Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling
et al., Cells, doi:10.3390/cells13161331, Aug 2024
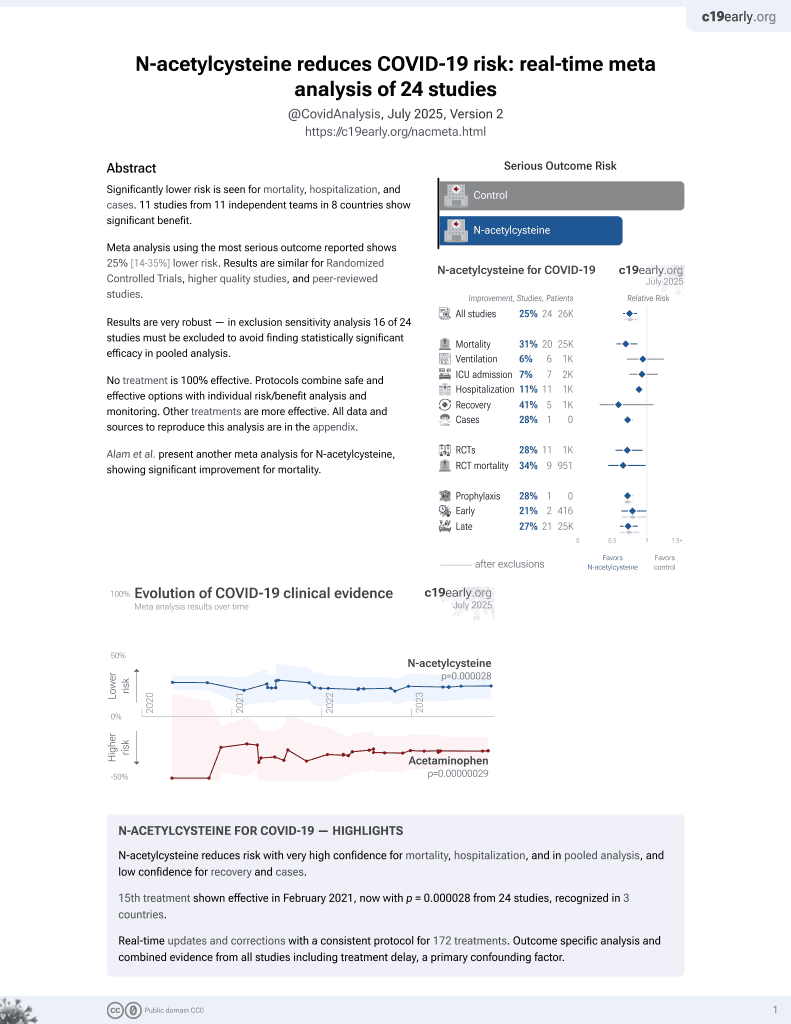
16th treatment shown to reduce risk in
February 2021, now with p = 0.0000032 from 25 studies, recognized in 3 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
In vitro study showing that the SARS-CoV-2 spike protein can activate cardiac fibroblasts through ACE2-dependent mechanisms, leading to cardiac fibrosis via the NLRP3 inflammasome and NF-κB signaling pathways. The results suggest that COVID-19 could directly contribute to long-term cardiovascular complications, particularly fibrosis, raising concerns about persistent cardiac damage.
The results point to several classes of therapeutics that may limit cardiac damage including NLRP3 inflammasome inhibitors (e.g., colchicine), NF-κB pathway inhibitors (e.g. curcumin), and antioxidants (e.g., vitamin C, NAC).
14 preclinical studies support the efficacy of N-acetylcysteine for COVID-19:
Severe COVID-19 is marked by endotheliopathy with elevated von Willebrand factor (VWF) levels and platelet/VWF-rich microthrombi; N-acetylcysteine can reduce VWF multimers and lyse VWF-dependent clots in vivo, potentially helping to alleviate thrombosis associated with COVID-1910-12.
N-acetylcysteine shows dose-dependent inhibition of SARS-CoV-24,7,9 , shows anti-inflammatory and immunomodulatory effects against SARS-CoV-2-induced immune responses in combination with bromelain6, suppressed virus-induced reactive oxygen species and blocked viral replication in a humanized mouse model and in human lung cells5, may limit COVID-19 induced cardiac damage by boosting cellular antioxidant defenses and potentially mitigating the oxidative stress caused by spike protein-induced ROS production in cardiac fibroblasts3, and reduces disulfide bonds in proteins and exhibits antioxidant properties that may inhibit viral replication and modulate inflammatory responses2.
NAC may be beneficial for COVID-19 by replenishing glutathione stores and reinforcing the glutathione peroxidase-4 pathway to inhibit ferroptosis, an oxidative stress-induced cell death pathway implicated in COVID-1913.
NAC reinforces glutathione levels, reduces ROS, and minimizes ferroptosis and cytokine storm14.
1.
Agamah et al., Network-based multi-omics-disease-drug associations reveal drug repurposing candidates for COVID-19 disease phases, ScienceOpen, doi:10.58647/DRUGARXIV.PR000010.v1.
2.
Reis et al., Antiviral effect of Bromelain combined with acetylcysteine against SARS-CoV-2 Omicron variant, Scientific Reports, doi:10.1038/s41598-025-92242-y.
3.
Van Tin et al., Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling, Cells, doi:10.3390/cells13161331.
4.
Chaopreecha et al., Andrographolide attenuates SARS-CoV-2 infection via an up-regulation of glutamate-cysteine ligase catalytic subunit (GCLC), Phytomedicine, doi:10.1016/j.phymed.2024.156279.
5.
Frasson et al., Identification of druggable host dependency factors shared by multiple SARS-CoV-2 variants of concern, Journal of Molecular Cell Biology. doi:10.1093/jmcb/mjae004, academic.oup.com/jmcb/advance-article/doi/10.1093/jmcb/mjae004/7596546.
6.
Ferreira et al., Taming the SARS-CoV-2-mediated proinflammatory response with BromAc®, Frontiers in Immunology, doi:10.3389/fimmu.2023.1308477.
7.
La Maestra et al., Inhibition of the Cell Uptake of Delta and Omicron SARS-CoV-2 Pseudoviruses by N-Acetylcysteine Irrespective of the Oxidoreductive Environment, Cells, doi:10.3390/cells11203313.
8.
Goc et al., Inhibitory effects of specific combination of natural compounds against SARS-CoV-2 and its Alpha, Beta, Gamma, Delta, Kappa, and Mu variants, European Journal of Microbiology and Immunology, doi:10.1556/1886.2021.00022.
9.
Akhter et al., The Combination of Bromelain and Acetylcysteine (BromAc) Synergistically Inactivates SARS-CoV-2, Viruses, doi:10.3390/v13030425.
10.
Martinez de Lizarrondo et al., Potent Thrombolytic Effect of N-Acetylcysteine on Arterial Thrombi, Circulation, doi:10.1161/CIRCULATIONAHA.117.027290.
11.
Chen et al., N-acetylcysteine reduces the size and activity of von Willebrand factor in human plasma and mice, Journal of Clinical Investigation, doi:10.1172/JCI41062.
12.
Goshua et al., Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study, The Lancet Haematology, doi:10.1016/S2352-3026(20)30216-7.
Van Tin et al., 11 Aug 2024, peer-reviewed, 5 authors.
Contact: yuhsunkao@gmail.com (corresponding author), d142109010@tmu.edu.tw, lekha@tmu.edu.tw, higa@haku-ai.or.jp, yjchen@tmu.edu.tw.
In vitro studies are an important part of preclinical research, however results may be very different in vivo.
Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling
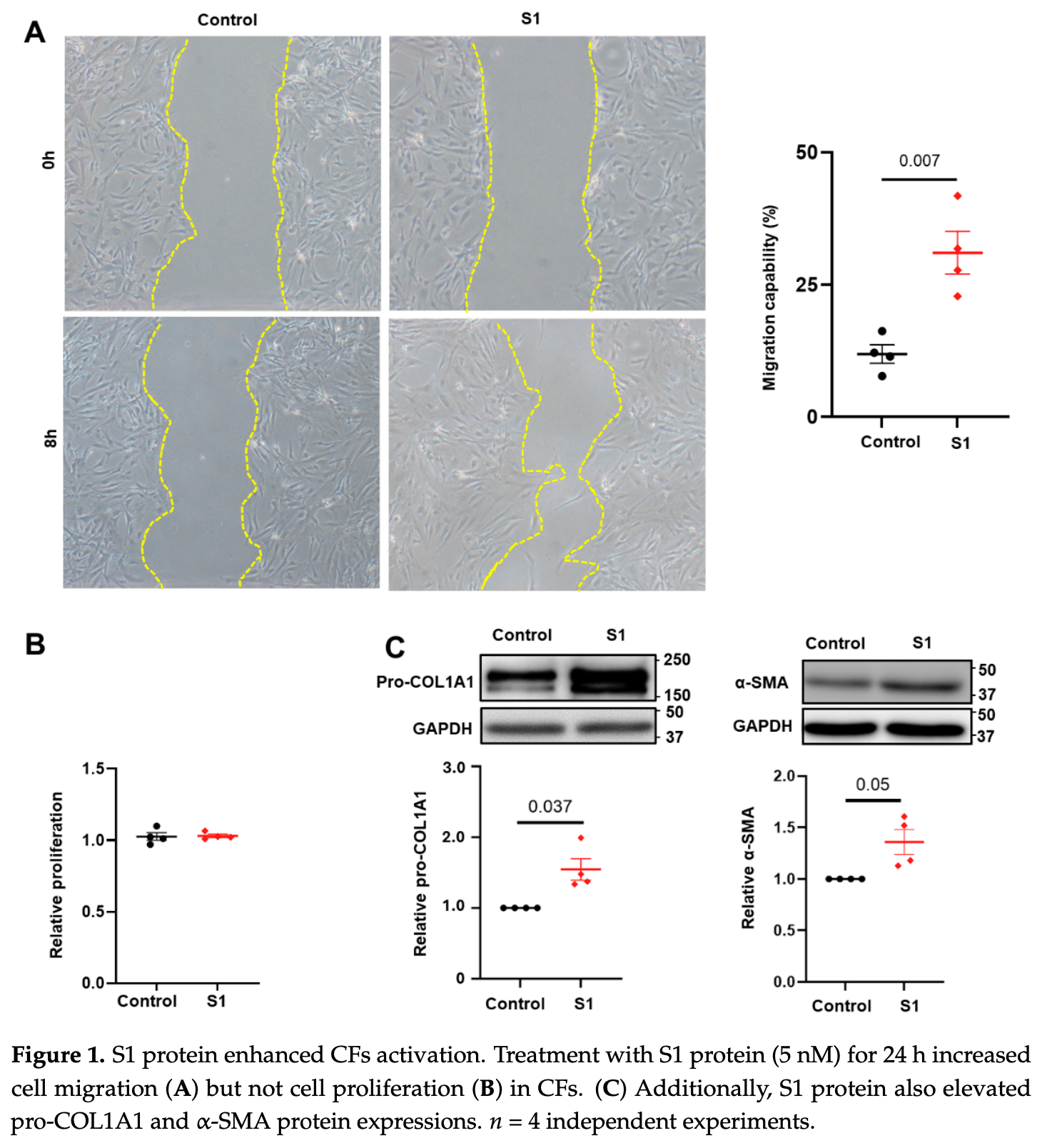
Cells, doi:10.3390/cells13161331
Background: The spike protein of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is crucial to viral entry and can cause cardiac injuries. Toll-like receptor 4 (TLR4) and NOD-, LPR-, and pyrin-domain-containing 3 (NLRP3) inflammasome are critical immune system components implicated in cardiac fibrosis. The spike proteins activate NLRP3 inflammasome through TLR4 or angiotensin-converting enzyme 2 (ACE2) receptors, damaging various organs. However, the role of spike proteins in cardiac fibrosis in humans and the interactions of spike proteins with NLRP3 inflammasomes and TLR4 remain poorly understood. Methods: We utilized scratch assays, Western blotting, and immunofluorescence to evaluate the migration, fibrosis signaling, mitochondrial calcium levels, reactive oxygen species (ROS) production, and cell morphology of cultured human cardiac fibroblasts (CFs) treated with spike (S1) proteins for 24 h with or without an anti-ACE2 neutralizing antibody, a TLR4 blocker, or an NLRP3 inhibitor. Results: S1 protein enhanced CFs migration and the expressions of collagen 1, α-smooth muscle actin, transforming growth factor β1 (TGF-β1), phosphorylated SMAD2/3, interleukin 1β (IL-1β), and nuclear factor kappa-light-chainenhancer of activated B cells (NF-κB). S1 increased ROS production but did not affect mitochondrial calcium content and cell morphology. Treatment with an anti-ACE2 neutralizing antibody attenuated the effects of S1 on collagen 1 and TGF-β1 expressions. Moreover, NLRP3 (MCC950) and NF-kB inhibitors, but not the TLR4 inhibitor TAK-242, prevented the S1-enhanced CFs migration and overexpression of collagen 1, TGF-β1, and IL-1β. Conclusion: S1 activates human CFs by priming NLRP3 inflammasomes through NF-κB signaling in an ACE2-dependent manner.
Supplementary Materials: The following supporting information can be downloaded at: https://www. mdpi.com/article/10.3390/cells13161331/s1, Figure S1 : Effect of S1 protein on CFs mitochondrial morphology; Figure S2 : Effect of S1 protein on CFs mitochondrial calcium levels; Figure S3 : Effect of S1 protein on CFs mitochondrial ROS production.
References
Albornoz, Amarilla, Modhiran, Parker, Li et al., SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein, Mol. Psychiatry, doi:10.1038/s41380-022-01831-0
Avolio, Carrabba, Milligan, Kavanagh Williamson, Beltrami et al., The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147 receptor-mediated signalling: A potential non-infective mechanism of COVID-19 microvascular disease, Clin. Sci, doi:10.1042/CS20210735
Avolio, Srivastava, Ji, Carrabba, Tsang et al., Murine studies and expressional analyses of human cardiac pericytes reveal novel trajectories of SARS-CoV-2 Spike protein-induced microvascular damage, Signal Transduct. Target. Ther, doi:10.1038/s41392-023-01489-2
Babadaei, Hasan, Bloukh, Edis, Sharifi et al., The expression level of angiotensinconverting enzyme 2 determines the severity of COVID-19: Lung and heart tissue as targets, J. Biomol. Struct. Dyn, doi:10.1080/07391102.2020.1767211
Bai, Li, Liu, Gao, Zhang et al., Effects of IL-1β and IL-18 induced by NLRP3 inflammasome activation on myocardial reperfusion injury after PCI, Eur. Rev. Med. Pharmacol. Sci, doi:10.26355/eurrev_201911_19579
Boretti, PQQ Supplementation and SARS-CoV-2 Spike Protein-Induced Heart Inflammation, Nat. Prod. Commun, doi:10.1177/1934578X221080929
Borkotoky, Dey, Hazarika, Interactions of angiotensin-converting enzyme-2 (ACE2) and SARS-CoV-2 spike receptorbinding domain (RBD): A structural perspective, Mol. Biol. Rep, doi:10.1007/s11033-022-08193-4
Cao, Nguyen, Tsai, Gao, Tian et al., The SARS-CoV-2 spike protein induces long-term transcriptional perturbations of mitochondrial metabolic genes, causes cardiac fibrosis, and reduces myocardial contractile in obese mice, Mol. Metab, doi:10.1016/j.molmet.2023.101756
Clemens, Ye, Zhou, Kim, Pease et al., SARS-CoV-2 spike protein-mediated cardiomyocyte fusion may contribute to increased arrhythmic risk in COVID-19, PLoS ONE, doi:10.1371/journal.pone.0282151
Corpetti, Del Re, Seguella, Palenca, Rurgo et al., Cannabidiol inhibits SARS-Cov-2 spike (S) protein-induced cytotoxicity and inflammation through a PPARγ-dependent TLR4/NLRP3/Caspase-1 signaling suppression in Caco-2 cell line, Phytother. Res, doi:10.1002/ptr.7302
Del Re, Corpetti, Pesce, Seguella, Steardo et al., Ultramicronized Palmitoylethanolamide Inhibits NLRP3 Inflammasome Expression and Pro-Inflammatory Response Activated by SARS-CoV-2 Spike Protein in Cultured Murine Alveolar Macrophages, Metabolites, doi:10.3390/metabo11090592
Driggin, Madhavan, Bikdeli, Chuich, Laracy et al., Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic, J. Am. Coll. Cardiol, doi:10.1016/j.jacc.2020.03.031
Fontes-Dantas, Fernandes, Gutman, De Lima, Antonio et al., SARS-CoV-2 Spike protein induces TLR4-mediated long-term cognitive dysfunction recapitulating post-COVID-19 syndrome in mice, Cell Rep, doi:10.1016/j.celrep.2023.112189
Gupta, Madhavan, Sehgal, Nair, Mahajan et al., Extrapulmonary manifestations of COVID-19, Nat. Med, doi:10.1038/s41591-020-0968-3
Guy, Lambert, Turner, Porter, Functional angiotensin-converting enzyme 2 is expressed in human cardiac myofibroblasts, Exp. Physiol, doi:10.1113/expphysiol.2007.040139
Han, Zeng, Jiang, Yang, Yuan et al., CSC expert consensus on principles of clinical management of patients with severe emergent cardiovascular diseases during the COVID-19 epidemic, Circulation, doi:10.1161/CIRCULATIONAHA.120.047011
Huang, Huang, He, Feng, Shi et al., Sars-Cov-2 Spike Protein-Induced Damage of hiPSC-Derived Cardiomyocytes, Adv. Biol, doi:10.1002/adbi.202101327
Huang, Yang, Xu, Xu, Liu, Structural and functional properties of SARS-CoV-2 spike protein: Potential antivirus drug development for COVID-19, Acta Pharmacol. Sin, doi:10.1038/s41401-020-0485-4
Huynh, Rethi, Lee, Higa, Kao et al., Spike Protein Impairs Mitochondrial Function in Human Cardiomyocytes: Mechanisms Underlying Cardiac Injury in COVID-19, Cells, doi:10.3390/cells12060877
Imig, SARS-CoV-2 spike protein causes cardiovascular disease independent of viral infection, Clin. Sci, doi:10.1042/CS20220028
Kato, Nishiyama, Man Lee, Ibuki, Imai et al., TRPC3-Nox2 Protein Complex Formation Increases the Risk of SARS-CoV-2 Spike Protein-Induced Cardiomyocyte Dysfunction through ACE2 Upregulation, Int. J. Mol. Sci, doi:10.3390/ijms24010102
Kelley, Jeltema, Duan, He, The NLRP3 Inflammasome: An Overview of Mechanisms of Activation and Regulation, Int. J. Mol. Sci, doi:10.3390/ijms20133328
Kole, Stefanou, Karvelas, Schizas, Toutouzas, Acute and Post-Acute COVID-19 Cardiovascular Complications: A Comprehensive Review, Cardiovasc. Drugs Ther, doi:10.1007/s10557-023-07465-w
Kong, Christia, Frangogiannis, The pathogenesis of cardiac fibrosis, Cell Mol. Life Sci, doi:10.1007/s00018-013-1349-6
Krishnan, Ellenberger, Phetsouphanh, Kelleher, Matthews et al., Myocardial fibrosis occurs in non-hospitalised patients with chronic symptoms after COVID-19, Int. J. Cardiol. Heart Vasc, doi:10.1016/j.ijcha.2022.100964
Liang, Bao, Yang, Liu, Sun et al., SARS-CoV-2 spike protein induces IL-18-mediated cardiopulmonary inflammation via reduced mitophagy, Signal Transduct. Target. Ther
Lin, More than a key-the pathological roles of SARS-CoV-2 spike protein in COVID-19 related cardiac injury, Sports Med. Health Sci, doi:10.1016/j.smhs.2023.03.004
Litvi Ňuková, Talavera-López, Maatz, Reichart, Worth et al., Cells of the adult human heart, Nature, doi:10.1038/s41586-020-2797-4
Liu, Gai, Wang, Zeng, Sun et al., Single-cell analysis of SARS-CoV-2 receptor ACE2 and spike protein priming expression of proteases in the human heart, Cardiovasc. Res, doi:10.1093/cvr/cvaa191
Liu, Liu, Wang, COVID-19 and cardiovascular diseases, J. Mol. Cell Biol, doi:10.1093/jmcb/mjaa064
Madjid, Safavi-Naeini, Solomon, Vardeny, Potential effects of coronaviruses on the cardiovascular system: A review, JAMA Cardiol, doi:10.1001/jamacardio.2020.1286
Oudit, Wang, Viveiros, Kellner, Penninger, Angiotensin-converting enzyme 2-at the heart of the COVID-19 pandemic, Cell, doi:10.1016/j.cell.2023.01.039
Parhizgar, Yazdankhah, Rzepka, Chung, Ali et al., Beyond Acute COVID-19: A Review of Long-term Cardiovascular Outcomes, Can. J. Cardiol, doi:10.1016/j.cjca.2023.01.031
Raafs, Ghossein, Brandt, Henkens, Kooi et al., Cardiovascular outcome 6 months after severe coronavirus disease 2019 infection, J. Hypertens, doi:10.1097/HJH.0000000000003110
Segura-Villalobos, Roa-Velázquez, Zavala-Vargas, Filisola-Villaseñor, Castillo Arellano et al., Jacareubin inhibits TLR4-induced lung inflammatory response caused by the RBD domain of SARS-CoV-2 Spike protein, Pharmacol. Rep, doi:10.1007/s43440-022-00398-5
Shen, Gong, Zhang, Cao, Mao et al., Besides TLR2 and TLR4, NLRP3 is also involved in regulating Escherichia coli infection-induced inflammatory responses in mice, Int. Immunopharmacol, doi:10.1016/j.intimp.2023.110556
Shi, Qin, Cai, Liu, Shen et al., Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019, Eur. Heart J, doi:10.1093/eurheartj/ehaa408
Shirato, Kizaki, SARS-CoV-2 spike protein S1 subunit induces pro-inflammatory responses via toll-like receptor 4 signaling in murine and human macrophages, Heliyon, doi:10.1016/j.heliyon.2021.e06187
Travers, Kamal, Robbins, Yutzey, Blaxall, Cardiac Fibrosis: The Fibroblast Awakens, Circ. Res, doi:10.1161/CIRCRESAHA.115.306565
Turner, Inflammatory and fibrotic responses of cardiac fibroblasts to myocardial damage associated molecular patterns (DAMPs), J. Mol. Cell Cardiol, doi:10.1016/j.yjmcc.2015.11.002
Wang, Zhang, Xiao, Zhang, Wu et al., NLRP3 Inflammasome and Inflammatory Diseases, Oxid. Med. Cell Longev, doi:10.1155/2020/4063562
Wicherska-Pawłowska, Wróbel, Rybka, Toll-Like Receptors (TLRs), NOD-Like Receptors (NLRs), and RIG-I-Like Receptors (RLRs) in Innate Immunity. TLRs, NLRs, and RLRs Ligands as Immunotherapeutic Agents for Hematopoietic Diseases, Int. J. Mol. Sci, doi:10.3390/ijms222413397
Zheng, Ma, Zhang, Xie, COVID-19 and the cardiovascular system, Nat. Rev. Cardiol, doi:10.1038/s41569-020-0360-5
Zhu, Zhang, Wang, Li, Yang et al., A Novel Coronavirus from Patients with Pneumonia in China, New Engl. J. Med, doi:10.1056/NEJMoa2001017
DOI record:
{
"DOI": "10.3390/cells13161331",
"ISSN": [
"2073-4409"
],
"URL": "http://dx.doi.org/10.3390/cells13161331",
"abstract": "<jats:p>Background: The spike protein of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is crucial to viral entry and can cause cardiac injuries. Toll-like receptor 4 (TLR4) and NOD-, LPR-, and pyrin-domain-containing 3 (NLRP3) inflammasome are critical immune system components implicated in cardiac fibrosis. The spike proteins activate NLRP3 inflammasome through TLR4 or angiotensin-converting enzyme 2 (ACE2) receptors, damaging various organs. However, the role of spike proteins in cardiac fibrosis in humans and the interactions of spike proteins with NLRP3 inflammasomes and TLR4 remain poorly understood. Methods: We utilized scratch assays, Western blotting, and immunofluorescence to evaluate the migration, fibrosis signaling, mitochondrial calcium levels, reactive oxygen species (ROS) production, and cell morphology of cultured human cardiac fibroblasts (CFs) treated with spike (S1) proteins for 24 h with or without an anti-ACE2 neutralizing antibody, a TLR4 blocker, or an NLRP3 inhibitor. Results: S1 protein enhanced CFs migration and the expressions of collagen 1, α-smooth muscle actin, transforming growth factor β1 (TGF-β1), phosphorylated SMAD2/3, interleukin 1β (IL-1β), and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB). S1 increased ROS production but did not affect mitochondrial calcium content and cell morphology. Treatment with an anti-ACE2 neutralizing antibody attenuated the effects of S1 on collagen 1 and TGF-β1 expressions. Moreover, NLRP3 (MCC950) and NF-kB inhibitors, but not the TLR4 inhibitor TAK-242, prevented the S1-enhanced CFs migration and overexpression of collagen 1, TGF-β1, and IL-1β. Conclusion: S1 activates human CFs by priming NLRP3 inflammasomes through NF-κB signaling in an ACE2-dependent manner.</jats:p>",
"alternative-id": [
"cells13161331"
],
"author": [
{
"affiliation": [
{
"name": "International Ph.D. Program in Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan"
}
],
"family": "Van Tin",
"given": "Huynh",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Orthopedics, Shuangho Hospital, Taipei Medical University, Taipei 11031, Taiwan"
}
],
"family": "Rethi",
"given": "Lekha",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5735-6249",
"affiliation": [
{
"name": "Cardiac Electrophysiology and Pacing Laboratory, Division of Cardiovascular Medicine, Makiminato Central Hospital, Okinawa 901-2131, Japan"
}
],
"authenticated-orcid": false,
"family": "Higa",
"given": "Satoshi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-8687-5091",
"affiliation": [
{
"name": "International Ph.D. Program in Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan"
},
{
"name": "Graduate Institute of Clinical Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan"
},
{
"name": "Department of Medical Education and Research, Wan Fang Hospital, Taipei Medical University, Taipei 11031, Taiwan"
}
],
"authenticated-orcid": false,
"family": "Kao",
"given": "Yu-Hsun",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7224-4491",
"affiliation": [
{
"name": "International Ph.D. Program in Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan"
},
{
"name": "Graduate Institute of Clinical Medicine, College of Medicine, Taipei Medical University, Taipei 11031, Taiwan"
},
{
"name": "Division of Cardiovascular Medicine, Department of Internal Medicine, Wan Fang Hospital, Taipei Medical University, Taipei 11031, Taiwan"
}
],
"authenticated-orcid": false,
"family": "Chen",
"given": "Yi-Jen",
"sequence": "additional"
}
],
"container-title": "Cells",
"container-title-short": "Cells",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
8,
12
]
],
"date-time": "2024-08-12T09:19:38Z",
"timestamp": 1723454378000
},
"deposited": {
"date-parts": [
[
2024,
8,
12
]
],
"date-time": "2024-08-12T09:47:48Z",
"timestamp": 1723456068000
},
"funder": [
{
"DOI": "10.13039/501100020950",
"award": [
"110-2314-B-038-128"
],
"doi-asserted-by": "publisher",
"name": "National Science and Technology Council"
},
{
"DOI": "10.13039/501100022600",
"award": [
"113-wf-eva-12"
],
"doi-asserted-by": "publisher",
"name": "Wan Fang Hospital"
},
{
"award": [
"6-02-003"
],
"name": "Foundation for the Development of Internal Medicine in Okinawa"
}
],
"indexed": {
"date-parts": [
[
2024,
8,
13
]
],
"date-time": "2024-08-13T00:17:05Z",
"timestamp": 1723508225225
},
"is-referenced-by-count": 0,
"issue": "16",
"issued": {
"date-parts": [
[
2024,
8,
11
]
]
},
"journal-issue": {
"issue": "16",
"published-online": {
"date-parts": [
[
2024,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
8,
11
]
],
"date-time": "2024-08-11T00:00:00Z",
"timestamp": 1723334400000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2073-4409/13/16/1331/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1331",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2024,
8,
11
]
]
},
"published-online": {
"date-parts": [
[
2024,
8,
11
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/j.jacc.2020.03.031",
"article-title": "Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic",
"author": "Driggin",
"doi-asserted-by": "crossref",
"first-page": "2352",
"journal-title": "J. Am. Coll. Cardiol.",
"key": "ref_1",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047011",
"article-title": "CSC expert consensus on principles of clinical management of patients with severe emergent cardiovascular diseases during the COVID-19 epidemic",
"author": "Han",
"doi-asserted-by": "crossref",
"first-page": "e810",
"journal-title": "Circulation",
"key": "ref_2",
"volume": "141",
"year": "2020"
},
{
"DOI": "10.1001/jamacardio.2020.1286",
"article-title": "Potential effects of coronaviruses on the cardiovascular system: A review",
"author": "Madjid",
"doi-asserted-by": "crossref",
"first-page": "831",
"journal-title": "JAMA Cardiol.",
"key": "ref_3",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1038/s41569-020-0360-5",
"article-title": "COVID-19 and the cardiovascular system",
"author": "Zheng",
"doi-asserted-by": "crossref",
"first-page": "259",
"journal-title": "Nat. Rev. Cardiol.",
"key": "ref_4",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.cjca.2023.01.031",
"article-title": "Beyond Acute COVID-19: A Review of Long-term Cardiovascular Outcomes",
"author": "Parhizgar",
"doi-asserted-by": "crossref",
"first-page": "726",
"journal-title": "Can. J. Cardiol.",
"key": "ref_5",
"volume": "39",
"year": "2023"
},
{
"DOI": "10.1097/HJH.0000000000003110",
"article-title": "Cardiovascular outcome 6 months after severe coronavirus disease 2019 infection",
"author": "Raafs",
"doi-asserted-by": "crossref",
"first-page": "1278",
"journal-title": "J. Hypertens.",
"key": "ref_6",
"volume": "40",
"year": "2022"
},
{
"article-title": "Myocardial fibrosis occurs in non-hospitalised patients with chronic symptoms after COVID-19",
"author": "Krishnan",
"first-page": "100964",
"journal-title": "Int. J. Cardiol. Heart Vasc.",
"key": "ref_7",
"volume": "39",
"year": "2022"
},
{
"article-title": "PQQ Supplementation and SARS-CoV-2 Spike Protein-Induced Heart Inflammation",
"author": "Boretti",
"first-page": "1934578x221080929",
"journal-title": "Nat. Prod. Commun.",
"key": "ref_8",
"volume": "17",
"year": "2022"
},
{
"DOI": "10.1016/j.molmet.2023.101756",
"article-title": "The SARS-CoV-2 spike protein induces long-term transcriptional perturbations of mitochondrial metabolic genes, causes cardiac fibrosis, and reduces myocardial contractile in obese mice",
"author": "Cao",
"doi-asserted-by": "crossref",
"first-page": "101756",
"journal-title": "Mol. Metab.",
"key": "ref_9",
"volume": "74",
"year": "2023"
},
{
"DOI": "10.3390/cells12060877",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Huynh, T.V., Rethi, L., Lee, T.W., Higa, S., Kao, Y.H., and Chen, Y.J. (2023). Spike Protein Impairs Mitochondrial Function in Human Cardiomyocytes: Mechanisms Underlying Cardiac Injury in COVID-19. Cells, 12."
},
{
"DOI": "10.1371/journal.pone.0282151",
"doi-asserted-by": "crossref",
"key": "ref_11",
"unstructured": "Clemens, D.J., Ye, D., Zhou, W., Kim, C.S.J., Pease, D.R., Navaratnarajah, C.K., Barkhymer, A., Tester, D.J., Nelson, T.J., and Cattaneo, R. (2023). SARS-CoV-2 spike protein-mediated cardiomyocyte fusion may contribute to increased arrhythmic risk in COVID-19. PLoS ONE, 18."
},
{
"DOI": "10.1093/cvr/cvaa191",
"article-title": "Single-cell analysis of SARS-CoV-2 receptor ACE2 and spike protein priming expression of proteases in the human heart",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "1733",
"journal-title": "Cardiovasc. Res.",
"key": "ref_12",
"volume": "116",
"year": "2020"
},
{
"DOI": "10.1038/s41392-023-01489-2",
"article-title": "Murine studies and expressional analyses of human cardiac pericytes reveal novel trajectories of SARS-CoV-2 Spike protein-induced microvascular damage",
"author": "Avolio",
"doi-asserted-by": "crossref",
"first-page": "232",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_13",
"volume": "8",
"year": "2023"
},
{
"DOI": "10.3390/ijms24010102",
"doi-asserted-by": "crossref",
"key": "ref_14",
"unstructured": "Kato, Y., Nishiyama, K., Man Lee, J., Ibuki, Y., Imai, Y., Noda, T., Kamiya, N., Kusakabe, T., Kanda, Y., and Nishida, M. (2022). TRPC3-Nox2 Protein Complex Formation Increases the Risk of SARS-CoV-2 Spike Protein-Induced Cardiomyocyte Dysfunction through ACE2 Upregulation. Int. J. Mol. Sci., 24."
},
{
"DOI": "10.1016/j.smhs.2023.03.004",
"doi-asserted-by": "crossref",
"key": "ref_15",
"unstructured": "Lin, Z. (2023). More than a key-the pathological roles of SARS-CoV-2 spike protein in COVID-19 related cardiac injury. Sports Med. Health Sci., in press."
},
{
"DOI": "10.1042/CS20210735",
"article-title": "The SARS-CoV-2 Spike protein disrupts human cardiac pericytes function through CD147 receptor-mediated signalling: A potential non-infective mechanism of COVID-19 microvascular disease",
"author": "Avolio",
"doi-asserted-by": "crossref",
"first-page": "2667",
"journal-title": "Clin. Sci.",
"key": "ref_16",
"volume": "135",
"year": "2021"
},
{
"DOI": "10.1007/s11033-022-08193-4",
"article-title": "Interactions of angiotensin-converting enzyme-2 (ACE2) and SARS-CoV-2 spike receptor-binding domain (RBD): A structural perspective",
"author": "Borkotoky",
"doi-asserted-by": "crossref",
"first-page": "2713",
"journal-title": "Mol. Biol. Rep.",
"key": "ref_17",
"volume": "50",
"year": "2023"
},
{
"DOI": "10.1038/s41401-020-0485-4",
"article-title": "Structural and functional properties of SARS-CoV-2 spike protein: Potential antivirus drug development for COVID-19",
"author": "Huang",
"doi-asserted-by": "crossref",
"first-page": "1141",
"journal-title": "Acta Pharmacol. Sin.",
"key": "ref_18",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1016/j.cell.2023.01.039",
"article-title": "Angiotensin-converting enzyme 2-at the heart of the COVID-19 pandemic",
"author": "Oudit",
"doi-asserted-by": "crossref",
"first-page": "906",
"journal-title": "Cell",
"key": "ref_19",
"volume": "186",
"year": "2023"
},
{
"DOI": "10.1080/07391102.2020.1767211",
"article-title": "The expression level of angiotensin-converting enzyme 2 determines the severity of COVID-19: Lung and heart tissue as targets",
"author": "Babadaei",
"doi-asserted-by": "crossref",
"first-page": "3780",
"journal-title": "J. Biomol. Struct. Dyn.",
"key": "ref_20",
"volume": "39",
"year": "2021"
},
{
"DOI": "10.1038/s41586-020-2797-4",
"article-title": "Cells of the adult human heart",
"author": "Maatz",
"doi-asserted-by": "crossref",
"first-page": "466",
"journal-title": "Nature",
"key": "ref_21",
"volume": "588",
"year": "2020"
},
{
"DOI": "10.1113/expphysiol.2007.040139",
"article-title": "Functional angiotensin-converting enzyme 2 is expressed in human cardiac myofibroblasts",
"author": "Guy",
"doi-asserted-by": "crossref",
"first-page": "579",
"journal-title": "Exp. Physiol.",
"key": "ref_22",
"volume": "93",
"year": "2008"
},
{
"DOI": "10.3390/ijms20133328",
"doi-asserted-by": "crossref",
"key": "ref_23",
"unstructured": "Kelley, N., Jeltema, D., Duan, Y., and He, Y. (2019). The NLRP3 Inflammasome: An Overview of Mechanisms of Activation and Regulation. Int. J. Mol. Sci., 20."
},
{
"article-title": "NLRP3 Inflammasome and Inflammatory Diseases",
"author": "Wang",
"first-page": "4063562",
"journal-title": "Oxid. Med. Cell Longev.",
"key": "ref_24",
"volume": "2020",
"year": "2020"
},
{
"DOI": "10.3390/ijms222413397",
"doi-asserted-by": "crossref",
"key": "ref_25",
"unstructured": "Wicherska-Pawłowska, K., Wróbel, T., and Rybka, J. (2021). Toll-Like Receptors (TLRs), NOD-Like Receptors (NLRs), and RIG-I-Like Receptors (RLRs) in Innate Immunity. TLRs, NLRs, and RLRs Ligands as Immunotherapeutic Agents for Hematopoietic Diseases. Int. J. Mol. Sci., 22."
},
{
"DOI": "10.1016/j.intimp.2023.110556",
"article-title": "Besides TLR2 and TLR4, NLRP3 is also involved in regulating Escherichia coli infection-induced inflammatory responses in mice",
"author": "Shen",
"doi-asserted-by": "crossref",
"first-page": "110556",
"journal-title": "Int. Immunopharmacol.",
"key": "ref_26",
"volume": "121",
"year": "2023"
},
{
"DOI": "10.1038/s41380-022-01831-0",
"article-title": "SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein",
"author": "Albornoz",
"doi-asserted-by": "crossref",
"first-page": "2878",
"journal-title": "Mol. Psychiatry",
"key": "ref_27",
"volume": "28",
"year": "2023"
},
{
"DOI": "10.3390/metabo11090592",
"doi-asserted-by": "crossref",
"key": "ref_28",
"unstructured": "Del Re, A., Corpetti, C., Pesce, M., Seguella, L., Steardo, L., Palenca, I., Rurgo, S., De Conno, B., Sarnelli, G., and Esposito, G. (2021). Ultramicronized Palmitoylethanolamide Inhibits NLRP3 Inflammasome Expression and Pro-Inflammatory Response Activated by SARS-CoV-2 Spike Protein in Cultured Murine Alveolar Macrophages. Metabolites, 11."
},
{
"DOI": "10.1016/j.heliyon.2021.e06187",
"article-title": "SARS-CoV-2 spike protein S1 subunit induces pro-inflammatory responses via toll-like receptor 4 signaling in murine and human macrophages",
"author": "Shirato",
"doi-asserted-by": "crossref",
"first-page": "e06187",
"journal-title": "Heliyon",
"key": "ref_29",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1002/ptr.7302",
"article-title": "Cannabidiol inhibits SARS-Cov-2 spike (S) protein-induced cytotoxicity and inflammation through a PPARγ-dependent TLR4/NLRP3/Caspase-1 signaling suppression in Caco-2 cell line",
"author": "Corpetti",
"doi-asserted-by": "crossref",
"first-page": "6893",
"journal-title": "Phytother. Res.",
"key": "ref_30",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2001017",
"article-title": "A Novel Coronavirus from Patients with Pneumonia in China, 2019",
"author": "Zhu",
"doi-asserted-by": "crossref",
"first-page": "727",
"journal-title": "New Engl. J. Med.",
"key": "ref_31",
"volume": "382",
"year": "2020"
},
{
"key": "ref_32",
"unstructured": "World Health Organization (2024, March 24). Data. Who. int, WHO Coronavirus (COVID-19) Dashboard Cases [Dashboard]. Available online: https://data.who.int/dashboards/covid19/cases."
},
{
"DOI": "10.1038/s41591-020-0968-3",
"article-title": "Extrapulmonary manifestations of COVID-19",
"author": "Gupta",
"doi-asserted-by": "crossref",
"first-page": "1017",
"journal-title": "Nat. Med.",
"key": "ref_33",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1093/jmcb/mjaa064",
"article-title": "COVID-19 and cardiovascular diseases",
"author": "Liu",
"doi-asserted-by": "crossref",
"first-page": "161",
"journal-title": "J. Mol. Cell Biol.",
"key": "ref_34",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1093/eurheartj/ehaa408",
"article-title": "Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019",
"author": "Shi",
"doi-asserted-by": "crossref",
"first-page": "2070",
"journal-title": "Eur. Heart J.",
"key": "ref_35",
"volume": "41",
"year": "2020"
},
{
"DOI": "10.1007/s10557-023-07465-w",
"doi-asserted-by": "crossref",
"key": "ref_36",
"unstructured": "Kole, C., Stefanou, Ε., Karvelas, N., Schizas, D., and Toutouzas, K.P. (2023). Acute and Post-Acute COVID-19 Cardiovascular Complications: A Comprehensive Review. Cardiovasc. Drugs Ther., 1–16."
},
{
"DOI": "10.1042/CS20220028",
"article-title": "SARS-CoV-2 spike protein causes cardiovascular disease independent of viral infection",
"author": "Imig",
"doi-asserted-by": "crossref",
"first-page": "431",
"journal-title": "Clin. Sci.",
"key": "ref_37",
"volume": "136",
"year": "2022"
},
{
"DOI": "10.1002/adbi.202101327",
"doi-asserted-by": "crossref",
"key": "ref_38",
"unstructured": "Huang, X., Huang, B., He, Y., Feng, L., Shi, J., Wang, L., Peng, J., and Chen, Y. (2022). Sars-Cov-2 Spike Protein-Induced Damage of hiPSC-Derived Cardiomyocytes. Adv. Biol., 6."
},
{
"DOI": "10.1007/s00018-013-1349-6",
"article-title": "The pathogenesis of cardiac fibrosis",
"author": "Kong",
"doi-asserted-by": "crossref",
"first-page": "549",
"journal-title": "Cell Mol. Life Sci.",
"key": "ref_39",
"volume": "71",
"year": "2014"
},
{
"DOI": "10.1161/CIRCRESAHA.115.306565",
"article-title": "Cardiac Fibrosis: The Fibroblast Awakens",
"author": "Travers",
"doi-asserted-by": "crossref",
"first-page": "1021",
"journal-title": "Circ. Res.",
"key": "ref_40",
"volume": "118",
"year": "2016"
},
{
"DOI": "10.1016/j.yjmcc.2015.11.002",
"article-title": "Inflammatory and fibrotic responses of cardiac fibroblasts to myocardial damage associated molecular patterns (DAMPs)",
"author": "Turner",
"doi-asserted-by": "crossref",
"first-page": "189",
"journal-title": "J. Mol. Cell Cardiol.",
"key": "ref_41",
"volume": "94",
"year": "2016"
},
{
"article-title": "Effects of IL-1β and IL-18 induced by NLRP3 inflammasome activation on myocardial reperfusion injury after PCI",
"author": "Bai",
"first-page": "10101",
"journal-title": "Eur. Rev. Med. Pharmacol. Sci.",
"key": "ref_42",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.1007/s43440-022-00398-5",
"article-title": "Jacareubin inhibits TLR4-induced lung inflammatory response caused by the RBD domain of SARS-CoV-2 Spike protein",
"doi-asserted-by": "crossref",
"first-page": "1315",
"journal-title": "Pharmacol. Rep.",
"key": "ref_43",
"volume": "74",
"year": "2022"
},
{
"DOI": "10.1016/j.celrep.2023.112189",
"article-title": "SARS-CoV-2 Spike protein induces TLR4-mediated long-term cognitive dysfunction recapitulating post-COVID-19 syndrome in mice",
"author": "Fernandes",
"doi-asserted-by": "crossref",
"first-page": "112189",
"journal-title": "Cell Rep.",
"key": "ref_44",
"volume": "42",
"year": "2023"
},
{
"DOI": "10.1038/s41392-023-01368-w",
"article-title": "SARS-CoV-2 spike protein induces IL-18-mediated cardiopulmonary inflammation via reduced mitophagy",
"author": "Liang",
"doi-asserted-by": "crossref",
"first-page": "108",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "ref_45",
"volume": "8",
"year": "2023"
}
],
"reference-count": 45,
"references-count": 45,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2073-4409/13/16/1331"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Spike Protein of SARS-CoV-2 Activates Cardiac Fibrogenesis through NLRP3 Inflammasomes and NF-κB Signaling",
"type": "journal-article",
"volume": "13"
}
vantin