Antiviral Activity of Repurposing Ivermectin against a Panel of 30 Clinical SARS-CoV-2 Strains Belonging to 14 Variants
et al., Pharmaceuticals, doi:10.3390/ph15040445, Apr 2022
Ivermectin for COVID-19
4th treatment shown to reduce risk in
August 2020, now with p < 0.00000000001 from 106 studies, recognized in 24 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
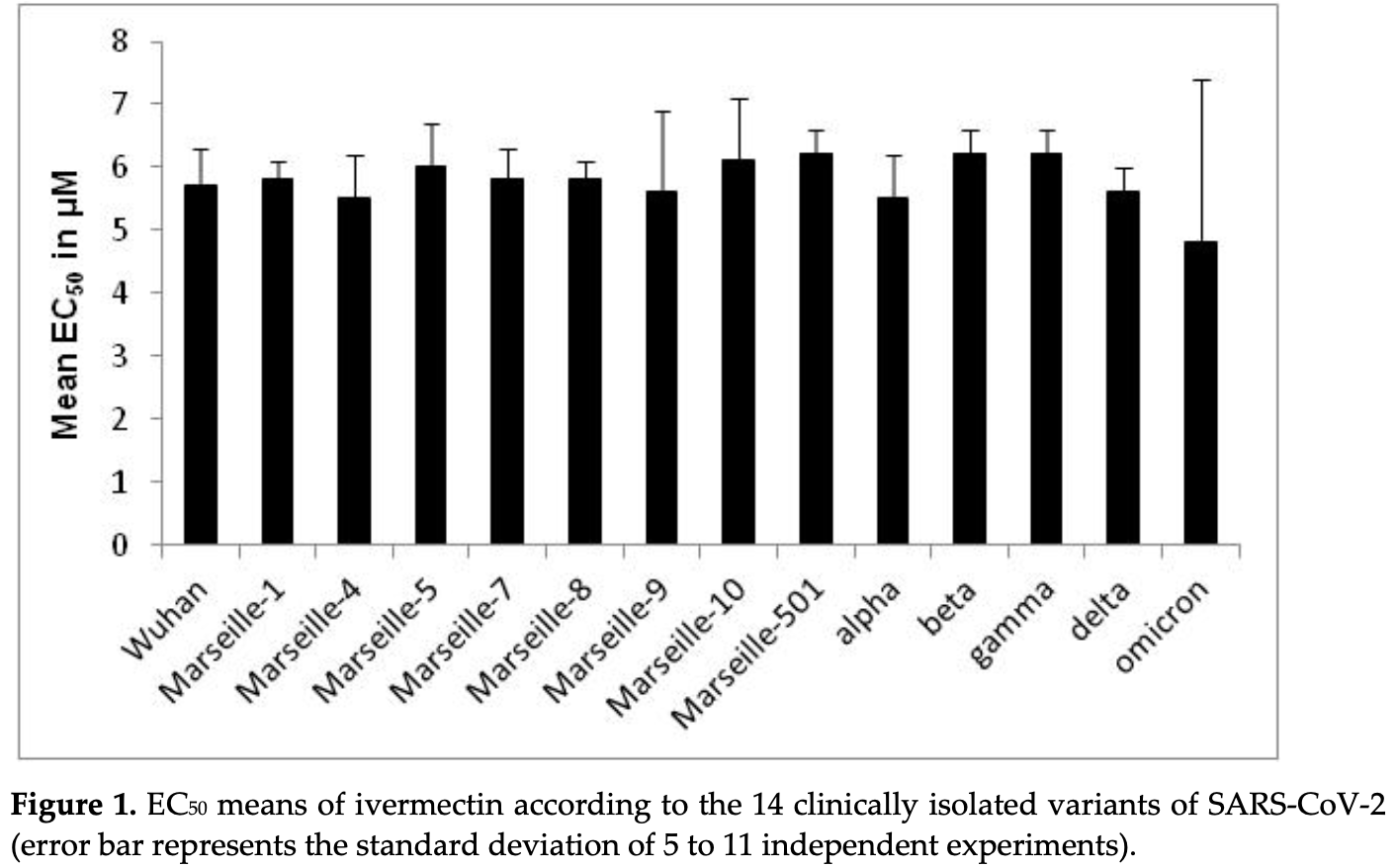
In vitro study with 30 COVID-19 strains from 14 variants, showing stronger efficacy with ivermectin compared to CQ and remdesivir, and relatively homogeneous efficacy with ivermectin regardless of strain/variant, in contrast to results for CQ and remdesivir.
74 preclinical studies support the efficacy of ivermectin for COVID-19:
Ivermectin, better known for antiparasitic activity, is a broad spectrum antiviral with activity against many viruses including H7N771, Dengue37,72,73 , HIV-173, Simian virus 4074, Zika37,75,76 , West Nile76, Yellow Fever77,78, Japanese encephalitis77, Chikungunya78, Semliki Forest virus78, Human papillomavirus57, Epstein-Barr57, BK Polyomavirus79, and Sindbis virus78.
Ivermectin inhibits importin-α/β-dependent nuclear import of viral proteins71,73,74,80 , shows spike-ACE2 disruption at 1nM with microfluidic diffusional sizing38, binds to glycan sites on the SARS-CoV-2 spike protein preventing interaction with blood and epithelial cells and inhibiting hemagglutination41,81, shows dose-dependent inhibition of wildtype and omicron variants36, exhibits dose-dependent inhibition of lung injury61,66, may inhibit SARS-CoV-2 via IMPase inhibition37, may inhibit SARS-CoV-2 induced formation of fibrin clots resistant to degradation9, inhibits SARS-CoV-2 3CLpro54, may inhibit SARS-CoV-2 RdRp activity28, may minimize viral myocarditis by inhibiting NF-κB/p65-mediated inflammation in macrophages60, may be beneficial for COVID-19 ARDS by blocking GSDMD and NET formation82, may interfere with SARS-CoV-2's immune evasion via ORF8 binding4, may inhibit SARS-CoV-2 by disrupting CD147 interaction83-86, may inhibit SARS-CoV-2 attachment to lipid rafts via spike NTD binding2, shows protection against inflammation, cytokine storm, and mortality in an LPS mouse model sharing key pathological features of severe COVID-1959,87, may be beneficial in severe COVID-19 by binding IGF1 to inhibit the promotion of inflammation, fibrosis, and cell proliferation that leads to lung damage8, may minimize SARS-CoV-2 induced cardiac damage40,48, may counter immune evasion by inhibiting NSP15-TBK1/KPNA1 interaction and restoring IRF3 activation88, may disrupt SARS-CoV-2 N and ORF6 protein nuclear transport and their suppression of host interferon responses1, reduces TAZ/YAP nuclear import, relieving SARS-CoV-2-driven suppression of IRF3 and NF-κB antiviral pathways35, increases Bifidobacteria which play a key role in the immune system89, has immunomodulatory51 and anti-inflammatory70,90 properties, and has an extensive and very positive safety profile91.
Study covers ivermectin, HCQ, and remdesivir.
1.
Gayozo et al., Binding affinities analysis of ivermectin, nucleocapsid and ORF6 proteins of SARS-CoV-2 to human importins α isoforms: A computational approach, Biotecnia, doi:10.18633/biotecnia.v27.2485.
2.
Lefebvre et al., Characterization and Fluctuations of an Ivermectin Binding Site at the Lipid Raft Interface of the N-Terminal Domain (NTD) of the Spike Protein of SARS-CoV-2 Variants, Viruses, doi:10.3390/v16121836.
3.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
4.
Bagheri-Far et al., Non-spike protein inhibition of SARS-CoV-2 by natural products through the key mediator protein ORF8, Molecular Biology Research Communications, doi:10.22099/mbrc.2024.50245.2001.
5.
de Oliveira Só et al., In Silico Comparative Analysis of Ivermectin and Nirmatrelvir Inhibitors Interacting with the SARS-CoV-2 Main Protease, Preprints, doi:10.20944/preprints202404.1825.v1.
6.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
7.
Oranu et al., Validation of the binding affinities and stabilities of ivermectin and moxidectin against SARS-CoV-2 receptors using molecular docking and molecular dynamics simulation, GSC Biological and Pharmaceutical Sciences, doi:10.30574/gscbps.2024.26.1.0030.
8.
Zhao et al., Identification of the shared gene signatures between pulmonary fibrosis and pulmonary hypertension using bioinformatics analysis, Frontiers in Immunology, doi:10.3389/fimmu.2023.1197752.
9.
Vottero et al., Computational Prediction of the Interaction of Ivermectin with Fibrinogen, Molecular Sciences, doi:10.3390/ijms241411449.
10.
Chellasamy et al., Docking and molecular dynamics studies of human ezrin protein with a modelled SARS-CoV-2 endodomain and their interaction with potential invasion inhibitors, Journal of King Saud University - Science, doi:10.1016/j.jksus.2022.102277.
11.
Umar et al., Inhibitory potentials of ivermectin, nafamostat, and camostat on spike protein and some nonstructural proteins of SARS-CoV-2: Virtual screening approach, Jurnal Teknologi Laboratorium, doi:10.29238/teknolabjournal.v11i1.344.
12.
Alvarado et al., Interaction of the New Inhibitor Paxlovid (PF-07321332) and Ivermectin With the Monomer of the Main Protease SARS-CoV-2: A Volumetric Study Based on Molecular Dynamics, Elastic Networks, Classical Thermodynamics and SPT, Computational Biology and Chemistry, doi:10.1016/j.compbiolchem.2022.107692.
13.
Aminpour et al., In Silico Analysis of the Multi-Targeted Mode of Action of Ivermectin and Related Compounds, Computation, doi:10.3390/computation10040051.
14.
Parvez et al., Insights from a computational analysis of the SARS-CoV-2 Omicron variant: Host–pathogen interaction, pathogenicity, and possible drug therapeutics, Immunity, Inflammation and Disease, doi:10.1002/iid3.639.
15.
Francés-Monerris et al., Microscopic interactions between ivermectin and key human and viral proteins involved in SARS-CoV-2 infection, Physical Chemistry Chemical Physics, doi:10.1039/D1CP02967C.
16.
González-Paz et al., Comparative study of the interaction of ivermectin with proteins of interest associated with SARS-CoV-2: A computational and biophysical approach, Biophysical Chemistry, doi:10.1016/j.bpc.2021.106677.
17.
González-Paz (B) et al., Structural Deformability Induced in Proteins of Potential Interest Associated with COVID-19 by binding of Homologues present in Ivermectin: Comparative Study Based in Elastic Networks Models, Journal of Molecular Liquids, doi:10.1016/j.molliq.2021.117284.
18.
Rana et al., A Computational Study of Ivermectin and Doxycycline Combination Drug Against SARS-CoV-2 Infection, Research Square, doi:10.21203/rs.3.rs-755838/v1.
19.
Muthusamy et al., Virtual Screening Reveals Potential Anti-Parasitic Drugs Inhibiting the Receptor Binding Domain of SARS-CoV-2 Spike protein, Journal of Virology & Antiviral Research, www.scitechnol.com/abstract/virtual-screening-reveals-potential-antiparasitic-drugs-inhibiting-the-receptor-binding-domain-of-sarscov2-spike-protein-16398.html.
20.
Qureshi et al., Mechanistic insights into the inhibitory activity of FDA approved ivermectin against SARS-CoV-2: old drug with new implications, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1906750.
21.
Schöning et al., Highly-transmissible Variants of SARS-CoV-2 May Be More Susceptible to Drug Therapy Than Wild Type Strains, Research Square, doi:10.21203/rs.3.rs-379291/v1.
22.
Bello et al., Elucidation of the inhibitory activity of ivermectin with host nuclear importin α and several SARS-CoV-2 targets, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1911857.
23.
Udofia et al., In silico studies of selected multi-drug targeting against 3CLpro and nsp12 RNA-dependent RNA-polymerase proteins of SARS-CoV-2 and SARS-CoV, Network Modeling Analysis in Health Informatics and Bioinformatics, doi:10.1007/s13721-021-00299-2.
24.
Choudhury et al., Exploring the binding efficacy of ivermectin against the key proteins of SARS-CoV-2 pathogenesis: an in silico approach, Future Medicine, doi:10.2217/fvl-2020-0342.
25.
Kern et al., Modeling of SARS-CoV-2 Treatment Effects for Informed Drug Repurposing, Frontiers in Pharmacology, doi:10.3389/fphar.2021.625678.
26.
Saha et al., The Binding mechanism of ivermectin and levosalbutamol with spike protein of SARS-CoV-2, Structural Chemistry, doi:10.1007/s11224-021-01776-0.
27.
Eweas et al., Molecular Docking Reveals Ivermectin and Remdesivir as Potential Repurposed Drugs Against SARS-CoV-2, Frontiers in Microbiology, doi:10.3389/fmicb.2020.592908.
28.
Parvez (B) et al., Prediction of potential inhibitors for RNA-dependent RNA polymerase of SARS-CoV-2 using comprehensive drug repurposing and molecular docking approach, International Journal of Biological Macromolecules, doi:10.1016/j.ijbiomac.2020.09.098.
29.
Francés-Monerris (B) et al., Has Ivermectin Virus-Directed Effects against SARS-CoV-2? Rationalizing the Action of a Potential Multitarget Antiviral Agent, ChemRxiv, doi:10.26434/chemrxiv.12782258.v1.
30.
Kalhor et al., Repurposing of the approved small molecule drugs in order to inhibit SARS-CoV-2 S protein and human ACE2 interaction through virtual screening approaches, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2020.1824816.
31.
Swargiary, A., Ivermectin as a promising RNA-dependent RNA polymerase inhibitor and a therapeutic drug against SARS-CoV2: Evidence from in silico studies, Research Square, doi:10.21203/rs.3.rs-73308/v1.
32.
Maurya, D., A Combination of Ivermectin and Doxycycline Possibly Blocks the Viral Entry and Modulate the Innate Immune Response in COVID-19 Patients, American Chemical Society (ACS), doi:10.26434/chemrxiv.12630539.v1.
33.
Lehrer et al., Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2, In Vivo, 34:5, 3023-3026, doi:10.21873/invivo.12134.
34.
Suravajhala et al., Comparative Docking Studies on Curcumin with COVID-19 Proteins, Preprints, doi:10.20944/preprints202005.0439.v3.
35.
Kofler et al., M-Motif, a potential non-conventional NLS in YAP/TAZ and other cellular and viral proteins that inhibits classic protein import, iScience, doi:10.1016/j.isci.2025.112105.
36.
Shahin et al., The selective effect of Ivermectin on different human coronaviruses; in-vitro study, Research Square, doi:10.21203/rs.3.rs-4180797/v1.
37.
Jitobaom et al., Identification of inositol monophosphatase as a broad‐spectrum antiviral target of ivermectin, Journal of Medical Virology, doi:10.1002/jmv.29552.
38.
Fauquet et al., Microfluidic Diffusion Sizing Applied to the Study of Natural Products and Extracts That Modulate the SARS-CoV-2 Spike RBD/ACE2 Interaction, Molecules, doi:10.3390/molecules28248072.
39.
García-Aguilar et al., In Vitro Analysis of SARS-CoV-2 Spike Protein and Ivermectin Interaction, International Journal of Molecular Sciences, doi:10.3390/ijms242216392.
40.
Liu et al., SARS-CoV-2 viral genes Nsp6, Nsp8, and M compromise cellular ATP levels to impair survival and function of human pluripotent stem cell-derived cardiomyocytes, Stem Cell Research & Therapy, doi:10.1186/s13287-023-03485-3.
41.
Boschi et al., SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects, bioRxiv, doi:10.1101/2022.11.24.517882.
42.
De Forni et al., Synergistic drug combinations designed to fully suppress SARS-CoV-2 in the lung of COVID-19 patients, PLoS ONE, doi:10.1371/journal.pone.0276751.
43.
Saha (B) et al., Manipulation of Spray-Drying Conditions to Develop an Inhalable Ivermectin Dry Powder, Pharmaceutics, doi:10.3390/pharmaceutics14071432.
44.
Jitobaom (B) et al., Synergistic anti-SARS-CoV-2 activity of repurposed anti-parasitic drug combinations, BMC Pharmacology and Toxicology, doi:10.1186/s40360-022-00580-8.
45.
Croci et al., Liposomal Systems as Nanocarriers for the Antiviral Agent Ivermectin, International Journal of Biomaterials, doi:10.1155/2016/8043983.
46.
Zheng et al., Red blood cell-hitchhiking mediated pulmonary delivery of ivermectin: Effects of nanoparticle properties, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121719.
47.
Delandre et al., Antiviral Activity of Repurposing Ivermectin against a Panel of 30 Clinical SARS-CoV-2 Strains Belonging to 14 Variants, Pharmaceuticals, doi:10.3390/ph15040445.
48.
Liu (B) et al., Genome-wide analyses reveal the detrimental impacts of SARS-CoV-2 viral gene Orf9c on human pluripotent stem cell-derived cardiomyocytes, Stem Cell Reports, doi:10.1016/j.stemcr.2022.01.014.
49.
Segatori et al., Effect of Ivermectin and Atorvastatin on Nuclear Localization of Importin Alpha and Drug Target Expression Profiling in Host Cells from Nasopharyngeal Swabs of SARS-CoV-2- Positive Patients, Viruses, doi:10.3390/v13102084.
50.
Jitobaom (C) et al., Favipiravir and Ivermectin Showed in Vitro Synergistic Antiviral Activity against SARS-CoV-2, Research Square, doi:10.21203/rs.3.rs-941811/v1.
51.
Munson et al., Niclosamide and ivermectin modulate caspase-1 activity and proinflammatory cytokine secretion in a monocytic cell line, British Society For Nanomedicine Early Career Researcher Summer Meeting, 2021, web.archive.org/web/20230401070026/https://michealmunson.github.io/COVID.pdf.
52.
Mountain Valley MD, Mountain Valley MD Receives Successful Results From BSL-4 COVID-19 Clearance Trial on Three Variants Tested With Ivectosol™, 5/18, www.globenewswire.com/en/news-release/2021/05/18/2231755/0/en/Mountain-Valley-MD-Receives-Successful-Results-From-BSL-4-COVID-19-Clearance-Trial-on-Three-Variants-Tested-With-Ivectosol.html.
53.
Yesilbag et al., Ivermectin also inhibits the replication of bovine respiratory viruses (BRSV, BPIV-3, BoHV-1, BCoV and BVDV) in vitro, Virus Research, doi:10.1016/j.virusres.2021.198384.
54.
Mody et al., Identification of 3-chymotrypsin like protease (3CLPro) inhibitors as potential anti-SARS-CoV-2 agents, Communications Biology, doi:10.1038/s42003-020-01577-x.
55.
Jeffreys et al., Remdesivir-ivermectin combination displays synergistic interaction with improved in vitro activity against SARS-CoV-2, International Journal of Antimicrobial Agents, doi:10.1016/j.ijantimicag.2022.106542.
56.
Surnar et al., Clinically Approved Antiviral Drug in an Orally Administrable Nanoparticle for COVID-19, ACS Pharmacol. Transl. Sci., doi:10.1021/acsptsci.0c00179.
57.
Li et al., Quantitative proteomics reveals a broad-spectrum antiviral property of ivermectin, benefiting for COVID-19 treatment, J. Cellular Physiology, doi:10.1002/jcp.30055.
58.
Caly et al., The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Research, doi:10.1016/j.antiviral.2020.104787.
59.
Zhang et al., Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice, Inflammation Research, doi:10.1007/s00011-008-8007-8.
60.
Gao et al., Ivermectin ameliorates acute myocarditis via the inhibition of importin-mediated nuclear translocation of NF-κB/p65, International Immunopharmacology, doi:10.1016/j.intimp.2024.112073.
61.
Abd-Elmawla et al., Suppression of NLRP3 inflammasome by ivermectin ameliorates bleomycin-induced pulmonary fibrosis, Journal of Zhejiang University-SCIENCE B, doi:10.1631/jzus.B2200385.
62.
Uematsu et al., Prophylactic administration of ivermectin attenuates SARS-CoV-2 induced disease in a Syrian Hamster Model, The Journal of Antibiotics, doi:10.1038/s41429-023-00623-0.
63.
Albariqi et al., Pharmacokinetics and Safety of Inhaled Ivermectin in Mice as a Potential COVID-19 Treatment, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121688.
64.
Errecalde et al., Safety and Pharmacokinetic Assessments of a Novel Ivermectin Nasal Spray Formulation in a Pig Model, Journal of Pharmaceutical Sciences, doi:10.1016/j.xphs.2021.01.017.
65.
Madrid et al., Safety of oral administration of high doses of ivermectin by means of biocompatible polyelectrolytes formulation, Heliyon, doi:10.1016/j.heliyon.2020.e05820.
66.
Ma et al., Ivermectin contributes to attenuating the severity of acute lung injury in mice, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2022.113706.
67.
de Melo et al., Attenuation of clinical and immunological outcomes during SARS-CoV-2 infection by ivermectin, EMBO Mol. Med., doi:10.15252/emmm.202114122.
68.
Arévalo et al., Ivermectin reduces in vivo coronavirus infection in a mouse experimental model, Scientific Reports, doi:10.1038/s41598-021-86679-0.
69.
Chaccour et al., Nebulized ivermectin for COVID-19 and other respiratory diseases, a proof of concept, dose-ranging study in rats, Scientific Reports, doi:10.1038/s41598-020-74084-y.
70.
Yan et al., Anti-inflammatory effects of ivermectin in mouse model of allergic asthma, Inflammation Research, doi:10.1007/s00011-011-0307-8.
71.
Götz et al., Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import, Scientific Reports, doi:10.1038/srep23138.
72.
Tay et al., Nuclear localization of dengue virus (DENV) 1–4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin, Antiviral Research, doi:10.1016/j.antiviral.2013.06.002.
73.
Wagstaff et al., Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus, Biochemical Journal, doi:10.1042/BJ20120150.
74.
Wagstaff (B) et al., An AlphaScreen®-Based Assay for High-Throughput Screening for Specific Inhibitors of Nuclear Import, SLAS Discovery, doi:10.1177/1087057110390360.
75.
Barrows et al., A Screen of FDA-Approved Drugs for Inhibitors of Zika Virus Infection, Cell Host & Microbe, doi:10.1016/j.chom.2016.07.004.
76.
Yang et al., The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer, Antiviral Research, doi:10.1016/j.antiviral.2020.104760.
77.
Mastrangelo et al., Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: new prospects for an old drug, Journal of Antimicrobial Chemotherapy, doi:10.1093/jac/dks147.
78.
Varghese et al., Discovery of berberine, abamectin and ivermectin as antivirals against chikungunya and other alphaviruses, Antiviral Research, doi:10.1016/j.antiviral.2015.12.012.
79.
Bennett et al., Role of a nuclear localization signal on the minor capsid Proteins VP2 and VP3 in BKPyV nuclear entry, Virology, doi:10.1016/j.virol.2014.10.013.
80.
Kosyna et al., The importin α/β-specific inhibitor Ivermectin affects HIF-dependent hypoxia response pathways, Biological Chemistry, doi:10.1515/hsz-2015-0171.
81.
Scheim et al., Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms242317039.
82.
Liu (C) et al., Crosstalk between neutrophil extracellular traps and immune regulation: insights into pathobiology and therapeutic implications of transfusion-related acute lung injury, Frontiers in Immunology, doi:10.3389/fimmu.2023.1324021.
83.
Shouman et al., SARS-CoV-2-associated lymphopenia: possible mechanisms and the role of CD147, Cell Communication and Signaling, doi:10.1186/s12964-024-01718-3.
84.
Scheim (B), D., Ivermectin for COVID-19 Treatment: Clinical Response at Quasi-Threshold Doses Via Hypothesized Alleviation of CD147-Mediated Vascular Occlusion, SSRN, doi:10.2139/ssrn.3636557.
85.
Scheim (C), D., From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate and Then Clot Blood Cells, Center for Open Science, doi:10.31219/osf.io/sgdj2.
86.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
87.
DiNicolantonio et al., Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19, Open Heart, doi:10.1136/openhrt-2020-001350.
88.
Mothae et al., SARS-CoV-2 host-pathogen interactome: insights into more players during pathogenesis, Virology, doi:10.1016/j.virol.2025.110607.
89.
Hazan et al., Treatment with Ivermectin Increases the Population of Bifidobacterium in the Gut, ACG 2023, acg2023posters.eventscribe.net/posterspeakers.asp.
Delandre et al., 2 Apr 2022, peer-reviewed, 12 authors.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Antiviral Activity of Repurposing Ivermectin against a Panel of 30 Clinical SARS-CoV-2 Strains Belonging to 14 Variants
Pharmaceuticals, doi:10.3390/ph15040445
Over the past two years, several variants of SARS-CoV-2 have emerged and spread all over the world. However, infectivity, clinical severity, re-infection, virulence, transmissibility, vaccine responses and escape, and epidemiological aspects have differed between SARS-CoV-2 variants. Currently, very few treatments are recommended against SARS-CoV-2. Identification of effective drugs among repurposing FDA-approved drugs is a rapid, efficient and low-cost strategy against SARS-CoV-2. One of those drugs is ivermectin. Ivermectin is an antihelminthic agent that previously showed in vitro effects against a SARS-CoV-2 isolate (Australia/VI01/2020 isolate) with an IC50 of around 2 µM. We evaluated the in vitro activity of ivermectin on Vero E6 cells infected with 30 clinically isolated SARS-CoV-2 strains belonging to 14 different variants, and particularly 17 strains belonging to six variants of concern (VOC) (variants related to Wuhan, alpha, beta, gamma, delta and omicron). The in vitro activity of ivermectin was compared to those of chloroquine and remdesivir. Unlike chloroquine (EC50 from 4.3 ± 2.5 to 29.3 ± 5.2 µM) or remdesivir (EC50 from 0.4 ± 0.3 to 25.2 ± 9.4 µM), ivermectin showed a relatively homogeneous in vitro activity against SARS-CoV-2 regardless of the strains or variants (EC50 from 5.1 ± 0.5 to 6.7 ± 0.4 µM), except for one omicron strain (EC50 = 1.3 ± 0.5 µM). Ivermectin (No. EC50 = 219, mean EC50 = 5.7 ± 1.0 µM) was, overall, more potent in vitro than chloroquine (No. EC50 = 214, mean EC50 = 16.1 ± 9.0 µM) (p = 1.3 × 10 −34 ) and remdesivir (No. EC50 = 201, mean EC50 = 11.9 ± 10.0 µM) (p = 1.6 × 10 −13 ). These results should be interpreted with caution regarding the potential use of ivermectin in SARS-CoV-2-infected patients: it is difficult to translate in vitro study results into actual clinical treatment in patients.
Supplementary Materials: The following supporting information can be downloaded at: www.mdpi.com/article/10.3390/ph15040445/s1, Table S1 : List of nucleotide and amino acid changes associated with the different SARS-CoV-2 variants.
Conflicts of Interest: The authors declare no conflicts of interest. The findings and conclusion of this report are those of the authors and do not represent the views of the Ministère des Armées and Ministère de l'Enseignement Supérieur, de la Recherche et de l'Innovation.
References
Adhikari, Banerjee, Baidya, Ghosh, Jha, Ligand-based quantitative structural assessements of SARS-CoV-2 3CLpro inhibitors: An analysis in light of structure-based multi-molecular modeling evidences, J. Mol. Struct
Al-Awaida, Al Hourani, Swedan, Nimer, Alzoughool et al., Correlates of SARS-CoV-2 variants on death, case incidence and case fatality ratio among the continents for the period of 1 December 2020 to 15, Genes
Amrane, Tissot-Dupont, Doudier, Eldin, Hocquart et al., Rapid viral diagnosis and ambulatory management of suspected COVID-19 cases presenting at the infectious disease referral hospital in Marseille, France, -January 31st to March 1st, 2020: A respiratory virus snapshot, Travel Med. Infect. Dis
Andreani, Le Bideau, Duflot, Jardot, Rolland et al., In vitro testing of hydroxychloroquine and azithromycin on SARS-CoV-2 shows synergistic effect, Microb. Pathog
Arshed, Pertinez, Box, Tatham, Rajoli et al., priorisation of anti-SARS-CoV-2 drug repurposing opportunities based on plasma and target site concentrations derived from their established human pharmacokinetics, Clin. Pharmacol. Ther
Arévalo, Pagotto, Porfido, Daghero, Segovia et al., Ivermectin reduced in vivo coronavirus in a mouse experimental model, Sci. Rep
Audus, Knaub, Guillot, Schaeffer, The effect of protein binding on ivermectin uptake by bovine brain microvessel endothelial cell, Vet. Res. Commun
Azam, Taban, Eid, Iqbal, Alam et al., An insilico analysis of ivermectin interaction with potential SARS-CoV-2 targets and host nuclear importin α, J. Biomol. Struct. Dyn
Baildya, Ghosh, Chattopadhyay, Inhibitory capacity of chloroquine against SARS-CoV-2 by effective binding with angiotensin converting enzyme-2 receptor: An insight from molecular docking and MD-simulation studies, J. Mol. Struct
Bello, Elucidation of the inhibitory activity of ivermectin with host nuclear importin α and several SARS-CoV-2 targets, J. Biomol. Struct. Dyn
Braz, Silveira, Marinho, De Moraes, Filho et al., In silico study of azithromycin, chloroquine and hydroxychloroquine and their potential mechanisms of action against SARS-CoV-2 infection, Int. J. Antimicrob. Agents
Brown, Won, Graham, Dinnon, Sims et al., Broad spectrum antiviral remdesivir inhibits human endemic and zoonotic deltacoronavirus with a highly divergent RNA dependent RNA polymerase, Antiviral Res
Caly, Druce, Catton, Jans, Wagstaff, The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Anviral Res
Caly, Wagstaff, Jans, Nuclear trafficking of proteins from RNA viruses: Potential target for antivirals, Antiviral Res
Camprubi, Almuedo-Riera, Marti-Soler, Soriano, Hurtado et al., Lack of efficacy of stanadrd doses of ivermectin in severe COVID-19 patients, PLoS ONE
Chaccour, Abizanda, Irigoyen-Barrio, Casellas, Aldaz et al., Nebulized ivermectin for COVID-19 and other respiratory diseases, a proof of concept, does-ranging study in rats, Sci. Rep
Chaccour, Casellas, Matteo, Pineda, Fernandez-Montero et al., The effect of eraly treatment with ivermectin on viral load, symptoms and humoral response in patients with non-severe COVID-19: A pilot, doule-blind, placebo-controlled, randomized clinical trial, EClinicalMedicine
Choudhury, Das, Patra, Bhattacharya, Ghosh et al., Exploring the binding efficacy of ivermectin against the key proteins of SARS-CoV-2 pathogenesis: An in silico approach, Future Virol
Choy, Wong, Kaewpreedee, Sia, Chen et al., lopinavir, emetine, and homoharringtonine inhibit SARS-CoV-2 replication in vitro, Antivir. Res
Colson, Levasseur, Delerce, Pinault, Dudouet et al., Spreading of new SARS-CoV-2 N501Y spike variant in a new lineage, Clin. Microb. Infect
Colson, Levasseur, Gautret, Fenollar, Hoang et al., Introduction into the Marseille geographical area of a mild SARS-CoV-2 variant originating from sub-Saharan Africa: An investigational study, Travel Med. Infect. Dis
Colson, Rolain, Lagier, Brouqui, Raoult, Chloroquine and hydroxychloroquine as available weapons to fight COVID-19, Int. J. Antimicrob. Agents
Dao, Hoang, Colson, Lagier, Million et al., SARS-CoV-2 infectivity and severity of COVID-19 according to SARS-CoV-2 variants: Current evidence, J. Clin. Med
Dao, Hoang, Nguyen, Delerce, Chaudet et al., Clinical outcomes in COVID-19 patients infected with different SARS-CoV-2 variants in Marseille, France, Clin. Microbiol. Infect
Deshpande, Tiwari, Nyayanit, Modak, In silico molecular docking analysis for repurposing therapeutics against multiple proteins from SARS-CoV-2, Eur. J. Pharmacol
Devaux, Rolain, Colson, Raoult, New insights on the antiviral effects of chloroquine against coronavirus: What to expect for COVID-19, Int. J. Antimicrob. Agents
Dittmar, Lee, Whig, Segrist, Li et al., Drug repurposing screens reveal cell-type-specific entry and FDA-approved drugs active against SARS-CoV-2, Cell Rep
Drayman, Jones, Azizi, Froggatt, Tan et al., Drug repurposing screen identifies masitinib as a 3CLpro inhibitor that blocks replication of SARS-CoV-2 in vitro, bioRxiv, doi:10.1101/2020.08.31.274639
Elfiky, Azzam, Shafaa, The anti-HCV, Sofosbuvir, versus the anti-EBOV Remdesivir against SARS-CoV-2 RNA dependent RNA polymerase in silico, Mol. Divers
Errecalde, Lifschitz, Veccioli, Ceballos, Errecalde et al., Safety and phramacokinetic assessments of a novel ivermectin nasal spray formulation in a pig model, J. Pharm. Sci
Eweas, Alhossary, Abdel-Moneim, Molecular docking reveals ivermectin and remdesivir as potential repurposed drugs against SARS-CoV-2, Front. Microbiol
Fantini, Di Scala, Chahinian, Yahi, Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection, Int. J. Antimicrob. Agents
Fantini, Yahi, Colson, Chahinian, La Scola et al., The puzzling mutational landscape of the SARS-2-variant Omicron, J. Med. Virol, doi:10.1002/jmv.27577
Fathizadeh, Afshar, Masoudi, Gholizadeh, Asgharzadeh et al., SARS-CoV-2 (COVID-19) vaccines structure, mechanisms and effectiveness: A review, Int. J. Biol. Macromol, doi:10.1016/j.ijbiomac.2021.08.076
Flanagan, Macintyre, Mcintyre, Nelson, SARS-CoV-2 vaccines: Where are we now?, J. Allergy Clin. Immunol. Pract, doi:10.1016/j.laip.2021.07.016
Fournier, Colson, Levasseur, Devaux, Gautret et al., Emergence and outcomes of the SARS-CoV-2 'Marseille-4' variant, Int. J. Infect. Dis
Galan, Santos, Asato, Araujo, De Lima Moreira et al., Phase 2 randomized study on chloroquine, hydroxychloroquine or ivermectin in hospitalized patients with severe manifestations of SARS-CoV-2 infection, Pathog. Glob. Health
Gautret, Houhamdi, Nguyen, Hoang, Giraud-Gatineau et al., Does SARS-CoV-2 re-infection depend on virus variant?, Clin. Microb. Infect
Gendrot, Andreani, Boxberger, Jardot, Fonta et al., Antimalarial drugs inhibit the replication of SARS-CoV-2: An in vitro evaluation, Travel Med. Infect. Dis
Gendrot, Andreani, Duflot, Boxberger, Le Bideau et al., Methylene blue inhibits replication of SARS-CoV-2 in vitro, Int. J. Antimicrob. Agents
Gendrot, Andreani, Jardot, Hutter, Delandre et al., In vitro antiviral activity of doxycycline against SARS-CoV-2, Molecules
Gendrot, Duflot, Boxberger, Delandre, Jardot et al., Antimalarial artemisinin-based combination therapies (ACT) and COVID-19 in Africa: In vitro inhibition of SARS-CoV-2 replication by mefloquine-artesunate, Int. J. Infect. Dis
Gendrot, Jardot, Delandre, Boxberger, Andreani et al., In vitro evaluation of the antiviral activity of methylene blue alone or in combination against SARS-CoV-2, J. Clin. Med
Gonzalez-Paz, Hurtado-Leon, Lossada, Fernandez-Materan, Vera-Villalobas et al., Comparative study of the interaction of ivermectin with proteins of interest associated with SARS-CoV-2: A computational and biophysical approach, Biophys. Chem
Gordon, Tchesnokov, Woolner, Perry, Feng et al., Remdesivir is a direct-acting antiviral that inhibits RNA-dependent RNA polymerase from severe acute respiratory syndrome coronavirus 2 with high potency, J. Biol. Chem
Gorial, Mashhadani, Sayaly, Dakhil, Almashhadani et al., Effectiveness of Ivermectin as add-on therapy in COVID-19 management, medRxiv, doi:10.1101/2020.07.07.20145979
Haribabu, Garisetti, Malekshah, Srividya, Gayathri et al., Design and synthesis of heteroclic azole based bioactive compounds: Molecular structures, quantum simulation, and mechanistic studies through docking as multi-target inhibitors of QARS-CoV-2 and cytotoxicity, J. Mol. Struct
Heidary, Gharebaghi, Ivermectin: A systematic review from antiviral effects to COVID-19 complementary regimen, J. Antibiot
Hill, Garratt, Levi, Falconner, Ellis et al., Meta-analysis of randomized trials of ivermectin to treat SARS-CoV-2 infection, Open Forum Infect. Dis
Hill, Mirchandani, Pilkington, Ivermectin for COVID-19: Adressing potential bias and medical fraud, Open Forum Infect. Dis
Hoang, Colson, Levasseur, Delerce, Lagier et al., Clinical outcomes in patients infected with different SARS-CoV-2 variants at one hospital during three phases of the COVID-19 epidemic in Marseille. France, Infect. Genet. Evol
Holwerda, V'kovski, Wider, Thiel, Djikman, Identification of an antiviral compound from the pandemic response box that efficiently inhibits SARS-CoV-2 infection in vitro, Microorganisms
Ikegame, Siddiquey, Hung, Haas, Brambilla et al., Neutralizing activity of Sputnik V vaccine sera against SARS-CoV-2 variants, Nat. Commun
Isaac-Lam, Molecular modeling of the interaction of ligands with ACE2-SARS-CoV-2 spike protein complex, Silico Pharmacol
Izcovich, Peiris, Ragusa, Tortosa, Rda et al., Bias as a source of inconsistency in ivermectin trials for COVID-19: A systematic review. Ivermectin's suggested benefits are mainly based on potentially biased results, J. Clin. Epidemiol
Jaafar, Boschi, Aherfi, Bancod, Le Bideau et al., High individual heterogeneity of neutralizing activities against the original strain and nine different variants of SARS-CoV-2, Viruses
Jans, Martin, Wagstaff, Inhibitors of nuclear transport, Curr. Opin. Cell Biol
Jermain, Hanafin, Cao, Lifschitz, Lanusse et al., Development of a minimal physiologically-based pharmacokinetic model to simulate lung exposure in humans following oral administration of ivermectin for COVID-19 drug repurposing, J. Pharm. Sci
Kato, Matsuyama, Kawase, Hishiki, Katoh et al., Antiviral activities of mycophenolic acid and IMD-0354 against SARS-CoV-2, Microbiol. Immunol
Kern, Schöning, Chaccour, Hammann, Modeling of SARS-CoV-2 treatment effects for informed drug repurposing, Front. Pharmacol
Kirti, Roy, Pattadar, Ray, Agarwal et al., Ivermectin as a potential treatment for mild to moderate COVID-19-A double blind randomized placebo-controlled trial, medRxiv, doi:10.1101/2021.01.05.21249310
Ko, Jeon, Ryu, Kim, Comparative analysis of antiviral efficacy of FDA-approved drugs against SARS-CoV-2 in human lung cells, J. Med. Virol
Kumar, Sarma, Kaur, Prajapat, Bhattacharyya et al., Clinically relevant cell culture models and their significance in isolation, pathogenesis, vaccine development, repurposing and screening of nex drugs for SARS-CoV-2: A systematic review, Tissue Cell
Lehrer, Rheinstein, Ivermectin docks to the SARS-CoV-2 spike receptor-binding domain attached to ACE, Vivo
Lim, Hor, Tay, Jelani, Tan et al., Efficacy of ivermectin treatment on disease progression among adults with mild to moderate COVID-19 and comorbidities: The I-TECH randomized clinical trial, JAMA Intern. Med, doi:10.1001/jamainternmed.2022.0189
Lima-Morales, Mendez-Hernandez, Flores, Osorno-Romero, Sancho-Hernandez et al., Effectiveness of multidrug therapy consisting of Ivermectin, Azithromycin, Montelukast, and Acethylsalicylic acid to prevent hospitalization and death among ambulatory COVID-19 cases in Tlaxcala, Mexico, Int. J. Infect. Dis
Lopez-Medina, Lopez, Hurtado, Davalos, Ramirez et al., Effect if ivermectin on time to resolution of symptoms among adults with mild COVID-19, JAMA
Low, Yip, Lal, Repositioning ivermectin for COVID-19 treatment: Molecular mechanisms of action against SARS-CoV-2 replication, Biochim. Biophys. Acta Mol. Basis Dis
Mahmud, Rahman, Alam, Ahmed, Kabir et al., Ivermectin in combination with doxycycline for treating COVID-19 symptoms: A randomized trial, J. Int. Med. Res
Marciniec, Beberok, Boryczka, Wrzesniok, The application of in silico experimental model in the assessement of ciprofloxacin and levofloxacin interaction with man SARS-CoV-2 targets: S-, E-and TMPRSS2 proteins, RNA-dependent RNA polymerase and papain-like protease (PLpro)-Preliminary molecular docking analysis, Pharmacol. Rep
Mody, Ho, Wills, Mawri, Lawson et al., Identification of 3-chymothrypsin like protease (3CLpro) inhibitors as potentail anti-SARS-CoV-2 agents, Commun. Biol
Mohan, Tiwari, Suri, Mittal, Patel et al., Single-dose oral ivermectin in mild and moderate COVID-19 (RIVET-COV): A single-centre randomized, placebo-controlled trial, J. Infect. Chemother
Mohapatra, Perekhoda, Azam, Suleiman, Sarangi et al., Computational investigations of three main drugs and their comparison with synthesized compounds as potent inhibitors of SARS-CoV-2 main protease (Mpro): DFT, QSAR, molecular docking, and in silico toxicity analysis, J. King Saud Univ. Sci
Ozer, Goksu, Conception, Ulker, Balderas et al., Effectiveness and safety of ivermectin in COVID-19 patients: A prospecive study at a safety-net hospital, J. Med. Virol, doi:10.1002/jmv.27469
Parvez, Karim, Hasan, Jaman, Karim et al., Prediction of potential inhibitors for RNA-dependent RNA polymerase of SARS-CoV-2 using comprehensive drug repurposing and molecular docking approach, Int. J. Biol. Macromol
Pena-Silva, Duffull, Steer, Jaramillo-Rincon, Gwee et al., Pharmacokinetic considerations on the repurposing of ivermectin for treatment of COVID-19, Br. J. Clin. Pharmacol
Pires De Souza, Le Bideau, Boschi, Ferreira, Wurtz et al., Emerging SARS-CoV-2 genotypes show different replication patterns in human pulmonary and intestnal epithelial cells, Viruses
Planas, Saunders, Maes, Guivel-Benhassine, Planchais et al., Considerable escape of SARS-CoV-2 Omicron to antibody neutralization, Nature, doi:10.1038/s41586-021-04389-z
Rajter, Sherman, Fatteh, Vogel, Sacks et al., Use of ivermectin is associated with lower mortality in hospitalized patients with coronavirus disease, Chest
Ribaudo, Coghi, Yang, Ng, Mastinu et al., Computational and experimental insights on the interaction of artemisinin, dihydroartemisinin and chloroquine with SARS-CoV-2 spike prtein receptor-binding domain (RBD), Nat. Prod. Res
Saha, Raihan, The binding mechanism of ivermectin and levosalbutamol with spike protein of SARS-CoV-2, Struct. Chem
Sanyaolu, Okorie, Marinkovic, Haider, Abbasi et al., The emerging SARS-CoV-2 variants of concern, Ther. Adv. Infect. Dis
Sarkar, Thakur, Ghadge, Rath, Computational studies reveal Fluorine based quinilines to be potent inhibitors for proteins involved in SARS-CoV-2 assembly, J. Fluor. Chem
Schmith, Zhou, Lohmer, The approved dose of ivermectin alone is not the ideal dose for the treatment of COVID-19, Clin. Pharmacol. Ther
Scola, Lavrad, Fournier, Colson, Lacoste et al., SARS-CoV-2 variant from India to Marseille: The still active role of ports in the introduction of epidemics, Travel Med. Infect. Dis
Segatory, Garona, Caligiuri, Bizzotto, Lavignolle et al., Effect of ivermectin and atorvastatin on nuclear localization of importin Alpha and drug target expression profiling in host cells from nasopharyngeal swabs of SARS-CoV-2-positive patients, Viruses
Sencanski, Perovic, Pajovic, Adzic, Paessler et al., Drug repurposing for candidate SARS-CoV-2 main protease inhibitors by a novel in silico methods, Molecules
Singh, Pandit, Mcarthur, Banerjee, Mossman, Evolutionary trajectory of SARS-CoV-2 and emerging variants, Virol. J
Tada, Zhou, Samanovic, Dcosta, Cornelius et al., Comparison of neutralizing antibody titers elicited by mRNA and adenoviral vector vaccine against SARS-CoV-2 variants, bioRxiv, doi:10.1101/2021.07.19.452771
Tan, Tan, Chu, Chow, Combination treatment with remdesivir and ivermectin exerts highly synergistic and potent antiviral activity against murine coronavirus infection, Front. Cell. Infect. Microbiol
Tregoning, Flight, Higham, Wang, Pierce, Progress of the COVID-19 vaccine effort: Viruses, vaccines and variants versus efficacy, effectiveness and escape, Nat. Rev. Immunol
Tripathi, Upadhyay, Singh, Raghavendhar, Bhardwaj et al., Sreening and evaluation of approved drugs as inhibitors of main protease of SARS-CoV-2, Int. J. Biol. Macromol
Udofia, Gbayo, Oloba-Whenu, Ogunbayo, Isanbor, In silico studies of selected multi-drug targeting against 3CLpro and nsp12 RNA-dependent RNA-polymerase proteins of SARS-CoV-2 and SARS-CoV, Netw. Model. Anal. Health Inform. Bioinform
Vallejos, Zoni, Bangher, Villamandos, Bobadilla et al., Ivermectin to prevent hospitalizations in patients with COVD-19 (IVERCOR-COVID19) a randomized, double-blind, placebo-controlled trial, BMC Infect. Dis
Wagstaff, Sivakumaran, Heaton, Harrich, Jans, Ivermectin is a specific inhibitor of importin α/βmediated nuclear import able to inhibit replication of HIV-1 and dengue virus, Biochem. J
Wang, Cao, Zhang, Yang, Liu et al., Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCov) in vitro, Cell Res
Wang, Chan, Wang, Li, Zhao et al., Orally administered bismuth drug together with N-acetyl cysteine as a broad-spectrum anti-coronavirus therapy, Chem. Sci
Wang, Li, Rajpoot, Saqib, Yu et al., Comparative assessement of favipiravir and remdesivir againt human coronavirus NL63 in molecular docking and cell culture lodels, Sci. Rep
Warren, Jordan, Lo, Ray, Mackman et al., Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys, Nature
Weston, Coleman, Haupt, Logue, Matthews et al., Broad anticoronavirus activity of Food and Drug Administration-approved drugs against SARS-CoV-2 in vitro and SARS-CoV in vivo, J. Virol
Willet, Grove, Maclean, Wilkie, Logan et al., The hyper-transmissible SARS-CoV-2 Omicron variant exhibite significant antigenic change, vaccine escape and a switch in cell entry mechanism, medRxiv, doi:10.1101/2022.01.03.21268111
Wu, Crich, Pegan, Lou, Hansen et al., Polyphenols as potential inhibitors of SARS-CoV-2 RNA dependent RNA polymerase (RdRp), Molecules
Wu, Zhao, Yu, Chen, Wang et al., A new coronavirus associated with human respiratory disease in China, Nature
Wurtz, Penant, Jardot, Duclos, La Scola, Culture of SARS-CoV-2 in a panel of laboratory cell lines, permissivity, and differences in growth profile, Eur. J. Clin. Microbiol. Infect. Dis
Yang, Atkinson, Fraser, Wang, Maher et al., Novel flavivirus antiviral that targets the host nuclear tranmport importin α/β1 heterodimer, Cells
Yang, Atkinson, Wang, Lee, Bogoyevitch et al., The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer, Antiviral Res
Yuan, Yin, Meng, Chan, Ye et al., Clofazimine broadly inhibits coronaviruses including SARS-CoV-2, Nature
Zaidi, Dehgani-Mobaraki, The mechanisms of action against SARS-CoV-2: An evidence-based clinical review article, J. Antibiot
Zhan, Dowell, Shen, Lee, Chloroquine to fight COVID-19: A consideration of mechanisms and adverse effects?, Heliyon
Zhang, Liu, Cao, Xu, Wu et al., Comparative antiviral efficacy of viral protease inhibitors against the novel SARS-CoV-2 in vitro, Virol. Sin
DOI record:
{
"DOI": "10.3390/ph15040445",
"ISSN": [
"1424-8247"
],
"URL": "http://dx.doi.org/10.3390/ph15040445",
"abstract": "<jats:p>Over the past two years, several variants of SARS-CoV-2 have emerged and spread all over the world. However, infectivity, clinical severity, re-infection, virulence, transmissibility, vaccine responses and escape, and epidemiological aspects have differed between SARS-CoV-2 variants. Currently, very few treatments are recommended against SARS-CoV-2. Identification of effective drugs among repurposing FDA-approved drugs is a rapid, efficient and low-cost strategy against SARS-CoV-2. One of those drugs is ivermectin. Ivermectin is an antihelminthic agent that previously showed in vitro effects against a SARS-CoV-2 isolate (Australia/VI01/2020 isolate) with an IC50 of around 2 µM. We evaluated the in vitro activity of ivermectin on Vero E6 cells infected with 30 clinically isolated SARS-CoV-2 strains belonging to 14 different variants, and particularly 17 strains belonging to six variants of concern (VOC) (variants related to Wuhan, alpha, beta, gamma, delta and omicron). The in vitro activity of ivermectin was compared to those of chloroquine and remdesivir. Unlike chloroquine (EC50 from 4.3 ± 2.5 to 29.3 ± 5.2 µM) or remdesivir (EC50 from 0.4 ± 0.3 to 25.2 ± 9.4 µM), ivermectin showed a relatively homogeneous in vitro activity against SARS-CoV-2 regardless of the strains or variants (EC50 from 5.1 ± 0.5 to 6.7 ± 0.4 µM), except for one omicron strain (EC50 = 1.3 ± 0.5 µM). Ivermectin (No. EC50 = 219, mean EC50 = 5.7 ± 1.0 µM) was, overall, more potent in vitro than chloroquine (No. EC50 = 214, mean EC50 = 16.1 ± 9.0 µM) (p = 1.3 × 10−34) and remdesivir (No. EC50 = 201, mean EC50 = 11.9 ± 10.0 µM) (p = 1.6 × 10−13). These results should be interpreted with caution regarding the potential use of ivermectin in SARS-CoV-2-infected patients: it is difficult to translate in vitro study results into actual clinical treatment in patients.</jats:p>",
"alternative-id": [
"ph15040445"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-8794-8923",
"affiliation": [],
"authenticated-orcid": false,
"family": "Delandre",
"given": "Océane",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-2322-5427",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gendrot",
"given": "Mathieu",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Jardot",
"given": "Priscilla",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Le Bideau",
"given": "Marion",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7740-0518",
"affiliation": [],
"authenticated-orcid": false,
"family": "Boxberger",
"given": "Manon",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Boschi",
"given": "Céline",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Fonta",
"given": "Isabelle",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Mosnier",
"given": "Joel",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hutter",
"given": "Sébastien",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Levasseur",
"given": "Anthony",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8006-7704",
"affiliation": [],
"authenticated-orcid": false,
"family": "La Scola",
"given": "Bernard",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2360-3803",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pradines",
"given": "Bruno",
"sequence": "additional"
}
],
"container-title": "Pharmaceuticals",
"container-title-short": "Pharmaceuticals",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
4,
3
]
],
"date-time": "2022-04-03T06:59:52Z",
"timestamp": 1648969192000
},
"deposited": {
"date-parts": [
[
2022,
4,
5
]
],
"date-time": "2022-04-05T10:25:31Z",
"timestamp": 1649154331000
},
"funder": [
{
"DOI": "10.13039/501100001665",
"award": [
"Investissement d'avenir ANR-10-IAHU-03"
],
"doi-asserted-by": "publisher",
"name": "French National Research Agency"
},
{
"award": [
"COVID-19"
],
"name": "Institut hospitalo-universitaire Méditerranée Infection"
}
],
"indexed": {
"date-parts": [
[
2024,
2,
9
]
],
"date-time": "2024-02-09T13:19:30Z",
"timestamp": 1707484770021
},
"is-referenced-by-count": 6,
"issue": "4",
"issued": {
"date-parts": [
[
2022,
4,
2
]
]
},
"journal-issue": {
"issue": "4",
"published-online": {
"date-parts": [
[
2022,
4
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
4,
2
]
],
"date-time": "2022-04-02T00:00:00Z",
"timestamp": 1648857600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1424-8247/15/4/445/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "445",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
4,
2
]
]
},
"published-online": {
"date-parts": [
[
2022,
4,
2
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1038/s41586-020-2008-3",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1186/s12985-021-01633-w",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1177/20499361211024372",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1016/j.jaip.2021.07.016",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1016/j.ijbiomac.2021.08.076",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1016/j.tmaid.2020.101873",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1016/j.ijid.2020.08.032",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1038/s41422-020-0282-0",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.3390/microorganisms8121872",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1016/j.micpath.2020.104228",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.3390/molecules25215064",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.1016/j.antiviral.2020.104786",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1007/s12250-020-00288-1",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1038/s41586-021-03431-4",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1128/JVI.01218-20",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1101/2020.08.31.274639",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1016/j.celrep.2021.108959",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1111/1348-0421.12828",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1002/jmv.26397",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1016/j.ijantimicag.2020.106202",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.3390/jcm10143007",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1039/D1SC04515F",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1038/s41429-020-0336-z",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1038/s41598-021-86679-0",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.3389/fcimb.2021.700502",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1016/j.antiviral.2020.104787",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1016/j.cmi.2021.05.029",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1016/j.cmi.2021.06.029",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.3390/jcm10122635",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1038/s41467-021-24909-9",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1038/s41577-021-00592-1",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.3390/genes12071061",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1101/2021.07.19.452771",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.3390/v13112177",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1002/jmv.27577",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.3390/v14010023",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1038/s41586-021-04389-z",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"article-title": "The mechanisms of action against SARS-CoV-2: An evidence-based clinical review article",
"author": "Zaidi",
"first-page": "1",
"journal-title": "J. Antibiot.",
"key": "ref38",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1016/j.antiviral.2012.06.008",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.3390/cells8030281",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1016/j.ceb.2019.01.001",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1042/BJ20120150",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1016/j.antiviral.2020.104760",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1016/j.bbadis.2021.166294",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1080/07391102.2020.1841028",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1080/07391102.2021.1911857",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1016/j.bpc.2021.106677",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.2217/fvl-2020-0342",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.1007/s13721-021-00299-2",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1016/j.ijbiomac.2020.09.098",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.3389/fmicb.2020.592908",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.1038/nature17180",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.1074/jbc.RA120.013679",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.3390/molecules25173830",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.1038/s42003-020-01577-x",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.1016/j.jksus.2020.101315",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.21873/invivo.12134",
"doi-asserted-by": "publisher",
"key": "ref57"
},
{
"DOI": "10.1007/s11224-021-01776-0",
"doi-asserted-by": "publisher",
"key": "ref58"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105960",
"doi-asserted-by": "publisher",
"key": "ref59"
},
{
"DOI": "10.1016/j.molstruc.2021.129891",
"doi-asserted-by": "publisher",
"key": "ref60"
},
{
"DOI": "10.1080/14786419.2021.1925894",
"doi-asserted-by": "publisher",
"key": "ref61"
},
{
"DOI": "10.1007/s40203-021-00114-w",
"doi-asserted-by": "publisher",
"key": "ref62"
},
{
"DOI": "10.1016/j.molstruc.2021.131782",
"doi-asserted-by": "publisher",
"key": "ref63"
},
{
"DOI": "10.1016/j.jfluchem.2021.109865",
"doi-asserted-by": "publisher",
"key": "ref64"
},
{
"DOI": "10.1007/s43440-021-00282-8",
"article-title": "The application of in silico experimental model in the assessement of ciprofloxacin and levofloxacin interaction with man SARS-CoV-2 targets: S-, E- and TMPRSS2 proteins, RNA-dependent RNA polymerase and papain-like protease (PLpro)—Preliminary molecular docking analysis",
"author": "Marciniec",
"doi-asserted-by": "crossref",
"first-page": "1765",
"journal-title": "Pharmacol. Rep.",
"key": "ref65",
"volume": "73",
"year": "2021"
},
{
"DOI": "10.1016/j.ijbiomac.2020.08.166",
"doi-asserted-by": "publisher",
"key": "ref66"
},
{
"DOI": "10.1016/j.ijantimicag.2020.106119",
"doi-asserted-by": "publisher",
"key": "ref67"
},
{
"DOI": "10.1101/2022.01.03.21268111",
"doi-asserted-by": "publisher",
"key": "ref68"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105932",
"doi-asserted-by": "publisher",
"key": "ref69"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105938",
"doi-asserted-by": "publisher",
"key": "ref70"
},
{
"DOI": "10.1016/j.heliyon.2020.e04900",
"doi-asserted-by": "publisher",
"key": "ref71"
},
{
"DOI": "10.1016/j.antiviral.2019.104541",
"doi-asserted-by": "publisher",
"key": "ref72"
},
{
"DOI": "10.3390/molecules26247438",
"doi-asserted-by": "publisher",
"key": "ref73"
},
{
"DOI": "10.1038/s41598-021-02972-y",
"doi-asserted-by": "publisher",
"key": "ref74"
},
{
"DOI": "10.1007/s11030-020-10178-z",
"doi-asserted-by": "publisher",
"key": "ref75"
},
{
"DOI": "10.1016/j.ejphar.2020.173430",
"doi-asserted-by": "publisher",
"key": "ref76"
},
{
"DOI": "10.1016/j.molstruc.2021.132041",
"doi-asserted-by": "publisher",
"key": "ref77"
},
{
"DOI": "10.1007/BF01839186",
"doi-asserted-by": "publisher",
"key": "ref78"
},
{
"DOI": "10.1111/bcp.14476",
"doi-asserted-by": "publisher",
"key": "ref79"
},
{
"DOI": "10.1016/j.xphs.2020.08.024",
"doi-asserted-by": "publisher",
"key": "ref80"
},
{
"DOI": "10.1002/cpt.1889",
"doi-asserted-by": "publisher",
"key": "ref81"
},
{
"DOI": "10.3389/fphar.2021.625678",
"doi-asserted-by": "publisher",
"key": "ref82"
},
{
"DOI": "10.1002/cpt.1909",
"doi-asserted-by": "publisher",
"key": "ref83"
},
{
"DOI": "10.3390/v13102084",
"doi-asserted-by": "publisher",
"key": "ref84"
},
{
"DOI": "10.1177/03000605211013550",
"doi-asserted-by": "publisher",
"key": "ref85"
},
{
"DOI": "10.1101/2020.07.07.20145979",
"doi-asserted-by": "publisher",
"key": "ref86"
},
{
"DOI": "10.1038/s41598-020-74084-y",
"doi-asserted-by": "publisher",
"key": "ref87"
},
{
"DOI": "10.1016/j.xphs.2021.01.017",
"doi-asserted-by": "publisher",
"key": "ref88"
},
{
"DOI": "10.1371/journal.pone.0242184",
"doi-asserted-by": "publisher",
"key": "ref89"
},
{
"DOI": "10.1080/20477724.2021.1890887",
"doi-asserted-by": "publisher",
"key": "ref90"
},
{
"DOI": "10.1101/2021.01.05.21249310",
"doi-asserted-by": "publisher",
"key": "ref91"
},
{
"DOI": "10.1186/s12879-021-06348-5",
"doi-asserted-by": "publisher",
"key": "ref92"
},
{
"DOI": "10.1001/jama.2021.3071",
"doi-asserted-by": "publisher",
"key": "ref93"
},
{
"DOI": "10.1016/j.jiac.2021.08.021",
"doi-asserted-by": "publisher",
"key": "ref94"
},
{
"DOI": "10.1001/jamainternmed.2022.0189",
"doi-asserted-by": "publisher",
"key": "ref95"
},
{
"DOI": "10.1016/j.ijid.2021.02.014",
"doi-asserted-by": "publisher",
"key": "ref96"
},
{
"DOI": "10.1016/j.eclinm.2020.100720",
"doi-asserted-by": "publisher",
"key": "ref97"
},
{
"DOI": "10.1002/jmv.27469",
"doi-asserted-by": "publisher",
"key": "ref98"
},
{
"DOI": "10.1016/j.chest.2020.10.009",
"doi-asserted-by": "publisher",
"key": "ref99"
},
{
"DOI": "10.1093/ofid/ofab645",
"doi-asserted-by": "publisher",
"key": "ref100"
},
{
"DOI": "10.1016/j.jclinepi.2021.12.018",
"doi-asserted-by": "publisher",
"key": "ref101"
},
{
"DOI": "10.1093/ofid/ofab358",
"doi-asserted-by": "publisher",
"key": "ref102"
},
{
"DOI": "10.1016/j.meegid.2021.105092",
"doi-asserted-by": "publisher",
"key": "ref103"
},
{
"DOI": "10.1016/j.tmaid.2021.101980",
"doi-asserted-by": "publisher",
"key": "ref104"
},
{
"DOI": "10.1016/j.ijid.2021.03.068",
"doi-asserted-by": "publisher",
"key": "ref105"
},
{
"DOI": "10.1016/j.cmi.2021.05.006",
"doi-asserted-by": "publisher",
"key": "ref106"
},
{
"DOI": "10.1016/j.tmaid.2021.102085",
"doi-asserted-by": "publisher",
"key": "ref107"
},
{
"DOI": "10.1007/s10096-020-04106-0",
"doi-asserted-by": "publisher",
"key": "ref108"
},
{
"DOI": "10.1016/j.tice.2021.101497",
"doi-asserted-by": "publisher",
"key": "ref109"
},
{
"DOI": "10.1016/j.tmaid.2020.101632",
"doi-asserted-by": "publisher",
"key": "ref110"
}
],
"reference-count": 110,
"references-count": 110,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1424-8247/15/4/445"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Antiviral Activity of Repurposing Ivermectin against a Panel of 30 Clinical SARS-CoV-2 Strains Belonging to 14 Variants",
"type": "journal-article",
"volume": "15"
}
