Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality
et al., Life Sciences, doi:10.1016/j.lfs.2022.120368, Jan 2022
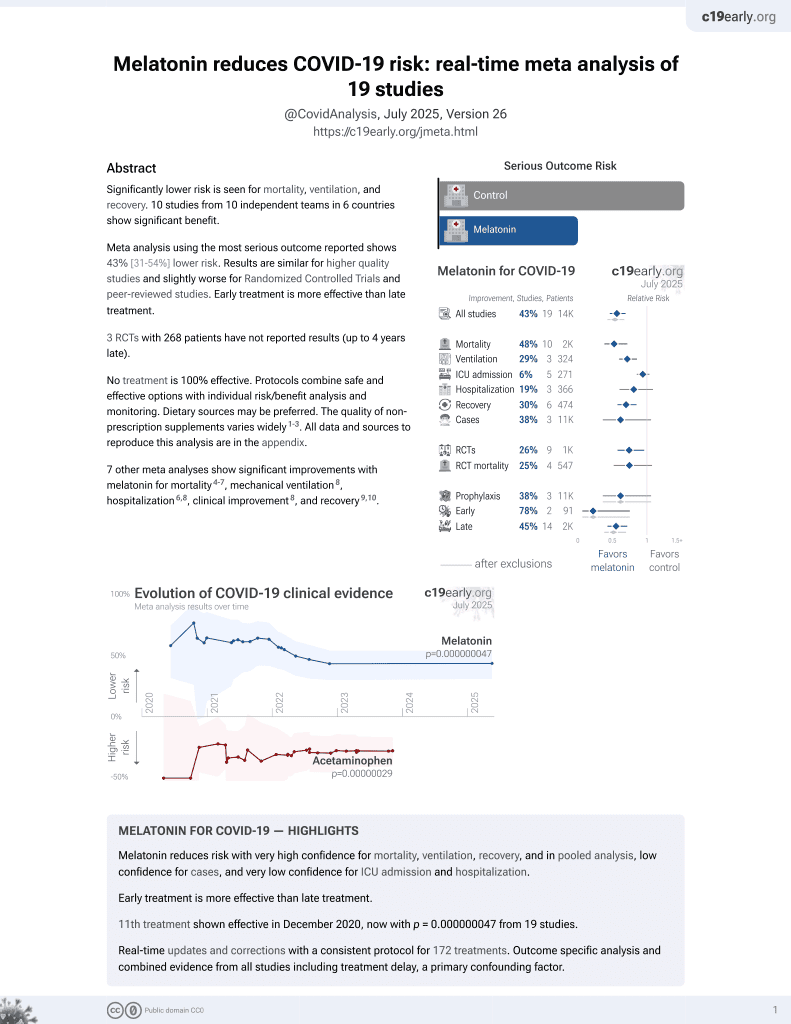
Melatonin for COVID-19
12th treatment shown to reduce risk in
December 2020, now with p = 0.0000000099 from 19 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Review of the mechanisms of action and clinical evidence supporting the use of melatonin for severe COVID-19.
1.
Chen et al., Viral mitochondriopathy in COVID-19, Redox Biology, doi:10.1016/j.redox.2025.103766.
2.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
3.
Xie et al., The role of reactive oxygen species in severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) infection-induced cell death, Cellular & Molecular Biology Letters, doi:10.1186/s11658-024-00659-6.
4.
Zhao et al., Melatonin Potentially Acts as a Widely-Acting Protective Tool in COVID-19, Medicine Research, doi:10.21127/yaoyimr20240006.
5.
Yehia et al., Melatonin: a ferroptosis inhibitor with potential therapeutic efficacy for the post-COVID-19 trajectory of accelerated brain aging and neurodegeneration, Molecular Neurodegeneration, doi:10.1186/s13024-024-00728-6.
6.
Chacin-Bonilla et al., Melatonin and viral infections: A review focusing on therapeutic effects and SARS-CoV-2, Melatonin Research, doi:10.32794/mr112500168.
7.
Lempesis et al., A mid‑pandemic night's dream: Melatonin, from harbinger of anti‑inflammation to mitochondrial savior in acute and long COVID‑19 (Review), International Journal of Molecular Medicine, doi:10.3892/ijmm.2024.5352.
8.
Alomari et al., Assessing the antiviral potential of melatonin: A comprehensive systematic review, Reviews in Medical Virology, doi:10.1002/rmv.2499.
9.
Donzelli, A., Neglected Effective Early Therapies against COVID-19: Focus on Functional Foods and Related Active Substances. A Review, MDPI AG, doi:10.20944/preprints202312.1178.v1.
10.
Langen, M., Melatonin - the Hormone of Both Sun and Darkness - Protects Your Health and Can Save Your Life, Rounding The Earth, roundingtheearth.substack.com/p/melatonin-the-hormone-of-both-sun.
11.
Hosseinzadeh et al., Melatonin effect on platelets and coagulation: Implications for a prophylactic indication in COVID-19, Life Sciences, doi:10.1016/j.lfs.2022.120866.
12.
Loh et al., Melatonin: Regulation of Viral Phase Separation and Epitranscriptomics in Post-Acute Sequelae of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms23158122.
13.
Reiter et al., Melatonin: highlighting its use as a potential treatment for SARS-CoV-2 infection, Cellular and Molecular Life Sciences, doi:10.1007/s00018-021-04102-3.
14.
Tan et al., Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality, Life Sciences, doi:10.1016/j.lfs.2022.120368.
15.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
16.
Castle et al., Implications for Systemic Approaches to COVID-19: Effect Sizes of Remdesivir, Tocilizumab, Melatonin, Vitamin D3, and Meditation, Journal of Inflammation Research, doi:10.2147/JIR.S323356.
17.
Ramos et al., The Coronavirus Disease 2019 (COVID-19): Key Emphasis on Melatonin Safety and Therapeutic Efficacy, Antioxidants, doi:10.3390/antiox10071152.
18.
Camp et al., Melatonin interferes with COVID-19 at several distinct ROS-related steps, Journal of Inorganic Biochemistry, doi:10.1016/j.jinorgbio.2021.111546.
19.
Cross et al., Melatonin for the Early Treatment of COVID-19: A Narrative Review of Current Evidence and Possible Efficacy, Endocrine Practice, doi:10.1016/j.eprac.2021.06.001.
20.
DiNicolantonio et al., Melatonin may decrease risk for and aid treatment of COVID-19 and other RNA viral infections, Open Heart, doi:10.1136/openhrt-2020-001568.
21.
Reiter (B) et al., Therapeutic Algorithm for Use of Melatonin in Patients With COVID-19, Frontiers in Medicine, doi:10.3389/fmed.2020.00226.
22.
Charaa et al., Prophylactic Treatment Protocol against the Severity of COVID-19 Using Melatonin, SSRN, doi:10.2139/ssrn.3601861.
Tan et al., 31 Jan 2022, peer-reviewed, 2 authors.
Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality
Life Sciences, doi:10.1016/j.lfs.2022.120368
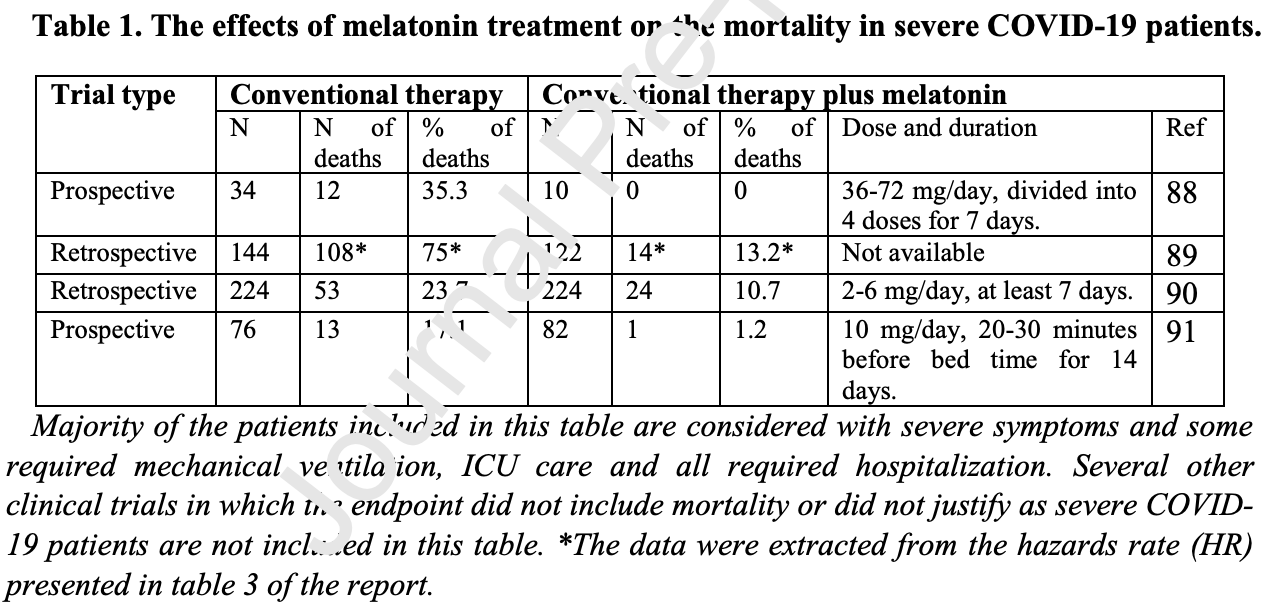
The fear of SARS-CoV-2 infection is due to its high mortality related to seasonal flu. To date, few medicines have been developed to significantly reduce the mortality of the severe COVID-19 patients, especially those requiring tracheal intubation. The severity and mortality of SARS-CoV-2 infection not only depend on the viral virulence, but are primarily determined by the cytokine storm and the destructive inflammation driven by the host immune reaction. Thus, to target the host immune response might be a better strategy to combat this pandemic. Melatonin is a molecule with multiple activities on a virus infection. These include that it downregulates the overreaction of innate immune response to suppress inflammation, promotes the adaptive immune reaction to enhance antibody formation, inhibits the entrance of the virus into the cell as well as limits its replication. These render it a potentially excellent candidate for treatment of the severe COVID-19 cases. Several clinical trials have confirmed that melatonin when added to the conventional therapy significantly reduces the mortality of the severe COVID-19 patients. The cost of melatonin is a small fraction of those medications approved by FDA for emergency use to treat COVID-19. Because of its self-administered, low cost and high safety margin, melatonin could be made available to every country in the world at an affordable cost. We recommend melatonin be used to treat severe COVID-19 patients with the intent of reducing mortality. If successful, it would make the SARS-CoV-2 pandemic less fearful and help to return life back to normalcy.
References
Alizadeh, Keyhanian, Ghaderkhani, Dashti-Khavidaki, Shoormasti et al., A pilot study on controlling coronavirus disease 2019 (COVID-19) inflammation using melatonin supplement, Iran, J. Allergy. Asthma. Immunol, doi:10.18502/ijaai.v20i4.6959
Anand, Ziebuhr, Wadhwani, Mesters, Hilgenfeld, Coronavirus main proteinase (3CLpro) structure: basis for design of anti-SARS drugs, Science, doi:10.1126/SCIENCE.1085658
Ashrafizadeh, Najafi, Kavyiani, Mohammadinejad, Farkhondeh et al., Anti-inflammatory activity of melatonin: a focus on the role of NLRP3 inflammasome, Inflammation, doi:10.1007/S10753-021-01428-9
Aslan, Gül, Tektemur, Sahna, Ischemic postconditioning reduced myocardial ischemia-reperfusion injury: the roles of melatonin and uncoupling protein 3, anatol, J. Cardiol, doi:10.14744/ANATOLJCARDIOL.2019.72609
Authorizes, Pfizer oral COVID-19 treatment, first for at-home use
Behl, Kaur, Aleya, Sehgal, Singh et al., CD147-spike protein interaction in COVID-19: get the ball rolling with a novel receptor and therapeutic target, Sci. Total Environ, doi:10.1016/J.SCITOTENV.2021.152072
Boga, Coto-Montes, Rosales-Corral, Tan, Reiter et al., Beneficial actions of melatonin in the management of viral infections: a new use for this "molecular handyman, Rev. Med. Virol, doi:10.3389/FIMMU.2020.576745
Bologna, Madonna, Pone, Efficacy of prolonged-release melatonin 2 mg (PRM 2 mg) prescribed for insomnia in hospitalized patients for COVID-19: a retrospective observational study, J. Clin. Med, doi:10.3390/JCM10245857
Büki, Okonkwo, Wang, Povlishock, Cytochrome c release and caspase activation in traumatic axonal injury, J. Neurosci, doi:10.1523/JNEUROSCI.20-08-02825.2000
Cao, Shrestha, Li, Yu, Chen et al., Melatonin-mediated mitophagy protects against early brain injury after subarachnoid hemorrhage through inhibition of NLRP3 inflammasome activation, Sci. Rep, doi:10.1038/S41598-017-02679-Z
Cardinali, Brown, Pandi-Perumal, An urgent proposal for the immediate use of melatonin as an adjuvant to anti-SARS-CoV-2 vaccination, Melatonin Res, doi:10.32794/MR11250091
Cardinali, Brown, Reiter, Pandi-Perumal, Elderly as a high-risk group during COVID-19 pandemic: effect of circadian misalignmentSleep Dysregulation and Melatonin Administration, Sleep Vigil, doi:10.1007/S41782-020-00111-7
Castillo, Quizon, Juco, Roman, De Leon et al., Melatonin as adjuvant treatment for coronavirus disease 2019 pneumonia patients requiring hospitalization (MAC-19 PRO): a case series, Melatonin Res, doi:10.32794/MR11250063
Castrillón, Esquifino, Varas, Zapata, Cutrera et al., Effect of melatonin treatment on 24-h variations in responses to mitogens and lymphocyte subset populations in rat submaxillary lymph nodes, J. Neuroendocrinol, doi:10.1046/J.1365-2826.2000.00519.X
Cecon, Fernandois, Renault, Coelho, Wenzel et al., into the brain and virus-induced damage of cerebral small vessels, doi:10.1101/2021.12.30.474561
Cecon, Izabelle, Le Poder, Real, Zhu et al., Therapeutic potential of melatonin and melatonergic drugs on K18-hACE2 mice infected with SARS-CoV-2, J. Pineal Res, doi:10.1111/JPI.12772
Costantino, Cuzzocrea, Mazzon, Caputi, Protective effects of melatonin in zymosan-activated plasma-induced paw inflammation, Eur. J. Pharmacol, doi:10.1016/s0014-2999(98)00673-6
Crespo, Fernández-Palanca, San-Miguel, Álvarez, González-Gallego et al., Melatonin modulates mitophagy, innate immunity and circadian clocks in a model of viral-induced fulminant hepatic failure, J. Cell. Mol. Med, doi:10.1111/JCMM.15398
Cuesta, Cerezuela, Esteban, Meseguer, In vivo actions of melatonin on the innate immune parameters in the teleost fish gilthead seabream, J. Pineal Res, doi:10.1111/J.1600-079X.2008.00557.X
Cuzzocrea, Zingarelli, Costantino, Caputi, Protective effect of melatonin in a non-septic shock model induced by zymosan in the rat, J. Pineal Res, doi:10.1111/j.1600-079x.1998.tb00382.x
Cuzzocrea, Zingarelli, Gilad, Hake, Salzman et al., Protective effect of melatonin in carrageenan-induced models of local inflammation: relationship to its inhibitory effect on nitric oxide production and its peroxynitrite scavenging activity, J. Pineal Res, doi:10.1111/j.1600-079x.1997.tb00342.x
Davies, Adlimoghaddam, Albensi, The effect of COVID-19 on NF-κB and neurological manifestations of disease, Mol. Neurobiol, doi:10.1007/S12035-021-02438-2
Ding, Fu, Wang, Liu, Wang et al., The complex interplay between autophagy and NLRP3 inflammasome in renal diseases, Int. J. Mol. Sci, doi:10.3390/IJMS222312766
Duan, Guo, Yang, Han, Thakur et al., Modeling COVID-19 with human pluripotent stem cell-derived cells reveals synergistic effects of antiinflammatory macrophages with ACE2 inhibition against SARS-CoV-2, Res. Sq, doi:10.21203/RS.3.RS-62758/V1
El-Sokkary, Omar, Hassanein, Cuzzocrea, Reiter, Melatonin reduces oxidative damage and increases survival of mice infected with Schistosoma mansoni, Free Radic, Biol. Med
Fakhriravari, Jin, Kachouei, Le, Lopez, Systemic corticosteroids for management of COVID-19: saving lives or causing harm?, Int. J. Immunopathol. Pharmacol, doi:10.1177/20587384211063976
Fehr, Perlman, Coronaviruses: an overview of their replication and pathogenesis, Coronaviruses, doi:10.1007/978-1-4939-2438-7_1
Feitosa, Júnior, Neto, Matos, Moura et al., COVID-19: rational discovery of the therapeutic potential of melatonin as a SARS-CoV-2 main protease inhibitor, Int. J. Med. Sci, doi:10.7150/IJMS.48053
Feng, Adeniran, Huang, Li, Ma et al., The ameliorative effect of melatonin on LPS-induced sertoli cells inflammatory and tight junctions damage via suppression of the TLR4/MyD88/NF-κB signaling pathway in newborn calf, Theriogenology, doi:10.1016/J.THERIOGENOLOGY.2021.11.020
Gupta, Singh, Goyal, Tripti, Ansari et al., Bats and viruses: a death-defying friendship, Virusdisease, doi:10.1007/S13337-021-00716-0
Gurunathan, Kang, Choi, Reiter, Kim, Melatonin: a potential therapeutic agent against COVID-19, Melatonin Res, doi:10.32794/MR11250081
Hardeland, Neuroprotection by radical avoidance: search for suitable agents, Molecules, doi:10.3390/molecules14125054
Hasan, Atrakji, Mehuaiden, The effect of melatonin on thrombosis, sepsis and mortality rate in COVID-19 patients, Int. J. Infect. Dis, doi:10.1016/J.IJID.2021.10.012
Hasan, Islam, Matsumoto, Kawai, Meta-analysis of single-cell RNAseq data reveals phenotypic switching of immune cells in severe COVID-19 patients, Comput. Biol. Med, doi:10.1016/J.COMPBIOMED.2021.104792
Hazra, Chaudhuri, Tiwary, Chakrabarti, Matrix metallopeptidase 9 as a host protein target of chloroquine and melatonin for immunoregulation in COVID-19: a network-based meta-analysis, Life Sci, doi:10.1016/J.LFS.2020.118096
Heskin, Pallett, Mughal, Davies, Moore et al., Caution required with use of ritonavir-boosted PF-07321332 in COVID-19 management, Lancet, doi:10.1016/S0140-6736(21)02657-X
Hosseini, Esmaeili Gouvarchin, Ghaleh, Aghamollaei, Fasihi Ramandi et al., Evaluation of Th1 and Th2 mediated cellular and humoral immunity in patients with COVID-19 following the use of melatonin as an adjunctive treatment, Eur. J. Pharmacol, doi:10.1016/J.EJPHAR.2021.174193
Hu, Li, Wang, Guo, Li et al., Melatonin inhibits endoplasmic reticulum stress-associated TXNIP/NLRP3 inflammasome activation in lipopolysaccharide-induced endometritis in mice, Int. Immunopharmacol, doi:10.1016/j.intimp.2018.08.028
Hu, Zhang, Wen, Liu, Cai et al., Melatonin decreases M1 polarization via attenuating mitochondrial oxidative damage depending on UCP2 pathway in prorenin-treated microglia, PLoS One, doi:10.1371/JOURNAL.PONE.0212138
Jauhari, Baranov, Suofu, Kim, Singh et al., Melatonin inhibits cytosolic mitochondrial DNA-induced neuroinflammatory signaling in accelerated aging and neurodegeneration, J. Clin. Invest, doi:10.1172/JCI135026
Kaivola, Nyman, Matikainen, Inflammasomes and SARS-CoV-2 infection, Viruses, doi:10.3390/V13122513
Khalili, Karamouzian, Nasiri, Javadi, Mirzazadeh et al., Epidemiological characteristics of COVID-19: a systematic review and metaanalysis, Epidemiol. Infect, doi:10.1017/S0950268820001430
Klann, Bojkova, Tascher, Ciesek, Münch et al., Growth factor receptor signaling inhibition prevents SARS-CoV-2 replication, Mol. Cell, doi:10.1016/J.MOLCEL.2020.08.006
Kong, Zhang, Liu, Li, Liu et al., Melatonin attenuates angiotensin II-induced abdominal aortic aneurysm through the down-regulation of matrix metalloproteinases, Oncotarget, doi:10.18632/oncotarget.15093
Kucia, Ratajczak, Bujko, Adamiak, Ciechanowicz et al., An evidence that SARS-Cov-2/COVID-19 spike protein (SP) damages hematopoietic stem/progenitor cells in the mechanism of pyroptosis in Nlrp3 inflammasome-dependent manner, Leukemia, doi:10.1038/S41375-021-01332-Z
Lei, Hou, Yu, Zhang, Ndzouboukou et al., Kinetics of neutralizing antibody response underscores clinical COVID-19 progression, J. Immunol. Res, doi:10.1155/2021/9822706
Li, Ying, Cai, Yang, Wu, Exogenous melatonin alleviates hemorrhagic shock-induced hepatic ischemic injury in rats by inhibiting the NF-κB/IκBα signaling pathway, Mol. Med. Rep, doi:10.3892/MMR.2021.11980
Loh, The potential of melatonin in the prevention and attenuation of oxidative hemolysis and myocardial injury from cd147 SARS-CoV-2 spike protein receptor binding, Melatonin Res, doi:10.32794/mr11250069
Luo, Song, Zhang, Zhang, Liu et al., Melatonin mediated Foxp3-downregulation decreases cytokines production via the TLR2 and TLR4 pathways in H. Pylori infected mice, Int. Immunopharmacol, doi:10.1016/J.INTIMP.2018.08.034
Ma, Idle, Krausz, Gonzalez, Metabolism of melatonin by human cytochromes p450, Drug Metab. Dispos, doi:10.1124/DMD.104.002410
Mahase, Covid-19: UK becomes first country to authorise antiviral molnupiravir, BMJ, doi:10.1136/BMJ.N2697
Maldonado, García-Moreno, González-Yanes, Calvo, Possible involvement of the inhibition of NF-κB factor in anti-inflammatory actions that melatonin exerts on mast cells, J. Cell. Biochem, doi:10.1002/JCB.25491
Maldonado, Mora-Santos, Naji, Carrascosa-Salmoral, Naranjo et al., Evidence of melatonin synthesis and release by mast cells. Possible modulatory role on inflammation, Pharmacol. Res, doi:10.1016/j.phrs.2009.11.014
Manik, Singh, Role of toll-like receptors in modulation of cytokine storm signaling in SARS-CoV-2-induced COVID-19, J. Med. Virol, doi:10.1002/JMV.27405
Marqueze, Nogueira, Vetter, Skene, Cipolla-Neto et al., Exogenous melatonin decreases circadian misalignment and body weight among early types, J. Pineal Res, doi:10.1111/JPI.12750
Mayo, Sainz, Antolín, Herrera, Martin et al., Melatonin regulation of antioxidant enzyme gene expression, Cell. Mol. Life Sci, doi:10.1007/PL00012498
Mayo, Sainz, Tan, Hardeland, Leon et al., Anti-inflammatory actions of melatonin and its metabolites, N1-acetyl-N2-formyl-5-methoxykynuramine (AFMK) and N1-acetyl-5-methoxykynuramine (AMK), in macrophages, J. Neuroimmunol, doi:10.1016/j.jneuroim.2005.05.002
Mohapatra, Sarangi, Kandi, Azam, Tiwari et al., Omicron (B.1.1.529 variant of SARS-CoV-2); an emerging threat: current global scenario, J. Med. Virol, doi:10.1002/JMV.27561
Morchang, Malakar, Poonudom, Noisakran, Yenchitsomanus et al., Melatonin inhibits dengue virus infection via the sirtuin 1-mediated interferon pathway, Viruses, doi:10.3390/V13040659
Mousavi, Heydari, Mehravaran, Saeedi, Alizadeh-Navaei et al., Melatonin effects on sleep quality and outcomes of COVID-19 patients: an open-label, randomized, controlled trial, J. Med. Virol, doi:10.1002/JMV.27312
Muxel, Pires-Lapa, Monteiro, Cecon, Tamura et al., NF-κB drives the synthesis of melatonin in RAW 264.7 macrophages by inducing the transcription of the arylalkylamine-Nacetyltransferase (AA-NAT) gene, PLoS One, doi:10.1371/JOURNAL.PONE.0052010
Ouoba, Okimoto, Nagashima, Kitahara, Miwata et al., Sequential dynamics of virological and serological changes in the serum of SARS-CoV-2 infected patients, J. Med. Virol, doi:10.1002/JMV.27518
Pan, Zhang, Su, Wang, Liu, Melatonin balance the autophagy and apoptosis by regulating UCP2 in the LPS-induced cardiomyopathy, Molecules, doi:10.3390/MOLECULES23030675
Pavlovich, Lovett, Koroleva, Guito, Arnold et al., The egyptian rousette genome reveals unexpected features of bat antiviral immunity, Cell, doi:10.1016/j.cell.2018.03.070
Polidoro, Hagan, De Santis, Santiago, Schmidt, Overview: systemic inflammatory response derived from lung injury caused by SARS-CoV-2 infection explains severe outcomes in COVID-19, Front. Immunol, doi:10.3389/FIMMU.2020.01626
Qin, Liu, Sun, Li, Xu et al., Protective effects of melatonin on the white matter damage of neonatal rats by regulating NLRP3 inflammasome activity, Neuroreport, doi:10.1097/WNR.0000000000001642
Ramlall, Zucker, Tatonetti, Melatonin is significantly associated with survival of intubated COVID-19 patients, MedRxiv Prepr. Serv. Heal. Sci, doi:10.1101/2020.10.15.20213546
Ramos, Míguez, Morgado, Sanchez-Correa, Gordillo et al., Melatonin enhances responsiveness to dichelobacter nodosus vaccine in sheep and increases peripheral blood CD4 T lymphocytes and IgG-expressing B lymphocytes, Vet. Immunol. Immunopathol, doi:10.1016/J.VETIMM.2018.11.006
Regeneron, New, Government Agreement to Purchase Additional Doses of REGEN-COVTM (casirivimab and imdevimab) Antibody Cocktail
Reiter, Abreu-Gonzalez, Marik, Dominguez-Rodriguez, Therapeutic algorithm for use of melatonin in patients with COVID-19, Front. Med, doi:10.3389/FMED.2020.00226
Reiter, Sharma, Ma, Liu, Manucha et al., Plasticity of glucose metabolism in activated immune cells: advantages for melatonin inhibition of COVID-19 disease, Melatonin Res, doi:10.32794/MR11250068
Reiter, Tan, Rosales-Corral, Galano, Zhou et al., Mitochondria: central organelles for melatonin's antioxidant and anti-aging actions, Molecules, doi:10.3390/molecules23020509
Ren, Sun, Li, Chen, Ge et al., Exogenous melatonin inhibits neutrophil migration through suppression of ERK activation, J. Endocrinol, doi:10.1530/JOE-15-0329
Ryu, Park, Kim, Lee, Seo et al., SARS-CoV 3CLpro inhibitory effects of quinone-methide triterpenes from tripterygium regelii, Bioorg. Med. Chem. Lett, doi:10.1016/J.BMCL.2010.01.152
Sanchez-Barcelo, Rueda, Mediavilla, Rodriguez-Cue, Reiter, Clinical uses of melatonin in neurological diseases and mental and behavioural disorders, Curr. Med. Chem, doi:10.2174/0929867324666170718105557
Sen, Does serotonin deficiency lead to anosmia, ageusia, dysfunctional chemesthesis and increased severity of illness in COVID-19?, Med. Hypotheses, doi:10.1016/j.mehy.2021.110627
Shukla, Htoo, Wintachai, Hernandez, Dubois et al., Melatonin stimulates the nonamyloidogenic processing of βaPP through the positive transcriptional regulation of ADAM10 and ADAM17, J. Pineal Res, doi:10.1111/jpi.12200
Simko, Reiter, Is melatonin deficiency a unifying pathomechanism of high risk patients with COVID-19?, Life Sci, doi:10.1016/J.LFS.2020.117902
Simpson, Oliver, ROS generation in microglia: understanding oxidative stress and inflammation in neurodegenerative disease, Antioxidants, doi:10.3390/ANTIOX9080743
Sygitowicz, Sitkiewicz, Molecular mechanisms of organ damage in sepsis: an overview, Braz. J. Infect. Dis, doi:10.1016/J.BJID.2020.09.004
Szewczyk-Golec, Rajewski, Gackowski, Mila-Kierzenkowska, Wesołowski et al., Melatonin supplementation lowers oxidative stress and regulates adipokines in obese patients on a calorie-restricted diet, Oxidative Med. Cell. Longev, doi:10.1155/2017/8494107
Sánchez-González, Mahíllo-Fernández, Villar-Álvarez, Llanos, What if melatonin could help COVID-19 severe patients?, J. Clin. Sleep Med, doi:10.5664/JCSM.9554
Tan, Chen, Poeggeler, Manchester, Reiter, Melatonin: a potent, endogenous hydroxyl radical scavenger, Endocr. J
Tan, Hardeland, Estimated doses of melatonin for treating deadly virus infections: focus on COVID-19, Melatonin Res, doi:10.32794/mr11250062
Tan, Hardeland, Manchester, Poeggeler, Lopez-Burillo et al., Mechanistic and comparative studies of melatonin and classic antioxidants in terms of their interactions with the ABTS cation radical, J. Pineal Res, doi:10.1034/J.1600-079X.2003.00037.X
Tan, Hardeland, Potential utility of melatonin in deadly infectious diseases related to the overreaction of innate immune response and destructive inflammation: focus on COVID-19, Melatonin Res, doi:10.32794/mr11250052
Tan, Manchester, Fuentes-Broto, Paredes, Reiter, Significance and application of melatonin in the regulation of brown adipose tissue metabolism: relation to human obesity, Obes. Rev, doi:10.1111/j.1467-789X.2010.00756.x
Tan, Manchester, Terron, Flores, Reiter, One molecule, many derivatives: a never-ending interaction of melatonin with reactive oxygen and nitrogen species?, J. Pineal Res, doi:10.1111/j.1600-079X.2006.00407.x
Tan, Ruediger, Targeting host defense system and rescuing compromised mitochondria to increase tolerance against pathogens by melatonin may impact outcome of deadly virus infection pertinent to COVID-19, Molecules, doi:10.3390/MOLECULES25194410
Tan, Zanghi, Manchester, Reiter, Melatonin identified in meats and other food stuffs: potentially nutritional impact, J. Pineal Res, doi:10.1111/jpi.12152
Tan, Zheng, Kong, Manchester, Hardeland et al., Fundamental issues related to the origin of melatonin and melatonin isomers during evolution: relation to their biological functions, Int. J. Mol. Sci, doi:10.3390/ijms150915858
Tesarik, Melatonin attenuates growth factor receptor signaling required for SARS-CoV-2 replication, Melatonin Res, doi:10.32794/MR11250077
Venkatraja, Srilakshminarayana, Kumar, The dominance of severe acute respiratory syndrome coronavirus 2 B.1.617 and its sublineages and associations with mortality during the COVID-19 pandemic in India between 2020 and 2021, Am. J. Trop. Med. Hyg, doi:10.4269/AJTMH.21-0812
Wang, Chen, Zhang, Deng, Lian et al., CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells, Signal Transduct, doi:10.1038/s41392-020-00426-x
Wright, Aldhous, Franey, English, Arendt, The effects of exogenous melatonin on endocrine function in man, Clin. Endocrinol, doi:10.1111/J.1365-2265.1986.TB01641.X
Xu, Wang, Ai, Shi, Zhang et al., Melatonin suppresses TLR9-triggered proinflammatory cytokine production in macrophages by inhibiting ERK1/2 and AKT activation, Sci. Rep, doi:10.1038/S41598-018-34011-8
Zhai, Wang, Jiao, Zhang, Li et al., Melatonin and other indoles show antiviral activities against swine coronaviruses in vitro at pharmacological concentrations, J. Pineal Res, doi:10.1111/JPI.12754
Zhang, Karam, Glycemic profile of intravenous dexamethasone-induced hyperglycemia using continuous glucose monitoring, Am. J. Case Rep, doi:10.12659/AJCR.930733
Zhang, Li, Grailer, Wang, Wang et al., Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome, J. Pineal Res, doi:10.1111/jpi.12322
Zhang, Wang, Ni, Di, Ma et al., COVID-19: melatonin as a potential adjuvant treatment, Life Sci, doi:10.1016/j.lfs.2020.117583
Zhou, Hou, Shen, Huang, Martin et al., Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2, Cell Discov, doi:10.1038/s41421-020-0153-3
Zhou, Hou, Shen, Mehra, Kallianpur et al., A network medicine approach to investigation and population-based validation of disease manifestations and drug repurposing for COVID-19, PLoS Biol, doi:10.1371/JOURNAL.PBIO.3000970
Zlacká, Stebelová, Zeman, Herichová, Interactions of renin-angiotensin system and COVID-19: the importance of daily rhythms in ACE2, ADAM17 and TMPRSS2 expression, Physiol. Res, doi:10.33549/PHYSIOLRES.934754
DOI record:
{
"DOI": "10.1016/j.lfs.2022.120368",
"ISSN": [
"0024-3205"
],
"URL": "http://dx.doi.org/10.1016/j.lfs.2022.120368",
"alternative-id": [
"S0024320522000686"
],
"article-number": "120368",
"author": [
{
"affiliation": [],
"family": "Tan",
"given": "Dun-Xian",
"sequence": "first"
},
{
"affiliation": [],
"family": "Reiter",
"given": "Russel J.",
"sequence": "additional"
}
],
"container-title": [
"Life Sciences"
],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
1,
30
]
],
"date-time": "2022-01-30T07:16:41Z",
"timestamp": 1643527001000
},
"deposited": {
"date-parts": [
[
2022,
1,
30
]
],
"date-time": "2022-01-30T15:32:39Z",
"timestamp": 1643556759000
},
"indexed": {
"date-parts": [
[
2022,
1,
31
]
],
"date-time": "2022-01-31T05:42:30Z",
"timestamp": 1643607750955
},
"is-referenced-by-count": 0,
"issn-type": [
{
"type": "print",
"value": "0024-3205"
}
],
"issued": {
"date-parts": [
[
2022,
1
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
1,
1
]
],
"date-time": "2022-01-01T00:00:00Z",
"timestamp": 1640995200000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0024320522000686?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0024320522000686?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "120368",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2022,
1
]
]
},
"published-print": {
"date-parts": [
[
2022,
1
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"article-title": "The dominance of severe acute respiratory syndrome coronavirus 2 B.1.617 and its sublineages and associations with mortality during the COVID-19 pandemic in India between 2020 and 2021",
"author": "Venkatraja",
"journal-title": "Am. J. Trop. Med. Hyg.",
"key": "10.1016/j.lfs.2022.120368_bb0005",
"year": "2021"
},
{
"article-title": "Omicron (B.1.1.529 variant of SARS-CoV-2); an emerging threat: current global scenario",
"author": "Mohapatra",
"journal-title": "J. Med. Virol.",
"key": "10.1016/j.lfs.2022.120368_bb0010",
"year": "2021"
},
{
"DOI": "10.1007/s13337-021-00716-0",
"article-title": "Bats and viruses: a death-defying friendship",
"author": "Gupta",
"doi-asserted-by": "crossref",
"first-page": "467",
"journal-title": "Virusdisease",
"key": "10.1016/j.lfs.2022.120368_bb0015",
"volume": "32",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2018.03.070",
"article-title": "The egyptian rousette genome reveals unexpected features of bat antiviral immunity",
"author": "Pavlovich",
"doi-asserted-by": "crossref",
"first-page": "1098",
"journal-title": "Cell",
"key": "10.1016/j.lfs.2022.120368_bb0020",
"volume": "173",
"year": "2018"
},
{
"DOI": "10.32794/mr11250052",
"article-title": "Potential utility of melatonin in deadly infectious diseases related to the overreaction of innate immune response and destructive inflammation: focus on COVID-19",
"author": "Tan",
"doi-asserted-by": "crossref",
"first-page": "120",
"journal-title": "Melatonin Res.",
"key": "10.1016/j.lfs.2022.120368_bb0025",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.3390/jcm10245857",
"article-title": "Efficacy of prolonged-release melatonin 2 mg (PRM 2 mg) prescribed for insomnia in hospitalized patients for COVID-19: a retrospective observational study",
"author": "Bologna",
"doi-asserted-by": "crossref",
"first-page": "5857",
"journal-title": "J. Clin. Med.",
"key": "10.1016/j.lfs.2022.120368_bb0030",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27312",
"article-title": "Melatonin effects on sleep quality and outcomes of COVID-19 patients: an open-label, randomized, controlled trial",
"author": "Mousavi",
"doi-asserted-by": "crossref",
"first-page": "263",
"journal-title": "J. Med. Virol.",
"key": "10.1016/j.lfs.2022.120368_bb0035",
"volume": "94",
"year": "2022"
},
{
"article-title": "A pilot study on controlling coronavirus disease 2019 (COVID-19) inflammation using melatonin supplement, Iran",
"author": "Alizadeh",
"first-page": "494",
"journal-title": "J. Allergy. Asthma. Immunol.",
"key": "10.1016/j.lfs.2022.120368_bb0040",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.3390/ijms150915858",
"article-title": "Fundamental issues related to the origin of melatonin and melatonin isomers during evolution: relation to their biological functions",
"author": "Tan",
"doi-asserted-by": "crossref",
"first-page": "15858",
"journal-title": "Int. J. Mol. Sci.",
"key": "10.1016/j.lfs.2022.120368_bb0045",
"volume": "15",
"year": "2014"
},
{
"DOI": "10.1111/jpi.12152",
"article-title": "Melatonin identified in meats and other food stuffs: potentially nutritional impact",
"author": "Tan",
"doi-asserted-by": "crossref",
"first-page": "213",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0050",
"volume": "57",
"year": "2014"
},
{
"DOI": "10.32794/mr11250062",
"article-title": "Estimated doses of melatonin for treating deadly virus infections: focus on COVID-19",
"author": "Tan",
"doi-asserted-by": "crossref",
"first-page": "276",
"journal-title": "Melatonin Res.",
"key": "10.1016/j.lfs.2022.120368_bb0055",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1111/j.1365-2265.1986.tb01641.x",
"article-title": "The effects of exogenous melatonin on endocrine function in man",
"author": "Wright",
"doi-asserted-by": "crossref",
"first-page": "375",
"journal-title": "Clin. Endocrinol.",
"key": "10.1016/j.lfs.2022.120368_bb0060",
"volume": "24",
"year": "1986"
},
{
"DOI": "10.1111/jpi.12750",
"article-title": "Exogenous melatonin decreases circadian misalignment and body weight among early types",
"author": "Marqueze",
"doi-asserted-by": "crossref",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0065",
"volume": "71",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2020.01626",
"article-title": "Overview: systemic inflammatory response derived from lung injury caused by SARS-CoV-2 infection explains severe outcomes in COVID-19",
"author": "Polidoro",
"doi-asserted-by": "crossref",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.lfs.2022.120368_bb0070",
"volume": "11",
"year": "2020"
},
{
"article-title": "ROS generation in microglia: understanding oxidative stress and inflammation in neurodegenerative disease",
"author": "Simpson",
"first-page": "1",
"journal-title": "Antioxidants (Basel, Switzerland)",
"key": "10.1016/j.lfs.2022.120368_bb0075",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2020.00226",
"article-title": "Therapeutic algorithm for use of melatonin in patients with COVID-19",
"author": "Reiter",
"doi-asserted-by": "crossref",
"journal-title": "Front. Med.",
"key": "10.1016/j.lfs.2022.120368_bb0080",
"volume": "7",
"year": "2020"
},
{
"article-title": "Melatonin: a potent, endogenous hydroxyl radical scavenger",
"author": "Tan",
"first-page": "57",
"journal-title": "Endocr. J.",
"key": "10.1016/j.lfs.2022.120368_bb0085",
"volume": "1",
"year": "1993"
},
{
"DOI": "10.1111/j.1600-079X.2006.00407.x",
"article-title": "One molecule, many derivatives: a never-ending interaction of melatonin with reactive oxygen and nitrogen species?",
"author": "Tan",
"doi-asserted-by": "crossref",
"first-page": "28",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0090",
"volume": "42",
"year": "2007"
},
{
"DOI": "10.1034/j.1600-079X.2003.00037.x",
"article-title": "Mechanistic and comparative studies of melatonin and classic antioxidants in terms of their interactions with the ABTS cation radical",
"author": "Tan",
"doi-asserted-by": "crossref",
"first-page": "249",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0095",
"volume": "34",
"year": "2003"
},
{
"DOI": "10.1007/PL00012498",
"article-title": "Melatonin regulation of antioxidant enzyme gene expression",
"author": "Mayo",
"doi-asserted-by": "crossref",
"first-page": "1706",
"journal-title": "Cell. Mol. Life Sci.",
"key": "10.1016/j.lfs.2022.120368_bb0100",
"volume": "59",
"year": "2002"
},
{
"article-title": "Melatonin supplementation lowers oxidative stress and regulates adipokines in obese patients on a calorie-restricted diet",
"author": "Szewczyk-Golec",
"first-page": "8494107",
"journal-title": "Oxidative Med. Cell. Longev.",
"key": "10.1016/j.lfs.2022.120368_bb0105",
"year": "2017"
},
{
"DOI": "10.3390/molecules23030675",
"article-title": "Melatonin balance the autophagy and apoptosis by regulating UCP2 in the LPS-induced cardiomyopathy",
"author": "Pan",
"doi-asserted-by": "crossref",
"journal-title": "Molecules",
"key": "10.1016/j.lfs.2022.120368_bb0110",
"volume": "23",
"year": "2018"
},
{
"article-title": "Melatonin decreases M1 polarization via attenuating mitochondrial oxidative damage depending on UCP2 pathway in prorenin-treated microglia",
"author": "Hu",
"journal-title": "PLoS One",
"key": "10.1016/j.lfs.2022.120368_bb0115",
"volume": "14",
"year": "2019"
},
{
"article-title": "Ischemic postconditioning reduced myocardial ischemia-reperfusion injury: the roles of melatonin and uncoupling protein 3, anatol",
"author": "Aslan",
"first-page": "19",
"journal-title": "J. Cardiol.",
"key": "10.1016/j.lfs.2022.120368_bb0120",
"volume": "23",
"year": "2020"
},
{
"DOI": "10.1111/j.1467-789X.2010.00756.x",
"article-title": "Significance and application of melatonin in the regulation of brown adipose tissue metabolism: relation to human obesity",
"author": "Tan",
"doi-asserted-by": "crossref",
"first-page": "167",
"journal-title": "Obes. Rev.",
"key": "10.1016/j.lfs.2022.120368_bb0125",
"volume": "12",
"year": "2011"
},
{
"DOI": "10.3390/molecules14125054",
"article-title": "Neuroprotection by radical avoidance: search for suitable agents",
"author": "Hardeland",
"doi-asserted-by": "crossref",
"first-page": "5054",
"journal-title": "Molecules",
"key": "10.1016/j.lfs.2022.120368_bb0130",
"volume": "14",
"year": "2009"
},
{
"DOI": "10.2174/0929867324666170718105557",
"article-title": "Clinical uses of melatonin in neurological diseases and mental and behavioural disorders",
"author": "Sanchez-Barcelo",
"doi-asserted-by": "crossref",
"journal-title": "Curr. Med. Chem.",
"key": "10.1016/j.lfs.2022.120368_bb0135",
"volume": "24",
"year": "2017"
},
{
"DOI": "10.3390/molecules23020509",
"article-title": "Mitochondria: central organelles for melatonin’s antioxidant and anti-aging actions",
"author": "Reiter",
"doi-asserted-by": "crossref",
"first-page": "509",
"journal-title": "Molecules",
"key": "10.1016/j.lfs.2022.120368_bb0140",
"volume": "23",
"year": "2018"
},
{
"DOI": "10.1111/j.1600-079X.1997.tb00342.x",
"article-title": "Protective effect of melatonin in carrageenan-induced models of local inflammation: relationship to its inhibitory effect on nitric oxide production and its peroxynitrite scavenging activity",
"author": "Cuzzocrea",
"doi-asserted-by": "crossref",
"first-page": "106",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0145",
"volume": "23",
"year": "1997"
},
{
"DOI": "10.1111/j.1600-079X.1998.tb00382.x",
"article-title": "Protective effect of melatonin in a non-septic shock model induced by zymosan in the rat",
"author": "Cuzzocrea",
"doi-asserted-by": "crossref",
"first-page": "24",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0150",
"volume": "25",
"year": "1998"
},
{
"DOI": "10.1016/S0014-2999(98)00673-6",
"article-title": "Protective effects of melatonin in zymosan-activated plasma-induced paw inflammation",
"author": "Costantino",
"doi-asserted-by": "crossref",
"first-page": "57",
"journal-title": "Eur. J. Pharmacol.",
"key": "10.1016/j.lfs.2022.120368_bb0155",
"volume": "363",
"year": "1998"
},
{
"DOI": "10.1016/j.jneuroim.2005.05.002",
"article-title": "Anti-inflammatory actions of melatonin and its metabolites, N1-acetyl-N2-formyl-5-methoxykynuramine (AFMK) and N1-acetyl-5-methoxykynuramine (AMK), in macrophages",
"author": "Mayo",
"doi-asserted-by": "crossref",
"first-page": "139",
"journal-title": "J. Neuroimmunol.",
"key": "10.1016/j.lfs.2022.120368_bb0160",
"volume": "165",
"year": "2005"
},
{
"DOI": "10.1016/S0891-5849(01)00753-5",
"article-title": "Melatonin reduces oxidative damage and increases survival of mice infected with Schistosoma mansoni",
"author": "El-Sokkary",
"doi-asserted-by": "crossref",
"first-page": "319",
"journal-title": "Free Radic. Biol. Med.",
"key": "10.1016/j.lfs.2022.120368_bb0165",
"volume": "32",
"year": "2002"
},
{
"DOI": "10.18632/oncotarget.15093",
"article-title": "Melatonin attenuates angiotensin II-induced abdominal aortic aneurysm through the down-regulation of matrix metalloproteinases",
"author": "Kong",
"doi-asserted-by": "crossref",
"first-page": "14283",
"journal-title": "Oncotarget",
"key": "10.1016/j.lfs.2022.120368_bb0170",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.1111/jpi.12322",
"article-title": "Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "405",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0175",
"volume": "60",
"year": "2016"
},
{
"DOI": "10.1016/j.intimp.2018.08.028",
"article-title": "Melatonin inhibits endoplasmic reticulum stress-associated TXNIP/NLRP3 inflammasome activation in lipopolysaccharide-induced endometritis in mice",
"author": "Hu",
"doi-asserted-by": "crossref",
"first-page": "101",
"journal-title": "Int. Immunopharmacol.",
"key": "10.1016/j.lfs.2022.120368_bb0180",
"volume": "64",
"year": "2018"
},
{
"DOI": "10.3390/v13122513",
"article-title": "Inflammasomes and SARS-CoV-2 infection",
"author": "Kaivola",
"doi-asserted-by": "crossref",
"first-page": "2513",
"journal-title": "Viruses",
"key": "10.1016/j.lfs.2022.120368_bb0185",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1038/s41375-021-01332-z",
"article-title": "An evidence that SARS-Cov-2/COVID-19 spike protein (SP) damages hematopoietic stem/progenitor cells in the mechanism of pyroptosis in Nlrp3 inflammasome-dependent manner",
"author": "Kucia",
"doi-asserted-by": "crossref",
"first-page": "3026",
"journal-title": "Leukemia",
"key": "10.1016/j.lfs.2022.120368_bb0190",
"volume": "35",
"year": "2021"
},
{
"DOI": "10.1007/s10753-021-01428-9",
"article-title": "Anti-inflammatory activity of melatonin: a focus on the role of NLRP3 inflammasome",
"author": "Ashrafizadeh",
"doi-asserted-by": "crossref",
"first-page": "1207",
"journal-title": "Inflammation",
"key": "10.1016/j.lfs.2022.120368_bb0195",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1007/s12035-021-02438-2",
"article-title": "The effect of COVID-19 on NF-κB and neurological manifestations of disease",
"author": "Davies",
"doi-asserted-by": "crossref",
"first-page": "4178",
"journal-title": "Mol. Neurobiol.",
"key": "10.1016/j.lfs.2022.120368_bb0200",
"volume": "58",
"year": "2021"
},
{
"article-title": "Role of toll-like receptors in modulation of cytokine storm signaling in SARS-CoV-2-induced COVID-19",
"author": "Manik",
"journal-title": "J. Med. Virol.",
"key": "10.1016/j.lfs.2022.120368_bb0205",
"year": "2021"
},
{
"DOI": "10.3892/mmr.2021.11980",
"article-title": "Exogenous melatonin alleviates hemorrhagic shock-induced hepatic ischemic injury in rats by inhibiting the NF-κB/IκBα signaling pathway",
"author": "Li",
"doi-asserted-by": "crossref",
"journal-title": "Mol. Med. Rep.",
"key": "10.1016/j.lfs.2022.120368_bb0210",
"volume": "23",
"year": "2021"
},
{
"DOI": "10.3390/ijms222312766",
"article-title": "The complex interplay between autophagy and NLRP3 inflammasome in renal diseases",
"author": "Ding",
"doi-asserted-by": "crossref",
"journal-title": "Int. J. Mol. Sci.",
"key": "10.1016/j.lfs.2022.120368_bb0215",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1097/WNR.0000000000001642",
"article-title": "Protective effects of melatonin on the white matter damage of neonatal rats by regulating NLRP3 inflammasome activity",
"author": "Qin",
"doi-asserted-by": "crossref",
"first-page": "739",
"journal-title": "Neuroreport.",
"key": "10.1016/j.lfs.2022.120368_bb0220",
"volume": "32",
"year": "2021"
},
{
"article-title": "Melatonin-mediated mitophagy protects against early brain injury after subarachnoid hemorrhage through inhibition of NLRP3 inflammasome activation",
"author": "Cao",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.lfs.2022.120368_bb0225",
"volume": "7",
"year": "2017"
},
{
"DOI": "10.3390/molecules25194410",
"article-title": "Targeting host defense system and rescuing compromised mitochondria to increase tolerance against pathogens by melatonin may impact outcome of deadly virus infection pertinent to COVID-19",
"author": "Tan",
"doi-asserted-by": "crossref",
"journal-title": "Molecules",
"key": "10.1016/j.lfs.2022.120368_bb0230",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.1016/j.bjid.2020.09.004",
"article-title": "Molecular mechanisms of organ damage in sepsis: an overview",
"author": "Sygitowicz",
"doi-asserted-by": "crossref",
"first-page": "552",
"journal-title": "Braz. J. Infect. Dis.",
"key": "10.1016/j.lfs.2022.120368_bb0235",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1016/j.intimp.2018.08.034",
"article-title": "Melatonin mediated Foxp3-downregulation decreases cytokines production via the TLR2 and TLR4 pathways in H. Pylori infected mice",
"author": "Luo",
"doi-asserted-by": "crossref",
"first-page": "116",
"journal-title": "Int. Immunopharmacol.",
"key": "10.1016/j.lfs.2022.120368_bb0240",
"volume": "64",
"year": "2018"
},
{
"DOI": "10.1172/JCI135026",
"article-title": "Melatonin inhibits cytosolic mitochondrial DNA-induced neuroinflammatory signaling in accelerated aging and neurodegeneration",
"author": "Jauhari",
"doi-asserted-by": "crossref",
"first-page": "3124",
"journal-title": "J. Clin. Invest.",
"key": "10.1016/j.lfs.2022.120368_bb0245",
"volume": "130",
"year": "2020"
},
{
"DOI": "10.1038/s41598-018-34011-8",
"article-title": "Melatonin suppresses TLR9-triggered proinflammatory cytokine production in macrophages by inhibiting ERK1/2 and AKT activation",
"author": "Xu",
"doi-asserted-by": "crossref",
"journal-title": "Sci. Rep.",
"key": "10.1016/j.lfs.2022.120368_bb0250",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.1016/j.theriogenology.2021.11.020",
"article-title": "The ameliorative effect of melatonin on LPS-induced sertoli cells inflammatory and tight junctions damage via suppression of the TLR4/MyD88/NF-κB signaling pathway in newborn calf",
"author": "Feng",
"doi-asserted-by": "crossref",
"first-page": "103",
"journal-title": "Theriogenology",
"key": "10.1016/j.lfs.2022.120368_bb0255",
"volume": "179",
"year": "2022"
},
{
"DOI": "10.1530/JOE-15-0329",
"article-title": "Exogenous melatonin inhibits neutrophil migration through suppression of ERK activation",
"author": "Ren",
"doi-asserted-by": "crossref",
"first-page": "49",
"journal-title": "J. Endocrinol.",
"key": "10.1016/j.lfs.2022.120368_bb0260",
"volume": "227",
"year": "2015"
},
{
"DOI": "10.1016/j.phrs.2009.11.014",
"article-title": "Evidence of melatonin synthesis and release by mast cells. Possible modulatory role on inflammation",
"author": "Maldonado",
"doi-asserted-by": "crossref",
"first-page": "282",
"journal-title": "Pharmacol. Res.",
"key": "10.1016/j.lfs.2022.120368_bb0265",
"volume": "62",
"year": "2010"
},
{
"DOI": "10.1371/journal.pone.0052010",
"article-title": "NF-κB drives the synthesis of melatonin in RAW 264.7 macrophages by inducing the transcription of the arylalkylamine-N-acetyltransferase (AA-NAT) gene",
"author": "Muxel",
"doi-asserted-by": "crossref",
"journal-title": "PLoS One.",
"key": "10.1016/j.lfs.2022.120368_bb0270",
"volume": "7",
"year": "2012"
},
{
"DOI": "10.1002/jcb.25491",
"article-title": "Possible involvement of the inhibition of NF-κB factor in anti-inflammatory actions that melatonin exerts on mast cells",
"author": "Maldonado",
"doi-asserted-by": "crossref",
"first-page": "1926",
"journal-title": "J. Cell. Biochem.",
"key": "10.1016/j.lfs.2022.120368_bb0275",
"volume": "117",
"year": "2016"
},
{
"DOI": "10.1016/j.compbiomed.2021.104792",
"article-title": "Meta-analysis of single-cell RNA-seq data reveals phenotypic switching of immune cells in severe COVID-19 patients",
"author": "Hasan",
"doi-asserted-by": "crossref",
"journal-title": "Comput. Biol. Med.",
"key": "10.1016/j.lfs.2022.120368_bb0280",
"volume": "137",
"year": "2021"
},
{
"DOI": "10.32794/mr11250068",
"article-title": "Plasticity of glucose metabolism in activated immune cells: advantages for melatonin inhibition of COVID-19 disease",
"author": "Reiter",
"doi-asserted-by": "crossref",
"first-page": "362",
"journal-title": "Melatonin Res.",
"key": "10.1016/j.lfs.2022.120368_bb0285",
"volume": "3",
"year": "2020"
},
{
"article-title": "Modeling COVID-19 with human pluripotent stem cell-derived cells reveals synergistic effects of anti-inflammatory macrophages with ACE2 inhibition against SARS-CoV-2",
"author": "Duan",
"journal-title": "Res. Sq.",
"key": "10.1016/j.lfs.2022.120368_bb0290",
"year": "2020"
},
{
"DOI": "10.1111/j.1600-079X.2008.00557.x",
"article-title": "In vivo actions of melatonin on the innate immune parameters in the teleost fish gilthead seabream",
"author": "Cuesta",
"doi-asserted-by": "crossref",
"first-page": "70",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0295",
"volume": "45",
"year": "2008"
},
{
"DOI": "10.1111/jcmm.15398",
"article-title": "Melatonin modulates mitophagy, innate immunity and circadian clocks in a model of viral-induced fulminant hepatic failure",
"author": "Crespo",
"doi-asserted-by": "crossref",
"first-page": "7625",
"journal-title": "J. Cell. Mol. Med.",
"key": "10.1016/j.lfs.2022.120368_bb0300",
"volume": "24",
"year": "2020"
},
{
"DOI": "10.1046/j.1365-2826.2000.00519.x",
"article-title": "Effect of melatonin treatment on 24-h variations in responses to mitogens and lymphocyte subset populations in rat submaxillary lymph nodes",
"author": "Castrillón",
"doi-asserted-by": "crossref",
"first-page": "758",
"journal-title": "J. Neuroendocrinol.",
"key": "10.1016/j.lfs.2022.120368_bb0305",
"volume": "12",
"year": "2000"
},
{
"DOI": "10.1016/j.vetimm.2018.11.006",
"article-title": "Melatonin enhances responsiveness to dichelobacter nodosus vaccine in sheep and increases peripheral blood CD4 T lymphocytes and IgG-expressing B lymphocytes",
"author": "Ramos",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Vet. Immunol. Immunopathol.",
"key": "10.1016/j.lfs.2022.120368_bb0310",
"volume": "206",
"year": "2018"
},
{
"DOI": "10.32794/mr11250081",
"article-title": "Melatonin: a potential therapeutic agent against COVID-19",
"author": "Gurunathan",
"doi-asserted-by": "crossref",
"first-page": "30",
"journal-title": "Melatonin Res.",
"key": "10.1016/j.lfs.2022.120368_bb0315",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.32794/mr11250091",
"article-title": "An urgent proposal for the immediate use of melatonin as an adjuvant to anti- SARS-CoV-2 vaccination",
"author": "Cardinali",
"doi-asserted-by": "crossref",
"first-page": "206",
"journal-title": "Melatonin Res.",
"key": "10.1016/j.lfs.2022.120368_bb0320",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1002/rmv.1714",
"article-title": "Beneficial actions of melatonin in the management of viral infections: a new use for this “molecular handyman”?",
"author": "Boga",
"doi-asserted-by": "crossref",
"first-page": "323",
"journal-title": "Rev. Med. Virol.",
"key": "10.1016/j.lfs.2022.120368_bb0325",
"volume": "22",
"year": "2012"
},
{
"DOI": "10.3389/fimmu.2020.576745",
"article-title": "ACE2/ADAM17/TMPRSS2 interplay may be the main risk factor for COVID-19",
"author": "Zipeto",
"doi-asserted-by": "crossref",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.lfs.2022.120368_bb0330",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.33549/physiolres.934754",
"article-title": "Interactions of renin-angiotensin system and COVID-19: the importance of daily rhythms in ACE2, ADAM17 and TMPRSS2 expression",
"author": "Zlacká",
"doi-asserted-by": "crossref",
"first-page": "S177",
"journal-title": "Physiol. Res.",
"key": "10.1016/j.lfs.2022.120368_bb0335",
"year": "2021"
},
{
"DOI": "10.1111/jpi.12200",
"article-title": "Melatonin stimulates the nonamyloidogenic processing of βaPP through the positive transcriptional regulation of ADAM10 and ADAM17",
"author": "Shukla",
"doi-asserted-by": "crossref",
"first-page": "151",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0340",
"volume": "58",
"year": "2015"
},
{
"DOI": "10.1016/j.mehy.2021.110627",
"article-title": "Does serotonin deficiency lead to anosmia, ageusia, dysfunctional chemesthesis and increased severity of illness in COVID-19?",
"author": "Sen",
"doi-asserted-by": "crossref",
"journal-title": "Med. Hypotheses",
"key": "10.1016/j.lfs.2022.120368_bb0345",
"volume": "153",
"year": "2021"
},
{
"DOI": "10.7150/ijms.48053",
"article-title": "COVID-19: rational discovery of the therapeutic potential of melatonin as a SARS-CoV-2 main protease inhibitor",
"author": "Feitosa",
"doi-asserted-by": "crossref",
"first-page": "2133",
"journal-title": "Int. J. Med. Sci.",
"key": "10.1016/j.lfs.2022.120368_bb0350",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.lfs.2020.118096",
"article-title": "Matrix metallopeptidase 9 as a host protein target of chloroquine and melatonin for immunoregulation in COVID-19: a network-based meta-analysis",
"author": "Hazra",
"doi-asserted-by": "crossref",
"journal-title": "Life Sci.",
"key": "10.1016/j.lfs.2022.120368_bb0355",
"volume": "257",
"year": "2020"
},
{
"DOI": "10.1111/jpi.12772",
"article-title": "Therapeutic potential of melatonin and melatonergic drugs on K18-hACE2 mice infected with SARS-CoV-2",
"author": "Cecon",
"doi-asserted-by": "crossref",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0360",
"volume": "72",
"year": "2022"
},
{
"article-title": "Melatonin drugs inhibit SARS-CoV-2 entry into the brain and virus-induced damage of cerebral small vessels",
"author": "Cecon",
"journal-title": "BioRxiv.",
"key": "10.1016/j.lfs.2022.120368_bb0365",
"year": "2022"
},
{
"article-title": "CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells",
"author": "Wang",
"journal-title": "Signal Transduct. Target. Ther.",
"key": "10.1016/j.lfs.2022.120368_bb0370",
"volume": "5",
"year": "2020"
},
{
"article-title": "CD147-spike protein interaction in COVID-19: get the ball rolling with a novel receptor and therapeutic target",
"author": "Behl",
"journal-title": "Sci. Total Environ.",
"key": "10.1016/j.lfs.2022.120368_bb0375",
"volume": "808",
"year": "2021"
},
{
"DOI": "10.32794/mr11250069",
"article-title": "The potential of melatonin in the prevention and attenuation of oxidative hemolysis and myocardial injury from cd147 SARS-CoV-2 spike protein receptor binding",
"author": "Loh",
"doi-asserted-by": "crossref",
"first-page": "380",
"journal-title": "Melatonin Res.",
"key": "10.1016/j.lfs.2022.120368_bb0380",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.3390/v13040659",
"article-title": "Melatonin inhibits dengue virus infection via the sirtuin 1-mediated interferon pathway",
"author": "Morchang",
"doi-asserted-by": "crossref",
"journal-title": "Viruses.",
"key": "10.1016/j.lfs.2022.120368_bb0385",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1111/jpi.12754",
"article-title": "Melatonin and other indoles show antiviral activities against swine coronaviruses in vitro at pharmacological concentrations",
"author": "Zhai",
"doi-asserted-by": "crossref",
"journal-title": "J. Pineal Res.",
"key": "10.1016/j.lfs.2022.120368_bb0390",
"volume": "71",
"year": "2021"
},
{
"DOI": "10.32794/mr11250077",
"article-title": "Melatonin attenuates growth factor receptor signaling required for SARS-CoV-2 replication",
"author": "Tesarik",
"doi-asserted-by": "crossref",
"first-page": "534",
"journal-title": "Melatonin Res.",
"key": "10.1016/j.lfs.2022.120368_bb0395",
"volume": "3",
"year": "2020"
},
{
"DOI": "10.1016/j.molcel.2020.08.006",
"article-title": "Growth factor receptor signaling inhibition prevents SARS-CoV-2 replication",
"author": "Klann",
"doi-asserted-by": "crossref",
"first-page": "164",
"journal-title": "Mol. Cell",
"key": "10.1016/j.lfs.2022.120368_bb0400",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1007/978-1-4939-2438-7_1",
"article-title": "Coronaviruses: an overview of their replication and pathogenesis",
"author": "Fehr",
"doi-asserted-by": "crossref",
"first-page": "1",
"journal-title": "Coronaviruses.",
"key": "10.1016/j.lfs.2022.120368_bb0405",
"volume": "1282",
"year": "2015"
},
{
"DOI": "10.1126/science.1085658",
"article-title": "Coronavirus main proteinase (3CLpro) structure: basis for design of anti-SARS drugs",
"author": "Anand",
"doi-asserted-by": "crossref",
"first-page": "1763",
"journal-title": "Science",
"key": "10.1016/j.lfs.2022.120368_bb0410",
"volume": "300",
"year": "2003"
},
{
"DOI": "10.1016/j.bmcl.2010.01.152",
"article-title": "SARS-CoV 3CLpro inhibitory effects of quinone-methide triterpenes from tripterygium regelii",
"author": "Ryu",
"doi-asserted-by": "crossref",
"first-page": "1873",
"journal-title": "Bioorg. Med. Chem. Lett.",
"key": "10.1016/j.lfs.2022.120368_bb0415",
"volume": "20",
"year": "2010"
},
{
"DOI": "10.1016/j.lfs.2020.117583",
"article-title": "COVID-19: melatonin as a potential adjuvant treatment",
"author": "Zhang",
"doi-asserted-by": "crossref",
"journal-title": "Life Sci.",
"key": "10.1016/j.lfs.2022.120368_bb0420",
"volume": "250",
"year": "2020"
},
{
"DOI": "10.1038/s41421-020-0153-3",
"article-title": "Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2",
"author": "Zhou",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "Cell Discov.",
"key": "10.1016/j.lfs.2022.120368_bb0425",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1371/journal.pbio.3000970",
"article-title": "A network medicine approach to investigation and population-based validation of disease manifestations and drug repurposing for COVID-19",
"author": "Zhou",
"doi-asserted-by": "crossref",
"journal-title": "PLoS Biol.",
"key": "10.1016/j.lfs.2022.120368_bb0430",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1016/j.ejphar.2021.174193",
"article-title": "Evaluation of Th1 and Th2 mediated cellular and humoral immunity in patients with COVID-19 following the use of melatonin as an adjunctive treatment",
"author": "Hosseini",
"doi-asserted-by": "crossref",
"journal-title": "Eur. J. Pharmacol.",
"key": "10.1016/j.lfs.2022.120368_bb0435",
"volume": "904",
"year": "2021"
},
{
"DOI": "10.32794/mr11250063",
"article-title": "Melatonin as adjuvant treatment for coronavirus disease 2019 pneumonia patients requiring hospitalization (MAC-19 PRO): a case series",
"author": "Castillo",
"doi-asserted-by": "crossref",
"first-page": "297",
"journal-title": "Melatonin Res.",
"key": "10.1016/j.lfs.2022.120368_bb0440",
"volume": "3",
"year": "2020"
},
{
"article-title": "Melatonin is significantly associated with survival of intubated COVID-19 patients",
"author": "Ramlall",
"journal-title": "MedRxiv Prepr. Serv. Heal. Sci.",
"key": "10.1016/j.lfs.2022.120368_bb0445",
"year": "2020"
},
{
"article-title": "What if melatonin could help COVID-19 severe patients?",
"author": "Sánchez-González",
"journal-title": "J. Clin. Sleep Med.",
"key": "10.1016/j.lfs.2022.120368_bb0450",
"year": "2021"
},
{
"article-title": "The effect of melatonin on thrombosis, sepsis and mortality rate in COVID-19 patients",
"author": "Hasan",
"journal-title": "Int. J. Infect. Dis.",
"key": "10.1016/j.lfs.2022.120368_bb0455",
"year": "2021"
},
{
"DOI": "10.1155/2021/9822706",
"article-title": "Kinetics of neutralizing antibody response underscores clinical COVID-19 progression",
"author": "Lei",
"doi-asserted-by": "crossref",
"journal-title": "J. Immunol. Res.",
"key": "10.1016/j.lfs.2022.120368_bb0460",
"volume": "2021",
"year": "2021"
},
{
"DOI": "10.1002/jmv.27518",
"article-title": "Sequential dynamics of virological and serological changes in the serum of SARS-CoV-2 infected patients",
"author": "Ouoba",
"doi-asserted-by": "crossref",
"journal-title": "J. Med. Virol.",
"key": "10.1016/j.lfs.2022.120368_bb0465",
"year": "2021"
},
{
"DOI": "10.1017/S0950268820001430",
"article-title": "Epidemiological characteristics of COVID-19: a systematic review and meta-analysis",
"author": "Khalili",
"doi-asserted-by": "crossref",
"journal-title": "Epidemiol. Infect.",
"key": "10.1016/j.lfs.2022.120368_bb0470",
"volume": "148",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2021436",
"article-title": "Dexamethasone in hospitalized patients with Covid-19",
"doi-asserted-by": "crossref",
"first-page": "693",
"journal-title": "N. Engl. J. Med.",
"key": "10.1016/j.lfs.2022.120368_bb0475",
"volume": "384",
"year": "2021"
},
{
"DOI": "10.12659/AJCR.930733",
"article-title": "Glycemic profile of intravenous dexamethasone-induced hyperglycemia using continuous glucose monitoring",
"author": "Zhang",
"doi-asserted-by": "crossref",
"journal-title": "Am. J. Case Rep.",
"key": "10.1016/j.lfs.2022.120368_bb0480",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1177/20587384211063976",
"article-title": "Systemic corticosteroids for management of COVID-19: saving lives or causing harm?",
"author": "FakhriRavari",
"doi-asserted-by": "crossref",
"journal-title": "Int. J. Immunopathol. Pharmacol.",
"key": "10.1016/j.lfs.2022.120368_bb0485",
"volume": "35",
"year": "2021"
},
{
"article-title": "Covid-19: UK becomes first country to authorise antiviral molnupiravir",
"author": "Mahase",
"journal-title": "BMJ",
"key": "10.1016/j.lfs.2022.120368_bb0490",
"volume": "375",
"year": "2021"
},
{
"DOI": "10.47287/cen-09942-buscon14",
"doi-asserted-by": "crossref",
"key": "10.1016/j.lfs.2022.120368_bb0495",
"unstructured": "Pfizer’s Novel COVID-19 Oral Antiviral Treatment Candidate Reduced Risk of Hospitalization or Death by 89% in Interim Analysis of Phase 2/3 EPIC-HR Study | Pfizer, (n.d.). https://www.pfizer.com/news/press-release/press-release-detail/pfizers-novel-covid-19-oral-antiviral-treatment-candidate (accessed November 24, 2021)."
},
{
"DOI": "10.1016/S0140-6736(21)02657-X",
"article-title": "Caution required with use of ritonavir-boosted PF-07321332 in COVID-19 management",
"author": "Heskin",
"doi-asserted-by": "crossref",
"first-page": "21",
"journal-title": "Lancet (London, England)",
"key": "10.1016/j.lfs.2022.120368_bb0500",
"volume": "399",
"year": "2022"
},
{
"DOI": "10.1124/dmd.104.002410",
"article-title": "Metabolism of melatonin by human cytochromes p450",
"author": "Ma",
"doi-asserted-by": "crossref",
"first-page": "489",
"journal-title": "Drug Metab. Dispos.",
"key": "10.1016/j.lfs.2022.120368_bb0505",
"volume": "33",
"year": "2005"
},
{
"DOI": "10.1007/s41782-020-00111-7",
"article-title": "Elderly as a high-risk group during COVID-19 pandemic: effect of circadian misalignmentSleep Dysregulation and Melatonin Administration",
"author": "Cardinali",
"doi-asserted-by": "crossref",
"first-page": "81",
"journal-title": "Sleep Vigil.",
"key": "10.1016/j.lfs.2022.120368_bb0510",
"volume": "4",
"year": "2020"
},
{
"DOI": "10.1523/JNEUROSCI.20-08-02825.2000",
"article-title": "Cytochrome c release and caspase activation in traumatic axonal injury",
"author": "Büki",
"doi-asserted-by": "crossref",
"first-page": "2825",
"journal-title": "J. Neurosci.",
"key": "10.1016/j.lfs.2022.120368_bb0515",
"volume": "20",
"year": "2000"
},
{
"DOI": "10.1016/j.lfs.2020.117902",
"article-title": "Is melatonin deficiency a unifying pathomechanism of high risk patients with COVID-19?",
"author": "Simko",
"doi-asserted-by": "crossref",
"journal-title": "Life Sci.",
"key": "10.1016/j.lfs.2022.120368_bb0520",
"volume": "256",
"year": "2020"
},
{
"key": "10.1016/j.lfs.2022.120368_bb0525",
"unstructured": "Regeneron Announces New U.S. Government Agreement to Purchase Additional Doses of REGEN-COVTM (casirivimab and imdevimab) Antibody Cocktail | Regeneron Pharmaceuticals Inc., (n.d.). https://investor.regeneron.com/news-releases/news-release-details/regeneron-announces-new-us-government-agreement-purchase (accessed November 24, 2021)."
},
{
"key": "10.1016/j.lfs.2022.120368_bb0530",
"unstructured": "Gilead’s coronavirus treatment remdesivir to cost $3,120 for U.S. insured patients, (n.d.). https://www.cnbc.com/2020/06/29/gileads-coronavirus-treatment-remdesivir-to-cost-3120-for-us-insured-patients.html (accessed November 24, 2021)."
},
{
"key": "10.1016/j.lfs.2022.120368_bb0535",
"unstructured": "Merck’s COVID Pills Price Could Change From $700 Federal Government Paid, (n.d.). https://www.newsweek.com/merck-covid-pill-cost-molnupiravir-1637550 (accessed January 4, 2022)."
},
{
"key": "10.1016/j.lfs.2022.120368_bb0540",
"unstructured": "U.S. authorizes Pfizer oral COVID-19 treatment, first for at-home use | Reuters, (n.d.). https://www.reuters.com/business/healthcare-pharmaceuticals/pfizer-oral-covid-19-pill-gets-us-authorization-at-home-use-2021-12-22/ (accessed January 4, 2022)."
}
],
"reference-count": 108,
"references-count": 108,
"relation": {},
"score": 1,
"short-container-title": [
"Life Sciences"
],
"short-title": [],
"source": "Crossref",
"subject": [
"General Pharmacology, Toxicology and Pharmaceutics",
"General Biochemistry, Genetics and Molecular Biology",
"General Medicine"
],
"subtitle": [],
"title": [
"Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality"
],
"type": "journal-article"
}