Inhaled Ivermectin-Loaded Lipid Polymer Hybrid Nanoparticles: Development and Characterization
et al., Pharmaceutics, doi:10.3390/pharmaceutics16081061, Aug 2024
Ivermectin for COVID-19
4th treatment shown to reduce risk in
August 2020, now with p < 0.00000000001 from 106 studies, recognized in 24 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
In vitro study developing ivermectin-loaded lipid polymer hybrid nanoparticles (LPHNPs) as a potential dry powder inhalation formulation for pulmonary delivery.
74 preclinical studies support the efficacy of ivermectin for COVID-19:
Ivermectin, better known for antiparasitic activity, is a broad spectrum antiviral with activity against many viruses including H7N771, Dengue37,72,73 , HIV-173, Simian virus 4074, Zika37,75,76 , West Nile76, Yellow Fever77,78, Japanese encephalitis77, Chikungunya78, Semliki Forest virus78, Human papillomavirus57, Epstein-Barr57, BK Polyomavirus79, and Sindbis virus78.
Ivermectin inhibits importin-α/β-dependent nuclear import of viral proteins71,73,74,80 , shows spike-ACE2 disruption at 1nM with microfluidic diffusional sizing38, binds to glycan sites on the SARS-CoV-2 spike protein preventing interaction with blood and epithelial cells and inhibiting hemagglutination41,81, shows dose-dependent inhibition of wildtype and omicron variants36, exhibits dose-dependent inhibition of lung injury61,66, may inhibit SARS-CoV-2 via IMPase inhibition37, may inhibit SARS-CoV-2 induced formation of fibrin clots resistant to degradation9, inhibits SARS-CoV-2 3CLpro54, may inhibit SARS-CoV-2 RdRp activity28, may minimize viral myocarditis by inhibiting NF-κB/p65-mediated inflammation in macrophages60, may be beneficial for COVID-19 ARDS by blocking GSDMD and NET formation82, may interfere with SARS-CoV-2's immune evasion via ORF8 binding4, may inhibit SARS-CoV-2 by disrupting CD147 interaction83-86, may inhibit SARS-CoV-2 attachment to lipid rafts via spike NTD binding2, shows protection against inflammation, cytokine storm, and mortality in an LPS mouse model sharing key pathological features of severe COVID-1959,87, may be beneficial in severe COVID-19 by binding IGF1 to inhibit the promotion of inflammation, fibrosis, and cell proliferation that leads to lung damage8, may minimize SARS-CoV-2 induced cardiac damage40,48, may counter immune evasion by inhibiting NSP15-TBK1/KPNA1 interaction and restoring IRF3 activation88, may disrupt SARS-CoV-2 N and ORF6 protein nuclear transport and their suppression of host interferon responses1, reduces TAZ/YAP nuclear import, relieving SARS-CoV-2-driven suppression of IRF3 and NF-κB antiviral pathways35, increases Bifidobacteria which play a key role in the immune system89, has immunomodulatory51 and anti-inflammatory70,90 properties, and has an extensive and very positive safety profile91.
1.
Gayozo et al., Binding affinities analysis of ivermectin, nucleocapsid and ORF6 proteins of SARS-CoV-2 to human importins α isoforms: A computational approach, Biotecnia, doi:10.18633/biotecnia.v27.2485.
2.
Lefebvre et al., Characterization and Fluctuations of an Ivermectin Binding Site at the Lipid Raft Interface of the N-Terminal Domain (NTD) of the Spike Protein of SARS-CoV-2 Variants, Viruses, doi:10.3390/v16121836.
3.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
4.
Bagheri-Far et al., Non-spike protein inhibition of SARS-CoV-2 by natural products through the key mediator protein ORF8, Molecular Biology Research Communications, doi:10.22099/mbrc.2024.50245.2001.
5.
de Oliveira Só et al., In Silico Comparative Analysis of Ivermectin and Nirmatrelvir Inhibitors Interacting with the SARS-CoV-2 Main Protease, Preprints, doi:10.20944/preprints202404.1825.v1.
6.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
7.
Oranu et al., Validation of the binding affinities and stabilities of ivermectin and moxidectin against SARS-CoV-2 receptors using molecular docking and molecular dynamics simulation, GSC Biological and Pharmaceutical Sciences, doi:10.30574/gscbps.2024.26.1.0030.
8.
Zhao et al., Identification of the shared gene signatures between pulmonary fibrosis and pulmonary hypertension using bioinformatics analysis, Frontiers in Immunology, doi:10.3389/fimmu.2023.1197752.
9.
Vottero et al., Computational Prediction of the Interaction of Ivermectin with Fibrinogen, Molecular Sciences, doi:10.3390/ijms241411449.
10.
Chellasamy et al., Docking and molecular dynamics studies of human ezrin protein with a modelled SARS-CoV-2 endodomain and their interaction with potential invasion inhibitors, Journal of King Saud University - Science, doi:10.1016/j.jksus.2022.102277.
11.
Umar et al., Inhibitory potentials of ivermectin, nafamostat, and camostat on spike protein and some nonstructural proteins of SARS-CoV-2: Virtual screening approach, Jurnal Teknologi Laboratorium, doi:10.29238/teknolabjournal.v11i1.344.
12.
Alvarado et al., Interaction of the New Inhibitor Paxlovid (PF-07321332) and Ivermectin With the Monomer of the Main Protease SARS-CoV-2: A Volumetric Study Based on Molecular Dynamics, Elastic Networks, Classical Thermodynamics and SPT, Computational Biology and Chemistry, doi:10.1016/j.compbiolchem.2022.107692.
13.
Aminpour et al., In Silico Analysis of the Multi-Targeted Mode of Action of Ivermectin and Related Compounds, Computation, doi:10.3390/computation10040051.
14.
Parvez et al., Insights from a computational analysis of the SARS-CoV-2 Omicron variant: Host–pathogen interaction, pathogenicity, and possible drug therapeutics, Immunity, Inflammation and Disease, doi:10.1002/iid3.639.
15.
Francés-Monerris et al., Microscopic interactions between ivermectin and key human and viral proteins involved in SARS-CoV-2 infection, Physical Chemistry Chemical Physics, doi:10.1039/D1CP02967C.
16.
González-Paz et al., Comparative study of the interaction of ivermectin with proteins of interest associated with SARS-CoV-2: A computational and biophysical approach, Biophysical Chemistry, doi:10.1016/j.bpc.2021.106677.
17.
González-Paz (B) et al., Structural Deformability Induced in Proteins of Potential Interest Associated with COVID-19 by binding of Homologues present in Ivermectin: Comparative Study Based in Elastic Networks Models, Journal of Molecular Liquids, doi:10.1016/j.molliq.2021.117284.
18.
Rana et al., A Computational Study of Ivermectin and Doxycycline Combination Drug Against SARS-CoV-2 Infection, Research Square, doi:10.21203/rs.3.rs-755838/v1.
19.
Muthusamy et al., Virtual Screening Reveals Potential Anti-Parasitic Drugs Inhibiting the Receptor Binding Domain of SARS-CoV-2 Spike protein, Journal of Virology & Antiviral Research, www.scitechnol.com/abstract/virtual-screening-reveals-potential-antiparasitic-drugs-inhibiting-the-receptor-binding-domain-of-sarscov2-spike-protein-16398.html.
20.
Qureshi et al., Mechanistic insights into the inhibitory activity of FDA approved ivermectin against SARS-CoV-2: old drug with new implications, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1906750.
21.
Schöning et al., Highly-transmissible Variants of SARS-CoV-2 May Be More Susceptible to Drug Therapy Than Wild Type Strains, Research Square, doi:10.21203/rs.3.rs-379291/v1.
22.
Bello et al., Elucidation of the inhibitory activity of ivermectin with host nuclear importin α and several SARS-CoV-2 targets, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2021.1911857.
23.
Udofia et al., In silico studies of selected multi-drug targeting against 3CLpro and nsp12 RNA-dependent RNA-polymerase proteins of SARS-CoV-2 and SARS-CoV, Network Modeling Analysis in Health Informatics and Bioinformatics, doi:10.1007/s13721-021-00299-2.
24.
Choudhury et al., Exploring the binding efficacy of ivermectin against the key proteins of SARS-CoV-2 pathogenesis: an in silico approach, Future Medicine, doi:10.2217/fvl-2020-0342.
25.
Kern et al., Modeling of SARS-CoV-2 Treatment Effects for Informed Drug Repurposing, Frontiers in Pharmacology, doi:10.3389/fphar.2021.625678.
26.
Saha et al., The Binding mechanism of ivermectin and levosalbutamol with spike protein of SARS-CoV-2, Structural Chemistry, doi:10.1007/s11224-021-01776-0.
27.
Eweas et al., Molecular Docking Reveals Ivermectin and Remdesivir as Potential Repurposed Drugs Against SARS-CoV-2, Frontiers in Microbiology, doi:10.3389/fmicb.2020.592908.
28.
Parvez (B) et al., Prediction of potential inhibitors for RNA-dependent RNA polymerase of SARS-CoV-2 using comprehensive drug repurposing and molecular docking approach, International Journal of Biological Macromolecules, doi:10.1016/j.ijbiomac.2020.09.098.
29.
Francés-Monerris (B) et al., Has Ivermectin Virus-Directed Effects against SARS-CoV-2? Rationalizing the Action of a Potential Multitarget Antiviral Agent, ChemRxiv, doi:10.26434/chemrxiv.12782258.v1.
30.
Kalhor et al., Repurposing of the approved small molecule drugs in order to inhibit SARS-CoV-2 S protein and human ACE2 interaction through virtual screening approaches, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2020.1824816.
31.
Swargiary, A., Ivermectin as a promising RNA-dependent RNA polymerase inhibitor and a therapeutic drug against SARS-CoV2: Evidence from in silico studies, Research Square, doi:10.21203/rs.3.rs-73308/v1.
32.
Maurya, D., A Combination of Ivermectin and Doxycycline Possibly Blocks the Viral Entry and Modulate the Innate Immune Response in COVID-19 Patients, American Chemical Society (ACS), doi:10.26434/chemrxiv.12630539.v1.
33.
Lehrer et al., Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2, In Vivo, 34:5, 3023-3026, doi:10.21873/invivo.12134.
34.
Suravajhala et al., Comparative Docking Studies on Curcumin with COVID-19 Proteins, Preprints, doi:10.20944/preprints202005.0439.v3.
35.
Kofler et al., M-Motif, a potential non-conventional NLS in YAP/TAZ and other cellular and viral proteins that inhibits classic protein import, iScience, doi:10.1016/j.isci.2025.112105.
36.
Shahin et al., The selective effect of Ivermectin on different human coronaviruses; in-vitro study, Research Square, doi:10.21203/rs.3.rs-4180797/v1.
37.
Jitobaom et al., Identification of inositol monophosphatase as a broad‐spectrum antiviral target of ivermectin, Journal of Medical Virology, doi:10.1002/jmv.29552.
38.
Fauquet et al., Microfluidic Diffusion Sizing Applied to the Study of Natural Products and Extracts That Modulate the SARS-CoV-2 Spike RBD/ACE2 Interaction, Molecules, doi:10.3390/molecules28248072.
39.
García-Aguilar et al., In Vitro Analysis of SARS-CoV-2 Spike Protein and Ivermectin Interaction, International Journal of Molecular Sciences, doi:10.3390/ijms242216392.
40.
Liu et al., SARS-CoV-2 viral genes Nsp6, Nsp8, and M compromise cellular ATP levels to impair survival and function of human pluripotent stem cell-derived cardiomyocytes, Stem Cell Research & Therapy, doi:10.1186/s13287-023-03485-3.
41.
Boschi et al., SARS-CoV-2 Spike Protein Induces Hemagglutination: Implications for COVID-19 Morbidities and Therapeutics and for Vaccine Adverse Effects, bioRxiv, doi:10.1101/2022.11.24.517882.
42.
De Forni et al., Synergistic drug combinations designed to fully suppress SARS-CoV-2 in the lung of COVID-19 patients, PLoS ONE, doi:10.1371/journal.pone.0276751.
43.
Saha (B) et al., Manipulation of Spray-Drying Conditions to Develop an Inhalable Ivermectin Dry Powder, Pharmaceutics, doi:10.3390/pharmaceutics14071432.
44.
Jitobaom (B) et al., Synergistic anti-SARS-CoV-2 activity of repurposed anti-parasitic drug combinations, BMC Pharmacology and Toxicology, doi:10.1186/s40360-022-00580-8.
45.
Croci et al., Liposomal Systems as Nanocarriers for the Antiviral Agent Ivermectin, International Journal of Biomaterials, doi:10.1155/2016/8043983.
46.
Zheng et al., Red blood cell-hitchhiking mediated pulmonary delivery of ivermectin: Effects of nanoparticle properties, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121719.
47.
Delandre et al., Antiviral Activity of Repurposing Ivermectin against a Panel of 30 Clinical SARS-CoV-2 Strains Belonging to 14 Variants, Pharmaceuticals, doi:10.3390/ph15040445.
48.
Liu (B) et al., Genome-wide analyses reveal the detrimental impacts of SARS-CoV-2 viral gene Orf9c on human pluripotent stem cell-derived cardiomyocytes, Stem Cell Reports, doi:10.1016/j.stemcr.2022.01.014.
49.
Segatori et al., Effect of Ivermectin and Atorvastatin on Nuclear Localization of Importin Alpha and Drug Target Expression Profiling in Host Cells from Nasopharyngeal Swabs of SARS-CoV-2- Positive Patients, Viruses, doi:10.3390/v13102084.
50.
Jitobaom (C) et al., Favipiravir and Ivermectin Showed in Vitro Synergistic Antiviral Activity against SARS-CoV-2, Research Square, doi:10.21203/rs.3.rs-941811/v1.
51.
Munson et al., Niclosamide and ivermectin modulate caspase-1 activity and proinflammatory cytokine secretion in a monocytic cell line, British Society For Nanomedicine Early Career Researcher Summer Meeting, 2021, web.archive.org/web/20230401070026/https://michealmunson.github.io/COVID.pdf.
52.
Mountain Valley MD, Mountain Valley MD Receives Successful Results From BSL-4 COVID-19 Clearance Trial on Three Variants Tested With Ivectosol™, 5/18, www.globenewswire.com/en/news-release/2021/05/18/2231755/0/en/Mountain-Valley-MD-Receives-Successful-Results-From-BSL-4-COVID-19-Clearance-Trial-on-Three-Variants-Tested-With-Ivectosol.html.
53.
Yesilbag et al., Ivermectin also inhibits the replication of bovine respiratory viruses (BRSV, BPIV-3, BoHV-1, BCoV and BVDV) in vitro, Virus Research, doi:10.1016/j.virusres.2021.198384.
54.
Mody et al., Identification of 3-chymotrypsin like protease (3CLPro) inhibitors as potential anti-SARS-CoV-2 agents, Communications Biology, doi:10.1038/s42003-020-01577-x.
55.
Jeffreys et al., Remdesivir-ivermectin combination displays synergistic interaction with improved in vitro activity against SARS-CoV-2, International Journal of Antimicrobial Agents, doi:10.1016/j.ijantimicag.2022.106542.
56.
Surnar et al., Clinically Approved Antiviral Drug in an Orally Administrable Nanoparticle for COVID-19, ACS Pharmacol. Transl. Sci., doi:10.1021/acsptsci.0c00179.
57.
Li et al., Quantitative proteomics reveals a broad-spectrum antiviral property of ivermectin, benefiting for COVID-19 treatment, J. Cellular Physiology, doi:10.1002/jcp.30055.
58.
Caly et al., The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro, Antiviral Research, doi:10.1016/j.antiviral.2020.104787.
59.
Zhang et al., Ivermectin inhibits LPS-induced production of inflammatory cytokines and improves LPS-induced survival in mice, Inflammation Research, doi:10.1007/s00011-008-8007-8.
60.
Gao et al., Ivermectin ameliorates acute myocarditis via the inhibition of importin-mediated nuclear translocation of NF-κB/p65, International Immunopharmacology, doi:10.1016/j.intimp.2024.112073.
61.
Abd-Elmawla et al., Suppression of NLRP3 inflammasome by ivermectin ameliorates bleomycin-induced pulmonary fibrosis, Journal of Zhejiang University-SCIENCE B, doi:10.1631/jzus.B2200385.
62.
Uematsu et al., Prophylactic administration of ivermectin attenuates SARS-CoV-2 induced disease in a Syrian Hamster Model, The Journal of Antibiotics, doi:10.1038/s41429-023-00623-0.
63.
Albariqi et al., Pharmacokinetics and Safety of Inhaled Ivermectin in Mice as a Potential COVID-19 Treatment, International Journal of Pharmaceutics, doi:10.1016/j.ijpharm.2022.121688.
64.
Errecalde et al., Safety and Pharmacokinetic Assessments of a Novel Ivermectin Nasal Spray Formulation in a Pig Model, Journal of Pharmaceutical Sciences, doi:10.1016/j.xphs.2021.01.017.
65.
Madrid et al., Safety of oral administration of high doses of ivermectin by means of biocompatible polyelectrolytes formulation, Heliyon, doi:10.1016/j.heliyon.2020.e05820.
66.
Ma et al., Ivermectin contributes to attenuating the severity of acute lung injury in mice, Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2022.113706.
67.
de Melo et al., Attenuation of clinical and immunological outcomes during SARS-CoV-2 infection by ivermectin, EMBO Mol. Med., doi:10.15252/emmm.202114122.
68.
Arévalo et al., Ivermectin reduces in vivo coronavirus infection in a mouse experimental model, Scientific Reports, doi:10.1038/s41598-021-86679-0.
69.
Chaccour et al., Nebulized ivermectin for COVID-19 and other respiratory diseases, a proof of concept, dose-ranging study in rats, Scientific Reports, doi:10.1038/s41598-020-74084-y.
70.
Yan et al., Anti-inflammatory effects of ivermectin in mouse model of allergic asthma, Inflammation Research, doi:10.1007/s00011-011-0307-8.
71.
Götz et al., Influenza A viruses escape from MxA restriction at the expense of efficient nuclear vRNP import, Scientific Reports, doi:10.1038/srep23138.
72.
Tay et al., Nuclear localization of dengue virus (DENV) 1–4 non-structural protein 5; protection against all 4 DENV serotypes by the inhibitor Ivermectin, Antiviral Research, doi:10.1016/j.antiviral.2013.06.002.
73.
Wagstaff et al., Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus, Biochemical Journal, doi:10.1042/BJ20120150.
74.
Wagstaff (B) et al., An AlphaScreen®-Based Assay for High-Throughput Screening for Specific Inhibitors of Nuclear Import, SLAS Discovery, doi:10.1177/1087057110390360.
75.
Barrows et al., A Screen of FDA-Approved Drugs for Inhibitors of Zika Virus Infection, Cell Host & Microbe, doi:10.1016/j.chom.2016.07.004.
76.
Yang et al., The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer, Antiviral Research, doi:10.1016/j.antiviral.2020.104760.
77.
Mastrangelo et al., Ivermectin is a potent inhibitor of flavivirus replication specifically targeting NS3 helicase activity: new prospects for an old drug, Journal of Antimicrobial Chemotherapy, doi:10.1093/jac/dks147.
78.
Varghese et al., Discovery of berberine, abamectin and ivermectin as antivirals against chikungunya and other alphaviruses, Antiviral Research, doi:10.1016/j.antiviral.2015.12.012.
79.
Bennett et al., Role of a nuclear localization signal on the minor capsid Proteins VP2 and VP3 in BKPyV nuclear entry, Virology, doi:10.1016/j.virol.2014.10.013.
80.
Kosyna et al., The importin α/β-specific inhibitor Ivermectin affects HIF-dependent hypoxia response pathways, Biological Chemistry, doi:10.1515/hsz-2015-0171.
81.
Scheim et al., Sialylated Glycan Bindings from SARS-CoV-2 Spike Protein to Blood and Endothelial Cells Govern the Severe Morbidities of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms242317039.
82.
Liu (C) et al., Crosstalk between neutrophil extracellular traps and immune regulation: insights into pathobiology and therapeutic implications of transfusion-related acute lung injury, Frontiers in Immunology, doi:10.3389/fimmu.2023.1324021.
83.
Shouman et al., SARS-CoV-2-associated lymphopenia: possible mechanisms and the role of CD147, Cell Communication and Signaling, doi:10.1186/s12964-024-01718-3.
84.
Scheim (B), D., Ivermectin for COVID-19 Treatment: Clinical Response at Quasi-Threshold Doses Via Hypothesized Alleviation of CD147-Mediated Vascular Occlusion, SSRN, doi:10.2139/ssrn.3636557.
85.
Scheim (C), D., From Cold to Killer: How SARS-CoV-2 Evolved without Hemagglutinin Esterase to Agglutinate and Then Clot Blood Cells, Center for Open Science, doi:10.31219/osf.io/sgdj2.
86.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
87.
DiNicolantonio et al., Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19, Open Heart, doi:10.1136/openhrt-2020-001350.
88.
Mothae et al., SARS-CoV-2 host-pathogen interactome: insights into more players during pathogenesis, Virology, doi:10.1016/j.virol.2025.110607.
89.
Hazan et al., Treatment with Ivermectin Increases the Population of Bifidobacterium in the Gut, ACG 2023, acg2023posters.eventscribe.net/posterspeakers.asp.
Kassaee et al., 12 Aug 2024, peer-reviewed, 5 authors.
Contact: nazrul.islam@qut.edu.au (corresponding author).
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Inhaled Ivermectin-Loaded Lipid Polymer Hybrid Nanoparticles: Development and Characterization
Pharmaceutics, doi:10.3390/pharmaceutics16081061
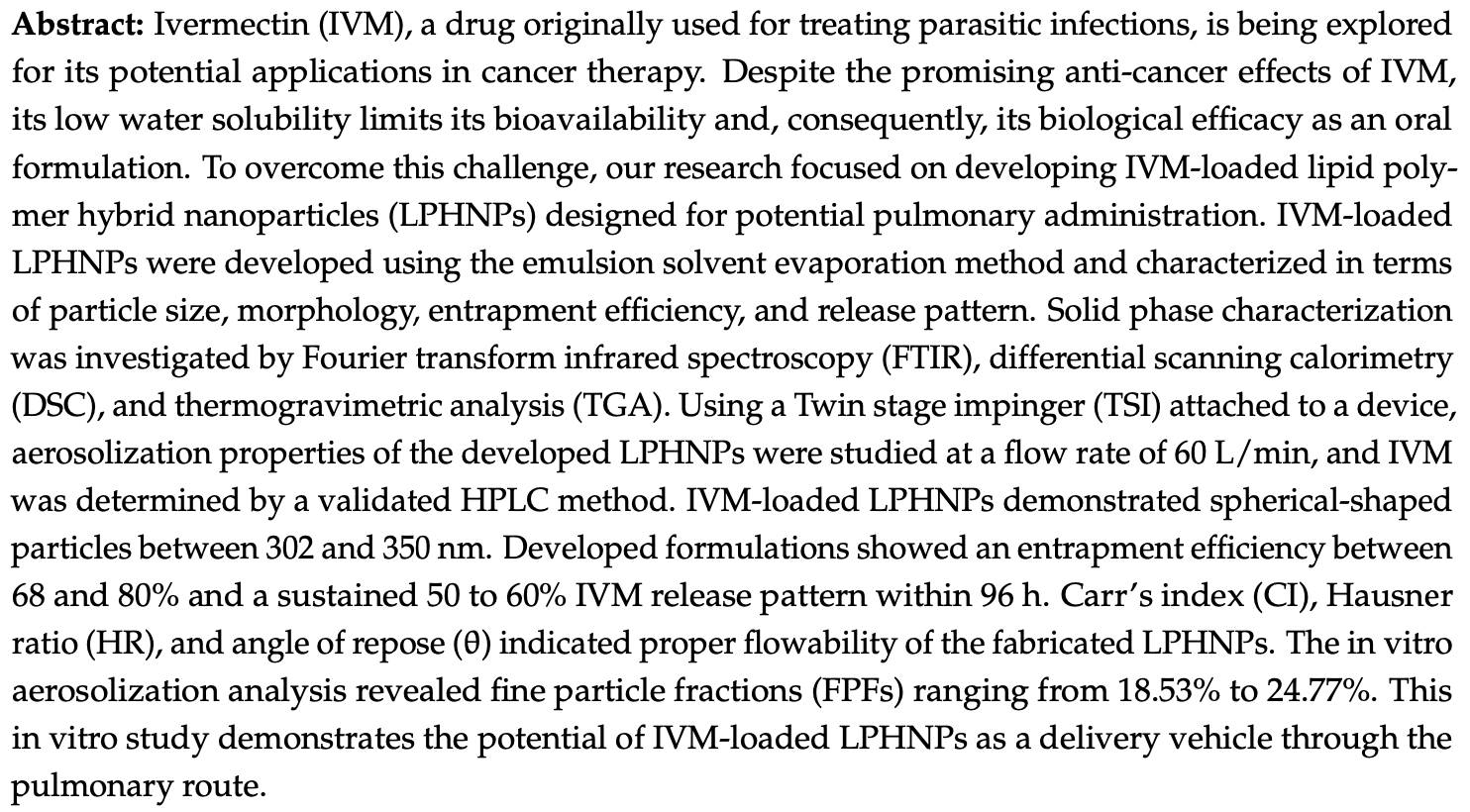
Ivermectin (IVM), a drug originally used for treating parasitic infections, is being explored for its potential applications in cancer therapy. Despite the promising anti-cancer effects of IVM, its low water solubility limits its bioavailability and, consequently, its biological efficacy as an oral formulation. To overcome this challenge, our research focused on developing IVM-loaded lipid polymer hybrid nanoparticles (LPHNPs) designed for potential pulmonary administration. IVM-loaded LPHNPs were developed using the emulsion solvent evaporation method and characterized in terms of particle size, morphology, entrapment efficiency, and release pattern. Solid phase characterization was investigated by Fourier transform infrared spectroscopy (FTIR), differential scanning calorimetry (DSC), and thermogravimetric analysis (TGA). Using a Twin stage impinger (TSI) attached to a device, aerosolization properties of the developed LPHNPs were studied at a flow rate of 60 L/min, and IVM was determined by a validated HPLC method. IVM-loaded LPHNPs demonstrated spherical-shaped particles between 302 and 350 nm. Developed formulations showed an entrapment efficiency between 68 and 80% and a sustained 50 to 60% IVM release pattern within 96 h. Carr's index (CI), Hausner ratio (HR), and angle of repose (θ) indicated proper flowability of the fabricated LPHNPs. The in vitro aerosolization analysis revealed fine particle fractions (FPFs) ranging from 18.53% to 24.77%. This in vitro study demonstrates the potential of IVM-loaded LPHNPs as a delivery vehicle through the pulmonary route.
Conflicts of Interest: The authors have declared no conflicts of interest.
References
Abdelaziz, Gaber, Abd-Elwakil, Mabrouk, Elgohary et al., Inhalable particulate drug delivery systems for lung cancer therapy: Nanoparticles, microparticles, nanocomposites and nanoaggregates, J. Control. Release, doi:10.1016/j.jconrel.2017.11.036
Abou-Elnour, El-Habashy, Essawy, Abdallah, Codelivery of ivermectin and methyl dihydrojasmonate in nanostructured lipid carrier for synergistic antileukemia therapy, Int. J. Pharm, doi:10.1016/j.ijpharm.2024.124086
Ali, Afzal, Verma, Misra-Bhattacharya, Ahmad et al., Improved antifilarial activity of ivermectin in chitosan-alginate nanoparticles against human lymphatic filarial parasite, Brugia malayi, Parasitol. Res, doi:10.1007/s00436-013-3466-4
Anderson, Grimmett, Domalewski, Cui, Inhalable nanotherapeutics to improve treatment efficacy for common lung diseases, Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol, doi:10.1002/wnan.1586
Ayoub, Mowaka, LC-MS/MS determination of empagliflozin and metformin, J. Chromatogr. Sci, doi:10.1093/chromsci/bmx030
Bardoliwala, Patel, Misra, Sawant, Systematic development and characterization of inhalable dry powder containing Polymeric Lipid Hybrid Nanocarriers co-loaded with ABCB1 shRNA and docetaxel using QbD approach, J. Drug Deliv. Sci. Technol, doi:10.1016/j.jddst.2021.102903
Bhardwaj, Mehta, Yadav, Singh, Grobler et al., Pulmonary delivery of antitubercular drugs using spray-dried lipid-polymer hybrid nanoparticles, Artif. Cells Nanomed. Biotechnol, doi:10.3109/21691401.2015.1062389
Bhattacharyya, Reddy, Effect of surfactant on azithromycin dihydrate loaded stearic acid solid lipid nanoparticles, Turk. J. Pharm. Sci, doi:10.4274/tjps.galenos.2018.82160
Conte, Costabile, Baldassi, Rondelli, Bassi et al., Hybrid lipid/polymer nanoparticles to tackle the cystic fibrosis mucus barrier in siRNA delivery to the lungs: Does PEGylation make the difference?, ACS Appl. Mater. Interfaces, doi:10.1021/acsami.1c14975
Craparo, Cabibbo, Scialabba, Giammona, Cavallaro, Inhalable Formulation Based on Lipid-Polymer Hybrid Nanoparticles for the Macrophage Targeted Delivery of Roflumilast, Biomacromolecules, doi:10.1021/acs.biomac.2c00576
Das, Lee, Chia, Chow, Macbeath et al., Development of microemulsion based topical ivermectin formulations: Pre-formulation and formulation studies, Colloids Surf. B Biointerfaces, doi:10.1016/j.colsurfb.2020.110823
Dave, Tak, Sohgaura, Gupta, Sadhu et al., Lipid-polymer hybrid nanoparticles: Synthesis strategies and biomedical applications, J. Microbiol. Methods, doi:10.1016/j.mimet.2019.03.017
De Souza, Júnior, Pinheiro, De Souza Rebouças, De Abreu et al., Ameliorating the antiparasitic activity of the multifaceted drug ivermectin through a polymer nanocapsule formulation, Int. J. Pharm, doi:10.1016/j.ijpharm.2023.122965
Dong, Zhuang, Insights into Inhalation Drug Disposition: The Roles of Pulmonary Drug-Metabolizing Enzymes and Transporters, Int. J. Mol. Sci, doi:10.3390/ijms25094671
Doroudian, O'neill, Mac Loughlin, Prina-Mello, Volkov et al., Nanotechnology in pulmonary medicine, Curr. Opin. Pharmacol, doi:10.1016/j.coph.2020.11.002
Esfahani, Islam, Cabot, Izake, Development of thiabendazole-loaded mesoporous silica nanoparticles for cancer therapy, ACS Biomater. Sci. Eng, doi:10.1021/acsbiomaterials.1c00066
Ferreira, Chaves, Lima, Reis, Optimization of nanostructured lipid carriers loaded with methotrexate: A tool for inflammatory and cancer therapy, Int. J. Pharm, doi:10.1016/j.ijpharm.2015.07.013
Gajbhiye, Salve, Narwade, Sheikh, Kesharwani et al., Lipid polymer hybrid nanoparticles: A custom-tailored next-generation approach for cancer therapeutics, Mol. Cancer, doi:10.1186/s12943-023-01849-0
Gajra, Dalwadi, Patel, Formulation and optimization of itraconazole polymeric lipid hybrid nanoparticles (Lipomer) using box behnken design, DARU J. Pharm. Sci, doi:10.1186/s40199-014-0087-0
Gan, Dai, Yuan, Qian, Sha et al., Effect of size on the cellular endocytosis and controlled release of mesoporous silica nanoparticles for intracellular delivery, Biomed. Microdevices, doi:10.1007/s10544-011-9604-9
Gandhi, Roy, Lipid-Based inhalable micro-and nanocarriers of active agents for treating non-small-cell lung cancer, Pharmaceutics, doi:10.3390/pharmaceutics15051457
Godara, Lather, Kirthanashri, Awasthi, Pandita, Lipid-PLGA hybrid nanoparticles of paclitaxel: Preparation, characterization, in vitro and in vivo evaluation, Mater. Sci. Eng. C, doi:10.1016/j.msec.2019.110576
Guo, Dou, Li, Zhang, Bhutto et al., Ivermection-loaded solid lipid nanoparticles: Preparation, characterisation, stability and transdermal behaviour, Artif. Cells Nanomed. Biotechnol, doi:10.1080/21691401.2017.1307207
Hadinoto, Sundaresan, Cheow, Lipid-polymer hybrid nanoparticles as a new generation therapeutic delivery platform: A review, Eur. J. Pharm. Biopharm, doi:10.1016/j.ejpb.2013.07.002
Honary, Zahir, Effect of zeta potential on the properties of nano-drug delivery systems-a review (Part 2), Trop. J. Pharm. Res
Hu, Dong, Pastorin, Ng, Tan, Spherical agglomerates of pure drug nanoparticles for improved pulmonary delivery in dry powder inhalers, J. Nanopart. Res, doi:10.1007/s11051-013-1560-2
Islam, Rahman, Pulmonary drug delivery: Implication for new strategy for pharmacotherapy for neurodegenerative disorders, Drug Discov. Ther
Jahromi, Ghazali, Ashrafi, Azadi, A comparison of models for the analysis of the kinetics of drug release from PLGA-based nanoparticles, Heliyon, doi:10.1016/j.heliyon.2020.e03451
Johnson-Arbor, Ivermectin: A mini-review, Clin. Toxicol, doi:10.1080/15563650.2022.2043338
Kassaee, Nili-Ahmadabadi, Mahboobian, Fabrication of poloxamer based besifloxacin thermosensitive in situ gelling nanoemulsions for ophthalmic delivery, J. Bioact. Compat. Polym, doi:10.1177/08839115231167587
Khan, Aamir, Madni, Jan, Khan et al., Lipid poly (E-caprolactone) hybrid nanoparticles of 5-fluorouracil for sustained release and enhanced anticancer efficacy, Life Sci, doi:10.1016/j.lfs.2021.119909
Kovacevic, Savic, Vuleta, Mueller, Keck, Polyhydroxy surfactants for the formulation of lipid nanoparticles (SLN and NLC): Effects on size, physical stability and particle matrix structure, Int. J. Pharm, doi:10.1016/j.ijpharm.2010.12.036
Kumbhar, Manjappa, Shah, Jha, Singh et al., Inhalation delivery of repurposed drugs for lung cancer: Approaches, benefits and challenges, J. Control. Release, doi:10.1016/j.jconrel.2021.11.015
Kuperkar, Atanase, Bahadur, Crivei, Bahadur, Degradable polymeric bio (nano) materials and their biomedical applications: A comprehensive overview and recent updates, Polymers, doi:10.3390/polym16020206
Li, Wong, Shuhendler, Rauth, Wu, Molecular interactions, internal structure and drug release kinetics of rationally developed polymer-lipid hybrid nanoparticles, J. Control. Release, doi:10.1016/j.jconrel.2008.02.014
Liu, Cheng, Xin, Liu, Wang et al., Nanoparticles advanced from preclinical studies to clinical trials for lung cancer therapy, Cancer Nanotechnol, doi:10.1186/s12645-023-00174-x
Liu, Pan, Feng, Nanoparticles of lipid monolayer shell and biodegradable polymer core for controlled release of paclitaxel: Effects of surfactants on particles size, characteristics and in vitro performance, Int. J. Pharm, doi:10.1016/j.ijpharm.2010.05.008
Liu, Yang, Jin, Xu, Zhao, Development of high-drug-loading nanoparticles, ChemPlusChem, doi:10.1002/cplu.202000496
Liu, Zhao, Zhu, Cheng, Liu et al., Docetaxel liposomes for lung targeted delivery: Development and evaluation, Pharm. Dev. Technol, doi:10.1080/10837450.2023.2265472
Lu, Xiong, Sun, Yu, Hu et al., Sustained release ivermectin-loaded solid lipid dispersion for subcutaneous delivery: In vitro and in vivo evaluation, Drug Deliv, doi:10.1080/10717544.2017.1284945
Macho, Demková, Gabrišová, Čierny, Mužíková et al., Analysis of static angle of repose with respect to powder material properties, Acta Polytech, doi:10.14311/AP.2020.60.0073
Majeed, Manochakian, Zhao, Lou, Targeted therapy in advanced non-small cell lung cancer: Current advances and future trends, J. Hematol. Oncol, doi:10.1186/s13045-021-01121-2
Mandal, Mittal, Balabathula, Thoma, Wood, Development and in vitro evaluation of core-shell type lipid-polymer hybrid nanoparticles for the delivery of erlotinib in non-small cell lung cancer, Eur. J. Pharm. Sci, doi:10.1016/j.ejps.2015.10.021
Marante, Viegas, Duarte, Macedo, Fonte, An overview on spray-drying of protein-loaded polymeric nanoparticles for dry powder inhalation, Pharmaceutics, doi:10.3390/pharmaceutics12111032
Mohammed, El-Megrab, Hasan, Gomaa, A remodeled ivermectin polycaprolactone-based nanoparticles for inhalation as a promising treatment of pulmonary inflammatory diseases, Eur. J. Pharm. Sci, doi:10.1016/j.ejps.2024.106714
Mukherjee, Waters, Kalyan, Achrol, Kesari et al., Lipid-polymer hybrid nanoparticles as a next-generation drug delivery platform: State of the art, emerging technologies, and perspectives, Int. J. Nanomed, doi:10.2147/IJN.S198353
Noori, Dehpour, Alavi, Hosseini, Korani et al., Synthesis and evaluation of the effects of solid lipid nanoparticles of ivermectin and ivermectin on cuprizone-induced demyelination via targeting the TRPA1/NF-kB/GFAP signaling pathway, J. Basic Med. Sci
Othman, Vladisavljevic, Nagy, Holdich, Encapsulation and controlled release of rapamycin from polycaprolactone nanoparticles prepared by membrane micromixing combined with antisolvent precipitation, Langmuir, doi:10.1021/acs.langmuir.6b03178
Patel, Bardoliwala, Lalani, Patil, Ghosh et al., Development of a dry powder for inhalation of nanoparticles codelivering cisplatin and ABCC3 siRNA in lung cancer, Ther. Deliv, doi:10.4155/tde-2020-0117
Patel, Karampuri, Kansara, Vyas, Inhalable dry powder containing lipid polymer hybrid nanoparticles of Nintedanib esylate: In vitro and in vivo evaluations, J. Drug Deliv. Sci. Technol, doi:10.1016/j.jddst.2023.104716
Pellosi, Angelo, Maiolino, Mitidieri, Di Villa Bianca et al., In vitro/in vivo investigation on the potential of Pluronic ® mixed micelles for pulmonary drug delivery, Eur. J. Pharm. Biopharm, doi:10.1016/j.ejpb.2018.06.006
Ren, Qi, Ruan, Cao, Ma et al., Selenized polymer-lipid hybrid nanoparticles for oral delivery of tripterine with ameliorative oral anti-enteritis activity and bioavailability, Pharmaceutics, doi:10.3390/pharmaceutics15030821
Sabuj, Dargaville, Nissen, Islam, Inhaled ciprofloxacin-loaded poly (2-ethyl-2-oxazoline) nanoparticles from dry powder inhaler formulation for the potential treatment of lower respiratory tract infections, PLoS ONE, doi:10.1371/journal.pone.0261720
Schabath, Cote, Cancer progress and priorities: Lung cancer, Cancer Epidemiol. Biomark. Prev, doi:10.1158/1055-9965.EPI-19-0221
Sengel-Turk, Hascicek, Design of lipid-polymer hybrid nanoparticles for therapy of BPH: Part I. Formulation optimization using a design of experiment approach, J. Drug Deliv. Sci. Technol, doi:10.1016/j.jddst.2017.02.012
Shen, Wu, Liu, Wu, High drug-loading nanomedicines: Progress, current status, and prospects, Int. J. Nanomed, doi:10.2147/IJN.S132780
Sinha, Mukherjee, Development of an inhalation chamber and a dry powder inhaler device for administration of pulmonary medication in animal model, Drug Dev. Ind. Pharm, doi:10.3109/03639045.2011.592532
Soomherun, Kreua-Ongarjnukool, Niyomthai, Chumnanvej, Lipid-Polymer Hybrid Nanoparticles Synthesized via Lipid-Based Surface Engineering for a robust drug delivery platform, Colloids Surf. B Biointerfaces, doi:10.1016/j.colsurfb.2024.113858
Tahir, Madni, Balasubramanian, Rehman, Correia et al., Development and optimization of methotrexate-loaded lipid-polymer hybrid nanoparticles for controlled drug delivery applications, Int. J. Pharm, doi:10.1016/j.ijpharm.2017.09.061
Tang, Hu, Wang, Yao, Zhang et al., Ivermectin, a potential anticancer drug derived from an antiparasitic drug, Pharmacol. Res, doi:10.1016/j.phrs.2020.105207
Tang, Zhang, Sun, Luo, Zhou et al., Pulmonary delivery of mucus-traversing PF127-modified silk fibroin nanoparticles loading with quercetin for lung cancer therapy, Asian J. Pharm. Sci, doi:10.1016/j.ajps.2023.100833
Thakur, Chellappan, Dua, Mehta, Satija et al., Patented therapeutic drug delivery strategies for targeting pulmonary diseases, Expert Opin. Ther. Pat, doi:10.1080/13543776.2020.1741547
Thanki, Van Eetvelde, Geyer, Fraire, Hendrix et al., Mechanistic profiling of the release kinetics of siRNA from lipidoid-polymer hybrid nanoparticles in vitro and in vivo after pulmonary administration, J. Control. Release, doi:10.1016/j.jconrel.2019.08.004
Tiyaboonchai, Tungpradit, Plianbangchang, Formulation and characterization of curcuminoids loaded solid lipid nanoparticles, Int. J. Pharm, doi:10.1016/j.ijpharm.2006.12.043
Valarini Junior, Cardoso, De Souza, Machado Giufrida, Cardozo-Filho, Single step encapsulation process of ivermectin in biocompatible polymer using a supercritical antisolvent system process, Asia-Pac. J. Chem. Eng, doi:10.1002/apj.2672
Velho, Funk, Deon, Benvenutti, Buchner et al., Ivermectin-Loaded Mesoporous Silica and Polymeric Nanocapsules: Impact on Drug Loading, In Vitro Solubility Enhancement, and Release Performance, Pharmaceutics, doi:10.3390/pharmaceutics16030325
Vencken, Foged, Ramsey, Sweeney, Cryan et al., Nebulised lipid-polymer hybrid nanoparticles for the delivery of a therapeutic anti-inflammatory microRNA to bronchial epithelial cells, ERJ Open Res, doi:10.1183/23120541.00161-2018
Wadhwa, Bobak, Bohrmann, Geczy, Sekar et al., Pulmonary delivery of siRNA-loaded lipid-polymer hybrid nanoparticles: Effect of nanoparticle size, OpenNano, doi:10.1016/j.onano.2023.100180
Wang, George, Bartlett, Gao, Islam, Nicotine hydrogen tartrate loaded chitosan nanoparticles: Formulation, characterization and in vitro delivery from dry powder inhaler formulation, Eur. J. Pharm. Biopharm, doi:10.1016/j.ejpb.2016.12.023
Wang, Holgate, Bartlett, Islam, Assessment of nicotine release from nicotine-loaded chitosan nanoparticles dry powder inhaler formulations via locomotor activity of C57BL/6 mice, Eur. J. Pharm. Biopharm
DOI record:
{
"DOI": "10.3390/pharmaceutics16081061",
"ISSN": [
"1999-4923"
],
"URL": "http://dx.doi.org/10.3390/pharmaceutics16081061",
"abstract": "<jats:p>Ivermectin (IVM), a drug originally used for treating parasitic infections, is being explored for its potential applications in cancer therapy. Despite the promising anti-cancer effects of IVM, its low water solubility limits its bioavailability and, consequently, its biological efficacy as an oral formulation. To overcome this challenge, our research focused on developing IVM-loaded lipid polymer hybrid nanoparticles (LPHNPs) designed for potential pulmonary administration. IVM-loaded LPHNPs were developed using the emulsion solvent evaporation method and characterized in terms of particle size, morphology, entrapment efficiency, and release pattern. Solid phase characterization was investigated by Fourier transform infrared spectroscopy (FTIR), differential scanning calorimetry (DSC), and thermogravimetric analysis (TGA). Using a Twin stage impinger (TSI) attached to a device, aerosolization properties of the developed LPHNPs were studied at a flow rate of 60 L/min, and IVM was determined by a validated HPLC method. IVM-loaded LPHNPs demonstrated spherical-shaped particles between 302 and 350 nm. Developed formulations showed an entrapment efficiency between 68 and 80% and a sustained 50 to 60% IVM release pattern within 96 h. Carr’s index (CI), Hausner ratio (HR), and angle of repose (θ) indicated proper flowability of the fabricated LPHNPs. The in vitro aerosolization analysis revealed fine particle fractions (FPFs) ranging from 18.53% to 24.77%. This in vitro study demonstrates the potential of IVM-loaded LPHNPs as a delivery vehicle through the pulmonary route.</jats:p>",
"alternative-id": [
"pharmaceutics16081061"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-4000-3498",
"affiliation": [
{
"name": "Pharmacy Discipline, School of Clinical Sciences, Faculty of Health, Queensland University of Technology (QUT), Brisbane, QLD 4000, Australia"
}
],
"authenticated-orcid": false,
"family": "Kassaee",
"given": "Seyedeh Negin",
"sequence": "first"
},
{
"affiliation": [
{
"name": "School of Chemistry and Physics, Science and Engineering Faculty, Queensland University of Technology (QUT), Brisbane, QLD 4000, Australia"
}
],
"family": "Ayoko",
"given": "Godwin A.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Centre for Genomics and Personalised Health, School of Biomedical Sciences, Queensland University of Technology (QUT), Brisbane, QLD 4000, Australia"
}
],
"family": "Richard",
"given": "Derek",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4278-0888",
"affiliation": [
{
"name": "Central Analytical Research Facility, Institution for Future Environment, Queensland University of Technology (QUT), Brisbane, QLD 4000, Australia"
}
],
"authenticated-orcid": false,
"family": "Wang",
"given": "Tony",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6751-6915",
"affiliation": [
{
"name": "Pharmacy Discipline, School of Clinical Sciences, Faculty of Health, Queensland University of Technology (QUT), Brisbane, QLD 4000, Australia"
},
{
"name": "Centre for Materials Science, Queensland University of Technology, Brisbane, QLD 4000, Australia"
},
{
"name": "Centre for Immunology and Infection Control (CIIC), Queensland University of Technology (QUT), Brisbane, QLD 4000, Australia"
}
],
"authenticated-orcid": false,
"family": "Islam",
"given": "Nazrul",
"sequence": "additional"
}
],
"container-title": "Pharmaceutics",
"container-title-short": "Pharmaceutics",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
8,
13
]
],
"date-time": "2024-08-13T10:02:37Z",
"timestamp": 1723543357000
},
"deposited": {
"date-parts": [
[
2024,
8,
13
]
],
"date-time": "2024-08-13T10:19:08Z",
"timestamp": 1723544348000
},
"indexed": {
"date-parts": [
[
2024,
8,
14
]
],
"date-time": "2024-08-14T00:27:14Z",
"timestamp": 1723595234897
},
"is-referenced-by-count": 0,
"issue": "8",
"issued": {
"date-parts": [
[
2024,
8,
12
]
]
},
"journal-issue": {
"issue": "8",
"published-online": {
"date-parts": [
[
2024,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
8,
12
]
],
"date-time": "2024-08-12T00:00:00Z",
"timestamp": 1723420800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/1999-4923/16/8/1061/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1061",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
8,
12
]
]
},
"published-online": {
"date-parts": [
[
2024,
8,
12
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1080/13543776.2020.1741547",
"article-title": "Patented therapeutic drug delivery strategies for targeting pulmonary diseases",
"author": "Thakur",
"doi-asserted-by": "crossref",
"first-page": "375",
"journal-title": "Expert Opin. Ther. Pat.",
"key": "ref_1",
"volume": "30",
"year": "2020"
},
{
"article-title": "Pulmonary drug delivery: Implication for new strategy for pharmacotherapy for neurodegenerative disorders",
"author": "Islam",
"first-page": "264",
"journal-title": "Drug Discov. Ther.",
"key": "ref_2",
"volume": "2",
"year": "2008"
},
{
"DOI": "10.3390/ijms25094671",
"doi-asserted-by": "crossref",
"key": "ref_3",
"unstructured": "Dong, L., and Zhuang, X. (2024). Insights into Inhalation Drug Disposition: The Roles of Pulmonary Drug-Metabolizing Enzymes and Transporters. Int. J. Mol. Sci., 25."
},
{
"DOI": "10.3390/pharmaceutics15051457",
"doi-asserted-by": "crossref",
"key": "ref_4",
"unstructured": "Gandhi, S., and Roy, I. (2023). Lipid-Based inhalable micro-and nanocarriers of active agents for treating non-small-cell lung cancer. Pharmaceutics, 15."
},
{
"DOI": "10.1016/j.coph.2020.11.002",
"article-title": "Nanotechnology in pulmonary medicine",
"author": "Doroudian",
"doi-asserted-by": "crossref",
"first-page": "85",
"journal-title": "Curr. Opin. Pharmacol.",
"key": "ref_5",
"volume": "56",
"year": "2021"
},
{
"DOI": "10.1186/s12645-023-00174-x",
"article-title": "Nanoparticles advanced from preclinical studies to clinical trials for lung cancer therapy",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "28",
"journal-title": "Cancer Nanotechnol.",
"key": "ref_6",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1158/1055-9965.EPI-19-0221",
"article-title": "Cancer progress and priorities: Lung cancer",
"author": "Schabath",
"doi-asserted-by": "crossref",
"first-page": "1563",
"journal-title": "Cancer Epidemiol. Biomark. Prev.",
"key": "ref_7",
"volume": "28",
"year": "2019"
},
{
"DOI": "10.1186/s13045-021-01121-2",
"article-title": "Targeted therapy in advanced non-small cell lung cancer: Current advances and future trends",
"author": "Majeed",
"doi-asserted-by": "crossref",
"first-page": "108",
"journal-title": "J. Hematol. Oncol.",
"key": "ref_8",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1016/j.ejps.2015.10.021",
"article-title": "Development and in vitro evaluation of core–shell type lipid–polymer hybrid nanoparticles for the delivery of erlotinib in non-small cell lung cancer",
"author": "Mandal",
"doi-asserted-by": "crossref",
"first-page": "162",
"journal-title": "Eur. J. Pharm. Sci.",
"key": "ref_9",
"volume": "81",
"year": "2016"
},
{
"DOI": "10.1016/j.jconrel.2021.11.015",
"article-title": "Inhalation delivery of repurposed drugs for lung cancer: Approaches, benefits and challenges",
"author": "Kumbhar",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "J. Control. Release",
"key": "ref_10",
"volume": "341",
"year": "2022"
},
{
"DOI": "10.1016/j.ejps.2024.106714",
"article-title": "A remodeled ivermectin polycaprolactone-based nanoparticles for inhalation as a promising treatment of pulmonary inflammatory diseases",
"author": "Mohammed",
"doi-asserted-by": "crossref",
"first-page": "106714",
"journal-title": "Eur. J. Pharm. Sci.",
"key": "ref_11",
"volume": "195",
"year": "2024"
},
{
"DOI": "10.1016/j.phrs.2020.105207",
"article-title": "Ivermectin, a potential anticancer drug derived from an antiparasitic drug",
"author": "Tang",
"doi-asserted-by": "crossref",
"first-page": "105207",
"journal-title": "Pharmacol. Res.",
"key": "ref_12",
"volume": "163",
"year": "2021"
},
{
"DOI": "10.1080/15563650.2022.2043338",
"article-title": "Ivermectin: A mini-review",
"doi-asserted-by": "crossref",
"first-page": "571",
"journal-title": "Clin. Toxicol.",
"key": "ref_13",
"volume": "60",
"year": "2022"
},
{
"DOI": "10.1016/j.ijpharm.2023.122965",
"article-title": "Ameliorating the antiparasitic activity of the multifaceted drug ivermectin through a polymer nanocapsule formulation",
"author": "Pinheiro",
"doi-asserted-by": "crossref",
"first-page": "122965",
"journal-title": "Int. J. Pharm.",
"key": "ref_14",
"volume": "639",
"year": "2023"
},
{
"DOI": "10.1021/acsbiomaterials.1c00066",
"article-title": "Development of thiabendazole-loaded mesoporous silica nanoparticles for cancer therapy",
"author": "Esfahani",
"doi-asserted-by": "crossref",
"first-page": "4153",
"journal-title": "ACS Biomater. Sci. Eng.",
"key": "ref_15",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/j.jconrel.2017.11.036",
"article-title": "Inhalable particulate drug delivery systems for lung cancer therapy: Nanoparticles, microparticles, nanocomposites and nanoaggregates",
"author": "Abdelaziz",
"doi-asserted-by": "crossref",
"first-page": "374",
"journal-title": "J. Control. Release",
"key": "ref_16",
"volume": "269",
"year": "2018"
},
{
"DOI": "10.2147/IJN.S198353",
"article-title": "Lipid–polymer hybrid nanoparticles as a next-generation drug delivery platform: State of the art, emerging technologies, and perspectives",
"author": "Mukherjee",
"doi-asserted-by": "crossref",
"first-page": "1937",
"journal-title": "Int. J. Nanomed.",
"key": "ref_17",
"volume": "14",
"year": "2019"
},
{
"DOI": "10.3390/polym16020206",
"doi-asserted-by": "crossref",
"key": "ref_18",
"unstructured": "Kuperkar, K., Atanase, L.I., Bahadur, A., Crivei, I.C., and Bahadur, P. (2024). Degradable polymeric bio (nano) materials and their biomedical applications: A comprehensive overview and recent updates. Polymers, 16."
},
{
"DOI": "10.1186/s12943-023-01849-0",
"article-title": "Lipid polymer hybrid nanoparticles: A custom-tailored next-generation approach for cancer therapeutics",
"author": "Gajbhiye",
"doi-asserted-by": "crossref",
"first-page": "160",
"journal-title": "Mol. Cancer",
"key": "ref_19",
"volume": "22",
"year": "2023"
},
{
"DOI": "10.1002/wnan.1586",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "Anderson, C.F., Grimmett, M.E., Domalewski, C.J., and Cui, H. (2020). Inhalable nanotherapeutics to improve treatment efficacy for common lung diseases. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol., 12."
},
{
"DOI": "10.1016/j.ejpb.2013.07.002",
"article-title": "Lipid–polymer hybrid nanoparticles as a new generation therapeutic delivery platform: A review",
"author": "Hadinoto",
"doi-asserted-by": "crossref",
"first-page": "427",
"journal-title": "Eur. J. Pharm. Biopharm.",
"key": "ref_21",
"volume": "85",
"year": "2013"
},
{
"DOI": "10.1016/j.mimet.2019.03.017",
"article-title": "Lipid-polymer hybrid nanoparticles: Synthesis strategies and biomedical applications",
"author": "Dave",
"doi-asserted-by": "crossref",
"first-page": "130",
"journal-title": "J. Microbiol. Methods",
"key": "ref_22",
"volume": "160",
"year": "2019"
},
{
"DOI": "10.1016/j.jddst.2021.102903",
"article-title": "Systematic development and characterization of inhalable dry powder containing Polymeric Lipid Hybrid Nanocarriers co-loaded with ABCB1 shRNA and docetaxel using QbD approach",
"author": "Bardoliwala",
"doi-asserted-by": "crossref",
"first-page": "102903",
"journal-title": "J. Drug Deliv. Sci. Technol.",
"key": "ref_23",
"volume": "66",
"year": "2021"
},
{
"DOI": "10.4155/tde-2020-0117",
"article-title": "Development of a dry powder for inhalation of nanoparticles codelivering cisplatin and ABCC3 siRNA in lung cancer",
"author": "Patel",
"doi-asserted-by": "crossref",
"first-page": "651",
"journal-title": "Ther. Deliv.",
"key": "ref_24",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.3109/21691401.2015.1062389",
"article-title": "Pulmonary delivery of antitubercular drugs using spray-dried lipid–polymer hybrid nanoparticles",
"author": "Bhardwaj",
"doi-asserted-by": "crossref",
"first-page": "1544",
"journal-title": "Artif. Cells Nanomed. Biotechnol.",
"key": "ref_25",
"volume": "44",
"year": "2016"
},
{
"DOI": "10.1016/j.jconrel.2019.08.004",
"article-title": "Mechanistic profiling of the release kinetics of siRNA from lipidoid-polymer hybrid nanoparticles in vitro and in vivo after pulmonary administration",
"author": "Thanki",
"doi-asserted-by": "crossref",
"first-page": "82",
"journal-title": "J. Control. Release",
"key": "ref_26",
"volume": "310",
"year": "2019"
},
{
"DOI": "10.1183/23120541.00161-2018",
"article-title": "Nebulised lipid–polymer hybrid nanoparticles for the delivery of a therapeutic anti-inflammatory microRNA to bronchial epithelial cells",
"author": "Vencken",
"doi-asserted-by": "crossref",
"first-page": "161",
"journal-title": "ERJ Open Res.",
"key": "ref_27",
"volume": "5",
"year": "2019"
},
{
"DOI": "10.1021/acsami.1c14975",
"article-title": "Hybrid lipid/polymer nanoparticles to tackle the cystic fibrosis mucus barrier in siRNA delivery to the lungs: Does PEGylation make the difference?",
"author": "Conte",
"doi-asserted-by": "crossref",
"first-page": "7565",
"journal-title": "ACS Appl. Mater. Interfaces",
"key": "ref_28",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1021/acs.biomac.2c00576",
"article-title": "Inhalable Formulation Based on Lipid–Polymer Hybrid Nanoparticles for the Macrophage Targeted Delivery of Roflumilast",
"author": "Craparo",
"doi-asserted-by": "crossref",
"first-page": "3439",
"journal-title": "Biomacromolecules",
"key": "ref_29",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.1016/j.jddst.2023.104716",
"article-title": "Inhalable dry powder containing lipid polymer hybrid nanoparticles of Nintedanib esylate: In vitro and in vivo evaluations",
"author": "Patel",
"doi-asserted-by": "crossref",
"first-page": "104716",
"journal-title": "J. Drug Deliv. Sci. Technol.",
"key": "ref_30",
"volume": "86",
"year": "2023"
},
{
"DOI": "10.1016/j.onano.2023.100180",
"article-title": "Pulmonary delivery of siRNA-loaded lipid-polymer hybrid nanoparticles: Effect of nanoparticle size",
"author": "Wadhwa",
"doi-asserted-by": "crossref",
"first-page": "100180",
"journal-title": "OpenNano",
"key": "ref_31",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1016/j.ajps.2023.100833",
"article-title": "Pulmonary delivery of mucus-traversing PF127-modified silk fibroin nanoparticles loading with quercetin for lung cancer therapy",
"author": "Tang",
"doi-asserted-by": "crossref",
"first-page": "100833",
"journal-title": "Asian J. Pharm. Sci.",
"key": "ref_32",
"volume": "18",
"year": "2023"
},
{
"DOI": "10.1016/j.ejpb.2018.06.006",
"article-title": "In vitro/in vivo investigation on the potential of Pluronic® mixed micelles for pulmonary drug delivery",
"author": "Pellosi",
"doi-asserted-by": "crossref",
"first-page": "30",
"journal-title": "Eur. J. Pharm. Biopharm.",
"key": "ref_33",
"volume": "130",
"year": "2018"
},
{
"DOI": "10.1016/j.msec.2019.110576",
"article-title": "Lipid-PLGA hybrid nanoparticles of paclitaxel: Preparation, characterization, in vitro and in vivo evaluation",
"author": "Godara",
"doi-asserted-by": "crossref",
"first-page": "110576",
"journal-title": "Mater. Sci. Eng. C",
"key": "ref_34",
"volume": "109",
"year": "2020"
},
{
"DOI": "10.1080/21691401.2017.1307207",
"article-title": "Ivermection-loaded solid lipid nanoparticles: Preparation, characterisation, stability and transdermal behaviour",
"author": "Guo",
"doi-asserted-by": "crossref",
"first-page": "255",
"journal-title": "Artif. Cells Nanomed. Biotechnol.",
"key": "ref_35",
"volume": "46",
"year": "2018"
},
{
"DOI": "10.1016/j.ejpb.2016.12.023",
"article-title": "Nicotine hydrogen tartrate loaded chitosan nanoparticles: Formulation, characterization and in vitro delivery from dry powder inhaler formulation",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "118",
"journal-title": "Eur. J. Pharm. Biopharm.",
"key": "ref_36",
"volume": "113",
"year": "2017"
},
{
"DOI": "10.1016/j.colsurfb.2020.110823",
"doi-asserted-by": "crossref",
"key": "ref_37",
"unstructured": "Das, S., Lee, S.H., Chia, V.D., Chow, P.S., Macbeath, C., Liu, Y., and Shlieout, G. (2020). Development of microemulsion based topical ivermectin formulations: Pre-formulation and formulation studies. Colloids Surf. B Biointerfaces, 189."
},
{
"DOI": "10.1093/chromsci/bmx030",
"article-title": "LC–MS/MS determination of empagliflozin and metformin",
"author": "Ayoub",
"doi-asserted-by": "crossref",
"first-page": "742",
"journal-title": "J. Chromatogr. Sci.",
"key": "ref_38",
"volume": "55",
"year": "2017"
},
{
"DOI": "10.3390/pharmaceutics15030821",
"doi-asserted-by": "crossref",
"key": "ref_39",
"unstructured": "Ren, Y., Qi, C., Ruan, S., Cao, G., Ma, Z., and Zhang, X. (2023). Selenized polymer-lipid hybrid nanoparticles for oral delivery of tripterine with ameliorative oral anti-enteritis activity and bioavailability. Pharmaceutics, 15."
},
{
"DOI": "10.1186/s40199-014-0087-0",
"article-title": "Formulation and optimization of itraconazole polymeric lipid hybrid nanoparticles (Lipomer) using box behnken design",
"author": "Gajra",
"doi-asserted-by": "crossref",
"first-page": "3",
"journal-title": "DARU J. Pharm. Sci.",
"key": "ref_40",
"volume": "23",
"year": "2015"
},
{
"DOI": "10.1016/j.lfs.2021.119909",
"article-title": "Lipid poly (ɛ-caprolactone) hybrid nanoparticles of 5-fluorouracil for sustained release and enhanced anticancer efficacy",
"author": "Khan",
"doi-asserted-by": "crossref",
"first-page": "119909",
"journal-title": "Life Sci.",
"key": "ref_41",
"volume": "284",
"year": "2021"
},
{
"DOI": "10.1016/j.ijpharm.2006.12.043",
"article-title": "Formulation and characterization of curcuminoids loaded solid lipid nanoparticles",
"author": "Tiyaboonchai",
"doi-asserted-by": "crossref",
"first-page": "299",
"journal-title": "Int. J. Pharm.",
"key": "ref_42",
"volume": "337",
"year": "2007"
},
{
"DOI": "10.1371/journal.pone.0261720",
"doi-asserted-by": "crossref",
"key": "ref_43",
"unstructured": "Sabuj, M.Z.R., Dargaville, T.R., Nissen, L., and Islam, N. (2021). Inhaled ciprofloxacin-loaded poly (2-ethyl-2-oxazoline) nanoparticles from dry powder inhaler formulation for the potential treatment of lower respiratory tract infections. PLoS ONE, 16."
},
{
"DOI": "10.1016/j.ijpharm.2010.12.036",
"article-title": "Polyhydroxy surfactants for the formulation of lipid nanoparticles (SLN and NLC): Effects on size, physical stability and particle matrix structure",
"author": "Kovacevic",
"doi-asserted-by": "crossref",
"first-page": "163",
"journal-title": "Int. J. Pharm.",
"key": "ref_44",
"volume": "406",
"year": "2011"
},
{
"article-title": "Effect of zeta potential on the properties of nano-drug delivery systems-a review (Part 2)",
"author": "Honary",
"first-page": "265",
"journal-title": "Trop. J. Pharm. Res.",
"key": "ref_45",
"volume": "12",
"year": "2013"
},
{
"DOI": "10.1016/j.ijpharm.2010.05.008",
"article-title": "Nanoparticles of lipid monolayer shell and biodegradable polymer core for controlled release of paclitaxel: Effects of surfactants on particles size, characteristics and in vitro performance",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "243",
"journal-title": "Int. J. Pharm.",
"key": "ref_46",
"volume": "395",
"year": "2010"
},
{
"DOI": "10.1016/j.ijpharm.2017.09.061",
"article-title": "Development and optimization of methotrexate-loaded lipid-polymer hybrid nanoparticles for controlled drug delivery applications",
"author": "Tahir",
"doi-asserted-by": "crossref",
"first-page": "156",
"journal-title": "Int. J. Pharm.",
"key": "ref_47",
"volume": "533",
"year": "2017"
},
{
"DOI": "10.1016/j.ijpharm.2015.07.013",
"article-title": "Optimization of nanostructured lipid carriers loaded with methotrexate: A tool for inflammatory and cancer therapy",
"author": "Ferreira",
"doi-asserted-by": "crossref",
"first-page": "65",
"journal-title": "Int. J. Pharm.",
"key": "ref_48",
"volume": "492",
"year": "2015"
},
{
"DOI": "10.1002/cplu.202000496",
"article-title": "Development of high-drug-loading nanoparticles",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "2143",
"journal-title": "ChemPlusChem",
"key": "ref_49",
"volume": "85",
"year": "2020"
},
{
"DOI": "10.2147/IJN.S132780",
"article-title": "High drug-loading nanomedicines: Progress, current status, and prospects",
"author": "Shen",
"doi-asserted-by": "crossref",
"first-page": "4085",
"journal-title": "Int. J. Nanomed.",
"key": "ref_50",
"volume": "12",
"year": "2017"
},
{
"DOI": "10.1016/j.jconrel.2008.02.014",
"article-title": "Molecular interactions, internal structure and drug release kinetics of rationally developed polymer–lipid hybrid nanoparticles",
"author": "Li",
"doi-asserted-by": "crossref",
"first-page": "60",
"journal-title": "J. Control. Release",
"key": "ref_51",
"volume": "128",
"year": "2008"
},
{
"DOI": "10.1007/s10544-011-9604-9",
"article-title": "Effect of size on the cellular endocytosis and controlled release of mesoporous silica nanoparticles for intracellular delivery",
"author": "Gan",
"doi-asserted-by": "crossref",
"first-page": "259",
"journal-title": "Biomed. Microdevices",
"key": "ref_52",
"volume": "14",
"year": "2012"
},
{
"DOI": "10.4274/tjps.galenos.2018.82160",
"article-title": "Effect of surfactant on azithromycin dihydrate loaded stearic acid solid lipid nanoparticles",
"author": "Bhattacharyya",
"doi-asserted-by": "crossref",
"first-page": "425",
"journal-title": "Turk. J. Pharm. Sci.",
"key": "ref_53",
"volume": "16",
"year": "2019"
},
{
"DOI": "10.1016/j.jddst.2017.02.012",
"article-title": "Design of lipid-polymer hybrid nanoparticles for therapy of BPH: Part I. Formulation optimization using a design of experiment approach",
"author": "Hascicek",
"doi-asserted-by": "crossref",
"first-page": "16",
"journal-title": "J. Drug Deliv. Sci. Technol.",
"key": "ref_54",
"volume": "39",
"year": "2017"
},
{
"DOI": "10.1016/j.heliyon.2020.e03451",
"article-title": "A comparison of models for the analysis of the kinetics of drug release from PLGA-based nanoparticles",
"author": "Jahromi",
"doi-asserted-by": "crossref",
"first-page": "e03451",
"journal-title": "Heliyon",
"key": "ref_55",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1016/j.colsurfb.2024.113858",
"doi-asserted-by": "crossref",
"key": "ref_56",
"unstructured": "Soomherun, N., Kreua-Ongarjnukool, N., Niyomthai, S.T., and Chumnanvej, S. (2024). Lipid-Polymer Hybrid Nanoparticles Synthesized via Lipid-Based Surface Engineering for a robust drug delivery platform. Colloids Surf. B Biointerfaces, 237."
},
{
"DOI": "10.1177/08839115231167587",
"article-title": "Fabrication of poloxamer based besifloxacin thermosensitive in situ gelling nanoemulsions for ophthalmic delivery",
"author": "Kassaee",
"doi-asserted-by": "crossref",
"first-page": "298",
"journal-title": "J. Bioact. Compat. Polym.",
"key": "ref_57",
"volume": "38",
"year": "2023"
},
{
"DOI": "10.1016/j.ijpharm.2024.124086",
"article-title": "Codelivery of ivermectin and methyl dihydrojasmonate in nanostructured lipid carrier for synergistic antileukemia therapy",
"author": "Essawy",
"doi-asserted-by": "crossref",
"first-page": "124086",
"journal-title": "Int. J. Pharm.",
"key": "ref_58",
"volume": "656",
"year": "2024"
},
{
"DOI": "10.1080/10837450.2023.2265472",
"article-title": "Docetaxel liposomes for lung targeted delivery: Development and evaluation",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "856",
"journal-title": "Pharm. Dev. Technol.",
"key": "ref_59",
"volume": "28",
"year": "2023"
},
{
"DOI": "10.3390/pharmaceutics16030325",
"doi-asserted-by": "crossref",
"key": "ref_60",
"unstructured": "Velho, M.C., Funk, N.L., Deon, M., Benvenutti, E.V., Buchner, S., Hinrichs, R., Pilger, D.A., and Beck, R.C.R. (2024). Ivermectin-Loaded Mesoporous Silica and Polymeric Nanocapsules: Impact on Drug Loading, In Vitro Solubility Enhancement, and Release Performance. Pharmaceutics, 16."
},
{
"DOI": "10.1002/apj.2672",
"article-title": "Single step encapsulation process of ivermectin in biocompatible polymer using a supercritical antisolvent system process",
"author": "Cardoso",
"doi-asserted-by": "crossref",
"first-page": "e2672",
"journal-title": "Asia-Pac. J. Chem. Eng.",
"key": "ref_61",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1080/10717544.2017.1284945",
"article-title": "Sustained release ivermectin-loaded solid lipid dispersion for subcutaneous delivery: In vitro and in vivo evaluation",
"author": "Lu",
"doi-asserted-by": "crossref",
"first-page": "622",
"journal-title": "Drug Deliv.",
"key": "ref_62",
"volume": "24",
"year": "2017"
},
{
"DOI": "10.1007/s00436-013-3466-4",
"article-title": "Improved antifilarial activity of ivermectin in chitosan–alginate nanoparticles against human lymphatic filarial parasite, Brugia malayi",
"author": "Ali",
"doi-asserted-by": "crossref",
"first-page": "2933",
"journal-title": "Parasitol. Res.",
"key": "ref_63",
"volume": "112",
"year": "2013"
},
{
"article-title": "Synthesis and evaluation of the effects of solid lipid nanoparticles of ivermectin and ivermectin on cuprizone-induced demyelination via targeting the TRPA1/NF-kB/GFAP signaling pathway",
"author": "Noori",
"first-page": "1272",
"journal-title": "Iran. J. Basic Med. Sci.",
"key": "ref_64",
"volume": "26",
"year": "2023"
},
{
"DOI": "10.1021/acs.langmuir.6b03178",
"article-title": "Encapsulation and controlled release of rapamycin from polycaprolactone nanoparticles prepared by membrane micromixing combined with antisolvent precipitation",
"author": "Othman",
"doi-asserted-by": "crossref",
"first-page": "10685",
"journal-title": "Langmuir",
"key": "ref_65",
"volume": "32",
"year": "2016"
},
{
"DOI": "10.14311/AP.2020.60.0073",
"article-title": "Analysis of static angle of repose with respect to powder material properties",
"author": "Macho",
"doi-asserted-by": "crossref",
"first-page": "73",
"journal-title": "Acta Polytech.",
"key": "ref_66",
"volume": "60",
"year": "2020"
},
{
"DOI": "10.1007/s11051-013-1560-2",
"article-title": "Spherical agglomerates of pure drug nanoparticles for improved pulmonary delivery in dry powder inhalers",
"author": "Hu",
"doi-asserted-by": "crossref",
"first-page": "1560",
"journal-title": "J. Nanopart. Res.",
"key": "ref_67",
"volume": "15",
"year": "2013"
},
{
"DOI": "10.3109/03639045.2011.592532",
"article-title": "Development of an inhalation chamber and a dry powder inhaler device for administration of pulmonary medication in animal model",
"author": "Sinha",
"doi-asserted-by": "crossref",
"first-page": "171",
"journal-title": "Drug Dev. Ind. Pharm.",
"key": "ref_68",
"volume": "38",
"year": "2012"
},
{
"DOI": "10.3390/pharmaceutics12111032",
"doi-asserted-by": "crossref",
"key": "ref_69",
"unstructured": "Marante, T., Viegas, C., Duarte, I., Macedo, A.S., and Fonte, P. (2020). An overview on spray-drying of protein-loaded polymeric nanoparticles for dry powder inhalation. Pharmaceutics, 12."
},
{
"DOI": "10.1016/j.ejpb.2020.07.011",
"article-title": "Assessment of nicotine release from nicotine-loaded chitosan nanoparticles dry powder inhaler formulations via locomotor activity of C57BL/6 mice",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "175",
"journal-title": "Eur. J. Pharm. Biopharm.",
"key": "ref_70",
"volume": "154",
"year": "2020"
}
],
"reference-count": 70,
"references-count": 70,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/1999-4923/16/8/1061"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Inhaled Ivermectin-Loaded Lipid Polymer Hybrid Nanoparticles: Development and Characterization",
"type": "journal-article",
"volume": "16"
}
