"doi-asserted-by": "crossref",
"first-page": "779",
"journal-title": "Acta Diabetol.",
"key": "10.1016/j.pcd.2022.10.001_bib12",
"volume": "57",
"year": "2020"
},
{
"DOI": "10.1016/j.diabet.2020.07.006",
"article-title": "Metformin and COVID-19: from cellular mechanisms to reduced mortality",
"author": "Scheen",
"doi-asserted-by": "crossref",
"first-page": "423",
"journal-title": "Diabetes Metab.",
"key": "10.1016/j.pcd.2022.10.001_bib13",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.1016/j.tim.2021.03.004",
"article-title": "Therapeutic potential of metformin in COVID-19: reasoning for its protective role",
"author": "Samuel",
"doi-asserted-by": "crossref",
"first-page": "894",
"journal-title": "Trends Microbiol.",
"key": "10.1016/j.pcd.2022.10.001_bib14",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.4269/ajtmh.20-0375",
"article-title": "Metformin treatment was associated with decreased mortality in COVID-19 patients with diabetes in a retrospective analysis",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "69",
"journal-title": "Am. J. Trop. Med. Hyg.",
"key": "10.1016/j.pcd.2022.10.001_bib15",
"volume": "103",
"year": "2020"
},
{
"DOI": "10.1111/1753-0407.13135",
"article-title": "The potential effects of clinical antidiabetic agents on SARS‐CoV‐2",
"author": "Qu",
"doi-asserted-by": "crossref",
"first-page": "243",
"journal-title": "J. Diabetes",
"key": "10.1016/j.pcd.2022.10.001_bib16",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1111/cob.12439",
"article-title": "Glucagon‐like peptide‐1 receptor agonists in the era of COVID ‐19: Friend or foe?",
"author": "Belančić",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Clin. Obes.",
"key": "10.1016/j.pcd.2022.10.001_bib17",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1210/endrev/bnaa011",
"article-title": "Coronavirus infections and type 2 diabetes—shared pathways with therapeutic implications",
"author": "Drucker",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Endocr. Rev.",
"key": "10.1016/j.pcd.2022.10.001_bib18",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.3389/fendo.2021.649525",
"article-title": "COVID-19 and diabetes: understanding the interrelationship and risks for a severe course",
"author": "Landstra",
"doi-asserted-by": "crossref",
"journal-title": "Front. Endocrinol.",
"key": "10.1016/j.pcd.2022.10.001_bib19",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1136/bmjdrc-2020-001343",
"article-title": "Clinical characteristics and outcomes of patients with severe covid-19 with diabetes",
"author": "Yan",
"doi-asserted-by": "crossref",
"journal-title": "BMJ Open Diabetes Res. Care.",
"key": "10.1016/j.pcd.2022.10.001_bib20",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1007/s40618-020-01236-2",
"article-title": "Prevalence and impact of diabetes among people infected with SARS-CoV-2",
"author": "Fadini",
"doi-asserted-by": "crossref",
"first-page": "867",
"journal-title": "J. Endocrinol. Investig.",
"key": "10.1016/j.pcd.2022.10.001_bib21",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1093/ije/dyac068",
"article-title": "Data resource profile: the information system for research in primary care (SIDIAP)",
"author": "Recalde",
"doi-asserted-by": "crossref",
"journal-title": "Int. J. Epidemiol.",
"key": "10.1016/j.pcd.2022.10.001_bib23",
"year": "2022"
},
{
"article-title": "Data resource profile: the information system for research in primary care (SIDIAP",
"author": "Recalde",
"first-page": "1",
"journal-title": "Int. J. Epidemiol.",
"key": "10.1016/j.pcd.2022.10.001_bib24",
"year": "2022"
},
{
"author": "WHO, ICD-10 Version: 2019",
"journal-title": "Int. Stat. Classif. Dis. Relat. Health Probl. 10th Revis.",
"key": "10.1016/j.pcd.2022.10.001_bib25",
"year": "2019"
},
{
"key": "10.1016/j.pcd.2022.10.001_bib26",
"unstructured": "WHO Collaborating Centre for Drug Statistics Methodology, ATC/DDD Index 2022, (2022). https://www.whocc.no/atc_ddd_index/."
},
{
"key": "10.1016/j.pcd.2022.10.001_bib27",
"unstructured": "CatSalut. Servei Català de la Salut, Conjunt mínim bàsic de dades (CMBD), (2022). http://catsalut.gencat.cat/ca/proveidors-professionals/registres-catalegs/registres/cmbd/."
},
{
"key": "10.1016/j.pcd.2022.10.001_bib28",
"unstructured": "Catalan Agency for Health Quality and Evaluation (AQuAS), Updated SARS-CoV-2 data, (2022). https://aquas.gencat.cat/ca/actualitat/ultimes-dades-coronavirus/index.html#googtrans(ca%7Cen)."
},
{
"key": "10.1016/j.pcd.2022.10.001_bib29",
"unstructured": "Departament de Salut Generalitat de Catalunya, COVID Data, (2022). https://dadescovid.cat/?lang=eng."
},
{
"DOI": "10.3390/jcm11082092",
"article-title": "Diabetes does not increase the risk of hospitalization due to COVID-19 in patients aged 50 years or older in primary care—APHOSDIAB—COVID-19 multicenter study",
"author": "Orozco-Beltrán",
"doi-asserted-by": "crossref",
"journal-title": "J. Clin. Med.",
"key": "10.1016/j.pcd.2022.10.001_bib30",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/j.diabres.2021.108977",
"article-title": "The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus",
"author": "Yang",
"doi-asserted-by": "crossref",
"journal-title": "Diabetes Res. Clin. Pract.",
"key": "10.1016/j.pcd.2022.10.001_bib31",
"volume": "178",
"year": "2021"
},
{
"article-title": "The association between antidiabetic agents and clinical outcomes of COVID-19 patients with diabetes: a bayesian network meta-analysis",
"author": "Chen",
"first-page": "926",
"journal-title": "Front. Endocrinol.",
"key": "10.1016/j.pcd.2022.10.001_bib32",
"volume": "0",
"year": "2022"
},
{
"DOI": "10.1016/j.metabol.2022.155196",
"article-title": "Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: a meta-analysis",
"author": "Nguyen",
"doi-asserted-by": "crossref",
"journal-title": "Metab.: Clin. Exp.",
"key": "10.1016/j.pcd.2022.10.001_bib33",
"volume": "131",
"year": "2022"
},
{
"DOI": "10.3389/fendo.2021.708494",
"article-title": "Mortality risk of antidiabetic agents for type 2 diabetes with COVID-19: a systematic review and meta-analysis",
"author": "Kan",
"doi-asserted-by": "crossref",
"first-page": "1158",
"journal-title": "Front. Endocrinol.",
"key": "10.1016/j.pcd.2022.10.001_bib34",
"volume": "12",
"year": "2021"
},
{
"article-title": "DPP-4 inhibitors may improve the mortality of coronavirus disease 2019: a meta-analysis",
"author": "Yang",
"journal-title": "PLoS One",
"key": "10.1016/j.pcd.2022.10.001_bib35",
"year": "2021"
},
{
"DOI": "10.3803/EnM.2021.1048",
"article-title": "Dipeptidyl peptidase-4 inhibitors and COVID-19-related deaths among patients with type 2 diabetes mellitus: a meta-analysis of observational studies",
"author": "Patoulias",
"doi-asserted-by": "crossref",
"first-page": "904",
"journal-title": "Endocrinol. Metab.",
"key": "10.1016/j.pcd.2022.10.001_bib36",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.2337/dc20-0660",
"article-title": "Clinical characteristics and outcomes of patients with diabetes and COVID-19 in association with glucose-lowering medication",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "1399",
"journal-title": "Diabetes Care",
"key": "10.1016/j.pcd.2022.10.001_bib37",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1016/j.cmet.2020.11.014",
"article-title": "Insulin treatment is associated with increased mortality in patients with COVID-19 and Type 2 diabetes",
"author": "Yu",
"doi-asserted-by": "crossref",
"journal-title": "Cell Metab.",
"key": "10.1016/j.pcd.2022.10.001_bib38",
"volume": "33",
"year": "2021"
},
{
"article-title": "Articles Risks of and risk factors for COVID-19 disease in people with diabetes: a cohort study of the total population of Scotland",
"author": "Mcgurnaghan",
"first-page": "82",
"journal-title": "Www. Thelancet. Com. /Diabetes-Endocrinol.",
"key": "10.1016/j.pcd.2022.10.001_bib39",
"volume": "9",
"year": "2021"
},
{
"article-title": "A novel method for COVID-19 diagnosis using artificial intelligence in chest X-ray images",
"author": "Almalki",
"first-page": "1",
"journal-title": "Healthc. (Basel)",
"key": "10.1016/j.pcd.2022.10.001_bib40",
"volume": "9",
"year": "2021"
}
],
"reference-count": 39,
"references-count": 39,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S175199182200167X"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Nutrition and Dietetics",
"Endocrinology, Diabetes and Metabolism",
"Internal Medicine",
"Family Practice"
],
"subtitle": [],
"title": "Antidiabetic treatment and COVID-19 Outcomes: A population-based cohort study in primary health care in Catalonia during the first wave of the pandemic",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy"
}
