Characterization and Fluctuations of an Ivermectin Binding Site at the Lipid Raft Interface of the N-Terminal Domain (NTD) of the Spike Protein of SARS-CoV-2 Variants
et al., Viruses, doi:10.3390/v16121836, Nov 2024
Ivermectin for COVID-19
4th treatment shown to reduce risk in
August 2020, now with p < 0.00000000001 from 106 studies, recognized in 24 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
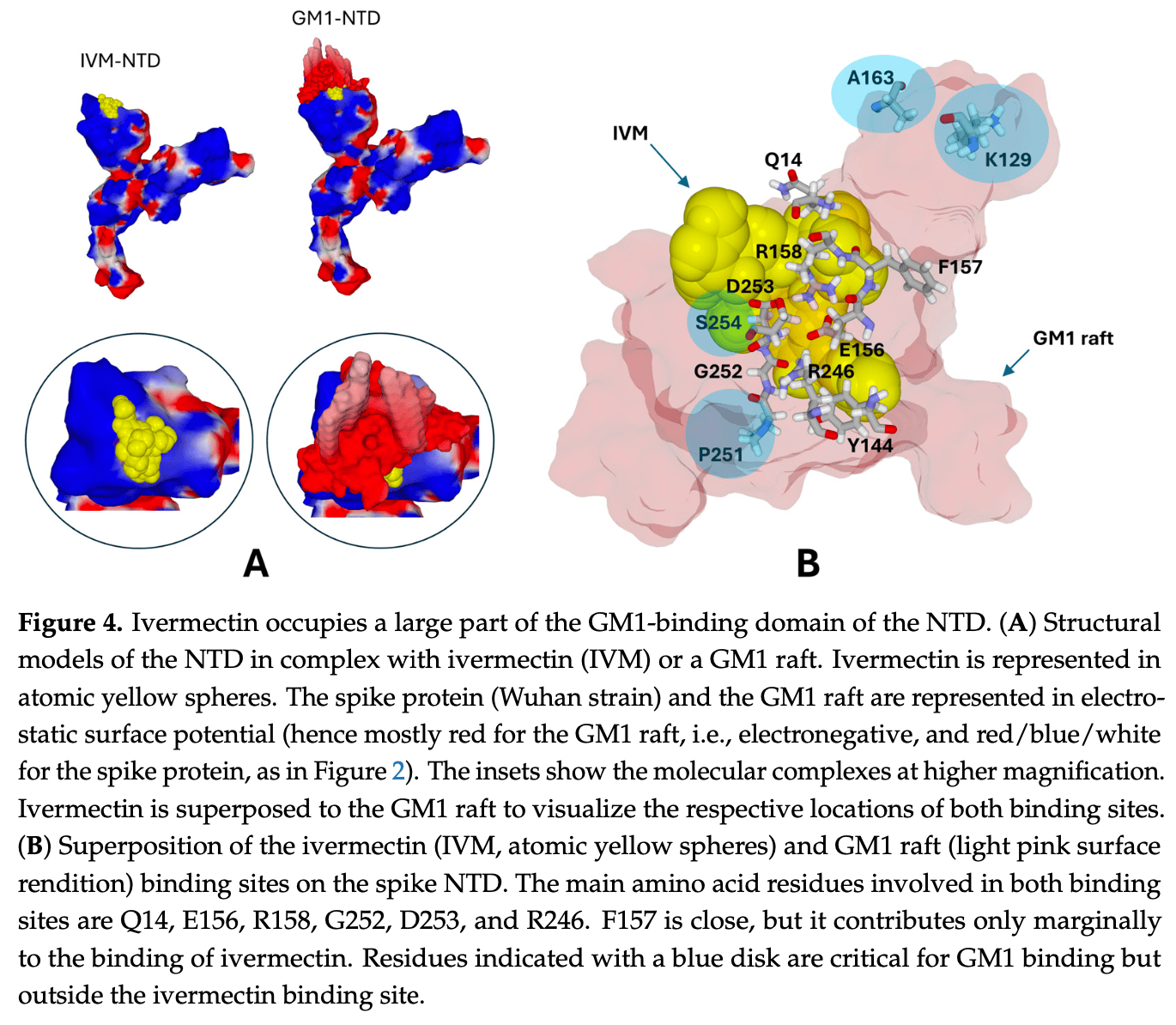
In silico and in vitro study showing that ivermectin binds to the N-terminal domain (NTD) of the spike protein of SARS-CoV-2 variants, potentially inhibiting initial viral attachment to host cell lipid rafts. Authors used molecular modeling to identify an ivermectin binding site on the NTD that overlaps with the ganglioside binding domain. Ivermectin showed flexibility to adapt its binding to variants from the original Wuhan strain to Omicron subvariants. In vitro, ivermectin inhibited the binding of Wuhan and Alpha variant spike protein trimers to GM1 ganglioside monolayers.
74 preclinical studies support the efficacy of ivermectin for COVID-19:
Ivermectin, better known for antiparasitic activity, is a broad spectrum antiviral with activity against many viruses including H7N771, Dengue37,72,73 , HIV-173, Simian virus 4074, Zika37,75,76 , West Nile76, Yellow Fever77,78, Japanese encephalitis77, Chikungunya78, Semliki Forest virus78, Human papillomavirus57, Epstein-Barr57, BK Polyomavirus79, and Sindbis virus78.
Ivermectin inhibits importin-α/β-dependent nuclear import of viral proteins71,73,74,80 , shows spike-ACE2 disruption at 1nM with microfluidic diffusional sizing38, binds to glycan sites on the SARS-CoV-2 spike protein preventing interaction with blood and epithelial cells and inhibiting hemagglutination41,81, shows dose-dependent inhibition of wildtype and omicron variants36, exhibits dose-dependent inhibition of lung injury61,66, may inhibit SARS-CoV-2 via IMPase inhibition37, may inhibit SARS-CoV-2 induced formation of fibrin clots resistant to degradation9, inhibits SARS-CoV-2 3CLpro54, may inhibit SARS-CoV-2 RdRp activity28, may minimize viral myocarditis by inhibiting NF-κB/p65-mediated inflammation in macrophages60, may be beneficial for COVID-19 ARDS by blocking GSDMD and NET formation82, may interfere with SARS-CoV-2's immune evasion via ORF8 binding4, may inhibit SARS-CoV-2 by disrupting CD147 interaction83-86, may inhibit SARS-CoV-2 attachment to lipid rafts via spike NTD binding2, shows protection against inflammation, cytokine storm, and mortality in an LPS mouse model sharing key pathological features of severe COVID-1959,87, may be beneficial in severe COVID-19 by binding IGF1 to inhibit the promotion of inflammation, fibrosis, and cell proliferation that leads to lung damage8, may minimize SARS-CoV-2 induced cardiac damage40,48, may counter immune evasion by inhibiting NSP15-TBK1/KPNA1 interaction and restoring IRF3 activation88, may disrupt SARS-CoV-2 N and ORF6 protein nuclear transport and their suppression of host interferon responses1, reduces TAZ/YAP nuclear import, relieving SARS-CoV-2-driven suppression of IRF3 and NF-κB antiviral pathways35, increases Bifidobacteria which play a key role in the immune system89, has immunomodulatory51 and anti-inflammatory70,90 properties, and has an extensive and very positive safety profile91.
1.
Gayozo et al., Binding affinities analysis of ivermectin, nucleocapsid and ORF6 proteins of SARS-CoV-2 to human importins α isoforms: A computational approach, Biotecnia, doi:10.18633/biotecnia.v27.2485.
2.
Lefebvre et al., Characterization and Fluctuations of an Ivermectin Binding Site at the Lipid Raft Interface of the N-Terminal Domain (NTD) of the Spike Protein of SARS-CoV-2 Variants, Viruses, doi:10.3390/v16121836.
3.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
4.
Bagheri-Far et al., Non-spike protein inhibition of SARS-CoV-2 by natural products through the key mediator protein ORF8, Molecular Biology Research Communications, doi:10.22099/mbrc.2024.50245.2001.
5.
de Oliveira Só et al., In Silico Comparative Analysis of Ivermectin and Nirmatrelvir Inhibitors Interacting with the SARS-CoV-2 Main Protease, Preprints, doi:10.20944/preprints202404.1825.v1.
6.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
7.
Oranu et al., Validation of the binding affinities and stabilities of ivermectin and moxidectin against SARS-CoV-2 receptors using molecular docking and molecular dynamics simulation, GSC Biological and Pharmaceutical Sciences, doi:10.30574/gscbps.2024.26.1.0030.
8.
Zhao et al., Identification of the shared gene signatures between pulmonary fibrosis and pulmonary hypertension using bioinformatics analysis, Frontiers in Immunology, doi:10.3389/fimmu.2023.1197752.
9.
Vottero et al., Computational Prediction of the Interaction of Ivermectin with Fibrinogen, Molecular Sciences, doi:10.3390/ijms241411449.
10.
Chellasamy et al., Docking and molecular dynamics studies of human ezrin protein with a modelled SARS-CoV-2 endodomain and their interaction with potential invasion inhibitors, Journal of King Saud University - Science, doi:10.1016/j.jksus.2022.102277.
11.
Umar et al., Inhibitory potentials of ivermectin, nafamostat, and camostat on spike protein and some nonstructural proteins of SARS-CoV-2: Virtual screening approach, Jurnal Teknologi Laboratorium, doi:10.29238/teknolabjournal.v11i1.344.
12.
Alvarado et al., Interaction of the New Inhibitor Paxlovid (PF-07321332) and Ivermectin With the Monomer of the Main Protease SARS-CoV-2: A Volumetric Study Based on Molecular Dynamics, Elastic Networks, Classical Thermodynamics and SPT, Computational Biology and Chemistry, doi:10.1016/j.compbiolchem.2022.107692.
13.
Aminpour et al., In Silico Analysis of the Multi-Targeted Mode of Action of Ivermectin and Related Compounds, Computation, doi:10.3390/computation10040051.
14.
Parvez et al., Insights from a computational analysis of the SARS-CoV-2 Omicron variant: Host–pathogen interaction, pathogenicity, and possible drug therapeutics, Immunity, Inflammation and Disease, doi:10.1002/iid3.639.
15.
Francés-Monerris et al., Microscopic interactions between ivermectin and key human and viral proteins involved in SARS-CoV-2 infection, Physical Chemistry Chemical Physics, doi:10.1039/D1CP02967C.
16.
González-Paz et al., Comparative study of the interaction of ivermectin with proteins of interest associated with SARS-CoV-2: A computational and biophysical approach, Biophysical Chemistry, doi:10.1016/j.bpc.2021.106677.
17.
González-Paz (B) et al., Structural Deformability Induced in Proteins of Potential Interest Associated with COVID-19 by binding of Homologues present in Ivermectin: Comparative Study Based in Elastic Networks Models, Journal of Molecular Liquids, doi:10.1016/j.molliq.2021.117284.
18.
Rana et al., A Computational Study of Ivermectin and Doxycycline Combination Drug Against SARS-CoV-2 Infection, Research Square, doi:10.21203/rs.3.rs-755838/v1.
19.
Muthusamy et al., Virtual Screening Reveals Potential Anti-Parasitic Drugs Inhibiting the Receptor Binding Domain of SARS-CoV-2 Spike protein, Journal of Virology & Antiviral Research, www.scitechnol.com/abstract/virtual-screening-reveals-potential-antiparasitic-drugs-inhibiting-the-receptor-binding-domain-of-sarscov2-spike-protein-16398.html.
20.
Qureshi et al., Mechanistic insights into the inhibitory activity of FDA approved ivermectin against SARS-CoV-2: old drug with new implications, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1906750.
21.
Schöning et al., Highly-transmissible Variants of SARS-CoV-2 May Be More Susceptible to Drug Therapy Than Wild Type Strains, Research Square, doi:10.21203/rs.3.rs-379291/v1.
22.
Bello et al., Elucidation of the inhibitory activity of ivermectin with host nuclear importin α and several SARS-CoV-2 targets, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1911857.
23.
Udofia et al., In silico studies of selected multi-drug targeting against 3CLpro and nsp12 RNA-dependent RNA-polymerase proteins of SARS-CoV-2 and SARS-CoV, Network Modeling Analysis in Health Informatics and Bioinformatics, doi:10.1007/s13721-021-00299-2.
24.
Choudhury et al., Exploring the binding efficacy of ivermectin against the key proteins of SARS-CoV-2 pathogenesis: an in silico approach, Future Medicine, doi:10.2217/fvl-2020-0342.
25.
Kern et al., Modeling of SARS-CoV-2 Treatment Effects for Informed Drug Repurposing, Frontiers in Pharmacology, doi:10.3389/fphar.2021.625678.
26.
Saha et al., The Binding mechanism of ivermectin and levosalbutamol with spike protein of SARS-CoV-2, Structural Chemistry, doi:10.1007/s11224-021-01776-0.
27.
Eweas et al., Molecular Docking Reveals Ivermectin and Remdesivir as Potential Repurposed Drugs Against SARS-CoV-2, Frontiers in Microbiology, doi:10.3389/fmicb.2020.592908.
28.
Parvez (B) et al., Prediction of potential inhibitors for RNA-dependent RNA polymerase of SARS-CoV-2 using comprehensive drug repurposing and molecular docking approach, International Journal of Biological Macromolecules, doi:10.1016/j.ijbiomac.2020.09.098.
29.
Francés-Monerris (B) et al., Has Ivermectin Virus-Directed Effects against SARS-CoV-2? Rationalizing the Action of a Potential Multitarget Antiviral Agent, ChemRxiv, doi:10.26434/chemrxiv.12782258.v1.
30.
Kalhor et al., Repurposing of the approved small molecule drugs in order to inhibit SARS-CoV-2 S protein and human ACE2 interaction through virtual screening approaches, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2020.1824816.
31.
Swargiary, A., Ivermectin as a promising RNA-dependent RNA polymerase inhibitor and a therapeutic drug against SARS-CoV2: Evidence from in silico studies, Research Square, doi:10.21203/rs.3.rs-73308/v1.
32.
Maurya, D., A Combination of Ivermectin and Doxycycline Possibly Blocks the Viral Entry and Modulate the Innate Immune Response in COVID-19 Patients, American Chemical Society (ACS), doi:10.26434/chemrxiv.12630539.v1.
33.
Lehrer et al., Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2, In Vivo, 34:5, 3023-3026, doi:10.21873/invivo.12134.
34.
Suravajhala et al., Comparative Docking Studies on Curcumin with COVID-19 Proteins, Preprints, doi:10.20944/preprints202005.0439.v3.
35.
Kofler et al., M-Motif, a potential non-conventional NLS in YAP/TAZ and other cellular and viral proteins that inhibits classic protein import, iScience, doi:10.1016/j.isci.2025.112105.
36.
Shahin et al., The selective effect of Ivermectin on different human coronaviruses; in-vitro study, Research Square, doi:10.21203/rs.3.rs-4180797/v1.
37.
Jitobaom et al., Identification of inositol monophosphatase as a broad‐spectrum antiviral target of ivermectin, Journal of Medical Virology, doi:10.1002/jmv.29552.
38.
Fauquet et al., Microfluidic Diffusion Sizing Applied to the Study of Natural Products and Extracts That Modulate the SARS-CoV-2 Spike RBD/ACE2 Interaction, Molecules, doi:10.3390/molecules28248072.
39.
García-Aguilar et al., In Vitro Analysis of SARS-CoV-2 Spike Protein and Ivermectin Interaction, International Journal of Molecular Sciences, doi:10.3390/ijms242216392.
40.
Liu et al., SARS-CoV-2 viral genes Nsp6, Nsp8, and M compromise cellular ATP levels to impair survival and function of human pluripotent stem cell-derived cardiomyocytes, Stem Cell Research & Therapy, doi:10.1186/s13287-023-03485-3.
41.
Boschi et al., SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects, bioRxiv, doi:10.1101/2022.11.24.517882.
42.
De Forni et al., Synergistic drug combinations designed to fully suppress SARS-CoV-2 in the lung of COVID-19 patients, PLoS ONE, doi:10.1371/journal.pone.0276751.
43.
Saha (B) et al., Manipulation of Spray-Drying Conditions to Develop an Inhalable Ivermectin Dry Powder, Pharmaceutics, doi:10.3390/pharmaceutics14071432.
44.
Jitobaom (B) et al., Synergistic anti-SARS-CoV-2 activity of repurposed anti-parasitic drug combinations, BMC Pharmacology and Toxicology, doi:10.1186/s40360-022-00580-8.
45.
Croci et al., Liposomal Systems as Nanocarriers for the Antiviral Agent Ivermectin, International Journal of Biomaterials, doi:10.1155/2016/8043983.
46.
Zheng et al., Red blood cell-hitchhiking mediated pulmonary delivery of ivermectin: Effects of nanoparticle properties, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121719.
47.
Delandre et al., Antiviral Activity of Repurposing Ivermectin against a Panel of 30 Clinical SARS-CoV-2 Strains Belonging to 14 Variants, Pharmaceuticals, doi:10.3390/ph15040445.
48.
Liu (B) et al., Genome-wide analyses reveal the detrimental impacts of SARS-CoV-2 viral gene Orf9c on human pluripotent stem cell-derived cardiomyocytes, Stem Cell Reports, doi:10.1016/j.stemcr.2022.01.014.
49.
Segatori et al., Effect of Ivermectin and Atorvastatin on Nuclear Localization of Importin Alpha and Drug Target Expression Profiling in Host Cells from Nasopharyngeal Swabs of SARS-CoV-2- Positive Patients, Viruses, doi:10.3390/v13102084.
50.
Jitobaom (C) et al., Favipiravir and Ivermectin Showed in Vitro Synergistic Antiviral Activity against SARS-CoV-2, Research Square, doi:10.21203/rs.3.rs-941811/v1.
51.
Munson et al., Niclosamide and ivermectin modulate caspase-1 activity and proinflammatory cytokine secretion in a monocytic cell line, British Society For Nanomedicine Early Career Researcher Summer Meeting, 2021, web.archive.org/web/20230401070026/https://michealmunson.github.io/COVID.pdf.
52.
Mountain Valley MD, Mountain Valley MD Receives Successful Results From BSL-4 COVID-19 Clearance Trial on Three Variants Tested With Ivectosol™, 5/18, www.globenewswire.com/en/news-release/2021/05/18/2231755/0/en/Mountain-Valley-MD-Receives-Successful-Results-From-BSL-4-COVID-19-Clearance-Trial-on-Three-Variants-Tested-With-Ivectosol.html.
53.
Yesilbag et al., Ivermectin also inhibits the replication of bovine respiratory viruses (BRSV, BPIV-3, BoHV-1, BCoV and BVDV) in vitro, Virus Research, doi:10.1016/j.virusres.2021.198384.
54.
Mody et al., Identification of 3-chymotrypsin like protease (3CLPro) inhibitors as potential anti-SARS-CoV-2 agents, Communications Biology, doi:10.1038/s42003-020-01577-x.
55.
Jeffreys et al., Remdesivir-ivermectin combination displays synergistic interaction with improved in vitro activity against SARS-CoV-2, International Journal of Antimicrobial Agents, doi:10.1016/j.ijantimicag.2022.106542.
56.
Surnar et al., Clinically Approved Antiviral Drug in an Orally Administrable Nanoparticle for COVID-19, ACS Pharmacol. Transl. Sci., doi:10.1021/acsptsci.0c00179.
57.
Li et al., Quantitative proteomics reveals a broad-spectrum antiviral property of ivermectin, benefiting for COVID-19 treatment, J. Cellular Physiology, doi:10.1002/jcp.30055.
58.
Caly et al., The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Research, doi:10.1016/j.antiviral.2020.104787.
59.
Zhang et al., Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice, Inflammation Research, doi:10.1007/s00011-008-8007-8.
60.
Gao et al., Ivermectin ameliorates acute myocarditis via the inhibition of importin-mediated nuclear translocation of NF-κB/p65, International Immunopharmacology, doi:10.1016/j.intimp.2024.112073.
61.
Abd-Elmawla et al., Suppression of NLRP3 inflammasome by ivermectin ameliorates bleomycin-induced pulmonary fibrosis, Journal of Zhejiang University-SCIENCE B, doi:10.1631/jzus.B2200385.
62.
Uematsu et al., Prophylactic administration of ivermectin attenuates SARS-CoV-2 induced disease in a Syrian Hamster Model, The Journal of Antibiotics, doi:10.1038/s41429-023-00623-0.
63.
Albariqi et al., Pharmacokinetics and Safety of Inhaled Ivermectin in Mice as a Potential COVID-19 Treatment, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121688.
64.
Errecalde et al., Safety and Pharmacokinetic Assessments of a Novel Ivermectin Nasal Spray Formulation in a Pig Model, Journal of Pharmaceutical Sciences, doi:10.1016/j.xphs.2021.01.017.
65.
Madrid et al., Safety of oral administration of high doses of ivermectin by means of biocompatible polyelectrolytes formulation, Heliyon, doi:10.1016/j.heliyon.2020.e05820.
66.
Ma et al., Ivermectin contributes to attenuating the severity of acute lung injury in mice, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2022.113706.
67.
de Melo et al., Attenuation of clinical and immunological outcomes during SARS-CoV-2 infection by ivermectin, EMBO Mol. Med., doi:10.15252/emmm.202114122.
68.
Arévalo et al., Ivermectin reduces in vivo coronavirus infection in a mouse experimental model, Scientific Reports, doi:10.1038/s41598-021-86679-0.
69.
Chaccour et al., Nebulized ivermectin for COVID-19 and other respiratory diseases, a proof of concept, dose-ranging study in rats, Scientific Reports, doi:10.1038/s41598-020-74084-y.
70.
Yan et al., Anti-inflammatory effects of ivermectin in mouse model of allergic asthma, Inflammation Research, doi:10.1007/s00011-011-0307-8.
71.
Götz et al., Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import, Scientific Reports, doi:10.1038/srep23138.
72.
Tay et al., Nuclear localization of dengue virus (DENV) 1–4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin, Antiviral Research, doi:10.1016/j.antiviral.2013.06.002.
73.
Wagstaff et al., Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus, Biochemical Journal, doi:10.1042/BJ20120150.
74.
Wagstaff (B) et al., An AlphaScreen®-Based Assay for High-Throughput Screening for Specific Inhibitors of Nuclear Import, SLAS Discovery, doi:10.1177/1087057110390360.
75.
Barrows et al., A Screen of FDA-Approved Drugs for Inhibitors of Zika Virus Infection, Cell Host & Microbe, doi:10.1016/j.chom.2016.07.004.
76.
Yang et al., The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer, Antiviral Research, doi:10.1016/j.antiviral.2020.104760.
77.
Mastrangelo et al., Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: new prospects for an old drug, Journal of Antimicrobial Chemotherapy, doi:10.1093/jac/dks147.
78.
Varghese et al., Discovery of berberine, abamectin and ivermectin as antivirals against chikungunya and other alphaviruses, Antiviral Research, doi:10.1016/j.antiviral.2015.12.012.
79.
Bennett et al., Role of a nuclear localization signal on the minor capsid Proteins VP2 and VP3 in BKPyV nuclear entry, Virology, doi:10.1016/j.virol.2014.10.013.
80.
Kosyna et al., The importin α/β-specific inhibitor Ivermectin affects HIF-dependent hypoxia response pathways, Biological Chemistry, doi:10.1515/hsz-2015-0171.
81.
Scheim et al., Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms242317039.
82.
Liu (C) et al., Crosstalk between neutrophil extracellular traps and immune regulation: insights into pathobiology and therapeutic implications of transfusion-related acute lung injury, Frontiers in Immunology, doi:10.3389/fimmu.2023.1324021.
83.
Shouman et al., SARS-CoV-2-associated lymphopenia: possible mechanisms and the role of CD147, Cell Communication and Signaling, doi:10.1186/s12964-024-01718-3.
84.
Scheim (B), D., Ivermectin for COVID-19 Treatment: Clinical Response at Quasi-Threshold Doses Via Hypothesized Alleviation of CD147-Mediated Vascular Occlusion, SSRN, doi:10.2139/ssrn.3636557.
85.
Scheim (C), D., From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate and Then Clot Blood Cells, Center for Open Science, doi:10.31219/osf.io/sgdj2.
86.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
87.
DiNicolantonio et al., Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19, Open Heart, doi:10.1136/openhrt-2020-001350.
88.
Mothae et al., SARS-CoV-2 host-pathogen interactome: insights into more players during pathogenesis, Virology, doi:10.1016/j.virol.2025.110607.
89.
Hazan et al., Treatment with Ivermectin Increases the Population of Bifidobacterium in the Gut, ACG 2023, acg2023posters.eventscribe.net/posterspeakers.asp.
Lefebvre et al., 27 Nov 2024, France, peer-reviewed, 4 authors.
Contact: jacques.fantini@univ-amu.fr (corresponding author), marinelfv@gmail.com, bernard.la-scola@univ-amu.fr, henrichahinian@gmail.com.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Characterization and Fluctuations of an Ivermectin Binding Site at the Lipid Raft Interface of the N-Terminal Domain (NTD) of the Spike Protein of SARS-CoV-2 Variants
Viruses, doi:10.3390/v16121836
Most studies on the docking of ivermectin on the spike protein of SARS-CoV-2 concern the receptor binding domain (RBD) and, more precisely, the RBD interface recognized by the ACE2 receptor. The N-terminal domain (NTD), which controls the initial attachment of the virus to lipid raft gangliosides, has not received the attention it deserves. In this study, we combined molecular modeling and physicochemical approaches to analyze the mode of interaction of ivermectin with the interface of the NTD-facing lipid rafts of the host cell membrane. We characterize a binding area that presents point mutations and deletions in successive SARS-CoV-2 variants from the initial strain to omicron KP.3 circulating in many countries in 2024. We show that ivermectin has exceptional flexibility, allowing the drug to bind to the spike protein of all variants tested. The energy of interaction is specific to each variant, allowing a classification according to their affinity for ivermectin in the following ascending order: Omicron KP.3 < Delta < Omicron BA.5 < Alpha < Wuhan (B.1) < Omicron BA.1. The binding site of ivermectin is subject to important variations of the NTD, including the Y144 deletion. It overlaps with the ganglioside binding domain of the NTD, as demonstrated by docking and physicochemical studies. These results suggest a new mechanism of antiviral action for ivermectin based on competitive inhibition for initial virus attachment to lipid rafts. The current KP.3 variant is still recognized by ivermectin, although with an affinity slightly lower than the Wuhan strain.
Conflicts of Interest: The authors declare no conflicts of interest. Viruses 2024, 16, 1836
References
Allen, Introduction to molecular dynamics simulation, Comput. Soft Matter Synth. Polym. Proteins
Alonso, Bliznyuk, Gready, Combining docking and molecular dynamic simulations in drug design, Med. Res. Rev, doi:10.1002/med.20067
Amanat, Thapa, Lei, Ahmed, Adelsberg et al., SARS-CoV-2 mRNA vaccination induces functionally diverse antibodies to NTD, RBD, and S2, Cell, doi:10.1016/j.cell.2021.06.005
Aminpour, Cannariato, Preto, Safaeeardebili, Moracchiato et al., In silico analysis of the multi-targeted mode of action of ivermectin and related compounds, Computation, doi:10.3390/computation10040051
Andreani, Le Bideau, Duflot, Jardot, Rolland et al., In vitro testing of combined hydroxychloroquine and azithromycin on SARS-CoV-2 shows synergistic effect, Microb. Pathog, doi:10.1016/j.micpath.2020.104228
Andrei, Conjugate Gradient Methods
Ayodele, Bamigbade, Bamigbade, Adeniyi, Tachin et al., Illustrated Procedure to Perform Molecular Docking Using PyRx and Biovia Discovery Studio Visualizer: A Case Study of 10kt With Atropine, Prog. Drug Discov. Biomed. Sci, doi:10.36877/pddbs.a0000424
Borcik, Eason, Yekefallah, Amani, Han et al., A cholesterol dimer stabilizes the inactivated state of an inward-rectifier Potassium Channel, Angew. Chem. Int. Ed, doi:10.1002/anie.202112232
Borges-Araújo, Patmanidis, Singh, Santos, Sieradzan et al., Pragmatic coarse-graining of proteins: Models and applications, J. Chem. Theory Comput, doi:10.1021/acs.jctc.3c00733
Boschi, Scheim, Bancod, Militello, Bideau et al., SARS-CoV-2 spike protein induces hemagglutination: Implications for COVID-19 morbidities and therapeutics and for vaccine adverse effects, Int. J. Mol. Sci, doi:10.3390/ijms232415480
Branda, Ciccozzi, Scarpa, Features of the SARS-CoV-2 KP. 3 variant mutations, Infect. Dis, doi:10.1080/23744235.2024.2385500
Buttenschoen, Morris, Deane, Posebusters, AI-based docking methods fail to generate physically valid poses or generalise to novel sequences, Chem. Sci, doi:10.1039/D3SC04185A
Caly, Druce, Catton, Jans, Wagstaff, The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antivir. Res, doi:10.1016/j.antiviral.2020.104787
Changeux, Edelstein, Conformational selection or induced fit? 50 years of debate resolved, Biol. Rep, doi:10.3410/B3-19
Chen, Beware of docking! Trends, Pharmacol. Sci, doi:10.1016/j.tips.2014.12.001
Choudhury, Das, Patra, Bhattacharya, Ghosh et al., Exploring the binding efficacy of ivermectin against the key proteins of SARS-CoV-2 pathogenesis: An in silico approach, Future Virol, doi:10.2217/fvl-2020-0342
Di Scala, Fantini, Hybrid In Silico/In Vitro Approaches for the Identification of Functional Cholesterol-Binding Domains in Membrane Proteins, Methods Mol. Biol, doi:10.1007/978-1-4939-6875-6_2
Di Scala, Troadec, Lelièvre, Garmy, Fantini et al., Mechanism of cholesterol-assisted oligomeric channel formation by a short Alzheimer β-amyloid peptide, J. Neurochem, doi:10.1111/jnc.12390
Dima, Salvagno, Lippi, Effects of recombinant SARS-CoV-2 spike protein variants on red blood cells parameters and red blood cell distribution width, Biomed. J, doi:10.1016/j.bj.2024.100787
Diociaiuti, Giordani, Kamel, Brasili, Sennato et al., Monosialoganglioside-GM1 triggers binding of the amyloid-protein salmon calcitonin to a Langmuir membrane model mimicking the occurrence of lipid-rafts, Biochem. Biophys. Rep, doi:10.1016/j.bbrep.2016.10.005
Elderdfi, Sikorski, Langmuir-monolayer methodologies for characterizing protein-lipid interactions, Chem. Phys. Lipids, doi:10.1016/j.chemphyslip.2018.01.008
Ewing, Makino, Skillman, Kuntz, Dock, 4.0: Search strategies for automated molecular docking of flexible molecule databases, J. Comput.-Aided Mol. Des, doi:10.1023/A:1011115820450
Fantini, Azzaz, Chahinian, Yahi, Electrostatic Surface Potential as a Key Parameter in Virus Transmission and Evolution: How to Manage Future Virus Pandemics in the Post-COVID-19 Era, Viruses, doi:10.3390/v15020284
Fantini, Chahinian, Yahi, Convergent Evolution Dynamics of SARS-CoV-2 and HIV Surface Envelope Glycoproteins Driven by Host Cell Surface Receptors and Lipid Rafts: Lessons for the Future, Int. J. Mol. Sci, doi:10.3390/ijms24031923
Fantini, Chahinian, Yahi, Leveraging coronavirus binding to gangliosides for innovative vaccine and therapeutic strategies against COVID-19, Biochem. Biophys. Res. Commun, doi:10.1016/j.bbrc.2020.10.015
Fantini, Chahinian, Yahi, Synergistic antiviral effect of hydroxychloroquine and azithromycin in combination against SARS-CoV-2: What molecular dynamics studies of virus-host interactions reveal, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2020.106020
Fantini, Di Scala, Chahinian, Yahi, Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection, Int. J. Antimicrob. Agents, doi:10.1016/j.ijantimicag.2020.105960
Fantini, Fundamental Mechanisms in Membrane Receptology: Old Paradigms, New Concepts and Perspectives, Receptors, doi:10.3390/receptors3010006
Fantini, Lipid rafts and human diseases: Why we need to target gangliosides, FEBS Open Bio, doi:10.1002/2211-5463.13612
Fantini, Yahi, Azzaz, Chahinian, Structural dynamics of SARS-CoV-2 variants: A health monitoring strategy for anticipating Covid-19 outbreaks, J. Infect, doi:10.1016/j.jinf.2021.06.001
Fantini, Yahi, Colson, Chahinian, La Scola et al., The puzzling mutational landscape of the SARS-2-variant Omicron, J. Med. Virol, doi:10.1002/jmv.27577
Gaetano, Capasso, Delre, Pirone, Saviano et al., More Is Always Better Than One: The N-Terminal Domain of the Spike Protein as Another Emerging Target for Hampering the SARS-CoV-2 Attachment to Host Cells, Int. J. Mol. Sci, doi:10.3390/ijms22126462
Ghoula, Naceri, Sitruk, Flatters, Moroy et al., Identifying promising druggable binding sites and their flexibility to target the receptor-binding domain of SARS-CoV-2 spike protein, Comput. Struct. Biotechnol. J, doi:10.1016/j.csbj.2023.03.029
Gianni, Dogan, Jemth, Distinguishing induced fit from conformational selection, Biophys. Chem, doi:10.1016/j.bpc.2014.03.003
Grippo, Lucidi, A globally convergent version of the Polak-Ribiere conjugate gradient method, Math. Program, doi:10.1007/BF02614362
Guex, Peitsch, SWISS-MODEL and the Swiss-Pdb Viewer: An environment for comparative protein modeling, Electrophoresis, doi:10.1002/elps.1150181505
Gyselinck, Janssens, Verhamme, Vos, Rationale for azithromycin in COVID-19: An overview of existing evidence, BMJ Open Respir. Res, doi:10.1136/bmjresp-2020-000806
Huang, Kalyanaraman, Bernacki, Jacobson, Molecular mechanics methods for predicting protein-ligand binding, Phys. Chem. Chem. Phys. PCCP, doi:10.1039/B608269F
Huang, Wong, Wheeler, Flexible protein-flexible ligand docking with disrupted velocity simulated annealing, Proteins, doi:10.1002/prot.21781
Islas, Scior, Allosteric Binding of MDMA to the Human Serotonin Transporter (hSERT) via Ensemble Binding Space Analysis with ∆G Calculations, Induced Fit Docking and Monte Carlo Simulations, Molecules, doi:10.3390/molecules27092977
Jaafar, Boschi, Aherfi, Bancod, Le Bideau et al., High individual heterogeneity of neutralizing activities against the original strain and nine different variants of SARS-CoV-2, Viruses, doi:10.3390/v13112177
Kaku, Uriu, Kosugi, Okumura, Yamasoba et al., Virological characteristics of the SARS-CoV-2 KP. 2 variant, Lancet Infect. Dis, doi:10.1016/S1473-3099(24)00298-6
Kaku, Yo, Tolentino, Uriu, Okumura et al., Virological characteristics of the SARS-CoV-2 KP. 3, LB. 1, and KP. 2.3 variants, Lancet Infect. Dis, doi:10.1016/S1473-3099(24)00415-8
Kharche, Sengupta, Dynamic protein interfaces and conformational landscapes of membrane protein complexes, Curr. Opin. Struct. Biol, doi:10.1016/j.sbi.2020.01.001
Khoda, Liu, Storey, Generalized Polak-Ribiere algorithm, J. Optim. Theory Appl, doi:10.1007/BF00941472
Kim, Cha, Choi, Kim, Omega class glutathione S-transferase: Antioxidant enzyme in pathogenesis of neurodegenerative diseases, Oxidative Med. Cell. Longev, doi:10.1155/2017/5049532
Kim, Chivian, Baker, Protein structure prediction and analysis using the Robetta server, Nucleic Acids Res, doi:10.1093/nar/gkh468
Klatzmann, Mcdougal, Maddon, The CD4 molecule and HIV infection, Immunodefic. Rev
Lan, Ge, Yu, Shan, Zhou et al., Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor, Nature, doi:10.1038/s41586-020-2180-5
Liu, Bakker, Narimatsu, Van Kuppeveld, Clausen et al., H3N2 influenza A virus gradually adapts to human-type receptor binding and entry specificity after the start of the 1968 pandemic, Proc. Natl. Acad. Sci, doi:10.1073/pnas.2304992120
Low, Yip, Lal, Repositioning Ivermectin for Covid-19 treatment: Molecular mechanisms of action against SARS-CoV-2 replication, Biochim. Biophys. Acta-Mol. Basis Dis, doi:10.1016/j.bbadis.2021.166294
Maginnis, Virus-Receptor Interactions: The Key to Cellular Invasion, J. Mol. Biol, doi:10.1016/j.jmb.2018.06.024
Maresca, Derghal, Caravagna, Dudin, Fantini, Controlled aggregation of adenine by sugars: Physicochemical studies, molecular modelling simulations of sugar-aromatic CH-pi stacking interactions, and biological significance, Phys. Chem. Chem. Phys. PCCP, doi:10.1039/b802594k
Matveeva, Lefebvre, Chahinian, Yahi, Fantini, Host membranes as drivers of virus evolution, Viruses, doi:10.3390/v15091854
Mcdougal, Maddon, Dalgleish, Clapham, Littman et al., The T4 glycoprotein is a cell-surface receptor for the AIDS virus, Cold Spring Harb. Symp. Quant. Biol, doi:10.1101/SQB.1986.051.01.083
Milanetti, Miotto, Di Rienzo, Nagaraj, Monti et al., In-silico evidence for a two receptor based strategy of SARS-CoV-2, Front. Mol. Biosci, doi:10.3389/fmolb.2021.690655
Monti, Milanetti, Frans, Miotto, Di Rienzo et al., Two Receptor Binding Strategy of SARS-CoV-2 Is Mediated by Both the N-Terminal and Receptor-Binding Spike Domain, J. Phys. Chem. B, doi:10.1021/acs.jpcb.3c06258
Nocedal, Wright, Conjugate gradient methods
Paggi, Pandit, Dror, The Art and Science of Molecular Docking, Annu. Rev. Biochem, doi:10.1146/annurev-biochem-030222-120000
Sarkar, Concilio, Sessa, Marrafino, Piotto, Advancements and novel approaches in modified autodock vina algorithms for enhanced molecular docking, Results Chem, doi:10.1016/j.rechem.2024.101319
Scheim, A deadly embrace: Hemagglutination mediated by SARS-CoV-2 spike protein at its 22 N-glycosylation sites, red blood cell surface sialoglycoproteins, and antibody, Int. J. Mol. Sci, doi:10.3390/ijms23052558
Scheim, Vottero, Santin, Hirsh, Sialylated glycan bindings from SARS-CoV-2 spike protein to blood and endothelial cells govern the severe morbidities of COVID-19, Int. J. Mol. Sci, doi:10.3390/ijms242317039
Seyran, Takayama, Uversky, Lundstrom, Palù et al., The structural basis of accelerated host cell entry by SARS-CoV-2, FEBS J, doi:10.1111/febs.15651
Shang, Ye, Shi, Wan, Luo et al., Structural basis of receptor recognition by SARS-CoV-2, Nature, doi:10.1038/s41586-020-2179-y
Shanmugaraj, Ever-evolving SARS-CoV-2: Latest variant KP. 2 is on the rise, Asian Pac. J. Trop. Med, doi:10.4103/apjtm.apjtm_341_24
Sinha, Tam, Wang, Applications of molecular dynamics simulation in protein study, Membranes, doi:10.3390/membranes12090844
Sokkar, Mohandass, Ramachandran, Multiple templates-based homology modeling enhances structure quality of AT1 receptor: Validation by molecular dynamics and antagonist docking, J. Mol. Model, doi:10.1007/s00894-010-0860-z
Srinivasu, Babu, Rao, Energy Minimization of CDK2 bound ligands: A Computational Approach, Int. J. Eng. Res. Appl
Ströh, Nagarathinam, Krey, Conformational flexibility in the CD81-binding site of the hepatitis C virus glycoprotein E2, Front. Immunol, doi:10.3389/fimmu.2018.01396
Sun, The role of cell surface sialic acids for SARS-CoV-2 infection, Glycobiology, doi:10.1093/glycob/cwab032
Suryadevara, Shrihari, Gilchuk, Vanblargan, Binshtein et al., Neutralizing and protective human monoclonal antibodies recognizing the N-terminal domain of the SARS-CoV-2 spike protein, Cell, doi:10.1016/j.cell.2021.03.029
Thakur, Micic, Leblanc, Surface chemistry of Alzheimer's disease: A Langmuir monolayer approach, Colloids Surf. B Biointerfaces, doi:10.1016/j.colsurfb.2009.07.043
Thomsen, Christensen, Moldock, A new technique for high-accuracy molecular docking, J. Med. Chem, doi:10.1021/jm051197e
Tronrud, Introduction to macromolecular refinement, Acta Crystallogr. Sect. D Biol. Crystallogr, doi:10.1107/S090744490402356X
Trott, Olson, AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading, J. Comput. Chem, doi:10.1002/jcc.21334
Tsuji, Docking Study with HyperChem, Revision G1
Tsuji, Homology Modeling Professional for HyperChem
Tsuji, Shudo, Kagechika, Docking simulations suggest that all-trans retinoic acid could bind to retinoid X receptors, J. Comput.-Aided Mol. Des, doi:10.1007/s10822-015-9869-9
Uversky, Intrinsically disordered proteins and novel strategies for drug discovery, Expert Opin. Drug Discov, doi:10.1517/17460441.2012.686489
Uversky, Intrinsically disordered proteins and their environment: Effects of strong denaturants, temperature, pH, counter ions, membranes, binding partners, osmolytes, and macromolecular crowding, Protein J, doi:10.1007/s10930-009-9201-4
Uversky, Introduction to intrinsically disordered proteins (IDPs), Chem. Rev, doi:10.1021/cr500288y
Wlodarski, Zagrovic, Conformational selection and induced fit mechanism underlie specificity in noncovalent interactions with ubiquitin, Proc. Natl. Acad. Sci, doi:10.1073/pnas.0906966106
Zaidi, Dehgani-Mobaraki, The mechanisms of action of ivermectin against SARS-CoV-2-An extensive review, J. Antibiot, doi:10.1038/s41429-021-00491-6
Zhao, Caflisch, Molecular dynamics in drug design, Eur. J. Med. Chem, doi:10.1016/j.ejmech.2014.08.004
DOI record:
{
"DOI": "10.3390/v16121836",
"ISSN": [
"1999-4915"
],
"URL": "http://dx.doi.org/10.3390/v16121836",
"abstract": "<jats:p>Most studies on the docking of ivermectin on the spike protein of SARS-CoV-2 concern the receptor binding domain (RBD) and, more precisely, the RBD interface recognized by the ACE2 receptor. The N-terminal domain (NTD), which controls the initial attachment of the virus to lipid raft gangliosides, has not received the attention it deserves. In this study, we combined molecular modeling and physicochemical approaches to analyze the mode of interaction of ivermectin with the interface of the NTD-facing lipid rafts of the host cell membrane. We characterize a binding area that presents point mutations and deletions in successive SARS-CoV-2 variants from the initial strain to omicron KP.3 circulating in many countries in 2024. We show that ivermectin has exceptional flexibility, allowing the drug to bind to the spike protein of all variants tested. The energy of interaction is specific to each variant, allowing a classification according to their affinity for ivermectin in the following ascending order: Omicron KP.3 < Delta < Omicron BA.5 < Alpha < Wuhan (B.1) < Omicron BA.1. The binding site of ivermectin is subject to important variations of the NTD, including the Y144 deletion. It overlaps with the ganglioside binding domain of the NTD, as demonstrated by docking and physicochemical studies. These results suggest a new mechanism of antiviral action for ivermectin based on competitive inhibition for initial virus attachment to lipid rafts. The current KP.3 variant is still recognized by ivermectin, although with an affinity slightly lower than the Wuhan strain.</jats:p>",
"alternative-id": [
"v16121836"
],
"author": [
{
"affiliation": [
{
"name": "IHU Méditerranée Infection, 19-21 Boulevard Jean Moulin, 13005 Marseille, France"
},
{
"name": "Microbes Evolution Phylogeny and Infections (MEPHI), Aix-Marseille Université, 27 Boulevard Jean Moulin, 13005 Marseille, France"
},
{
"name": "Assistance Publique-Hôpitaux de Marseille (AP-HM), 264 Rue Saint-Pierre, 13005 Marseille, France"
},
{
"name": "Department of Biology, Faculty of Medicine, Aix-Marseille University, INSERM UA16, 13015 Marseille, France"
}
],
"family": "Lefebvre",
"given": "Marine",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-9516-4168",
"affiliation": [
{
"name": "Department of Biology, Faculty of Medicine, Aix-Marseille University, INSERM UA16, 13015 Marseille, France"
}
],
"authenticated-orcid": false,
"family": "Chahinian",
"given": "Henri",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8006-7704",
"affiliation": [
{
"name": "IHU Méditerranée Infection, 19-21 Boulevard Jean Moulin, 13005 Marseille, France"
},
{
"name": "Microbes Evolution Phylogeny and Infections (MEPHI), Aix-Marseille Université, 27 Boulevard Jean Moulin, 13005 Marseille, France"
},
{
"name": "Assistance Publique-Hôpitaux de Marseille (AP-HM), 264 Rue Saint-Pierre, 13005 Marseille, France"
}
],
"authenticated-orcid": false,
"family": "La Scola",
"given": "Bernard",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8653-5521",
"affiliation": [
{
"name": "Department of Biology, Faculty of Medicine, Aix-Marseille University, INSERM UA16, 13015 Marseille, France"
}
],
"authenticated-orcid": false,
"family": "Fantini",
"given": "Jacques",
"sequence": "additional"
}
],
"container-title": "Viruses",
"container-title-short": "Viruses",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
11,
27
]
],
"date-time": "2024-11-27T09:20:12Z",
"timestamp": 1732699212000
},
"deposited": {
"date-parts": [
[
2024,
11,
27
]
],
"date-time": "2024-11-27T09:37:24Z",
"timestamp": 1732700244000
},
"indexed": {
"date-parts": [
[
2024,
11,
28
]
],
"date-time": "2024-11-28T05:23:07Z",
"timestamp": 1732771387549,
"version": "3.29.0"
},
"is-referenced-by-count": 0,
"issue": "12",
"issued": {
"date-parts": [
[
2024,
11,
27
]
]
},
"journal-issue": {
"issue": "12",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
11,
27
]
],
"date-time": "2024-11-27T00:00:00Z",
"timestamp": 1732665600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1999-4915/16/12/1836/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1836",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
11,
27
]
]
},
"published-online": {
"date-parts": [
[
2024,
11,
27
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1101/SQB.1986.051.01.083",
"article-title": "The T4 glycoprotein is a cell-surface receptor for the AIDS virus",
"author": "McDougal",
"doi-asserted-by": "crossref",
"first-page": "703",
"journal-title": "Cold Spring Harb. Symp. Quant. Biol.",
"key": "ref_1",
"volume": "51",
"year": "1986"
},
{
"article-title": "The CD4 molecule and HIV infection",
"author": "Klatzmann",
"first-page": "43",
"journal-title": "Immunodefic. Rev.",
"key": "ref_2",
"volume": "2",
"year": "1990"
},
{
"DOI": "10.1038/s41586-020-2179-y",
"article-title": "Structural basis of receptor recognition by SARS-CoV-2",
"author": "Shang",
"doi-asserted-by": "crossref",
"first-page": "221",
"journal-title": "Nature",
"key": "ref_3",
"volume": "581",
"year": "2020"
},
{
"DOI": "10.1016/j.jmb.2018.06.024",
"article-title": "Virus–Receptor Interactions: The Key to Cellular Invasion",
"author": "Maginnis",
"doi-asserted-by": "crossref",
"first-page": "2590",
"journal-title": "J. Mol. Biol.",
"key": "ref_4",
"volume": "430",
"year": "2018"
},
{
"DOI": "10.3390/v15020284",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Fantini, J., Azzaz, F., Chahinian, H., and Yahi, N. (2023). Electrostatic Surface Potential as a Key Parameter in Virus Transmission and Evolution: How to Manage Future Virus Pandemics in the Post-COVID-19 Era. Viruses, 15."
},
{
"DOI": "10.3390/v15091854",
"doi-asserted-by": "crossref",
"key": "ref_6",
"unstructured": "Matveeva, M., Lefebvre, M., Chahinian, H., Yahi, N., and Fantini, J. (2023). Host membranes as drivers of virus evolution. Viruses, 15."
},
{
"DOI": "10.3390/ijms24031923",
"doi-asserted-by": "crossref",
"key": "ref_7",
"unstructured": "Fantini, J., Chahinian, H., and Yahi, N. (2023). Convergent Evolution Dynamics of SARS-CoV-2 and HIV Surface Envelope Glycoproteins Driven by Host Cell Surface Receptors and Lipid Rafts: Lessons for the Future. Int. J. Mol. Sci., 24."
},
{
"DOI": "10.3389/fmolb.2021.690655",
"doi-asserted-by": "crossref",
"key": "ref_8",
"unstructured": "Milanetti, E., Miotto, M., Di Rienzo, L., Nagaraj, M., Monti, M., Golbek, T.W., Gosti, G., Roeters, S.J., Weidner, T., and Otzen, D.E. (2021). In-silico evidence for a two receptor based strategy of SARS-CoV-2. Front. Mol. Biosci., 8."
},
{
"DOI": "10.1021/acs.jpcb.3c06258",
"article-title": "Two Receptor Binding Strategy of SARS-CoV-2 Is Mediated by Both the N-Terminal and Receptor-Binding Spike Domain",
"author": "Monti",
"doi-asserted-by": "crossref",
"first-page": "451",
"journal-title": "J. Phys. Chem. B",
"key": "ref_9",
"volume": "128",
"year": "2024"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105960",
"article-title": "Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection",
"author": "Fantini",
"doi-asserted-by": "crossref",
"first-page": "105960",
"journal-title": "Int. J. Antimicrob. Agents",
"key": "ref_10",
"volume": "55",
"year": "2020"
},
{
"DOI": "10.1016/j.bbrc.2020.10.015",
"article-title": "Leveraging coronavirus binding to gangliosides for innovative vaccine and therapeutic strategies against COVID-19",
"author": "Fantini",
"doi-asserted-by": "crossref",
"first-page": "132",
"journal-title": "Biochem. Biophys. Res. Commun.",
"key": "ref_11",
"volume": "538",
"year": "2021"
},
{
"DOI": "10.1111/febs.15651",
"article-title": "The structural basis of accelerated host cell entry by SARS-CoV-2",
"author": "Seyran",
"doi-asserted-by": "crossref",
"first-page": "5010",
"journal-title": "FEBS J.",
"key": "ref_12",
"volume": "288",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2180-5",
"article-title": "Structure of the SARS-CoV-2 spike receptor-binding domain bound to the ACE2 receptor",
"author": "Lan",
"doi-asserted-by": "crossref",
"first-page": "215",
"journal-title": "Nature",
"key": "ref_13",
"volume": "581",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2021.03.029",
"article-title": "Neutralizing and protective human monoclonal antibodies recognizing the N-terminal domain of the SARS-CoV-2 spike protein",
"author": "Suryadevara",
"doi-asserted-by": "crossref",
"first-page": "2316",
"journal-title": "Cell",
"key": "ref_14",
"volume": "184",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2021.06.005",
"article-title": "SARS-CoV-2 mRNA vaccination induces functionally diverse antibodies to NTD, RBD, and S2",
"author": "Amanat",
"doi-asserted-by": "crossref",
"first-page": "3936",
"journal-title": "Cell",
"key": "ref_15",
"volume": "184",
"year": "2021"
},
{
"DOI": "10.3390/v13112177",
"doi-asserted-by": "crossref",
"key": "ref_16",
"unstructured": "Jaafar, R., Boschi, C., Aherfi, S., Bancod, A., Le Bideau, M., Edouard, S., Colson, P., Chahinian, H., Raoult, D., and Yahi, N. (2021). High individual heterogeneity of neutralizing activities against the original strain and nine different variants of SARS-CoV-2. Viruses, 13."
},
{
"DOI": "10.1016/j.ijantimicag.2020.106020",
"article-title": "Synergistic antiviral effect of hydroxychloroquine and azithromycin in combination against SARS-CoV-2: What molecular dynamics studies of virus-host interactions reveal",
"author": "Fantini",
"doi-asserted-by": "crossref",
"first-page": "106020",
"journal-title": "Int. J. Antimicrob. Agents",
"key": "ref_17",
"volume": "56",
"year": "2020"
},
{
"DOI": "10.1136/bmjresp-2020-000806",
"article-title": "Rationale for azithromycin in COVID-19: An overview of existing evidence",
"author": "Gyselinck",
"doi-asserted-by": "crossref",
"first-page": "e000806",
"journal-title": "BMJ Open Respir. Res.",
"key": "ref_18",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/j.micpath.2020.104228",
"article-title": "In vitro testing of combined hydroxychloroquine and azithromycin on SARS-CoV-2 shows synergistic effect",
"author": "Andreani",
"doi-asserted-by": "crossref",
"first-page": "104228",
"journal-title": "Microb. Pathog.",
"key": "ref_19",
"volume": "145",
"year": "2020"
},
{
"DOI": "10.1016/j.antiviral.2020.104787",
"article-title": "The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro",
"author": "Caly",
"doi-asserted-by": "crossref",
"first-page": "104787",
"journal-title": "Antivir. Res.",
"key": "ref_20",
"volume": "178",
"year": "2020"
},
{
"DOI": "10.1016/j.bbadis.2021.166294",
"doi-asserted-by": "crossref",
"key": "ref_21",
"unstructured": "Low, Z.Y., Yip, A.J.W., and Lal, S.K. (2022). Repositioning Ivermectin for Covid-19 treatment: Molecular mechanisms of action against SARS-CoV-2 replication. Biochim. Biophys. Acta-Mol. Basis Dis., 1868."
},
{
"DOI": "10.1080/23744235.2024.2385500",
"article-title": "Features of the SARS-CoV-2 KP. 3 variant mutations",
"author": "Branda",
"doi-asserted-by": "crossref",
"first-page": "894",
"journal-title": "Infect. Dis.",
"key": "ref_22",
"volume": "56",
"year": "2024"
},
{
"DOI": "10.1016/S1473-3099(24)00298-6",
"article-title": "Virological characteristics of the SARS-CoV-2 KP. 2 variant",
"author": "Kaku",
"doi-asserted-by": "crossref",
"first-page": "e416",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_23",
"volume": "24",
"year": "2024"
},
{
"DOI": "10.1016/S1473-3099(24)00415-8",
"article-title": "Virological characteristics of the SARS-CoV-2 KP. 3, LB. 1, and KP. 2.3 variants",
"author": "Kaku",
"doi-asserted-by": "crossref",
"first-page": "e482",
"journal-title": "Lancet Infect. Dis.",
"key": "ref_24",
"volume": "24",
"year": "2024"
},
{
"DOI": "10.4103/apjtm.apjtm_341_24",
"article-title": "Ever-evolving SARS-CoV-2: Latest variant KP. 2 is on the rise",
"author": "Shanmugaraj",
"doi-asserted-by": "crossref",
"first-page": "241",
"journal-title": "Asian Pac. J. Trop. Med.",
"key": "ref_25",
"volume": "17",
"year": "2024"
},
{
"DOI": "10.1016/j.jinf.2021.06.001",
"article-title": "Structural dynamics of SARS-CoV-2 variants: A health monitoring strategy for anticipating Covid-19 outbreaks",
"author": "Fantini",
"doi-asserted-by": "crossref",
"first-page": "197",
"journal-title": "J. Infect.",
"key": "ref_26",
"volume": "83",
"year": "2021"
},
{
"DOI": "10.1093/nar/gkh468",
"article-title": "Protein structure prediction and analysis using the Robetta server",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "W526",
"journal-title": "Nucleic Acids Res.",
"key": "ref_27",
"volume": "32",
"year": "2004"
},
{
"DOI": "10.1002/elps.1150181505",
"article-title": "SWISS-MODEL and the Swiss-Pdb Viewer: An environment for comparative protein modeling",
"author": "Guex",
"doi-asserted-by": "crossref",
"first-page": "2714",
"journal-title": "Electrophoresis",
"key": "ref_28",
"volume": "18",
"year": "1997"
},
{
"DOI": "10.1155/2017/5049532",
"article-title": "Omega class glutathione S-transferase: Antioxidant enzyme in pathogenesis of neurodegenerative diseases",
"author": "Kim",
"doi-asserted-by": "crossref",
"first-page": "5049532",
"journal-title": "Oxidative Med. Cell. Longev.",
"key": "ref_29",
"volume": "2017",
"year": "2017"
},
{
"key": "ref_30",
"unstructured": "Tsuji, M. (2015). Docking Study with HyperChem, Revision G1, Institute of Molecular Function."
},
{
"DOI": "10.1007/s10822-015-9869-9",
"article-title": "Docking simulations suggest that all-trans retinoic acid could bind to retinoid X receptors",
"author": "Tsuji",
"doi-asserted-by": "crossref",
"first-page": "975",
"journal-title": "J. Comput.-Aided Mol. Des.",
"key": "ref_31",
"volume": "29",
"year": "2015"
},
{
"key": "ref_32",
"unstructured": "Tsuji, M. (2015). Homology Modeling Professional for HyperChem, Revision G1, Institute of Molecular Function."
},
{
"article-title": "Energy Minimization of CDK2 bound ligands: A Computational Approach",
"author": "Srinivasu",
"first-page": "1884",
"journal-title": "Int. J. Eng. Res. Appl.",
"key": "ref_33",
"volume": "2",
"year": "2012"
},
{
"DOI": "10.1021/jm051197e",
"article-title": "MolDock: A new technique for high-accuracy molecular docking",
"author": "Thomsen",
"doi-asserted-by": "crossref",
"first-page": "3315",
"journal-title": "J. Med. Chem.",
"key": "ref_34",
"volume": "49",
"year": "2006"
},
{
"DOI": "10.1016/j.colsurfb.2009.07.043",
"article-title": "Surface chemistry of Alzheimer’s disease: A Langmuir monolayer approach",
"author": "Thakur",
"doi-asserted-by": "crossref",
"first-page": "436",
"journal-title": "Colloids Surf. B Biointerfaces",
"key": "ref_35",
"volume": "74",
"year": "2009"
},
{
"DOI": "10.1016/j.chemphyslip.2018.01.008",
"article-title": "Langmuir-monolayer methodologies for characterizing protein-lipid interactions",
"author": "Elderdfi",
"doi-asserted-by": "crossref",
"first-page": "61",
"journal-title": "Chem. Phys. Lipids",
"key": "ref_36",
"volume": "212",
"year": "2018"
},
{
"article-title": "Monosialoganglioside-GM1 triggers binding of the amyloid-protein salmon calcitonin to a Langmuir membrane model mimicking the occurrence of lipid-rafts",
"author": "Diociaiuti",
"first-page": "365",
"journal-title": "Biochem. Biophys. Rep.",
"key": "ref_37",
"volume": "8",
"year": "2016"
},
{
"DOI": "10.1007/978-1-4939-6875-6_2",
"article-title": "Hybrid In Silico/In Vitro Approaches for the Identification of Functional Cholesterol-Binding Domains in Membrane Proteins",
"author": "Fantini",
"doi-asserted-by": "crossref",
"first-page": "7",
"journal-title": "Methods Mol. Biol.",
"key": "ref_38",
"volume": "1583",
"year": "2017"
},
{
"DOI": "10.36877/pddbs.a0000424",
"article-title": "Illustrated Procedure to Perform Molecular Docking Using PyRx and Biovia Discovery Studio Visualizer: A Case Study of 10kt With Atropine",
"author": "Ayodele",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Prog. Drug Discov. Biomed. Sci.",
"key": "ref_39",
"volume": "6",
"year": "2023"
},
{
"DOI": "10.1023/A:1011115820450",
"article-title": "DOCK 4.0: Search strategies for automated molecular docking of flexible molecule databases",
"author": "Ewing",
"doi-asserted-by": "crossref",
"first-page": "411",
"journal-title": "J. Comput.-Aided Mol. Des.",
"key": "ref_40",
"volume": "15",
"year": "2001"
},
{
"DOI": "10.1002/jcc.21334",
"article-title": "AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading",
"author": "Trott",
"doi-asserted-by": "crossref",
"first-page": "455",
"journal-title": "J. Comput. Chem.",
"key": "ref_41",
"volume": "31",
"year": "2010"
},
{
"DOI": "10.1146/annurev-biochem-030222-120000",
"article-title": "The Art and Science of Molecular Docking",
"author": "Paggi",
"doi-asserted-by": "crossref",
"first-page": "389",
"journal-title": "Annu. Rev. Biochem.",
"key": "ref_42",
"volume": "93",
"year": "2024"
},
{
"DOI": "10.1016/j.tips.2014.12.001",
"article-title": "Beware of docking!",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "78",
"journal-title": "Trends Pharmacol. Sci.",
"key": "ref_43",
"volume": "36",
"year": "2015"
},
{
"DOI": "10.1039/D3SC04185A",
"article-title": "PoseBusters: AI-based docking methods fail to generate physically valid poses or generalise to novel sequences",
"author": "Buttenschoen",
"doi-asserted-by": "crossref",
"first-page": "3130",
"journal-title": "Chem. Sci.",
"key": "ref_44",
"volume": "15",
"year": "2024"
},
{
"DOI": "10.1016/j.rechem.2024.101319",
"article-title": "Advancements and novel approaches in modified autodock vina algorithms for enhanced molecular docking",
"author": "Sarkar",
"doi-asserted-by": "crossref",
"first-page": "101319",
"journal-title": "Results Chem.",
"key": "ref_45",
"volume": "7",
"year": "2024"
},
{
"DOI": "10.1002/prot.21781",
"article-title": "Flexible protein-flexible ligand docking with disrupted velocity simulated annealing",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "440",
"journal-title": "Proteins",
"key": "ref_46",
"volume": "71",
"year": "2008"
},
{
"DOI": "10.3410/B3-19",
"doi-asserted-by": "crossref",
"key": "ref_47",
"unstructured": "Changeux, J.-P., and Edelstein, S. (2011). Conformational selection or induced fit? 50 years of debate resolved. F1000 Biol. Rep., 3."
},
{
"DOI": "10.1016/j.bpc.2014.03.003",
"article-title": "Distinguishing induced fit from conformational selection",
"author": "Gianni",
"doi-asserted-by": "crossref",
"first-page": "33",
"journal-title": "Biophys. Chem.",
"key": "ref_48",
"volume": "189",
"year": "2014"
},
{
"DOI": "10.1073/pnas.0906966106",
"article-title": "Conformational selection and induced fit mechanism underlie specificity in noncovalent interactions with ubiquitin",
"author": "Wlodarski",
"doi-asserted-by": "crossref",
"first-page": "19346",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_49",
"volume": "106",
"year": "2009"
},
{
"DOI": "10.3390/molecules27092977",
"doi-asserted-by": "crossref",
"key": "ref_50",
"unstructured": "Islas, Á.A., and Scior, T. (2022). Allosteric Binding of MDMA to the Human Serotonin Transporter (hSERT) via Ensemble Binding Space Analysis with ΔG Calculations, Induced Fit Docking and Monte Carlo Simulations. Molecules, 27."
},
{
"DOI": "10.1007/s10930-009-9201-4",
"article-title": "Intrinsically disordered proteins and their environment: Effects of strong denaturants, temperature, pH, counter ions, membranes, binding partners, osmolytes, and macromolecular crowding",
"author": "Uversky",
"doi-asserted-by": "crossref",
"first-page": "305",
"journal-title": "Protein J.",
"key": "ref_51",
"volume": "28",
"year": "2009"
},
{
"DOI": "10.1517/17460441.2012.686489",
"article-title": "Intrinsically disordered proteins and novel strategies for drug discovery",
"author": "Uversky",
"doi-asserted-by": "crossref",
"first-page": "475",
"journal-title": "Expert Opin. Drug Discov.",
"key": "ref_52",
"volume": "7",
"year": "2012"
},
{
"DOI": "10.1021/cr500288y",
"article-title": "Introduction to intrinsically disordered proteins (IDPs)",
"author": "Uversky",
"doi-asserted-by": "crossref",
"first-page": "6557",
"journal-title": "Chem. Rev.",
"key": "ref_53",
"volume": "114",
"year": "2014"
},
{
"DOI": "10.1039/B608269F",
"article-title": "Molecular mechanics methods for predicting protein-ligand binding",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "5166",
"journal-title": "Phys. Chem. Chem. Phys. PCCP",
"key": "ref_54",
"volume": "8",
"year": "2006"
},
{
"article-title": "Introduction to molecular dynamics simulation",
"author": "Allen",
"first-page": "1",
"journal-title": "Comput. Soft Matter Synth. Polym. Proteins",
"key": "ref_55",
"volume": "23",
"year": "2004"
},
{
"DOI": "10.1007/s00894-010-0860-z",
"article-title": "Multiple templates-based homology modeling enhances structure quality of AT1 receptor: Validation by molecular dynamics and antagonist docking",
"author": "Sokkar",
"doi-asserted-by": "crossref",
"first-page": "1565",
"journal-title": "J. Mol. Model.",
"key": "ref_56",
"volume": "17",
"year": "2011"
},
{
"DOI": "10.1016/j.ejmech.2014.08.004",
"article-title": "Molecular dynamics in drug design",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "4",
"journal-title": "Eur. J. Med. Chem.",
"key": "ref_57",
"volume": "91",
"year": "2015"
},
{
"DOI": "10.1002/med.20067",
"article-title": "Combining docking and molecular dynamic simulations in drug design",
"author": "Alonso",
"doi-asserted-by": "crossref",
"first-page": "531",
"journal-title": "Med. Res. Rev.",
"key": "ref_58",
"volume": "26",
"year": "2006"
},
{
"DOI": "10.1002/anie.202112232",
"article-title": "A cholesterol dimer stabilizes the inactivated state of an inward-rectifier Potassium Channel",
"author": "Borcik",
"doi-asserted-by": "crossref",
"first-page": "e202112232",
"journal-title": "Angew. Chem. Int. Ed.",
"key": "ref_59",
"volume": "61",
"year": "2022"
},
{
"DOI": "10.3390/membranes12090844",
"doi-asserted-by": "crossref",
"key": "ref_60",
"unstructured": "Sinha, S., Tam, B., and Wang, S.M. (2022). Applications of molecular dynamics simulation in protein study. Membranes, 12."
},
{
"DOI": "10.1016/j.sbi.2020.01.001",
"article-title": "Dynamic protein interfaces and conformational landscapes of membrane protein complexes",
"author": "Kharche",
"doi-asserted-by": "crossref",
"first-page": "191",
"journal-title": "Curr. Opin. Struct. Biol.",
"key": "ref_61",
"volume": "61",
"year": "2020"
},
{
"DOI": "10.1021/acs.jctc.3c00733",
"article-title": "Pragmatic coarse-graining of proteins: Models and applications",
"author": "Patmanidis",
"doi-asserted-by": "crossref",
"first-page": "7112",
"journal-title": "J. Chem. Theory Comput.",
"key": "ref_62",
"volume": "19",
"year": "2023"
},
{
"DOI": "10.1007/978-0-387-40065-5_5",
"doi-asserted-by": "crossref",
"key": "ref_63",
"unstructured": "Nocedal, J., and Wright, S.J. (2006). Conjugate gradient methods. Numerical Optimization, Springer."
},
{
"DOI": "10.1007/978-3-031-08720-2_5",
"doi-asserted-by": "crossref",
"key": "ref_64",
"unstructured": "Andrei, N. (2022). Conjugate Gradient Methods. Modern Numerical Nonlinear Optimization, Springer International Publishing."
},
{
"DOI": "10.1007/BF02614362",
"article-title": "A globally convergent version of the Polak-Ribiere conjugate gradient method",
"author": "Grippo",
"doi-asserted-by": "crossref",
"first-page": "375",
"journal-title": "Math. Program.",
"key": "ref_65",
"volume": "78",
"year": "1997"
},
{
"DOI": "10.1007/BF00941472",
"article-title": "Generalized Polak-Ribiere algorithm",
"author": "Khoda",
"doi-asserted-by": "crossref",
"first-page": "345",
"journal-title": "J. Optim. Theory Appl.",
"key": "ref_66",
"volume": "75",
"year": "1992"
},
{
"DOI": "10.1039/b802594k",
"article-title": "Controlled aggregation of adenine by sugars: Physicochemical studies, molecular modelling simulations of sugar-aromatic CH-pi stacking interactions, and biological significance",
"author": "Maresca",
"doi-asserted-by": "crossref",
"first-page": "2792",
"journal-title": "Phys. Chem. Chem. Phys. PCCP",
"key": "ref_67",
"volume": "10",
"year": "2008"
},
{
"DOI": "10.1107/S090744490402356X",
"article-title": "Introduction to macromolecular refinement",
"author": "Tronrud",
"doi-asserted-by": "crossref",
"first-page": "2156",
"journal-title": "Acta Crystallogr. Sect. D Biol. Crystallogr.",
"key": "ref_68",
"volume": "60",
"year": "2004"
},
{
"DOI": "10.1111/jnc.12390",
"article-title": "Mechanism of cholesterol-assisted oligomeric channel formation by a short Alzheimer β-amyloid peptide",
"author": "Troadec",
"doi-asserted-by": "crossref",
"first-page": "186",
"journal-title": "J. Neurochem.",
"key": "ref_69",
"volume": "128",
"year": "2014"
},
{
"DOI": "10.2217/fvl-2020-0342",
"article-title": "Exploring the binding efficacy of ivermectin against the key proteins of SARS-CoV-2 pathogenesis: An in silico approach",
"author": "Choudhury",
"doi-asserted-by": "crossref",
"first-page": "277",
"journal-title": "Future Virol.",
"key": "ref_70",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.3390/computation10040051",
"doi-asserted-by": "crossref",
"key": "ref_71",
"unstructured": "Aminpour, M., Cannariato, M., Preto, J., Safaeeardebili, M.E., Moracchiato, A., Doria, D., Donato, F., Zizzi, E.A., Deriu, M.A., and Scheim, D.E. (2022). In silico analysis of the multi-targeted mode of action of ivermectin and related compounds. Computation, 10."
},
{
"DOI": "10.1093/glycob/cwab032",
"article-title": "The role of cell surface sialic acids for SARS-CoV-2 infection",
"author": "Sun",
"doi-asserted-by": "crossref",
"first-page": "1245",
"journal-title": "Glycobiology",
"key": "ref_72",
"volume": "31",
"year": "2021"
},
{
"DOI": "10.3390/ijms22126462",
"doi-asserted-by": "crossref",
"key": "ref_73",
"unstructured": "Di Gaetano, S., Capasso, D., Delre, P., Pirone, L., Saviano, M., Pedone, E., and Mangiatordi, G.F. (2021). More Is Always Better Than One: The N-Terminal Domain of the Spike Protein as Another Emerging Target for Hampering the SARS-CoV-2 Attachment to Host Cells. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.1101/2022.11.24.517882",
"doi-asserted-by": "crossref",
"key": "ref_74",
"unstructured": "Boschi, C., Scheim, D.E., Bancod, A., Militello, M., Bideau, M.L., Colson, P., Fantini, J., and Scola, B.L. (2022). SARS-CoV-2 spike protein induces hemagglutination: Implications for COVID-19 morbidities and therapeutics and for vaccine adverse effects. Int. J. Mol. Sci., 23."
},
{
"DOI": "10.1002/jmv.27577",
"article-title": "The puzzling mutational landscape of the SARS-2-variant Omicron",
"author": "Fantini",
"doi-asserted-by": "crossref",
"first-page": "2019",
"journal-title": "J. Med. Virol.",
"key": "ref_75",
"volume": "94",
"year": "2022"
},
{
"DOI": "10.1002/2211-5463.13612",
"article-title": "Lipid rafts and human diseases: Why we need to target gangliosides",
"author": "Fantini",
"doi-asserted-by": "crossref",
"first-page": "1636",
"journal-title": "FEBS Open Bio",
"key": "ref_76",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.3390/receptors3010006",
"article-title": "Fundamental Mechanisms in Membrane Receptology: Old Paradigms, New Concepts and Perspectives",
"author": "Fantini",
"doi-asserted-by": "crossref",
"first-page": "107",
"journal-title": "Receptors",
"key": "ref_77",
"volume": "3",
"year": "2024"
},
{
"DOI": "10.1073/pnas.2304992120",
"article-title": "H3N2 influenza A virus gradually adapts to human-type receptor binding and entry specificity after the start of the 1968 pandemic",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "e2304992120",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_78",
"volume": "120",
"year": "2023"
},
{
"DOI": "10.3389/fimmu.2018.01396",
"doi-asserted-by": "crossref",
"key": "ref_79",
"unstructured": "Ströh, L.J., Nagarathinam, K., and Krey, T. (2018). Conformational flexibility in the CD81-binding site of the hepatitis C virus glycoprotein E2. Front. Immunol., 9."
},
{
"DOI": "10.1016/j.csbj.2023.03.029",
"article-title": "Identifying promising druggable binding sites and their flexibility to target the receptor-binding domain of SARS-CoV-2 spike protein",
"author": "Ghoula",
"doi-asserted-by": "crossref",
"first-page": "2339",
"journal-title": "Comput. Struct. Biotechnol. J.",
"key": "ref_80",
"volume": "21",
"year": "2023"
},
{
"DOI": "10.1038/s41429-021-00491-6",
"article-title": "The mechanisms of action of ivermectin against SARS-CoV-2—An extensive review",
"author": "Zaidi",
"doi-asserted-by": "crossref",
"first-page": "60",
"journal-title": "J. Antibiot.",
"key": "ref_81",
"volume": "75",
"year": "2022"
},
{
"DOI": "10.3390/ijms23052558",
"doi-asserted-by": "crossref",
"key": "ref_82",
"unstructured": "Scheim, D.E. (2022). A deadly embrace: Hemagglutination mediated by SARS-CoV-2 spike protein at its 22 N-glycosylation sites, red blood cell surface sialoglycoproteins, and antibody. Int. J. Mol. Sci., 23."
},
{
"DOI": "10.3390/ijms242317039",
"doi-asserted-by": "crossref",
"key": "ref_83",
"unstructured": "Scheim, D.E., Vottero, P., Santin, A.D., and Hirsh, A.G. (2023). Sialylated glycan bindings from SARS-CoV-2 spike protein to blood and endothelial cells govern the severe morbidities of COVID-19. Int. J. Mol. Sci., 24."
},
{
"DOI": "10.1016/j.bj.2024.100787",
"doi-asserted-by": "crossref",
"key": "ref_84",
"unstructured": "Dima, F., Salvagno, G.L., and Lippi, G. (2024). Effects of recombinant SARS-CoV-2 spike protein variants on red blood cells parameters and red blood cell distribution width. Biomed. J., 47."
}
],
"reference-count": 84,
"references-count": 84,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1999-4915/16/12/1836"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Characterization and Fluctuations of an Ivermectin Binding Site at the Lipid Raft Interface of the N-Terminal Domain (NTD) of the Spike Protein of SARS-CoV-2 Variants",
"type": "journal-article",
"volume": "16"
}
