Clinical signs, symptoms, and severity of COVID-19 in patients with rheumatic diseases during the COVID-19 epidemic
et al., Immunopathologia Persa, doi:10.34172/ipp.2023.40568, Dec 2023
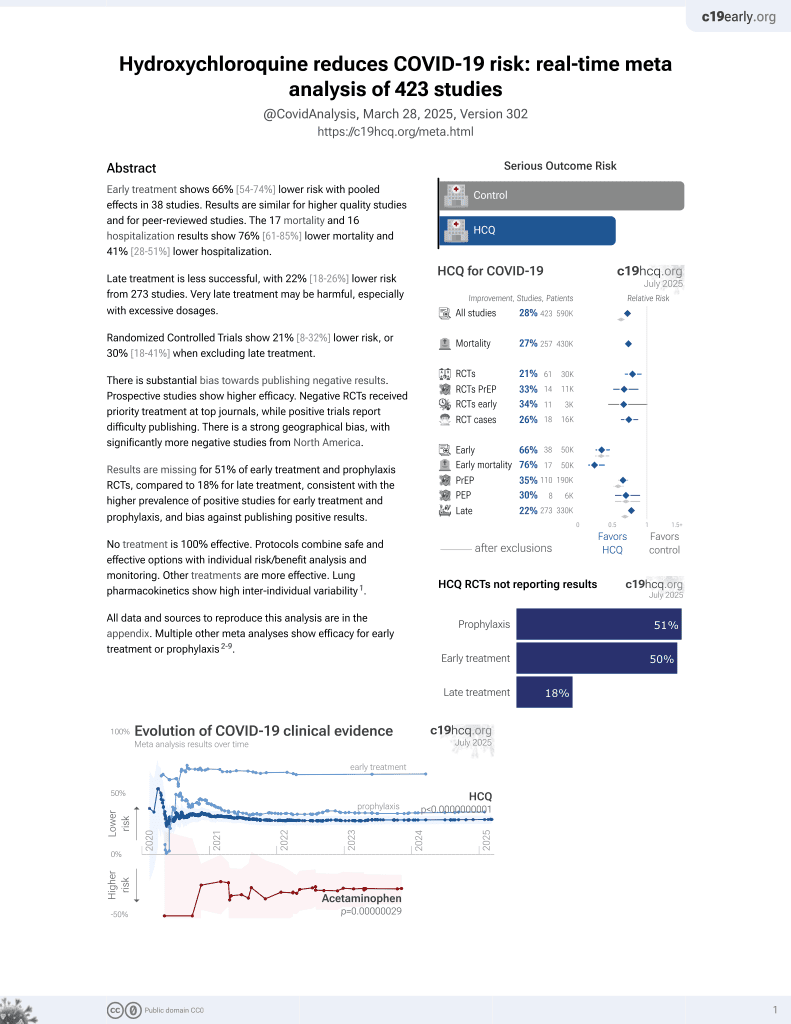
HCQ for COVID-19
1st treatment shown to reduce risk in
March 2020, now with p < 0.00000000001 from 424 studies, used in 59 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective study of 77 outpatients with rheumatic diseases diagnosed with COVID-19, showing lower risk of severe COVID-19 with HCQ use in unadjusted results.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with no group details.
|
risk of severe case, 85.0% lower, RR 0.15, p = 0.003, treatment 2 of 44 (4.5%), control 10 of 33 (30.3%), NNT 3.9.
|
|
risk of moderate/severe case, 18.2% lower, RR 0.82, p = 0.35, treatment 24 of 44 (54.5%), control 22 of 33 (66.7%), NNT 8.2.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Salesi et al., 18 Dec 2023, retrospective, Iran, peer-reviewed, 2 authors.
Clinical signs, symptoms, and severity of COVID-19 in patients with rheumatic diseases during the COVID-19 epidemic
doi:10.34172/ipp.2023.40568
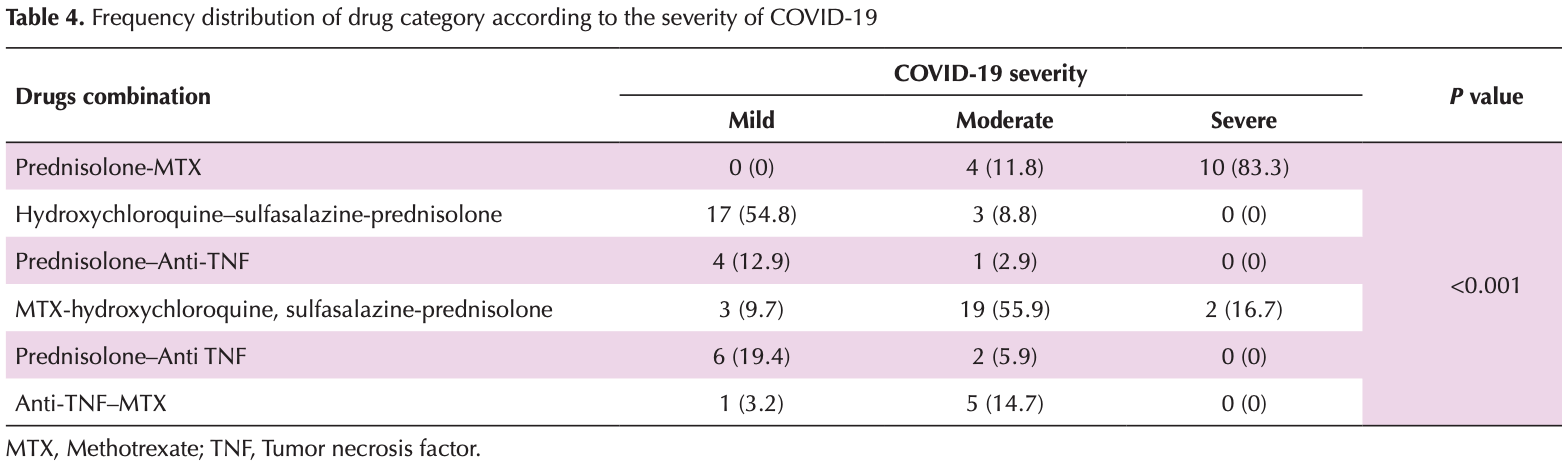
Introduction: Recent studies have shown that patients with rheumatic diseases are more likely to experience severe cases of COVID-19. Additionally, certain anti-inflammatory medications have been linked to a reduction in the severity of COVID-19 symptoms. Objectives: This cross-sectional study aimed to determine the frequency of clinical signs, symptoms, and severity of COVID-19 in outpatients with rheumatic diseases. Patients and Methods: A total of 77 patients with rheumatic disorders who were diagnosed with COVID-19 and referred to Isfahan rheumatology clinics in 2020 were selected for this study. The study investigated their clinical signs, symptoms, severity of COVID-19, type of rheumatic disease, and the medications they were using. Furthermore, the study examined the relationship between the severity of COVID-19 and the type of rheumatic disease. Results: Among the 77 patients, 79.2% had rheumatoid arthritis (RA), 9.1% had systemic lupus erythematosus (SLE), 9.1% had Sjogren's syndrome, and 2.6% had other rheumatic disorders. The severity of COVID-19 was classified as mild in 40.3% of cases, moderate in 44.2%, and severe in 15.6%. There was no statistically significant relationship between the type of rheumatic disease and the severity of COVID-19 (P = 0.093).
Conclusion: The findings suggest that patients with rheumatic diseases are more likely to experience severe cases of COVID-19. Conversely, the combination of hydroxychloroquine, sulfasalazine, and prednisolone has been associated with a lower prevalence of severe cases of COVID-19. In contrast, the administration of methotrexate and prednisolone has been linked to a higher prevalence of severe cases of COVID-19.
Authors' contribution
Conflicts of interest The authors declare that they have no competing interests.
Ethical issues The research followed the tenets of the Declaration of Helsinki. The Ethics Committee of Isfahan University of Medical Sciences approved this study. The institutional ethical committee at Isfahan University of Medical Sciences approved all study protocols (Ethical code#IR.MUI.MED.REC.1399.883). Accordingly, written informed consent was taken from all participants before any intervention. this study was extracted from a thesis of internal medicine specialty
References
Brownstone, Thibodeaux, Reddy, Myers, Chan et al., Novel Coronavirus Disease (COVID-19) and Biologic Therapy in Psoriasis: Infection Risk and Patient Counseling in Uncertain Times, Dermatol Ther (Heidelb), doi:10.1007/s13555-020-00377-9
Cai, Sun, Huang, Gamber, Wu et al., Indirect virus transmission in a cluster of COVID-19 cases, Wenzhou, China, Emerg Infect Dis, doi:10.3201/eid2606.200412
Chaudhuri, Sasaki, Karkar, Sharif, Lewis et al., Corticosteroids in COVID-19 and non-COVID-19 ARDS: a systematic review and meta-analysis, Intensive Care Med, doi:10.1007/s00134-021-06394-2
Chen, Liu, Liu, Liu, Liu et al., Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia, Zhonghua Jie He He Hu Xi Za Zhi, doi:10.3760/cma.j.issn.1001-0939.2020.0005
Chen, Zhou, Dong, Qu, Gong et al., Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study, Lancet, doi:10.1016/S0140-6736(20)30211-7
Cron, Chatham, The rheumatologist's role in COVID-19, J Rheumatol, doi:10.3899/jrheum.200334
Ferro, Elefante, Puxeddu, Baldini, Bartoloni et al., COVID-19: the new challenge for rheumatologists. First update, Clin Exp Rheumatol, doi:10.55563/clinexprheumatol/yvn0nh
Giacomelli, Pezzati, Conti, Bernacchia, Siano et al., Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study, Clin Infect Dis, doi:10.1093/cid/ciaa330
Jung, Kwon, Choi, Association between previous rheumatoid arthritis and COVID-19 and its severity: a nationwide cohort study in South Korea, BMJ Open, doi:10.1136/bmjopen-2021-054753
Misra, Agarwal, Gasparyan, Zimba, Rheumatologists' perspective on coronavirus disease 19 (COVID-19) and potential therapeutic targets, Clin Rheumatol, doi:10.1007/s10067-020-05073-9
Mukarram, Ghauri, Sethar, Afsar, Riaz et al., COVID-19: an emerging culprit of inflammatory arthritis, Case Rep Rheumatol, doi:10.1155/2021/6610340
Nocturne, Advances in understanding the pathogenesis of primary Sjögren's syndrome, Nat Rev Rheumatol, doi:10.1038/nrrheum.2013.110
Nunez, Leon, Mucientes, Rodriguez-Rodriguez, Urgelles et al., Risk factors for hospital admissions related to COVID-19 in patients with autoimmune inflammatory rheumatic diseases, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-217984
Pan, Ye, Sun, Gui, Liang et al., Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19), Radiology, doi:10.1148/radiol.2020200370
Rothan, Byrareddy, The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak, J Autoimmun, doi:10.1016/j.jaut.2020.102433
Smolen, Landewé, Bijlsma, Burmester, Chatzidionysiou et al., EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update, Ann Rheum Dis, doi:10.1136/annrheumdis-2016-210715
Sparks, Tedeschi, Improving COVID-19 vaccine immunogenicity by interrupting methotrexate treatment, Lancet Respir Med, doi:10.1016/S2213-2600(22)00224-7
Spinato, Fabbris, Polesel, Cazzador, Borsetto et al., Alterations in Smell or Taste in Mildly Symptomatic Outpatients With SARS-CoV-2 Infection, JAMA, doi:10.1001/jama.2020.6771
Tong, Wong, Zhu, Fastenberg, Tham, The Prevalence of Olfactory and Gustatory Dysfunction in COVID-19 Patients: A Systematic Review and Meta-analysis, Otolaryngol Head Neck Surg, doi:10.1177/0194599820926473
Tsokos, Lo, Reis, Sullivan, New insights into the immunopathogenesis of systemic lupus erythematosus, Nat Rev Rheumatol, doi:10.1038/nrrheum.2016.186
Vandewalle, Luypaert, Bosscher, Libert, Therapeutic mechanisms of glucocorticoids, Trends Endocrinol Metab, doi:10.1016/j.tem.2017.10.010
Wang, Hu, Hu, Zhu, Liu et al., Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China, JAMA, doi:10.1001/jama.2020.1585
Ye, Cai, Shen, Guan, Zhou et al., Clinical features of rheumatic patients infected with COVID-19 in Wuhan, China, Ann Rheum Dis, doi:10.1136/annrheumdis-2020-217627
DOI record:
{
"DOI": "10.34172/ipp.2023.40568",
"ISSN": [
"2423-8015"
],
"URL": "http://dx.doi.org/10.34172/ipp.2023.40568",
"abstract": "<jats:p>Introduction: Recent studies have shown that patients with rheumatic diseases are more likely to experience severe cases of COVID-19. Additionally, certain anti-inflammatory medications have been linked to a reduction in the severity of COVID-19 symptoms. Objectives: This cross-sectional study aimed to determine the frequency of clinical signs, symptoms, and severity of COVID-19 in outpatients with rheumatic diseases. Patients and Methods: A total of 77 patients with rheumatic disorders who were diagnosed with COVID-19 and referred to Isfahan rheumatology clinics in 2020 were selected for this study. The study investigated their clinical signs, symptoms, severity of COVID-19, type of rheumatic disease, and the medications they were using. Furthermore, the study examined the relationship between the severity of COVID-19 and the type of rheumatic disease. Results: Among the 77 patients, 79.2% had rheumatoid arthritis (RA), 9.1% had systemic lupus erythematosus (SLE), 9.1% had Sjogren’s syndrome, and 2.6% had other rheumatic disorders. The severity of COVID-19 was classified as mild in 40.3% of cases, moderate in 44.2%, and severe in 15.6%. There was no statistically significant relationship between the type of rheumatic disease and the severity of COVID-19 (P=0.093). Conclusion: The findings suggest that patients with rheumatic diseases are more likely to experience severe cases of COVID-19. Conversely, the combination of hydroxychloroquine, sulfasalazine, and prednisolone has been associated with a lower prevalence of severe cases of COVID-19. In contrast, the administration of methotrexate and prednisolone has been linked to a higher prevalence of severe cases of COVID-19.</jats:p>",
"assertion": [
{
"label": "Journal Owner",
"name": "journal_owner",
"value": "Nickan Research Institute"
},
{
"label": "Journal Publisher",
"name": "journal_publisher",
"value": "Nickan Research Institute"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "2023-07-16"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "2023-10-25"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 3,
"value": "2023-12-18"
}
],
"author": [
{
"affiliation": [
{
"name": "Acquired Immunodeficiency Research Centre, Isfahan University of Medical Sciences, Isfahan, Iran"
}
],
"family": "Salesi",
"given": "Mansour",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0009-0008-6308-2927",
"affiliation": [
{
"name": "Isfahan University of Medical Sciences, Isfahan, Iran"
}
],
"authenticated-orcid": true,
"family": "Sedarat",
"given": "Maryam",
"sequence": "additional"
}
],
"container-title": "Immunopathologia Persa",
"container-title-short": "Immunopathol Persa",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"immunopathol.com"
]
},
"created": {
"date-parts": [
[
2024,
1,
8
]
],
"date-time": "2024-01-08T11:56:01Z",
"timestamp": 1704714961000
},
"deposited": {
"date-parts": [
[
2024,
1,
8
]
],
"date-time": "2024-01-08T11:56:01Z",
"timestamp": 1704714961000
},
"indexed": {
"date-parts": [
[
2024,
1,
9
]
],
"date-time": "2024-01-09T00:21:40Z",
"timestamp": 1704759700617
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2023,
12,
18
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
1,
1
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://immunopathol.com/PDF/ipp-10-e40568.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://immunopathol.com/PDF/ipp-10-e40568.pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "20123",
"original-title": [],
"page": "e40568",
"prefix": "10.34172",
"published": {
"date-parts": [
[
2023,
12,
18
]
]
},
"published-online": {
"date-parts": [
[
2023,
12,
18
]
]
},
"publisher": "Maad Rayan Publishing Company",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "https://immunopathol.com/Article/ipp-40568"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Immunology and Microbiology (miscellaneous)",
"Hematology",
"Immunology",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Clinical signs, symptoms, and severity of COVID-19 in patients with rheumatic diseases during the COVID-19 epidemic",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.34172/crossmark_policy",
"volume": "10"
}