Anti-inflammatory effects of ivermectin in mouse model of allergic asthma
et al., Inflammation Research, doi:10.1007/s00011-011-0307-8, Jan 2011
Ivermectin for COVID-19
4th treatment shown to reduce risk in
August 2020, now with p < 0.00000000001 from 106 studies, recognized in 24 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
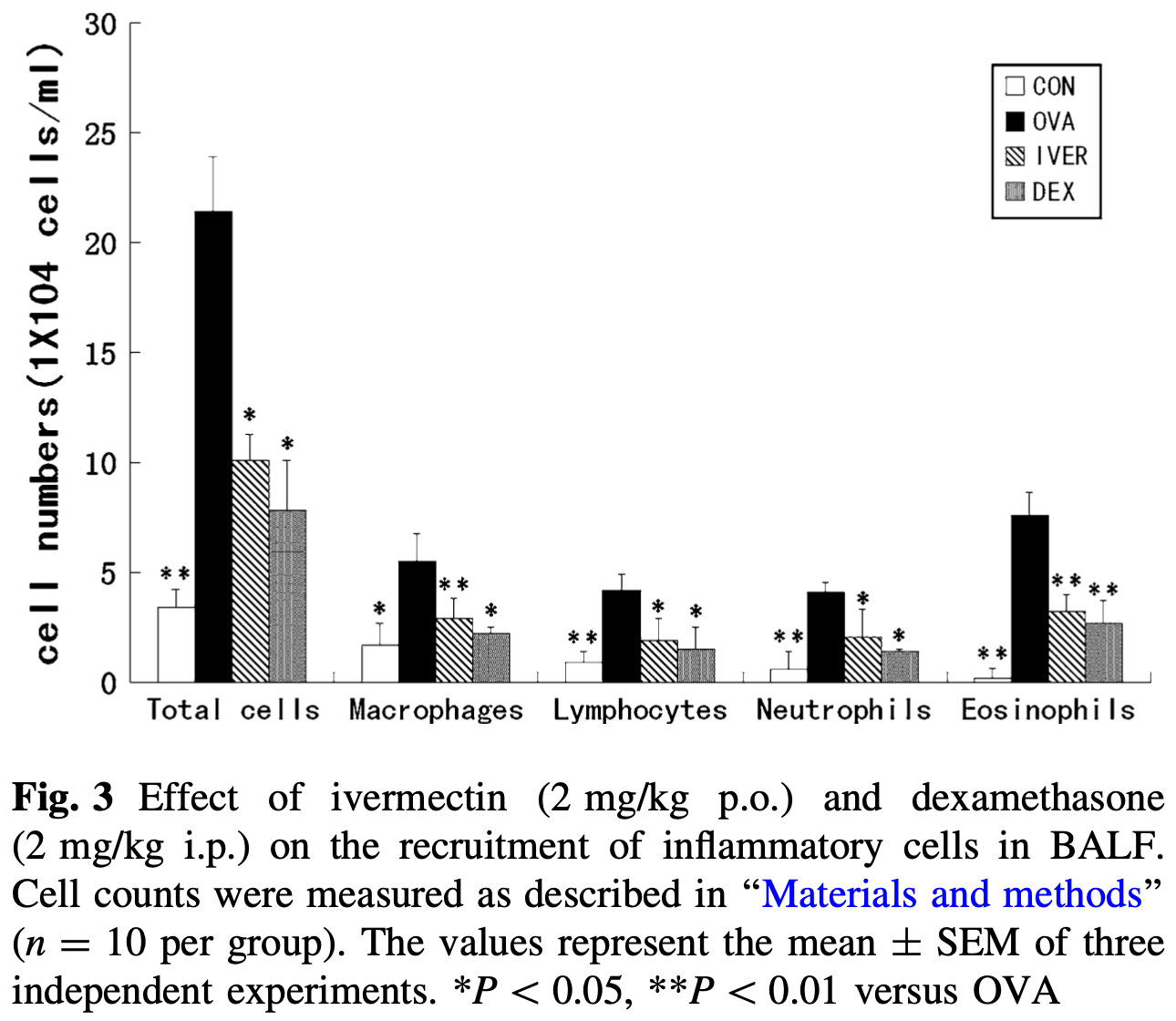
Mouse study showing ivermectin significantly reduced airway inflammation, Th2 cytokine production, mucus hypersecretion, and airway hyperresponsiveness in a mouse model of allergic asthma. Ivermectin lessened lung inflammation by decreasing inflammatory cell infiltration, mucus production, and IgE levels. The anti-inflammatory effects were similar to the steroid dexamethasone. Since uncontrolled inflammation and cytokine storm are major issues in severe COVID-19, these anti-inflammatory and immunomodulatory effects suggest ivermectin could potentially help prevent damaging inflammatory responses in the lungs that lead to respiratory failure.
74 preclinical studies support the efficacy of ivermectin for COVID-19:
Ivermectin, better known for antiparasitic activity, is a broad spectrum antiviral with activity against many viruses including H7N771, Dengue37,72,73 , HIV-173, Simian virus 4074, Zika37,75,76 , West Nile76, Yellow Fever77,78, Japanese encephalitis77, Chikungunya78, Semliki Forest virus78, Human papillomavirus57, Epstein-Barr57, BK Polyomavirus79, and Sindbis virus78.
Ivermectin inhibits importin-α/β-dependent nuclear import of viral proteins71,73,74,80 , shows spike-ACE2 disruption at 1nM with microfluidic diffusional sizing38, binds to glycan sites on the SARS-CoV-2 spike protein preventing interaction with blood and epithelial cells and inhibiting hemagglutination41,81, shows dose-dependent inhibition of wildtype and omicron variants36, exhibits dose-dependent inhibition of lung injury61,66, may inhibit SARS-CoV-2 via IMPase inhibition37, may inhibit SARS-CoV-2 induced formation of fibrin clots resistant to degradation9, inhibits SARS-CoV-2 3CLpro54, may inhibit SARS-CoV-2 RdRp activity28, may minimize viral myocarditis by inhibiting NF-κB/p65-mediated inflammation in macrophages60, may be beneficial for COVID-19 ARDS by blocking GSDMD and NET formation82, may interfere with SARS-CoV-2's immune evasion via ORF8 binding4, may inhibit SARS-CoV-2 by disrupting CD147 interaction83-86, may inhibit SARS-CoV-2 attachment to lipid rafts via spike NTD binding2, shows protection against inflammation, cytokine storm, and mortality in an LPS mouse model sharing key pathological features of severe COVID-1959,87, may be beneficial in severe COVID-19 by binding IGF1 to inhibit the promotion of inflammation, fibrosis, and cell proliferation that leads to lung damage8, may minimize SARS-CoV-2 induced cardiac damage40,48, may counter immune evasion by inhibiting NSP15-TBK1/KPNA1 interaction and restoring IRF3 activation88, may disrupt SARS-CoV-2 N and ORF6 protein nuclear transport and their suppression of host interferon responses1, reduces TAZ/YAP nuclear import, relieving SARS-CoV-2-driven suppression of IRF3 and NF-κB antiviral pathways35, increases Bifidobacteria which play a key role in the immune system89, has immunomodulatory51 and anti-inflammatory70,90 properties, and has an extensive and very positive safety profile91.
1.
Gayozo et al., Binding affinities analysis of ivermectin, nucleocapsid and ORF6 proteins of SARS-CoV-2 to human importins α isoforms: A computational approach, Biotecnia, doi:10.18633/biotecnia.v27.2485.
2.
Lefebvre et al., Characterization and Fluctuations of an Ivermectin Binding Site at the Lipid Raft Interface of the N-Terminal Domain (NTD) of the Spike Protein of SARS-CoV-2 Variants, Viruses, doi:10.3390/v16121836.
3.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
4.
Bagheri-Far et al., Non-spike protein inhibition of SARS-CoV-2 by natural products through the key mediator protein ORF8, Molecular Biology Research Communications, doi:10.22099/mbrc.2024.50245.2001.
5.
de Oliveira Só et al., In Silico Comparative Analysis of Ivermectin and Nirmatrelvir Inhibitors Interacting with the SARS-CoV-2 Main Protease, Preprints, doi:10.20944/preprints202404.1825.v1.
6.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
7.
Oranu et al., Validation of the binding affinities and stabilities of ivermectin and moxidectin against SARS-CoV-2 receptors using molecular docking and molecular dynamics simulation, GSC Biological and Pharmaceutical Sciences, doi:10.30574/gscbps.2024.26.1.0030.
8.
Zhao et al., Identification of the shared gene signatures between pulmonary fibrosis and pulmonary hypertension using bioinformatics analysis, Frontiers in Immunology, doi:10.3389/fimmu.2023.1197752.
9.
Vottero et al., Computational Prediction of the Interaction of Ivermectin with Fibrinogen, Molecular Sciences, doi:10.3390/ijms241411449.
10.
Chellasamy et al., Docking and molecular dynamics studies of human ezrin protein with a modelled SARS-CoV-2 endodomain and their interaction with potential invasion inhibitors, Journal of King Saud University - Science, doi:10.1016/j.jksus.2022.102277.
11.
Umar et al., Inhibitory potentials of ivermectin, nafamostat, and camostat on spike protein and some nonstructural proteins of SARS-CoV-2: Virtual screening approach, Jurnal Teknologi Laboratorium, doi:10.29238/teknolabjournal.v11i1.344.
12.
Alvarado et al., Interaction of the New Inhibitor Paxlovid (PF-07321332) and Ivermectin With the Monomer of the Main Protease SARS-CoV-2: A Volumetric Study Based on Molecular Dynamics, Elastic Networks, Classical Thermodynamics and SPT, Computational Biology and Chemistry, doi:10.1016/j.compbiolchem.2022.107692.
13.
Aminpour et al., In Silico Analysis of the Multi-Targeted Mode of Action of Ivermectin and Related Compounds, Computation, doi:10.3390/computation10040051.
14.
Parvez et al., Insights from a computational analysis of the SARS-CoV-2 Omicron variant: Host–pathogen interaction, pathogenicity, and possible drug therapeutics, Immunity, Inflammation and Disease, doi:10.1002/iid3.639.
15.
Francés-Monerris et al., Microscopic interactions between ivermectin and key human and viral proteins involved in SARS-CoV-2 infection, Physical Chemistry Chemical Physics, doi:10.1039/D1CP02967C.
16.
González-Paz et al., Comparative study of the interaction of ivermectin with proteins of interest associated with SARS-CoV-2: A computational and biophysical approach, Biophysical Chemistry, doi:10.1016/j.bpc.2021.106677.
17.
González-Paz (B) et al., Structural Deformability Induced in Proteins of Potential Interest Associated with COVID-19 by binding of Homologues present in Ivermectin: Comparative Study Based in Elastic Networks Models, Journal of Molecular Liquids, doi:10.1016/j.molliq.2021.117284.
18.
Rana et al., A Computational Study of Ivermectin and Doxycycline Combination Drug Against SARS-CoV-2 Infection, Research Square, doi:10.21203/rs.3.rs-755838/v1.
19.
Muthusamy et al., Virtual Screening Reveals Potential Anti-Parasitic Drugs Inhibiting the Receptor Binding Domain of SARS-CoV-2 Spike protein, Journal of Virology & Antiviral Research, www.scitechnol.com/abstract/virtual-screening-reveals-potential-antiparasitic-drugs-inhibiting-the-receptor-binding-domain-of-sarscov2-spike-protein-16398.html.
20.
Qureshi et al., Mechanistic insights into the inhibitory activity of FDA approved ivermectin against SARS-CoV-2: old drug with new implications, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1906750.
21.
Schöning et al., Highly-transmissible Variants of SARS-CoV-2 May Be More Susceptible to Drug Therapy Than Wild Type Strains, Research Square, doi:10.21203/rs.3.rs-379291/v1.
22.
Bello et al., Elucidation of the inhibitory activity of ivermectin with host nuclear importin α and several SARS-CoV-2 targets, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1911857.
23.
Udofia et al., In silico studies of selected multi-drug targeting against 3CLpro and nsp12 RNA-dependent RNA-polymerase proteins of SARS-CoV-2 and SARS-CoV, Network Modeling Analysis in Health Informatics and Bioinformatics, doi:10.1007/s13721-021-00299-2.
24.
Choudhury et al., Exploring the binding efficacy of ivermectin against the key proteins of SARS-CoV-2 pathogenesis: an in silico approach, Future Medicine, doi:10.2217/fvl-2020-0342.
25.
Kern et al., Modeling of SARS-CoV-2 Treatment Effects for Informed Drug Repurposing, Frontiers in Pharmacology, doi:10.3389/fphar.2021.625678.
26.
Saha et al., The Binding mechanism of ivermectin and levosalbutamol with spike protein of SARS-CoV-2, Structural Chemistry, doi:10.1007/s11224-021-01776-0.
27.
Eweas et al., Molecular Docking Reveals Ivermectin and Remdesivir as Potential Repurposed Drugs Against SARS-CoV-2, Frontiers in Microbiology, doi:10.3389/fmicb.2020.592908.
28.
Parvez (B) et al., Prediction of potential inhibitors for RNA-dependent RNA polymerase of SARS-CoV-2 using comprehensive drug repurposing and molecular docking approach, International Journal of Biological Macromolecules, doi:10.1016/j.ijbiomac.2020.09.098.
29.
Francés-Monerris (B) et al., Has Ivermectin Virus-Directed Effects against SARS-CoV-2? Rationalizing the Action of a Potential Multitarget Antiviral Agent, ChemRxiv, doi:10.26434/chemrxiv.12782258.v1.
30.
Kalhor et al., Repurposing of the approved small molecule drugs in order to inhibit SARS-CoV-2 S protein and human ACE2 interaction through virtual screening approaches, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2020.1824816.
31.
Swargiary, A., Ivermectin as a promising RNA-dependent RNA polymerase inhibitor and a therapeutic drug against SARS-CoV2: Evidence from in silico studies, Research Square, doi:10.21203/rs.3.rs-73308/v1.
32.
Maurya, D., A Combination of Ivermectin and Doxycycline Possibly Blocks the Viral Entry and Modulate the Innate Immune Response in COVID-19 Patients, American Chemical Society (ACS), doi:10.26434/chemrxiv.12630539.v1.
33.
Lehrer et al., Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2, In Vivo, 34:5, 3023-3026, doi:10.21873/invivo.12134.
34.
Suravajhala et al., Comparative Docking Studies on Curcumin with COVID-19 Proteins, Preprints, doi:10.20944/preprints202005.0439.v3.
35.
Kofler et al., M-Motif, a potential non-conventional NLS in YAP/TAZ and other cellular and viral proteins that inhibits classic protein import, iScience, doi:10.1016/j.isci.2025.112105.
36.
Shahin et al., The selective effect of Ivermectin on different human coronaviruses; in-vitro study, Research Square, doi:10.21203/rs.3.rs-4180797/v1.
37.
Jitobaom et al., Identification of inositol monophosphatase as a broad‐spectrum antiviral target of ivermectin, Journal of Medical Virology, doi:10.1002/jmv.29552.
38.
Fauquet et al., Microfluidic Diffusion Sizing Applied to the Study of Natural Products and Extracts That Modulate the SARS-CoV-2 Spike RBD/ACE2 Interaction, Molecules, doi:10.3390/molecules28248072.
39.
García-Aguilar et al., In Vitro Analysis of SARS-CoV-2 Spike Protein and Ivermectin Interaction, International Journal of Molecular Sciences, doi:10.3390/ijms242216392.
40.
Liu et al., SARS-CoV-2 viral genes Nsp6, Nsp8, and M compromise cellular ATP levels to impair survival and function of human pluripotent stem cell-derived cardiomyocytes, Stem Cell Research & Therapy, doi:10.1186/s13287-023-03485-3.
41.
Boschi et al., SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects, bioRxiv, doi:10.1101/2022.11.24.517882.
42.
De Forni et al., Synergistic drug combinations designed to fully suppress SARS-CoV-2 in the lung of COVID-19 patients, PLoS ONE, doi:10.1371/journal.pone.0276751.
43.
Saha (B) et al., Manipulation of Spray-Drying Conditions to Develop an Inhalable Ivermectin Dry Powder, Pharmaceutics, doi:10.3390/pharmaceutics14071432.
44.
Jitobaom (B) et al., Synergistic anti-SARS-CoV-2 activity of repurposed anti-parasitic drug combinations, BMC Pharmacology and Toxicology, doi:10.1186/s40360-022-00580-8.
45.
Croci et al., Liposomal Systems as Nanocarriers for the Antiviral Agent Ivermectin, International Journal of Biomaterials, doi:10.1155/2016/8043983.
46.
Zheng et al., Red blood cell-hitchhiking mediated pulmonary delivery of ivermectin: Effects of nanoparticle properties, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121719.
47.
Delandre et al., Antiviral Activity of Repurposing Ivermectin against a Panel of 30 Clinical SARS-CoV-2 Strains Belonging to 14 Variants, Pharmaceuticals, doi:10.3390/ph15040445.
48.
Liu (B) et al., Genome-wide analyses reveal the detrimental impacts of SARS-CoV-2 viral gene Orf9c on human pluripotent stem cell-derived cardiomyocytes, Stem Cell Reports, doi:10.1016/j.stemcr.2022.01.014.
49.
Segatori et al., Effect of Ivermectin and Atorvastatin on Nuclear Localization of Importin Alpha and Drug Target Expression Profiling in Host Cells from Nasopharyngeal Swabs of SARS-CoV-2- Positive Patients, Viruses, doi:10.3390/v13102084.
50.
Jitobaom (C) et al., Favipiravir and Ivermectin Showed in Vitro Synergistic Antiviral Activity against SARS-CoV-2, Research Square, doi:10.21203/rs.3.rs-941811/v1.
51.
Munson et al., Niclosamide and ivermectin modulate caspase-1 activity and proinflammatory cytokine secretion in a monocytic cell line, British Society For Nanomedicine Early Career Researcher Summer Meeting, 2021, web.archive.org/web/20230401070026/https://michealmunson.github.io/COVID.pdf.
52.
Mountain Valley MD, Mountain Valley MD Receives Successful Results From BSL-4 COVID-19 Clearance Trial on Three Variants Tested With Ivectosol™, 5/18, www.globenewswire.com/en/news-release/2021/05/18/2231755/0/en/Mountain-Valley-MD-Receives-Successful-Results-From-BSL-4-COVID-19-Clearance-Trial-on-Three-Variants-Tested-With-Ivectosol.html.
53.
Yesilbag et al., Ivermectin also inhibits the replication of bovine respiratory viruses (BRSV, BPIV-3, BoHV-1, BCoV and BVDV) in vitro, Virus Research, doi:10.1016/j.virusres.2021.198384.
54.
Mody et al., Identification of 3-chymotrypsin like protease (3CLPro) inhibitors as potential anti-SARS-CoV-2 agents, Communications Biology, doi:10.1038/s42003-020-01577-x.
55.
Jeffreys et al., Remdesivir-ivermectin combination displays synergistic interaction with improved in vitro activity against SARS-CoV-2, International Journal of Antimicrobial Agents, doi:10.1016/j.ijantimicag.2022.106542.
56.
Surnar et al., Clinically Approved Antiviral Drug in an Orally Administrable Nanoparticle for COVID-19, ACS Pharmacol. Transl. Sci., doi:10.1021/acsptsci.0c00179.
57.
Li et al., Quantitative proteomics reveals a broad-spectrum antiviral property of ivermectin, benefiting for COVID-19 treatment, J. Cellular Physiology, doi:10.1002/jcp.30055.
58.
Caly et al., The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Research, doi:10.1016/j.antiviral.2020.104787.
59.
Zhang et al., Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice, Inflammation Research, doi:10.1007/s00011-008-8007-8.
60.
Gao et al., Ivermectin ameliorates acute myocarditis via the inhibition of importin-mediated nuclear translocation of NF-κB/p65, International Immunopharmacology, doi:10.1016/j.intimp.2024.112073.
61.
Abd-Elmawla et al., Suppression of NLRP3 inflammasome by ivermectin ameliorates bleomycin-induced pulmonary fibrosis, Journal of Zhejiang University-SCIENCE B, doi:10.1631/jzus.B2200385.
62.
Uematsu et al., Prophylactic administration of ivermectin attenuates SARS-CoV-2 induced disease in a Syrian Hamster Model, The Journal of Antibiotics, doi:10.1038/s41429-023-00623-0.
63.
Albariqi et al., Pharmacokinetics and Safety of Inhaled Ivermectin in Mice as a Potential COVID-19 Treatment, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121688.
64.
Errecalde et al., Safety and Pharmacokinetic Assessments of a Novel Ivermectin Nasal Spray Formulation in a Pig Model, Journal of Pharmaceutical Sciences, doi:10.1016/j.xphs.2021.01.017.
65.
Madrid et al., Safety of oral administration of high doses of ivermectin by means of biocompatible polyelectrolytes formulation, Heliyon, doi:10.1016/j.heliyon.2020.e05820.
66.
Ma et al., Ivermectin contributes to attenuating the severity of acute lung injury in mice, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2022.113706.
67.
de Melo et al., Attenuation of clinical and immunological outcomes during SARS-CoV-2 infection by ivermectin, EMBO Mol. Med., doi:10.15252/emmm.202114122.
68.
Arévalo et al., Ivermectin reduces in vivo coronavirus infection in a mouse experimental model, Scientific Reports, doi:10.1038/s41598-021-86679-0.
69.
Chaccour et al., Nebulized ivermectin for COVID-19 and other respiratory diseases, a proof of concept, dose-ranging study in rats, Scientific Reports, doi:10.1038/s41598-020-74084-y.
70.
Yan et al., Anti-inflammatory effects of ivermectin in mouse model of allergic asthma, Inflammation Research, doi:10.1007/s00011-011-0307-8.
71.
Götz et al., Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import, Scientific Reports, doi:10.1038/srep23138.
72.
Tay et al., Nuclear localization of dengue virus (DENV) 1–4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin, Antiviral Research, doi:10.1016/j.antiviral.2013.06.002.
73.
Wagstaff et al., Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus, Biochemical Journal, doi:10.1042/BJ20120150.
74.
Wagstaff (B) et al., An AlphaScreen®-Based Assay for High-Throughput Screening for Specific Inhibitors of Nuclear Import, SLAS Discovery, doi:10.1177/1087057110390360.
75.
Barrows et al., A Screen of FDA-Approved Drugs for Inhibitors of Zika Virus Infection, Cell Host & Microbe, doi:10.1016/j.chom.2016.07.004.
76.
Yang et al., The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer, Antiviral Research, doi:10.1016/j.antiviral.2020.104760.
77.
Mastrangelo et al., Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: new prospects for an old drug, Journal of Antimicrobial Chemotherapy, doi:10.1093/jac/dks147.
78.
Varghese et al., Discovery of berberine, abamectin and ivermectin as antivirals against chikungunya and other alphaviruses, Antiviral Research, doi:10.1016/j.antiviral.2015.12.012.
79.
Bennett et al., Role of a nuclear localization signal on the minor capsid Proteins VP2 and VP3 in BKPyV nuclear entry, Virology, doi:10.1016/j.virol.2014.10.013.
80.
Kosyna et al., The importin α/β-specific inhibitor Ivermectin affects HIF-dependent hypoxia response pathways, Biological Chemistry, doi:10.1515/hsz-2015-0171.
81.
Scheim et al., Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms242317039.
82.
Liu (C) et al., Crosstalk between neutrophil extracellular traps and immune regulation: insights into pathobiology and therapeutic implications of transfusion-related acute lung injury, Frontiers in Immunology, doi:10.3389/fimmu.2023.1324021.
83.
Shouman et al., SARS-CoV-2-associated lymphopenia: possible mechanisms and the role of CD147, Cell Communication and Signaling, doi:10.1186/s12964-024-01718-3.
84.
Scheim (B), D., Ivermectin for COVID-19 Treatment: Clinical Response at Quasi-Threshold Doses Via Hypothesized Alleviation of CD147-Mediated Vascular Occlusion, SSRN, doi:10.2139/ssrn.3636557.
85.
Scheim (C), D., From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate and Then Clot Blood Cells, Center for Open Science, doi:10.31219/osf.io/sgdj2.
86.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
87.
DiNicolantonio et al., Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19, Open Heart, doi:10.1136/openhrt-2020-001350.
88.
Mothae et al., SARS-CoV-2 host-pathogen interactome: insights into more players during pathogenesis, Virology, doi:10.1016/j.virol.2025.110607.
89.
Hazan et al., Treatment with Ivermectin Increases the Population of Bifidobacterium in the Gut, ACG 2023, acg2023posters.eventscribe.net/posterspeakers.asp.
Yan et al., 29 Jan 2011, peer-reviewed, 8 authors.
Contact: xumingdeng@jluhp.edu.cn.
Anti-inflammatory effects of ivermectin in mouse model of allergic asthma
Inflammation Research, doi:10.1007/s00011-011-0307-8
Background and objective Asthma is an inflammatory disease of the lungs that is characterised by increased inflammatory cell infiltration into the airways and poor respiratory function. Ivermectin is a semi-synthetic derivative of a family of macrocyclic lactones that shows broad-spectrum anti-parasitic activity. This drug has been shown to possess anti-inflammatory activity, but whether it can be used in asthma treatment has not yet been investigated. In this study, we aimed to investigate the inhibitory effects of ivermectin on allergic asthma symptoms in mice.
Methods and results We used a mouse asthma model, in which allergic airway inflammation and airway remodelling were induced by ovalbumin (OVA) sensitisation and challenge. Ivermectin or PBS treatment was administered 1 h before OVA challenge. Ivermectin at 2 mg/kg significantly diminished recruitment of immune cells, production of cytokines in the bronchoalveolar lavage fluids and secretion of OVA-specific IgE and IgG1 in the serum. Histological studies indicated that ivermectin suppressed mucus hypersecretion by goblet cells in the airway. Conclusions This is the first study to demonstrate that ivermectin is an effective suppressor of inflammation and may be efficacious in the treatment of non-infectious airway inflammatory diseases such as allergic asthma.
References
Abu-Ghazaleh, Kita, Gleich, Eosinophil activation and function in health and disease, Immunol Ser
Agen, Danesi, Blandizzi, Costa, Stacchini et al., Macrolide antibiotics as antiinflammatory agents: roxithromycin in an unexpected role, Agents Actions
Anderson, Coyle, Th2 and 'Th2-like' cells in allergy and asthma: pharmacological perspectives, Trends Pharmacol Sci
Beigelman, Gunsten, Mikols, Vidavsky, Cannon et al., Azithromycin attenuates airway inflammation in a noninfectious mouse model of allergic asthma, Chest
Braman, The global burden of asthma, Chest
Bryskier, Agouridas, Chantot, New medical targets for macrolides, Exp Opin Invest Drugs
Caumes, Danis, New indications of ivermectin, Rev Med Interne
Coffman, Seymour, Hudak, Jackson, Rennick, Antibody to interleukin-5 inhibits helminth-induced eosinophilia in mice, Science
Corry, Grunig, Hadeiba, Kurup, Warnock et al., Requirementsfor allergen-induced airway hyperreactivity in T and B cell-deficient mice, Mol Med
Curtis, Byrd, Warnock, Kaltreider, Requirement of CD4-positive T cells for cellular recruitment to the lungs of mice in response to a particulate intratracheal antigen, J Clin Invest
Ej, Macrolides beyond the conventional antimicrobials: a class of potent immunomodulators, Int J Antimicrob Agents
Elias, Lee, Zheng, Ma, Homer et al., New insights into the pathogenesis of asthma, J Clin Invest
Flohe, Brigelius-Flohe, Saliou, Traber, Packer, Redox regulation of NF-kappa B activation, Free Radic Biol Med
Fostera, Martinez-Moczygembab, Hustonb, Db, Interleukins-4, -5, and -13: emerging therapeutic targets in allergic disease, Pharmacol Ther
Hrvac ˇic, Bos ˇnjak, Bosnar, Ferenc ˇic ´z ˇ, Glojnaric et al., Clarithromycin suppresses airway hyperresponsiveness and inflammation in mouse models of asthma, Eur J Pharmacol
Kimber, Stone, Dearman, Assessment of the inherent allergenic potential of proteins in mice, Environ Health Perspect
Kips, Cytokines in asthma, Eur Respir J
Kopf, Brombacher, Hodgkin, Ramsay, Milbourne et al., IL-5-deficient mice have a developmental defect in CD5? B-1 cells and lack eosinophilia but have normal antibody and cytotoxic T cell responses, Immunity
Lee, Mcgarry, Farmer, Denzler, Larson et al., Interleukin-5 expression in the lung epithelium of transgenic mice leads to pulmonary changes pathognomonic of asthma, J Exp Med
Mikasa, Kita, Sawaki, Kunimatsu, Hamada et al., The anti-inflammatory effect of erythromycin in zymosan-induced peritonitis of mice, J Antimicrob Chemother
Ngoc, Gold, Tzianabos, Weiss, Celedon, Cytokines, allergy, and asthma, Curr Opin Allergy Clin Immunol
Peat, Toelle, Salome, Predictive nature of bronchial responsiveness and respiratory symptoms in a one year cohort study of Sydney schoolchildren, Eur Respir J
Pene, Rousset, Briere, Chretien, Bonnefoy et al., IgE production by normal human lymphocytes is induced by interleukin 4 and suppressed by interferons a, g and prostaglandin E2, Proc Nat Acad Sci
Purkerson, Isakson, A two-signal model for regulation of immunoglobulin isotype switching, FASEB J
Stankiewicz, Cabaj, Moore, Millar, Ng Chie, Influence of ivermectin on cellular and humoral immune responses of lambs, Vet Immunol Immunopathol
Tarayre, Aliaga, Barbara, Villanova, Ballester et al., Cutaneously applied erythromycin base reduces various types of inflammatory reactions in mouse ear, Int J Tiss Reac
Toelle, Peat, Salome, Toward a definition of asthma for epidemiology, Am Rev Respir Dis
Umetsu, Dekruyff, TH1 and TH2 CD4? cells in human allergic diseases, J Allergy Clin Immunol
Van Rijt, Kuipers, Vos, Hijdra, Hoogsteden et al., A rapid flow cytometric method for determining the cellular composition of bronchoalveolar lavage fluid cells in mouse models of asthma, J Immunol Methods
Vanden Berghe, Plaisance, Boone, Bosscher, Schmitz et al., p38 and extracellular signal-regulated kinase mitogen-activated protein kinase pathways are required for nuclear factor-kappaB p65 transactivation mediated by tumor necrosis factor, J Biol Chem
Wills-Karp, Immunologic basis of antigen-induced airway hyperresponsiveness, Annu Rev Immunol
Wills-Karp, Interleukin-13 in asthma pathogenesis, Immunol Rev
Wills-Karp, Luyimbazi, Xu, Schofield, Interleukin-13: central mediator of allergic asthma, Science
Zhang, Song, Ci, Ju, Li, Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice, Inflamm Res
Zhang, Song, Xiong, Ci, Li et al., Inhibitory effects of ivermectin on nitric oxide and prostaglandin E 2 production in LPS-stimulated RAW 264.7 macrophages, Int J Immunopharmacol
Zhou, Kang, Xie, Liu, Lou et al., Rapid nongenomic effects of glucocorticoids on allergic asthma reaction in the guinea pig, J Endocrinol
Zhu, Homer, Wang, Pulmonary expression of interleukin-13 causes inflammation, mucus hypersesretion, subepithelial fibrosis, physiologic abnormalities, and eotaxin production, J Clin Invest
DOI record:
{
"DOI": "10.1007/s00011-011-0307-8",
"ISSN": [
"1023-3830",
"1420-908X"
],
"URL": "http://dx.doi.org/10.1007/s00011-011-0307-8",
"alternative-id": [
"307"
],
"author": [
{
"affiliation": [],
"family": "Yan",
"given": "Shuhan",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ci",
"given": "Xinxin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Na",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chen",
"given": "Chi",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Xiangchao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chu",
"given": "Xiao",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Li",
"given": "Jianhua",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Deng",
"given": "Xuming",
"sequence": "additional"
}
],
"container-title": "Inflammation Research",
"container-title-short": "Inflamm. Res.",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2011,
1,
28
]
],
"date-time": "2011-01-28T20:16:31Z",
"timestamp": 1296245791000
},
"deposited": {
"date-parts": [
[
2019,
6,
8
]
],
"date-time": "2019-06-08T06:01:31Z",
"timestamp": 1559973691000
},
"indexed": {
"date-parts": [
[
2023,
9,
20
]
],
"date-time": "2023-09-20T19:36:37Z",
"timestamp": 1695238597615
},
"is-referenced-by-count": 77,
"issue": "6",
"issued": {
"date-parts": [
[
2011,
1,
29
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2011,
6
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://www.springer.com/tdm",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2011,
1,
29
]
],
"date-time": "2011-01-29T00:00:00Z",
"timestamp": 1296259200000
}
}
],
"link": [
{
"URL": "http://link.springer.com/content/pdf/10.1007/s00011-011-0307-8.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://link.springer.com/article/10.1007/s00011-011-0307-8/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "http://link.springer.com/content/pdf/10.1007/s00011-011-0307-8",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"page": "589-596",
"prefix": "10.1007",
"published": {
"date-parts": [
[
2011,
1,
29
]
]
},
"published-online": {
"date-parts": [
[
2011,
1,
29
]
]
},
"published-print": {
"date-parts": [
[
2011,
6
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.1172/JCI17748",
"author": "JA Elias",
"doi-asserted-by": "crossref",
"first-page": "291",
"journal-title": "J Clin Invest",
"key": "307_CR1",
"unstructured": "Elias JA, Lee CG, Zheng T, Ma B, Homer RJ, Zhu Z. New insights into the pathogenesis of asthma. J Clin Invest. 2003;111:291–7.",
"volume": "111",
"year": "2003"
},
{
"DOI": "10.1146/annurev.immunol.17.1.255",
"author": "M Wills-Karp",
"doi-asserted-by": "crossref",
"first-page": "255",
"journal-title": "Annu Rev Immunol",
"key": "307_CR2",
"unstructured": "Wills-Karp M. Immunologic basis of antigen-induced airway hyperresponsiveness. Annu Rev Immunol. 1999;17:255–81.",
"volume": "17",
"year": "1999"
},
{
"DOI": "10.1016/0165-6147(94)90027-2",
"author": "GP Anderson",
"doi-asserted-by": "crossref",
"first-page": "324",
"journal-title": "Trends Pharmacol Sci",
"key": "307_CR3",
"unstructured": "Anderson GP, Coyle AJ. Th2 and ‘Th2-like’ cells in allergy and asthma: pharmacological perspectives. Trends Pharmacol Sci. 1994;15:324–32.",
"volume": "15",
"year": "1994"
},
{
"DOI": "10.1378/chest.130.1_suppl.4S",
"author": "SS Braman",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "Chest",
"key": "307_CR4",
"unstructured": "Braman SS. The global burden of asthma. Chest. 2006;130:4–12.",
"volume": "130",
"year": "2006"
},
{
"DOI": "10.1517/13543784.3.4.405",
"author": "A Bryskier",
"doi-asserted-by": "crossref",
"first-page": "405",
"journal-title": "Exp Opin Invest Drugs",
"key": "307_CR5",
"unstructured": "Bryskier A, Agouridas C, Chantot JF. New medical targets for macrolides. Exp Opin Invest Drugs. 1994;3:405–10.",
"volume": "3",
"year": "1994"
},
{
"author": "JP Tarayre",
"first-page": "77",
"journal-title": "Int J Tiss Reac",
"key": "307_CR6",
"unstructured": "Tarayre JP, Aliaga M, Barbara M, Villanova G, Ballester R, Tisne-Versailles J, et al. Cutaneously applied erythromycin base reduces various types of inflammatory reactions in mouse ear. Int J Tiss Reac. 1987;4:77–85.",
"volume": "4",
"year": "1987"
},
{
"DOI": "10.1093/jac/30.3.339",
"author": "K Mikasa",
"doi-asserted-by": "crossref",
"first-page": "339",
"journal-title": "J Antimicrob Chemother",
"key": "307_CR7",
"unstructured": "Mikasa K, Kita E, Sawaki M, Kunimatsu M, Hamada K, Konishi M, et al. The anti-inflammatory effect of erythromycin in zymosan-induced peritonitis of mice. J Antimicrob Chemother. 1992;30:339–48.",
"volume": "30",
"year": "1992"
},
{
"DOI": "10.1007/BF02027218",
"author": "C Agen",
"doi-asserted-by": "crossref",
"first-page": "85",
"journal-title": "Agents Actions",
"key": "307_CR8",
"unstructured": "Agen C, Danesi R, Blandizzi C, Costa M, Stacchini B, Favini P, et al. Macrolide antibiotics as antiinflammatory agents: roxithromycin in an unexpected role. Agents Actions. 1993;38:85–90.",
"volume": "38",
"year": "1993"
},
{
"DOI": "10.1016/j.ijantimicag.2007.08.001",
"author": "EJ Giamarellos-Bourboulis",
"doi-asserted-by": "crossref",
"first-page": "12",
"journal-title": "Int J Antimicrob Agents",
"key": "307_CR9",
"unstructured": "Giamarellos-Bourboulis EJ. Macrolides beyond the conventional antimicrobials: a class of potent immunomodulators. Int J Antimicrob Agents. 2008;31:12–20.",
"volume": "31",
"year": "2008"
},
{
"DOI": "10.1016/j.ejphar.2009.06.032",
"author": "B Hrvačić",
"doi-asserted-by": "crossref",
"first-page": "236",
"journal-title": "Eur J Pharmacol",
"key": "307_CR10",
"unstructured": "Hrvačić B, Bošnjak B, Bosnar M, Ferenčić Ž, Glojnarić I, Eraković Haber V. Clarithromycin suppresses airway hyperresponsiveness and inflammation in mouse models of asthma. Eur J Pharmacol. 2009;15:236–43.",
"volume": "15",
"year": "2009"
},
{
"DOI": "10.1378/chest.08-3056",
"author": "A Beigelman",
"doi-asserted-by": "crossref",
"first-page": "498",
"issue": "2",
"journal-title": "Chest",
"key": "307_CR11",
"unstructured": "Beigelman A, Gunsten S, Mikols CL, Vidavsky I, Cannon CL, Brody SL, et al. Azithromycin attenuates airway inflammation in a noninfectious mouse model of allergic asthma. Chest. 2009;136(2):498–506.",
"volume": "136",
"year": "2009"
},
{
"DOI": "10.1016/S0248-8663(01)00350-2",
"author": "E Caumes",
"doi-asserted-by": "crossref",
"first-page": "379",
"journal-title": "Rev Med Interne",
"key": "307_CR12",
"unstructured": "Caumes E, Danis M. New indications of ivermectin. Rev Med Interne. 2001;22:379–84.",
"volume": "22",
"year": "2001"
},
{
"DOI": "10.1016/0165-2427(94)05308-F",
"author": "M Stankiewicz",
"doi-asserted-by": "crossref",
"first-page": "347",
"journal-title": "Vet Immunol Immunopathol",
"key": "307_CR13",
"unstructured": "Stankiewicz M, Cabaj W, Jonas WE, Moore LG, Millar K, Ng Chie W. Influence of ivermectin on cellular and humoral immune responses of lambs. Vet Immunol Immunopathol. 1995;44:347–58.",
"volume": "44",
"year": "1995"
},
{
"DOI": "10.1016/j.intimp.2008.12.016",
"author": "X Zhang",
"doi-asserted-by": "crossref",
"first-page": "354",
"journal-title": "Int J Immunopharmacol",
"key": "307_CR14",
"unstructured": "Zhang X, Song Y, Xiong H, Ci X, Li H, Yu L, et al. Inhibitory effects of ivermectin on nitric oxide and prostaglandin E2 production in LPS-stimulated RAW 264.7 macrophages. Int J Immunopharmacol. 2009;9:354–9.",
"volume": "9",
"year": "2009"
},
{
"DOI": "10.1007/s00011-008-8007-8",
"author": "X Zhang",
"doi-asserted-by": "crossref",
"first-page": "524",
"journal-title": "Inflamm Res",
"key": "307_CR15",
"unstructured": "Zhang X, Song Y, Ci X, An N, Ju Y, Li H, et al. Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice. Inflamm Res. 2008;57:524–9.",
"volume": "57",
"year": "2008"
},
{
"DOI": "10.1016/j.jim.2004.03.004",
"author": "LS Rijt Van",
"doi-asserted-by": "crossref",
"first-page": "111",
"journal-title": "J Immunol Methods",
"key": "307_CR16",
"unstructured": "Van Rijt LS, Kuipers H, Vos N, Hijdra D, Hoogsteden HC, Lambrecht BN. A rapid flow cytometric method for determining the cellular composition of bronchoalveolar lavage fluid cells in mouse models of asthma. J Immunol Methods. 2004;288:111–21.",
"volume": "288",
"year": "2004"
},
{
"DOI": "10.1677/joe.0.177R001",
"author": "J Zhou",
"doi-asserted-by": "crossref",
"first-page": "R1",
"journal-title": "J Endocrinol",
"key": "307_CR17",
"unstructured": "Zhou J, Kang Z, Xie Q, Liu C, Lou S, Chen Y, et al. Rapid nongenomic effects of glucocorticoids on allergic asthma reaction in the guinea pig. J Endocrinol. 2003;177:R1–4.",
"volume": "177",
"year": "2003"
},
{
"DOI": "10.1073/pnas.85.18.6880",
"author": "J Pene",
"doi-asserted-by": "crossref",
"first-page": "6880",
"journal-title": "Proc Nat Acad Sci USA",
"key": "307_CR18",
"unstructured": "Pene J, Rousset F, Briere F, Chretien I, Bonnefoy JY, Spits H, et al. IgE production by normal human lymphocytes is induced by interleukin 4 and suppressed by interferons a, g and prostaglandin E2. Proc Nat Acad Sci USA. 1988;85:6880–4.",
"volume": "85",
"year": "1988"
},
{
"DOI": "10.1016/S0091-6749(97)70186-6",
"author": "DT Umetsu",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "J Allergy Clin Immunol",
"key": "307_CR19",
"unstructured": "Umetsu DT, DeKruyff RH. TH1 and TH2 CD4+ cells in human allergic diseases. J Allergy Clin Immunol. 1997;100:1–6.",
"volume": "100",
"year": "1997"
},
{
"DOI": "10.1007/s008940050092",
"author": "DB Corry",
"doi-asserted-by": "crossref",
"first-page": "344",
"journal-title": "Mol Med",
"key": "307_CR20",
"unstructured": "Corry DB, Grunig G, Hadeiba H, Kurup VP, Warnock ML, Sheppard D, et al. Requirementsfor allergen-induced airway hyperreactivity in T and B cell-deficient mice. Mol Med. 1998;4:344–55.",
"volume": "4",
"year": "1998"
},
{
"DOI": "10.1172/JCI115428",
"author": "JL Curtis",
"doi-asserted-by": "crossref",
"first-page": "1244",
"journal-title": "J Clin Invest",
"key": "307_CR21",
"unstructured": "Curtis JL, Byrd PK, Warnock ML, Kaltreider HB. Requirement of CD4-positive T cells for cellular recruitment to the lungs of mice in response to a particulate intratracheal antigen. J Clin Invest. 1991;88:1244–54.",
"volume": "88",
"year": "1991"
},
{
"DOI": "10.1183/09031936.01.00229601",
"doi-asserted-by": "crossref",
"key": "307_CR22",
"unstructured": "Kips JC. Cytokines in asthma. Eur Respir J. 2001;18:24–33."
},
{
"DOI": "10.1111/j.0105-2896.2004.00215.x",
"author": "M Wills-Karp",
"doi-asserted-by": "crossref",
"first-page": "175",
"journal-title": "Immunol Rev",
"key": "307_CR23",
"unstructured": "Wills-Karp M. Interleukin-13 in asthma pathogenesis. Immunol Rev. 2004;202:175–90.",
"volume": "202",
"year": "2004"
},
{
"DOI": "10.1097/01.all.0000162309.97480.45",
"author": "LP Ngoc",
"doi-asserted-by": "crossref",
"first-page": "161",
"journal-title": "Curr Opin Allergy Clin Immunol",
"key": "307_CR24",
"unstructured": "Ngoc LP, Gold DR, Tzianabos AO, Weiss ST, Celedon JC. Cytokines, allergy, and asthma. Curr Opin Allergy Clin Immunol. 2005;5:161–6.",
"volume": "5",
"year": "2005"
},
{
"DOI": "10.1126/science.282.5397.2258",
"author": "M Wills-Karp",
"doi-asserted-by": "crossref",
"first-page": "2258",
"journal-title": "Science",
"key": "307_CR25",
"unstructured": "Wills-Karp M, Luyimbazi J, Xu X, Schofield B. Interleukin-13: central mediator of allergic asthma. Science. 1998;282:2258–61.",
"volume": "282",
"year": "1998"
},
{
"DOI": "10.1096/fasebj.6.14.1385241",
"author": "J Purkerson",
"doi-asserted-by": "crossref",
"first-page": "3245",
"journal-title": "FASEB J",
"key": "307_CR26",
"unstructured": "Purkerson J, Isakson P. A two-signal model for regulation of immunoglobulin isotype switching. FASEB J. 1992;6:3245–52.",
"volume": "6",
"year": "1992"
},
{
"DOI": "10.1289/ehp.5703",
"author": "I Kimber",
"doi-asserted-by": "crossref",
"first-page": "227",
"journal-title": "Environ Health Perspect",
"key": "307_CR27",
"unstructured": "Kimber I, Stone S, Dearman RJ. Assessment of the inherent allergenic potential of proteins in mice. Environ Health Perspect. 2003;111:227–31.",
"volume": "111",
"year": "2003"
},
{
"author": "RI Abu-Ghazaleh",
"first-page": "137",
"journal-title": "Immunol Ser",
"key": "307_CR28",
"unstructured": "Abu-Ghazaleh RI, Kita H, Gleich GJ. Eosinophil activation and function in health and disease. Immunol Ser. 1992;57:137–67.",
"volume": "57",
"year": "1992"
},
{
"DOI": "10.1126/science.2787531",
"author": "RL Coffman",
"doi-asserted-by": "crossref",
"first-page": "308",
"journal-title": "Science",
"key": "307_CR29",
"unstructured": "Coffman RL, Seymour BW, Hudak S, Jackson J, Rennick D. Antibody to interleukin-5 inhibits helminth-induced eosinophilia in mice. Science. 1898;245:308–10.",
"volume": "245",
"year": "1898"
},
{
"DOI": "10.1016/S1074-7613(00)80294-0",
"author": "M Kopf",
"doi-asserted-by": "crossref",
"first-page": "15",
"journal-title": "Immunity",
"key": "307_CR30",
"unstructured": "Kopf M, Brombacher F, Hodgkin PD, Ramsay AJ, Milbourne EA, Dai WJ, et al. IL-5-deficient mice have a developmental defect in CD5+ B-1 cells and lack eosinophilia but have normal antibody and cytotoxic T cell responses. Immunity. 1996;4:15–24.",
"volume": "4",
"year": "1996"
},
{
"DOI": "10.1084/jem.185.12.2143",
"author": "JJ Lee",
"doi-asserted-by": "crossref",
"first-page": "2143",
"journal-title": "J Exp Med",
"key": "307_CR31",
"unstructured": "Lee JJ, McGarry MP, Farmer SC, Denzler KL, Larson KA, Carrigan PE, et al. Interleukin-5 expression in the lung epithelium of transgenic mice leads to pulmonary changes pathognomonic of asthma. J Exp Med. 1997;185:2143–56.",
"volume": "185",
"year": "1997"
},
{
"DOI": "10.1016/S0163-7258(02)00220-6",
"author": "PS Fostera",
"doi-asserted-by": "crossref",
"first-page": "253",
"journal-title": "Pharmacol Ther",
"key": "307_CR32",
"unstructured": "Fostera PS, Martinez-Moczygembab M, Hustonb DP, Corry DB. Interleukins-4, -5, and -13: emerging therapeutic targets in allergic disease. Pharmacol Ther. 2002;94:253–64.",
"volume": "94",
"year": "2002"
},
{
"DOI": "10.1164/ajrccm/146.3.633",
"author": "BG Toelle",
"doi-asserted-by": "crossref",
"first-page": "633",
"journal-title": "Am Rev Respir Dis",
"key": "307_CR33",
"unstructured": "Toelle BG, Peat JK, Salome CM. Toward a definition of asthma for epidemiology. Am Rev Respir Dis. 1992;146:633–7.",
"volume": "146",
"year": "1992"
},
{
"author": "J Peat",
"first-page": "662",
"journal-title": "Eur Respir J",
"key": "307_CR34",
"unstructured": "Peat J, Toelle B, Salome C. Predictive nature of bronchial responsiveness and respiratory symptoms in a one year cohort study of Sydney schoolchildren. Eur Respir J. 1993;6:662–9.",
"volume": "6",
"year": "1993"
},
{
"DOI": "10.1172/JCI5909",
"author": "Z Zhu",
"doi-asserted-by": "crossref",
"first-page": "779",
"journal-title": "J Clin Invest",
"key": "307_CR35",
"unstructured": "Zhu Z, Homer RJ, Wang Z. Pulmonary expression of interleukin-13 causes inflammation, mucus hypersesretion, subepithelial fibrosis, physiologic abnormalities, and eotaxin production. J Clin Invest. 1999;103:779–88.",
"volume": "103",
"year": "1999"
},
{
"DOI": "10.1016/S0891-5849(96)00501-1",
"author": "L Flohé",
"doi-asserted-by": "crossref",
"first-page": "1115",
"journal-title": "Free Radic Biol Med",
"key": "307_CR36",
"unstructured": "Flohé L, Brigelius-Flohé R, Saliou C, Traber MG, Packer L. Redox regulation of NF-kappa B activation. Free Radic Biol Med. 1997;22:1115–26.",
"volume": "22",
"year": "1997"
},
{
"DOI": "10.1074/jbc.273.6.3285",
"author": "W Berghe Vanden",
"doi-asserted-by": "crossref",
"first-page": "3285",
"journal-title": "J Biol Chem",
"key": "307_CR37",
"unstructured": "Vanden Berghe W, Plaisance S, Boone E, De Bosscher K, Schmitz ML, Fiers W. p38 and extracellular signal-regulated kinase mitogen-activated protein kinase pathways are required for nuclear factor-kappaB p65 transactivation mediated by tumor necrosis factor. J Biol Chem. 1998;273:3285–90.",
"volume": "273",
"year": "1998"
}
],
"reference-count": 37,
"references-count": 37,
"relation": {},
"resource": {
"primary": {
"URL": "http://link.springer.com/10.1007/s00011-011-0307-8"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology",
"Immunology"
],
"subtitle": [],
"title": "Anti-inflammatory effects of ivermectin in mouse model of allergic asthma",
"type": "journal-article",
"volume": "60"
}
