A novel film spray containing curcumin inhibits SARS-CoV-2 and influenza virus infection and enhances mucosal immunity
et al., Virology Journal, doi:10.1186/s12985-023-02282-x, Jan 2024
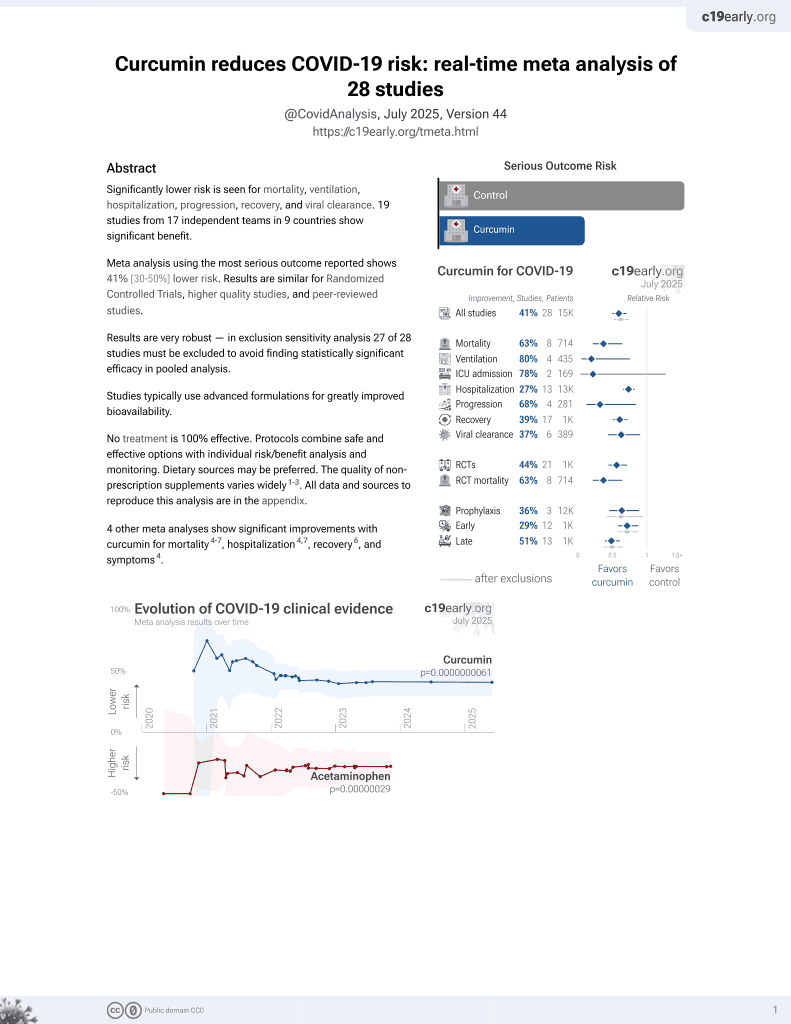
Curcumin for COVID-19
17th treatment shown to reduce risk in
February 2021, now with p = 0.0000000061 from 28 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
In vitro study showing that a novel oro-nasal curcumin film spray inhibits SARS-CoV-2 and influenza virus infection of cells while enhancing mucosal innate immunity. The spray demonstrated potent dose-dependent antiviral activity against SARS-CoV-2, influenza A H1N1, and influenza B viruses via plaque reduction assay. It was nontoxic to epithelial cell lines at antiviral concentrations. Additionally, the spray significantly induced secretion of antimicrobial peptides LL-37, HD-5 and anti-inflammatory cytokine IL-6 by oral keratinocytes, which may prevent viral entry and lung injury. Authors conclude that the spray could effectively inhibit SARS-CoV-2 and influenza infection while modulating inflammation.
62 preclinical studies support the efficacy of curcumin for COVID-19:
In silico studies predict inhibition of SARS-CoV-2 with curcumin or metabolites via binding to the spikeA,1,5,6,11,16,18,24,27 (and specifically the receptor binding domainB,2,4,14,17,20 ), MproC,4-6,11,13,15-17,19,20,22,25,27,28,30,48 , RNA-dependent RNA polymeraseD,4-6,17,26 , PLproE,6, ACE2F,2,18,19,21 , nucleocapsidG,12,29 , nsp10H,29, and helicaseI,36 proteins, and inhibition of spike-ACE2 interactionJ,3.
In vitro studies demonstrate inhibition of the spikeA,41 (and specifically the receptor binding domainB,51), MproC,23,41,48,50 , ACE2F,51, and TMPRSS2K,51 proteins, and inhibition of spike-ACE2 interactionJ,3,34 .
In vitro studies demonstrate efficacy in Calu-3L,49, A549M,41, A549-ATN,31, 293TO,7, HEK293-hACE2P,23,39 , 293T/hACE2/TMPRSS2Q,40, Vero E6R,1,13,17,27,39,41,43,45,47,49 , and SH-SY5YS,38 cells.
Curcumin decreases pro-inflammatory cytokines induced by SARS-CoV-2 in peripheral blood mononuclear cells47, alleviates SARS-CoV-2 spike protein-induced mitochondrial membrane damage and oxidative stress7, may limit COVID-19 induced cardiac damage by inhibiting the NF-κB signaling pathway which mediates the profibrotic effects of the SARS-CoV-2 spike protein on cardiac fibroblasts35, is predicted to inhibit the interaction between the SARS-CoV-2 spike protein receptor binding domain and the human ACE2 receptor for the delta and omicron variants14, lowers ACE2 and STAT3, curbing lung inflammation and ARDS in preclinical COVID-19 models32, inhibits SARS-CoV-2 ORF3a ion channel activity, which contributes to viral pathogenicity and cytotoxicity42, has direct virucidal action by disrupting viral envelope integrity44, may inhibit viral replication and modulate inflammatory pathways like NF-κB via SIRT1 activation52, and can function as a photosensitizer in photodynamic therapy to generate reactive oxygen species that damage the virus44.
1.
Marzouk et al., Computational and Experimental Insights into the Antiviral Mechanism of Turmeric (Curcuma longa) against SARS-CoV-2 D614G, BIO Web of Conferences, doi:10.1051/bioconf/202519804002.
2.
Wu et al., Utilizing natural compounds as ligands to disrupt the binding of SARS-CoV-2 receptor-binding domain to angiotensin-converting enzyme 2, impeding viral infection, Phytochemistry Letters, doi:10.1016/j.phytol.2025.102999.
3.
Najimi et al., Phytochemical Inhibitors of SARS‐CoV‐2 Entry: Targeting the ACE2‐RBD Interaction with l‐Tartaric Acid, l‐Ascorbic Acid, and Curcuma longa Extract, ChemistrySelect, doi:10.1002/slct.202406035.
4.
Rajamanickam et al., Exploring the Potential of Siddha Formulation MilagaiKudineer-Derived Phytotherapeutics Against SARS-CoV-2: An In-Silico Investigation for Antiviral Intervention, Journal of Pharmacy and Pharmacology Research, doi:10.26502/fjppr.0105.
5.
Al balawi et al., Assessing multi-target antiviral and antioxidant activities of natural compounds against SARS-CoV-2: an integrated in vitro and in silico study, Bioresources and Bioprocessing, doi:10.1186/s40643-024-00822-z.
6.
Haque et al., Exploring potential therapeutic candidates against COVID-19: a molecular docking study, Discover Molecules, doi:10.1007/s44345-024-00005-5.
7.
Zhang et al., Computational Discovery of Mitochondrial Dysfunction Biomarkers in Severe SARS-CoV-2 Infection: Facilitating Pytomedicine Screening, Phytomedicine, doi:10.1016/j.phymed.2024.155784.
8.
Öztürkkan et al., In Silico investigation of the effects of curcuminoids on the spike protein of the omicron variant of SARS-CoV-2, Baku State University Journal of Chemistry and Material Sciences, 1:2, bsuj.bsu.edu.az/uploads/pdf/ec4204d62f7802de54e6092bf7860029.pdf.
9.
Yunze et al., Therapeutic effect and potential mechanism of curcumin, an active ingredient in Tongnao Decoction, on COVID-19 combined with stroke: a network pharmacology study and GEO database mining, Research Square, doi:10.21203/rs.3.rs-4329762/v1.
10.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
11.
Boseila et al., Throat spray formulated with virucidal Pharmaceutical excipients as an effective early prophylactic or treatment strategy against pharyngitis post-exposure to SARS CoV-2, European Journal of Pharmaceutics and Biopharmaceutics, doi:10.1016/j.ejpb.2024.114279.
12.
Hidayah et al., Bioinformatics study of curcumin, demethoxycurcumin, bisdemethoxycurcumin and cyclocurcumin compounds in Curcuma longa as an antiviral agent via nucleocapsid on SARS-CoV-2 inhibition, International Conference on Organic and Applied Chemistry, doi:10.1063/5.0197724.
13.
Singh et al., Unlocking the potential of phytochemicals in inhibiting SARS-CoV-2 M Pro protein - An in-silico and cell-based approach, Research Square, doi:10.21203/rs.3.rs-3888947/v1.
14.
Kant et al., Structure-based drug discovery to identify SARS-CoV2 spike protein–ACE2 interaction inhibitors, Journal of Biomolecular Structure and Dynamics, doi:10.1080/07391102.2023.2300060.
15.
Naderi Beni et al., In silico studies of anti-oxidative and hot temperament-based phytochemicals as natural inhibitors of SARS-CoV-2 Mpro, PLOS ONE, doi:10.1371/journal.pone.0295014.
16.
Moschovou et al., Exploring the Binding Effects of Natural Products and Antihypertensive Drugs on SARS-CoV-2: An In Silico Investigation of Main Protease and Spike Protein, International Journal of Molecular Sciences, doi:10.3390/ijms242115894.
17.
Eleraky et al., Curcumin Transferosome-Loaded Thermosensitive Intranasal in situ Gel as Prospective Antiviral Therapy for SARS-Cov-2, International Journal of Nanomedicine, doi:10.2147/IJN.S423251.
18.
Singh (B) et al., Computational studies to analyze effect of curcumin inhibition on coronavirus D614G mutated spike protein, The Seybold Report, doi:10.17605/OSF.IO/TKEXJ.
19.
Thapa et al., In-silico Approach for Predicting the Inhibitory Effect of Home Remedies on Severe Acute Respiratory Syndrome Coronavirus-2, Makara Journal of Science, doi:10.7454/mss.v27i3.1609.
20.
Srivastava et al., Paradigm of Well-Orchestrated Pharmacokinetic Properties of Curcuminoids Relative to Conventional Drugs for the Inactivation of SARS-CoV-2 Receptors: An In Silico Approach, Stresses, doi:10.3390/stresses3030043.
21.
Alkafaas et al., A study on the effect of natural products against the transmission of B.1.1.529 Omicron, Virology Journal, doi:10.1186/s12985-023-02160-6.
22.
Winih Kinasih et al., Analisis in silico interaksi senyawa kurkuminoid terhadap enzim main protease 6LU7 dari SARS-CoV-2, Duta Pharma Journal, doi:10.47701/djp.v3i1.2904.
23.
Wu (B) et al., Potential Mechanism of Curcumin and Resveratrol against SARS-CoV-2, Research Square, doi:10.21203/rs.3.rs-2780614/v1.
24.
Nag et al., Curcumin inhibits spike protein of new SARS-CoV-2 variant of concern (VOC) Omicron, an in silico study, Computers in Biology and Medicine, doi:10.1016/j.compbiomed.2022.105552.
25.
Rampogu et al., Molecular Docking and Molecular Dynamics Simulations Discover Curcumin Analogue as a Plausible Dual Inhibitor for SARS-CoV-2, International Journal of Molecular Sciences, doi:10.3390/ijms23031771.
26.
Singh (C) et al., Potential of turmeric-derived compounds against RNA-dependent RNA polymerase of SARS-CoV-2: An in-silico approach, Computers in Biology and Medicine, doi:10.1016/j.compbiomed.2021.104965.
27.
Kandeil et al., Bioactive Polyphenolic Compounds Showing Strong Antiviral Activities against Severe Acute Respiratory Syndrome Coronavirus 2, Pathogens, doi:10.3390/pathogens10060758.
28.
Rajagopal et al., Activity of phytochemical constituents of Curcuma longa (turmeric) and Andrographis paniculata against coronavirus (COVID-19): an in silico approach, Future Journal of Pharmaceutical Sciences, doi:10.1186/s43094-020-00126-x.
29.
Suravajhala et al., Comparative Docking Studies on Curcumin with COVID-19 Proteins, Preprints, doi:10.20944/preprints202005.0439.v3.
30.
Sekiou et al., In-Silico Identification of Potent Inhibitors of COVID-19 Main Protease (Mpro) and Angiotensin Converting Enzyme 2 (ACE2) from Natural Products: Quercetin, Hispidulin, and Cirsimaritin Exhibited Better Potential Inhibition than Hydroxy-Chloroquine Against COVID-19 Main Protease Active Site and ACE2, ChemRxiv, doi:10.26434/chemrxiv.12181404.v1.
31.
Grüneberg et al., Dose-dependent antiviral effects of glycyrrhizin, curcumin, and harmaline against clinical SARS-CoV-2 isolates, including D614G, Omicron BA.5, and Omicron XBB.1, BMC Complementary Medicine and Therapies, doi:10.1186/s12906-026-05253-1.
32.
Aktay et al., Oral Administration of Water-Soluble Curcumin Complex Prevents ARDS With the Potential for COVID-19 Treatment, Phytotherapy Research, doi:10.1002/ptr.70046.
33.
Olubiyi et al., Novel dietary herbal preparations with inhibitory activities against multiple SARS-CoV-2 targets: A multidisciplinary investigation into antiviral activities, Food Chemistry Advances, doi:10.1016/j.focha.2025.100969.
34.
Emam et al., Establishment of in-house assay for screening of anti-SARS-CoV-2 protein inhibitors, AMB Express, doi:10.1186/s13568-024-01739-8.
35.
Van Tin et al., Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling, Cells, doi:10.3390/cells13161331.
36.
Li et al., Thermal shift assay (TSA)-based drug screening strategy for rapid discovery of inhibitors against the Nsp13 helicase of SARS-CoV-2, Animals and Zoonoses, doi:10.1016/j.azn.2024.06.001.
37.
Kamble et al., Nanoparticulate curcumin spray imparts prophylactic and therapeutic properties against SARS-CoV-2, Emergent Materials, doi:10.1007/s42247-024-00754-6.
38.
Nicoliche et al., Antiviral, anti-inflammatory and antioxidant effects of curcumin and curcuminoids in SH-SY5Y cells infected by SARS-CoV-2, Scientific Reports, doi:10.1038/s41598-024-61662-7.
39.
Nittayananta et al., A novel film spray containing curcumin inhibits SARS-CoV-2 and influenza virus infection and enhances mucosal immunity, Virology Journal, doi:10.1186/s12985-023-02282-x.
40.
Septisetyani et al., Curcumin and turmeric extract inhibited SARS-CoV-2 pseudovirus cell entry and Spike mediated cell fusion, bioRxiv, doi:10.1101/2023.09.28.560070.
41.
Mohd Abd Razak et al., In Vitro Anti-SARS-CoV-2 Activities of Curcumin and Selected Phenolic Compounds, Natural Product Communications, doi:10.1177/1934578X231188861.
42.
Fam et al., Channel activity of SARS-CoV-2 viroporin ORF3a inhibited by adamantanes and phenolic plant metabolites, Scientific Reports, doi:10.1038/s41598-023-31764-9.
43.
Teshima et al., Antiviral activity of curcumin and its analogs selected by an artificial intelligence-supported activity prediction system in SARS-CoV-2-infected VeroE6 cells, Natural Product Research, doi:10.1080/14786419.2023.2194647.
44.
Zupin et al., Optimization of Anti-SARS-CoV-2 Treatments Based on Curcumin, Used Alone or Employed as a Photosensitizer, Viruses, doi:10.3390/v14102132.
45.
Leka et al., In vitro antiviral activity against SARS-CoV-2 of common herbal medicinal extracts and their bioactive compounds, Phytotherapy Research, doi:10.1002/ptr.7463.
46.
Goc et al., Inhibitory effects of specific combination of natural compounds against SARS-CoV-2 and its Alpha, Beta, Gamma, Delta, Kappa, and Mu variants, European Journal of Microbiology and Immunology, doi:10.1556/1886.2021.00022.
47.
Marín-Palma et al., Curcumin Inhibits In Vitro SARS-CoV-2 Infection In Vero E6 Cells through Multiple Antiviral Mechanisms, Molecules, doi:10.3390/molecules26226900.
48.
Bahun et al., Inhibition of the SARS-CoV-2 3CLpro main protease by plant polyphenols, Food Chemistry, doi:10.1016/j.foodchem.2021.131594.
49.
Bormann et al., Turmeric Root and Its Bioactive Ingredient Curcumin Effectively Neutralize SARS-CoV-2 In Vitro, Viruses, doi:10.3390/v13101914.
50.
Guijarro-Real et al., Potential In Vitro Inhibition of Selected Plant Extracts against SARS-CoV-2 Chymotripsin-Like Protease (3CLPro) Activity, Foods, doi:10.3390/foods10071503.
a.
The trimeric spike (S) protein is a glycoprotein that mediates viral entry by binding to the host ACE2 receptor, is critical for SARS-CoV-2's ability to infect host cells, and is a target of neutralizing antibodies. Inhibition of the spike protein prevents viral attachment, halting infection at the earliest stage.
b.
The receptor binding domain is a specific region of the spike protein that binds ACE2 and is a major target of neutralizing antibodies. Focusing on the precise binding site allows highly specific disruption of viral attachment with reduced potential for off-target effects.
c.
The main protease or Mpro, also known as 3CLpro or nsp5, is a cysteine protease that cleaves viral polyproteins into functional units needed for replication. Inhibiting Mpro disrupts the SARS-CoV-2 lifecycle within the host cell, preventing the creation of new copies.
d.
RNA-dependent RNA polymerase (RdRp), also called nsp12, is the core enzyme of the viral replicase-transcriptase complex that copies the positive-sense viral RNA genome into negative-sense templates for progeny RNA synthesis. Inhibiting RdRp blocks viral genome replication and transcription.
e.
The papain-like protease (PLpro) has multiple functions including cleaving viral polyproteins and suppressing the host immune response by deubiquitination and deISGylation of host proteins. Inhibiting PLpro may block viral replication and help restore normal immune responses.
f.
The angiotensin converting enzyme 2 (ACE2) protein is a host cell transmembrane protein that serves as the cellular receptor for the SARS-CoV-2 spike protein. ACE2 is expressed on many cell types, including epithelial cells in the lungs, and allows the virus to enter and infect host cells. Inhibition may affect ACE2's physiological function in blood pressure control.
g.
The nucleocapsid (N) protein binds and encapsulates the viral genome by coating the viral RNA. N enables formation and release of infectious virions and plays additional roles in viral replication and pathogenesis. N is also an immunodominant antigen used in diagnostic assays.
h.
Non-structural protein 10 (nsp10) serves as an RNA chaperone and stabilizes conformations of nsp12 and nsp14 in the replicase-transcriptase complex, which synthesizes new viral RNAs. Nsp10 disruption may destabilize replicase-transcriptase complex activity.
i.
The helicase, or nsp13, protein unwinds the double-stranded viral RNA, a crucial step in replication and transcription. Inhibition may prevent viral genome replication and the creation of new virus components.
j.
The interaction between the SARS-CoV-2 spike protein and the human ACE2 receptor is a primary method of viral entry, inhibiting this interaction can prevent the virus from attaching to and entering host cells, halting infection at an early stage.
k.
Transmembrane protease serine 2 (TMPRSS2) is a host cell protease that primes the spike protein, facilitating cellular entry. TMPRSS2 activity helps enable cleavage of the spike protein required for membrane fusion and virus entry. Inhibition may especially protect respiratory epithelial cells, buy may have physiological effects.
l.
Calu-3 is a human lung adenocarcinoma cell line with moderate ACE2 and TMPRSS2 expression and SARS-CoV-2 susceptibility. It provides a model of the human respiratory epithelium, but many not be ideal for modeling early stages of infection due to the moderate expression levels of ACE2 and TMPRSS2.
m.
A549 is a human lung carcinoma cell line with low ACE2 expression and SARS-CoV-2 susceptibility. Viral entry/replication can be studied but the cells may not replicate all aspects of lung infection.
n.
A549-AT is a human lung carcinoma cell line stably transfected with ACE2 and TMPRSS2 receptors. Unlike the parental line, this overexpression ensures stable infection and enhanced viral entry, allowing for the evaluation of antiviral efficacy against various SARS-CoV-2 variants.
o.
293T is a human embryonic kidney cell line that can be engineered for high ACE2 expression and SARS-CoV-2 susceptibility. 293T cells are easily transfected and support high protein expression.
p.
HEK293-hACE2 is a human embryonic kidney cell line with high ACE2 expression and SARS-CoV-2 susceptibility. Cells have been transfected with a plasmid to express the human ACE2 (hACE2) protein.
q.
293T/hACE2/TMPRSS2 is a human embryonic kidney cell line engineered for high ACE2 and TMPRSS2 expression, which mimics key aspects of human infection. 293T/hACE2/TMPRSS2 cells are very susceptible to SARS-CoV-2 infection.
r.
Vero E6 is an African green monkey kidney cell line with low/no ACE2 expression and high SARS-CoV-2 susceptibility. The cell line is easy to maintain and supports robust viral replication, however the monkey origin may not accurately represent human responses.
s.
SH-SY5Y is a human neuroblastoma cell line that exhibits neuronal phenotypes. It is commonly used as an in vitro model for studying neurotoxicity, neurodegenerative diseases, and neuronal differentiation.
Nittayananta et al., 23 Jan 2024, peer-reviewed, 8 authors.
Contact: nwipawee@tu.ac.th.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
A novel film spray containing curcumin inhibits SARS-CoV-2 and influenza virus infection and enhances mucosal immunity
Virology Journal, doi:10.1186/s12985-023-02282-x
Background Infection by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and influenza virus is still a major worldwide health concern. Plants are a good source of bioactive compounds to be used as preventive measures for both inhibiting the virus binding and enhancing mucosal innate immunity. Curcumin has been shown to possess antiviral activity and modulate innate immunity. Therefore, the purpose of this study was to develop an oro-nasal film spray containing curcumin and determine its antiviral activity against SARS-CoV-2 and influenza virus infection, as well as its effects on mucosal innate immunity and inflammatory cytokines in vitro.
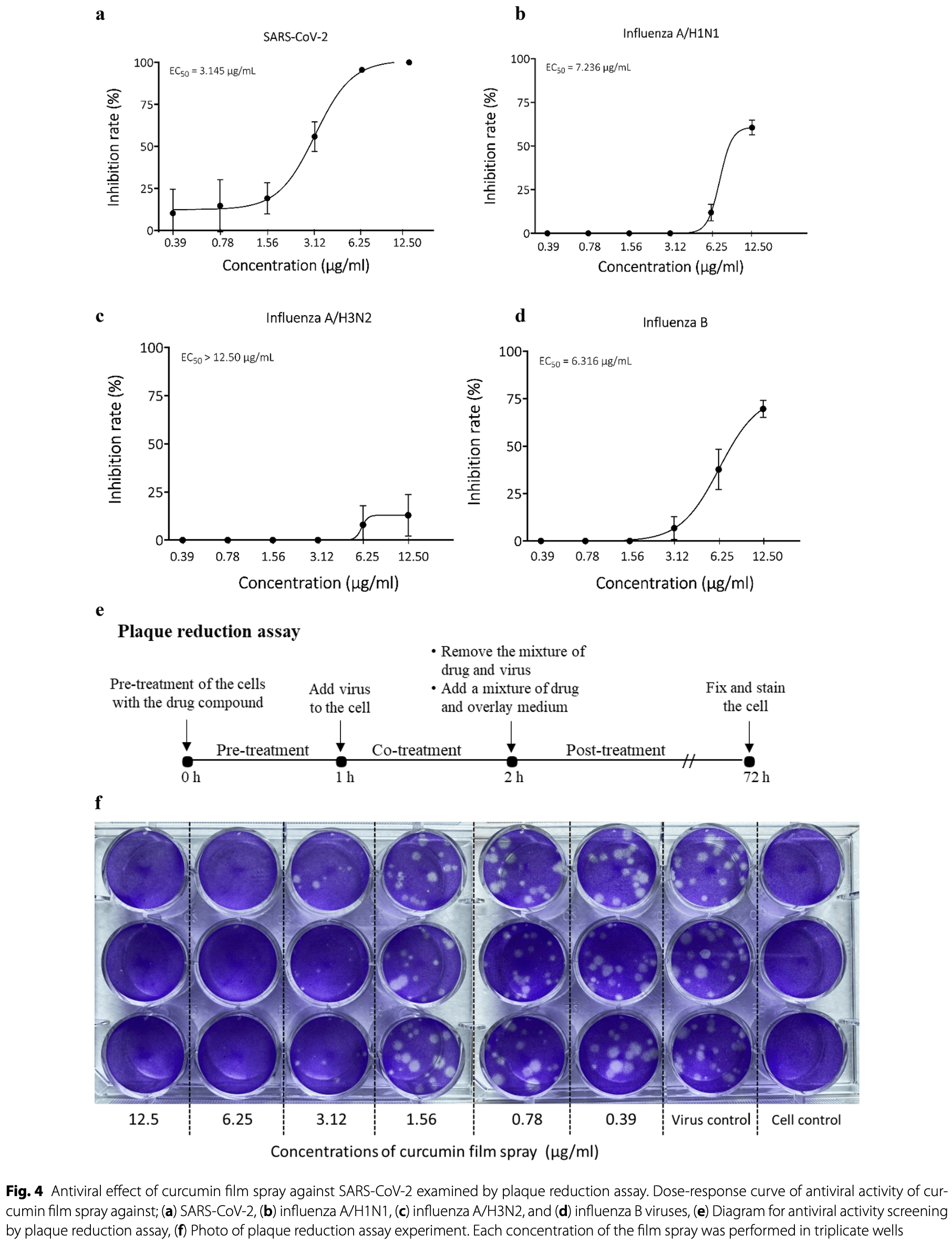
Methods The antiviral activity of the film spray against SARS-CoV-2, influenza A/H1N1, A/H3N2, and influenza B was assessed in vitro by plaque reduction assay. Cytotoxicity of the film spray to oral keratinocytes and nasal epithelial cells was assessed by MTT assay, and cytotoxicity to Vero and MDCK cells was assessed by an MTS-based cytotoxicity assay. Oral and nasal innate immune markers in response to the film spray were determined by ELISA and by a commercial Milliplex Map Kit, respectively.
Results Our data show that the film spray containing curcumin can inhibit both SARS-CoV-2 and influenza virus infections while maintaining cell viability. Results obtained among 4 viruses revealed that curcumin film spray demonstrated the highest inhibitory activity against SARS-CoV-2 with the lowest EC 50 of 3.15 µg/ml and the highest SI value of 4.62, followed by influenza B (EC 50 = 6.32 µg/ml, SI = 2.04), influenza A/H1N1 (EC 50 = 7.24 µg/ml, SI = 1.78), and influenza A/H3N2 (EC 50 > 12.5 µg/ml, SI < 1.03), respectively. Antimicrobial peptides LL-37 and HD-5, IL-6 and TNF-α produced by oral keratinocytes were significantly induced by the film spray, while hBD2 was significantly reduced.
Conclusion Film spray containing curcumin possesses multiple actions against SARS-CoV-2 infection by inhibiting ACE-2 binding in target cells and enhancing mucosal innate immunity. The film spray can also inhibit influenza virus infection. Therefore, the curcumin film spray may be effective in preventing the viral infection of both SARS-CoV-2 and influenza.
Author contributions W.N. designed the study and wrote the proposal, W.N., N.C., K.N., and J.K. applied for the research funding; W.N., H.L., N.C., A.P., T.S. interpreted data and drafted manuscript. H.L., N.C., A.P., T.S., K.N., J.P. performed the experiments. W.N., H.L., N.C., A.P., T.S., and K.N. participated in reviewing and editing the final manuscript. All authors have read and agreed to the published version of the manuscript.
Declarations Ethics approval and consent to participate Not applicable.
Consent for publication Not applicable.
Competing interests The authors declare no competing interests.
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Babaei, Nassiri-Asl, Hosseinzadeh, Curcumin (a constituent of turmeric): new treatment option against COVID-19, Food Sci Nutr, doi:10.1002/fsn3.1858
Barlow, Svoboda, Mackellar, Nash, York et al., Antiviral activity and increased host defense against Influenza Infection elicited by the human cathelicidin LL-37, PLoS ONE, doi:10.1371/journal.pone.0025333.]
Brice, Diamond, Activities of human host defense peptides, Curr Med Chem, doi:10.2174/0929867326666190805151654
Chai, Chen, Lin, Xie, Wang et al., Curcumin regulates the differentiation of naïve CD4 + T cells and activates IL-10 immune modulation against acute lung injury in mice, Biomed Pharmacother, doi:10.1016/j.biopha.2020.109946
Chen, Chen, Wen, Ou, Chiou et al., Inhibition of enveloped viruses infectivity by curcumin, PLoS ONE
Dai, Gu, Su, Wang, Zhao et al., Inhibition of curcumin on Influenza a virus Infection and influenzal Pneumonia via oxidative stress, TLR2/4, p38/JNK MAPK and NF-Κb pathways, Int Immunopharmacol, doi:10.1016/j.intimp.2017.11.009
Diamond, Molchanova, Herlan, Fortkort, Lin et al., Potent antiviral activity against HSV-1 and SARS-CoV-2 by antimicrobial peptoids, Pharmaceuticals, doi:10.3390/ph14040304
Doss, White, Tecle, Gantz, Crouch et al., Interactions of alpha-, beta-, and theta-defensins with Influenza a virus and surfactant protein D, J Immunol, doi:10.4049/jimmunol.0804049
Ferguson, Abbott, Garg, Anti-inflammatory effects of oral supplementation with curcumin: a systematic review and meta-analysis of randomized controlled trials, Nutr Rev, doi:10.1093/nutrit/nuaa114
Fu, Ho, Kang, Tsai, Wu et al., Pharmaceutical prospects of curcuminoids for the remedy of COVID-19: truth or myth, Front Pharmacol, doi:10.3389/fphar.2022.863082
Ghildiyal, Prakash, Chaudhary, Gupta, Gabrani, Phytochemicals as antiviral agents: recent updates, Plant-derived Bioactives, doi:10.1007/978-981-15-1761-7_12
Hasanoglu, Korukluoglu, Asilturk, Cosgun, Kalem et al., Higher viral loads in asymptomatic COVID-19 patients might be the invisible part of the iceberg, Infection
Jena, Kanungo, Nayak, Chainy, Dandapat, Catechin and curcumin interact with S protein of SARS-CoV2 and ACE2 of human cell membrane: insights from computational studies, Sci Rep
Jiang, Wang, Kuang, Wang, Li et al., Expression of mouse beta-defensin-3 in mdck cells and its anti-influenza-virus activity, Arch Virol, doi:10.1007/s00705-009-0352-6
Jiaranaikulwanitch, Yooin, Chutiwitoonchai, Thitikornpong, Sritularak et al., Discovery of natural lead compound from Dendrobium sp. against SARS-CoV-2 Infection, Pharmaceuticals, doi:10.3390/ph15050620
Junqueira, Crespo, Ranjbar, Lewandrowski, Ingber et al., SARS-CoV-2 infects blood monocytes to activate NLRP3 and AIM2 inflammasomes, pyroptosis and cytokine release, Res Sq Rs, doi:10.21203/rs.3.rs-153628/v1
Kandeel, Al-Nazawi, Virtual screening and repurposing of FDA approved Drugs against COVID-19 main protease, Life Sci
Kim, Choi, Kim, Kang, Kim, Elucidating the effects of curcumin against Influenza using in silico and in vitro approaches, Pharmaceuticals, doi:10.3390/ph14090880
Koonpaew, Kaewborisuth, Srisutthisamphan, Wanitchang, Thaweerattanasinp et al., A singlecycle influenza A virus-based SARS-CoV-2 vaccine elicits potent immune responses in a mouse model, Vaccines
Kunnumakkara, Rana, Parama, Banik, Girisa et al., COVID-19, cytokines, inflammation, and spices: how are they related?, Life Sci, doi:10.1016/j.lfs.2021.119201
Lai, Yan, Liao, Li, Ye et al., 3D-quantitative structureactivity relationship and antiviral effects of curcumin derivatives as potent inhibitors of Influenza H1N1 neuraminidase, Arch Pharmacal Res, doi:10.1007/s12272-020-01230-5
Lansbury, Lim, Baskaran, Lim, Co-infections in people with COVID-19: a systematic review and meta-analysis, J Infect
Li, Xie, He, Fan, Baril et al., Long-term persistence of robust antibody and cytotoxic T cell responses in recovered patients infected with SARS coronavirus, PLoS ONE
Marín-Palma, Tabares-Guevara, Zapata-Cardona, Flórez-Álvarez, Yepes et al., Curcumin inhibits in vitro SARS-CoV-2 Infection in Vero E6 cells through multiple antiviral mechanisms, Molecules, doi:10.3390/molecules26226900
Newman, Cragg, Natural products as sources of new Drugs from 1981 to 2014, J Nat Prod
Nittayananta, Limsuwan, Srichana, Sae-Wong, Amnuaikit, Oral spray containing plant-derived compounds is effective against common oral pathogens, Arch Oral Biol, doi:10.1016/j.archoralbio.2018.03.002
Nypaver, Dehlinger, Carter, Influenza and Influenza vaccine: a review, J Midwifery Womens Health, doi:10.1111/jmwh.13203
Oh, Shin, SARS-CoV-2 nucleocapsid protein targets RIG-I-like receptor pathways to inhibit the induction of interferon response, Cells, doi:10.3390/cells10030530
Promsong, Chung, Satthakarn, Nittayananta, Ellagic acid modulates the expression of oral innate immune mediators: potential role in mucosal protection, J Oral Pathol Med, doi:10.1111/jop.12223
Rattis, Ramos, Celes, Curcumin as a potential treatment for COVID-19, Front. Pharmacol, doi:10.3389/fphar.2021.675287
Roth, Lütke, Meinberger, Hermes, Sengle et al., LL-37 fights SARS-CoV-2: the vitamin D-inducible peptide LL-37 inhibits binding of SARS-CoV-2 spike protein to its cellular receptor angiotensin converting enzyme 2 in vitro, bioRxiv
Ryan, Dai, Yin, Megjugorac, Uhlhorn et al., Modulation of human beta-defensin-1 (hBD-1) in plasmacytoid dendritic cells (PDC), monocytes, and epithelial cells by Influenza virus, herpes simplex virus, and Sendai virus and its possible role in innate immunity, J Leukoc Biol, doi:10.1189/jlb.0209079
Shi, Huang, Chen, Pi, Hsu et al., Andrographolide and its fluorescent derivative inhibit the main proteases of 2019-nCoV and SARS-CoV through covalent linkage, Biochem Biophys Res Commun, doi:10.1016/j.bbrc.2020.08.086
Skyvalidas, Mavropoulos, Tsiogkas, Dardiotis, Liaskos et al., Curcumin mediates attenuation of pro-inflammatory interferon γ and interleukin 17 cytokine responses in psoriatic Disease, strengthening its role as a dietary immunosuppressant, Nutr Res, doi:10.1016/j.nutres.2020.01.005
Sungsuwan, Jongkaewwattana, Jaru-Ampornpan, Nucleocapsid proteins from other swine enteric coronaviruses differentially modulate PEDV replication, Virol
Tripathi, Wang, White, Rynkiewicz, Seaton et al., Identifying the critical domain of LL-37 involved in mediating neutrophil activation in the presence of Influenza virus: functional and structural analysis, PLoS ONE, doi:10.1371/journal.pone.0133454
Velazquez-Salinas, Verdugo-Rodriguez, Rodriguez, Borca, The role of interleukin 6 during viral Infections, Front Microbiol, doi:10.3389/fmicb.2019.01057
Wang, Wang, Li, Chen, Han et al., Human cathelicidin inhibits SARS-CoV-2 Infection: killing two birds with one stone, ACS infect Dis, doi:10.1021/acsinfecdis.1c00096
Wang, Wang, Li, Wei, Zhao et al., Human intestinal defensin 5 inhibits SARS-CoV-2 invasion by cloaking ACE2, Gastroenterology
Xu, Liu, Curcumin alleviates macrophage activation and lung inflammation induced by Influenza virus Infection through inhibiting the NF-κB signaling pathway, Influenza Other Respir Viruses, doi:10.1111/irv.12459
Yuan, Jiao, Qu, Yang, Liu, The development of COVID-19 treatment, Front Immunol, doi:10.3389/fimmu.2023.1125246
Yue, Zhang, Xing, The epidemiology and clinical characteristics of co-infection of SARS-CoV-2 and Influenza viruses in patients during COVID-19 outbreak, J Med Virol
Zhang, Ghosh, Basavarajappa, Chen, Shrestha et al., HBD-2 binds SARS-CoV-2 RBD and blocks viral entry: strategy to combat COVID-19, iScience, doi:10.1016/j.isci.2022.103856
DOI record:
{
"DOI": "10.1186/s12985-023-02282-x",
"ISSN": [
"1743-422X"
],
"URL": "http://dx.doi.org/10.1186/s12985-023-02282-x",
"abstract": "<jats:title>Abstract</jats:title><jats:sec>\n <jats:title>Background</jats:title>\n <jats:p>Infection by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) and influenza virus is still a major worldwide health concern. Plants are a good source of bioactive compounds to be used as preventive measures for both inhibiting the virus binding and enhancing mucosal innate immunity. Curcumin has been shown to possess antiviral activity and modulate innate immunity. Therefore, the purpose of this study was to develop an oro-nasal film spray containing curcumin and determine its antiviral activity against SARS-CoV-2 and influenza virus infection, as well as its effects on mucosal innate immunity and inflammatory cytokines in vitro.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Methods</jats:title>\n <jats:p>The antiviral activity of the film spray against SARS-CoV-2, influenza A/H1N1, A/H3N2, and influenza B was assessed in vitro by plaque reduction assay. Cytotoxicity of the film spray to oral keratinocytes and nasal epithelial cells was assessed by MTT assay, and cytotoxicity to Vero and MDCK cells was assessed by an MTS-based cytotoxicity assay. Oral and nasal innate immune markers in response to the film spray were determined by ELISA and by a commercial Milliplex Map Kit, respectively.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Results</jats:title>\n <jats:p>Our data show that the film spray containing curcumin can inhibit both SARS-CoV-2 and influenza virus infections while maintaining cell viability. Results obtained among 4 viruses revealed that curcumin film spray demonstrated the highest inhibitory activity against SARS-CoV-2 with the lowest EC<jats:sub>50</jats:sub> of 3.15 µg/ml and the highest SI value of 4.62, followed by influenza B (EC<jats:sub>50</jats:sub> = 6.32 µg/ml, SI = 2.04), influenza A/H1N1 (EC<jats:sub>50</jats:sub> = 7.24 µg/ml, SI = 1.78), and influenza A/H3N2 (EC<jats:sub>50</jats:sub> > 12.5 µg/ml, SI < 1.03), respectively. Antimicrobial peptides LL-37 and HD-5, IL-6 and TNF-α produced by oral keratinocytes were significantly induced by the film spray, while hBD2 was significantly reduced.</jats:p>\n </jats:sec><jats:sec>\n <jats:title>Conclusion</jats:title>\n <jats:p>Film spray containing curcumin possesses multiple actions against SARS-CoV-2 infection by inhibiting ACE-2 binding in target cells and enhancing mucosal innate immunity. The film spray can also inhibit influenza virus infection. Therefore, the curcumin film spray may be effective in preventing the viral infection of both SARS-CoV-2 and influenza.</jats:p>\n </jats:sec>",
"alternative-id": [
"2282"
],
"article-number": "26",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "1 November 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "29 December 2023"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "23 January 2024"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "Not applicable."
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Not applicable."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "The authors declare no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Nittayananta",
"given": "Wipawee",
"sequence": "first"
},
{
"affiliation": [],
"family": "Lerdsamran",
"given": "Hatairat",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chutiwitoonchai",
"given": "Nopporn",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Promsong",
"given": "Aornrutai",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Srichana",
"given": "Teerapol",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Netsomboon",
"given": "Kesinee",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Prasertsopon",
"given": "Jarunee",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kerdto",
"given": "Jaruta",
"sequence": "additional"
}
],
"container-title": "Virology Journal",
"container-title-short": "Virol J",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2024,
1,
23
]
],
"date-time": "2024-01-23T14:02:29Z",
"timestamp": 1706018549000
},
"deposited": {
"date-parts": [
[
2024,
1,
23
]
],
"date-time": "2024-01-23T14:05:36Z",
"timestamp": 1706018736000
},
"funder": [
{
"award": [
"CoV-19/2564.2"
],
"name": "Thammasat Hospital"
}
],
"indexed": {
"date-parts": [
[
2024,
1,
24
]
],
"date-time": "2024-01-24T00:36:48Z",
"timestamp": 1706056608281
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
1,
23
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
23
]
],
"date-time": "2024-01-23T00:00:00Z",
"timestamp": 1705968000000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
1,
23
]
],
"date-time": "2024-01-23T00:00:00Z",
"timestamp": 1705968000000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12985-023-02282-x.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s12985-023-02282-x/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s12985-023-02282-x.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2024,
1,
23
]
]
},
"published-online": {
"date-parts": [
[
2024,
1,
23
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.3389/fphar.2022.863082",
"author": "YS Fu",
"doi-asserted-by": "publisher",
"first-page": "863082",
"journal-title": "Front Pharmacol",
"key": "2282_CR1",
"unstructured": "Fu YS, Ho WY, Kang N, Tsai MJ, Wu J, Huang L, Weng CF. Pharmaceutical prospects of curcuminoids for the remedy of COVID-19: truth or myth. Front Pharmacol. 2022;13:863082. https://doi.org/10.3389/fphar.2022.863082.",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1111/jmwh.13203",
"author": "C Nypaver",
"doi-asserted-by": "publisher",
"first-page": "45",
"issue": "1",
"journal-title": "J Midwifery Womens Health",
"key": "2282_CR2",
"unstructured": "Nypaver C, Dehlinger C, Carter C. Influenza and Influenza vaccine: a review. J Midwifery Womens Health. 2021;66(1):45–53. https://doi.org/10.1111/jmwh.13203.",
"volume": "66",
"year": "2021"
},
{
"DOI": "10.1016/j.bbrc.2020.08.086",
"doi-asserted-by": "publisher",
"key": "2282_CR3",
"unstructured": "Shi TH, Huang YL, Chen CC, Pi WC, Hsu YL, Lo LC, Chen WY, Fu SL, Lin CH. Andrographolide and its fluorescent derivative inhibit the main proteases of 2019-nCoV and SARS-CoV through covalent linkage. Biochem Biophys Res Commun 2020 Dec 10; 533(3):467–73. https://doi.org/10.1016/j.bbrc.2020.08.086."
},
{
"DOI": "10.3390/cells10030530",
"author": "SJ Oh",
"doi-asserted-by": "publisher",
"first-page": "530",
"issue": "3",
"journal-title": "Cells",
"key": "2282_CR4",
"unstructured": "Oh SJ, Shin OS. SARS-CoV-2 nucleocapsid protein targets RIG-I-like receptor pathways to inhibit the induction of interferon response. Cells. 2021;10(3):530. https://doi.org/10.3390/cells10030530.",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.21203/rs.3.rs-153628/v1",
"author": "C Junqueira",
"doi-asserted-by": "publisher",
"first-page": "rs",
"journal-title": "Res Sq Rs",
"key": "2282_CR5",
"unstructured": "Junqueira C, Crespo Â, Ranjbar S, Lewandrowski M, Ingber J, de Lacerda LB, et al. SARS-CoV-2 infects blood monocytes to activate NLRP3 and AIM2 inflammasomes, pyroptosis and cytokine release. Res Sq Rs. 2021;3:rs–153628. https://doi.org/10.21203/rs.3.rs-153628/v1.",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1016/j.lfs.2021.119201",
"author": "AB Kunnumakkara",
"doi-asserted-by": "publisher",
"first-page": "119201",
"journal-title": "Life Sci",
"key": "2282_CR6",
"unstructured": "Kunnumakkara AB, Rana V, Parama D, Banik K, Girisa S, Henamayee S, et al. COVID-19, cytokines, inflammation, and spices: how are they related? Life Sci. 2021;284:119201. https://doi.org/10.1016/j.lfs.2021.119201.",
"volume": "284",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2023.1125246",
"author": "Y Yuan",
"doi-asserted-by": "publisher",
"first-page": "1125246",
"journal-title": "Front Immunol",
"key": "2282_CR7",
"unstructured": "Yuan Y, Jiao B, Qu L, Yang D, Liu R. The development of COVID-19 treatment. Front Immunol. 2023;14:1125246. https://doi.org/10.3389/fimmu.2023.1125246.",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1007/978-981-15-1761-7_12",
"doi-asserted-by": "publisher",
"key": "2282_CR8",
"unstructured": "Ghildiyal R, Prakash V, Chaudhary VK, Gupta V, Gabrani R. Phytochemicals as antiviral agents: recent updates. Plant-derived Bioactives.2020 May 12:279–95.https://doi.org/10.1007/978-981-15-1761-7_12."
},
{
"DOI": "10.1016/j.jinf.2020.05.046",
"author": "L Lansbury",
"doi-asserted-by": "publisher",
"first-page": "266",
"issue": "2",
"journal-title": "J Infect",
"key": "2282_CR9",
"unstructured": "Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta‐analysis. J Infect. 2020;81(2):266–75.",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26163",
"author": "H Yue",
"doi-asserted-by": "publisher",
"first-page": "2870",
"issue": "11",
"journal-title": "J Med Virol",
"key": "2282_CR10",
"unstructured": "Yue H, Zhang M, Xing L, et al. The epidemiology and clinical characteristics of co-infection of SARS-CoV-2 and Influenza viruses in patients during COVID-19 outbreak. J Med Virol. 2020;92(11):2870–3.",
"volume": "92",
"year": "2020"
},
{
"DOI": "10.1021/acs.jnatprod.5b01055",
"author": "DJ Newman",
"doi-asserted-by": "publisher",
"first-page": "629",
"issue": "3",
"journal-title": "J Nat Prod",
"key": "2282_CR11",
"unstructured": "Newman DJ, Cragg GM. Natural products as sources of new Drugs from 1981 to 2014. J Nat Prod. 2016;79(3):629–61.",
"volume": "79",
"year": "2016"
},
{
"DOI": "10.3390/molecules26226900",
"author": "D Marín-Palma",
"doi-asserted-by": "publisher",
"first-page": "6900",
"journal-title": "Molecules",
"key": "2282_CR12",
"unstructured": "Marín-Palma D, Tabares-Guevara JH, Zapata-Cardona MI, Flórez-Álvarez L, Yepes LM, Rugeles MT, Zapata-Builes W, Hernandez JC, Taborda NA. Curcumin inhibits in vitro SARS-CoV-2 Infection in Vero E6 cells through multiple antiviral mechanisms. Molecules. 2021;26:6900.https://doi.org/10.3390/molecules26226900",
"volume": "26",
"year": "2021"
},
{
"DOI": "10.3390/ph14090880",
"author": "M Kim",
"doi-asserted-by": "publisher",
"first-page": "880",
"issue": "9",
"journal-title": "Pharmaceuticals (Basel)",
"key": "2282_CR13",
"unstructured": "Kim M, Choi H, Kim S, Kang LW, Kim YB. Elucidating the effects of curcumin against Influenza using in silico and in vitro approaches. Pharmaceuticals (Basel). 2021;14(9):880. https://doi.org/10.3390/ph14090880.",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1371/journal.pone.0062482",
"author": "TY Chen",
"doi-asserted-by": "publisher",
"first-page": "e62482",
"journal-title": "PLoS ONE",
"key": "2282_CR14",
"unstructured": "Chen TY, Chen DY, Wen HW, Ou JL, Chiou SS, Chen JM, Wong ML, Hsu WL. Inhibition of enveloped viruses infectivity by curcumin. PLoS ONE. 2013;8:e62482.",
"volume": "8",
"year": "2013"
},
{
"DOI": "10.1038/s41598-021-81462-7",
"author": "AB Jena",
"doi-asserted-by": "publisher",
"first-page": "2043",
"journal-title": "Sci Rep",
"key": "2282_CR15",
"unstructured": "Jena AB, Kanungo N, Nayak V, Chainy GBN, Dandapat J. Catechin and curcumin interact with S protein of SARS-CoV2 and ACE2 of human cell membrane: insights from computational studies. Sci Rep. 2021;11:2043.",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.lfs.2020.117627",
"author": "M Kandeel",
"doi-asserted-by": "publisher",
"first-page": "117627",
"journal-title": "Life Sci",
"key": "2282_CR16",
"unstructured": "Kandeel M, Al-Nazawi M. Virtual screening and repurposing of FDA approved Drugs against COVID-19 main protease. Life Sci. 2020;251:117627.",
"volume": "251",
"year": "2020"
},
{
"DOI": "10.2174/0929867326666190805151654",
"author": "DC Brice",
"doi-asserted-by": "publisher",
"first-page": "1420",
"issue": "9",
"journal-title": "Curr Med Chem",
"key": "2282_CR17",
"unstructured": "Brice DC, Diamond G. Activities of human host defense peptides. Curr Med Chem. 2020;27(9):1420–43. https://doi.org/10.2174/0929867326666190805151654.",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1053/j.gastro.2020.05.015",
"author": "C Wang",
"doi-asserted-by": "publisher",
"first-page": "1145",
"issue": "3",
"journal-title": "Gastroenterology",
"key": "2282_CR18",
"unstructured": "Wang C, Wang S, Li D, Wei DQ, Zhao J, Wang J. Human intestinal defensin 5 inhibits SARS-CoV-2 invasion by cloaking ACE2. Gastroenterology. Sep; 2020;159(3):1145–7.",
"volume": "159",
"year": "2020"
},
{
"DOI": "10.1021/acsinfecdis.1c00096",
"doi-asserted-by": "publisher",
"key": "2282_CR19",
"unstructured": "Wang C, Wang S, Li D, Chen P, Han S, Zhao G, Chen Y, Zhao J, Xiong J, Qiu J et al. Human cathelicidin inhibits SARS-CoV-2 Infection: killing two birds with one stone. ACS infect Dis.2021, Jun 11;7(6):1545–54. https://doi.org/10.1021/acsinfecdis.1c00096."
},
{
"DOI": "10.1007/s15010-020-01548-8",
"author": "I Hasanoglu",
"doi-asserted-by": "publisher",
"first-page": "117",
"journal-title": "Infection",
"key": "2282_CR20",
"unstructured": "Hasanoglu I, Korukluoglu G, Asilturk D, Cosgun Y, Kalem AK, Altas AB, Bircan Kayaaslan B, Eser F, Kuzucu EA, Guner R. Higher viral loads in asymptomatic COVID-19 patients might be the invisible part of the iceberg. Infection. 2021;49:117–26.",
"volume": "49",
"year": "2021"
},
{
"DOI": "10.1016/j.archoralbio.2018.03.002",
"author": "W Nittayananta",
"doi-asserted-by": "publisher",
"first-page": "80",
"journal-title": "Arch Oral Biol",
"key": "2282_CR21",
"unstructured": "Nittayananta W, Limsuwan S, Srichana T, Sae-Wong C, Amnuaikit T. Oral spray containing plant-derived compounds is effective against common oral pathogens. Arch Oral Biol. 2018;90:80–5. https://doi.org/10.1016/j.archoralbio.2018.03.002.",
"volume": "90",
"year": "2018"
},
{
"DOI": "10.1016/j.virol.2019.11.007",
"doi-asserted-by": "crossref",
"key": "2282_CR22",
"unstructured": "Sungsuwan S, Jongkaewwattana A, Jaru-Ampornpan P. Nucleocapsid proteins from other swine enteric coronaviruses differentially modulate PEDV replication. Virol 2020 Jan 15;540:45–56."
},
{
"DOI": "10.3390/vaccines9080850",
"doi-asserted-by": "crossref",
"key": "2282_CR23",
"unstructured": "Koonpaew S, Kaewborisuth C, Srisutthisamphan K, Wanitchang A, Thaweerattanasinp T, Saenboonrueng J, Poonsuk S, Viriyakitkosol R, Kramyu J. A single-cycle influenza A virus-based SARS-CoV-2 vaccine elicits potent immune responses in a mouse model. Vaccines (Basel). 2021, Aug 3;9(8):850."
},
{
"DOI": "10.3390/ph15050620",
"author": "J Jiaranaikulwanitch",
"doi-asserted-by": "publisher",
"first-page": "620",
"issue": "5",
"journal-title": "Pharmaceuticals (Basel)",
"key": "2282_CR24",
"unstructured": "Jiaranaikulwanitch J, Yooin W, Chutiwitoonchai W, Thitikornpong W, Sritularak B, Rojsitthisak P, Vajragupta O. Discovery of natural lead compound from Dendrobium sp. against SARS-CoV-2 Infection. Pharmaceuticals (Basel). May; 2022;15(5):620. https://doi.org/10.3390/ph15050620",
"volume": "15",
"year": "2022"
},
{
"DOI": "10.1111/jop.12223",
"author": "A Promsong",
"doi-asserted-by": "publisher",
"first-page": "214",
"journal-title": "J Oral Pathol Med",
"key": "2282_CR25",
"unstructured": "Promsong A, Chung WO, Satthakarn S, Nittayananta W. Ellagic acid modulates the expression of oral innate immune mediators: potential role in mucosal protection. J Oral Pathol Med. 2015;44:214–21. https://doi.org/10.1111/jop.12223.",
"volume": "44",
"year": "2015"
},
{
"DOI": "10.1002/fsn3.1858",
"author": "F Babaei",
"doi-asserted-by": "publisher",
"first-page": "5215",
"issue": "10",
"journal-title": "Food Sci Nutr",
"key": "2282_CR26",
"unstructured": "Babaei F, Nassiri-Asl M, Hosseinzadeh H. Curcumin (a constituent of turmeric): new treatment option against COVID-19. Food Sci Nutr. 2020;8(10):5215–27. https://doi.org/10.1002/fsn3.1858.",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.3389/fphar.2021.675287",
"author": "BAC Rattis",
"doi-asserted-by": "publisher",
"first-page": "675287",
"journal-title": "Pharmacol",
"key": "2282_CR27",
"unstructured": "Rattis BAC, Ramos SG, Celes MRN. Curcumin as a potential treatment for COVID-19. Front. Pharmacol. 2021;12:675287. https://doi.org/10.3389/fphar.2021.675287.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1111/irv.12459",
"author": "Y Xu",
"doi-asserted-by": "publisher",
"first-page": "457",
"issue": "5",
"journal-title": "Influenza Other Respir Viruses",
"key": "2282_CR28",
"unstructured": "Xu Y, Liu L. Curcumin alleviates macrophage activation and lung inflammation induced by Influenza virus Infection through inhibiting the NF-κB signaling pathway. Influenza Other Respir Viruses. 2017;11(5):457–63. https://doi.org/10.1111/irv.12459",
"volume": "11",
"year": "2017"
},
{
"DOI": "10.1016/j.intimp.2017.11.009",
"author": "J Dai",
"doi-asserted-by": "publisher",
"first-page": "177",
"journal-title": "Int Immunopharmacol",
"key": "2282_CR29",
"unstructured": "Dai J, Gu L, Su Y, Wang Q, Zhao Y, Chen X, et al. Inhibition of curcumin on Influenza a virus Infection and influenzal Pneumonia via oxidative stress, TLR2/4, p38/JNK MAPK and NF-Κb pathways. Int Immunopharmacol. 2018;54:177–87. https://doi.org/10.1016/j.intimp.2017.11.009",
"volume": "54",
"year": "2018"
},
{
"DOI": "10.1007/s12272-020-01230-5",
"author": "Y Lai",
"doi-asserted-by": "publisher",
"first-page": "489",
"journal-title": "Arch Pharmacal Res",
"key": "2282_CR30",
"unstructured": "Lai Y, Yan Y, Liao S, Li Y, Ye Y, Liu N, Zhao F, Xu P. 3D-quantitative structure-activity relationship and antiviral effects of curcumin derivatives as potent inhibitors of Influenza H1N1 neuraminidase. Arch Pharmacal Res. 2020;43:489–502. https://doi.org/10.1007/s12272-020-01230-5",
"volume": "43",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0000024",
"author": "T Li",
"doi-asserted-by": "publisher",
"first-page": "e24",
"issue": "1",
"journal-title": "PLoS ONE",
"key": "2282_CR31",
"unstructured": "Li T, Xie J, He Y, Fan H, Baril L, Qiu Z, Zuo Y. Long-term persistence of robust antibody and cytotoxic T cell responses in recovered patients infected with SARS coronavirus. PLoS ONE. 2006;1(1):e24.",
"volume": "1",
"year": "2006"
},
{
"DOI": "10.3390/ph14040304",
"author": "G Diamond",
"doi-asserted-by": "publisher",
"journal-title": "Pharmaceuticals (Basel)",
"key": "2282_CR32",
"unstructured": "Diamond G, Molchanova N, Herlan C, Fortkort JA, Lin JS, Figgins E, Bopp N, Ryan LK, Chung D, Adcock RS, et al. Potent antiviral activity against HSV-1 and SARS-CoV-2 by antimicrobial peptoids. Pharmaceuticals (Basel). 2021. https://doi.org/10.3390/ph14040304.",
"year": "2021"
},
{
"DOI": "10.1101/2020.12.02.408153",
"doi-asserted-by": "crossref",
"key": "2282_CR33",
"unstructured": "Roth A, Lütke S, Meinberger D, Hermes G, Sengle G, Koch M, Streichert T, Klatt AR. LL-37 fights SARS-CoV-2: the vitamin D-inducible peptide LL-37 inhibits binding of SARS-CoV-2 spike protein to its cellular receptor angiotensin converting enzyme 2 in vitro. bioRxiv. 2020;210.1101/2020.12.02.408153."
},
{
"DOI": "10.1371/journal.pone.0133454",
"author": "S Tripathi",
"doi-asserted-by": "publisher",
"first-page": "e0133454",
"issue": "8",
"journal-title": "PLoS ONE",
"key": "2282_CR34",
"unstructured": "Tripathi S, Wang G, White M, Rynkiewicz M, Seaton B, Hartshorn K. Identifying the critical domain of LL-37 involved in mediating neutrophil activation in the presence of Influenza virus: functional and structural analysis. PLoS ONE. 2015;10(8):e0133454.PMID: 26308522; PMCID: PMC4550355. https://doi.org/10.1371/journal.pone.0133454",
"volume": "10",
"year": "2015"
},
{
"DOI": "10.1371/journal.pone.0025333.]",
"author": "PG Barlow",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "PLoS ONE",
"key": "2282_CR35",
"unstructured": "Barlow PG, Svoboda P, Mackellar A, Nash AA, York IA, Pohl J, Davidson DJ, Donis RO. Antiviral activity and increased host defense against Influenza Infection elicited by the human cathelicidin LL-37. PLoS ONE. 2011;6:53. https://doi.org/10.1371/journal.pone.0025333.]",
"volume": "6",
"year": "2011"
},
{
"DOI": "10.4049/jimmunol.0804049",
"author": "M Doss",
"doi-asserted-by": "publisher",
"first-page": "7878",
"journal-title": "J Immunol",
"key": "2282_CR36",
"unstructured": "Doss M, White MR, Tecle T, Gantz D, Crouch EC, Jung G, Ruchala P, Waring AJ, Lehrer RI, Hartshorn KL. Interactions of alpha-, beta-, and theta-defensins with Influenza a virus and surfactant protein D. J Immunol. 2009;182:7878–87. https://doi.org/10.4049/jimmunol.0804049",
"volume": "182",
"year": "2009"
},
{
"DOI": "10.1007/s00705-009-0352-6",
"author": "Y Jiang",
"doi-asserted-by": "publisher",
"first-page": "639",
"journal-title": "Arch Virol",
"key": "2282_CR37",
"unstructured": "Jiang Y, Wang Y, Kuang Y, Wang B, Li W, Gong T, Jiang Z, Yang D, Li M. Expression of mouse beta-defensin-3 in mdck cells and its anti-influenza-virus activity. Arch Virol. 2009;154:639–47. https://doi.org/10.1007/s00705-009-0352-6.",
"volume": "154",
"year": "2009"
},
{
"DOI": "10.1189/jlb.0209079",
"author": "LK Ryan",
"doi-asserted-by": "publisher",
"first-page": "343",
"journal-title": "J Leukoc Biol",
"key": "2282_CR38",
"unstructured": "Ryan LK, Dai J, Yin Z, Megjugorac N, Uhlhorn V, Yim S, Schwartz KD, Abrahams JM, Diamond G, Fitzgerald-Bocarsly P. Modulation of human beta-defensin-1 (hBD-1) in plasmacytoid dendritic cells (PDC), monocytes, and epithelial cells by Influenza virus, herpes simplex virus, and Sendai virus and its possible role in innate immunity. J Leukoc Biol. 2011;90:343–56. https://doi.org/10.1189/jlb.0209079",
"volume": "90",
"year": "2011"
},
{
"DOI": "10.1016/j.isci.2022.103856",
"doi-asserted-by": "publisher",
"key": "2282_CR39",
"unstructured": "Zhang L, Ghosh SK, Basavarajappa SC, Chen Y, Shrestha P, Penfield J, Ramakrishnan P, Buck M, Weinberg A. HBD-2 binds SARS-CoV-2 RBD and blocks viral entry: strategy to combat COVID-19. iScience. 2022, 18Mar 18;25(3):103856. https://doi.org/10.1016/j.isci.2022.103856."
},
{
"DOI": "10.3389/fmicb.2019.01057",
"author": "L Velazquez-Salinas",
"doi-asserted-by": "publisher",
"first-page": "1057",
"journal-title": "Front Microbiol",
"key": "2282_CR40",
"unstructured": "Velazquez-Salinas L, Verdugo-Rodriguez A, Rodriguez LL, Borca MV. The role of interleukin 6 during viral Infections. Front Microbiol. 2019;10:1057. PMID: 31134045; PMCID: PMC6524401. https://doi.org/10.3389/fmicb.2019.01057",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1093/nutrit/nuaa114",
"author": "JJA Ferguson",
"doi-asserted-by": "publisher",
"first-page": "1043",
"issue": "9",
"journal-title": "Nutr Rev",
"key": "2282_CR41",
"unstructured": "Ferguson JJA, Abbott KA, Garg ML. Anti-inflammatory effects of oral supplementation with curcumin: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2021;79(9):1043–66. https://doi.org/10.1093/nutrit/nuaa114.",
"volume": "79",
"year": "2021"
},
{
"DOI": "10.1016/j.nutres.2020.01.005",
"author": "DΝ Skyvalidas",
"doi-asserted-by": "publisher",
"first-page": "95",
"journal-title": "Nutr Res",
"key": "2282_CR42",
"unstructured": "Skyvalidas DΝ, Mavropoulos A, Tsiogkas S, Dardiotis E, Liaskos C, Mamuris Z, Roussaki-Schulze A, Sakkas LI, Zafiriou E, Bogdanos DP. Curcumin mediates attenuation of pro-inflammatory interferon γ and interleukin 17 cytokine responses in psoriatic Disease, strengthening its role as a dietary immunosuppressant. Nutr Res. 2020;75:95–108. https://doi.org/10.1016/j.nutres.2020.01.005",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1016/j.biopha.2020.109946",
"author": "YS Chai",
"doi-asserted-by": "publisher",
"first-page": "109946",
"journal-title": "Biomed Pharmacother",
"key": "2282_CR43",
"unstructured": "Chai YS, Chen YQ, Lin SH, Xie K, Wang CJ, Yang YZ, et al. Curcumin regulates the differentiation of naïve CD4 + T cells and activates IL-10 immune modulation against acute lung injury in mice. Biomed Pharmacother. 2020;125:109946. https://doi.org/10.1016/j.biopha.2020.109946.",
"volume": "125",
"year": "2020"
}
],
"reference-count": 43,
"references-count": 43,
"relation": {},
"resource": {
"primary": {
"URL": "https://virologyj.biomedcentral.com/articles/10.1186/s12985-023-02282-x"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Virology"
],
"subtitle": [],
"title": "A novel film spray containing curcumin inhibits SARS-CoV-2 and influenza virus infection and enhances mucosal immunity",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "21"
}