Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19
et al., Open Heart, doi:10.1136/openhrt-2020-001350, Sep 2020
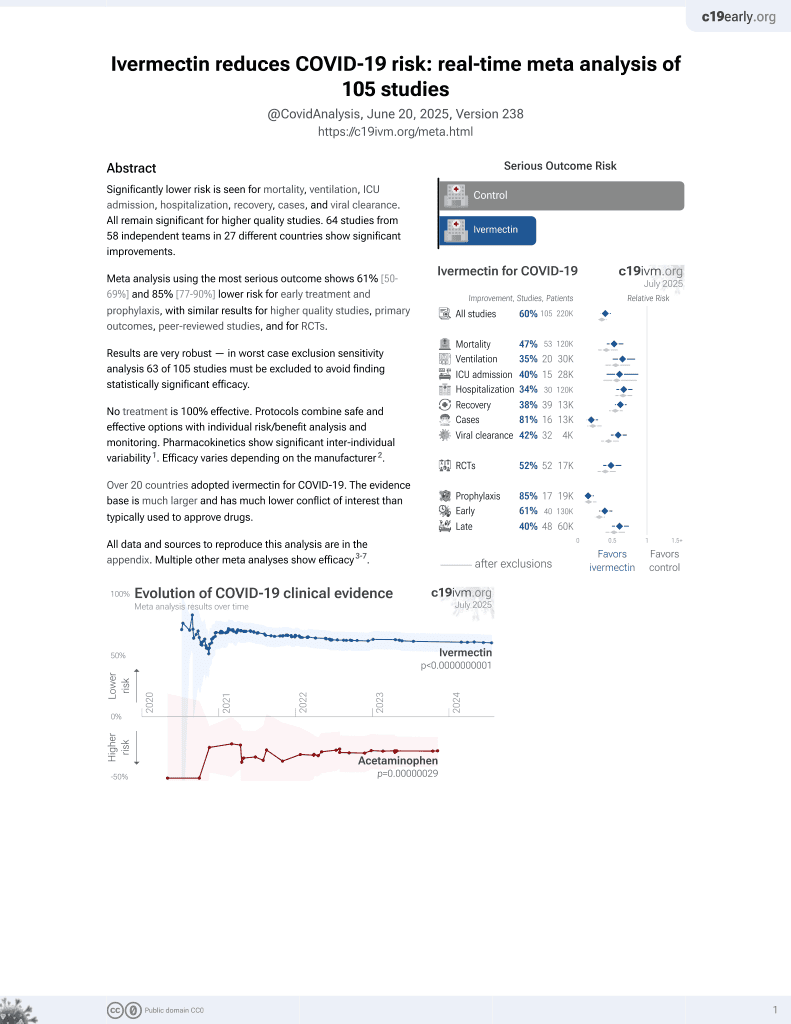
Ivermectin for COVID-19
4th treatment shown to reduce risk in
August 2020, now with p < 0.00000000001 from 106 studies, recognized in 24 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Review suggesting that ivermectin may be useful for late stage COVID-19. Authors note that ivermectin, in doses at or modestly above the standard clinical dose, may have important clinical potential for managing disorders associated with life-threatening respiratory distress and cytokine storm, such as advanced COVID-19.
1.
Reich, S., Methodological Analysis of Bias Risks in Adaptive Multi-Arm Platform Trials: A Case-Series from Three COVID-19 Studies, Center for Open Science, doi:10.31222/osf.io/h5kc8_v1.
2.
Mothae et al., SARS-CoV-2 host-pathogen interactome: insights into more players during pathogenesis, Virology, doi:10.1016/j.virol.2025.110607.
3.
Zhang et al., Rho-GTPases subfamily: cellular defectors orchestrating viral infection, Cellular & Molecular Biology Letters, doi:10.1186/s11658-025-00722-w.
4.
Saha et al., Inhaled Dry Powder of Antiviral Agents: A Promising Approach to Treating Respiratory Viral Pathogens, Viruses, doi:10.3390/v17020252.
5.
Ulloa-Aguilar et al., The Nucleolus and Its Interactions with Viral Proteins Required for Successful Infection, Cells, doi:10.3390/cells13181591.
6.
Enyeji et al., Effective Treatment of COVID-19 Infection with Repurposed Drugs: Case Reports, Viral Immunology, doi:10.1089/vim.2024.0034.
7.
Wimalawansa, S., Unlocking Insights: Navigating COVID-19 Challenges and Emulating Future Pandemic Resilience Strategies with Strengthening Natural Immunity, Heliyon, doi:10.1016/j.heliyon.2024.e34691.
8.
Shouman et al., SARS-CoV-2-associated lymphopenia: possible mechanisms and the role of CD147, Cell Communication and Signaling, doi:10.1186/s12964-024-01718-3.
9.
Mehraeen et al., Treatments for Olfactory Dysfunction in COVID-19: A Systematic Review, International Archives of Otorhinolaryngology, doi:10.1055/s-0044-1786046.
10.
Scheim et al., Back to the Basics of SARS-CoV-2 Biochemistry: Microvascular Occlusive Glycan Bindings Govern Its Morbidities and Inform Therapeutic Responses, Viruses, doi:10.3390/v16040647.
11.
Yagisawa et al., Global trends in clinical trials of ivermectin for COVID-19—Part 2, The Japanese Journal of Antibiotics, doi:10.11553/antibiotics.77.1_45.
12.
Liu et al., Crosstalk between neutrophil extracellular traps and immune regulation: insights into pathobiology and therapeutic implications of transfusion-related acute lung injury, Frontiers in Immunology, doi:10.3389/fimmu.2023.1324021.
13.
Scheim (B) et al., Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms242317039.
14.
Yemeke et al., Impact of the COVID-19 pandemic on the quality of medical products in Zimbabwe: a qualitative study based on key informant interviews with health system stakeholders, BMJ Open, doi:10.1136/bmjopen-2022-068923.
15.
Kory, P., The Global War on Ivermectin, International Covid Summit III, European Parliament, Brussels, covid19criticalcare.com/wp-content/uploads/2023/05/GLOBAL-WAR-ON-IVERMECTIN-PARLIAMENT.pdf.
16.
Babalola et al., The Place of Ivermectin in the Management of Covid-19: State of the Evidence, Medical Research Archives, doi:10.18103/mra.v11i4.3778.
17.
Loo et al., Recent Advances in Inhaled Nanoformulations of Vaccines and Therapeutics Targeting Respiratory Viral Infections, Pharmaceutical Research, doi:10.1007/s11095-023-03520-1.
18.
Scheim (C), D., From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate and Then Clot Blood Cells, Center for Open Science, doi:10.31219/osf.io/sgdj2.
19.
Kory (B), P., The Criminal Censorship of Ivermectin's Efficacy By The High-Impact Medical Journals - Part 1, Pierre Kory’s Medical Musings, pierrekory.substack.com/p/the-criminal-censorship-of-ivermectins.
20.
Al-kuraishy et al., Central effects of Ivermectin in alleviation of Covid-19-induced dysautonomia, Current Drug Targets, doi:10.2174/1389450123666220810102406.
21.
Schwartz, E., Does ivermectin have a place in the treatment of mild Covid-19?, New Microbes and New Infections, doi:10.1016/j.nmni.2022.100989.
22.
Marques et al., Ivermectin as a possible treatment for COVID-19: a review of the 2022 protocols, Brazilian Journal of Biology, doi:10.1590/1519-6984.258325.
23.
Semiz, S., SIT1 transporter as a potential novel target in treatment of COVID-19, Biomolecular Concepts, doi:10.1515/bmc-2021-0017.
24.
Zaidi et al., The mechanisms of action of ivermectin against SARS-CoV-2—an extensive review, The Journal of Antibiotics, doi:10.1038/s41429-021-00491-6.
25.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
26.
Low et al., Repositioning Ivermectin for Covid-19 treatment: Molecular mechanisms of action against SARS-CoV-2 replication, Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease, doi:10.1016/j.bbadis.2021.166294.
27.
Fordham et al., The uses and abuses of systematic reviews, OSF Preprints, doi:10.31219/osf.io/mp4f2.
28.
Kow et al., Pitfalls in Reporting Sample Size Calculation Across Randomized Controlled Trials Involving Ivermectin for the treatment of COVID-19, American Journal of Therapeutics, doi:10.1097/MJT.0000000000001441.
29.
Santin et al., Ivermectin: a multifaceted drug of Nobel prize-honored distinction with indicated efficacy against a new global scourge, COVID-19, New Microbes and New Infections, doi:10.1016/j.nmni.2021.100924.
30.
Adegboro et al., A review of the anti-viral effects of ivermectin, African Journal of Clinical and Experimental Microbiology, doi:10.4314/ajcem.v22i3.2.
31.
Turkia, M., A Continuation of a Timeline of Ivermectin-Related Events in the COVID-19 Pandemic [June 30, 2021], ResearchGate, doi:10.13140/RG.2.2.16973.36326.
32.
Jagiasi et al., Variation in therapeutic strategies for the management of severe COVID-19 in India- A nationwide cross-sectional survey, The International Journal of Clinical Practice, doi:10.1111/ijcp.14574.
33.
Lind et al., Increase in Outpatient Ivermectin Dispensing in the US During the COVID-19 Pandemic: A Cross-Sectional Analysis, Journal of General Internal Medicine, doi:10.1007/s11606-021-06948-6.
34.
Wang et al., Minimum manufacturing costs, national prices and estimated global availability of new repurposed therapies for COVID-19, medRxiv, doi:10.1101/2021.06.01.21258147.
35.
Kory (C) et al., Review of the Emerging Evidence Demonstrating the Efficacy of Ivermectin in the Prophylaxis and Treatment of COVID-19, American Journal of Therapeutics, doi:10.1097/MJT.0000000000001377.
36.
DiNicolantonio et al., Anti-inflammatory activity of ivermectin in late-stage COVID-19 may reflect activation of systemic glycine receptors, Open Heart, doi:10.1136/openhrt-2021-001655.
37.
Turkia (B), M., A timeline of ivermectin-related events in the COVID-19 pandemic, Research Gate, www.researchgate.net/publication/350610718_A_Timeline_of_Ivermectin-Related_Events_in_the_COVID-19_Pandemic_April_3_2021.
38.
Wehbe et al., Repurposing Ivermectin for COVID-19: Molecular Aspects and Therapeutic Possibilities, Front. Immunol., doi:10.3389/fimmu.2021.663586.
39.
Yagisawa (B) et al., Global trends in clinical studies of ivermectin in COVID-19, The Japanese Journal of Antibiotics, 74-1, Mar 2021, jja-contents.wdc-jp.com/pdf/JJA74/74-1-open/74-1_44-95.pdf.
40.
Jans et al., The broad spectrum host-directed agent ivermectin as an antiviral for SARS-CoV-2 ?, Biochemical and Biophysical Research Communications, doi:10.1016/j.bbrc.2020.10.042.
41.
Kory (D) et al., Review of the Emerging Evidence Demonstrating the Efficacy of Ivermectin in the Prophylaxis and Treatment of COVID-19, Frontiers in Pharmacology, doi:10.3389/fphar.2021.643369.
42.
Formiga et al., Ivermectin: an award-winning drug with expected antiviral activity against COVID-19, J. Control Release, doi:10.1016/j.jconrel.2020.10.009.
43.
Scheim (D), D., Ivermectin for COVID-19 Treatment: Clinical Response at Quasi-Threshold Doses Via Hypothesized Alleviation of CD147-Mediated Vascular Occlusion, SSRN, doi:10.2139/ssrn.3636557.
44.
Turkia (C), M., FLCCC Alliance MATH+ ascorbic acid and I-MASK+ ivermectin protocols for COVID-19 — a brief review, ResearchGate, www.researchgate.net/profile/Mika_Turkia/publication/345694745_FLCCC_Alliance_MATH_ascorbic_acid_and_I-MASK_ivermectin_protocols_for_COVID-19_-_A_Brief_Review/links/5fab010f4585150781078260/FLCCC-Alliance-MATH-ascorbic-acid-and-I-MASK-ivermectin-protocols-for-COVID-19-A-Brief-Review.pdf.
45.
Jans (B) et al., Ivermectin as a Broad-Spectrum Host-Directed Antiviral: The Real Deal?, Cells 2020, 9:9, 2100, doi:10.3390/cells9092100.
46.
Elkholy et al., Ivermectin: A Closer Look at a Potential Remedy, Cureus, doi:10.7759/cureus.10378.
47.
DiNicolantonio (B) et al., Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19, Open Heart, doi:10.1136/openhrt-2020-001350.
48.
Vora et al., White paper on Ivermectin as a potential therapy for COVID-19, Indian Journal of Tuberculosis, doi:10.1016/j.ijtb.2020.07.031.
DiNicolantonio et al., 6 Sep 2020, peer-reviewed, 3 authors.
Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19
Open Heart, doi:10.1136/openhrt-2020-001350
Author name Jorge Barroso has been corrected to Jorge Barroso-Aranda.
References
Andersson, Ottestad, Tracey, Extracellular HMGB1: a therapeutic target in severe pulmonary inflammation including COVID-19?, Mol Med, doi:10.1186/s10020-020-00172-4
Caly, Druce, Catton, The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Res, doi:10.1016/j.antiviral.2020.104787
Capellini, Venditti, Barton, Phylogeny and metabolic scaling in mammals, Ecology, doi:10.1890/09-0817.1
Ci, Li, Yu, Avermectin exerts anti-inflammatory effect by downregulating the nuclear transcription factor kappa-B and mitogen-activated protein kinase activation pathway, Fundam Clin Pharmacol, doi:10.1111/j.1472-8206.2009.00684.x
Gorial, Mashhadani, Sayaly, Effectiveness of ivermectin as add-on therapy in COVID-19 management, medRxiv
Rajter, Sm, Fatteh, Vogel, Icon (ivermectin Ni COvid nineteen) study: use of ivermectin is associated with lower mortality in hospitalized patients with COVID19, medRxiv
Schmith, Zhou, Lohmer, The Approved dose of ivermectin alone is not the ideal dose for the treatment of COVID-19, Clin Pharmacol Ther, doi:10.1002/cpt.1889
Ventre, Rozières, Lenief, Topical ivermectin improves allergic skin inflammation, Allergy, doi:10.1111/all.13118
Yan, Ci, Chen, Anti-Inflammatory effects of ivermectin in mouse model of allergic asthma, Inflamm Res, doi:10.1007/s00011-011-0307-8
Zhang, Song, Ci, Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice, Inflamm Res, doi:10.1007/s00011-008-8007-8
Zhang, Song, Xiong, Inhibitory effects of ivermectin on nitric oxide and prostaglandin E2 production in LPS-stimulated RAW 264.7 macrophages, Int Immunopharmacol, doi:10.1016/j.intimp.2008.12.016
DOI record:
{
"DOI": "10.1136/openhrt-2020-001350",
"ISSN": [
"2053-3624"
],
"URL": "http://dx.doi.org/10.1136/openhrt-2020-001350",
"alternative-id": [
"10.1136/openhrt-2020-001350"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-7888-1528",
"affiliation": [],
"authenticated-orcid": false,
"family": "DiNicolantonio",
"given": "James J",
"sequence": "first"
},
{
"affiliation": [],
"family": "Barroso",
"given": "Jorge",
"sequence": "additional"
},
{
"affiliation": [],
"family": "McCarty",
"given": "Mark",
"sequence": "additional"
}
],
"container-title": "Open Heart",
"container-title-short": "Open Heart",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"bmj.com"
]
},
"created": {
"date-parts": [
[
2020,
9,
7
]
],
"date-time": "2020-09-07T07:35:23Z",
"timestamp": 1599464123000
},
"deposited": {
"date-parts": [
[
2020,
9,
26
]
],
"date-time": "2020-09-26T10:50:00Z",
"timestamp": 1601117400000
},
"indexed": {
"date-parts": [
[
2024,
5,
14
]
],
"date-time": "2024-05-14T18:01:48Z",
"timestamp": 1715709708614
},
"is-referenced-by-count": 26,
"issue": "2",
"issued": {
"date-parts": [
[
2020,
9
]
]
},
"journal-issue": {
"issue": "2",
"published-online": {
"date-parts": [
[
2020,
9,
6
]
]
},
"published-print": {
"date-parts": [
[
2020,
9
]
]
}
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "unspecified",
"delay-in-days": 3,
"start": {
"date-parts": [
[
2020,
9,
4
]
],
"date-time": "2020-09-04T00:00:00Z",
"timestamp": 1599177600000
}
}
],
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1136/openhrt-2020-001350",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "239",
"original-title": [],
"page": "e001350",
"prefix": "10.1136",
"published": {
"date-parts": [
[
2020,
9
]
]
},
"published-online": {
"date-parts": [
[
2020,
9,
6
]
]
},
"published-print": {
"date-parts": [
[
2020,
9
]
]
},
"publisher": "BMJ",
"reference": [
{
"DOI": "10.1016/j.antiviral.2020.104787",
"article-title": "The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro",
"author": "Caly",
"doi-asserted-by": "crossref",
"journal-title": "Antiviral Res",
"key": "2020090700350916000_7.2.e001350.1",
"volume": "178",
"year": "2020"
},
{
"DOI": "10.1002/cpt.1889",
"article-title": "The Approved dose of ivermectin alone is not the ideal dose for the treatment of COVID-19",
"author": "Schmith",
"doi-asserted-by": "crossref",
"journal-title": "Clin Pharmacol Ther",
"key": "2020090700350916000_7.2.e001350.2",
"year": "2020"
},
{
"DOI": "10.1007/s00011-008-8007-8",
"doi-asserted-by": "publisher",
"key": "2020090700350916000_7.2.e001350.3"
},
{
"DOI": "10.1016/j.intimp.2008.12.016",
"article-title": "Inhibitory effects of ivermectin on nitric oxide and prostaglandin E2 production in LPS-stimulated RAW 264.7 macrophages",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "354",
"journal-title": "Int Immunopharmacol",
"key": "2020090700350916000_7.2.e001350.4",
"volume": "9",
"year": "2009"
},
{
"DOI": "10.1890/09-0817.1",
"doi-asserted-by": "publisher",
"key": "2020090700350916000_7.2.e001350.5"
},
{
"DOI": "10.1111/j.1472-8206.2009.00684.x",
"article-title": "Avermectin exerts anti-inflammatory effect by downregulating the nuclear transcription factor kappa-B and mitogen-activated protein kinase activation pathway",
"author": "Ci",
"doi-asserted-by": "crossref",
"first-page": "449",
"journal-title": "Fundam Clin Pharmacol",
"key": "2020090700350916000_7.2.e001350.6",
"volume": "23",
"year": "2009"
},
{
"DOI": "10.1007/s00011-011-0307-8",
"article-title": "Anti-Inflammatory effects of ivermectin in mouse model of allergic asthma",
"author": "Yan",
"doi-asserted-by": "crossref",
"first-page": "589",
"journal-title": "Inflamm Res",
"key": "2020090700350916000_7.2.e001350.7",
"volume": "60",
"year": "2011"
},
{
"DOI": "10.1111/all.13118",
"article-title": "Topical ivermectin improves allergic skin inflammation",
"author": "Ventre",
"doi-asserted-by": "crossref",
"first-page": "1212",
"journal-title": "Allergy",
"key": "2020090700350916000_7.2.e001350.8",
"volume": "72",
"year": "2017"
},
{
"DOI": "10.1186/s10020-020-00172-4",
"article-title": "Extracellular HMGB1: a therapeutic target in severe pulmonary inflammation including COVID-19?",
"author": "Andersson",
"doi-asserted-by": "crossref",
"first-page": "42",
"journal-title": "Mol Med",
"key": "2020090700350916000_7.2.e001350.9",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1101/2020.06.06.20124461",
"doi-asserted-by": "crossref",
"key": "2020090700350916000_7.2.e001350.10",
"unstructured": "Rajter.J.C. SM , Fatteh N , Vogel F , et al . Icon (ivermectin Ni COvid nineteen) study: use of ivermectin is associated with lower mortality in hospitalized patients with COVID19. medRxiv 2020."
},
{
"DOI": "10.1101/2020.07.07.20145979",
"doi-asserted-by": "crossref",
"key": "2020090700350916000_7.2.e001350.11",
"unstructured": "Gorial FI , Mashhadani S , Sayaly HM , et al . Effectiveness of ivermectin as add-on therapy in COVID-19 management (pilot trial). medRxiv 2020."
}
],
"reference-count": 11,
"references-count": 11,
"relation": {},
"resource": {
"primary": {
"URL": "https://openheart.bmj.com/lookup/doi/10.1136/openhrt-2020-001350"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1136/crossmarkpolicy",
"volume": "7"
}