Ivermectin for COVID-19
4th treatment shown to reduce risk in
August 2020, now with p < 0.00000000001 from 106 studies, recognized in 24 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Proposal to use inhaled ivermectin for COVID-19. Author notes that ivermectin may have broad-spectrum antiviral properties and research in this area may also be beneficial for other emerging viral outbreaks in the future.
1.
Reich, S., Methodological Analysis of Bias Risks in Adaptive Multi-Arm Platform Trials: A Case-Series from Three COVID-19 Studies, Center for Open Science, doi:10.31222/osf.io/h5kc8_v1.
2.
Mothae et al., SARS-CoV-2 host-pathogen interactome: insights into more players during pathogenesis, Virology, doi:10.1016/j.virol.2025.110607.
3.
Zhang et al., Rho-GTPases subfamily: cellular defectors orchestrating viral infection, Cellular & Molecular Biology Letters, doi:10.1186/s11658-025-00722-w.
4.
Saha et al., Inhaled Dry Powder of Antiviral Agents: A Promising Approach to Treating Respiratory Viral Pathogens, Viruses, doi:10.3390/v17020252.
5.
Ulloa-Aguilar et al., The Nucleolus and Its Interactions with Viral Proteins Required for Successful Infection, Cells, doi:10.3390/cells13181591.
6.
Enyeji et al., Effective Treatment of COVID-19 Infection with Repurposed Drugs: Case Reports, Viral Immunology, doi:10.1089/vim.2024.0034.
7.
Wimalawansa, S., Unlocking Insights: Navigating COVID-19 Challenges and Emulating Future Pandemic Resilience Strategies with Strengthening Natural Immunity, Heliyon, doi:10.1016/j.heliyon.2024.e34691.
8.
Shouman et al., SARS-CoV-2-associated lymphopenia: possible mechanisms and the role of CD147, Cell Communication and Signaling, doi:10.1186/s12964-024-01718-3.
9.
Mehraeen et al., Treatments for Olfactory Dysfunction in COVID-19: A Systematic Review, International Archives of Otorhinolaryngology, doi:10.1055/s-0044-1786046.
10.
Scheim et al., Back to the Basics of SARS-CoV-2 Biochemistry: Microvascular Occlusive Glycan Bindings Govern Its Morbidities and Inform Therapeutic Responses, Viruses, doi:10.3390/v16040647.
11.
Yagisawa et al., Global trends in clinical trials of ivermectin for COVID-19—Part 2, The Japanese Journal of Antibiotics, doi:10.11553/antibiotics.77.1_45.
12.
Liu et al., Crosstalk between neutrophil extracellular traps and immune regulation: insights into pathobiology and therapeutic implications of transfusion-related acute lung injury, Frontiers in Immunology, doi:10.3389/fimmu.2023.1324021.
13.
Scheim (B) et al., Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms242317039.
14.
Yemeke et al., Impact of the COVID-19 pandemic on the quality of medical products in Zimbabwe: a qualitative study based on key informant interviews with health system stakeholders, BMJ Open, doi:10.1136/bmjopen-2022-068923.
15.
Kory, P., The Global War on Ivermectin, International Covid Summit III, European Parliament, Brussels, covid19criticalcare.com/wp-content/uploads/2023/05/GLOBAL-WAR-ON-IVERMECTIN-PARLIAMENT.pdf.
16.
Babalola et al., The Place of Ivermectin in the Management of Covid-19: State of the Evidence, Medical Research Archives, doi:10.18103/mra.v11i4.3778.
17.
Loo et al., Recent Advances in Inhaled Nanoformulations of Vaccines and Therapeutics Targeting Respiratory Viral Infections, Pharmaceutical Research, doi:10.1007/s11095-023-03520-1.
18.
Scheim (C), D., From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate and Then Clot Blood Cells, Center for Open Science, doi:10.31219/osf.io/sgdj2.
19.
Kory (B), P., The Criminal Censorship of Ivermectin's Efficacy By The High-Impact Medical Journals - Part 1, Pierre Kory’s Medical Musings, pierrekory.substack.com/p/the-criminal-censorship-of-ivermectins.
20.
Al-kuraishy et al., Central effects of Ivermectin in alleviation of Covid-19-induced dysautonomia, Current Drug Targets, doi:10.2174/1389450123666220810102406.
21.
Schwartz, E., Does ivermectin have a place in the treatment of mild Covid-19?, New Microbes and New Infections, doi:10.1016/j.nmni.2022.100989.
22.
Marques et al., Ivermectin as a possible treatment for COVID-19: a review of the 2022 protocols, Brazilian Journal of Biology, doi:10.1590/1519-6984.258325.
23.
Semiz, S., SIT1 transporter as a potential novel target in treatment of COVID-19, Biomolecular Concepts, doi:10.1515/bmc-2021-0017.
24.
Zaidi et al., The mechanisms of action of ivermectin against SARS-CoV-2—an extensive review, The Journal of Antibiotics, doi:10.1038/s41429-021-00491-6.
25.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
26.
Low et al., Repositioning Ivermectin for Covid-19 treatment: Molecular mechanisms of action against SARS-CoV-2 replication, Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease, doi:10.1016/j.bbadis.2021.166294.
27.
Fordham et al., The uses and abuses of systematic reviews, OSF Preprints, doi:10.31219/osf.io/mp4f2.
28.
Kow et al., Pitfalls in Reporting Sample Size Calculation Across Randomized Controlled Trials Involving Ivermectin for the treatment of COVID-19, American Journal of Therapeutics, doi:10.1097/MJT.0000000000001441.
29.
Santin et al., Ivermectin: a multifaceted drug of Nobel prize-honored distinction with indicated efficacy against a new global scourge, COVID-19, New Microbes and New Infections, doi:10.1016/j.nmni.2021.100924.
30.
Adegboro et al., A review of the anti-viral effects of ivermectin, African Journal of Clinical and Experimental Microbiology, doi:10.4314/ajcem.v22i3.2.
31.
Turkia, M., A Continuation of a Timeline of Ivermectin-Related Events in the COVID-19 Pandemic [June 30, 2021], ResearchGate, doi:10.13140/RG.2.2.16973.36326.
32.
Jagiasi et al., Variation in therapeutic strategies for the management of severe COVID-19 in India- A nationwide cross-sectional survey, The International Journal of Clinical Practice, doi:10.1111/ijcp.14574.
33.
Lind et al., Increase in Outpatient Ivermectin Dispensing in the US During the COVID-19 Pandemic: A Cross-Sectional Analysis, Journal of General Internal Medicine, doi:10.1007/s11606-021-06948-6.
34.
Wang et al., Minimum manufacturing costs, national prices and estimated global availability of new repurposed therapies for COVID-19, medRxiv, doi:10.1101/2021.06.01.21258147.
35.
Kory (C) et al., Review of the Emerging Evidence Demonstrating the Efficacy of Ivermectin in the Prophylaxis and Treatment of COVID-19, American Journal of Therapeutics, doi:10.1097/MJT.0000000000001377.
36.
DiNicolantonio et al., Anti-inflammatory activity of ivermectin in late-stage COVID-19 may reflect activation of systemic glycine receptors, Open Heart, doi:10.1136/openhrt-2021-001655.
37.
Turkia (B), M., A timeline of ivermectin-related events in the COVID-19 pandemic, Research Gate, www.researchgate.net/publication/350610718_A_Timeline_of_Ivermectin-Related_Events_in_the_COVID-19_Pandemic_April_3_2021.
38.
Wehbe et al., Repurposing Ivermectin for COVID-19: Molecular Aspects and Therapeutic Possibilities, Front. Immunol., doi:10.3389/fimmu.2021.663586.
39.
Yagisawa (B) et al., Global trends in clinical studies of ivermectin in COVID-19, The Japanese Journal of Antibiotics, 74-1, Mar 2021, jja-contents.wdc-jp.com/pdf/JJA74/74-1-open/74-1_44-95.pdf.
40.
Jans et al., The broad spectrum host-directed agent ivermectin as an antiviral for SARS-CoV-2 ?, Biochemical and Biophysical Research Communications, doi:10.1016/j.bbrc.2020.10.042.
41.
Kory (D) et al., Review of the Emerging Evidence Demonstrating the Efficacy of Ivermectin in the Prophylaxis and Treatment of COVID-19, Frontiers in Pharmacology, doi:10.3389/fphar.2021.643369.
42.
Formiga et al., Ivermectin: an award-winning drug with expected antiviral activity against COVID-19, J. Control Release, doi:10.1016/j.jconrel.2020.10.009.
43.
Scheim (D), D., Ivermectin for COVID-19 Treatment: Clinical Response at Quasi-Threshold Doses Via Hypothesized Alleviation of CD147-Mediated Vascular Occlusion, SSRN, doi:10.2139/ssrn.3636557.
44.
Turkia (C), M., FLCCC Alliance MATH+ ascorbic acid and I-MASK+ ivermectin protocols for COVID-19 — a brief review, ResearchGate, www.researchgate.net/profile/Mika_Turkia/publication/345694745_FLCCC_Alliance_MATH_ascorbic_acid_and_I-MASK_ivermectin_protocols_for_COVID-19_-_A_Brief_Review/links/5fab010f4585150781078260/FLCCC-Alliance-MATH-ascorbic-acid-and-I-MASK-ivermectin-protocols-for-COVID-19-A-Brief-Review.pdf.
45.
Jans (B) et al., Ivermectin as a Broad-Spectrum Host-Directed Antiviral: The Real Deal?, Cells 2020, 9:9, 2100, doi:10.3390/cells9092100.
46.
Elkholy et al., Ivermectin: A Closer Look at a Potential Remedy, Cureus, doi:10.7759/cureus.10378.
47.
DiNicolantonio (B) et al., Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19, Open Heart, doi:10.1136/openhrt-2020-001350.
48.
Vora et al., White paper on Ivermectin as a potential therapy for COVID-19, Indian Journal of Tuberculosis, doi:10.1016/j.ijtb.2020.07.031.
Elkholy et al., 11 Sep 2020, peer-reviewed, 4 authors.
Contact: dr.karimelkholy@gmail.com.
Ivermectin: A Closer Look at a Potential Remedy
Cureus, doi:10.7759/cureus.10378
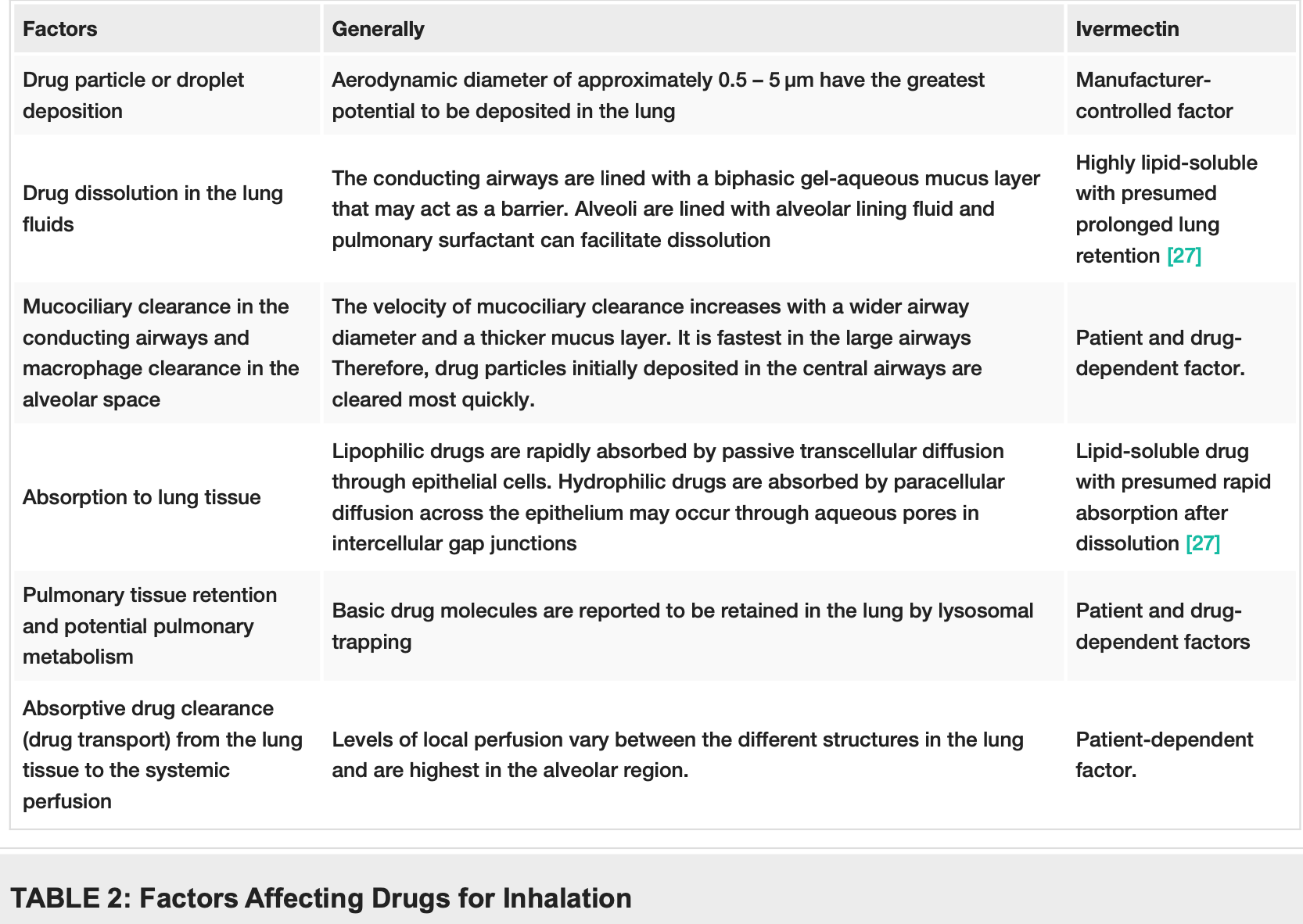
Amid the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, the search for effective treatment and vaccines has been exponentially on the rise. Finding effective treatment has been the core of attention of many scientific reports and antivirals are in the center of those treatments. Numerous antivirals are being studied for the management of the coronavirus disease 2019 (COVID-19) pneumonia caused by the SARS-CoV-2. Remdesivir was the first drug to gain emergency FDA approval to be used in COVID-19. Similarly, favipiravir, an anti-influenza drug, is being studied as a potential agent against COVID-19. Contrastingly, hydroxychloroquine has been a controversial drug in the management of COVID-19. Nevertheless, the National Institute of Health (NIH), along with the World Health Organization (WHO), have discontinued clinical trials for hydroxychloroquine as the drug showed little or no survival benefit. Ivermectin, an antihelminthic drug, has shown antiviral properties previously. Additionally, it was described to be effective in vivo against the SARS-CoV-2. However, its survival benefit in patients with COVID-19 has not been documented. We herein propose the theory of inhaled ivermectin which can attain the desired lung concentration that will render it effective against SARS-CoV-2.
Additional Information Disclosures
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
References
Beigel, Tomashek, Dodd, Remdesivir for the treatment of Covid-19 -preliminary report, {Epub ahead of print}, doi:10.1056/nejmoa2007764
Billiard, Baker, Chandrasekaran, Van Den Berg, Yang et al., PA4125: Dry powder inhaled ribavirin in healthy volunteers: safety, tolerability, lung and systemic pharmacokinetics, Eur Respir J, doi:10.1183/1393003.congress-2017.PA4125
Boivin, Goyette, Hardy, Aoki, Wagner et al., Rapid antiviral effect of inhaled zanamivir in the treatment of naturally occurring influenza in otherwise healthy adults, J Infect Dis, doi:10.1086/315392
Borghardt, Kloft, Sharma, Inhaled therapy in respiratory disease: the complex interplay of pulmonary kinetic processes, Can Respir J, doi:10.1155/2018/2732017
Cai, Yang, Liu, Experimental treatment with favipiravir for COVID-19: an open-label control study, doi:10.1016/j.eng.2020.03.007
Caly, Druce, Catton, Jans, Wagstaff, The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Res, doi:10.1016/j.antiviral.2020.104787
Canga, Prieto, Liébana, Martínez, Vega et al., The pharmacokinetics and interactions of ivermectin in humans--a mini-review, AAPS J, doi:10.1208/s12248-007-9000-9
Chiang, Sassaroli, Louie, Chen, Stecher et al., Inhibition of HIV-1 replication by hydroxychloroquine: mechanism of action and comparison with zidovudine, Clin Ther, doi:10.1016/s0149-2918(96)80063-4
Du, Chen, Favipiravir: pharmacokinetics and concerns about clinical trials for 2019-nCoV infection, Clin Pharmacol Ther, doi:10.1002/cpt.1844
Fantini, Scala, Chahinian, Yahi, Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.105960
Franks, Chong, Chui, Lung pathology of severe acute respiratory syndrome (SARS): a study of 8 autopsy cases from Singapore, Hum Pathol, doi:10.1016/s0046-8177(03)00367-8
Furuta, Gowen, Takahashi, Shiraki, Smee et al., Favipiravir (T-705), a novel viral RNA polymerase inhibitor, Antiviral Res, doi:10.1016/j.antiviral.2013.09.015
Gordon, Tchesnokov, Feng, Porter, Götte, The antiviral compound remdesivir potently inhibits RNA-dependent RNA polymerase from Middle East respiratory syndrome coronavirus, J Biol Chem, doi:10.1074/jbc.AC120.013056
Hiscox, Wurm, Wilson, Britton, Cavanagh et al., The coronavirus infectious bronchitis virus nucleoprotein localizes to the nucleolus, J Virol, doi:10.1128/jvi.75.1.506-512.2001
Ji, Cen, Lin, Hu, Fang et al., Study on the subacute inhalation toxicity of ivermectin TC in rats, Chinese J Comp Med
Krishna, Klotz, Determination of ivermectin in human plasma by high-performance liquid chromatography, Arzneimittelforschung
Kumar, Nyodu, Maurya, Saxena, Morphology, Genome Organization, Replication, and Pathogenesis 2020 Elkholy et al, Coronavirus Disease, doi:10.1007/978-981-15-4814-7_3
Martines, Ritter, Matkovic, Pathology and pathogenesis of SARS-CoV-2 associated with fatal coronavirus disease, United States, Emerg Infect Dis, doi:10.3201/eid2609.202095
Rajter, Sherman, Fatteh, Vogel, Sacks et al., ICON (Ivermectin in COvid Nineteen) study: use of ivermectin is associated with lower mortality in hospitalized patients with COVID19, doi:10.1101/2020.06.06.20124461
Rizzo, Ivermectin, antiviral properties and COVID-19: a possible new mechanism of action, Naunyn Schmiedebergs Arch Pharmacol, doi:10.1007/s00210-020-01902-5
Schmith, Zhou, Lohmer, The approved dose of ivermectin alone is not the ideal dose for the treatment of COVID-19, Clin Pharmacol Ther, doi:10.1002/cpt.1889
Timani, Liao, Ye, Nuclear/nucleolar localization properties of C-terminal nucleocapsid protein of SARS coronavirus, Virus Res, doi:10.1016/j.virusres.2005.05.007
Wulan, Heydet, Walker, Gahan, Ghildyal, Nucleocytoplasmic transport of nucleocapsid proteins of enveloped RNA viruses, Front Microbiol, doi:10.3389/fmicb.2015.00553€
Yang, Atkinson, Wang, Lee, Bogoyevitch et al., The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer, Antiviral Res, doi:10.1016/j.antiviral.2020.104760
DOI record:
{
"DOI": "10.7759/cureus.10378",
"ISSN": [
"2168-8184"
],
"URL": "http://dx.doi.org/10.7759/cureus.10378",
"author": [
{
"affiliation": [],
"family": "Elkholy",
"given": "Karim O",
"sequence": "first"
},
{
"affiliation": [],
"family": "Hegazy",
"given": "Omar",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Erdinc",
"given": "Burak",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abowali",
"given": "Hesham",
"sequence": "additional"
}
],
"container-title": "Cureus",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2020,
9,
11
]
],
"date-time": "2020-09-11T15:05:02Z",
"timestamp": 1599836702000
},
"deposited": {
"date-parts": [
[
2020,
9,
11
]
],
"date-time": "2020-09-11T15:05:06Z",
"timestamp": 1599836706000
},
"indexed": {
"date-parts": [
[
2023,
1,
7
]
],
"date-time": "2023-01-07T22:51:47Z",
"timestamp": 1673131907825
},
"is-referenced-by-count": 1,
"issued": {
"date-parts": [
[
2020,
9,
11
]
]
},
"language": "en",
"link": [
{
"URL": "https://www.cureus.com/articles/37039-ivermectin-a-closer-look-at-a-potential-remedy",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "4492",
"original-title": [],
"prefix": "10.7759",
"published": {
"date-parts": [
[
2020,
9,
11
]
]
},
"published-print": {
"date-parts": [
[
2020,
9,
11
]
]
},
"publisher": "Cureus, Inc.",
"reference": [
{
"key": "ref1",
"unstructured": "WHO Coronavirus Disease (COVID-19) Dashboard. (2020). http.//coronavirus.jhu.edu/map.html."
},
{
"DOI": "10.1007/978-981-15-4814-7_3",
"article-title": "Morphology, Genome Organization, Replication, and Pathogenesis of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)",
"author": "Kumar S",
"doi-asserted-by": "publisher",
"key": "ref2",
"unstructured": "Kumar S, Nyodu R, Maurya V, Saxena SK. Morphology, Genome Organization, Replication, and Pathogenesis of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). Coronavirus Disease 2019 (COVID-19). Epidemiology, Pathogenesis, Diagnosis, and Therapeutics. Saxena SK (ed): Springer, Singapore; 2020. 23-31. 10.1007/978-981-15-4814-7_3",
"year": "2020"
},
{
"DOI": "10.1016/s0046-8177(03)00367-8",
"article-title": "Lung pathology of severe acute respiratory syndrome (SARS): a study of 8 autopsy cases from Singapore",
"author": "Franks TJ",
"doi-asserted-by": "publisher",
"journal-title": "Hum Pathol",
"key": "ref3",
"unstructured": "Franks TJ, Chong PY, Chui P, et al.. Lung pathology of severe acute respiratory syndrome (SARS): a study of 8 autopsy cases from Singapore. Hum Pathol. 2003, 34:743-748. 10.1016/s0046-8177(03)00367-8",
"volume": "34",
"year": "2003"
},
{
"DOI": "10.3201/eid2609.202095",
"article-title": "Pathology and pathogenesis of SARS-CoV-2 associated with fatal coronavirus disease, United States",
"author": "Martines RB",
"doi-asserted-by": "publisher",
"journal-title": "Emerg Infect Dis",
"key": "ref4",
"unstructured": "Martines RB, Ritter JM, Matkovic E, et al.. Pathology and pathogenesis of SARS-CoV-2 associated with fatal coronavirus disease, United States. Emerg Infect Dis. 2020, 26:2005-2015. 10.3201/eid2609.202095",
"volume": "26",
"year": "2020"
},
{
"key": "ref5",
"unstructured": "CDC Public Health Image Library (PHIL) #23312. (2020). Accessed. August 31, 2020: http://phil.cdc.gov/Details.aspx?pid=23312."
},
{
"DOI": "10.1074/jbc.AC120.013056",
"article-title": "The antiviral compound remdesivir potently inhibits RNA-dependent RNA polymerase from Middle East respiratory syndrome coronavirus",
"author": "Gordon CJ",
"doi-asserted-by": "publisher",
"journal-title": "J Biol Chem",
"key": "ref6",
"unstructured": "Gordon CJ, Tchesnokov EP, Feng JY, Porter DP, Götte M. The antiviral compound remdesivir potently inhibits RNA-dependent RNA polymerase from Middle East respiratory syndrome coronavirus. J Biol Chem. 2020, 295:4773-4779. 10.1074/jbc.AC120.013056",
"volume": "295",
"year": "2020"
},
{
"DOI": "10.1056/nejmoa2007764",
"article-title": "Remdesivir for the treatment of Covid-19 — preliminary report",
"author": "Beigel JH",
"doi-asserted-by": "publisher",
"journal-title": "N Engl J Med",
"key": "ref7",
"unstructured": "Beigel JH, Tomashek KM, Dodd LE, et al.. Remdesivir for the treatment of Covid-19 — preliminary report. N Engl J Med. 2020, {Epub ahead of print}:NEJMoa2007764. 10.1056/nejmoa2007764",
"volume": "{Epub ahead of print}",
"year": "2020"
},
{
"DOI": "10.1016/s0149-2918(96)80063-4",
"article-title": "Inhibition of HIV-1 replication by hydroxychloroquine: mechanism of action and comparison with zidovudine",
"author": "Chiang G",
"doi-asserted-by": "publisher",
"journal-title": "Clin Ther",
"key": "ref8",
"unstructured": "Chiang G, Sassaroli M, Louie M, Chen H, Stecher VJ, Sperber K. Inhibition of HIV-1 replication by hydroxychloroquine: mechanism of action and comparison with zidovudine. Clin Ther. 1996, 18:1080-1092. 10.1016/s0149-2918(96)80063-4",
"volume": "18",
"year": "1996"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105960",
"article-title": "Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection",
"author": "Fantini J",
"doi-asserted-by": "publisher",
"journal-title": "Int J Antimicrob Agents",
"key": "ref9",
"unstructured": "Fantini J, Di Scala C, Chahinian H, Yahi N. Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection. Int J Antimicrob Agents. 2020, 55:105960. 10.1016/j.ijantimicag.2020.105960",
"volume": "55",
"year": "2020"
},
{
"key": "ref10",
"unstructured": "NIH halts clinical trial of hydroxychloroquine. (2020). http.//www.nih.gov/news-events/news-releases/nih-halts-clinical-trial-hydroxychloroquine."
},
{
"key": "ref11",
"unstructured": "WHO discontinues hydroxychloroquine and lopinavir/ritonavir treatment arms for COVID-19. (2020). Accessed. August 31, 2020: http://www.who.int/news-room/detail/04-07-2020-who-discontinues-hydroxychloroquine-and-lopinavir-ritonavir-treatment-...."
},
{
"DOI": "10.1002/cpt.1844",
"article-title": "Favipiravir: pharmacokinetics and concerns about clinical trials for 2019-nCoV infection",
"author": "Du YX",
"doi-asserted-by": "publisher",
"journal-title": "Clin Pharmacol Ther",
"key": "ref12",
"unstructured": "Du YX, Chen XP. Favipiravir: pharmacokinetics and concerns about clinical trials for 2019-nCoV infection. Clin Pharmacol Ther. 2020, 108:242-247. 10.1002/cpt.1844",
"volume": "108",
"year": "2020"
},
{
"DOI": "10.1016/j.antiviral.2013.09.015",
"article-title": "Favipiravir (T-705), a novel viral RNA polymerase inhibitor",
"author": "Furuta Y",
"doi-asserted-by": "publisher",
"journal-title": "Antiviral Res",
"key": "ref13",
"unstructured": "Furuta Y, Gowen BB, Takahashi K, Shiraki K, Smee DF, Barnard DL. Favipiravir (T-705), a novel viral RNA polymerase inhibitor. Antiviral Res. 2013, 100:446-454. 10.1016/j.antiviral.2013.09.015",
"volume": "100",
"year": "2013"
},
{
"DOI": "10.1016/j.eng.2020.03.007",
"article-title": "Experimental treatment with favipiravir for COVID-19: an open-label control study",
"author": "Cai Q",
"doi-asserted-by": "publisher",
"journal-title": "Engineering (Beijing)",
"key": "ref14",
"unstructured": "Cai Q, Yang M, Liu D, et al.. Experimental treatment with favipiravir for COVID-19: an open-label control study. Engineering (Beijing). 2020, {Epub ahead of print}:10.1016/j.eng.2020.03.007. 10.1016/j.eng.2020.03.007",
"volume": "{Epub ahead of print}",
"year": "2020"
},
{
"DOI": "10.1208/s12248-007-9000-9",
"article-title": "The pharmacokinetics and interactions of ivermectin in humans--a mini-review",
"author": "González Canga A",
"doi-asserted-by": "publisher",
"journal-title": "AAPS J",
"key": "ref15",
"unstructured": "González Canga A, Sahagún Prieto AM, Diez Liébana MJ, Fernández Martínez N, Sierra Vega M, García Vieitez JJ. The pharmacokinetics and interactions of ivermectin in humans--a mini-review. AAPS J. 2008, 10:42-46. 10.1208/s12248-007-9000-9",
"volume": "10",
"year": "2008"
},
{
"DOI": "10.1007/s00210-020-01902-5",
"article-title": "Ivermectin, antiviral properties and COVID- 19: a possible new mechanism of action",
"author": "Rizzo E",
"doi-asserted-by": "publisher",
"journal-title": "Naunyn Schmiedebergs Arch Pharmacol",
"key": "ref16",
"unstructured": "Rizzo E. Ivermectin, antiviral properties and COVID- 19: a possible new mechanism of action. Naunyn Schmiedebergs Arch Pharmacol. 2020, 393:1153-1156. 10.1007/s00210-020-01902-5",
"volume": "393",
"year": "2020"
},
{
"DOI": "10.1016/j.antiviral.2020.104760",
"article-title": "The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer",
"author": "Yang SNY",
"doi-asserted-by": "publisher",
"journal-title": "Antiviral Res",
"key": "ref17",
"unstructured": "Yang SNY, Atkinson SC, Wang C, Lee A, Bogoyevitch MA, Borg NA, Jans DA. The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer. Antiviral Res. 2020, 177:104760. 10.1016/j.antiviral.2020.104760",
"volume": "177",
"year": "2020"
},
{
"DOI": "10.1016/j.virusres.2005.05.007",
"article-title": "Nuclear/nucleolar localization properties of C-terminal nucleocapsid protein of SARS coronavirus",
"author": "Timani KA",
"doi-asserted-by": "publisher",
"journal-title": "Virus Res",
"key": "ref18",
"unstructured": "Timani KA, Liao Q, Ye L, et al.. Nuclear/nucleolar localization properties of C-terminal nucleocapsid protein of SARS coronavirus. Virus Res. 2005, 114:23-34. 10.1016/j.virusres.2005.05.007",
"volume": "114",
"year": "2005"
},
{
"DOI": "10.1128/jvi.75.1.506-512.2001",
"article-title": "The coronavirus infectious bronchitis virus nucleoprotein localizes to the nucleolus",
"author": "Hiscox JA",
"doi-asserted-by": "publisher",
"journal-title": "J Virol",
"key": "ref19",
"unstructured": "Hiscox JA, Wurm T, Wilson L, Britton P, Cavanagh D, Brooks G. The coronavirus infectious bronchitis virus nucleoprotein localizes to the nucleolus. J Virol. 2001, 75:506-512. 10.1128/jvi.75.1.506-512.2001",
"volume": "75",
"year": "2001"
},
{
"DOI": "10.3389/fmicb.2015.00553 ",
"article-title": "Nucleocytoplasmic transport of nucleocapsid proteins of enveloped RNA viruses",
"author": "Wulan WN",
"doi-asserted-by": "publisher",
"journal-title": "Front Microbiol",
"key": "ref20",
"unstructured": "Wulan WN, Heydet D, Walker EJ, Gahan ME, Ghildyal R. Nucleocytoplasmic transport of nucleocapsid proteins of enveloped RNA viruses. Front Microbiol. 2015, 6:553. 10.3389/fmicb.2015.00553 ",
"volume": "6",
"year": "2015"
},
{
"DOI": "10.1016/j.antiviral.2020.104787",
"article-title": "The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro",
"author": "Caly L",
"doi-asserted-by": "publisher",
"journal-title": "Antiviral Res",
"key": "ref21",
"unstructured": "Caly L, Druce JD, Catton MG, Jans DA, Wagstaff KM. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Res. 2020, 178:104787. 10.1016/j.antiviral.2020.104787",
"volume": "178",
"year": "2020"
},
{
"DOI": "10.1002/cpt.1889",
"article-title": "The approved dose of ivermectin alone is not the ideal dose for the treatment of COVID‐19",
"author": "Schmith VD",
"doi-asserted-by": "publisher",
"journal-title": "Clin Pharmacol Ther",
"key": "ref22",
"unstructured": "Schmith VD, Zhou JJ, Lohmer LRL. The approved dose of ivermectin alone is not the ideal dose for the treatment of COVID‐19. Clin Pharmacol Ther. 2020, {Epub ahead of print}:10.1002/cpt.1889. 10.1002/cpt.1889",
"volume": "{Epub ahead of print}",
"year": "2020"
},
{
"DOI": "10.1101/2020.06.06.20124461",
"article-title": "ICON (Ivermectin in COvid Nineteen) study: use of ivermectin is associated with lower mortality in hospitalized patients with COVID19 [PREPRINT]",
"author": "Rajter JC",
"doi-asserted-by": "publisher",
"journal-title": "medRxiv",
"key": "ref23",
"unstructured": "Rajter JC, Sherman M, Fatteh N, Vogel F, Sacks J, Rajter JJ. ICON (Ivermectin in COvid Nineteen) study: use of ivermectin is associated with lower mortality in hospitalized patients with COVID19 [PREPRINT]. medRxiv. 2020, 2020.06.06.20124461. 10.1101/2020.06.06.20124461",
"year": "2020"
},
{
"DOI": "10.1183/1393003.congress-2017.PA4125",
"article-title": "PA4125: Dry powder inhaled ribavirin in healthy volunteers: safety, tolerability, lung and systemic pharmacokinetics",
"author": "Billiard J",
"doi-asserted-by": "publisher",
"journal-title": "Eur Respir J",
"key": "ref24",
"unstructured": "Billiard J, Baker S, Chandrasekaran V, van den Berg F, Yang S, Dumont E. PA4125: Dry powder inhaled ribavirin in healthy volunteers: safety, tolerability, lung and systemic pharmacokinetics. Eur Respir J. 2017, 50:4125. 10.1183/1393003.congress-2017.PA4125",
"volume": "50",
"year": "2017"
},
{
"DOI": "10.1086/315392",
"article-title": "Rapid antiviral effect of inhaled zanamivir in the treatment of naturally occurring influenza in otherwise healthy adults",
"author": "Boivin G",
"doi-asserted-by": "publisher",
"journal-title": "J Infect Dis",
"key": "ref25",
"unstructured": "Boivin G, Goyette N, Hardy I, Aoki F, Wagner A, Trottier S. Rapid antiviral effect of inhaled zanamivir in the treatment of naturally occurring influenza in otherwise healthy adults. J Infect Dis. 2000, 181:1471-1474. 10.1086/315392",
"volume": "181",
"year": "2000"
},
{
"DOI": "10.1155/2018/2732017",
"article-title": "Inhaled therapy in respiratory disease: the complex interplay of pulmonary kinetic processes",
"author": "Borghardt JM",
"doi-asserted-by": "publisher",
"journal-title": "Can Respir J",
"key": "ref26",
"unstructured": "Borghardt JM, Kloft C, Sharma A. Inhaled therapy in respiratory disease: the complex interplay of pulmonary kinetic processes. Can Respir J. 2018, 2018:2732017. 10.1155/2018/2732017",
"volume": "2018",
"year": "2018"
},
{
"article-title": "Determination of ivermectin in human plasma by high-performance liquid chromatography",
"author": "Krishna DR",
"journal-title": "Arzneimittelforschung",
"key": "ref27",
"unstructured": "Krishna DR, Klotz U. Determination of ivermectin in human plasma by high-performance liquid chromatography. Arzneimittelforschung. 1993, 43:609-611.",
"volume": "43",
"year": "1993"
},
{
"article-title": "Study on the subacute inhalation toxicity of ivermectin TC in rats",
"author": "Ji L",
"journal-title": "Chinese J Comp Med",
"key": "ref28",
"unstructured": "Ji L, Cen J, Lin S, Hu C, Fang H, Xu J, Chen J. Study on the subacute inhalation toxicity of ivermectin TC in rats. Chinese J Comp Med. 2016, 26:70-74.",
"volume": "26",
"year": "2016"
}
],
"reference-count": 28,
"references-count": 28,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.cureus.com/articles/37039-ivermectin-a-closer-look-at-a-potential-remedy"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Aerospace Engineering"
],
"subtitle": [],
"title": "Ivermectin: A Closer Look at a Potential Remedy",
"type": "journal-article"
}