Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling
et al., Cells, doi:10.3390/cells13161331, Aug 2024
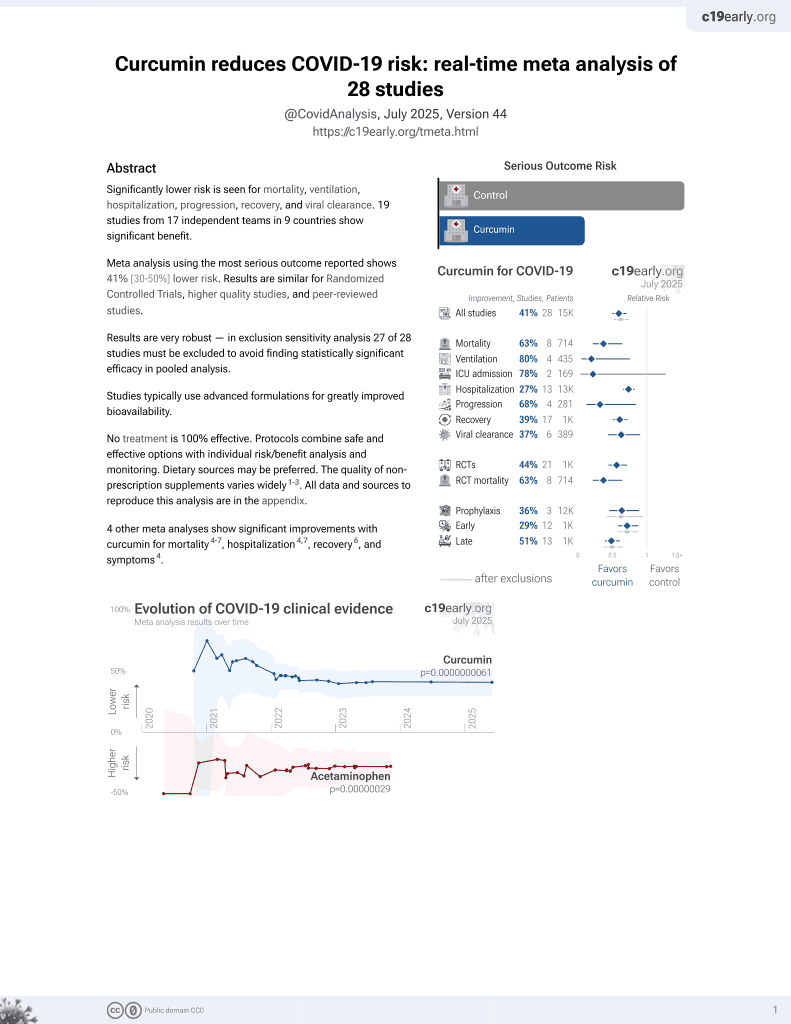
Curcumin for COVID-19
17th treatment shown to reduce risk in
February 2021, now with p = 0.0000000061 from 28 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
In vitro study showing that the SARS-CoV-2 spike protein can activate cardiac fibroblasts through ACE2-dependent mechanisms, leading to cardiac fibrosis via the NLRP3 inflammasome and NF-κB signaling pathways. The results suggest that COVID-19 could directly contribute to long-term cardiovascular complications, particularly fibrosis, raising concerns about persistent cardiac damage.
The results point to several classes of therapeutics that may limit cardiac damage including NLRP3 inflammasome inhibitors (e.g., colchicine), NF-κB pathway inhibitors (e.g. curcumin), and antioxidants (e.g., vitamin C, NAC).
62 preclinical studies support the efficacy of curcumin for COVID-19:
In silico studies predict inhibition of SARS-CoV-2 with curcumin or metabolites via binding to the spikeA,1,5,6,11,16,18,24,27 (and specifically the receptor binding domainB,2,4,14,17,20 ), MproC,4-6,11,13,15-17,19,20,22,25,27,28,30,48 , RNA-dependent RNA polymeraseD,4-6,17,26 , PLproE,6, ACE2F,2,18,19,21 , nucleocapsidG,12,29 , nsp10H,29, and helicaseI,36 proteins, and inhibition of spike-ACE2 interactionJ,3.
In vitro studies demonstrate inhibition of the spikeA,41 (and specifically the receptor binding domainB,51), MproC,23,41,48,50 , ACE2F,51, and TMPRSS2K,51 proteins, and inhibition of spike-ACE2 interactionJ,3,34 .
In vitro studies demonstrate efficacy in Calu-3L,49, A549M,41, A549-ATN,31, 293TO,7, HEK293-hACE2P,23,39 , 293T/hACE2/TMPRSS2Q,40, Vero E6R,1,13,17,27,39,41,43,45,47,49 , and SH-SY5YS,38 cells.
Curcumin decreases pro-inflammatory cytokines induced by SARS-CoV-2 in peripheral blood mononuclear cells47, alleviates SARS-CoV-2 spike protein-induced mitochondrial membrane damage and oxidative stress7, may limit COVID-19 induced cardiac damage by inhibiting the NF-κB signaling pathway which mediates the profibrotic effects of the SARS-CoV-2 spike protein on cardiac fibroblasts35, is predicted to inhibit the interaction between the SARS-CoV-2 spike protein receptor binding domain and the human ACE2 receptor for the delta and omicron variants14, lowers ACE2 and STAT3, curbing lung inflammation and ARDS in preclinical COVID-19 models32, inhibits SARS-CoV-2 ORF3a ion channel activity, which contributes to viral pathogenicity and cytotoxicity42, has direct virucidal action by disrupting viral envelope integrity44, may inhibit viral replication and modulate inflammatory pathways like NF-κB via SIRT1 activation52, and can function as a photosensitizer in photodynamic therapy to generate reactive oxygen species that damage the virus44.
1.
Marzouk et al., Computational and Experimental Insights into the Antiviral Mechanism of Turmeric (Curcuma longa) against SARS-CoV-2 D614G, BIO Web of Conferences, doi:10.1051/bioconf/202519804002.
2.
Wu et al., Utilizing natural compounds as ligands to disrupt the binding of SARS-CoV-2 receptor-binding domain to angiotensin-converting enzyme 2, impeding viral infection, Phytochemistry Letters, doi:10.1016/j.phytol.2025.102999.
3.
Najimi et al., Phytochemical Inhibitors of SARS‐CoV‐2 Entry: Targeting the ACE2‐RBD Interaction with l‐Tartaric Acid, l‐Ascorbic Acid, and Curcuma longa Extract, ChemistrySelect, doi:10.1002/slct.202406035.
4.
Rajamanickam et al., Exploring the Potential of Siddha Formulation MilagaiKudineer-Derived Phytotherapeutics Against SARS-CoV-2: An In-Silico Investigation for Antiviral Intervention, Journal of Pharmacy and Pharmacology Research, doi:10.26502/fjppr.0105.
5.
Al balawi et al., Assessing multi-target antiviral and antioxidant activities of natural compounds against SARS-CoV-2: an integrated in vitro and in silico study, Bioresources and Bioprocessing, doi:10.1186/s40643-024-00822-z.
6.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
7.
Zhang et al., Computational Discovery of Mitochondrial Dysfunction Biomarkers in Severe SARS-CoV-2 Infection: Facilitating Pytomedicine Screening, Phytomedicine, doi:10.1016/j.phymed.2024.155784.
8.
Öztürkkan et al., In Silico investigation of the effects of curcuminoids on the spike protein of the omicron variant of SARS-CoV-2, Baku State University Journal of Chemistry and Material Sciences, 1:2, bsuj.bsu.edu.az/uploads/pdf/ec4204d62f7802de54e6092bf7860029.pdf.
9.
Yunze et al., Therapeutic effect and potential mechanism of curcumin, an active ingredient in Tongnao Decoction, on COVID-19 combined with stroke: a network pharmacology study and GEO database mining, Research Square, doi:10.21203/rs.3.rs-4329762/v1.
10.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
11.
Boseila et al., Throat spray formulated with virucidal Pharmaceutical excipients as an effective early prophylactic or treatment strategy against pharyngitis post-exposure to SARS CoV-2, European Journal of Pharmaceutics and Biopharmaceutics, doi:10.1016/j.ejpb.2024.114279.
12.
Hidayah et al., Bioinformatics study of curcumin, demethoxycurcumin, bisdemethoxycurcumin and cyclocurcumin compounds in Curcuma longa as an antiviral agent via nucleocapsid on SARS-CoV-2 inhibition, International Conference on Organic and Applied Chemistry, doi:10.1063/5.0197724.
13.
Singh et al., Unlocking the potential of phytochemicals in inhibiting SARS-CoV-2 M Pro protein - An in-silico and cell-based approach, Research Square, doi:10.21203/rs.3.rs-3888947/v1.
14.
Kant et al., Structure-based drug discovery to identify SARS-CoV2 spike protein–ACE2 interaction inhibitors, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2023.2300060.
15.
Naderi Beni et al., In silico studies of anti-oxidative and hot temperament-based phytochemicals as natural inhibitors of SARS-CoV-2 Mpro, PLOS ONE, doi:10.1371/journal.pone.0295014.
16.
Moschovou et al., Exploring the Binding Effects of Natural Products and Antihypertensive Drugs on SARS-CoV-2: An In Silico Investigation of Main Protease and Spike Protein, International Journal of Molecular Sciences, doi:10.3390/ijms242115894.
17.
Eleraky et al., Curcumin Transferosome-Loaded Thermosensitive Intranasal in situ Gel as Prospective Antiviral Therapy for SARS-Cov-2, International Journal of Nanomedicine, doi:10.2147/IJN.S423251.
18.
Singh (B) et al., Computational studies to analyze effect of curcumin inhibition on coronavirus D614G mutated spike protein, The Seybold Report, doi:10.17605/OSF.IO/TKEXJ.
19.
Thapa et al., In-silico Approach for Predicting the Inhibitory Effect of Home Remedies on Severe Acute Respiratory Syndrome Coronavirus-2, Makara Journal of Science, doi:10.7454/mss.v27i3.1609.
20.
Srivastava et al., Paradigm of Well-Orchestrated Pharmacokinetic Properties of Curcuminoids Relative to Conventional Drugs for the Inactivation of SARS-CoV-2 Receptors: An In Silico Approach, Stresses, doi:10.3390/stresses3030043.
21.
Alkafaas et al., A study on the effect of natural products against the transmission of B.1.1.529 Omicron, Virology Journal, doi:10.1186/s12985-023-02160-6.
22.
Winih Kinasih et al., Analisis in silico interaksi senyawa kurkuminoid terhadap enzim main protease 6LU7 dari SARS-CoV-2, Duta Pharma Journal, doi:10.47701/djp.v3i1.2904.
23.
Wu (B) et al., Potential Mechanism of Curcumin and Resveratrol against SARS-CoV-2, Research Square, doi:10.21203/rs.3.rs-2780614/v1.
24.
Nag et al., Curcumin inhibits spike protein of new SARS-CoV-2 variant of concern (VOC) Omicron, an in silico study, Computers in Biology and Medicine, doi:10.1016/j.compbiomed.2022.105552.
25.
Rampogu et al., Molecular Docking and Molecular Dynamics Simulations Discover Curcumin Analogue as a Plausible Dual Inhibitor for SARS-CoV-2, International Journal of Molecular Sciences, doi:10.3390/ijms23031771.
26.
Singh (C) et al., Potential of turmeric-derived compounds against RNA-dependent RNA polymerase of SARS-CoV-2: An in-silico approach, Computers in Biology and Medicine, doi:10.1016/j.compbiomed.2021.104965.
27.
Kandeil et al., Bioactive Polyphenolic Compounds Showing Strong Antiviral Activities against Severe Acute Respiratory Syndrome Coronavirus 2, Pathogens, doi:10.3390/pathogens10060758.
28.
Rajagopal et al., Activity of phytochemical constituents of Curcuma longa (turmeric) and Andrographis paniculata against coronavirus (COVID-19): an in silico approach, Future Journal of Pharmaceutical Sciences, doi:10.1186/s43094-020-00126-x.
29.
Suravajhala et al., Comparative Docking Studies on Curcumin with COVID-19 Proteins, Preprints, doi:10.20944/preprints202005.0439.v3.
30.
Sekiou et al., In-Silico Identification of Potent Inhibitors of COVID-19 Main Protease (Mpro) and Angiotensin Converting Enzyme 2 (ACE2) from Natural Products: Quercetin, Hispidulin, and Cirsimaritin Exhibited Better Potential Inhibition than Hydroxy-Chloroquine Against COVID-19 Main Protease Active Site and ACE2, ChemRxiv, doi:10.26434/chemrxiv.12181404.v1.
31.
Grüneberg et al., Dose-dependent antiviral effects of glycyrrhizin, curcumin, and harmaline against clinical SARS-CoV-2 isolates, including D614G, Omicron BA.5, and Omicron XBB.1, BMC Complementary Medicine and Therapies, doi:10.1186/s12906-026-05253-1.
32.
Aktay et al., Oral Administration of Water-Soluble Curcumin Complex Prevents ARDS With the Potential for COVID-19 Treatment, Phytotherapy Research, doi:10.1002/ptr.70046.
33.
Olubiyi et al., Novel dietary herbal preparations with inhibitory activities against multiple SARS-CoV-2 targets: A multidisciplinary investigation into antiviral activities, Food Chemistry Advances, doi:10.1016/j.focha.2025.100969.
34.
Emam et al., Establishment of in-house assay for screening of anti-SARS-CoV-2 protein inhibitors, AMB Express, doi:10.1186/s13568-024-01739-8.
35.
Van Tin et al., Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling, Cells, doi:10.3390/cells13161331.
36.
Li et al., Thermal shift assay (TSA)-based drug screening strategy for rapid discovery of inhibitors against the Nsp13 helicase of SARS-CoV-2, Animals and Zoonoses, doi:10.1016/j.azn.2024.06.001.
37.
Kamble et al., Nanoparticulate curcumin spray imparts prophylactic and therapeutic properties against SARS-CoV-2, Emergent Materials, doi:10.1007/s42247-024-00754-6.
38.
Nicoliche et al., Antiviral, anti-inflammatory and antioxidant effects of curcumin and curcuminoids in SH-SY5Y cells infected by SARS-CoV-2, Scientific Reports, doi:10.1038/s41598-024-61662-7.
39.
Nittayananta et al., A novel film spray containing curcumin inhibits SARS-CoV-2 and influenza virus infection and enhances mucosal immunity, Virology Journal, doi:10.1186/s12985-023-02282-x.
40.
Septisetyani et al., Curcumin and turmeric extract inhibited SARS-CoV-2 pseudovirus cell entry and Spike mediated cell fusion, bioRxiv, doi:10.1101/2023.09.28.560070.
41.
Mohd Abd Razak et al., In Vitro Anti-SARS-CoV-2 Activities of Curcumin and Selected Phenolic Compounds, Natural Product Communications, doi:10.1177/1934578X231188861.
42.
Fam et al., Channel activity of SARS-CoV-2 viroporin ORF3a inhibited by adamantanes and phenolic plant metabolites, Scientific Reports, doi:10.1038/s41598-023-31764-9.
43.
Teshima et al., Antiviral activity of curcumin and its analogs selected by an artificial intelligence-supported activity prediction system in SARS-CoV-2-infected VeroE6 cells, Natural Product Research, doi:10.1080/14786419.2023.2194647.
44.
Zupin et al., Optimization of Anti-SARS-CoV-2 Treatments Based on Curcumin, Used Alone or Employed as a Photosensitizer, Viruses, doi:10.3390/v14102132.
45.
Leka et al., In vitro antiviral activity against SARS-CoV-2 of common herbal medicinal extracts and their bioactive compounds, Phytotherapy Research, doi:10.1002/ptr.7463.
46.
Goc et al., Inhibitory effects of specific combination of natural compounds against SARS-CoV-2 and its Alpha, Beta, Gamma, Delta, Kappa, and Mu variants, European Journal of Microbiology and Immunology, doi:10.1556/1886.2021.00022.
47.
Marín-Palma et al., Curcumin Inhibits In Vitro SARS-CoV-2 Infection In Vero E6 Cells through Multiple Antiviral Mechanisms, Molecules, doi:10.3390/molecules26226900.
48.
Bahun et al., Inhibition of the SARS-CoV-2 3CLpro main protease by plant polyphenols, Food Chemistry, doi:10.1016/j.foodchem.2021.131594.
49.
Bormann et al., Turmeric Root and Its Bioactive Ingredient Curcumin Effectively Neutralize SARS-CoV-2 In Vitro, Viruses, doi:10.3390/v13101914.
50.
Guijarro-Real et al., Potential In Vitro Inhibition of Selected Plant Extracts against SARS-CoV-2 Chymotripsin-Like Protease (3CLPro) Activity, Foods, doi:10.3390/foods10071503.
a.
The trimeric spike (S) protein is a glycoprotein that mediates viral entry by binding to the host ACE2 receptor, is critical for SARS-CoV-2's ability to infect host cells, and is a target of neutralizing antibodies. Inhibition of the spike protein prevents viral attachment, halting infection at the earliest stage.
b.
The receptor binding domain is a specific region of the spike protein that binds ACE2 and is a major target of neutralizing antibodies. Focusing on the precise binding site allows highly specific disruption of viral attachment with reduced potential for off-target effects.
c.
The main protease or Mpro, also known as 3CLpro or nsp5, is a cysteine protease that cleaves viral polyproteins into functional units needed for replication. Inhibiting Mpro disrupts the SARS-CoV-2 lifecycle within the host cell, preventing the creation of new copies.
d.
RNA-dependent RNA polymerase (RdRp), also called nsp12, is the core enzyme of the viral replicase-transcriptase complex that copies the positive-sense viral RNA genome into negative-sense templates for progeny RNA synthesis. Inhibiting RdRp blocks viral genome replication and transcription.
e.
The papain-like protease (PLpro) has multiple functions including cleaving viral polyproteins and suppressing the host immune response by deubiquitination and deISGylation of host proteins. Inhibiting PLpro may block viral replication and help restore normal immune responses.
f.
The angiotensin converting enzyme 2 (ACE2) protein is a host cell transmembrane protein that serves as the cellular receptor for the SARS-CoV-2 spike protein. ACE2 is expressed on many cell types, including epithelial cells in the lungs, and allows the virus to enter and infect host cells. Inhibition may affect ACE2's physiological function in blood pressure control.
g.
The nucleocapsid (N) protein binds and encapsulates the viral genome by coating the viral RNA. N enables formation and release of infectious virions and plays additional roles in viral replication and pathogenesis. N is also an immunodominant antigen used in diagnostic assays.
h.
Non-structural protein 10 (nsp10) serves as an RNA chaperone and stabilizes conformations of nsp12 and nsp14 in the replicase-transcriptase complex, which synthesizes new viral RNAs. Nsp10 disruption may destabilize replicase-transcriptase complex activity.
i.
The helicase, or nsp13, protein unwinds the double-stranded viral RNA, a crucial step in replication and transcription. Inhibition may prevent viral genome replication and the creation of new virus components.
j.
The interaction between the SARS-CoV-2 spike protein and the human ACE2 receptor is a primary method of viral entry, inhibiting this interaction can prevent the virus from attaching to and entering host cells, halting infection at an early stage.
k.
Transmembrane protease serine 2 (TMPRSS2) is a host cell protease that primes the spike protein, facilitating cellular entry. TMPRSS2 activity helps enable cleavage of the spike protein required for membrane fusion and virus entry. Inhibition may especially protect respiratory epithelial cells, buy may have physiological effects.
l.
Calu-3 is a human lung adenocarcinoma cell line with moderate ACE2 and TMPRSS2 expression and SARS-CoV-2 susceptibility. It provides a model of the human respiratory epithelium, but many not be ideal for modeling early stages of infection due to the moderate expression levels of ACE2 and TMPRSS2.
m.
A549 is a human lung carcinoma cell line with low ACE2 expression and SARS-CoV-2 susceptibility. Viral entry/replication can be studied but the cells may not replicate all aspects of lung infection.
n.
A549-AT is a human lung carcinoma cell line stably transfected with ACE2 and TMPRSS2 receptors. Unlike the parental line, this overexpression ensures stable infection and enhanced viral entry, allowing for the evaluation of antiviral efficacy against various SARS-CoV-2 variants.
o.
293T is a human embryonic kidney cell line that can be engineered for high ACE2 expression and SARS-CoV-2 susceptibility. 293T cells are easily transfected and support high protein expression.
p.
HEK293-hACE2 is a human embryonic kidney cell line with high ACE2 expression and SARS-CoV-2 susceptibility. Cells have been transfected with a plasmid to express the human ACE2 (hACE2) protein.
q.
293T/hACE2/TMPRSS2 is a human embryonic kidney cell line engineered for high ACE2 and TMPRSS2 expression, which mimics key aspects of human infection. 293T/hACE2/TMPRSS2 cells are very susceptible to SARS-CoV-2 infection.
r.
Vero E6 is an African green monkey kidney cell line with low/no ACE2 expression and high SARS-CoV-2 susceptibility. The cell line is easy to maintain and supports robust viral replication, however the monkey origin may not accurately represent human responses.
s.
SH-SY5Y is a human neuroblastoma cell line that exhibits neuronal phenotypes. It is commonly used as an in vitro model for studying neurotoxicity, neurodegenerative diseases, and neuronal differentiation.
Van Tin et al., 11 Aug 2024, peer-reviewed, 5 authors.
Contact: yuhsunkao@gmail.com (corresponding author), d142109010@tmu.edu.tw, lekha@tmu.edu.tw, higa@haku-ai.or.jp, yjchen@tmu.edu.tw.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling
Cells, doi:10.3390/cells13161331
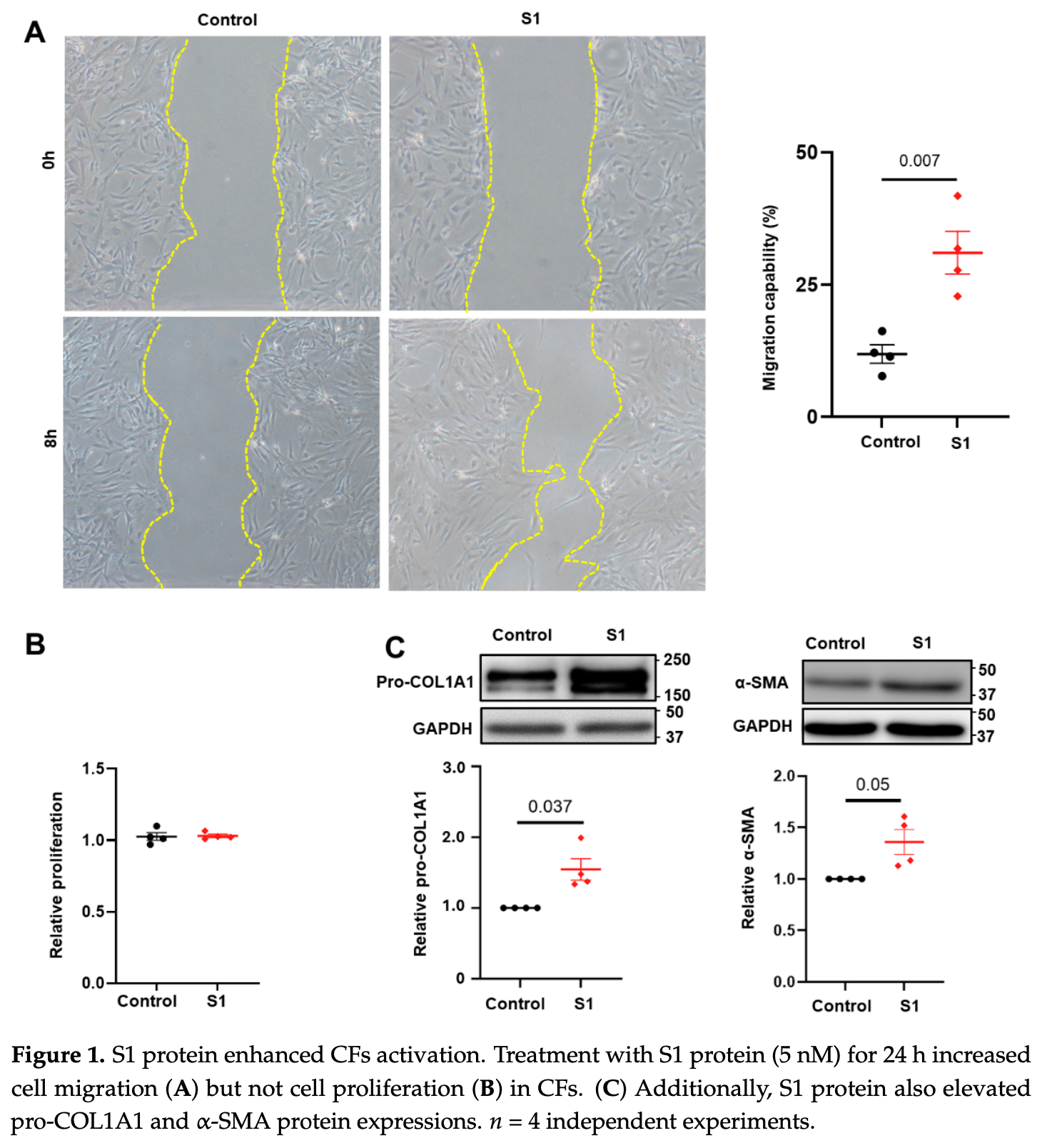
Background: The spike protein of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is crucial to viral entry and can cause cardiac injuries. Toll-like receptor 4 (TLR4) and NOD-, LPR-, and pyrin-domain-containing 3 (NLRP3) inflammasome are critical immune system components implicated in cardiac fibrosis. The spike proteins activate NLRP3 inflammasome through TLR4 or angiotensin-converting enzyme 2 (ACE2) receptors, damaging various organs. However, the role of spike proteins in cardiac fibrosis in humans and the interactions of spike proteins with NLRP3 inflammasomes and TLR4 remain poorly understood. Methods: We utilized scratch assays, Western blotting, and immunofluorescence to evaluate the migration, fibrosis signaling, mitochondrial calcium levels, reactive oxygen species (ROS) production, and cell morphology of cultured human cardiac fibroblasts (CFs) treated with spike (S1) proteins for 24 h with or without an anti-ACE2 neutralizing antibody, a TLR4 blocker, or an NLRP3 inhibitor. Results: S1 protein enhanced CFs migration and the expressions of collagen 1, α-smooth muscle actin, transforming growth factor β1 (TGF-β1), phosphorylated SMAD2/3, interleukin 1β (IL-1β), and nuclear factor kappa-light-chainenhancer of activated B cells (NF-κB). S1 increased ROS production but did not affect mitochondrial calcium content and cell morphology. Treatment with an anti-ACE2 neutralizing antibody attenuated the effects of S1 on collagen 1 and TGF-β1 expressions. Moreover, NLRP3 (MCC950) and NF-kB inhibitors, but not the TLR4 inhibitor TAK-242, prevented the S1-enhanced CFs migration and overexpression of collagen 1, TGF-β1, and IL-1β. Conclusion: S1 activates human CFs by priming NLRP3 inflammasomes through NF-κB signaling in an ACE2-dependent manner.
Supplementary Materials: The following supporting information can be downloaded at: https://www. mdpi.com/article/10.3390/cells13161331/s1, Figure S1 : Effect of S1 protein on CFs mitochondrial morphology; Figure S2 : Effect of S1 protein on CFs mitochondrial calcium levels; Figure S3 : Effect of S1 protein on CFs mitochondrial ROS production.
References
Albornoz, Amarilla, Modhiran, Parker, Li et al., SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein, Mol. Psychiatry, doi:10.1038/s41380-022-01831-0
Avolio, Carrabba, Milligan, Kavanagh Williamson, Beltrami et al., The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147 receptor-mediated signalling: A potential non-infective mechanism of COVID-19 microvascular disease, Clin. Sci, doi:10.1042/CS20210735
Avolio, Srivastava, Ji, Carrabba, Tsang et al., Murine studies and expressional analyses of human cardiac pericytes reveal novel trajectories of SARS-CoV-2 Spike protein-induced microvascular damage, Signal Transduct. Target. Ther, doi:10.1038/s41392-023-01489-2
Babadaei, Hasan, Bloukh, Edis, Sharifi et al., The expression level of angiotensinconverting enzyme 2 determines the severity of COVID-19: Lung and heart tissue as targets, J. Biomol. Struct. Dyn, doi:10.1080/07391102.2020.1767211
Bai, Li, Liu, Gao, Zhang et al., Effects of IL-1β and IL-18 induced by NLRP3 inflammasome activation on myocardial reperfusion injury after PCI, Eur. Rev. Med. Pharmacol. Sci, doi:10.26355/eurrev_201911_19579
Boretti, PQQ Supplementation and SARS-CoV-2 Spike Protein-Induced Heart Inflammation, Nat. Prod. Commun, doi:10.1177/1934578X221080929
Borkotoky, Dey, Hazarika, Interactions of angiotensin-converting enzyme-2 (ACE2) and SARS-CoV-2 spike receptorbinding domain (RBD): A structural perspective, Mol. Biol. Rep, doi:10.1007/s11033-022-08193-4
Cao, Nguyen, Tsai, Gao, Tian et al., The SARS-CoV-2 spike protein induces long-term transcriptional perturbations of mitochondrial metabolic genes, causes cardiac fibrosis, and reduces myocardial contractile in obese mice, Mol. Metab, doi:10.1016/j.molmet.2023.101756
Clemens, Ye, Zhou, Kim, Pease et al., SARS-CoV-2 spike protein-mediated cardiomyocyte fusion may contribute to increased arrhythmic risk in COVID-19, PLoS ONE, doi:10.1371/journal.pone.0282151
Corpetti, Del Re, Seguella, Palenca, Rurgo et al., Cannabidiol inhibits SARS-Cov-2 spike (S) protein-induced cytotoxicity and inflammation through a PPARγ-dependent TLR4/NLRP3/Caspase-1 signaling suppression in Caco-2 cell line, Phytother. Res, doi:10.1002/ptr.7302
Del Re, Corpetti, Pesce, Seguella, Steardo et al., Ultramicronized Palmitoylethanolamide Inhibits NLRP3 Inflammasome Expression and Pro-Inflammatory Response Activated by SARS-CoV-2 Spike Protein in Cultured Murine Alveolar Macrophages, Metabolites, doi:10.3390/metabo11090592
Driggin, Madhavan, Bikdeli, Chuich, Laracy et al., Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic, J. Am. Coll. Cardiol, doi:10.1016/j.jacc.2020.03.031
Fontes-Dantas, Fernandes, Gutman, De Lima, Antonio et al., SARS-CoV-2 Spike protein induces TLR4-mediated long-term cognitive dysfunction recapitulating post-COVID-19 syndrome in mice, Cell Rep, doi:10.1016/j.celrep.2023.112189
Gupta, Madhavan, Sehgal, Nair, Mahajan et al., Extrapulmonary manifestations of COVID-19, Nat. Med, doi:10.1038/s41591-020-0968-3
Guy, Lambert, Turner, Porter, Functional angiotensin-converting enzyme 2 is expressed in human cardiac myofibroblasts, Exp. Physiol, doi:10.1113/expphysiol.2007.040139
Han, Zeng, Jiang, Yang, Yuan et al., CSC expert consensus on principles of clinical management of patients with severe emergent cardiovascular diseases during the COVID-19 epidemic, Circulation, doi:10.1161/CIRCULATIONAHA.120.047011
Huang, Huang, He, Feng, Shi et al., Sars-Cov-2 Spike Protein-Induced Damage of hiPSC-Derived Cardiomyocytes, Adv. Biol, doi:10.1002/adbi.202101327
Huang, Yang, Xu, Xu, Liu, Structural and functional properties of SARS-CoV-2 spike protein: Potential antivirus drug development for COVID-19, Acta Pharmacol. Sin, doi:10.1038/s41401-020-0485-4
Huynh, Rethi, Lee, Higa, Kao et al., Spike Protein Impairs Mitochondrial Function in Human Cardiomyocytes: Mechanisms Underlying Cardiac Injury in COVID-19, Cells, doi:10.3390/cells12060877
Imig, SARS-CoV-2 spike protein causes cardiovascular disease independent of viral infection, Clin. Sci, doi:10.1042/CS20220028
Kato, Nishiyama, Man Lee, Ibuki, Imai et al., TRPC3-Nox2 Protein Complex Formation Increases the Risk of SARS-CoV-2 Spike Protein-Induced Cardiomyocyte Dysfunction through ACE2 Upregulation, Int. J. Mol. Sci, doi:10.3390/ijms24010102
Kelley, Jeltema, Duan, He, The NLRP3 Inflammasome: An Overview of Mechanisms of Activation and Regulation, Int. J. Mol. Sci, doi:10.3390/ijms20133328
Kole, Stefanou, Karvelas, Schizas, Toutouzas, Acute and Post-Acute COVID-19 Cardiovascular Complications: A Comprehensive Review, Cardiovasc. Drugs Ther, doi:10.1007/s10557-023-07465-w
Kong, Christia, Frangogiannis, The pathogenesis of cardiac fibrosis, Cell Mol. Life Sci, doi:10.1007/s00018-013-1349-6
Krishnan, Ellenberger, Phetsouphanh, Kelleher, Matthews et al., Myocardial fibrosis occurs in non-hospitalised patients with chronic symptoms after COVID-19, Int. J. Cardiol. Heart Vasc, doi:10.1016/j.ijcha.2022.100964
Liang, Bao, Yang, Liu, Sun et al., SARS-CoV-2 spike protein induces IL-18-mediated cardiopulmonary inflammation via reduced mitophagy, Signal Transduct. Target. Ther
Lin, More than a key-the pathological roles of SARS-CoV-2 spike protein in COVID-19 related cardiac injury, Sports Med. Health Sci, doi:10.1016/j.smhs.2023.03.004
Litvi Ňuková, Talavera-López, Maatz, Reichart, Worth et al., Cells of the adult human heart, Nature, doi:10.1038/s41586-020-2797-4
Liu, Gai, Wang, Zeng, Sun et al., Single-cell analysis of SARS-CoV-2 receptor ACE2 and spike protein priming expression of proteases in the human heart, Cardiovasc. Res, doi:10.1093/cvr/cvaa191
Liu, Liu, Wang, COVID-19 and cardiovascular diseases, J. Mol. Cell Biol, doi:10.1093/jmcb/mjaa064
Madjid, Safavi-Naeini, Solomon, Vardeny, Potential effects of coronaviruses on the cardiovascular system: A review, JAMA Cardiol, doi:10.1001/jamacardio.2020.1286
Oudit, Wang, Viveiros, Kellner, Penninger, Angiotensin-converting enzyme 2-at the heart of the COVID-19 pandemic, Cell, doi:10.1016/j.cell.2023.01.039
Parhizgar, Yazdankhah, Rzepka, Chung, Ali et al., Beyond Acute COVID-19: A Review of Long-term Cardiovascular Outcomes, Can. J. Cardiol, doi:10.1016/j.cjca.2023.01.031
Raafs, Ghossein, Brandt, Henkens, Kooi et al., Cardiovascular outcome 6 months after severe coronavirus disease 2019 infection, J. Hypertens, doi:10.1097/HJH.0000000000003110
Segura-Villalobos, Roa-Velázquez, Zavala-Vargas, Filisola-Villaseñor, Castillo Arellano et al., Jacareubin inhibits TLR4-induced lung inflammatory response caused by the RBD domain of SARS-CoV-2 Spike protein, Pharmacol. Rep, doi:10.1007/s43440-022-00398-5
Shen, Gong, Zhang, Cao, Mao et al., Besides TLR2 and TLR4, NLRP3 is also involved in regulating Escherichia coli infection-induced inflammatory responses in mice, Int. Immunopharmacol, doi:10.1016/j.intimp.2023.110556
Shi, Qin, Cai, Liu, Shen et al., Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019, Eur. Heart J, doi:10.1093/eurheartj/ehaa408
Shirato, Kizaki, SARS-CoV-2 spike protein S1 subunit induces pro-inflammatory responses via toll-like receptor 4 signaling in murine and human macrophages, Heliyon, doi:10.1016/j.heliyon.2021.e06187
Travers, Kamal, Robbins, Yutzey, Blaxall, Cardiac Fibrosis: The Fibroblast Awakens, Circ. Res, doi:10.1161/CIRCRESAHA.115.306565
Turner, Inflammatory and fibrotic responses of cardiac fibroblasts to myocardial damage associated molecular patterns (DAMPs), J. Mol. Cell Cardiol, doi:10.1016/j.yjmcc.2015.11.002
Wang, Zhang, Xiao, Zhang, Wu et al., NLRP3 Inflammasome and Inflammatory Diseases, Oxid. Med. Cell Longev, doi:10.1155/2020/4063562
Wicherska-Pawłowska, Wróbel, Rybka, Toll-Like Receptors (TLRs), NOD-Like Receptors (NLRs), and RIG-I-Like Receptors (RLRs) in Innate Immunity. TLRs, NLRs, and RLRs Ligands as Immunotherapeutic Agents for Hematopoietic Diseases, Int. J. Mol. Sci, doi:10.3390/ijms222413397
Zheng, Ma, Zhang, Xie, COVID-19 and the cardiovascular system, Nat. Rev. Cardiol, doi:10.1038/s41569-020-0360-5
Zhu, Zhang, Wang, Li, Yang et al., A Novel Coronavirus from Patients with Pneumonia in China, New Engl. J. Med, doi:10.1056/NEJMoa2001017
DOI record:
{
"DOI": "10.3390/cells13161331",
"ISSN": [
"2073-4409"
],
"URL": "http://dx.doi.org/10.3390/cells13161331",
"abstract": "<jats:p>Background: The spike protein of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is crucial to viral entry and can cause cardiac injuries. Toll-like receptor 4 (TLR4) and NOD-, LPR-, and pyrin-domain-containing 3 (NLRP3) inflammasome are critical immune system components implicated in cardiac fibrosis. The spike proteins activate NLRP3 inflammasome through TLR4 or angiotensin-converting enzyme 2 (ACE2) receptors, damaging various organs. However, the role of spike proteins in cardiac fibrosis in humans and the interactions of spike proteins with NLRP3 inflammasomes and TLR4 remain poorly understood. Methods: We utilized scratch assays, Western blotting, and immunofluorescence to evaluate the migration, fibrosis signaling, mitochondrial calcium levels, reactive oxygen species (ROS) production, and cell morphology of cultured human cardiac fibroblasts (CFs) treated with spike (S1) proteins for 24 h with or without an anti-ACE2 neutralizing antibody, a TLR4 blocker, or an NLRP3 inhibitor. Results: S1 protein enhanced CFs migration and the expressions of collagen 1, α-smooth muscle actin, transforming growth factor β1 (TGF-β1), phosphorylated SMAD2/3, interleukin 1β (IL-1β), and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB). S1 increased ROS production but did not affect mitochondrial calcium content and cell morphology. Treatment with an anti-ACE2 neutralizing antibody attenuated the effects of S1 on collagen 1 and TGF-β1 expressions. Moreover, NLRP3 (MCC950) and NF-kB inhibitors, but not the TLR4 inhibitor TAK-242, prevented the S1-enhanced CFs migration and overexpression of collagen 1, TGF-β1, and IL-1β. Conclusion: S1 activates human CFs by priming NLRP3 inflammasomes through NF-κB signaling in an ACE2-dependent manner.</jats:p>",
"alternative-id": [
"cells13161331"
],
"author": [
{
"affiliation": [
{
"name": "International Ph.D. Program in Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan"
}
],
"family": "Van Tin",
"given": "Huynh",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Orthopedics, Shuangho Hospital, Taipei Medical University, Taipei 11031, Taiwan"
}
],
"family": "Rethi",
"given": "Lekha",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5735-6249",
"affiliation": [
{
"name": "Cardiac Electrophysiology and Pacing Laboratory, Division of Cardiovascular Medicine, Makiminato Central Hospital, Okinawa 901-2131, Japan"
}
],
"authenticated-orcid": false,
"family": "Higa",
"given": "Satoshi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8687-5091",
"affiliation": [
{
"name": "International Ph.D. Program in Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan"
},
{
"name": "Graduate Institute of Clinical Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan"
},
{
"name": "Department of Medical Education and Research, Wan Fang Hospital, Taipei Medical University, Taipei 11031, Taiwan"
}
],
"authenticated-orcid": false,
"family": "Kao",
"given": "Yu-Hsun",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7224-4491",
"affiliation": [
{
"name": "International Ph.D. Program in Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan"
},
{
"name": "Graduate Institute of Clinical Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan"
},
{
"name": "Division of Cardiovascular Medicine, Department of Internal Medicine, Wan Fang Hospital, Taipei Medical University, Taipei 11031, Taiwan"
}
],
"authenticated-orcid": false,
"family": "Chen",
"given": "Yi-Jen",
"sequence": "additional"
}
],
"container-title": "Cells",
"container-title-short": "Cells",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
8,
12
]
],
"date-time": "2024-08-12T09:19:38Z",
"timestamp": 1723454378000
},
"deposited": {
"date-parts": [
[
2024,
8,
12
]
],
"date-time": "2024-08-12T09:47:48Z",
"timestamp": 1723456068000
},
"funder": [
{
"DOI": "10.13039/501100020950",
"award": [
"110-2314-B-038-128"
],
"doi-asserted-by": "publisher",
"name": "National Science and Technology Council"
},
{
"DOI": "10.13039/501100022600",
"award": [
"113-wf-eva-12"
],
"doi-asserted-by": "publisher",
"name": "Wan Fang Hospital"
},
{
"award": [
"6-02-003"
],
"name": "Foundation for the Development of Internal Medicine in Okinawa"
}
],
"indexed": {
"date-parts": [
[
2024,
8,
13
]
],
"date-time": "2024-08-13T00:17:05Z",
"timestamp": 1723508225225
},
"is-referenced-by-count": 0,
"issue": "16",
"issued": {
"date-parts": [
[
2024,
8,
11
]
]
},
"journal-issue": {
"issue": "16",
"published-online": {
"date-parts": [
[
2024,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
8,
11
]
],
"date-time": "2024-08-11T00:00:00Z",
"timestamp": 1723334400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2073-4409/13/16/1331/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1331",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
8,
11
]
]
},
"published-online": {
"date-parts": [
[
2024,
8,
11
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/j.jacc.2020.03.031",
"article-title": "Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic",
"author": "Driggin",
"doi-asserted-by": "crossref",
"first-page": "2352",
"journal-title": "J. Am. Coll. Cardiol.",
"key": "ref_1",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047011",
"article-title": "CSC expert consensus on principles of clinical management of patients with severe emergent cardiovascular diseases during the COVID-19 epidemic",
"author": "Han",
"doi-asserted-by": "crossref",
"first-page": "e810",
"journal-title": "Circulation",
"key": "ref_2",
"volume": "141",
"year": "2020"
},
{
"DOI": "10.1001/jamacardio.2020.1286",
"article-title": "Potential effects of coronaviruses on the cardiovascular system: A review",
"author": "Madjid",
"doi-asserted-by": "crossref",
"first-page": "831",
"journal-title": "JAMA Cardiol.",
"key": "ref_3",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1038/s41569-020-0360-5",
"article-title": "COVID-19 and the cardiovascular system",
"author": "Zheng",
"doi-asserted-by": "crossref",
"first-page": "259",
"journal-title": "Nat. Rev. Cardiol.",
"key": "ref_4",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.cjca.2023.01.031",
"article-title": "Beyond Acute COVID-19: A Review of Long-term Cardiovascular Outcomes",
"author": "Parhizgar",
"doi-asserted-by": "crossref",
"first-page": "726",
"journal-title": "Can. J. Cardiol.",
"key": "ref_5",
"volume": "39",
"year": "2023"
},
{
"DOI": "10.1097/HJH.0000000000003110",
"article-title": "Cardiovascular outcome 6 months after severe coronavirus disease 2019 infection",
"author": "Raafs",
"doi-asserted-by": "crossref",
"first-page": "1278",
"journal-title": "J. Hypertens.",
"key": "ref_6",
"volume": "40",
"year": "2022"
},
{
"article-title": "Myocardial fibrosis occurs in non-hospitalised patients with chronic symptoms after COVID-19",
"author": "Krishnan",
"first-page": "100964",
"journal-title": "Int. J. Cardiol. Heart Vasc.",
"key": "ref_7",
"volume": "39",
"year": "2022"
},
{
"article-title": "PQQ Supplementation and SARS-CoV-2 Spike Protein-Induced Heart Inflammation",
"author": "Boretti",
"first-page": "1934578x221080929",
"journal-title": "Nat. Prod. Commun.",
"key": "ref_8",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1016/j.molmet.2023.101756",
"article-title": "The SARS-CoV-2 spike protein induces long-term transcriptional perturbations of mitochondrial metabolic genes, causes cardiac fibrosis, and reduces myocardial contractile in obese mice",
"author": "Cao",
"doi-asserted-by": "crossref",
"first-page": "101756",
"journal-title": "Mol. Metab.",
"key": "ref_9",
"volume": "74",
"year": "2023"
},
{
"DOI": "10.3390/cells12060877",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Huynh, T.V., Rethi, L., Lee, T.W., Higa, S., Kao, Y.H., and Chen, Y.J. (2023). Spike Protein Impairs Mitochondrial Function in Human Cardiomyocytes: Mechanisms Underlying Cardiac Injury in COVID-19. Cells, 12."
},
{
"DOI": "10.1371/journal.pone.0282151",
"doi-asserted-by": "crossref",
"key": "ref_11",
"unstructured": "Clemens, D.J., Ye, D., Zhou, W., Kim, C.S.J., Pease, D.R., Navaratnarajah, C.K., Barkhymer, A., Tester, D.J., Nelson, T.J., and Cattaneo, R. (2023). SARS-CoV-2 spike protein-mediated cardiomyocyte fusion may contribute to increased arrhythmic risk in COVID-19. PLoS ONE, 18."
},
{
"DOI": "10.1093/cvr/cvaa191",
"article-title": "Single-cell analysis of SARS-CoV-2 receptor ACE2 and spike protein priming expression of proteases in the human heart",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "1733",
"journal-title": "Cardiovasc. Res.",
"key": "ref_12",
"volume": "116",
"year": "2020"
},
{
"DOI": "10.1038/s41392-023-01489-2",
"article-title": "Murine studies and expressional analyses of human cardiac pericytes reveal novel trajectories of SARS-CoV-2 Spike protein-induced microvascular damage",
"author": "Avolio",
"doi-asserted-by": "crossref",
"first-page": "232",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_13",
"volume": "8",
"year": "2023"
},
{
"DOI": "10.3390/ijms24010102",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Kato, Y., Nishiyama, K., Man Lee, J., Ibuki, Y., Imai, Y., Noda, T., Kamiya, N., Kusakabe, T., Kanda, Y., and Nishida, M. (2022). TRPC3-Nox2 Protein Complex Formation Increases the Risk of SARS-CoV-2 Spike Protein-Induced Cardiomyocyte Dysfunction through ACE2 Upregulation. Int. J. Mol. Sci., 24."
},
{
"DOI": "10.1016/j.smhs.2023.03.004",
"doi-asserted-by": "crossref",
"key": "ref_15",
"unstructured": "Lin, Z. (2023). More than a key-the pathological roles of SARS-CoV-2 spike protein in COVID-19 related cardiac injury. Sports Med. Health Sci., in press."
},
{
"DOI": "10.1042/CS20210735",
"article-title": "The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147 receptor-mediated signalling: A potential non-infective mechanism of COVID-19 microvascular disease",
"author": "Avolio",
"doi-asserted-by": "crossref",
"first-page": "2667",
"journal-title": "Clin. Sci.",
"key": "ref_16",
"volume": "135",
"year": "2021"
},
{
"DOI": "10.1007/s11033-022-08193-4",
"article-title": "Interactions of angiotensin-converting enzyme-2 (ACE2) and SARS-CoV-2 spike receptor-binding domain (RBD): A structural perspective",
"author": "Borkotoky",
"doi-asserted-by": "crossref",
"first-page": "2713",
"journal-title": "Mol. Biol. Rep.",
"key": "ref_17",
"volume": "50",
"year": "2023"
},
{
"DOI": "10.1038/s41401-020-0485-4",
"article-title": "Structural and functional properties of SARS-CoV-2 spike protein: Potential antivirus drug development for COVID-19",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "1141",
"journal-title": "Acta Pharmacol. Sin.",
"key": "ref_18",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2023.01.039",
"article-title": "Angiotensin-converting enzyme 2-at the heart of the COVID-19 pandemic",
"author": "Oudit",
"doi-asserted-by": "crossref",
"first-page": "906",
"journal-title": "Cell",
"key": "ref_19",
"volume": "186",
"year": "2023"
},
{
"DOI": "10.1080/07391102.2020.1767211",
"article-title": "The expression level of angiotensin-converting enzyme 2 determines the severity of COVID-19: Lung and heart tissue as targets",
"author": "Babadaei",
"doi-asserted-by": "crossref",
"first-page": "3780",
"journal-title": "J. Biomol. Struct. Dyn.",
"key": "ref_20",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2797-4",
"article-title": "Cells of the adult human heart",
"author": "Maatz",
"doi-asserted-by": "crossref",
"first-page": "466",
"journal-title": "Nature",
"key": "ref_21",
"volume": "588",
"year": "2020"
},
{
"DOI": "10.1113/expphysiol.2007.040139",
"article-title": "Functional angiotensin-converting enzyme 2 is expressed in human cardiac myofibroblasts",
"author": "Guy",
"doi-asserted-by": "crossref",
"first-page": "579",
"journal-title": "Exp. Physiol.",
"key": "ref_22",
"volume": "93",
"year": "2008"
},
{
"DOI": "10.3390/ijms20133328",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Kelley, N., Jeltema, D., Duan, Y., and He, Y. (2019). The NLRP3 Inflammasome: An Overview of Mechanisms of Activation and Regulation. Int. J. Mol. Sci., 20."
},
{
"article-title": "NLRP3 Inflammasome and Inflammatory Diseases",
"author": "Wang",
"first-page": "4063562",
"journal-title": "Oxid. Med. Cell Longev.",
"key": "ref_24",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.3390/ijms222413397",
"doi-asserted-by": "crossref",
"key": "ref_25",
"unstructured": "Wicherska-Pawłowska, K., Wróbel, T., and Rybka, J. (2021). Toll-Like Receptors (TLRs), NOD-Like Receptors (NLRs), and RIG-I-Like Receptors (RLRs) in Innate Immunity. TLRs, NLRs, and RLRs Ligands as Immunotherapeutic Agents for Hematopoietic Diseases. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.1016/j.intimp.2023.110556",
"article-title": "Besides TLR2 and TLR4, NLRP3 is also involved in regulating Escherichia coli infection-induced inflammatory responses in mice",
"author": "Shen",
"doi-asserted-by": "crossref",
"first-page": "110556",
"journal-title": "Int. Immunopharmacol.",
"key": "ref_26",
"volume": "121",
"year": "2023"
},
{
"DOI": "10.1038/s41380-022-01831-0",
"article-title": "SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein",
"author": "Albornoz",
"doi-asserted-by": "crossref",
"first-page": "2878",
"journal-title": "Mol. Psychiatry",
"key": "ref_27",
"volume": "28",
"year": "2023"
},
{
"DOI": "10.3390/metabo11090592",
"doi-asserted-by": "crossref",
"key": "ref_28",
"unstructured": "Del Re, A., Corpetti, C., Pesce, M., Seguella, L., Steardo, L., Palenca, I., Rurgo, S., De Conno, B., Sarnelli, G., and Esposito, G. (2021). Ultramicronized Palmitoylethanolamide Inhibits NLRP3 Inflammasome Expression and Pro-Inflammatory Response Activated by SARS-CoV-2 Spike Protein in Cultured Murine Alveolar Macrophages. Metabolites, 11."
},
{
"DOI": "10.1016/j.heliyon.2021.e06187",
"article-title": "SARS-CoV-2 spike protein S1 subunit induces pro-inflammatory responses via toll-like receptor 4 signaling in murine and human macrophages",
"author": "Shirato",
"doi-asserted-by": "crossref",
"first-page": "e06187",
"journal-title": "Heliyon",
"key": "ref_29",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1002/ptr.7302",
"article-title": "Cannabidiol inhibits SARS-Cov-2 spike (S) protein-induced cytotoxicity and inflammation through a PPARγ-dependent TLR4/NLRP3/Caspase-1 signaling suppression in Caco-2 cell line",
"author": "Corpetti",
"doi-asserted-by": "crossref",
"first-page": "6893",
"journal-title": "Phytother. Res.",
"key": "ref_30",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2001017",
"article-title": "A Novel Coronavirus from Patients with Pneumonia in China, 2019",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "727",
"journal-title": "New Engl. J. Med.",
"key": "ref_31",
"volume": "382",
"year": "2020"
},
{
"key": "ref_32",
"unstructured": "World Health Organization (2024, March 24). Data. Who. int, WHO Coronavirus (COVID-19) Dashboard Cases [Dashboard]. Available online: https://data.who.int/dashboards/covid19/cases."
},
{
"DOI": "10.1038/s41591-020-0968-3",
"article-title": "Extrapulmonary manifestations of COVID-19",
"author": "Gupta",
"doi-asserted-by": "crossref",
"first-page": "1017",
"journal-title": "Nat. Med.",
"key": "ref_33",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1093/jmcb/mjaa064",
"article-title": "COVID-19 and cardiovascular diseases",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "161",
"journal-title": "J. Mol. Cell Biol.",
"key": "ref_34",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1093/eurheartj/ehaa408",
"article-title": "Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "2070",
"journal-title": "Eur. Heart J.",
"key": "ref_35",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1007/s10557-023-07465-w",
"doi-asserted-by": "crossref",
"key": "ref_36",
"unstructured": "Kole, C., Stefanou, Ε., Karvelas, N., Schizas, D., and Toutouzas, K.P. (2023). Acute and Post-Acute COVID-19 Cardiovascular Complications: A Comprehensive Review. Cardiovasc. Drugs Ther., 1–16."
},
{
"DOI": "10.1042/CS20220028",
"article-title": "SARS-CoV-2 spike protein causes cardiovascular disease independent of viral infection",
"author": "Imig",
"doi-asserted-by": "crossref",
"first-page": "431",
"journal-title": "Clin. Sci.",
"key": "ref_37",
"volume": "136",
"year": "2022"
},
{
"DOI": "10.1002/adbi.202101327",
"doi-asserted-by": "crossref",
"key": "ref_38",
"unstructured": "Huang, X., Huang, B., He, Y., Feng, L., Shi, J., Wang, L., Peng, J., and Chen, Y. (2022). Sars-Cov-2 Spike Protein-Induced Damage of hiPSC-Derived Cardiomyocytes. Adv. Biol., 6."
},
{
"DOI": "10.1007/s00018-013-1349-6",
"article-title": "The pathogenesis of cardiac fibrosis",
"author": "Kong",
"doi-asserted-by": "crossref",
"first-page": "549",
"journal-title": "Cell Mol. Life Sci.",
"key": "ref_39",
"volume": "71",
"year": "2014"
},
{
"DOI": "10.1161/CIRCRESAHA.115.306565",
"article-title": "Cardiac Fibrosis: The Fibroblast Awakens",
"author": "Travers",
"doi-asserted-by": "crossref",
"first-page": "1021",
"journal-title": "Circ. Res.",
"key": "ref_40",
"volume": "118",
"year": "2016"
},
{
"DOI": "10.1016/j.yjmcc.2015.11.002",
"article-title": "Inflammatory and fibrotic responses of cardiac fibroblasts to myocardial damage associated molecular patterns (DAMPs)",
"author": "Turner",
"doi-asserted-by": "crossref",
"first-page": "189",
"journal-title": "J. Mol. Cell Cardiol.",
"key": "ref_41",
"volume": "94",
"year": "2016"
},
{
"article-title": "Effects of IL-1β and IL-18 induced by NLRP3 inflammasome activation on myocardial reperfusion injury after PCI",
"author": "Bai",
"first-page": "10101",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "ref_42",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.1007/s43440-022-00398-5",
"article-title": "Jacareubin inhibits TLR4-induced lung inflammatory response caused by the RBD domain of SARS-CoV-2 Spike protein",
"doi-asserted-by": "crossref",
"first-page": "1315",
"journal-title": "Pharmacol. Rep.",
"key": "ref_43",
"volume": "74",
"year": "2022"
},
{
"DOI": "10.1016/j.celrep.2023.112189",
"article-title": "SARS-CoV-2 Spike protein induces TLR4-mediated long-term cognitive dysfunction recapitulating post-COVID-19 syndrome in mice",
"author": "Fernandes",
"doi-asserted-by": "crossref",
"first-page": "112189",
"journal-title": "Cell Rep.",
"key": "ref_44",
"volume": "42",
"year": "2023"
},
{
"DOI": "10.1038/s41392-023-01368-w",
"article-title": "SARS-CoV-2 spike protein induces IL-18-mediated cardiopulmonary inflammation via reduced mitophagy",
"author": "Liang",
"doi-asserted-by": "crossref",
"first-page": "108",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_45",
"volume": "8",
"year": "2023"
}
],
"reference-count": 45,
"references-count": 45,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2073-4409/13/16/1331"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling",
"type": "journal-article",
"volume": "13"
}
vantin