Dados de Vida Real sobre o Uso da Hidroxicloroquina ou da Cloroquina Combinadas ou Não à Azitromicina em Pacientes com Covid-19: Uma Análise Retrospectiva no Brasil
et al., Arquivos Brasileiros de Cardiologia, doi:10.36660/abc.20220935, Sep 2023
HCQ for COVID-19
1st treatment shown to reduce risk in
March 2020, now with p < 0.00000000001 from 424 studies, used in 59 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
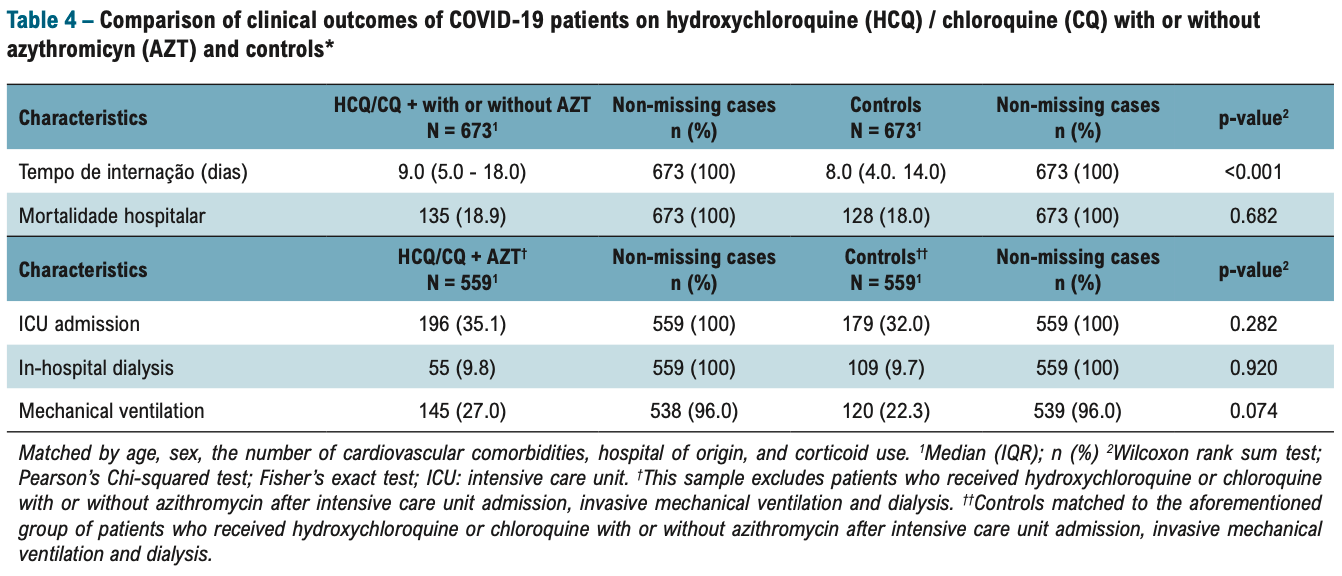
Retrospective 7,580 hospitalized patients in Brazil, showing longer hospitalization, and no significant difference in mortality, mechanical ventilation, and ICU admission with HCQ treatment.
Authors note confounding by indication due to selected use in a compassionate use context. Authors match only on age, sex, cardiovascular comorbidities, and in-hospital use of corticosteroid, and only 10% of patients received HCQ/CQ, therefore confounding by indication is likely to be significant. A different matching list is included in the text, but neither includes COVID-19 severity.
In the first line of the abstract authors falsely state that there is no evidence of benefit for HCQ treatment. While misrepresenting prior research is common, this is an extreme case and raises concern for validity of the analysis. In reality 150 controlled studies show statistically significant positive results for one or more outcomes (including 13 RCTs)1-148. Authors discussion of prior research shows similar bias.
This study is excluded in the after exclusion results of meta-analysis:
substantial unadjusted confounding by indication likely; authors discussion of prior research exhibits strong bias, raising concern for bias in analysis.
|
risk of death, 5.5% higher, RR 1.05, p = 0.68, treatment 135 of 673 (20.1%), control 128 of 673 (19.0%).
|
|
risk of mechanical ventilation, 21.1% higher, RR 1.21, p = 0.08, treatment 145 of 538 (27.0%), control 120 of 539 (22.3%).
|
|
risk of ICU admission, 9.5% higher, RR 1.09, p = 0.31, treatment 196 of 559 (35.1%), control 179 of 559 (32.0%).
|
|
hospitalization time, 12.5% higher, relative time 1.12, p = 0.03, treatment median 9.0 IQR 13.0 n=673, control median 8.0 IQR 10.0 n=673.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
1.
Esper et al., Empirical treatment with hydroxychloroquine and azithromycin for suspected cases of COVID-19 followed-up by telemedicine, Prevent Senior Institute, São Paulo, Brazil, pgibertie.com/wp-content/uploads/2020/04/2020.04.15-journal-manuscript-final.pdf.
2.
Huang et al., Preliminary evidence from a multicenter prospective observational study of the safety and efficacy of chloroquine for the treatment of COVID-19, National Science Review, doi:10.1093/nsr/nwaa113.
3.
Guérin et al., Azithromycin and Hydroxychloroquine Accelerate Recovery of Outpatients with Mild/Moderate COVID-19, Asian Journal of Medicine and Health, doi:10.9734/ajmah/2020/v18i730224.
4.
Derwand et al., COVID-19 Outpatients – Early Risk-Stratified Treatment with Zinc Plus Low Dose Hydroxychloroquine and Azithromycin: A Retrospective Case Series Study, International Journal of Antimicrobial Agents, doi:10.1016/j.ijantimicag.2020.106214.
5.
Hong et al., Early Hydroxychloroquine Administration for Rapid Severe Acute Respiratory Syndrome Coronavirus 2 Eradication, Infection & Chemotherapy, 2020, doi:10.3947/ic.2020.52.3.396.
6.
Bernabeu-Wittel et al., Effectiveness of a On-Site Medicalization Program for Nursing Homes with COVID-19 Outbreaks, J. Gerontol. A Biol. Sci. Med. Sci., doi:10.1093/gerona/glaa192.
7.
Yu et al., Beneficial effects exerted by hydroxychloroquine in treating COVID-19 patients via protecting multiple organs, Science China Life Sciences, 2020 Aug 3, doi:10.1007/s11427-020-1782-1.
8.
Ly et al., Pattern of SARS-CoV-2 infection among dependant elderly residents living in retirement homes in Marseille, France, March-June 2020, International Journal of Antimicrobial Agents, doi:10.1016/j.ijantimicag.2020.106219.
9.
Ip et al., Hydroxychloroquine in the treatment of outpatients with mildly symptomatic COVID-19: A multi-center observational study, BMC Infectious Diseases, doi:10.1186/s12879-021-05773-w.
10.
Heras et al., COVID-19 mortality risk factors in older people in a long-term care center, European Geriatric Medicine, doi:10.1007/s41999-020-00432-w.
11.
Sulaiman et al., The Effect of Early Hydroxychloroquine-based Therapy in COVID-19 Patients in Ambulatory Care Settings: A Nationwide Prospective Cohort Study, medRxiv, doi:10.1101/2020.09.09.20184143.
12.
Szente Fonseca et al., Risk of Hospitalization for Covid-19 Outpatients Treated with Various Drug Regimens in Brazil: Comparative Analysis, Travel Medicine and Infectious Disease, doi:10.1016/j.tmaid.2020.101906.
13.
Cadegiani et al., Early COVID-19 Therapy with azithromycin plus nitazoxanide, ivermectin or hydroxychloroquine in Outpatient Settings Significantly Improved COVID-19 outcomes compared to Known outcomes in untreated patients, New Microbes and New Infections, doi:10.1016/j.nmni.2021.100915.
14.
Simova et al., Hydroxychloroquine for prophylaxis and treatment of COVID-19 in health care workers, New Microbes and New Infections, doi:10.1016/j.nmni.2020.100813.
15.
Su et al., Efficacy of early hydroxychloroquine treatment in preventing COVID-19 pneumonia aggravation, the experience from Shanghai, China, BioScience Trends, doi:10.5582/bst.2020.03340.
16.
Mokhtari et al., Clinical outcomes of patients with mild COVID-19 following treatment with hydroxychloroquine in an outpatient setting, International Immunopharmacology, doi:10.1016/j.intimp.2021.107636.
17.
Corradini et al., Clinical factors associated with death in 3044 COVID-19 patients managed in internal medicine wards in Italy: results from the SIMI-COVID-19 study of the Italian Society of Internal Medicine (SIMI), Internal and Emergency Medicine, doi:10.1007/s11739-021-02742-8.
18.
Million et al., Early Treatment with Hydroxychloroquine and Azithromycin in 10,429 COVID-19 Outpatients: A Monocentric Retrospective Cohort Study, Reviews in Cardiovascular Medicine, doi:10.31083/j.rcm2203116.
19.
Atipornwanich et al., Various Combinations of Favipiravir, Lopinavir-Ritonavir, Darunavir-Ritonavir, High-Dose Oseltamivir, and Hydroxychloroquine for the Treatment of COVID-19: A Randomized Controlled Trial (FIGHT-COVID-19 Study), SSRN Electronic Journal, doi:10.2139/ssrn.3936499.
20.
Chechter et al., Evaluation of patients treated by telemedicine in the beginning of the COVID-19 pandemic in São Paulo, Brazil: A non-randomized clinical trial preliminary study, Heliyon, doi:10.1016/j.heliyon.2023.e15337.
21.
Rathod et al., Risk Factors associated with COVID-19 Patients in India: A Single Center Retrospective Cohort Study, The Journal of the Association of Physicians of India, doi:10.5005/japi-11001-0263.
22.
Azhar et al., Effectiveness of early pharmaceutical interventions in symptomatic COVID-19 patients: A randomized clinical trial, Pakistan Journal of Medical Sciences, doi:10.12669/pjms.40.5.8757.
23.
Zhong Nanshan, Efficacy and safety of chloroquine for treatment of COVID-19. An open-label, multi-center, non-randomized trial, 3/26, twitter.com/JamesTodaroMD/status/1243260720944480265.
24.
Chen et al., Efficacy of hydroxychloroquine in patients with COVID-19: results of a randomized clinical trial, medRxiv, doi:10.1101/2020.03.22.20040758.
25.
Sánchez-Álvarez et al., Status of SARS-CoV-2 infection in patients on renal replacement therapy. Report of the COVID-19 Registry of the Spanish Society of Nephrology (SEN), Nefrología, doi:10.1016/j.nefroe.2020.04.002.
26.
Membrillo de Novales et al., Early Hydroxychloroquine Is Associated with an Increase of Survival in COVID-19 Patients: An Observational Study, Preprints, doi:10.20944/preprints202005.0057.v1.
27.
Yu (B) et al., Low Dose of Hydroxychloroquine Reduces Fatality of Critically Ill Patients With COVID-19, Science China Life Sciences, 2020 May 15, 1-7, doi:10.1007/s11427-020-1732-2.
28.
Kim et al., Treatment Response to Hydroxychloroquine, Lopinavir/Ritonavir, and Antibiotics for Moderate COVID 19: A First Report on the Pharmacological Outcomes from South Korea, medRxiv, doi:10.1101/2020.05.13.20094193.
29.
Huang (B) et al., Preliminary evidence from a multicenter prospective observational study of the safety and efficacy of chloroquine for the treatment of COVID-19, National Science Review, doi:10.1093/nsr/nwaa113.
30.
Rogado et al., Covid-19 and lung cancer: A greater fatality rate?, Lung Cancer, doi:10.1016/j.lungcan.2020.05.034.
31.
Sbidian et al., Hydroxychloroquine with or without azithromycin and in-hospital mortality or discharge in patients hospitalized for COVID-19 infection: a cohort study of 4,642 in-patients in France, medRxiv, doi:10.1101/2020.06.16.20132597.
32.
Chen (B) et al., Efficacy and safety of chloroquine or hydroxychloroquine in moderate type of COVID-19: a prospective open-label randomized controlled study, medRxiv, doi:10.1101/2020.06.19.20136093.
33.
Lagier et al., Outcomes of 3,737 COVID-19 patients treated with hydroxychloroquine/azithromycin and other regimens in Marseille, France: A retrospective analysis, Travel Medicine and Infectious Disease, doi:10.1016/j.tmaid.2020.101791.
34.
Mikami et al., Risk Factors for Mortality in Patients with COVID-19 in New York City, J. Gen. Intern. Med., doi:10.1007/s11606-020-05983-z.
35.
Arshad et al., Treatment with Hydroxychloroquine, Azithromycin, and Combination in Patients Hospitalized with COVID-19, International Journal of Infectious Diseases, doi:10.1016/j.ijid.2020.06.099.
36.
Bernaola et al., Observational Study of the Efficiency of Treatments in Patients Hospitalized with Covid-19 in Madrid, medRxiv, doi:10.1101/2020.07.17.20155960.
37.
D'Arminio Monforte et al., Effectiveness of Hydroxychloroquine in COVID-19 disease: A done and dusted situation?, International Journal of Infectious Diseases, doi:10.1016/j.ijid.2020.07.056.
38.
Davido et al., Impact of medical care including anti-infective agents use on the prognosis of COVID-19 hospitalized patients over time, International Journal of Antimicrobial Agents, 2020, doi:10.1016/j.ijantimicag.2020.106129.
39.
Yu (C) et al., Beneficial effects exerted by hydroxychloroquine in treating COVID-19 patients via protecting multiple organs, Science China Life Sciences, 2020 Aug 3, doi:10.1007/s11427-020-1782-1.
40.
Berenguer et al., Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain, Clinical Microbiology and Infection, doi:10.1016/j.cmi.2020.07.024.
41.
Kamran et al., Clearing the fog: Is HCQ effective in reducing COVID-19 progression: A randomized controlled trial, medRxiv, doi:10.1101/2020.07.30.20165365.
42.
Pinato et al., Clinical portrait of the SARS-CoV-2 epidemic in European cancer patients, Cancer Discovery, doi:10.1158/2159-8290.CD-20-0773.
43.
Dubernet et al., A comprehensive strategy for the early treatment of COVID-19 with azithromycin/hydroxychloroquine and/or corticosteroids: results of a retrospective observational study in the French overseas department of Reunion Island, Journal of Global Antimicrobial Resistance, doi:10.1016/j.jgar.2020.08.001.
44.
Catteau et al., Low-dose Hydroxychloroquine Therapy and Mortality in Hospitalized Patients with COVID-19: A Nationwide Observational Study of 8075 Participants, International Journal of Antimicrobial Agents, doi:10.1016/j.ijantimicag.2020.106144.
45.
Di Castelnuovo et al., Use of hydroxychloroquine in hospitalised COVID-19 patients is associated with reduced mortality: Findings from the observational multicentre Italian CORIST study, European Journal of Internal Medicine, doi:10.1016/j.ejim.2020.08.019.
46.
Alamdari et al., Mortality Risk Factors among Hospitalized COVID-19 Patients in a Major Referral Center in Iran, The Tohoku Journal of Experimental Medicine, doi:10.1620/tjem.252.73.
47.
Heberto et al., Implications of myocardial injury in Mexican hospitalized patients with coronavirus disease 2019 (COVID-19), IJC Heart & Vasculature, doi:10.1016/j.ijcha.2020.100638.
48.
Lauriola et al., Effect of combination therapy of hydroxychloroquine and azithromycin on mortality in COVID-19 patients, Clinical and Translational Science, doi:10.1111/cts.12860.
49.
Ashinyo et al., Clinical characteristics, treatment regimen and duration of hospitalization among COVID-19 patients in Ghana: a retrospective cohort study, Pan African Medical Journal, 37:1, doi:10.11604/pamj.supp.2020.37.1.25718.
50.
Shoaibi et al., Comparative Effectiveness of Famotidine in Hospitalized COVID-19 Patients, medRxiv, doi:10.1101/2020.09.23.20199463.
51.
Lammers et al., Early hydroxychloroquine but not chloroquine use reduces ICU admission in COVID-19 patients, International Journal of Infectious Diseases, doi:10.1016/j.ijid.2020.09.1460.
52.
Ayerbe et al., The association of treatment with hydroxychloroquine and hospital mortality in COVID-19 patients, Internal and Emergency Medicine, doi:10.1007/s11739-020-02505-x.
53.
Soto-Becerra et al., Real-World Effectiveness of hydroxychloroquine, azithromycin, and ivermectin among hospitalized COVID-19 patients: Results of a target trial emulation using observational data from a nationwide Healthcare System in Peru, medRxiv, doi:10.1101/2020.10.06.20208066.
54.
Aparisi et al., Low-density lipoprotein cholesterol levels are associated with poor clinical outcomes in COVID-19, medRxiv, doi:10.1101/2020.10.06.20207092.
55.
Ñamendys-Silva et al., Outcomes of patients with COVID-19 in the Intensive Care Unit in Mexico: A multicenter observational study, Heart & Lung, doi:10.1016/j.hrtlng.2020.10.013.
56.
Coll et al., Covid-19 in transplant recipients: the spanish experience, American Journal of Transplantation, doi:10.1111/ajt.16369.
57.
Frontera et al., Treatment with Zinc is Associated with Reduced In-Hospital Mortality Among COVID-19 Patients: A Multi-Center Cohort Study, Research Square, doi:10.21203/rs.3.rs-94509/v1.
58.
Niwas et al., Clinical outcome, viral response and safety profile of chloroquine in COVID-19 patients — initial experience, Advances in Respiratory Medicine, doi:10.5603/ARM.a2020.0139.
59.
López et al., Telemedicine follow-ups for COVID-19: experience in a tertiary hospital, Annals of Pediatrics, doi:10.1016/j.anpedi.2020.10.017.
60.
Núñez-Gil et al., Mortality risk assessment in Spain and Italy, insights of the HOPE COVID-19 registry, Internal and Emergency Medicine, doi:10.1007/s11739-020-02543-5.
61.
Sheshah et al., Prevalence of Diabetes, Management and Outcomes among Covid-19 Adult Patients Admitted in a Specialized Tertiary Hospital in Riyadh, Saudi Arabia, Diabetes Research and Clinical Practice, doi:10.1016/j.diabres.2020.108538.
62.
Boari et al., Prognostic factors and predictors of outcome in patients with COVID-19 and related pneumonia: a retrospective cohort study, Bioscience Reports, doi:10.1042/BSR20203455.
63.
Budhiraja et al., Clinical Profile of First 1000 COVID-19 Cases Admitted at Tertiary Care Hospitals and the Correlates of their Mortality: An Indian Experience, medRxiv, doi:10.1101/2020.11.16.20232223.
64.
Falcone et al., Role of low-molecular weight heparin in hospitalized patients with SARS-CoV-2 pneumonia: a prospective observational study, Open Forum Infectious Diseases, doi:10.1093/ofid/ofaa563.
65.
Burdick et al., Is Machine Learning a Better Way to IdentifyCOVID-19 Patients Who Might Benefit fromHydroxychloroquineTreatment?—The IDENTIFY Trial, Journal of Clinical Medicine, doi:10.3390/jcm9123834.
66.
van Halem et al., Risk factors for mortality in hospitalized patients with COVID-19 at the start of the pandemic in Belgium: a retrospective cohort study, BMC Infectious Diseases, doi:10.1186/s12879-020-05605-3.
67.
Modrák et al., Detailed disease progression of 213 patients hospitalized with Covid-19 in the Czech Republic: An exploratory analysis, medRxiv, doi:10.1101/2020.12.03.20239863.
68.
Johnston et al., Hydroxychloroquine with or Without Azithromycin for Treatment of Early SARS-CoV-2 Infection Among High-Risk Outpatient Adults: A Randomized Clinical Trial, eClinicalMedicine, doi:10.1016/j.eclinm.2021.100773.
69.
Tan et al., A retrospective comparison of drugs against COVID-19, Virus Research, doi:10.1016/j.virusres.2020.198262.
70.
Signes-Costa et al., Prevalence and 30-day mortality in hospitalized patients with COVID-19 and prior lung diseases, Archivos de Bronconeumología, doi:10.1016/j.arbres.2020.11.012.
71.
Cangiano et al., Mortality in an Italian nursing home during COVID-19 pandemic: correlation with gender, age, ADL, vitamin D supplementation, and limitations of the diagnostic tests, Aging, doi:10.18632/aging.202307.
72.
Taccone et al., The role of organizational characteristics on the outcome of COVID-19 patients admitted to the ICU in Belgium, The Lancet Regional Health - Europe, doi:10.1016/j.lanepe.2020.100019.
73.
Di Castelnuovo (B) et al., Disentangling the Association of Hydroxychloroquine Treatment with Mortality in Covid-19 Hospitalized Patients through Hierarchical Clustering, Journal of Healthcare Engineering, doi:10.1155/2021/5556207.
74.
Ouedraogo et al., Factors associated with the occurrence of acute respiratory distress and death in patients with COVID-19 in Burkina Faso, Revue des Maladies Respiratoires, doi:10.1016/j.rmr.2021.02.001.
75.
Purwati et al., A Randomized, Double-Blind, Multicenter Clinical Study Comparing the Efficacy and Safety of a Drug Combination of Lopinavir/Ritonavir-Azithromycin, Lopinavir/Ritonavir-Doxycycline, and Azithromycin-Hydroxychloroquine for Patients Diagnosed with Mild to Moderate COVID-19 Infections, Biochemistry Research International, doi:10.1155/2021/6685921.
76.
Lora-Tamayo et al., Early Lopinavir/ritonavir does not reduce mortality in COVID-19 patients: results of a large multicenter study, Journal of Infection, doi:10.1016/j.jinf.2021.02.011.
77.
Rubio-Sánchez et al., Prognostic factors for the severity of SARS-CoV-2 infection, Advances in Laboratory Medicine / Avances en Medicina de Laboratorio, doi:10.1515/almed-2021-0017.
78.
De Rosa et al., Risk Factors for Mortality in COVID-19 Hospitalized Patients in Piedmont, Italy: Results from the Multicenter, Regional, CORACLE Registry, Journal of Clinical Medicine, doi:10.3390/jcm10091951.
79.
Smith et al., Observational Study on 255 Mechanically Ventilated Covid Patients at the Beginning of the USA Pandemic, medRxiv, doi:10.1101/2021.05.28.21258012.
80.
Ramírez-García et al., Hydroxychloroquine and Tocilizumab in the Treatment of COVID-19: A Longitudinal Observational Study, Archivos de Medicina Universitaria, 3:1, digibug.ugr.es/handle/10481/69170.
81.
Lagier (B) et al., Outcomes of 2,111 COVID-19 hospitalised patients treated with 2 hydroxychloroquine/azithromycin and other regimens in Marseille, France: a 3 monocentric retrospective analysis, Therapeutics and Clinical Risk Management, doi:10.2147/TCRM.S364022.
82.
Taieb et al., Hydroxychloroquine and Azithromycin Treatment of Hospitalized Patients Infected with SARS-CoV-2 in Senegal from March to October 2020, Journal of Clinical Medicine, doi:10.3390/jcm10132954.
83.
AbdelGhaffar et al., Prediction of mortality in hospitalized Egyptian patients with Coronavirus disease-2019: A multicenter retrospective study, PLOS ONE, doi:10.1371/journal.pone.0262348.
84.
Lavilla Olleros et al., Use of glucocorticoids megadoses in SARS-CoV-2 infection in a spanish registry: SEMI-COVID-19, PLOS ONE, doi:10.1371/journal.pone.0261711.
85.
Omma et al., Hydroxychloroquine shortened hospital stay and reduced intensive care unit admissions in hospitalized COVID-19 patients, The Journal of Infection in Developing Countries, doi:10.3855/jidc.14933.
86.
Rouamba et al., Assessment of Recovery Time, Worsening and Death, among COVID-19 inpatients and outpatients, under treatment with Hydroxychloroquine or Chloroquine plus Azithromycin Combination in Burkina Faso, International Journal of Infectious Diseases, doi:10.1016/j.ijid.2022.02.034.
87.
Tsanovska et al., Hydroxychloroquine (HCQ) treatment for hospitalized patients with COVID-19, Infectious Disorders - Drug Targets, doi:10.2174/1871526522666220303121209.
88.
Azaña Gómez et al., Mortality risk factors in patients with SARS-CoV-2 infection and atrial fibrillation: Data from the SEMI-COVID-19 registry, Medicina Clínica, doi:10.1016/j.medcli.2022.01.008.
89.
Ebongue et al., Factors predicting in-hospital all-cause mortality in COVID 19 patients at the Laquintinie Hospital Douala, Cameroon, Travel Medicine and Infectious Disease, doi:10.1016/j.tmaid.2022.102292.
90.
Bowen et al., Reduction in risk of death among patients admitted with COVID-19 between first and second epidemic waves in New York City, Open Forum Infectious Diseases, doi:10.1093/ofid/ofac436.
91.
Núñez-Gil (B) et al., Hydroxychloroquine and Mortality in SARS-Cov-2 Infection; The HOPE- Covid-19 Registry., Anti-Infective Agents, doi:10.2174/2211352520666220514112951.
92.
Go et al., Hydroxychloroquine, azithromycin and methylprednisolone and in hospital survival in severe COVID-19 pneumonia, Frontiers in Pharmacology, doi:10.3389/fphar.2022.935370.
93.
Assad, H., Pharmacotherapy prescribing pattern and outcome for hospitalized patients with severe and critical COVID-19, Current Issues in Pharmacy and Medical Sciences, doi:10.2478/cipms-2022-0020.
94.
Bubenek-Turconi et al., Clinical characteristics and factors associated with ICU mortality during the first year of the SARS-Cov-2 pandemic in Romania, European Journal of Anaesthesiology, doi:10.1097/EJA.0000000000001776.
95.
Charif et al., Predictive Factors of Death and the Clinical Profile of Hospitalized Covid-19 Patients in Morocco: A One-Year Mixed Cohort Study, Cureus, doi:10.7759/cureus.32462.
96.
Delgado et al., Investigational medications in 9,638 hospitalized patients with severe COVID-19: lessons from the “fail-and-learn” strategy during the first two waves of the pandemic in 2020, Research Square, doi:10.21203/rs.3.rs-2596201/v1.
97.
Said et al., Profiles of Independent-Comorbidity Groups in Senior COVID-19 Patients Reveal Low Fatality Associated with Standard Care and Low-Dose Hydroxychloroquine over Antivirals, Journal of Multidisciplinary Healthcare, doi:10.2147/JMDH.S403700.
98.
AlQadheeb et al., Impact of common comorbidities on antimicrobial consumption and mortality amongst critically ill COVID-19 patients: A retrospective two center study in Saudi Arabia, Clinical Infection in Practice, doi:10.1016/j.clinpr.2023.100229.
99.
Yilgwan et al., Clinical profile and Predictors of Outcomes of Hospitalized Patients with Laboratory-Confirmed Severe Acute Respiratory Syndrome Coronavirus 2 in Nigeria: A Retrospective Analysis of 13 High Burden States in Nigeria, Nigerian Medical Journal, 64:2, nigerianmedjournal.org/index.php/nmj/article/view/174.
100.
Meeus et al., Efficacy and safety of in-hospital treatment of Covid-19 infection with low-dose hydroxychloroquine and azithromycin in hospitalized patients: A retrospective controlled cohort study, New Microbes and New Infections, doi:10.1016/j.nmni.2023.101172.
101.
Mehrizi et al., Drug prescription patterns and their association with mortality and hospitalization duration in COVID-19 patients: insights from big data, Frontiers in Public Health, doi:10.3389/fpubh.2023.1280434.
102.
AlShehhi et al., Utilizing machine learning for survival analysis to identify risk factors for COVID-19 intensive care unit admission: A retrospective cohort study from the United Arab Emirates, PLOS ONE, doi:10.1371/journal.pone.0291373.
103.
Brouqui et al., SARS-CoV 2 Viral Clearance in 1276 Patients: Associated Factors and the Role of Treatment with Hydroxychloroquine and Azithromycin, Acta Scientific Microbiology, doi:10.31080/ASMI.2024.07.1413.
104.
He et al., Clinical characteristics and risk factors for in-hospital mortality of COVID-19 patients in Hubei Province: A multicenter retrospective study, IJC Heart & Vasculature, doi:10.1016/j.ijcha.2024.101574.
105.
He (B) et al., Low dose of hydroxychloroquine is associated with reduced COVID-19 mortality: a multicenter study in China, Frontiers of Medicine, doi:10.1007/s11684-025-1123-9.
106.
Hobbs et al., The PRINCIPLE randomised controlled open label platform trial of hydroxychloroquine for treating COVID19 in community based patients at high risk, Scientific Reports, doi:10.1038/s41598-025-09275-6.
107.
Chatterjee et al., Healthcare workers & SARS-CoV-2 infection in India: A case-control investigation in the time of COVID-19, Indian Journal of Medical Research, doi:10.4103/ijmr.IJMR_2234_20.
108.
Bhattacharya et al., Pre exposure Hydroxychloroquine use is associated with reduced COVID19 risk in healthcare workers, medRxiv, doi:10.1101/2020.06.09.20116806.
109.
Huang (C) et al., Clinical characteristics of 17 patients with COVID-19 and systemic autoimmune diseases: a retrospective study, Annals of the Rheumatic Diseases, doi:10.1136/annrheumdis-2020-217425.
110.
Ferreira et al., Chronic treatment with hydroxychloroquine and SARS-CoV-2 infection, Journal of Medical Virology, doi:10.1002/jmv.26286.
111.
Zhong et al., COVID-19 in patients with rheumatic disease in Hubei province, China: a multicentre retrospective observational study, Lancent Rheumatology, doi:10.1016/S2665-9913(20)30227-7.
112.
Kadnur et al., Hydroxychloroquine pre-exposure prophylaxis for COVID-19 among healthcare workers: Initial experience from India, Journal of Family Medicine and Primary Care, doi:10.4103/jfmpc.jfmpc_1177_21.
113.
Khurana et al., Prevalence and clinical correlates of COVID-19 outbreak among healthcare workers in a tertiary level hospital, medRxiv, doi:10.1101/2020.07.21.20159301.
114.
Ferri et al., COVID-19 and rheumatic autoimmune systemic diseases: report of a large Italian patients series, Clinical Rheumatology, doi:10.1007/s10067-020-05334-7.
115.
Yadav et al., Sero-survey for health-care workers provides corroborative evidence for the effectiveness of Hydroxychloroquine prophylaxis against COVID-19 infection, ResearchGate, doi:10.13140/RG.2.2.34411.77603.
116.
Goenka et al., Seroprevalence of COVID-19 Amongst Health Care Workers in a Tertiary Care Hospital of a Metropolitan City from India, SSRN, doi:10.2139/ssrn.3689618.
117.
Mathai et al., Hydroxychloroquine as pre-exposure prophylaxis against COVID-19 in health-care workers: A single-center experience, Journal of Marine Medical Society, doi:10.4103/jmms.jmms_115_20.
118.
Strangfeld et al., Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 Global Rheumatology Alliance physician-reported registry, Annals of the Rheumatic Diseases, doi:10.1136/annrheumdis-2020-219498.
119.
Dev et al., Risk factors and frequency of COVID-19 among healthcare workers at a tertiary care centre in India: a case–control study, Transactions of The Royal Society of Tropical Medicine and Hygiene, doi:10.1093/trstmh/trab047.
120.
Seet et al., Positive impact of oral hydroxychloroquine and povidone-iodine throat spray for COVID-19 prophylaxis: an open-label randomized trial, International Journal of Infectious Diseases, doi:10.1016/j.ijid.2021.04.035.
121.
Alegiani et al., Risk of COVID-19 hospitalization and mortality in rheumatic patients treated with hydroxychloroquine or other conventional DMARDs in Italy, Rheumatology, doi:10.1093/rheumatology/keab348.
122.
Korkmaz et al., The effect of Hydroxychloroquine use due to rheumatic disease on the risk of Covid-19 infection and its course, Authorea, doi:10.22541/au.162257516.68665404/v1.
123.
Badyal et al., Hydroxychloroquine for SARS CoV2 Prophylaxis in Healthcare Workers – A Multicentric Cohort Study Assessing Effectiveness and Safety, Journal of the Association of Physicians of India, 69:6, June 2021, www.researchgate.net/publication/357700064_Hydroxychloroquine_for_SARS_CoV2_Prophylaxis_in_Healthcare_Workers_-_A_Multicentric_Cohort_Study_Assessing_Effectiveness_and_Safety.
124.
Shaw et al., COVID-19 in Individuals Treated With Long-Term Hydroxychloroquine: A Propensity Score-Matched Analysis of Cicatricial Alopecia Patients, Journal of Drugs in Dermatology, doi:10.36849/JDD.5843.
125.
McCullough et al., Hydroxychloroquine in the Prevention of COVID-19 Infection in Healthcare Workers, NCT04333225, clinicaltrials.gov/study/NCT04333225.
126.
Naggie et al., Hydroxychloroquine for pre-exposure prophylaxis of COVID-19 in health care workers: A randomized, multicenter, placebo-controlled trial (HERO-HCQ), International Journal of Infectious Diseases, doi:10.1016/j.ijid.2023.01.019.
127.
Fung et al., Effect of common maintenance drugs on the risk and severity of COVID-19 in elderly patients, PLoS ONE, doi:10.1371/journal.pone.0266922.
128.
Samajdar et al., Ivermectin and Hydroxychloroquine for Chemo-Prophylaxis of COVID-19: A Questionnaire Survey of Perception and Prescribing Practice of Physicians vis-a-vis Outcomes, Journal of the Association of Physicians India, 69:11, www.researchgate.net/publication/356294136_Ivermectin_and_Hydroxychloroquine_for_Chemo-Prophylaxis_of_COVID-19_A_Questionnaire_Survey_of_Perception_and_Prescribing_Practice_of_Physicians_vis-a-vis_Outcomes.
129.
Ugarte-Gil et al., Characteristics associated with poor COVID-19 outcomes in individuals with systemic lupus erythematosus: data from the COVID-19 Global Rheumatology Alliance, Annals of the Rheumatic Diseases, doi:10.1136/annrheumdis-2021-221636.
130.
MacFadden et al., Screening Large Population Health Databases for Potential COVID-19 Therapeutics: A Pharmacopeia-Wide Association Study (PWAS) of Commonly Prescribed Medications, Open Forum Infectious Diseases, doi:10.1093/ofid/ofac156.
131.
Satti et al., Characteristics and Obstetric Outcomes in Women With Autoimmune Rheumatic Disease During the COVID-19 Pandemic in Qatar, Cureus, doi:10.7759/cureus.24382.
132.
Yadav (B) et al., Hydroxychloroquine/chloroquine prophylaxis among health-care workers: Was it really preventive? – Evidence from a multicentric cross-sectional study, Indian Journal of Community Medicine, doi:10.4103/ijcm.ijcm_684_21.
133.
Patel et al., Factors Associated with COVID-19 Breakthrough Infection in the Pre-Omicron Era Among Vaccinated Patients with Rheumatic Diseases: A Cohort Study, medRxiv, doi:10.1101/2022.07.13.22277606.
134.
Becetti et al., Prevalence of coronavirus disease 2019 in a multiethnic cohort of patients with autoimmune rheumatic diseases in Qatar, Qatar Medical Journal, doi:10.5339/qmj.2022.37.
135.
Loucera et al., Real-world evidence with a retrospective cohort of 15,968 COVID-19 hospitalized patients suggests 21 new effective treatments, Virology Journal, doi:10.1186/s12985-023-02195-9.
136.
Sahebari et al., Influence of biologic and conventional disease-modifying antirheumatic drugs on COVID-19 incidence among rheumatic patients during the first and second wave of the pandemic in Iran, Reumatologia/Rheumatology, doi:10.5114/reum.2022.119039.
137.
Obrișcă et al., Characteristics of SARS-CoV-2 Infection in an Actively Monitored Cohort of Patients with Lupus Nephritis, Biomedicines, doi:10.3390/biomedicines10102423.
138.
Isnardi et al., Sociodemographic and clinical factors associated with poor COVID-19 outcomes in patients with rheumatic diseases: data from the SAR-COVID Registry, Clinical Rheumatology, doi:10.1007/s10067-022-06393-8.
139.
Nasri et al., Efficacy of hydroxychloroquine in pre-exposure severe acute respiratory syndrome coronavirus 2 prophylaxis among high-risk healthcare workers: A multicenter study, Advanced Biomedical Research, doi:10.4103/abr.abr_104_21.
140.
Finkelstein et al., The Efficacy of Long-Term Hydroxychloroquine Use in the Prevention of COVID-19: A Retrospective Cohort Study, Studies in Health Technology and Informatics, doi:10.3233/SHTI230489.
141.
Scirocco et al., COVID-19 prognosis in systemic lupus erythematosus compared with rheumatoid arthritis and spondyloarthritis: results from the CONTROL-19 Study by the Italian Society for Rheumatology, Lupus Science & Medicine, doi:10.1136/lupus-2023-000945.
142.
Salesi et al., Clinical signs, symptoms, and severity of COVID-19 in patients with rheumatic diseases during the COVID-19 epidemic, Immunopathologia Persa, doi:10.34172/ipp.2023.40568.
143.
Chouhdari et al., The prophylactic effect of hydroxychloroquine on the severity of COVID-19 infection in an asymptomatic population: A randomized clinical trial, Social Determinants of Health, doi:10.22037/sdh.v10i1.43032.
144.
Schilling et al., Evaluation of hydroxychloroquine or chloroquine for the prevention of COVID-19 (COPCOV): A double-blind, randomised, placebo-controlled trial, PLOS Medicine, doi:10.1371/journal.pmed.1004428.
145.
Patel (B) et al., Patients with systemic autoimmune rheumatic diseases remain at risk for hospitalisation for COVID-19 infection in the Omicron era (2022–2024): a retrospective cohort study, RMD Open, doi:10.1136/rmdopen-2024-005114.
146.
Polat et al., Hydroxychloroquine Use on Healthcare Workers Exposed to COVID-19 - A Pandemic Hospital Experience, Medical Journal of Bakirkoy, 16:3, 280-6, doi:10.5222/BMJ.2020.50469.
Souza-Silva et al., 30 Sep 2023, retrospective, Brazil, peer-reviewed, median age 60.0, 29 authors, study period March 2020 - September 2020.
Contact: dani_nunesp@hotmail.com.
Dados de Vida Real sobre o Uso da Hidroxicloroquina ou da Cloroquina Combinadas ou Não à Azitromicina em Pacientes com Covid-19: Uma Análise Retrospectiva no Brasil
Arquivos Brasileiros de Cardiologia, doi:10.36660/abc.20220935
Background: Despite no evidence showing benefits of hydroxychloroquine and chloroquine with or without azithromycin for COVID-19 treatment, these medications have been largely prescribed in Brazil. Objectives: To assess outcomes, including in-hospital mortality, electrocardiographic abnormalities, hospital length-of-stay, admission to the intensive care unit, and need for dialysis and mechanical ventilation, in hospitalized COVID-19 patients who received chloroquine or hydroxychloroquine, and to compare outcomes between those patients and their matched controls. Methods: A retrospective multicenter cohort study that included consecutive laboratory-confirmed COVID-19 patients from 37 Brazilian hospitals from March to September 2020. Propensity score was used to select matching controls by age, sex, cardiovascular comorbidities, and in-hospital use of corticosteroid. A p-value <0.05 was considered statistically significant. Results: From 7,850 COVID-19 patients, 673 (8.6%) received hydroxychloroquine and 67 (0.9%) chloroquine. The median age in the study group was 60 years (46 -71) and 59.1% were women. During hospitalization, 3.2% of patients presented side effects and 2.2% required therapy discontinuation. Electrocardiographic abnormalities were more prevalent in the chloroquine/hydroxychloroquine group (13.2% vs. 8.2%, p=0.01), and the long corrected QT interval was the main difference (3.6% vs. 0.4%, p<0.001). The median hospital length of stay was longer in the HCQ/CQ + AZT group than in controls (9.0 [5.0, 18.0] vs. 8.0 [4.0, 14.0] days). There was no statistical differences between groups in intensive care unit admission (35.1% vs. 32.0%; p=0.282), invasive mechanical ventilation support (27.0% vs. 22.3%; p=0.074) or mortality (18.9% vs. 18.0%; p=0.682). Conclusion: COVID-19 patients treated with chloroquine or hydroxychloroquine had a longer hospital length of stay, when compared to matched controls. Intensive care unit admission, invasive mechanical ventilation, dialysis and inhospital mortality were similar.
Potential conflict of interest No potential conflict of interest relevant to this article was reported.
Sources of funding
Study association This study is not associated with any thesis or dissertation work.
Ethics approval and consent to participate This study was approved by the Comitê Nacional de Ética em Pesquisa under the protocol number CAAE 30350820.5.1001.0008. All the procedures in this study were in accordance with the 1975 Helsinki Declaration, updated in 2013.
References
Axfors, Schmitt, Janiaud, Van't Hooft, Abd-Elsalam et al., Mortality Outcomes with Hydroxychloroquine and Chloroquine in COVID-19 from an International Collaborative Meta-Analysis of Randomized Trials, Nat Commun, doi:10.1038/s41467-021-22446-z
Brasil, Fundamentação e decisão Acerca das Diretrizes Terapêuticas para o Tratamento Farmacológico da COVID-19 (Hospitalar e Ambulatorial)
Cavalcanti, Zampieri, Rosa, Azevedo, Veiga et al., Hydroxychloroquine with or without Azithromycin in Mildto-Moderate Covid-19, N Engl J Med, doi:10.1056/NEJMoa2019014
Chi, Montazerin, Lee, Kazmi, Shojaei et al., Effect of Azithromycin and Hydroxychloroquine in Patients Hospitalized with COVID-19: Network Meta-Analysis of Randomized Controlled Trials, J Med Virol, doi:10.1002/jmv.27259
Chivese, Musa, Hindy, Al-Wattary, Badran et al., Efficacy of Chloroquine and Hydroxychloroquine in Treating COVID-19 Infection: A Meta-Review of Systematic Reviews and an Updated Meta-Analysis, Travel Med Infect Dis, doi:10.1016/j.tmaid.2021.102135
Diaz-Arocutipa, Brañez-Condorena, Hernandez, QTc Prolongation in COVID-19 Patients Treated with Hydroxychloroquine, Chloroquine, Azithromycin, or Lopinavir/Ritonavir: A Systematic Review and Meta-Analysis, Pharmacoepidemiol Drug Saf, doi:10.1002/pds.5234
Elavarasi, Prasad, Seth, Sahoo, Madan et al., Chloroquine and Hydroxychloroquine for the Treatment of COVID-19: a Systematic Review and Meta-analysis, J Gen Intern Med, doi:10.1007/s11606-020-06146-w
Ferreira, Beranger, Sampaio, Mansur, Filho et al., Outcomes Associated with Hydroxychloroquine and Ivermectin in Hospitalized Patients with COVID-19: A Single-Center Experience, Rev Assoc Med Bras, doi:10.1590/1806-9282.20210661
Fiolet, Guihur, Rebeaud, Mulot, Peiffer-Smadja et al., Effect of Hydroxychloroquine with or Without Azithromycin on the Mortality of Coronavirus Disease 2019 (COVID-19) Patients: A Systematic Review and Meta-Analysis, Clin Microbiol Infect, doi:10.1016/j.cmi.2020.08.022
Ghazy, Almaghraby, Shaaban, Kamal, Beshir et al., A Systematic Review and Meta-Analysis on Chloroquine and Hydroxychloroquine as Monotherapy or Combined with Azithromycin in COVID-19 Treatment, Sci Rep, doi:10.1038/s41598-020-77748-x
Group; Horby, Mafham, Linsell, Bell, Staplin, Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19, N Engl J Med, doi:10.1056/NEJMoa2022926
Harris, Taylor, Minor, Elliott, Fernandez et al., The REDCap Consortium: Building an International Community of Software Platform Partners, J Biomed Inform, doi:10.1016/j.jbi.2019.103208
I B Á Ñ E Z S , M A R T Í N E Z O, Va l e n z u e l a F, S i l v a F, Va l e n z u e l a O. Hydroxychloroquine and Chloroquine in COVID-19: Should They be Used as Standard Therapy?, Clin Rheumatol, doi:10.1007/s10067-020-05202-4
Kashour, Riaz, Garbati, Aldosary, Tlayjeh et al., Efficacy of Chloroquine or Hydroxychloroquine in COVID-19 Patients: A Systematic Review and Meta-Analysis, J Antimicrob Chemother, doi:10.1093/jac/dkaa403
Marcolino, Figueira, Santos, Cardoso, Ribeiro et al., The Experience of a Sustainable Large Scale Brazilian Telehealth Network, Telemed J E Health, doi:10.1089/tmj.2015.0234
Marcolino, Ziegelmann, Souza-Silva, Nascimento, Oliveira et al., Clinical Characteristics and Outcomes of Patients Hospitalized with COVID-19 in Brazil: Results from the Brazilian COVID-19 Registry, Int J Infect Dis, doi:10.1016/j.ijid.2021.01.019
Mgt, Bicalho, Nogueira, Guimarães-Júnior, Aguiar et al., This is an open-access article distributed under the terms of the Creative Commons Attribution License *Supplemental Materials For additional information
Nascimento, Paixão, Tonaco, Alves, Peixoto et al., Clinical and Electrocardiographic Outcomes Evaluated by Telemedicine of Outpatients with Clinical Suspicion of COVID-19 Treated with Chloroquine Compounds in Brazil †, Front Cardiovasc Med, doi:10.3389/fcvm.2023.1028398
Pan, Peto, Henao-Restrepo, Preziosi, Sathiyamoorthy, Repurposed Antiviral Drugs for Covid-19 -Interim WHO Solidarity Trial Results, N Engl J Med, doi:10.1056/NEJMoa2023184
Rosa, Cavalcanti, Azevedo, Veiga, Souza et al., Association between Acute Disease Severity and One-Year Quality of Life among Post-Hospitalisation COVID-19 Patients: Coalition VII Prospective Cohort Study, Intensive Care Med, doi:10.1007/s00134-022-06953-1
Satarker, Ahuja, Banerjee, Balaji, Dogra et al., Hydroxychloroquine in COVID-19: Potential Mechanism of Action Against SARS-CoV-2, Curr Pharmacol Rep, doi:10.1007/s40495-020-00231-8
Von Elm, Altman, Egger, Pocock, Gøtzsche et al., Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies, BMJ, doi:10.1136/bmj.39335.541782
DOI record:
{
"DOI": "10.36660/abc.20220935",
"ISSN": [
"0066-782X",
"1678-4170"
],
"URL": "http://dx.doi.org/10.36660/abc.20220935",
"alternative-id": [
"10.36660/abc.20220935"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0003-2079-7291",
"affiliation": [],
"authenticated-orcid": false,
"family": "Souza-Silva",
"given": "Maíra Viana Rego",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-3124-9322",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pereira",
"given": "Daniella Nunes",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3312-4002",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pires",
"given": "Magda Carvalho",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-4342-7958",
"affiliation": [],
"authenticated-orcid": false,
"family": "Vasconcelos",
"given": "Isabela Muzzi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5535-6288",
"affiliation": [],
"authenticated-orcid": false,
"family": "Schwarzbold",
"given": "Alexandre Vargas",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8605-2121",
"affiliation": [],
"authenticated-orcid": false,
"family": "Vasconcelos",
"given": "Diego Henrique de",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-1178-669X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Pereira",
"given": "Elayne Crestani",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1592-4727",
"affiliation": [],
"authenticated-orcid": false,
"family": "Manenti",
"given": "Euler Roberto Fernandes",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9923-236X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Costa",
"given": "Felício Roberto",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8277-2631",
"affiliation": [],
"authenticated-orcid": false,
"family": "Aguiar",
"given": "Filipe Carrilho de",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2657-5406",
"affiliation": [],
"authenticated-orcid": false,
"family": "Anschau",
"given": "Fernando",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9696-4685",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bartolazzi",
"given": "Frederico",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-9064-7067",
"affiliation": [],
"authenticated-orcid": false,
"family": "Nascimento",
"given": "Guilherme Fagundes",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1144-6262",
"affiliation": [],
"authenticated-orcid": false,
"family": "Vianna",
"given": "Heloisa Reniers",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3703-2845",
"affiliation": [],
"authenticated-orcid": false,
"family": "Batista",
"given": "Joanna d’Arc Lyra",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3984-4959",
"affiliation": [],
"authenticated-orcid": false,
"family": "Machado-Rugolo",
"given": "Juliana",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6362-1889",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ruschel",
"given": "Karen Brasil",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0961-524X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ferreira",
"given": "Maria Angélica Pires",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1575-6559",
"affiliation": [],
"authenticated-orcid": false,
"family": "Oliveira",
"given": "Leonardo Seixas de",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-6621-3338",
"affiliation": [],
"authenticated-orcid": false,
"family": "Menezes",
"given": "Luanna Silva Monteiro",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2851-2011",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ziegelmann",
"given": "Patricia Klarmann",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2738-0747",
"affiliation": [],
"authenticated-orcid": false,
"family": "Tofani",
"given": "Marcela Gonçalves Trindade",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6298-9377",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bicalho",
"given": "Maria Aparecida Camargos",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-0241-9046",
"affiliation": [],
"authenticated-orcid": false,
"family": "Nogueira",
"given": "Matheus Carvalho Alves",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2127-8015",
"affiliation": [],
"authenticated-orcid": false,
"family": "Guimarães-Júnior",
"given": "Milton Henriques",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-3138-7717",
"affiliation": [],
"authenticated-orcid": false,
"family": "Aguiar",
"given": "Rúbia Laura Oliveira",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6377-241X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Rios",
"given": "Danyelle Romana Alves",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2447-2577",
"affiliation": [],
"authenticated-orcid": false,
"family": "Polanczyk",
"given": "Carisi Anne",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4278-3771",
"affiliation": [],
"authenticated-orcid": false,
"family": "Marcolino",
"given": "Milena Soriano",
"sequence": "additional"
}
],
"container-title": "Arquivos Brasileiros de Cardiologia",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
10,
4
]
],
"date-time": "2023-10-04T11:41:18Z",
"timestamp": 1696419678000
},
"deposited": {
"date-parts": [
[
2023,
10,
4
]
],
"date-time": "2023-10-04T11:41:38Z",
"timestamp": 1696419698000
},
"indexed": {
"date-parts": [
[
2023,
10,
5
]
],
"date-time": "2023-10-05T11:17:06Z",
"timestamp": 1696504626370
},
"is-referenced-by-count": 0,
"issue": "9",
"issued": {
"date-parts": [
[
2023,
9
]
]
},
"journal-issue": {
"issue": "9",
"published-print": {
"date-parts": [
[
2023,
10,
3
]
]
}
},
"language": "en",
"member": "22636",
"original-title": [],
"prefix": "10.36660",
"published": {
"date-parts": [
[
2023,
9
]
]
},
"published-print": {
"date-parts": [
[
2023,
10,
3
]
]
},
"publisher": "Sociedade Brasileira de Cardiologia",
"reference": [
{
"DOI": "10.1007/s40495-020-00231-8",
"article-title": "Hydroxychloroquine in COVID-19: Potential Mechanism of Action Against SARS-CoV-2",
"author": "Satarker",
"doi-asserted-by": "crossref",
"first-page": "203",
"issue": "5",
"journal-title": "Curr Pharmacol Rep",
"key": "key20231004074113_B1",
"unstructured": "1. Satarker S, Ahuja T, Banerjee M, Balaji V, Dogra S, Agarwal T, et al. Hydroxychloroquine in COVID-19: Potential Mechanism of Action Against SARS-CoV-2. Curr Pharmacol Rep. 2020;6(5):203-11. doi: 10.1007/s40495-020-00231-8.",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1007/s10067-020-05202-4",
"article-title": "Hydroxychloroquine and Chloroquine in COVID-19: Should They be Used as Standard Therapy?",
"author": "Ibáñez",
"doi-asserted-by": "crossref",
"first-page": "2461",
"issue": "8",
"journal-title": "Clin Rheumatol",
"key": "key20231004074113_B2",
"unstructured": "2. Ibáñez S, Martínez O, Valenzuela F, Silva F, Valenzuela O. Hydroxychloroquine and Chloroquine in COVID-19: Should They be Used as Standard Therapy? Clin Rheumatol. 2020;39(8):2461-65. doi: 10.1007/s10067-020-05202-4.",
"volume": "39",
"year": "2020"
},
{
"DOI": "10.1007/s11606-020-06146-w",
"article-title": "Chloroquine and Hydroxychloroquine for the Treatment of COVID-19: a Systematic Review and Meta-analysis",
"author": "Elavarasi",
"doi-asserted-by": "crossref",
"first-page": "3308",
"issue": "11",
"journal-title": "J Gen Intern Med",
"key": "key20231004074113_B3",
"unstructured": "3. Elavarasi A, Prasad M, Seth T, Sahoo RK, Madan K, Nischal N, et al. Chloroquine and Hydroxychloroquine for the Treatment of COVID-19: a Systematic Review and Meta-analysis. J Gen Intern Med. 2020;35(11):3308-14. doi: 10.1007/s11606-020-06146-w.",
"volume": "35",
"year": "2020"
},
{
"DOI": "10.1093/jac/dkaa403",
"article-title": "Efficacy of Chloroquine or Hydroxychloroquine in COVID-19 Patients: A Systematic Review and Meta-Analysis",
"author": "Kashour",
"doi-asserted-by": "crossref",
"first-page": "30",
"issue": "1",
"journal-title": "J Antimicrob Chemother",
"key": "key20231004074113_B4",
"unstructured": "4. Kashour Z, Riaz M, Garbati MA, AlDosary O, Tlayjeh H, Gerberi D, et al. Efficacy of Chloroquine or Hydroxychloroquine in COVID-19 Patients: A Systematic Review and Meta-Analysis. J Antimicrob Chemother. 2021;76(1):30-42. doi: 10.1093/jac/dkaa403.",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2022926",
"article-title": "Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19",
"author": "RECOVERY Collaborative Group",
"doi-asserted-by": "crossref",
"first-page": "2030",
"issue": "21",
"journal-title": "N Engl J Med",
"key": "key20231004074113_B5",
"unstructured": "5. RECOVERY Collaborative Group; Horby P, Mafham M, Linsell L, Bell JL, Staplin N, et al. Effect of Hydroxychloroquine in Hospitalized Patients with Covid-19. N Engl J Med. 2020;383(21):2030-40. doi: 10.1056/NEJMoa2022926.",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2023184",
"article-title": "Repurposed Antiviral Drugs for Covid-19 - Interim WHO Solidarity Trial Results",
"author": "WHO Solidarity Trial Consortium",
"doi-asserted-by": "crossref",
"first-page": "497",
"issue": "6",
"journal-title": "N Engl J Med",
"key": "key20231004074113_B6",
"unstructured": "6. WHO Solidarity Trial Consortium; Pan H, Peto R, Henao-Restrepo AM, Preziosi MP, Sathiyamoorthy V, et al. Repurposed Antiviral Drugs for Covid-19 - Interim WHO Solidarity Trial Results. N Engl J Med. 2021;384(6):497-511. doi: 10.1056/NEJMoa2023184.",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.1038/s41598-020-77748-x",
"article-title": "A Systematic Review and Meta-Analysis on Chloroquine and Hydroxychloroquine as Monotherapy or Combined with Azithromycin in COVID-19 Treatment",
"author": "Ghazy",
"doi-asserted-by": "crossref",
"issue": "1",
"journal-title": "Sci Rep",
"key": "key20231004074113_B7",
"unstructured": "7. Ghazy RM, Almaghraby A, Shaaban R, Kamal A, Beshir H, Moursi A, et al. A Systematic Review and Meta-Analysis on Chloroquine and Hydroxychloroquine as Monotherapy or Combined with Azithromycin in COVID-19 Treatment. Sci Rep. 2020;10(1):22139. doi: 10.1038/s41598-020-77748-x.",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1002/jmv.27259",
"article-title": "Effect of Azithromycin and Hydroxychloroquine in Patients Hospitalized with COVID-19: Network Meta-Analysis of Randomized Controlled Trials",
"author": "Chi",
"doi-asserted-by": "crossref",
"first-page": "6737",
"issue": "12",
"journal-title": "J Med Virol",
"key": "key20231004074113_B8",
"unstructured": "8. Chi G, Montazerin SM, Lee JJ, Kazmi SHA, Shojaei F, Fitzgerald C, et al. Effect of Azithromycin and Hydroxychloroquine in Patients Hospitalized with COVID-19: Network Meta-Analysis of Randomized Controlled Trials. J Med Virol. 2021;93(12):6737-49. doi: 10.1002/jmv.27259.",
"volume": "93",
"year": "2021"
},
{
"author": "Brasil",
"journal-title": "Fundamentação e decisão Acerca das Diretrizes Terapêuticas para o Tratamento Farmacológico da COVID-19 (Hospitalar e Ambulatorial). Conitec",
"key": "key20231004074113_B9",
"unstructured": "9. Brasil. Ministério da Saúde. Fundamentação e decisão Acerca das Diretrizes Terapêuticas para o Tratamento Farmacológico da COVID-19 (Hospitalar e Ambulatorial). Conitec [Internet]. Brasília: Ministério da Saúde; 2022 [cited 2023 Aug 17]. Available from: http://conitec.gov.br/images/Audiencias_Publicas/Nota_tecnica_n2_2022_SCTIE-MS.pdf.",
"year": "2022"
},
{
"DOI": "10.1016/j.ijid.2021.01.019",
"article-title": "Clinical Characteristics and Outcomes of Patients Hospitalized with COVID-19 in Brazil: Results from the Brazilian COVID-19 Registry",
"author": "Marcolino",
"doi-asserted-by": "crossref",
"first-page": "300",
"journal-title": "Int J Infect Dis",
"key": "key20231004074113_B10",
"unstructured": "10. Marcolino MS, Ziegelmann PK, Souza-Silva MVR, Nascimento IJB, Oliveira LM, Monteiro LS, et al. Clinical Characteristics and Outcomes of Patients Hospitalized with COVID-19 in Brazil: Results from the Brazilian COVID-19 Registry. Int J Infect Dis. 2021;107:300-10. doi: 10.1016/j.ijid.2021.01.019.",
"volume": "107",
"year": "2021"
},
{
"author": "World Health Organization",
"journal-title": "Diagnostic testing for SARS-CoV-2",
"key": "key20231004074113_B11",
"unstructured": "11. World Health Organization. Diagnostic testing for SARS-CoV-2 [Internet]. Geneva: WHO; 2020 [cited 2023 Aug 17]. Available from: https://www.who.int/publications/i/item/diagnostic-testing-for-sars-cov-2.",
"year": "2020"
},
{
"DOI": "10.1136/bmj.39335.541782.AD",
"article-title": "Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies",
"author": "von Elm",
"doi-asserted-by": "crossref",
"first-page": "806",
"issue": "7624",
"journal-title": "BMJ",
"key": "key20231004074113_B12",
"unstructured": "12. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. BMJ. 2007;335(7624):806-8. doi: 10.1136/bmj.39335.541782.AD.",
"volume": "335",
"year": "2007"
},
{
"DOI": "10.1016/j.jbi.2019.103208",
"article-title": "The REDCap Consortium: Building an International Community of Software Platform Partners",
"author": "Harris",
"doi-asserted-by": "crossref",
"journal-title": "J Biomed Inform",
"key": "key20231004074113_B13",
"unstructured": "13. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208.",
"volume": "95",
"year": "2019"
},
{
"DOI": "10.1089/tmj.2015.0234",
"article-title": "The Experience of a Sustainable Large Scale Brazilian Telehealth Network",
"author": "Marcolino",
"doi-asserted-by": "crossref",
"first-page": "899",
"issue": "11",
"journal-title": "Telemed J E Health",
"key": "key20231004074113_B14",
"unstructured": "14. Marcolino MS, Figueira RM, Santos JPA, Cardoso CS, Ribeiro ALP, Alkmim MB. The Experience of a Sustainable Large Scale Brazilian Telehealth Network. Telemed J E Health. 2016;22(11):899-908. doi: 10.1089/tmj.2015.0234.",
"volume": "22",
"year": "2016"
},
{
"DOI": "10.1002/pds.5234",
"article-title": "QTc Prolongation in COVID-19 Patients Treated with Hydroxychloroquine, Chloroquine, Azithromycin, or Lopinavir/Ritonavir: A Systematic Review and Meta-Analysis",
"author": "Diaz-Arocutipa",
"doi-asserted-by": "crossref",
"first-page": "694",
"issue": "6",
"journal-title": "Pharmacoepidemiol Drug Saf",
"key": "key20231004074113_B15",
"unstructured": "15. Diaz-Arocutipa C, Brañez-Condorena A, Hernandez AV. QTc Prolongation in COVID-19 Patients Treated with Hydroxychloroquine, Chloroquine, Azithromycin, or Lopinavir/Ritonavir: A Systematic Review and Meta-Analysis. Pharmacoepidemiol Drug Saf. 2021;30(6):694-706. doi: 10.1002/pds.5234.",
"volume": "30",
"year": "2021"
},
{
"DOI": "10.1016/j.cmi.2020.08.022",
"article-title": "Effect of Hydroxychloroquine with or Without Azithromycin on the Mortality of Coronavirus Disease 2019 (COVID-19) Patients: A Systematic Review and Meta-Analysis",
"author": "Fiolet",
"doi-asserted-by": "crossref",
"first-page": "19",
"issue": "1",
"journal-title": "Clin Microbiol Infect",
"key": "key20231004074113_B16",
"unstructured": "16. Fiolet T, Guihur A, Rebeaud ME, Mulot M, Peiffer-Smadja N, Mahamat-Saleh Y. Effect of Hydroxychloroquine with or Without Azithromycin on the Mortality of Coronavirus Disease 2019 (COVID-19) Patients: A Systematic Review and Meta-Analysis. Clin Microbiol Infect. 2021;27(1):19-27. doi: 10.1016/j.cmi.2020.08.022.",
"volume": "27",
"year": "2021"
},
{
"DOI": "10.1016/j.tmaid.2021.102135",
"article-title": "Efficacy of Chloroquine and Hydroxychloroquine in Treating COVID-19 Infection: A Meta-Review of Systematic Reviews and an Updated Meta-Analysis",
"author": "Chivese",
"doi-asserted-by": "crossref",
"journal-title": "Travel Med Infect Dis",
"key": "key20231004074113_B17",
"unstructured": "17. Chivese T, Musa OAH, Hindy G, Al-Wattary N, Badran S, Soliman N, et al. Efficacy of Chloroquine and Hydroxychloroquine in Treating COVID-19 Infection: A Meta-Review of Systematic Reviews and an Updated Meta-Analysis. Travel Med Infect Dis. 2021;43:102135. doi: 10.1016/j.tmaid.2021.102135.",
"volume": "43",
"year": "2021"
},
{
"article-title": "Mortality Outcomes with Hydroxychloroquine and Chloroquine in COVID-19 from an International Collaborative Meta-Analysis of Randomized Trials",
"author": "Axfors",
"issue": "1",
"journal-title": "Nat Commun",
"key": "key20231004074113_B18",
"unstructured": "18. Axfors C, Schmitt AM, Janiaud P, Van’t Hooft J, Abd-Elsalam S, Abdo EF, et al. Mortality Outcomes with Hydroxychloroquine and Chloroquine in COVID-19 from an International Collaborative Meta-Analysis of Randomized Trials. Nat Commun. 2021;12(1):2349. doi: 10.1038/s41467-021-22446-z.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1056/NEJMoa2019014",
"article-title": "Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19",
"author": "Cavalcanti",
"doi-asserted-by": "crossref",
"first-page": "2041",
"issue": "21",
"journal-title": "N Engl J Med",
"key": "key20231004074113_B19",
"unstructured": "19. Cavalcanti AB, Zampieri FG, Rosa RG, Azevedo LCP, Veiga VC, Avezum A, et al. Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19. N Engl J Med. 2020;383(21):2041-52. doi: 10.1056/NEJMoa2019014.",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.3389/fcvm.2023.1028398",
"article-title": "Clinical and Electrocardiographic Outcomes Evaluated by Telemedicine of Outpatients with Clinical Suspicion of COVID-19 Treated with Chloroquine Compounds in Brazil†",
"author": "Nascimento",
"doi-asserted-by": "crossref",
"journal-title": "Front Cardiovasc Med",
"key": "key20231004074113_B20",
"unstructured": "20. Nascimento BR, Paixão GMM, Tonaco LAB, Alves ACD, Peixoto DC, Ribeiro LB, et al. Clinical and Electrocardiographic Outcomes Evaluated by Telemedicine of Outpatients with Clinical Suspicion of COVID-19 Treated with Chloroquine Compounds in Brazil†. Front Cardiovasc Med. 2023;10:1028398. doi: 10.3389/fcvm.2023.1028398.",
"volume": "10",
"year": "2023"
},
{
"DOI": "10.1590/1806-9282.20210661",
"article-title": "Outcomes Associated with Hydroxychloroquine and Ivermectin in Hospitalized Patients with COVID-19: A Single-Center Experience",
"author": "Ferreira",
"doi-asserted-by": "crossref",
"first-page": "1466",
"issue": "10",
"journal-title": "Rev Assoc Med Bras",
"key": "key20231004074113_B21",
"unstructured": "21. Ferreira RM, Beranger RW, Sampaio PPN, Mansur J Filho, Lima RAC. Outcomes Associated with Hydroxychloroquine and Ivermectin in Hospitalized Patients with COVID-19: A Single-Center Experience. Rev Assoc Med Bras. 2021;67(10):1466-71. doi: 10.1590/1806-9282.20210661.",
"volume": "67",
"year": "2021"
},
{
"DOI": "10.1007/s00134-022-06953-1",
"article-title": "Association between Acute Disease Severity and One-Year Quality of Life among Post-Hospitalisation COVID-19 Patients: Coalition VII Prospective Cohort Study",
"author": "Rosa",
"doi-asserted-by": "crossref",
"first-page": "166",
"issue": "2",
"journal-title": "Intensive Care Med",
"key": "key20231004074113_B22",
"unstructured": "22. Rosa RG, Cavalcanti AB, Azevedo LCP, Veiga VC, Souza D, Santos RDRM, et al. Association between Acute Disease Severity and One-Year Quality of Life among Post-Hospitalisation COVID-19 Patients: Coalition VII Prospective Cohort Study. Intensive Care Med. 2023;49(2):166-77. doi: 10.1007/s00134-022-06953-1.",
"volume": "49",
"year": "2023"
}
],
"reference-count": 22,
"references-count": 22,
"relation": {},
"resource": {
"primary": {
"URL": "https://abccardiol.org/article/dados-de-vida-real-sobre-o-uso-da-hidroxicloroquina-ou-da-cloroquina-combinadas-ou-nao-a-azitromicina-em-pacientes-com-covid-19-uma-analise-retrospectiva-no-brasil/"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cardiology and Cardiovascular Medicine"
],
"subtitle": [],
"title": "Dados de Vida Real sobre o Uso da Hidroxicloroquina ou da Cloroquina Combinadas ou Não à Azitromicina em Pacientes com Covid-19: Uma Análise Retrospectiva no Brasil",
"type": "journal-article",
"volume": "120"
}
