Favipiravir and Ivermectin Showed in Vitro Synergistic Antiviral Activity against SARS-CoV-2
et al., Research Square, doi:10.21203/rs.3.rs-941811/v1, Oct 2021
Ivermectin for COVID-19
4th treatment shown to reduce risk in
August 2020, now with p < 0.00000000001 from 106 studies, recognized in 24 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
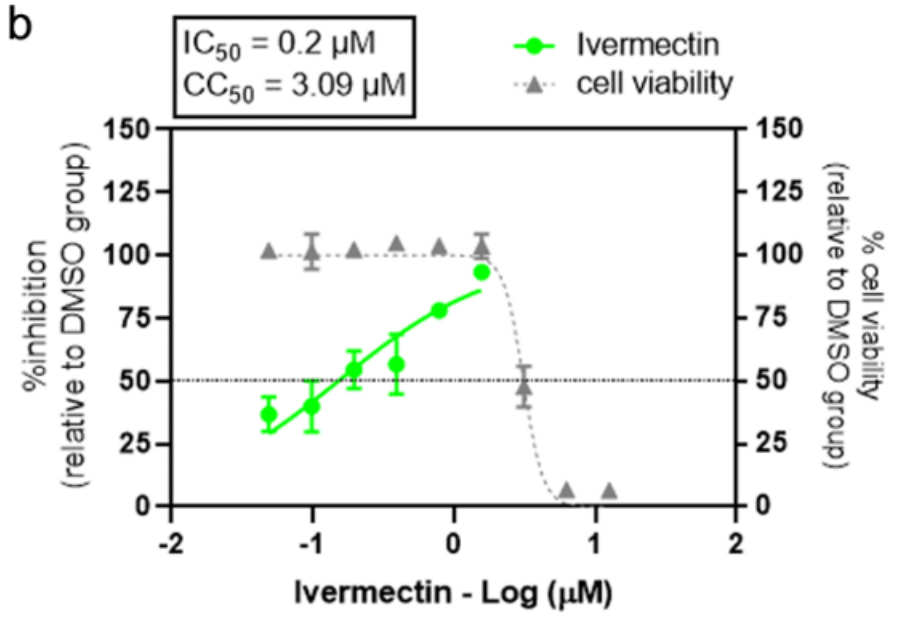
In vitro study showing a strong synergistic effect of ivermectin and favipiravir. Combining multiple antiviral drugs with different mechanisms of action helps to minimize drug resistance and toxicity.
For ivermectin alone, IC50 for Calu-3 was 0.2µM, supporting in vivo efficacy at 0.6 mg/kg.
74 preclinical studies support the efficacy of ivermectin for COVID-19:
Ivermectin, better known for antiparasitic activity, is a broad spectrum antiviral with activity against many viruses including H7N771, Dengue37,72,73 , HIV-173, Simian virus 4074, Zika37,75,76 , West Nile76, Yellow Fever77,78, Japanese encephalitis77, Chikungunya78, Semliki Forest virus78, Human papillomavirus57, Epstein-Barr57, BK Polyomavirus79, and Sindbis virus78.
Ivermectin inhibits importin-α/β-dependent nuclear import of viral proteins71,73,74,80 , shows spike-ACE2 disruption at 1nM with microfluidic diffusional sizing38, binds to glycan sites on the SARS-CoV-2 spike protein preventing interaction with blood and epithelial cells and inhibiting hemagglutination41,81, shows dose-dependent inhibition of wildtype and omicron variants36, exhibits dose-dependent inhibition of lung injury61,66, may inhibit SARS-CoV-2 via IMPase inhibition37, may inhibit SARS-CoV-2 induced formation of fibrin clots resistant to degradation9, inhibits SARS-CoV-2 3CLpro54, may inhibit SARS-CoV-2 RdRp activity28, may minimize viral myocarditis by inhibiting NF-κB/p65-mediated inflammation in macrophages60, may be beneficial for COVID-19 ARDS by blocking GSDMD and NET formation82, may interfere with SARS-CoV-2's immune evasion via ORF8 binding4, may inhibit SARS-CoV-2 by disrupting CD147 interaction83-86, may inhibit SARS-CoV-2 attachment to lipid rafts via spike NTD binding2, shows protection against inflammation, cytokine storm, and mortality in an LPS mouse model sharing key pathological features of severe COVID-1959,87, may be beneficial in severe COVID-19 by binding IGF1 to inhibit the promotion of inflammation, fibrosis, and cell proliferation that leads to lung damage8, may minimize SARS-CoV-2 induced cardiac damage40,48, may counter immune evasion by inhibiting NSP15-TBK1/KPNA1 interaction and restoring IRF3 activation88, may disrupt SARS-CoV-2 N and ORF6 protein nuclear transport and their suppression of host interferon responses1, reduces TAZ/YAP nuclear import, relieving SARS-CoV-2-driven suppression of IRF3 and NF-κB antiviral pathways35, increases Bifidobacteria which play a key role in the immune system89, has immunomodulatory51 and anti-inflammatory70,90 properties, and has an extensive and very positive safety profile91.
1.
Gayozo et al., Binding affinities analysis of ivermectin, nucleocapsid and ORF6 proteins of SARS-CoV-2 to human importins α isoforms: A computational approach, Biotecnia, doi:10.18633/biotecnia.v27.2485.
2.
Lefebvre et al., Characterization and Fluctuations of an Ivermectin Binding Site at the Lipid Raft Interface of the N-Terminal Domain (NTD) of the Spike Protein of SARS-CoV-2 Variants, Viruses, doi:10.3390/v16121836.
3.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
4.
Bagheri-Far et al., Non-spike protein inhibition of SARS-CoV-2 by natural products through the key mediator protein ORF8, Molecular Biology Research Communications, doi:10.22099/mbrc.2024.50245.2001.
5.
de Oliveira Só et al., In Silico Comparative Analysis of Ivermectin and Nirmatrelvir Inhibitors Interacting with the SARS-CoV-2 Main Protease, Preprints, doi:10.20944/preprints202404.1825.v1.
6.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
7.
Oranu et al., Validation of the binding affinities and stabilities of ivermectin and moxidectin against SARS-CoV-2 receptors using molecular docking and molecular dynamics simulation, GSC Biological and Pharmaceutical Sciences, doi:10.30574/gscbps.2024.26.1.0030.
8.
Zhao et al., Identification of the shared gene signatures between pulmonary fibrosis and pulmonary hypertension using bioinformatics analysis, Frontiers in Immunology, doi:10.3389/fimmu.2023.1197752.
9.
Vottero et al., Computational Prediction of the Interaction of Ivermectin with Fibrinogen, Molecular Sciences, doi:10.3390/ijms241411449.
10.
Chellasamy et al., Docking and molecular dynamics studies of human ezrin protein with a modelled SARS-CoV-2 endodomain and their interaction with potential invasion inhibitors, Journal of King Saud University - Science, doi:10.1016/j.jksus.2022.102277.
11.
Umar et al., Inhibitory potentials of ivermectin, nafamostat, and camostat on spike protein and some nonstructural proteins of SARS-CoV-2: Virtual screening approach, Jurnal Teknologi Laboratorium, doi:10.29238/teknolabjournal.v11i1.344.
12.
Alvarado et al., Interaction of the New Inhibitor Paxlovid (PF-07321332) and Ivermectin With the Monomer of the Main Protease SARS-CoV-2: A Volumetric Study Based on Molecular Dynamics, Elastic Networks, Classical Thermodynamics and SPT, Computational Biology and Chemistry, doi:10.1016/j.compbiolchem.2022.107692.
13.
Aminpour et al., In Silico Analysis of the Multi-Targeted Mode of Action of Ivermectin and Related Compounds, Computation, doi:10.3390/computation10040051.
14.
Parvez et al., Insights from a computational analysis of the SARS-CoV-2 Omicron variant: Host–pathogen interaction, pathogenicity, and possible drug therapeutics, Immunity, Inflammation and Disease, doi:10.1002/iid3.639.
15.
Francés-Monerris et al., Microscopic interactions between ivermectin and key human and viral proteins involved in SARS-CoV-2 infection, Physical Chemistry Chemical Physics, doi:10.1039/D1CP02967C.
16.
González-Paz et al., Comparative study of the interaction of ivermectin with proteins of interest associated with SARS-CoV-2: A computational and biophysical approach, Biophysical Chemistry, doi:10.1016/j.bpc.2021.106677.
17.
González-Paz (B) et al., Structural Deformability Induced in Proteins of Potential Interest Associated with COVID-19 by binding of Homologues present in Ivermectin: Comparative Study Based in Elastic Networks Models, Journal of Molecular Liquids, doi:10.1016/j.molliq.2021.117284.
18.
Rana et al., A Computational Study of Ivermectin and Doxycycline Combination Drug Against SARS-CoV-2 Infection, Research Square, doi:10.21203/rs.3.rs-755838/v1.
19.
Muthusamy et al., Virtual Screening Reveals Potential Anti-Parasitic Drugs Inhibiting the Receptor Binding Domain of SARS-CoV-2 Spike protein, Journal of Virology & Antiviral Research, www.scitechnol.com/abstract/virtual-screening-reveals-potential-antiparasitic-drugs-inhibiting-the-receptor-binding-domain-of-sarscov2-spike-protein-16398.html.
20.
Qureshi et al., Mechanistic insights into the inhibitory activity of FDA approved ivermectin against SARS-CoV-2: old drug with new implications, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1906750.
21.
Schöning et al., Highly-transmissible Variants of SARS-CoV-2 May Be More Susceptible to Drug Therapy Than Wild Type Strains, Research Square, doi:10.21203/rs.3.rs-379291/v1.
22.
Bello et al., Elucidation of the inhibitory activity of ivermectin with host nuclear importin α and several SARS-CoV-2 targets, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1911857.
23.
Udofia et al., In silico studies of selected multi-drug targeting against 3CLpro and nsp12 RNA-dependent RNA-polymerase proteins of SARS-CoV-2 and SARS-CoV, Network Modeling Analysis in Health Informatics and Bioinformatics, doi:10.1007/s13721-021-00299-2.
24.
Choudhury et al., Exploring the binding efficacy of ivermectin against the key proteins of SARS-CoV-2 pathogenesis: an in silico approach, Future Medicine, doi:10.2217/fvl-2020-0342.
25.
Kern et al., Modeling of SARS-CoV-2 Treatment Effects for Informed Drug Repurposing, Frontiers in Pharmacology, doi:10.3389/fphar.2021.625678.
26.
Saha et al., The Binding mechanism of ivermectin and levosalbutamol with spike protein of SARS-CoV-2, Structural Chemistry, doi:10.1007/s11224-021-01776-0.
27.
Eweas et al., Molecular Docking Reveals Ivermectin and Remdesivir as Potential Repurposed Drugs Against SARS-CoV-2, Frontiers in Microbiology, doi:10.3389/fmicb.2020.592908.
28.
Parvez (B) et al., Prediction of potential inhibitors for RNA-dependent RNA polymerase of SARS-CoV-2 using comprehensive drug repurposing and molecular docking approach, International Journal of Biological Macromolecules, doi:10.1016/j.ijbiomac.2020.09.098.
29.
Francés-Monerris (B) et al., Has Ivermectin Virus-Directed Effects against SARS-CoV-2? Rationalizing the Action of a Potential Multitarget Antiviral Agent, ChemRxiv, doi:10.26434/chemrxiv.12782258.v1.
30.
Kalhor et al., Repurposing of the approved small molecule drugs in order to inhibit SARS-CoV-2 S protein and human ACE2 interaction through virtual screening approaches, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2020.1824816.
31.
Swargiary, A., Ivermectin as a promising RNA-dependent RNA polymerase inhibitor and a therapeutic drug against SARS-CoV2: Evidence from in silico studies, Research Square, doi:10.21203/rs.3.rs-73308/v1.
32.
Maurya, D., A Combination of Ivermectin and Doxycycline Possibly Blocks the Viral Entry and Modulate the Innate Immune Response in COVID-19 Patients, American Chemical Society (ACS), doi:10.26434/chemrxiv.12630539.v1.
33.
Lehrer et al., Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2, In Vivo, 34:5, 3023-3026, doi:10.21873/invivo.12134.
34.
Suravajhala et al., Comparative Docking Studies on Curcumin with COVID-19 Proteins, Preprints, doi:10.20944/preprints202005.0439.v3.
35.
Kofler et al., M-Motif, a potential non-conventional NLS in YAP/TAZ and other cellular and viral proteins that inhibits classic protein import, iScience, doi:10.1016/j.isci.2025.112105.
36.
Shahin et al., The selective effect of Ivermectin on different human coronaviruses; in-vitro study, Research Square, doi:10.21203/rs.3.rs-4180797/v1.
37.
Jitobaom et al., Identification of inositol monophosphatase as a broad‐spectrum antiviral target of ivermectin, Journal of Medical Virology, doi:10.1002/jmv.29552.
38.
Fauquet et al., Microfluidic Diffusion Sizing Applied to the Study of Natural Products and Extracts That Modulate the SARS-CoV-2 Spike RBD/ACE2 Interaction, Molecules, doi:10.3390/molecules28248072.
39.
García-Aguilar et al., In Vitro Analysis of SARS-CoV-2 Spike Protein and Ivermectin Interaction, International Journal of Molecular Sciences, doi:10.3390/ijms242216392.
40.
Liu et al., SARS-CoV-2 viral genes Nsp6, Nsp8, and M compromise cellular ATP levels to impair survival and function of human pluripotent stem cell-derived cardiomyocytes, Stem Cell Research & Therapy, doi:10.1186/s13287-023-03485-3.
41.
Boschi et al., SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects, bioRxiv, doi:10.1101/2022.11.24.517882.
42.
De Forni et al., Synergistic drug combinations designed to fully suppress SARS-CoV-2 in the lung of COVID-19 patients, PLoS ONE, doi:10.1371/journal.pone.0276751.
43.
Saha (B) et al., Manipulation of Spray-Drying Conditions to Develop an Inhalable Ivermectin Dry Powder, Pharmaceutics, doi:10.3390/pharmaceutics14071432.
44.
Jitobaom (B) et al., Synergistic anti-SARS-CoV-2 activity of repurposed anti-parasitic drug combinations, BMC Pharmacology and Toxicology, doi:10.1186/s40360-022-00580-8.
45.
Croci et al., Liposomal Systems as Nanocarriers for the Antiviral Agent Ivermectin, International Journal of Biomaterials, doi:10.1155/2016/8043983.
46.
Zheng et al., Red blood cell-hitchhiking mediated pulmonary delivery of ivermectin: Effects of nanoparticle properties, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121719.
47.
Delandre et al., Antiviral Activity of Repurposing Ivermectin against a Panel of 30 Clinical SARS-CoV-2 Strains Belonging to 14 Variants, Pharmaceuticals, doi:10.3390/ph15040445.
48.
Liu (B) et al., Genome-wide analyses reveal the detrimental impacts of SARS-CoV-2 viral gene Orf9c on human pluripotent stem cell-derived cardiomyocytes, Stem Cell Reports, doi:10.1016/j.stemcr.2022.01.014.
49.
Segatori et al., Effect of Ivermectin and Atorvastatin on Nuclear Localization of Importin Alpha and Drug Target Expression Profiling in Host Cells from Nasopharyngeal Swabs of SARS-CoV-2- Positive Patients, Viruses, doi:10.3390/v13102084.
50.
Jitobaom (C) et al., Favipiravir and Ivermectin Showed in Vitro Synergistic Antiviral Activity against SARS-CoV-2, Research Square, doi:10.21203/rs.3.rs-941811/v1.
51.
Munson et al., Niclosamide and ivermectin modulate caspase-1 activity and proinflammatory cytokine secretion in a monocytic cell line, British Society For Nanomedicine Early Career Researcher Summer Meeting, 2021, web.archive.org/web/20230401070026/https://michealmunson.github.io/COVID.pdf.
52.
Mountain Valley MD, Mountain Valley MD Receives Successful Results From BSL-4 COVID-19 Clearance Trial on Three Variants Tested With Ivectosol™, 5/18, www.globenewswire.com/en/news-release/2021/05/18/2231755/0/en/Mountain-Valley-MD-Receives-Successful-Results-From-BSL-4-COVID-19-Clearance-Trial-on-Three-Variants-Tested-With-Ivectosol.html.
53.
Yesilbag et al., Ivermectin also inhibits the replication of bovine respiratory viruses (BRSV, BPIV-3, BoHV-1, BCoV and BVDV) in vitro, Virus Research, doi:10.1016/j.virusres.2021.198384.
54.
Mody et al., Identification of 3-chymotrypsin like protease (3CLPro) inhibitors as potential anti-SARS-CoV-2 agents, Communications Biology, doi:10.1038/s42003-020-01577-x.
55.
Jeffreys et al., Remdesivir-ivermectin combination displays synergistic interaction with improved in vitro activity against SARS-CoV-2, International Journal of Antimicrobial Agents, doi:10.1016/j.ijantimicag.2022.106542.
56.
Surnar et al., Clinically Approved Antiviral Drug in an Orally Administrable Nanoparticle for COVID-19, ACS Pharmacol. Transl. Sci., doi:10.1021/acsptsci.0c00179.
57.
Li et al., Quantitative proteomics reveals a broad-spectrum antiviral property of ivermectin, benefiting for COVID-19 treatment, J. Cellular Physiology, doi:10.1002/jcp.30055.
58.
Caly et al., The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Research, doi:10.1016/j.antiviral.2020.104787.
59.
Zhang et al., Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice, Inflammation Research, doi:10.1007/s00011-008-8007-8.
60.
Gao et al., Ivermectin ameliorates acute myocarditis via the inhibition of importin-mediated nuclear translocation of NF-κB/p65, International Immunopharmacology, doi:10.1016/j.intimp.2024.112073.
61.
Abd-Elmawla et al., Suppression of NLRP3 inflammasome by ivermectin ameliorates bleomycin-induced pulmonary fibrosis, Journal of Zhejiang University-SCIENCE B, doi:10.1631/jzus.B2200385.
62.
Uematsu et al., Prophylactic administration of ivermectin attenuates SARS-CoV-2 induced disease in a Syrian Hamster Model, The Journal of Antibiotics, doi:10.1038/s41429-023-00623-0.
63.
Albariqi et al., Pharmacokinetics and Safety of Inhaled Ivermectin in Mice as a Potential COVID-19 Treatment, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121688.
64.
Errecalde et al., Safety and Pharmacokinetic Assessments of a Novel Ivermectin Nasal Spray Formulation in a Pig Model, Journal of Pharmaceutical Sciences, doi:10.1016/j.xphs.2021.01.017.
65.
Madrid et al., Safety of oral administration of high doses of ivermectin by means of biocompatible polyelectrolytes formulation, Heliyon, doi:10.1016/j.heliyon.2020.e05820.
66.
Ma et al., Ivermectin contributes to attenuating the severity of acute lung injury in mice, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2022.113706.
67.
de Melo et al., Attenuation of clinical and immunological outcomes during SARS-CoV-2 infection by ivermectin, EMBO Mol. Med., doi:10.15252/emmm.202114122.
68.
Arévalo et al., Ivermectin reduces in vivo coronavirus infection in a mouse experimental model, Scientific Reports, doi:10.1038/s41598-021-86679-0.
69.
Chaccour et al., Nebulized ivermectin for COVID-19 and other respiratory diseases, a proof of concept, dose-ranging study in rats, Scientific Reports, doi:10.1038/s41598-020-74084-y.
70.
Yan et al., Anti-inflammatory effects of ivermectin in mouse model of allergic asthma, Inflammation Research, doi:10.1007/s00011-011-0307-8.
71.
Götz et al., Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import, Scientific Reports, doi:10.1038/srep23138.
72.
Tay et al., Nuclear localization of dengue virus (DENV) 1–4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin, Antiviral Research, doi:10.1016/j.antiviral.2013.06.002.
73.
Wagstaff et al., Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus, Biochemical Journal, doi:10.1042/BJ20120150.
74.
Wagstaff (B) et al., An AlphaScreen®-Based Assay for High-Throughput Screening for Specific Inhibitors of Nuclear Import, SLAS Discovery, doi:10.1177/1087057110390360.
75.
Barrows et al., A Screen of FDA-Approved Drugs for Inhibitors of Zika Virus Infection, Cell Host & Microbe, doi:10.1016/j.chom.2016.07.004.
76.
Yang et al., The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer, Antiviral Research, doi:10.1016/j.antiviral.2020.104760.
77.
Mastrangelo et al., Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: new prospects for an old drug, Journal of Antimicrobial Chemotherapy, doi:10.1093/jac/dks147.
78.
Varghese et al., Discovery of berberine, abamectin and ivermectin as antivirals against chikungunya and other alphaviruses, Antiviral Research, doi:10.1016/j.antiviral.2015.12.012.
79.
Bennett et al., Role of a nuclear localization signal on the minor capsid Proteins VP2 and VP3 in BKPyV nuclear entry, Virology, doi:10.1016/j.virol.2014.10.013.
80.
Kosyna et al., The importin α/β-specific inhibitor Ivermectin affects HIF-dependent hypoxia response pathways, Biological Chemistry, doi:10.1515/hsz-2015-0171.
81.
Scheim et al., Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms242317039.
82.
Liu (C) et al., Crosstalk between neutrophil extracellular traps and immune regulation: insights into pathobiology and therapeutic implications of transfusion-related acute lung injury, Frontiers in Immunology, doi:10.3389/fimmu.2023.1324021.
83.
Shouman et al., SARS-CoV-2-associated lymphopenia: possible mechanisms and the role of CD147, Cell Communication and Signaling, doi:10.1186/s12964-024-01718-3.
84.
Scheim (B), D., Ivermectin for COVID-19 Treatment: Clinical Response at Quasi-Threshold Doses Via Hypothesized Alleviation of CD147-Mediated Vascular Occlusion, SSRN, doi:10.2139/ssrn.3636557.
85.
Scheim (C), D., From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate and Then Clot Blood Cells, Center for Open Science, doi:10.31219/osf.io/sgdj2.
86.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
87.
DiNicolantonio et al., Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19, Open Heart, doi:10.1136/openhrt-2020-001350.
88.
Mothae et al., SARS-CoV-2 host-pathogen interactome: insights into more players during pathogenesis, Virology, doi:10.1016/j.virol.2025.110607.
89.
Hazan et al., Treatment with Ivermectin Increases the Population of Bifidobacterium in the Gut, ACG 2023, acg2023posters.eventscribe.net/posterspeakers.asp.
Jitobaom et al., 14 Oct 2021, preprint, 8 authors.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Favipiravir and Ivermectin Showed in Vitro Synergistic Antiviral Activity against SARS-CoV-2
doi:10.21203/rs.3.rs-941811/v1
Despite the urgent need for effective antivirals against SARS-CoV-2 to mitigate the catastrophic impact of the COVID-19 pandemic, there are still no proven effective and widely available antivirals for COVID-19 treatment. Favipiravir and Ivermectin are among common repurposed drugs, which have been provisionally used in some countries. There have been clinical trials with mixed results, and therefore, it is still inconclusive whether they are effective or should be dismissed. It is plausible that the lack of clearcut clinical bene ts was due to the nding of only marginal levels of in vivo antiviral activity. An obvious way to improve the activity of antivirals is to use them in synergistic combinations. Here we show that Favipiravir and Ivermectin had the synergistic effects against SARS-CoV-2 in Vero cells. The combination may provide better e cacy in COVID-19 treatment. In addition, we found that Favipiravir had an additive effect with Niclosamide, another repurposed anti-parasitic drug with anti-SARS-CoV-2 activity. However, the anti-SARS-CoV-2 activity of Favipiravir was drastically reduced when tested in Calu-3 cells. This suggested that this cell type might not be able to metabolize Favipiravir into its active form, and that this de ciency in some cell types may affect in vivo e cacy of this drug.
Vero E6 cells were seeded in 12-well plates at a density of 2.2×10 5 cells/well, which allowed 100% con uence to be reached within 18 hr. The culture medium was removed, and the cells were inoculated with 100µl of 10-fold serial dilutions of virus supernatants for 1 hr. at 37 o C with 5%CO 2 . After that, the virus supernatants were removed, and the cells were overlaid with 1.56% microcrystalline cellulose (Avicel, RC-591) in 2%FBS-MEM. The cells were further incubated in the standard condition for three days. The overlaid medium was removed, and the cells were xed with 10% (v/v) formalin in phosphatebuffered saline (PBS) for 2 hr. The xed infected cells were washed in tap water, stained with 1% (w/v) crystal violet in 20% (v/v) ethanol for 5 min and washed to remove the excess dyes. The plaques were counted, and the viral titers were calculated in plaque forming units per ml (pfu/ml). 50% cell culture infectious dose (TCID 50 ) endpoint dilution assay Vero E6 cells were seeded in 96-well plates at a density of 3×10 4 cells/well. The culture medium was removed, and the cells were incubated with half-log10 serial dilution of the virus stock for 48 hr. at 37 o C with 5%CO 2 . After that, the cells were xed with 1:1 methanol/acetone for 30 min at 4 o C and the infectivity was detected with an antibody against the SARS-CoV-2 nucleocapsid protein (40143-R001, Sino Biological). The viral TCID 50 titers were calculated using the Reed and Muench method 73 .
One-step qRT-PCR for..
References
Aasld, HCV Guidance: Recommendations for testing, managing, and treating Hepatitis C Virus infection
Agrawal, Raju, Udwadia, Favipiravir: A new and emerging antiviral option in COVID-19
Alam, Therapeutic effectiveness and safety of repurposing drugs for the treatment of COVID-19: position standing in 2021, Front Pharmacol12, doi:10.3389/fphar.2021.659577
Ansems, Remdesivir for the treatment of COVID-19, Cochrane Database Syst Rev8, doi:10.1002/14651858.Cd014962
Backer, A randomized, double-blind, placebo-controlled phase 1 trial of inhaled and intranasal niclosamide: A broad spectrum antiviral candidate for treatment of COVID-19, Lancet Reg Health Eur4, doi:10.1016/j.lanepe.2021.100084
Baraka, Ivermectin distribution in the plasma and tissues of patients infected with Onchocerca volvulus, Eur J Clin Pharmacol50, doi:10.1007/s002280050131
Baranovich, T-705 (favipiravir) induces lethal mutagenesis in in uenza A H1N1 viruses in vitro, J Virol87, doi:10.1128/jvi.02346-12
Bobrowski, Synergistic and antagonistic drug combinations against SARS-CoV-2, Mol Ther29, doi:10.1016/j.ymthe.2020.12.016
Bryant, Ivermectin for prevention and treatment of COVID-19 infection: a systematic review, meta-analysis, and trial sequential analysis to inform clinical guidelines, Am J Ther28, doi:10.1097/mjt.0000000000001402
Cai, Experimental treatment with favipiravir for COVID-19: an open-label control study, Engineering, doi:10.1016/j.eng.2020.03.007
Caly, Druce, Catton, Jans, Wagstaff, The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral, doi:10.1016/j.antiviral.2020.104787
Day, Siu, Approaches to modernize the combination drug development paradigm, Genome Med, doi:10.1186/s13073-016-0369-x
Delang, Abdelnabi, Neyts, Favipiravir as a potential countermeasure against neglected and emerging RNA viruses, Antiviral, doi:10.1016/j.antiviral.2018.03.003
Dittmar, Drug repurposing screens reveal cell-type-speci c entry pathways and FDA-approved drugs active against SARS-Cov-2, Cell, doi:10.1016/j.celrep.2021.108959
Driouich, Favipiravir antiviral e cacy against SARS-CoV-2 in a hamster model, Nat Commun12, doi:10.1038/s41467-021-21992-w
Escribano-Romero, Jiménez De Oya, Domingo, Saiz, Extinction of West Nile Virus by Favipiravir through Lethal Mutagenesis, Antimicrob Agents Chemother61, doi:10.1128/aac.01400-17
Fang, Identi cation of three antiviral inhibitors against Japanese encephalitis virus from library of pharmacologically active compounds 1280, PLoS One8, doi:10.1371/journal.pone.0078425
Favié, Pharmacokinetics of favipiravir during continuous venovenous haemo ltration in a critically ill patient with in uenza, Antivir Ther23, doi:10.3851/imp3210
Furuta, Komeno, Nakamura, Favipiravir (T-705), a broad spectrum inhibitor of viral RNA polymerase, Proc Jpn Acad Ser B Phys Biol Sci93, doi:10.2183/pjab.93.027
Furuta, T-705 (favipiravir) and related compounds: Novel broad-spectrum inhibitors of RNA viral infections, Antiviral Res82, doi:10.1016/j.antiviral.2009.02.198
Furuta, T-705 (favipiravir) and related compounds: Novel broad-spectrum inhibitors of RNA viral infections, Antiviral Res82, doi:10.1016/j.antiviral.2009.02.198
Ganguly, SYBR green one-step qRT-PCR for the detection of SARS-CoV-2 RNA in saliva, doi:10.1101/2020.05.29.109702%JbioRxiv
Gassen, SKP2 attenuates autophagy through Beclin1-ubiquitination and its inhibition reduces MERS-Coronavirus infection, Nat Commun10, doi:10.1038/s41467-019-13659-4
Goldhill, Favipiravir-resistant in uenza A virus shows potential for transmission, PLoS, doi:10.1371/journal.ppat.1008937
Guedj, Antiviral e cacy of favipiravir against Ebola virus: A translational study in cynomolgus macaques, PLoS, doi:10.1371/journal.pmed.1002535
Guzzo, Safety, tolerability, and pharmacokinetics of escalating high doses of ivermectin in healthy adult subjects, J Clin Pharmacol42, doi:10.1177/009127002401382731
Götz, In uenza A viruses escape from MxA restriction at the expense of e cient nuclear vRNP import, Sci, doi:10.1038/srep23138
Hassanipour, The e cacy and safety of Favipiravir in treatment of COVID-19: a systematic review and meta-analysis of clinical trials, Sci, doi:10.1038/s41598-021-90551-6
Hassanipour, The e cacy and safety of Favipiravir in treatment of COVID-19: a systematic review and meta-analysis of clinical trials, Sci, doi:10.1038/s41598-021-90551-6
Hoffmann, Chloroquine does not inhibit infection of human lung cells with SARS-CoV-2, Nature585, doi:10.1038/s41586-020-2575-3
Hoffmann, SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor, doi:10.1016/j.cell.2020.02.052
Huang, Yang, Yuan, Li, Kuang, Niclosamide inhibits lytic replication of Epstein-Barr virus by disrupting mTOR activation, Antiviral, doi:10.1016/j.antiviral.2016.12.002
Huchting, Vanderlinden, Van Berwaer, Meier, Naesens, Cell line-dependent activation and antiviral activity of T-1105, the non-uorinated analogue of T-705 (favipiravir), Antiviral, doi:10.1016/j.antiviral.2019.04.002
Hurt, Wheatley, Neutralizing Antibody Therapeutics for COVID-19, Viruses13
Ianevski, Giri, Aittokallio, SynergyFinder 2.0: visual analytics of multi-drug combination synergies, Nucleic Acids Research, doi:10.1093/nar/gkaa216%J
Irie, Pharmacokinetics of Favipiravir in Critically Ill Patients With COVID-19, Clin Transl, doi:10.1111/cts.12827
Jeffreys, Remdesivir-Ivermectin combination displays synergistic interaction with improved in vitro antiviral activity against SARS-CoV-2, BioRxiv, doi:10.1101/2020.12.23.424232%JbioRxiv
Jeon, Identi cation of Antiviral Drug Candidates against SARS-CoV-2 from FDA-Approved Drugs, Antimicrob Agents Chemother64, doi:10.1128/aac.00819-20
Jochmans, Antiviral activity of Favipiravir (T-705) against a broad range of paramyxoviruses in vitro and against Human Metapneumovirus in hamsters, Antimicrob Agents Chemother60, doi:10.1128/aac.00709-16
Kadri, Lambourne, Mehellou, Niclosamide, a drug with many Repurposes, Chem Med, doi:10.1002/cmdc.201800100
Kamat, Kumari, Repurposing chloroquine against multiple diseases with special attention to SARS-CoV-2 and associated toxicity, Front Pharmacol12, doi:10.3389/fphar.2021.576093
Kanjanasirirat, High-content screening of Thai medicinal plants reveals Boesenbergia rotunda extract and its component Panduratin A as anti-SARS-CoV-2 agents, Sci, doi:10.1038/s41598-020-77003-3
Kao, The antiparasitic drug niclosamide inhibits dengue virus infection by interfering with endosomal acidi cation independent of mTOR, PLOS Negl Trop, doi:10.1371/journal.pntd.0006715
Kaptein, Favipiravir at high doses has potent antiviral activity in SARS-CoV-2-infected hamsters, whereas hydroxychloroquine lacks activity, Proc Natl Acad Sci U S, doi:10.1073/pnas.2014441117
Kashour, E cacy of chloroquine or hydroxychloroquine in COVID-19 patients: a systematic review and meta-analysis, J Antimicrob Chemother76, doi:10.1093/jac/dkaa403
Kim, Seong, Kumar, Shin, Favipiravir and Ribavirin Inhibit Replication of Asian and African Strains of Zika Virus in Different Cell Models, Viruses10, doi:10.3390/v10020072
Kongmanas, Immortalized stem cell-derived hepatocyte-like cells: An alternative model for studying dengue pathogenesis and therapy, PLOS Negl Trop, doi:10.1371/journal.pntd.0008835
Li, Multi-targeted therapy of cancer by niclosamide: A new application for an old drug, Cancer, doi:10.1016/j.canlet.2014.04.003
Mazzon, Identi cation of broad-spectrum antiviral compounds by targeting viral entry, Viruses11, doi:10.3390/v11020176
Melville, Rodriguez, Dobrovolny, Investigating different mechanisms of action in combination therapy for in uenza, Front Pharmacol9, doi:10.3389/fphar.2018.01207
Mentré, Dose regimen of favipiravir for Ebola virus disease, Lancet Infect Dis15, doi:10.1016/S1473-3099(14)71047-3
Musa, Potential antiviral effect of chloroquine therapy against SARS-CoV-2 infection, Open Access Maced J Med Sci8, doi:10.3889/oamjms.2020.4854
Ngo, The time to offer treatments for COVID-19, Expert Opin Investig, doi:10.1080/13543784.2021.1901883
Nguyen, Favipiravir pharmacokinetics in Ebola-Infected patients of the JIKI trial reveals concentrations lower than targeted, PLoS Negl Trop, doi:10.1371/journal.pntd.0005389
Niyomdecha, Suptawiwat, Boonarkart, Jitobaom, Auewarakul, Inhibition of human immunode ciency virus type 1 by niclosamide through mTORC1 inhibition, Heliyon6, doi:10.1016/j.heliyon.2020.e04050
Ohashi, Potential anti-COVID-19 agents, cepharanthine and nel navir, and their usage for combination treatment, iScience24, doi:10.1016/j.isci.2021.102367
Phougat, Combination therapy: the propitious rationale for drug development, Comb Chem High Throughput Screen17, doi:10.2174/13862073113166660065
Pires De Mello, Clinical regimens of Favipiravir inhibit Zika virus replication in the hollowber infection model, Antimicrob Agents Chemother62, doi:10.1128/aac.00967-18
Popp, Metzendorf, Gould, Kranke, Meybohm et al., Ivermectin for preventing and treating COVID-19, Cochrane Database Syst Rev, doi:10.1002/14651858.CD015017.pub2
Reed, Muench, A simple method of estimating fty percent enpoint, Am J Epidemiol27, doi:10.1093/oxfordjournals.aje.a118408%J
Schilling, The WHO guideline on drugs to prevent COVID-19: small numbers-big conclusions, Wellcome Open Res6, doi:10.12688/wellcomeopenres.16741.1
Shannon, Rapid incorporation of Favipiravir by the fast and permissive viral RNA polymerase complex results in SARS-CoV-2 lethal mutagenesis, Nat Commun11, doi:10.1038/s41467-020-18463-z
Suputtamongkol, Ivermectin accelerates circulating nonstructural protein 1 (NS1) clearance in adult dengue patients: a combined phase 2/3 randomized double-blinded placebo controlled trial, Clin Infect, doi:10.1093/cid/ciaa1332
Tan, Tan, Chu, Chow, Combination treatment with Remdesivir and Ivermectin exerts highly synergistic and potent antiviral activity against murine coronavirus infection, Front Cell Infect Microbiol11, doi:10.3389/fcimb.2021.700502
Vallejos, Ivermectin to prevent hospitalizations in patients with COVID-19 (IVERCOR-COVID19): a structured summary of a study protocol for a randomized controlled trial, Trials21, doi:10.1186/s13063-020-04813-1
Vincent, Chloroquine is a potent inhibitor of SARS coronavirus infection and spread, Virol J2, doi:10.1186/1743-422X-2-69
Wagstaff, Sivakumaran, Heaton, Harrich, Jans, Ivermectin is a speci c inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus, Biochem, doi:10.1042/bj20120150
Wang, Quality of and recommendations for relevant clinical practice guidelines for COVID-19 management: a systematic review and critical appraisal, Front Med8, doi:10.3389/fmed.2021.630765
Wang, The mechanism of action of T-705 as a unique delayed chain terminator on in uenza viral polymerase transcription, Biophys, doi:10.1016/j.bpc.2021.106652
Who, -line antiretroviral regimens and postexposure prophylaxis and recommendations on early infant diagnosis of HIV
Xu, Antivirus effectiveness of ivermectin on dengue virus type 2 in Aedes albopictus, PLOS Negl Trop Dis12, doi:10.1371/journal.pntd.0006934
Xu, Shi, Li, Zhou, Broad spectrum antiviral agent Niclosamide and its therapeutic potential, ACS Infect Dis6, doi:10.1021/acsinfecdis.0c00052
Yadav, Wennerberg, Aittokallio, Tang, Searching for drug synergy in complex doseresponse landscapes using an interaction potency model, Comput Struct Biotechnol13, doi:10.1016/j.csbj.2015.09.001
Yang, The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer, Antiviral, doi:10.1016/j.antiviral.2020.104760
DOI record:
{
"DOI": "10.21203/rs.3.rs-941811/v1",
"URL": "http://dx.doi.org/10.21203/rs.3.rs-941811/v1",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p>Despite the urgent need for effective antivirals against SARS-CoV-2 to mitigate the catastrophic impact of the COVID-19 pandemic, there are still no proven effective and widely available antivirals for COVID-19 treatment. Favipiravir and Ivermectin are among common repurposed drugs, which have been provisionally used in some countries. There have been clinical trials with mixed results, and therefore, it is still inconclusive whether they are effective or should be dismissed. It is plausible that the lack of clear-cut clinical benefits was due to the finding of only marginal levels of <jats:italic>in vivo</jats:italic> antiviral activity. An obvious way to improve the activity of antivirals is to use them in synergistic combinations. Here we show that Favipiravir and Ivermectin had the synergistic effects against SARS-CoV-2 in Vero cells. The combination may provide better efficacy in COVID-19 treatment. In addition, we found that Favipiravir had an additive effect with Niclosamide, another repurposed anti-parasitic drug with anti-SARS-CoV-2 activity. However, the anti-SARS-CoV-2 activity of Favipiravir was drastically reduced when tested in Calu-3 cells. This suggested that this cell type might not be able to metabolize Favipiravir into its active form, and that this deficiency in some cell types may affect <jats:italic>in vivo</jats:italic> efficacy of this drug.</jats:p>",
"accepted": {
"date-parts": [
[
2021,
9,
27
]
]
},
"author": [
{
"affiliation": [
{
"name": "Siriraj Hospital"
}
],
"family": "Jitobaom",
"given": "Kunlakanya",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Siriraj Hospital"
}
],
"family": "Boonarkart",
"given": "Chompunuch",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Mahidol University"
}
],
"family": "Manopwisedjaroen",
"given": "Suwimon",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Siriraj Hospital"
}
],
"family": "Punyadee",
"given": "Nuntaya",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Mahidol University"
}
],
"family": "Borwornpinyo",
"given": "Suparerk",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Mahidol University"
}
],
"family": "Thitithanyanont",
"given": "Arunee",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Siriraj Hospital"
}
],
"family": "Avirutnan",
"given": "Panisadee",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Siriraj Hospital"
}
],
"family": "Auewarakul",
"given": "Prasert",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
10,
14
]
],
"date-time": "2021-10-14T15:45:28Z",
"timestamp": 1634226328000
},
"deposited": {
"date-parts": [
[
2021,
12,
31
]
],
"date-time": "2021-12-31T08:29:25Z",
"timestamp": 1640939365000
},
"group-title": "In Review",
"indexed": {
"date-parts": [
[
2023,
2,
24
]
],
"date-time": "2023-02-24T10:53:40Z",
"timestamp": 1677236020276
},
"institution": [
{
"name": "Research Square"
}
],
"is-referenced-by-count": 3,
"issued": {
"date-parts": [
[
2021,
10,
14
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
10,
14
]
],
"date-time": "2021-10-14T00:00:00Z",
"timestamp": 1634169600000
}
}
],
"link": [
{
"URL": "https://www.researchsquare.com/article/rs-941811/v1",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.researchsquare.com/article/rs-941811/v1.html",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "8761",
"original-title": [],
"posted": {
"date-parts": [
[
2021,
10,
14
]
]
},
"prefix": "10.21203",
"published": {
"date-parts": [
[
2021,
10,
14
]
]
},
"publisher": "Research Square Platform LLC",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.researchsquare.com/article/rs-941811/v1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"subtype": "preprint",
"title": "Favipiravir and Ivermectin Showed in Vitro Synergistic Antiviral Activity against SARS-CoV-2",
"type": "posted-content"
}
