Enhanced In Vitro Antiviral Activity of Ivermectin-Loaded Nanostructured Lipid Carriers against Porcine Epidemic Diarrhea Virus via Improved Intracellular Delivery
et al., Pharmaceutics, doi:10.3390/pharmaceutics16050601, Apr 2024
Ivermectin for COVID-19
4th treatment shown to reduce risk in
August 2020, now with p < 0.00000000001 from 106 studies, recognized in 24 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
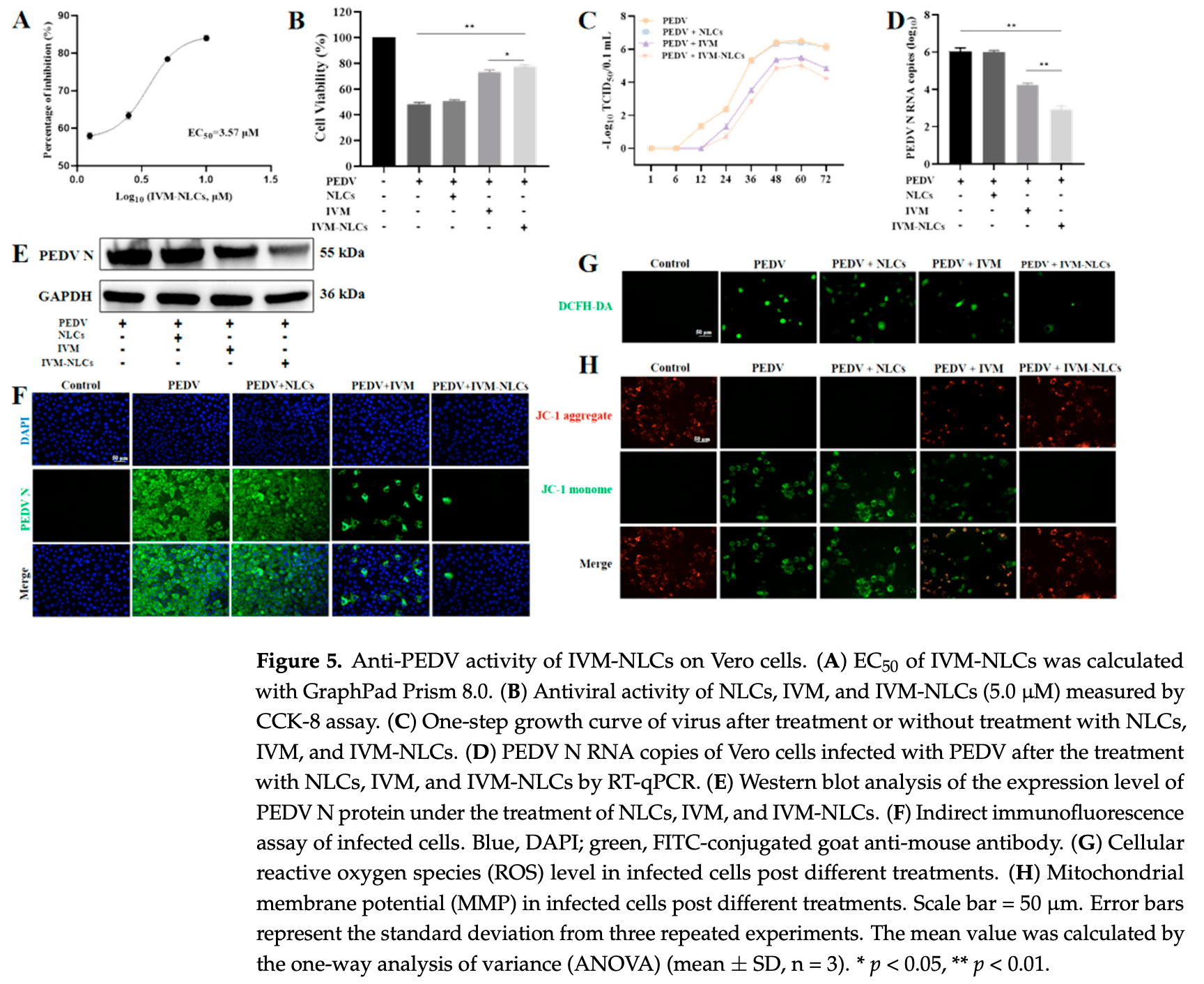
Non-COVID-19 in vitro study showing enhanced antiviral activity of ivermectin against porcine epidemic diarrhea virus when loaded into nanostructured lipid carriers. Ivermectin-loaded nanostructured lipid carriers (IVM-NLCs) inhibited viral proliferation by up to 3 orders of magnitude compared to free ivermectin. IVM-NLCs also reduced reactive oxygen species accumulation, mitigated mitochondrial dysfunction, and decreased apoptosis in infected cells compared to free ivermectin. The enhanced efficacy is attributed to improved intracellular delivery of ivermectin by the nanostructured lipid carriers.
While this is not a COVID-19 study, the IVM-NLCs may potentially have similar advantages for COVID-19. As SARS-CoV-2 replicates inside host cells, improved intracellular delivery of ivermectin could be beneficial for COVID-19 treatment. IVM-NLCs reduced reactive oxygen species accumulation, mitigated mitochondrial dysfunction, and decreased apoptosis in PEDV-infected cells. These effects could potentially help to reduce the severity of COVID-19 by limiting virus-induced cell damage.
74 preclinical studies support the efficacy of ivermectin for COVID-19:
Ivermectin, better known for antiparasitic activity, is a broad spectrum antiviral with activity against many viruses including H7N771, Dengue37,72,73 , HIV-173, Simian virus 4074, Zika37,75,76 , West Nile76, Yellow Fever77,78, Japanese encephalitis77, Chikungunya78, Semliki Forest virus78, Human papillomavirus57, Epstein-Barr57, BK Polyomavirus79, and Sindbis virus78.
Ivermectin inhibits importin-α/β-dependent nuclear import of viral proteins71,73,74,80 , shows spike-ACE2 disruption at 1nM with microfluidic diffusional sizing38, binds to glycan sites on the SARS-CoV-2 spike protein preventing interaction with blood and epithelial cells and inhibiting hemagglutination41,81, shows dose-dependent inhibition of wildtype and omicron variants36, exhibits dose-dependent inhibition of lung injury61,66, may inhibit SARS-CoV-2 via IMPase inhibition37, may inhibit SARS-CoV-2 induced formation of fibrin clots resistant to degradation9, inhibits SARS-CoV-2 3CLpro54, may inhibit SARS-CoV-2 RdRp activity28, may minimize viral myocarditis by inhibiting NF-κB/p65-mediated inflammation in macrophages60, may be beneficial for COVID-19 ARDS by blocking GSDMD and NET formation82, may interfere with SARS-CoV-2's immune evasion via ORF8 binding4, may inhibit SARS-CoV-2 by disrupting CD147 interaction83-86, may inhibit SARS-CoV-2 attachment to lipid rafts via spike NTD binding2, shows protection against inflammation, cytokine storm, and mortality in an LPS mouse model sharing key pathological features of severe COVID-1959,87, may be beneficial in severe COVID-19 by binding IGF1 to inhibit the promotion of inflammation, fibrosis, and cell proliferation that leads to lung damage8, may minimize SARS-CoV-2 induced cardiac damage40,48, may counter immune evasion by inhibiting NSP15-TBK1/KPNA1 interaction and restoring IRF3 activation88, may disrupt SARS-CoV-2 N and ORF6 protein nuclear transport and their suppression of host interferon responses1, reduces TAZ/YAP nuclear import, relieving SARS-CoV-2-driven suppression of IRF3 and NF-κB antiviral pathways35, increases Bifidobacteria which play a key role in the immune system89, has immunomodulatory51 and anti-inflammatory70,90 properties, and has an extensive and very positive safety profile91.
1.
Gayozo et al., Binding affinities analysis of ivermectin, nucleocapsid and ORF6 proteins of SARS-CoV-2 to human importins α isoforms: A computational approach, Biotecnia, doi:10.18633/biotecnia.v27.2485.
2.
Lefebvre et al., Characterization and Fluctuations of an Ivermectin Binding Site at the Lipid Raft Interface of the N-Terminal Domain (NTD) of the Spike Protein of SARS-CoV-2 Variants, Viruses, doi:10.3390/v16121836.
3.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
4.
Bagheri-Far et al., Non-spike protein inhibition of SARS-CoV-2 by natural products through the key mediator protein ORF8, Molecular Biology Research Communications, doi:10.22099/mbrc.2024.50245.2001.
5.
de Oliveira Só et al., In Silico Comparative Analysis of Ivermectin and Nirmatrelvir Inhibitors Interacting with the SARS-CoV-2 Main Protease, Preprints, doi:10.20944/preprints202404.1825.v1.
6.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
7.
Oranu et al., Validation of the binding affinities and stabilities of ivermectin and moxidectin against SARS-CoV-2 receptors using molecular docking and molecular dynamics simulation, GSC Biological and Pharmaceutical Sciences, doi:10.30574/gscbps.2024.26.1.0030.
8.
Zhao et al., Identification of the shared gene signatures between pulmonary fibrosis and pulmonary hypertension using bioinformatics analysis, Frontiers in Immunology, doi:10.3389/fimmu.2023.1197752.
9.
Vottero et al., Computational Prediction of the Interaction of Ivermectin with Fibrinogen, Molecular Sciences, doi:10.3390/ijms241411449.
10.
Chellasamy et al., Docking and molecular dynamics studies of human ezrin protein with a modelled SARS-CoV-2 endodomain and their interaction with potential invasion inhibitors, Journal of King Saud University - Science, doi:10.1016/j.jksus.2022.102277.
11.
Umar et al., Inhibitory potentials of ivermectin, nafamostat, and camostat on spike protein and some nonstructural proteins of SARS-CoV-2: Virtual screening approach, Jurnal Teknologi Laboratorium, doi:10.29238/teknolabjournal.v11i1.344.
12.
Alvarado et al., Interaction of the New Inhibitor Paxlovid (PF-07321332) and Ivermectin With the Monomer of the Main Protease SARS-CoV-2: A Volumetric Study Based on Molecular Dynamics, Elastic Networks, Classical Thermodynamics and SPT, Computational Biology and Chemistry, doi:10.1016/j.compbiolchem.2022.107692.
13.
Aminpour et al., In Silico Analysis of the Multi-Targeted Mode of Action of Ivermectin and Related Compounds, Computation, doi:10.3390/computation10040051.
14.
Parvez et al., Insights from a computational analysis of the SARS-CoV-2 Omicron variant: Host–pathogen interaction, pathogenicity, and possible drug therapeutics, Immunity, Inflammation and Disease, doi:10.1002/iid3.639.
15.
Francés-Monerris et al., Microscopic interactions between ivermectin and key human and viral proteins involved in SARS-CoV-2 infection, Physical Chemistry Chemical Physics, doi:10.1039/D1CP02967C.
16.
González-Paz et al., Comparative study of the interaction of ivermectin with proteins of interest associated with SARS-CoV-2: A computational and biophysical approach, Biophysical Chemistry, doi:10.1016/j.bpc.2021.106677.
17.
González-Paz (B) et al., Structural Deformability Induced in Proteins of Potential Interest Associated with COVID-19 by binding of Homologues present in Ivermectin: Comparative Study Based in Elastic Networks Models, Journal of Molecular Liquids, doi:10.1016/j.molliq.2021.117284.
18.
Rana et al., A Computational Study of Ivermectin and Doxycycline Combination Drug Against SARS-CoV-2 Infection, Research Square, doi:10.21203/rs.3.rs-755838/v1.
19.
Muthusamy et al., Virtual Screening Reveals Potential Anti-Parasitic Drugs Inhibiting the Receptor Binding Domain of SARS-CoV-2 Spike protein, Journal of Virology & Antiviral Research, www.scitechnol.com/abstract/virtual-screening-reveals-potential-antiparasitic-drugs-inhibiting-the-receptor-binding-domain-of-sarscov2-spike-protein-16398.html.
20.
Qureshi et al., Mechanistic insights into the inhibitory activity of FDA approved ivermectin against SARS-CoV-2: old drug with new implications, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1906750.
21.
Schöning et al., Highly-transmissible Variants of SARS-CoV-2 May Be More Susceptible to Drug Therapy Than Wild Type Strains, Research Square, doi:10.21203/rs.3.rs-379291/v1.
22.
Bello et al., Elucidation of the inhibitory activity of ivermectin with host nuclear importin α and several SARS-CoV-2 targets, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1911857.
23.
Udofia et al., In silico studies of selected multi-drug targeting against 3CLpro and nsp12 RNA-dependent RNA-polymerase proteins of SARS-CoV-2 and SARS-CoV, Network Modeling Analysis in Health Informatics and Bioinformatics, doi:10.1007/s13721-021-00299-2.
24.
Choudhury et al., Exploring the binding efficacy of ivermectin against the key proteins of SARS-CoV-2 pathogenesis: an in silico approach, Future Medicine, doi:10.2217/fvl-2020-0342.
25.
Kern et al., Modeling of SARS-CoV-2 Treatment Effects for Informed Drug Repurposing, Frontiers in Pharmacology, doi:10.3389/fphar.2021.625678.
26.
Saha et al., The Binding mechanism of ivermectin and levosalbutamol with spike protein of SARS-CoV-2, Structural Chemistry, doi:10.1007/s11224-021-01776-0.
27.
Eweas et al., Molecular Docking Reveals Ivermectin and Remdesivir as Potential Repurposed Drugs Against SARS-CoV-2, Frontiers in Microbiology, doi:10.3389/fmicb.2020.592908.
28.
Parvez (B) et al., Prediction of potential inhibitors for RNA-dependent RNA polymerase of SARS-CoV-2 using comprehensive drug repurposing and molecular docking approach, International Journal of Biological Macromolecules, doi:10.1016/j.ijbiomac.2020.09.098.
29.
Francés-Monerris (B) et al., Has Ivermectin Virus-Directed Effects against SARS-CoV-2? Rationalizing the Action of a Potential Multitarget Antiviral Agent, ChemRxiv, doi:10.26434/chemrxiv.12782258.v1.
30.
Kalhor et al., Repurposing of the approved small molecule drugs in order to inhibit SARS-CoV-2 S protein and human ACE2 interaction through virtual screening approaches, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2020.1824816.
31.
Swargiary, A., Ivermectin as a promising RNA-dependent RNA polymerase inhibitor and a therapeutic drug against SARS-CoV2: Evidence from in silico studies, Research Square, doi:10.21203/rs.3.rs-73308/v1.
32.
Maurya, D., A Combination of Ivermectin and Doxycycline Possibly Blocks the Viral Entry and Modulate the Innate Immune Response in COVID-19 Patients, American Chemical Society (ACS), doi:10.26434/chemrxiv.12630539.v1.
33.
Lehrer et al., Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2, In Vivo, 34:5, 3023-3026, doi:10.21873/invivo.12134.
34.
Suravajhala et al., Comparative Docking Studies on Curcumin with COVID-19 Proteins, Preprints, doi:10.20944/preprints202005.0439.v3.
35.
Kofler et al., M-Motif, a potential non-conventional NLS in YAP/TAZ and other cellular and viral proteins that inhibits classic protein import, iScience, doi:10.1016/j.isci.2025.112105.
36.
Shahin et al., The selective effect of Ivermectin on different human coronaviruses; in-vitro study, Research Square, doi:10.21203/rs.3.rs-4180797/v1.
37.
Jitobaom et al., Identification of inositol monophosphatase as a broad‐spectrum antiviral target of ivermectin, Journal of Medical Virology, doi:10.1002/jmv.29552.
38.
Fauquet et al., Microfluidic Diffusion Sizing Applied to the Study of Natural Products and Extracts That Modulate the SARS-CoV-2 Spike RBD/ACE2 Interaction, Molecules, doi:10.3390/molecules28248072.
39.
García-Aguilar et al., In Vitro Analysis of SARS-CoV-2 Spike Protein and Ivermectin Interaction, International Journal of Molecular Sciences, doi:10.3390/ijms242216392.
40.
Liu et al., SARS-CoV-2 viral genes Nsp6, Nsp8, and M compromise cellular ATP levels to impair survival and function of human pluripotent stem cell-derived cardiomyocytes, Stem Cell Research & Therapy, doi:10.1186/s13287-023-03485-3.
41.
Boschi et al., SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects, bioRxiv, doi:10.1101/2022.11.24.517882.
42.
De Forni et al., Synergistic drug combinations designed to fully suppress SARS-CoV-2 in the lung of COVID-19 patients, PLoS ONE, doi:10.1371/journal.pone.0276751.
43.
Saha (B) et al., Manipulation of Spray-Drying Conditions to Develop an Inhalable Ivermectin Dry Powder, Pharmaceutics, doi:10.3390/pharmaceutics14071432.
44.
Jitobaom (B) et al., Synergistic anti-SARS-CoV-2 activity of repurposed anti-parasitic drug combinations, BMC Pharmacology and Toxicology, doi:10.1186/s40360-022-00580-8.
45.
Croci et al., Liposomal Systems as Nanocarriers for the Antiviral Agent Ivermectin, International Journal of Biomaterials, doi:10.1155/2016/8043983.
46.
Zheng et al., Red blood cell-hitchhiking mediated pulmonary delivery of ivermectin: Effects of nanoparticle properties, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121719.
47.
Delandre et al., Antiviral Activity of Repurposing Ivermectin against a Panel of 30 Clinical SARS-CoV-2 Strains Belonging to 14 Variants, Pharmaceuticals, doi:10.3390/ph15040445.
48.
Liu (B) et al., Genome-wide analyses reveal the detrimental impacts of SARS-CoV-2 viral gene Orf9c on human pluripotent stem cell-derived cardiomyocytes, Stem Cell Reports, doi:10.1016/j.stemcr.2022.01.014.
49.
Segatori et al., Effect of Ivermectin and Atorvastatin on Nuclear Localization of Importin Alpha and Drug Target Expression Profiling in Host Cells from Nasopharyngeal Swabs of SARS-CoV-2- Positive Patients, Viruses, doi:10.3390/v13102084.
50.
Jitobaom (C) et al., Favipiravir and Ivermectin Showed in Vitro Synergistic Antiviral Activity against SARS-CoV-2, Research Square, doi:10.21203/rs.3.rs-941811/v1.
51.
Munson et al., Niclosamide and ivermectin modulate caspase-1 activity and proinflammatory cytokine secretion in a monocytic cell line, British Society For Nanomedicine Early Career Researcher Summer Meeting, 2021, web.archive.org/web/20230401070026/https://michealmunson.github.io/COVID.pdf.
52.
Mountain Valley MD, Mountain Valley MD Receives Successful Results From BSL-4 COVID-19 Clearance Trial on Three Variants Tested With Ivectosol™, 5/18, www.globenewswire.com/en/news-release/2021/05/18/2231755/0/en/Mountain-Valley-MD-Receives-Successful-Results-From-BSL-4-COVID-19-Clearance-Trial-on-Three-Variants-Tested-With-Ivectosol.html.
53.
Yesilbag et al., Ivermectin also inhibits the replication of bovine respiratory viruses (BRSV, BPIV-3, BoHV-1, BCoV and BVDV) in vitro, Virus Research, doi:10.1016/j.virusres.2021.198384.
54.
Mody et al., Identification of 3-chymotrypsin like protease (3CLPro) inhibitors as potential anti-SARS-CoV-2 agents, Communications Biology, doi:10.1038/s42003-020-01577-x.
55.
Jeffreys et al., Remdesivir-ivermectin combination displays synergistic interaction with improved in vitro activity against SARS-CoV-2, International Journal of Antimicrobial Agents, doi:10.1016/j.ijantimicag.2022.106542.
56.
Surnar et al., Clinically Approved Antiviral Drug in an Orally Administrable Nanoparticle for COVID-19, ACS Pharmacol. Transl. Sci., doi:10.1021/acsptsci.0c00179.
57.
Li et al., Quantitative proteomics reveals a broad-spectrum antiviral property of ivermectin, benefiting for COVID-19 treatment, J. Cellular Physiology, doi:10.1002/jcp.30055.
58.
Caly et al., The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Research, doi:10.1016/j.antiviral.2020.104787.
59.
Zhang et al., Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice, Inflammation Research, doi:10.1007/s00011-008-8007-8.
60.
Gao et al., Ivermectin ameliorates acute myocarditis via the inhibition of importin-mediated nuclear translocation of NF-κB/p65, International Immunopharmacology, doi:10.1016/j.intimp.2024.112073.
61.
Abd-Elmawla et al., Suppression of NLRP3 inflammasome by ivermectin ameliorates bleomycin-induced pulmonary fibrosis, Journal of Zhejiang University-SCIENCE B, doi:10.1631/jzus.B2200385.
62.
Uematsu et al., Prophylactic administration of ivermectin attenuates SARS-CoV-2 induced disease in a Syrian Hamster Model, The Journal of Antibiotics, doi:10.1038/s41429-023-00623-0.
63.
Albariqi et al., Pharmacokinetics and Safety of Inhaled Ivermectin in Mice as a Potential COVID-19 Treatment, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121688.
64.
Errecalde et al., Safety and Pharmacokinetic Assessments of a Novel Ivermectin Nasal Spray Formulation in a Pig Model, Journal of Pharmaceutical Sciences, doi:10.1016/j.xphs.2021.01.017.
65.
Madrid et al., Safety of oral administration of high doses of ivermectin by means of biocompatible polyelectrolytes formulation, Heliyon, doi:10.1016/j.heliyon.2020.e05820.
66.
Ma et al., Ivermectin contributes to attenuating the severity of acute lung injury in mice, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2022.113706.
67.
de Melo et al., Attenuation of clinical and immunological outcomes during SARS-CoV-2 infection by ivermectin, EMBO Mol. Med., doi:10.15252/emmm.202114122.
68.
Arévalo et al., Ivermectin reduces in vivo coronavirus infection in a mouse experimental model, Scientific Reports, doi:10.1038/s41598-021-86679-0.
69.
Chaccour et al., Nebulized ivermectin for COVID-19 and other respiratory diseases, a proof of concept, dose-ranging study in rats, Scientific Reports, doi:10.1038/s41598-020-74084-y.
70.
Yan et al., Anti-inflammatory effects of ivermectin in mouse model of allergic asthma, Inflammation Research, doi:10.1007/s00011-011-0307-8.
71.
Götz et al., Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import, Scientific Reports, doi:10.1038/srep23138.
72.
Tay et al., Nuclear localization of dengue virus (DENV) 1–4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin, Antiviral Research, doi:10.1016/j.antiviral.2013.06.002.
73.
Wagstaff et al., Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus, Biochemical Journal, doi:10.1042/BJ20120150.
74.
Wagstaff (B) et al., An AlphaScreen®-Based Assay for High-Throughput Screening for Specific Inhibitors of Nuclear Import, SLAS Discovery, doi:10.1177/1087057110390360.
75.
Barrows et al., A Screen of FDA-Approved Drugs for Inhibitors of Zika Virus Infection, Cell Host & Microbe, doi:10.1016/j.chom.2016.07.004.
76.
Yang et al., The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer, Antiviral Research, doi:10.1016/j.antiviral.2020.104760.
77.
Mastrangelo et al., Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: new prospects for an old drug, Journal of Antimicrobial Chemotherapy, doi:10.1093/jac/dks147.
78.
Varghese et al., Discovery of berberine, abamectin and ivermectin as antivirals against chikungunya and other alphaviruses, Antiviral Research, doi:10.1016/j.antiviral.2015.12.012.
79.
Bennett et al., Role of a nuclear localization signal on the minor capsid Proteins VP2 and VP3 in BKPyV nuclear entry, Virology, doi:10.1016/j.virol.2014.10.013.
80.
Kosyna et al., The importin α/β-specific inhibitor Ivermectin affects HIF-dependent hypoxia response pathways, Biological Chemistry, doi:10.1515/hsz-2015-0171.
81.
Scheim et al., Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms242317039.
82.
Liu (C) et al., Crosstalk between neutrophil extracellular traps and immune regulation: insights into pathobiology and therapeutic implications of transfusion-related acute lung injury, Frontiers in Immunology, doi:10.3389/fimmu.2023.1324021.
83.
Shouman et al., SARS-CoV-2-associated lymphopenia: possible mechanisms and the role of CD147, Cell Communication and Signaling, doi:10.1186/s12964-024-01718-3.
84.
Scheim (B), D., Ivermectin for COVID-19 Treatment: Clinical Response at Quasi-Threshold Doses Via Hypothesized Alleviation of CD147-Mediated Vascular Occlusion, SSRN, doi:10.2139/ssrn.3636557.
85.
Scheim (C), D., From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate and Then Clot Blood Cells, Center for Open Science, doi:10.31219/osf.io/sgdj2.
86.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
87.
DiNicolantonio et al., Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19, Open Heart, doi:10.1136/openhrt-2020-001350.
88.
Mothae et al., SARS-CoV-2 host-pathogen interactome: insights into more players during pathogenesis, Virology, doi:10.1016/j.virol.2025.110607.
89.
Hazan et al., Treatment with Ivermectin Increases the Population of Bifidobacterium in the Gut, ACG 2023, acg2023posters.eventscribe.net/posterspeakers.asp.
Xu et al., 29 Apr 2024, China, peer-reviewed, 12 authors.
Contact: gdawei0123@njau.edu.cn (corresponding author).
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Enhanced In Vitro Antiviral Activity of Ivermectin-Loaded Nanostructured Lipid Carriers against Porcine Epidemic Diarrhea Virus via Improved Intracellular Delivery
Pharmaceutics, doi:10.3390/pharmaceutics16050601
Porcine epidemic diarrhea virus (PEDV) is an acute enteric coronavirus, inducing watery diarrhea and high mortality in piglets, leading to huge economic losses in global pig industry. Ivermectin (IVM), an FDA-approved antiparasitic agent, is characterized by high efficacy and wide applicability. However, the poor bioavailability limits its application. Since the virus is parasitized inside the host cells, increasing the intracellular drug uptake can improve antiviral efficacy. Hence, we aimed to develop nanostructured lipid carriers (NLCs) to enhance the antiviral efficacy of IVM. The findings first revealed the capacity of IVM to inhibit the infectivity of PEDV by reducing viral replication with a certain direct inactivation effect. The as-prepared IVM-NLCs possessed hydrodynamic diameter of 153.5 nm with a zeta potential of -31.5 mV and high encapsulation efficiency (95.72%) and drug loading (11.17%). IVM interacted with lipids and was enveloped in lipid carriers with an amorphous state. Furthermore, its encapsulation in NLCs could enhance drug internalization. Meanwhile, IVM-NLCs inhibited PEDV proliferation by up to three orders of magnitude in terms of viral RNA copies, impeding the accumulation of reactive oxygen species and mitigating the mitochondrial dysfunction caused by PEDV infection. Moreover, IVM-NLCs markedly decreased the apoptosis rate of PEDV-induced Vero cells. Hence, IVM-NLCs showed superior inhibitory effect against PEDV compared to free IVM. Together, these results implied that NLCs is an efficient delivery system for IVM to improve its antiviral efficacy against PEDV via enhanced intracellular uptake.
to biological tests, IVM-NLCs exhibited stronger antiviral activity against PEDV than free IVM and reduced PEDV-induced mitochondrial dysfunction, which prevented ROS generation and improved viability of infected Vero cell. Moreover, IVM-NLCs also reduced PEDV-induced cell apoptosis rate. In view of the in vitro results, it would be necessary to carry out in vivo tests as soon as possible, to explore its potential in the clinical treatment of PEDV. Consequently, IVM-NLCs were demonstrated to be a potential drug against PEDV, which might provide a basis for the development of novel drugs to antagonize PEDV.
Supplementary Materials: The following supporting information can be downloaded at: https://www. mdpi.com/article/10.3390/pharmaceutics16050601/s1, Figure S1 : Cytotoxicity of Vero cells treated with different concentration of IVM at the appointed time via CCK-8 assay; Figure S2 : Antiviral activity of IVM-NLCs was measured by CCK-8 assay; Table S1 Characterization of as-prepared IVM-NLCs. Author Contributions: Conceptualization, D.G. and X.X.; methodology, X.X., S.G., Q.Z., J.G. and X.S.; formal analysis, X.X., S.G., Q.Z., J.G., X.S., Y.L., J.X., M.Z. and X.G.; investigation, X.X., S.G., Q.Z. and D.G.; resources, Y.L., J.X. and M.Z.; data curation, X.Z. and H.S.; writing-original draft preparation, X.X., S.G., Q.Z., X.S. and J.X.; writing-review and editing, D.G., J.G., Y.L., H.S., X.Z., M.Z. and X.G.; supervision, D.G., X.G., X.Z. and H.S,; project administration,..
References
Aref, Bazeed, Hassan, Hassan, Rashad et al., Biochemical and Molecular Evaluations of Ivermectin Mucoadhesive Nanosuspension Nasal Spray in Reducing Upper Respiratory Symptoms of Mild COVID-19, IJN, doi:10.2147/IJN.S313093
Baram-Pinto, Shukla, Gedanken, Sarid, Inhibition of HSV-1 Attachment, Entry, and Cell-to-Cell Spread by Functionalized Multivalent Gold Nanoparticles, Small, doi:10.1002/smll.200902384
Bugnicourt, Peers, Dalverny, Ladavière, Tunable morphology of lipid/chitosan particle assemblies, J. Colloid. Interface Sci, doi:10.1016/j.jcis.2018.08.098
Caly, Druce, Catton, Jans, Wagstaff, The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antivir. Res, doi:10.1016/j.antiviral.2020.104787
Cohen, Livney, Assaraf, Targeted nanomedicine modalities for prostate cancer treatment, Drug Resist. Updates, doi:10.1016/j.drup.2021.100762
Cui, Li, Shi, Origin and evolution of pathogenic coronaviruses, Nat. Rev. Microbiol, doi:10.1038/s41579-018-0118-9
Das, Lee, Chia, Chow, Macbeath et al., Development of microemulsion based topical ivermectin formulations: Pre-formulation and formulation studies, Colloids Surf. B Biointerfaces, doi:10.1016/j.colsurfb.2020.110823
Date, Nimbalkar, Kamat, Mittal, Mahato et al., Lipid-polymer hybrid nanocarriers for delivering cancer therapeutics, J. Control. Release, doi:10.1016/j.jconrel.2017.12.016
Garciafuentes, Torres, Alonso, New surface-modified lipid nanoparticles as delivery vehicles for salmon calcitonin, Int. J. Pharm, doi:10.1016/j.ijpharm.2004.12.030
Guo, Dou, Li, Zhang, Bhutto et al., Ivermection-loaded solid lipid nanoparticles: Preparation, characterisation, stability and transdermal behaviour, Artif. Cells Nanomed. Biotechnol, doi:10.1080/21691401.2017.1307207
Götz, Magar, Dornfeld, Giese, Pohlmann et al., Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import, Sci. Rep, doi:10.1038/srep23138
Hamanaka, Chandel, Mitochondrial reactive oxygen species regulate cellular signaling and dictate biological outcomes, Trends Biochem. Sci, doi:10.1016/j.tibs.2010.04.002
Hou, Ke, Kim, Yoo, Su et al., Engineering a Live Attenuated Porcine Epidemic Diarrhea Virus Vaccine Candidate via Inactivation of the Viral 2 ′ -O.-Methyltransferase and the Endocytosis Signal of the Spike Protein, J. Virol, doi:10.1128/JVI.00406-19
Huang, In situ structure and dynamics of an alphacoronavirus spike protein by cryo-ET and cryo-EM, Nat. Commun, doi:10.1038/s41467-022-32588-3
Jaru-Ampornpan, Jengarn, Wanitchang, Jongkaewwattana, Porcine Epidemic Diarrhea Virus 3C-Like Protease-Mediated Nucleocapsid Processing: Possible Link to Viral Cell Culture Adaptability, J. Virol, doi:10.1128/JVI.01660-16
Jung, Porcine epidemic diarrhea virus (PEDV)_An update on etiology, transmission, pathogenesis, and prevention and control, Virus Res, doi:10.1016/j.virusres.2020.198045
Liu, Liu, Jiang, Yang, Huang et al., Surface-Displayed Porcine IFN-λ3 in Lactobacillus plantarum Inhibits Porcine Enteric Coronavirus Infection of Porcine Intestinal Epithelial Cells, J. Microbiol. Biotechnol, doi:10.4014/jmb.1909.09041
Lv, Liu, Wang, Dang, Qiu et al., Ivermectin inhibits DNA polymerase UL42 of pseudorabies virus entrance into the nucleus and proliferation of the virus in vitro and vivo, Antivir. Res, doi:10.1016/j.antiviral.2018.09.010
Martin, Robertson, Choudhary, Ivermectin: An Anthelmintic, an Insecticide, and Much More, Trends Parasitol, doi:10.1016/j.pt.2020.10.005
Mastrangelo, Pezzullo, De Burghgraeve, Kaptein, Pastorino et al., Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: New prospects for an old drug, J. Antimicrob. Chemother, doi:10.1093/jac/dks147
Ng, Salim, Chu, Drug repurposing for COVID-19: Approaches, challenges and promising candidates, Pharmacol. Ther, doi:10.1016/j.pharmthera.2021.107930
Pina, Pinto, Sousa, Craig, Zhao, Generation of hydrate forms of paroxetine HCl from the amorphous state: An evaluation of thermodynamic and experimental predictive approaches, Int. J. Pharm, doi:10.1016/j.ijpharm.2014.12.033
Pushpakom, Iorio, Eyers, Escott, Hopper et al., Drug repurposing: Progress, challenges and recommendations, Nat. Rev. Drug Discov, doi:10.1038/nrd.2018.168
Raman, Polli, Prediction of positive food effect: Bioavailability enhancement of BCS class II drugs, Int. J. Pharm, doi:10.1016/j.ijpharm.2016.04.013
Rehman, Tong, Jafari, Assadpour, Shehzad et al., Carotenoid-loaded nanocarriers: A comprehensive review, Adv. Colloid Interface Sci, doi:10.1016/j.cis.2019.102048
Roessler, Knoers, Van Haelst, Van Haaften, Drug Repurposing for Rare Diseases, Trends Pharmacol. Sci, doi:10.1016/j.tips.2021.01.003
Schorey, Cheng, Singh, Smith, Exosomes and other extracellular vesicles in host-pathogen interactions, EMBO Rep, doi:10.15252/embr.201439363
Sun, Chen, Ming, Bo, Shin et al., Porcine Epidemic Diarrhea Virus Infection Induces Caspase-8-Mediated G3BP1 Cleavage and Subverts Stress Granules To Promote Viral Replication, J. Virol, doi:10.1128/JVI.02344-20
Tay, Fraser, Chan, Moreland, Rathore et al., Nuclear localization of dengue virus (DENV) 1-4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin, Antivir. Res, doi:10.1016/j.antiviral.2013.06.002
Thomas, Lundberg, Pinkham, Shechter, Debono et al., Identification of novel antivirals inhibiting recognition of Venezuelan equine encephalitis virus capsid protein by the Importin α/β1 heterodimer through high-throughput screening, Antivir. Res, doi:10.1016/j.antiviral.2018.01.007
Ud-Din, Roujeinikova, Cloning, purification, crystallization and X-ray crystallographic analysis of the periplasmic sensing domain of Pseudomonas fluorescens chemotactic transducer of amino acids type A (CtaA), BST, doi:10.5582/bst.2016.01059
Ungaro, Yzet, Bossuyt, Baert, Vanasek et al., Deep Remission at 1 Year Prevents Progression of Early Crohn's Disease, Gastroenterology, doi:10.1053/j.gastro.2020.03.039
Valencia-Lazcano, Hassan, Pourmadadi, Shamsabadipour, Behzadmehr et al., 5-Fluorouracil nano-delivery systems as a cutting-edge for cancer therapy, Eur. J. Med. Chem, doi:10.1016/j.ejmech.2022.114995
Wang, Gao, Dou, Chen, Li et al., Ivermectin induces PAK1-mediated cytostatic autophagy in breast cancer, Autophagy, doi:10.1080/15548627.2016.1231494
Wang, Kong, Jiao, Dong, Sun et al., EGR1 Suppresses Porcine Epidemic Diarrhea Virus Replication by Regulating IRAV to Degrade Viral Nucleocapsid Protein, J. Virol, doi:10.1128/JVI.00645-21
Wilson, Prud'homme, Nanoparticle size distribution quantification from transmission electron microscopy (TEM) of ruthenium tetroxide stained polymeric nanoparticles, J. Colloid. Interface Sci, doi:10.1016/j.jcis.2021.04.081
Wu, Wu, Zhang, Yuan, Lu et al., Colloid properties of hydrophobic modified alginate: Surface tension, ζ-potential, viscosity and emulsification, Carbohydr. Polym, doi:10.1016/j.carbpol.2017.10.052
Yang, Atkinson, Wang, Lee, Bogoyevitch et al., The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer, Antivir. Res, doi:10.1016/j.antiviral.2020.104760
Ye, Shao, Li, Guo, Zuo et al., Antiviral Activity of Graphene Oxide: How Sharp Edged Structure and Charge Matter, ACS Appl. Mater. Interfaces, doi:10.1021/acsami.5b06876
Zhai, Kong, Zhang, Song, Qin et al., N protein of PEDV plays chess game with host proteins by selective autophagy, Autophagy, doi:10.1080/15548627.2023.2181615
Zhai, Wang, Jiao, Zhang, Li et al., Melatonin and other indoles show antiviral activities against swine coronaviruses in vitro at pharmacological concentrations, J. Pineal Res, doi:10.1111/jpi.12754
Zhang, Chen, Li, Wen, Song et al., Construction of ivermectin producer by domain swaps of avermectin polyketide synthase in Streptomyces avermitilis, Appl. Microbiol. Biotechnol, doi:10.1007/s00253-006-0361-2
Zhang, Yang, Sahito, Li, Peng et al., Nanostructured lipid carriers with exceptional gastrointestinal stability and inhibition of P-gp efflux for improved oral delivery of tilmicosin, Colloids Surf. B Biointerfaces, doi:10.1016/j.colsurfb.2019.110649
Zorov, Juhaszova, Sollott, Mitochondrial Reactive Oxygen Species (ROS) and ROS-Induced ROS Release, Physiol. Rev, doi:10.1152/physrev.00026.2013
DOI record:
{
"DOI": "10.3390/pharmaceutics16050601",
"ISSN": [
"1999-4923"
],
"URL": "http://dx.doi.org/10.3390/pharmaceutics16050601",
"abstract": "<jats:p>Porcine epidemic diarrhea virus (PEDV) is an acute enteric coronavirus, inducing watery diarrhea and high mortality in piglets, leading to huge economic losses in global pig industry. Ivermectin (IVM), an FDA-approved antiparasitic agent, is characterized by high efficacy and wide applicability. However, the poor bioavailability limits its application. Since the virus is parasitized inside the host cells, increasing the intracellular drug uptake can improve antiviral efficacy. Hence, we aimed to develop nanostructured lipid carriers (NLCs) to enhance the antiviral efficacy of IVM. The findings first revealed the capacity of IVM to inhibit the infectivity of PEDV by reducing viral replication with a certain direct inactivation effect. The as-prepared IVM-NLCs possessed hydrodynamic diameter of 153.5 nm with a zeta potential of −31.5 mV and high encapsulation efficiency (95.72%) and drug loading (11.17%). IVM interacted with lipids and was enveloped in lipid carriers with an amorphous state. Furthermore, its encapsulation in NLCs could enhance drug internalization. Meanwhile, IVM-NLCs inhibited PEDV proliferation by up to three orders of magnitude in terms of viral RNA copies, impeding the accumulation of reactive oxygen species and mitigating the mitochondrial dysfunction caused by PEDV infection. Moreover, IVM-NLCs markedly decreased the apoptosis rate of PEDV-induced Vero cells. Hence, IVM-NLCs showed superior inhibitory effect against PEDV compared to free IVM. Together, these results implied that NLCs is an efficient delivery system for IVM to improve its antiviral efficacy against PEDV via enhanced intracellular uptake.</jats:p>",
"alternative-id": [
"pharmaceutics16050601"
],
"author": [
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"family": "Xu",
"given": "Xiaolin",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"family": "Gao",
"given": "Shasha",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"family": "Zuo",
"given": "Qindan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"family": "Gong",
"given": "Jiahao",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"family": "Song",
"given": "Xinhao",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"family": "Liu",
"given": "Yongshi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"family": "Xiao",
"given": "Jing",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
},
{
"name": "Academy for Advanced Interdisciplinary Studies, Nanjing Agricultural University, Nanjing 210095, China"
}
],
"family": "Zhai",
"given": "Xiaofeng",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"family": "Sun",
"given": "Haifeng",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8439-8989",
"affiliation": [
{
"name": "Jiangsu Key Laboratory of Pesticide Science, College of Sciences, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"authenticated-orcid": false,
"family": "Zhang",
"given": "Mingzhi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"family": "Gao",
"given": "Xiuge",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Engineering Center of Innovative Veterinary Drugs, Center for Veterinary Drug Research and Evaluation, MOE Joint International Research Laboratory of Animal Health and Food Safety, College of Veterinary Medicine, Nanjing Agricultural University, 1 Weigang, Nanjing 210095, China"
}
],
"family": "Guo",
"given": "Dawei",
"sequence": "additional"
}
],
"container-title": "Pharmaceutics",
"container-title-short": "Pharmaceutics",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
5,
2
]
],
"date-time": "2024-05-02T07:57:56Z",
"timestamp": 1714636676000
},
"deposited": {
"date-parts": [
[
2024,
5,
2
]
],
"date-time": "2024-05-02T08:27:48Z",
"timestamp": 1714638468000
},
"funder": [
{
"award": [
"KYCXJC2023005",
"KYCYXT2022010"
],
"name": "Fundamental Research Funds for the Central Universities"
},
{
"name": "Priority Academic Program Development of Jiangsu Higher Education Institutions"
}
],
"indexed": {
"date-parts": [
[
2024,
5,
3
]
],
"date-time": "2024-05-03T00:35:16Z",
"timestamp": 1714696516369
},
"is-referenced-by-count": 0,
"issue": "5",
"issued": {
"date-parts": [
[
2024,
4,
29
]
]
},
"journal-issue": {
"issue": "5",
"published-online": {
"date-parts": [
[
2024,
5
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
4,
29
]
],
"date-time": "2024-04-29T00:00:00Z",
"timestamp": 1714348800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1999-4923/16/5/601/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "601",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
4,
29
]
]
},
"published-online": {
"date-parts": [
[
2024,
4,
29
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1038/s41579-018-0118-9",
"article-title": "Origin and evolution of pathogenic coronaviruses",
"author": "Cui",
"doi-asserted-by": "crossref",
"first-page": "181",
"journal-title": "Nat. Rev. Microbiol.",
"key": "ref_1",
"volume": "17",
"year": "2019"
},
{
"DOI": "10.1016/j.antiviral.2020.104787",
"article-title": "The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro",
"author": "Caly",
"doi-asserted-by": "crossref",
"first-page": "104787",
"journal-title": "Antivir. Res.",
"key": "ref_2",
"volume": "178",
"year": "2020"
},
{
"DOI": "10.1128/JVI.02344-20",
"article-title": "Porcine Epidemic Diarrhea Virus Infection Induces Caspase-8-Mediated G3BP1 Cleavage and Subverts Stress Granules To Promote Viral Replication",
"author": "Sun",
"doi-asserted-by": "crossref",
"first-page": "e02344-20",
"journal-title": "J. Virol.",
"key": "ref_3",
"volume": "95",
"year": "2021"
},
{
"DOI": "10.1016/j.virusres.2020.198045",
"article-title": "Porcine epidemic diarrhea virus (PEDV)_An update on etiology, transmission, pathogenesis, and prevention and control",
"author": "Jung",
"doi-asserted-by": "crossref",
"first-page": "198045",
"journal-title": "Virus Res.",
"key": "ref_4",
"volume": "286",
"year": "2020"
},
{
"DOI": "10.1038/s41467-022-32588-3",
"article-title": "In situ structure and dynamics of an alphacoronavirus spike protein by cryo-ET and cryo-EM",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "4877",
"journal-title": "Nat. Commun.",
"key": "ref_5",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1128/JVI.00406-19",
"article-title": "Engineering a Live Attenuated Porcine Epidemic Diarrhea Virus Vaccine Candidate via Inactivation of the Viral 2′-O.-Methyltransferase and the Endocytosis Signal of the Spike Protein",
"author": "Hou",
"doi-asserted-by": "crossref",
"first-page": "e00406-19",
"journal-title": "J. Virol.",
"key": "ref_6",
"volume": "93",
"year": "2019"
},
{
"DOI": "10.1111/jpi.12754",
"article-title": "Melatonin and other indoles show antiviral activities against swine coronaviruses in vitro at pharmacological concentrations",
"author": "Zhai",
"doi-asserted-by": "crossref",
"first-page": "e12754",
"journal-title": "J. Pineal Res.",
"key": "ref_7",
"volume": "71",
"year": "2021"
},
{
"DOI": "10.1128/JVI.00645-21",
"article-title": "EGR1 Suppresses Porcine Epidemic Diarrhea Virus Replication by Regulating IRAV to Degrade Viral Nucleocapsid Protein",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "e00645-21",
"journal-title": "J. Virol.",
"key": "ref_8",
"volume": "95",
"year": "2021"
},
{
"DOI": "10.1016/j.tips.2021.01.003",
"article-title": "Drug Repurposing for Rare Diseases",
"author": "Roessler",
"doi-asserted-by": "crossref",
"first-page": "255",
"journal-title": "Trends Pharmacol. Sci.",
"key": "ref_9",
"volume": "42",
"year": "2021"
},
{
"DOI": "10.1016/j.pharmthera.2021.107930",
"article-title": "Drug repurposing for COVID-19: Approaches, challenges and promising candidates",
"author": "Ng",
"doi-asserted-by": "crossref",
"first-page": "107930",
"journal-title": "Pharmacol. Ther.",
"key": "ref_10",
"volume": "228",
"year": "2021"
},
{
"DOI": "10.1053/j.gastro.2020.03.039",
"article-title": "Deep Remission at 1 Year Prevents Progression of Early Crohn’s Disease",
"author": "Ungaro",
"doi-asserted-by": "crossref",
"first-page": "139",
"journal-title": "Gastroenterology",
"key": "ref_11",
"volume": "159",
"year": "2020"
},
{
"DOI": "10.1038/nrd.2018.168",
"article-title": "Drug repurposing: Progress, challenges and recommendations",
"author": "Pushpakom",
"doi-asserted-by": "crossref",
"first-page": "41",
"journal-title": "Nat. Rev. Drug Discov.",
"key": "ref_12",
"volume": "18",
"year": "2019"
},
{
"DOI": "10.2147/IJN.S313093",
"article-title": "Clinical, Biochemical and Molecular Evaluations of Ivermectin Mucoadhesive Nanosuspension Nasal Spray in Reducing Upper Respiratory Symptoms of Mild COVID-19",
"author": "Aref",
"doi-asserted-by": "crossref",
"first-page": "4063",
"journal-title": "IJN",
"key": "ref_13",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1007/s00253-006-0361-2",
"article-title": "Construction of ivermectin producer by domain swaps of avermectin polyketide synthase in Streptomyces avermitilis",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "986",
"journal-title": "Appl. Microbiol. Biotechnol.",
"key": "ref_14",
"volume": "72",
"year": "2006"
},
{
"DOI": "10.1080/15548627.2016.1231494",
"article-title": "Ivermectin induces PAK1-mediated cytostatic autophagy in breast cancer",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "2498",
"journal-title": "Autophagy",
"key": "ref_15",
"volume": "12",
"year": "2016"
},
{
"DOI": "10.1016/j.pt.2020.10.005",
"article-title": "Ivermectin: An Anthelmintic, an Insecticide, and Much More",
"author": "Martin",
"doi-asserted-by": "crossref",
"first-page": "48",
"journal-title": "Trends Parasitol.",
"key": "ref_16",
"volume": "37",
"year": "2021"
},
{
"DOI": "10.1016/j.antiviral.2018.09.010",
"article-title": "Ivermectin inhibits DNA polymerase UL42 of pseudorabies virus entrance into the nucleus and proliferation of the virus in vitro and vivo",
"author": "Lv",
"doi-asserted-by": "crossref",
"first-page": "55",
"journal-title": "Antivir. Res.",
"key": "ref_17",
"volume": "159",
"year": "2018"
},
{
"DOI": "10.1016/j.antiviral.2013.06.002",
"article-title": "Nuclear localization of dengue virus (DENV) 1–4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin",
"author": "Tay",
"doi-asserted-by": "crossref",
"first-page": "301",
"journal-title": "Antivir. Res.",
"key": "ref_18",
"volume": "99",
"year": "2013"
},
{
"DOI": "10.1093/jac/dks147",
"article-title": "Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: New prospects for an old drug",
"author": "Mastrangelo",
"doi-asserted-by": "crossref",
"first-page": "1884",
"journal-title": "J. Antimicrob. Chemother.",
"key": "ref_19",
"volume": "67",
"year": "2012"
},
{
"DOI": "10.1038/srep23138",
"article-title": "Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import",
"author": "Magar",
"doi-asserted-by": "crossref",
"first-page": "23138",
"journal-title": "Sci. Rep.",
"key": "ref_20",
"volume": "6",
"year": "2016"
},
{
"DOI": "10.1016/j.antiviral.2018.01.007",
"article-title": "Identification of novel antivirals inhibiting recognition of Venezuelan equine encephalitis virus capsid protein by the Importin α/β1 heterodimer through high-throughput screening",
"author": "Thomas",
"doi-asserted-by": "crossref",
"first-page": "8",
"journal-title": "Antivir. Res.",
"key": "ref_21",
"volume": "151",
"year": "2018"
},
{
"DOI": "10.1016/j.antiviral.2020.104760",
"article-title": "The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "104760",
"journal-title": "Antivir. Res.",
"key": "ref_22",
"volume": "177",
"year": "2020"
},
{
"DOI": "10.1016/j.colsurfb.2020.110823",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Das, S., Lee, S.H., Chia, V.D., Chow, P.S., Macbeath, C., Liu, Y., and Shlieout, G. (2020). Development of microemulsion based topical ivermectin formulations: Pre-formulation and formulation studies. Colloids Surf. B Biointerfaces, 189."
},
{
"DOI": "10.1016/j.ijpharm.2016.04.013",
"article-title": "Prediction of positive food effect: Bioavailability enhancement of BCS class II drugs",
"author": "Raman",
"doi-asserted-by": "crossref",
"first-page": "110",
"journal-title": "Int. J. Pharm.",
"key": "ref_24",
"volume": "506",
"year": "2016"
},
{
"DOI": "10.1016/j.ijpharm.2004.12.030",
"article-title": "New surface-modified lipid nanoparticles as delivery vehicles for salmon calcitonin",
"author": "Garciafuentes",
"doi-asserted-by": "crossref",
"first-page": "122",
"journal-title": "Int. J. Pharm.",
"key": "ref_25",
"volume": "296",
"year": "2005"
},
{
"DOI": "10.1016/j.ejmech.2022.114995",
"article-title": "5-Fluorouracil nano-delivery systems as a cutting-edge for cancer therapy",
"author": "Hassan",
"doi-asserted-by": "crossref",
"first-page": "114995",
"journal-title": "Eur. J. Med. Chem.",
"key": "ref_26",
"volume": "246",
"year": "2023"
},
{
"DOI": "10.1016/j.cis.2019.102048",
"article-title": "Carotenoid-loaded nanocarriers: A comprehensive review",
"author": "Rehman",
"doi-asserted-by": "crossref",
"first-page": "102048",
"journal-title": "Adv. Colloid Interface Sci.",
"key": "ref_27",
"volume": "275",
"year": "2020"
},
{
"DOI": "10.1016/j.jconrel.2017.12.016",
"article-title": "Lipid-polymer hybrid nanocarriers for delivering cancer therapeutics",
"author": "Date",
"doi-asserted-by": "crossref",
"first-page": "60",
"journal-title": "J. Control. Release",
"key": "ref_28",
"volume": "271",
"year": "2018"
},
{
"DOI": "10.1016/j.colsurfb.2019.110649",
"doi-asserted-by": "crossref",
"key": "ref_29",
"unstructured": "Zhang, Q., Yang, H., Sahito, B., Li, X., Peng, L., Gao, X., Ji, H., Wang, L., Jiang, S., and Guo, D. (2020). Nanostructured lipid carriers with exceptional gastrointestinal stability and inhibition of P-gp efflux for improved oral delivery of tilmicosin. Colloids Surf. B Biointerfaces, 187."
},
{
"DOI": "10.1080/21691401.2017.1307207",
"article-title": "Ivermection-loaded solid lipid nanoparticles: Preparation, characterisation, stability and transdermal behaviour",
"author": "Guo",
"doi-asserted-by": "crossref",
"first-page": "255",
"journal-title": "Artif. Cells Nanomed. Biotechnol.",
"key": "ref_30",
"volume": "46",
"year": "2018"
},
{
"DOI": "10.1002/smll.200902384",
"article-title": "Inhibition of HSV-1 Attachment, Entry, and Cell-to-Cell Spread by Functionalized Multivalent Gold Nanoparticles",
"author": "Shukla",
"doi-asserted-by": "crossref",
"first-page": "1044",
"journal-title": "Small",
"key": "ref_31",
"volume": "6",
"year": "2010"
},
{
"DOI": "10.1021/acsami.5b06876",
"article-title": "Antiviral Activity of Graphene Oxide: How Sharp Edged Structure and Charge Matter",
"author": "Ye",
"doi-asserted-by": "crossref",
"first-page": "21571",
"journal-title": "ACS Appl. Mater. Interfaces",
"key": "ref_32",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.4014/jmb.1909.09041",
"article-title": "Surface-Displayed Porcine IFN-λ3 in Lactobacillus plantarum Inhibits Porcine Enteric Coronavirus Infection of Porcine Intestinal Epithelial Cells",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "515",
"journal-title": "J. Microbiol. Biotechnol.",
"key": "ref_33",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1080/15548627.2023.2181615",
"article-title": "N protein of PEDV plays chess game with host proteins by selective autophagy",
"author": "Zhai",
"doi-asserted-by": "crossref",
"first-page": "2338",
"journal-title": "Autophagy",
"key": "ref_34",
"volume": "19",
"year": "2023"
},
{
"DOI": "10.1128/JVI.01660-16",
"article-title": "Porcine Epidemic Diarrhea Virus 3C-Like Protease-Mediated Nucleocapsid Processing: Possible Link to Viral Cell Culture Adaptability",
"author": "Jengarn",
"doi-asserted-by": "crossref",
"first-page": "e01660-16",
"journal-title": "J. Virol.",
"key": "ref_35",
"volume": "91",
"year": "2017"
},
{
"DOI": "10.1016/j.carbpol.2017.10.052",
"article-title": "Colloid properties of hydrophobic modified alginate: Surface tension, ζ-potential, viscosity and emulsification",
"author": "Wu",
"doi-asserted-by": "crossref",
"first-page": "56",
"journal-title": "Carbohydr. Polym.",
"key": "ref_36",
"volume": "181",
"year": "2018"
},
{
"DOI": "10.1016/j.jcis.2021.04.081",
"article-title": "Nanoparticle size distribution quantification from transmission electron microscopy (TEM) of ruthenium tetroxide stained polymeric nanoparticles",
"author": "Wilson",
"doi-asserted-by": "crossref",
"first-page": "208",
"journal-title": "J. Colloid. Interface Sci.",
"key": "ref_37",
"volume": "604",
"year": "2021"
},
{
"DOI": "10.1016/j.jcis.2018.08.098",
"article-title": "Tunable morphology of lipid/chitosan particle assemblies",
"author": "Bugnicourt",
"doi-asserted-by": "crossref",
"first-page": "105",
"journal-title": "J. Colloid. Interface Sci.",
"key": "ref_38",
"volume": "534",
"year": "2019"
},
{
"DOI": "10.1016/j.ijpharm.2014.12.033",
"article-title": "Generation of hydrate forms of paroxetine HCl from the amorphous state: An evaluation of thermodynamic and experimental predictive approaches",
"author": "Pina",
"doi-asserted-by": "crossref",
"first-page": "114",
"journal-title": "Int. J. Pharm.",
"key": "ref_39",
"volume": "481",
"year": "2015"
},
{
"DOI": "10.5582/bst.2016.01059",
"article-title": "Cloning, purification, crystallization and X-ray crystallographic analysis of the periplasmic sensing domain of Pseudomonas fluorescens chemotactic transducer of amino acids type A (CtaA)",
"author": "Roujeinikova",
"doi-asserted-by": "crossref",
"first-page": "320",
"journal-title": "BST",
"key": "ref_40",
"volume": "10",
"year": "2016"
},
{
"DOI": "10.15252/embr.201439363",
"article-title": "Exosomes and other extracellular vesicles in host–pathogen interactions",
"author": "Schorey",
"doi-asserted-by": "crossref",
"first-page": "24",
"journal-title": "EMBO Rep.",
"key": "ref_41",
"volume": "16",
"year": "2015"
},
{
"DOI": "10.1016/j.drup.2021.100762",
"article-title": "Targeted nanomedicine modalities for prostate cancer treatment",
"author": "Cohen",
"doi-asserted-by": "crossref",
"first-page": "100762",
"journal-title": "Drug Resist. Updates",
"key": "ref_42",
"volume": "56",
"year": "2021"
},
{
"DOI": "10.1016/j.tibs.2010.04.002",
"article-title": "Mitochondrial reactive oxygen species regulate cellular signaling and dictate biological outcomes",
"author": "Hamanaka",
"doi-asserted-by": "crossref",
"first-page": "505",
"journal-title": "Trends Biochem. Sci.",
"key": "ref_43",
"volume": "35",
"year": "2010"
},
{
"DOI": "10.1152/physrev.00026.2013",
"article-title": "Mitochondrial Reactive Oxygen Species (ROS) and ROS-Induced ROS Release",
"author": "Zorov",
"doi-asserted-by": "crossref",
"first-page": "909",
"journal-title": "Physiol. Rev.",
"key": "ref_44",
"volume": "94",
"year": "2014"
}
],
"reference-count": 44,
"references-count": 44,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1999-4923/16/5/601"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Enhanced In Vitro Antiviral Activity of Ivermectin-Loaded Nanostructured Lipid Carriers against Porcine Epidemic Diarrhea Virus via Improved Intracellular Delivery",
"type": "journal-article",
"volume": "16"
}
