The Coronavirus Disease 2019 (COVID-19): Key Emphasis on Melatonin Safety and Therapeutic Efficacy
et al., Antioxidants, doi:10.3390/antiox10071152 , Jul 2021
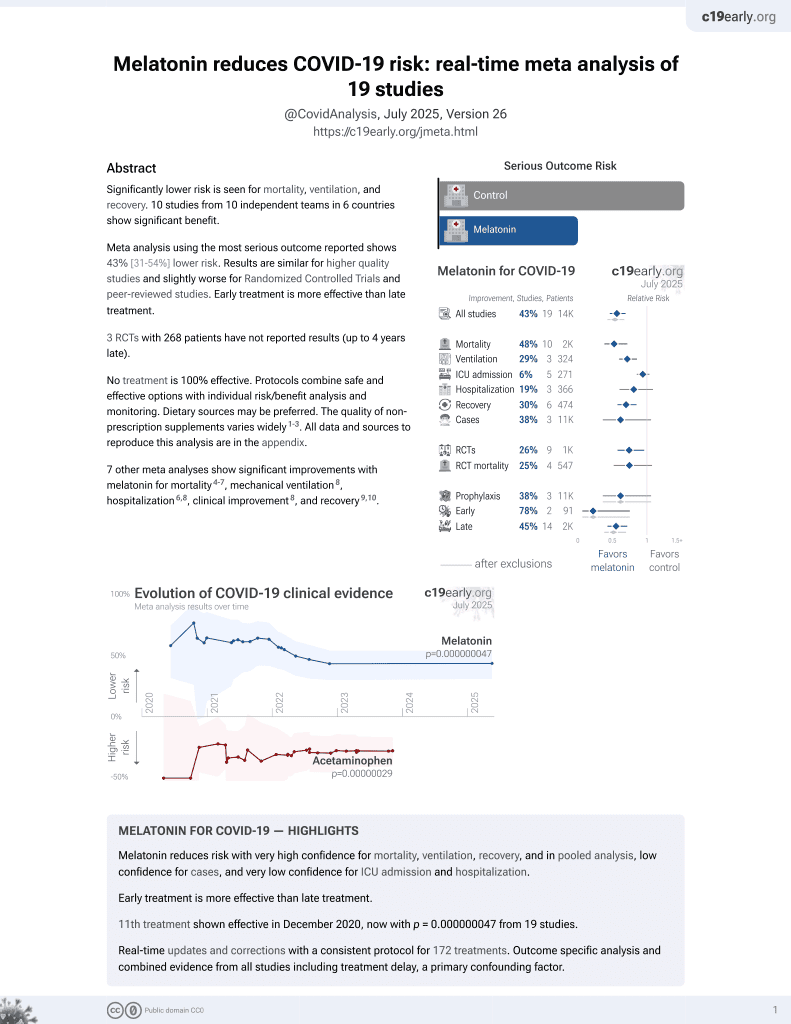
Melatonin for COVID-19
12th treatment shown to reduce risk in
December 2020, now with p = 0.0000000099 from 19 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Review of melatonin for COVID-19 discussing mechanisms of action and ongoing trials.
1.
Chen et al., Viral mitochondriopathy in COVID-19, Redox Biology, doi:10.1016/j.redox.2025.103766.
2.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
3.
Xie et al., The role of reactive oxygen species in severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) infection-induced cell death, Cellular & Molecular Biology Letters, doi:10.1186/s11658-024-00659-6.
4.
Zhao et al., Melatonin Potentially Acts as a Widely-Acting Protective Tool in COVID-19, Medicine Research, doi:10.21127/yaoyimr20240006.
5.
Yehia et al., Melatonin: a ferroptosis inhibitor with potential therapeutic efficacy for the post-COVID-19 trajectory of accelerated brain aging and neurodegeneration, Molecular Neurodegeneration, doi:10.1186/s13024-024-00728-6.
6.
Chacin-Bonilla et al., Melatonin and viral infections: A review focusing on therapeutic effects and SARS-CoV-2, Melatonin Research, doi:10.32794/mr112500168.
7.
Lempesis et al., A mid‑pandemic night's dream: Melatonin, from harbinger of anti‑inflammation to mitochondrial savior in acute and long COVID‑19 (Review), International Journal of Molecular Medicine, doi:10.3892/ijmm.2024.5352.
8.
Alomari et al., Assessing the antiviral potential of melatonin: A comprehensive systematic review, Reviews in Medical Virology, doi:10.1002/rmv.2499.
9.
Donzelli, A., Neglected Effective Early Therapies against COVID-19: Focus on Functional Foods and Related Active Substances. A Review, MDPI AG, doi:10.20944/preprints202312.1178.v1.
10.
Langen, M., Melatonin - the Hormone of Both Sun and Darkness - Protects Your Health and Can Save Your Life, Rounding The Earth, roundingtheearth.substack.com/p/melatonin-the-hormone-of-both-sun.
11.
Hosseinzadeh et al., Melatonin effect on platelets and coagulation: Implications for a prophylactic indication in COVID-19, Life Sciences, doi:10.1016/j.lfs.2022.120866.
12.
Loh et al., Melatonin: Regulation of Viral Phase Separation and Epitranscriptomics in Post-Acute Sequelae of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms23158122.
13.
Reiter et al., Melatonin: highlighting its use as a potential treatment for SARS-CoV-2 infection, Cellular and Molecular Life Sciences, doi:10.1007/s00018-021-04102-3.
14.
Tan et al., Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality, Life Sciences, doi:10.1016/j.lfs.2022.120368.
15.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
16.
Castle et al., Implications for Systemic Approaches to COVID-19: Effect Sizes of Remdesivir, Tocilizumab, Melatonin, Vitamin D3, and Meditation, Journal of Inflammation Research, doi:10.2147/JIR.S323356.
17.
Ramos et al., The Coronavirus Disease 2019 (COVID-19): Key Emphasis on Melatonin Safety and Therapeutic Efficacy, Antioxidants, doi:10.3390/antiox10071152.
18.
Camp et al., Melatonin interferes with COVID-19 at several distinct ROS-related steps, Journal of Inorganic Biochemistry, doi:10.1016/j.jinorgbio.2021.111546.
19.
Cross et al., Melatonin for the Early Treatment of COVID-19: A Narrative Review of Current Evidence and Possible Efficacy, Endocrine Practice, doi:10.1016/j.eprac.2021.06.001.
20.
DiNicolantonio et al., Melatonin may decrease risk for and aid treatment of COVID-19 and other RNA viral infections, Open Heart, doi:10.1136/openhrt-2020-001568.
21.
Reiter (B) et al., Therapeutic Algorithm for Use of Melatonin in Patients With COVID-19, Frontiers in Medicine, doi:10.3389/fmed.2020.00226.
22.
Charaa et al., Prophylactic Treatment Protocol against the Severity of COVID-19 Using Melatonin, SSRN, doi:10.2139/ssrn.3601861.
Ramos et al., 20 Jul 2021, peer-reviewed, 10 authors.
The Coronavirus Disease 2019 (COVID-19): Key Emphasis on Melatonin Safety and Therapeutic Efficacy
Antioxidants, doi:10.3390/antiox10071152
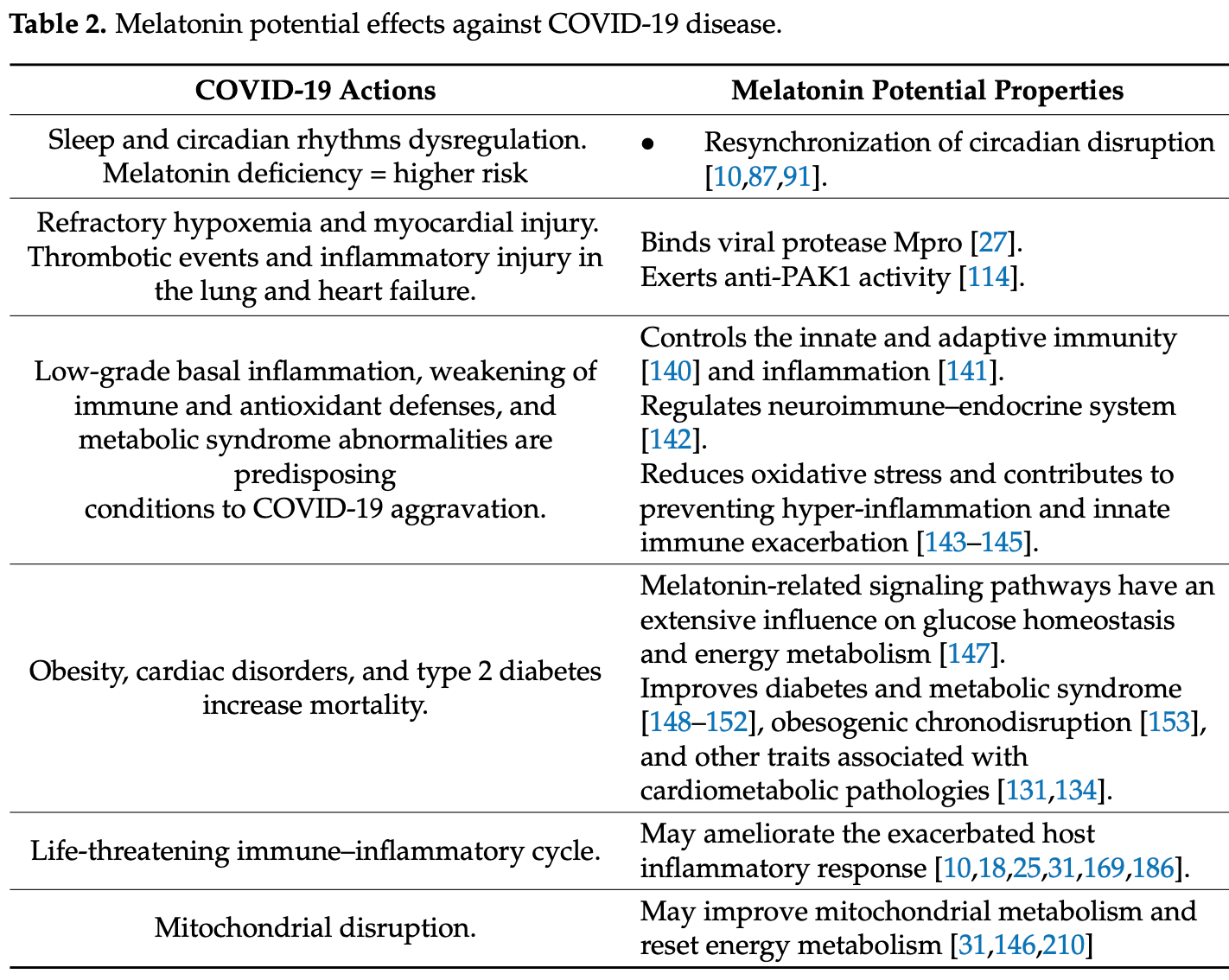
Viral infections constitute a tectonic convulsion in the normophysiology of the hosts. The current coronavirus disease 2019 (COVID-19) pandemic is not an exception, and therefore the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, like any other invading microbe, enacts a generalized immune response once the virus contacts the body. Melatonin is a systemic dealer that does not overlook any homeostasis disturbance, which consequently brings into play its cooperative triad, antioxidant, anti-inflammatory, and immune-stimulant backbone, to stop the infective cycle of SARS-CoV-2 or any other endogenous or exogenous threat. In COVID-19, the corporal propagation of SARS-CoV-2 involves an exacerbated oxidative activity and therefore the overproduction of great amounts of reactive oxygen and nitrogen species (RONS). The endorsement of melatonin as a possible protective agent against the current pandemic is indirectly supported by its widely demonstrated beneficial role in preclinical and clinical studies of other respiratory diseases. In addition, focusing the therapeutic action on strengthening the host protection responses in critical phases of the infective cycle makes it likely that multi-tasking melatonin will provide multi-protection, maintaining its efficacy against the virus variants that are already emerging and will emerge as long as SARS-CoV-2 continues to circulate among us.
References
Abood, Abdulsahib, Hussain, Ismail, Melatonin potentiates the therapeutic effects of metformin in women with metabolic syndrome, Sci. Pharm, doi:10.3390/scipharm88020028
Acuna-Castroviejo, Carretero, Doerrier, Lopez, Garcia-Corzo et al., Melatonin protects lung mitochondria from aging, Age, doi:10.1007/s11357-011-9267-8
Acuna-Castroviejo, Escames, Figueira, De La Oliva, Borobia et al., Clinical trial to test the efficacy of melatonin in COVID-19, J. Pineal Res, doi:10.1111/jpi.12683
Ahmed, Avoiding room light during night may stimulate immunity in COVID-19 patients by promoting melatonin production, Melatonin Res, doi:10.32794/mr11250073
Akbari, Ostadmohammadi, Tabrizi, Lankarani, Heydari et al., The effects of melatonin supplementation on inflammatory markers among patients with metabolic syndrome or related disorders: A systematic review and meta-analysis of randomized controlled trials, Inflammopharmacology, doi:10.1007/s10787-018-0508-7
Al-Zaqri, Pooventhiran, Alsalme, Warad, John et al., Structural and physico-chemical evaluation of melatonin and its solution-state excited properties, with emphasis on its binding with novel coronavirus proteins, J. Mol. Liq, doi:10.1016/j.molliq.2020.114082
Anand, Tikoo, Viruses as modulators of mitochondrial functions, Adv. Virol, doi:10.1155/2013/738794
Andersen, Werner, Rosenkilde, Fenger, Petersen et al., Pharmacokinetics of high-dose intravenous melatonin in humans, J. Clin. Pharmacol, doi:10.1002/jcph.592
Anderson, Carbone, Mazzoccoli, Aryl hydrocarbon receptor role in co-ordinating sars-cov-2 entry and symptomatology: Linking cytotoxicity changes in COVID-19 and cancers; modulation by racial discrimination stress, Biology, doi:10.3390/biology9090249
Anderson, Carbone, Mazzoccoli, Tryptophan metabolites and aryl hydrocarbon receptor in severe acute respiratory syndrome, Coronavirus-2 (SARS-CoV-2) pathophysiology, Int. J. Mol. Sci, doi:10.3390/ijms22041597
Anderson, Reiter, COVID-19 pathophysiology: Interactions of gut microbiome, melatonin, vitamin D, stress, kynurenine and the alpha 7 nicotinic receptor: Treatment implications, Melatonin Res, doi:10.32794/mr11250066
Anderson, Reiter, Melatonin: Roles in influenza, Covid-19, and other viral infections, Rev. Med. Virol, doi:10.1002/rmv.2109
Anderson, Rodriguez, Reiter, Multiple sclerosis: Melatonin, orexin, and ceramide interact with platelet activation coagulation factors and gut-microbiome-derived butyrate in the circadian dysregulation of mitochondria in glia and immune cells, Int. J. Mol. Sci, doi:10.3390/ijms20215500
Anisimov, Popovich, Zabezhinski, Anisimov, Vesnushkin et al., Melatonin as antioxidant, geroprotector and anticarcinogen, Biochim. Biophys. Acta, doi:10.1016/j.bbabio.2006.03.012
Arendt, Skene, Melatonin as a chronobiotic, Sleep Med. Rev, doi:10.1016/j.smrv.2004.05.002
Artigas, Coma, Matos-Filipe, Aguirre-Plans, Farres et al., In-silico drug repurposing study predicts the combination of pirfenidone and melatonin as a promising candidate therapy to reduce SARS-CoV-2 infection progression and respiratory distress caused by cytokine storm, PLoS ONE, doi:10.1371/journal.pone.0240149
Bansal, Gubbi, Muniyappa, Metabolic syndrome and COVID 19: Endocrine-immune-vascular interactions shapes clinical course, Endocrinology, doi:10.1210/endocr/bqaa112
Barek, Aziz, Islam, Impact of age, sex, comorbidities and clinical symptoms on the severity of COVID-19 cases: A meta-analysis with 55 studies and 10014 cases, Heliyon, doi:10.1016/j.heliyon.2020.e05684
Barone, Ngongo, Menna-Barreto, Sleep-wake cycle impairment adding on the risk for COVID-19 severity in people with diabetes, Sleep Sci, doi:10.5935/1984-0063.20200038
Batabyal, Freishtat, Hill, Rehman, Freishtat et al., Metabolic dysfunction and immunometabolism in COVID-19 pathophysiology and therapeutics, Int. J. Obes, doi:10.1038/s41366-021-00804-7
Baumgartner, Lam, Lai, Barnett, Thompson et al., Effectiveness of melatonin for the prevention of intensive care unit delirium, Pharmacotherapy, doi:10.1002/phar.2222
Biswas, Rahaman, Biswas, Haque, Ibrahim, Association of sex, age, and comorbidities with mortality in covid-19 patients: A systematic review and meta-analysis, Intervirology, doi:10.1159/000512592
Blanco-Melo, Nilsson-Payant, Liu, Uhl, Hoagland et al., Imbalanced host response to SARS-CoV-2 drives development of COVID-19, Cell, doi:10.1016/j.cell.2020.04.026
Boga, Coto-Montes, Rosales-Corral, Tan, Reiter, Beneficial actions of melatonin in the management of viral infections: A new use for this "molecular handyman, Rev. Med. Virol, doi:10.1002/rmv.1714
Bonilla, Valero, Chacin-Bonilla, Medina-Leendertz, Melatonin and viral infections, J. Pineal Res
Bouhafs, Jarstrand, Effects of antioxidants on surfactant peroxidation by stimulated human polymorphonuclear leukocytes, Free Radic. Res, doi:10.1080/10715760290032593
Brown, Karthikeyan, Pandi-Perumal, Cardinali, Autism spectrum disorder patients may be susceptible to COVID-19 disease due to deficiency in melatonin, Med. Hypotheses, doi:10.1016/j.mehy.2021.110544
Brum, Filho, Schnorr, Bottega, Rodrigues, Shift work and its association with metabolic disorders, Diabetol. Metab. Syndr, doi:10.1186/s13098-015-0041-4
Calvo, Guerrero, Osuna, Molinero, Carrillo-Vico, Melatonin triggers Crohn's disease symptoms, J. Pineal Res, doi:10.1034/k.1600-079x.2002.01881.x
Capote-Moreno, Ramos, Egea, Lopez-Munoz, Gil-Martin et al., Potential of melatonin as adjuvant therapy of oral cancer in the era of epigenomics, Cancers, doi:10.3390/cancers11111712
Cardinali, Brown, Pandi-Perumal, An urgent proposal for the immediate use of melatonin as an adjuvant to anti-SARS-CoV-2 vaccination, Melatonin Res, doi:10.32794/mr11250091
Cardinali, Brown, Pandi-Perumal, Can melatonin be a potential "Silver Bullet" in treating COVID-19 patients?, Diseases, doi:10.3390/diseases8040044
Cardinali, Brown, Reiter, Pandi-Perumal, Elderly as a high-risk group during COVID-19 pandemic: Effect of circadian misalignment, sleep dysregulation and melatonin administration, Sleep Vigil, doi:10.1007/s41782-020-00111-7
Cardinali, Hardeland, Inflammaging, metabolic syndrome and melatonin: A call for treatment studies, Neuroendocrinology, doi:10.1159/000446543
Cardinali, High doses of melatonin as a potential therapeutic tool for the neurologic sequels of covid-19 infection, Melatonin Res, doi:10.32794/mr11250064
Cardinali, Vigo, Melatonin, mitochondria, and the metabolic syndrome, Cell. Mol. Life Sci, doi:10.1007/s00018-017-2611-0
Carrillo-Vico, Calvo, Abreu, Lardone, Garcia-Maurino et al., Evidence of melatonin synthesis by human lymphocytes and its physiological significance: Possible role as intracrine, autocrine, and/or paracrine substance, FASEB J, doi:10.1096/fj.03-0694fje
Carrillo-Vico, Lardone, Alvarez-Sanchez, Rodriguez-Rodriguez, Guerrero, Melatonin: Buffering the immune system, Int. J. Mol. Sci, doi:10.3390/ijms14048638
Castillo, Quizon, Juco, Roman, De Leon et al., Melatonin as adjuvant treatment for coronavirus disease 2019 pneumonia patients requiring hospitalization (MAC-19 PRO): A case series, Melatonin Res, doi:10.32794/mr11250063
Chakraborty, Maity, COVID-19 outbreak: Migration, effects on society, global environment and prevention, Sci. Total Environ, doi:10.1016/j.scitotenv.2020.138882
Chan, Kok, Zhu, Chu, To et al., Genomic characterization of the 2019 novel humanpathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan, Emerg. Microbes Infect, doi:10.1080/22221751.2020.1719902
Chavarria, Vazquez, Cherit, Bello, Suastegui et al., Antioxidants and pentoxifylline as coadjuvant measures to standard therapy to improve prognosis of patients with pneumonia by COVID-19, Comput. Struct. Biotechnol. J, doi:10.1016/j.csbj.2021.02.009
Chen, Huang, Chen, Wang, Yang et al., Melatonin enhances interleukin-10 expression and suppresses chemotaxis to inhibit inflammation in situ and reduce the severity of experimental autoimmune encephalomyelitis, Int. Immunopharmacol, doi:10.1016/j.intimp.2015.12.020
Chen, Zhang, Wei, Cai, Yao et al., Association between cytokine profiles and lung injury in COVID-19 pneumonia, Respir. Res, doi:10.1186/s12931-020-01465-2
Cheng, Luo, Wang, Zhang, Wang et al., Kidney disease is associated with in-hospital death of patients with COVID-19, Kidney Int, doi:10.1016/j.kint.2020.03.005
Cheng, Rao, Mehra, COVID-19 treatment: Combining anti-inflammatory and antiviral therapeutics using a network-based approach, Clevel. Clin. J. Med, doi:10.3949/ccjm.87a.ccc037
Choudhury, Das, Patra, Mukherjee, In silico analyses on the comparative sensing of SARS-CoV-2 mRNA by the intracellular TLRs of humans, J. Med. Virol, doi:10.1002/jmv.26776
Cipolla-Neto, Amaral, Afeche, Tan, Reiter, Melatonin, energy metabolism, and obesity: A review, J. Pineal Res, doi:10.1111/jpi.12137
Crespi, Evolutionary medical insights into the SARS-CoV-2 pandemic, Evol. Med. Public Health, doi:10.1093/emph/eoaa036
Cuadrado, Pajares, Benito, Jimenez-Villegas, Escoll et al., Can activation of NRF2 be a strategy against COVID-19?, Trends Pharmacol. Sci, doi:10.1016/j.tips.2020.07.003
Cunha, Perazzio, Azzi, Cravedi, Riella, Remodeling of the immune response with aging: Immunosenescence and its potential impact on COVID-19 immune response, Front. Immunol, doi:10.3389/fimmu.2020.01748
Cutando, Lopez-Valverde, Arias-Santiago, De Vicente, De Diego, Role of melatonin in cancer treatment, Anticancer Res
De Bleecker, Lamont, Verstraete, Schelfhout, Melatonin and painful gynecomastia, Neurology
Dinicolantonio, Mccarty, Barroso-Aranda, Melatonin may decrease risk for and aid treatment of COVID-19 and other RNA viral infections, Open Heart, doi:10.1136/openhrt-2020-001568
Donoghue, Hsieh, Baronas, Godbout, Gosselin et al., A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9, Circ. Res, doi:10.1161/01.RES.87.5.e1
Dorward, Russell, Um, Elshani, Armstrong et al., Tissue-specific tolerance in fatal Covid-19, medRxiv, doi:10.1101/2020.07.02.20145003
El-Missiry, El-Missiry, Othman, Melatonin is a potential adjuvant to improve clinical outcomes in individuals with obesity and diabetes with coexistence of Covid-19, Eur. J. Pharmacol, doi:10.1016/j.ejphar.2020.173329
Esser, Paquot, Scheen, Inflammatory markers and cardiometabolic diseases, Acta Clin. Belg
Farre-Alins, Narros-Fernandez, Palomino-Antolin, Decouty-Perez, Lopez-Rodriguez et al., Melatonin reduces NLRP3 inflammasome activation by increasing alpha7 nAChR-mediated autophagic flux, Antioxidants, doi:10.3390/antiox9121299
Feitosa, Junior, Neto, Matos, Moura et al., COVID-19: Rational discovery of the therapeutic potential of melatonin as a SARS-CoV-2 main protease inhibitor, Int. J. Med. Sci, doi:10.7150/ijms.48053
Ferlazzo, Andolina, Cannata, Costanzo, Rizzo et al., Is melatonin the cornucopia of the 21st century?, Antioxidants, doi:10.3390/antiox9111088
Fernandes, Cecon, Markus, Ferreira, Effect of TNF-alpha on the melatonin synthetic pathway in the rat pineal gland: Basis for a 'feedback' of the immune response on circadian timing, J. Pineal Res, doi:10.1111/j.1600-079X.2006.00373.x
Foley, Steel, Adverse events associated with oral administration of melatonin: A critical systematic review of clinical evidence, Complement. Ther. Med, doi:10.1016/j.ctim.2018.11.003
Friedman, Analysis, nutrition, and health benefits of tryptophan, Int. J. Tryptophan Res, doi:10.1177/1178646918802282
Garcia, Rodriguez-Rubio, Mariblanca, De Soto, Garcia et al., A randomized multicenter clinical trial to evaluate the efficacy of melatonin in the prophylaxis of SARS-CoV-2 infection in high-risk contacts (MeCOVID Trial): A structured summary of a study protocol for a randomised controlled trial, Trials, doi:10.1186/s13063-020-04436-6
Gardinassi, Souza, Sales-Campos, Fonseca, Immune and metabolic signatures of COVID-19 revealed by transcriptomics data reuse, Front. Immunol, doi:10.3389/fimmu.2020.01636
Gatti, Ilamathi, Todkar, Germain, Mitochondria targeted viral replication and survival strategies-prospective on SARS-CoV-2, Front. Pharmacol, doi:10.3389/fphar.2020.578599
Gil-Martin, Egea, Reiter, Romero, The emergence of melatonin in oncology: Focus on colorectal cancer, Med. Res. Rev, doi:10.1002/med.21582
Gimenez, Inserra, Tajer, Mariani, Ferder et al., Lungs as target of COVID-19 infection: Protective common molecular mechanisms of vitamin D and melatonin as a new potential synergistic treatment, Life Sci, doi:10.1016/j.lfs.2020.117808
Golan, Kollet, Markus, Lapidot, Daily light and darkness onset and circadian rhythms metabolically synchronize hematopoietic stem cell differentiation and maintenance: The role of bone marrow norepinephrine, tumor necrosis factor, and melatonin cycles, Exp. Hematol, doi:10.1016/j.exphem.2019.08.008
Gomez-Pastora, Weigand, Kim, Wu, Strayer et al., Hyperferritinemia in critically ill COVID-19 patients-Is ferritin the product of inflammation or a pathogenic mediator?, Clin. Chim. Acta, doi:10.1016/j.cca.2020.06.033
Goyal, Terry, Superak, Nell-Dybdahl, Chowdhury et al., Melatonin supplementation to treat the metabolic syndrome: A randomized controlled trial, Diabetol. Metab. Syndr, doi:10.1186/1758-5996-6-124
Grilo-Bensusan, Gomez-Delgado, Gomez-Regife, Melatonin as a probable cause of diarrhoea, Rev. Esp. Enferm. Dig
Grunewald, Shaban, Mackin, Fehr, Perlman, Murine coronavirus infection activates the aryl hydrocarbon receptor in an indoleamine 2,3-dioxygenase-independent manner, contributing to cytokine modulation and proviral TCDDinducible-PARP expression, J. Virol, doi:10.1128/JVI.01743-19
Guan, Gao, Wang, Wen, Mao et al., Exploring the mechanism of liver enzyme abnormalities in patients with novel coronavirus-infected pneumonia, Zhonghua Gan Zang Bing Za Zhi, doi:10.3760/cma.j.issn.1007-3418.2020.02.002
Guzzi, Mercatelli, Ceraolo, Giorgi, Master regulator analysis of the SARS-CoV-2/human interactome, J. Clin. Med, doi:10.3390/jcm9040982
Habtemariam, Daglia, Sureda, Selamoglu, Gulhan et al., Melatonin and respiratory diseases: A review, Curr. Top. Med. Chem, doi:10.2174/1568026616666160824120338
Hardeland, Aging, melatonin, and the pro-and anti-inflammatory networks, Int. J. Mol. Sci, doi:10.3390/ijms20051223
Hardeland, Melatonin in aging and disease -multiple consequences of reduced secretion, options and limits of treatment, Aging Dis
Hardeland, Tan, Protection by melatonin in respiratory diseases: Valuable information for the treatment of COVID-19, Melatonin Res, doi:10.32794/mr11250061
Herrera, Gonzalez-Candia, Comment on Melatonin as a potential adjuvant treatment for COVID-19, Life Sci, doi:10.1016/j.lfs.2020.117739
Hosseinzadeh, Javad-Moosavi, Reiter, Hemati, Ghaznavi et al., Idiopathic pulmonary fibrosis (IPF) signaling pathways and protective roles of melatonin, Life Sci, doi:10.1016/j.lfs.2018.03.032
Hotamisligil, Inflammation and metabolic disorders, Nature, doi:10.1038/nature05485
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat. Rev. Microbiol
Hu, Huang, Yin, The cytokine storm and COVID-19, J. Med. Virol, doi:10.1002/jmv.26232
Huang, Liao, Chen, Shi, Lin et al., Melatonin possesses an anti-influenza potential through its immune modulatory effect, J. Funct. Foods, doi:10.1016/j.jff.2019.04.062
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Huang, Zheng, Jiang, Lin, Zhang et al., Effect of oral melatonin and wearing earplugs and eye masks on nocturnal sleep in healthy subjects in a simulated intensive care unit environment: Which might be a more promising strategy for ICU sleep deprivation?, Crit. Care, doi:10.1186/s13054-015-0842-8
Huo, Wang, Yu, Peng, Wang et al., Human transporters, PEPT1/2, facilitate melatonin transportation into mitochondria of cancer cells: An implication of the therapeutic potential, J. Pineal Res, doi:10.1111/jpi.12390
Hussman, Cellular and molecular pathways of COVID-19 and potential points of therapeutic intervention, Front. Pharmacol, doi:10.3389/fphar.2020.01169
Imenshahidi, Karimi, Hosseinzadeh, Effects of melatonin on cardiovascular risk factors and metabolic syndrome: A comprehensive review, Naunyn Schmiedebergs Arch. Pharmacol, doi:10.1007/s00210-020-01822-4
Jacob, Poeggeler, Weishaupt, Siren, Hardeland et al., Melatonin as a candidate compound for neuroprotection in amyotrophic lateral sclerosis (ALS): High tolerability of daily oral melatonin administration in ALS patients, J. Pineal Res, doi:10.1034/j.1600-079X.2002.02943.x
Jehi, Ji, Milinovich, Erzurum, Rubin et al., Individualizing risk prediction for positive coronavirus disease 2019 testing: Results from 11,672 patients, Chest, doi:10.1016/j.chest.2020.05.580
Jiang, Zhang, Meng, Xie, Li et al., SARS-CoV-2 Orf9b suppresses type I interferon responses by targeting TOM70, Cell. Mol. Immunol, doi:10.1038/s41423-020-0514-8
Jin, Bai, He, Wu, Liu et al., Gender differences in patients with COVID-19: Focus on severity and mortality, Front. Public Health, doi:10.3389/fpubh.2020.00152
Juybari, Pourhanifeh, Hosseinzadeh, Hemati, Mehrzadi, Melatonin potentials against viral infections including COVID-19: Current evidence and new findings, Virus Res, doi:10.1016/j.virusres.2020.198108
Karamitri, Jockers, Melatonin in type 2 diabetes mellitus and obesity, Nat. Rev. Endocrinol, doi:10.1038/s41574-018-0130-1
Karasek, Melatonin, human aging, and age-related diseases, Exp. Gerontol, doi:10.1016/j.exger.2004.04.012
Khomich, Kochetkov, Bartosch, Ivanov, Redox biology of respiratory viral infections, Viruses, doi:10.3390/v10080392
Klann, Bojkova, Tascher, Ciesek, Munch et al., Growth factor receptor signaling inhibition prevents SARS-CoV-2 replication, Mol. Cell, doi:10.1016/j.molcel.2020.08.006
Kleszczynski, Slominski, Steinbrink, Reiter, Clinical trials for use of melatonin to fight against COVID-19 are urgently needed, Nutrients, doi:10.3390/nu12092561
Kloc, Ghobrial, Kubiak, The role of genetic sex and mitochondria in response to COVID-19 infection, Int. Arch. Allergy Immunol, doi:10.1159/000508560
Kubatka, Zubor, Busselberg, Kwon, Adamek et al., Melatonin and breast cancer: Evidences from preclinical and human studies, Crit. Rev. Oncol. Hematol, doi:10.1016/j.critrevonc.2017.12.018
Kulkarni, Schow, Shubrook, Shift workers at risk for metabolic syndrome, J. Am. Osteopath. Assoc
Labonia, Rubio, Arias, Melatonin corrects reticuloendothelial blockade and iron status in haemodialysed patients, Nephrology, doi:10.1111/j.1440-1797.2005.00488.x
Lefkowitz, Dempsey, Hendrickson, Orton, Siddell et al., Virus taxonomy: The database of the International Committee on Taxonomy of Viruses (ICTV), Nucleic Acids Res, doi:10.1093/nar/gkx932
Li, Fan, Lai, Han, Li et al., Coronavirus infections and immune responses, J. Med. Virol, doi:10.1002/jmv.25685
Li, Jiang, Han, Yang, Lv et al., Exogenous melatonin as a treatment for secondary sleep disorders: A systematic review and meta-analysis, Front. Neuroendocr, doi:10.1016/j.yfrne.2018.06.004
Li, Li, Zhou, Meng, Zhang et al., Melatonin for the prevention and treatment of cancer, Oncotarget, doi:10.18632/oncotarget.16379
Li, Moore, Vasilieva, Sui, Wong et al., Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus, Nature, doi:10.1038/nature02145
Li, Structure, function, and evolution of coronavirus spike proteins, Annu. Rev. Virol, doi:10.1146/annurev-virology-110615-042301
Licastro, Rajasekharan, Monego, Segat, D'agaro et al., Isolation and full-length genome characterization of SARS-CoV-2 from COVID-19 cases in Northern Italy, J. Virol, doi:10.1128/JVI.00543-20
Lim, Wambier, Goren, Are night shift workers at an increased risk for COVID-19?, Med. Hypotheses, doi:10.1016/j.mehy.2020.110147
Liu, Yang, Zhang, Huang, Wang et al., Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury, Sci. China Life Sci, doi:10.1007/s11427-020-1643-8
Loh, The potential of melatonin in the prevention and attenuation of oxidative hemolysis and myocardial injury from cd147 SARS-CoV-2 spike protein receptor binding, Melatonin Res, doi:10.32794/mr11250069
Lu, Zhao, Li, Niu, Yang et al., Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding, Lancet, doi:10.1016/S0140-6736(20)30251-8
Luchetti, Canonico, Betti, Arcangeletti, Pilolli et al., Melatonin signaling and cell protection function, FASEB J, doi:10.1096/fj.10-154450
Lumeng, Bodzin, Saltiel, Obesity induces a phenotypic switch in adipose tissue macrophage polarization, J. Clin. Investig, doi:10.1172/JCI29881
Maestroni, Exogenous melatonin as potential adjuvant in anti-SarsCov2 vaccines, J. Neuroimmune Pharmacol
Makowski, Chaib, Rathmell, Immunometabolism: From basic mechanisms to translation, Immunol. Rev, doi:10.1111/imr.12858
Mallapaty, The coronavirus is most deadly if you are older and male-New data reveal the risks, Nature, doi:10.1038/d41586-020-02483-2
Mao, Jin, Wang, Hu, Chen et al., Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China, JAMA Neurol, doi:10.1001/jamaneurol.2020.1127
Maruta, He, PAK1-blockers: Potential therapeutics against COVID-19, Med. Drug Discov, doi:10.1016/j.medidd.2020.100039
Mauvais-Jarvis, Aging, male sex, obesity, and metabolic inflammation create the perfect storm for COVID-19, Diabetes, doi:10.2337/dbi19-0023
Mazzoccoli, Kvetnoy, Mironova, Yablonskiy, Sokolovich et al., The melatonergic pathway and its interactions in modulating respiratory system disorders, Biomed. Pharmacother
Mehrzadi, Karimi, Fatemi, Reiter, Hosseinzadeh, SARS-CoV-2 and other coronaviruses negatively influence mitochondrial quality control: Beneficial effects of melatonin, Pharmacol. Ther, doi:10.1016/j.pharmthera.2021.107825
Menni, Sudre, Steves, Ourselin, Spector, Quantifying additional COVID-19 symptoms will save lives, Lancet, doi:10.1016/S0140-6736(20)31281-2
Miller, Cappuccio, A systematic review of COVID-19 and obstructive sleep apnoea, Sleep Med. Rev, doi:10.1016/j.smrv.2020.101382
Miller, Silverstein, Flores, Cao, Kumagai et al., Host mitochondrial transcriptome response to SARS-CoV-2 in multiple cell models and clinical samples, Sci. Rep, doi:10.1038/s41598-020-79552-z
Mokhtari, Hassani, Ghaffari, Ebrahimi, Yarahmadi et al., COVID-19 and multiorgan failure: A narrative review on potential mechanisms, J. Mol. Histol, doi:10.1007/s10735-020-09915-3
Ng, Tipih, Makoah, Vermeulen, Goedhals et al., Comorbidities in SARS-CoV-2 patients: A systematic review and meta-analysis, mBio, doi:10.1128/mBio.03647-20
Nunn, Guy, Brysch, Botchway, Frasch et al., SARS-CoV-2 and mitochondrial health: Implications of lifestyle and ageing, Immun. Ageing, doi:10.1186/s12979-020-00204-x
Owino, Buonfiglio, Tchio, Tosini, Melatonin signaling a key regulator of glucose homeostasis and energy metabolism, Front. Endocrinol, doi:10.3389/fendo.2019.00488
Oxenkrug, Requintina, Bachurin, Antioxidant and antiaging activity of N-acetylserotonin and melatonin in the in vivo models, Ann. N. Y. Acad. Sci, doi:10.1111/j.1749-6632.2001.tb03626.x
Pal, Chattopadhyay, Bandyopadhyay, Melatonin as a potential therapeutic molecule against COVID-19 associated gastrointestinal complications: An unrevealed link, Melatonin Res, doi:10.32794/mr11250070
Palagini, Manni, Aguglia, Amore, Brugnoli et al., Evaluation and management of insomnia in clinical practice and in the time of COVID-19 in Italy: Expert consensus and task-force recommendations from five scientific societies, Riv. Psichiatr, doi:10.1708/3503.34891
Pandi-Perumal, Bahammam, Brown, Spence, Bharti et al., Melatonin antioxidative defense: Therapeutical implications for aging and neurodegenerative processes, Neurotox. Res, doi:10.1007/s12640-012-9337-4
Parlakpinar, Polat, Acet, Pharmacological agents under investigation in the treatment of coronavirus disease 2019 and the importance of melatonin, Fundam. Clin. Pharmacol, doi:10.1111/fcp.12589
Paulose, Wright, Patel, Cassone, Human gut bacteria are sensitive to melatonin and express endogenous circadian rhythmicity, PLoS ONE, doi:10.1371/journal.pone.0146643
Peschke, Bahr, Muhlbauer, Experimental and clinical aspects of melatonin and clock genes in diabetes, J. Pineal Res, doi:10.1111/jpi.12240
Picca, Lezza, Leeuwenburgh, Pesce, Calvani et al., Fueling inflamm-aging through mitochondrial dysfunction: Mechanisms and molecular targets, Int. J. Mol. Sci, doi:10.3390/ijms18050933
Pietrobon, Teixeira, Sato, Immunosenescence and inflammaging: Risk factors of severe COVID-19 in older people, Front. Immunol, doi:10.3389/fimmu.2020.579220
Polyakova, Kvetnoy, Anderson, Rosati, Mazzoccoli et al., Reciprocal interactions of mitochondria and the neuroimmunoendocrine system in neurodegenerative disorders: An important role for melatonin regulation, Front. Physiol, doi:10.3389/fphys.2018.00199
Pourhanifeh, Mehrzadi, Kamali, Hosseinzadeh, Melatonin and gastrointestinal cancers: Current evidence based on underlying signaling pathways, Eur. J. Pharmacol, doi:10.1016/j.ejphar.2020.173471
Puelles, Lutgehetmann, Lindenmeyer, Sperhake, Wong et al., Multiorgan and renal tropism of SARS-CoV-2, N. Engl. J. Med, doi:10.1056/NEJMc2011400
Rahman, Talukder, Chowdhury, Talukder, Akter, Coronaviruses in wild birds-A potential and suitable vector for global distribution, Vet. Med. Sci, doi:10.1002/vms3.360
Ramis, Esteban, Miralles, Tan, Reiter, Protective effects of melatonin and mitochondria-targeted antioxidants against oxidative stress: A Review, Curr. Med. Chem, doi:10.2174/0929867322666150619104143
Ramlall, Zucker, Tatonetti, Melatonin is significantly associated with survival of intubated COVID-19 patients, medRxiv, doi:10.1101/2020.10.15.20213546
Ramos, Farre-Alins, Egea, Lopez-Munoz, Reiter et al., Melatonin's efficacy in stroke patients; a matter of dose? A systematic review, Toxicol. Appl. Pharmacol, doi:10.1016/j.taap.2020.114933
Ramos, Miguez, Morgado, Sanchez-Correa, Gordillo et al., Melatonin enhances responsiveness to dichelobacter nodosus vaccine in sheep and increases peripheral blood CD4 T lymphocytes and IgG-expressing B lymphocytes, Vet. Immunol. Immunopathol, doi:10.1016/j.vetimm.2018.11.006
Ratajczak, Kucia, SARS-CoV-2 infection and overactivation of Nlrp3 inflammasome as a trigger of cytokine "storm" and risk factor for damage of hematopoietic stem cells, Leukemia, doi:10.1038/s41375-020-0887-9
Reiter, Abreu-Gonzalez, Marik, Dominguez-Rodriguez, Therapeutic algorithm for use of melatonin in patients with COVID-19, Front. Med, doi:10.3389/fmed.2020.00226
Reiter, Calvo, Karbownik, Qi, Tan, Melatonin and its relation to the immune system and inflammation, Ann. N. Y. Acad. Sci, doi:10.1111/j.1749-6632.2000.tb05402.x
Reiter, Ma, Sharma, Treatment of ebola and other infectious diseases: Melatonin "goes viral, Melatonin Res, doi:10.32794/mr11250047
Reiter, Melatonin: Clinical relevance, Best Pract. Res. Clin. Endocrinol. Metab, doi:10.1016/S1521-690X(03)00016-2
Reiter, Oxidative processes and antioxidative defense mechanisms in the aging brain, FASEB J, doi:10.1096/fasebj.9.7.7737461
Reiter, Rosales-Corral, Tan, Jou, Galano et al., Melatonin as a mitochondria-targeted antioxidant: One of evolution's best ideas, Cell. Mol. Life Sci, doi:10.1007/s00018-017-2609-7
Reiter, Sharma, Ma, Dominquez-Rodriguez, Marik et al., Melatonin inhibits COVID-19-induced cytokine storm by reversing aerobic glycolysis in immune cells: A mechanistic analysis, Med. Drug Discov
Reiter, Sharma, Ma, Liu, Manucha et al., Metabolic plasticity of activated immune cells: Advantages for suppression of COVID-19 Disease by melatonin, Melatonin Res, doi:10.32794/mr11250068
Reiter, Sharma, Ma, Rorsales-Corral, De Almeida Chuffa, Melatonin inhibits warburg-dependent cancer by redirecting glucose oxidation to the mitochondria: A mechanistic hypothesis, Cell. Mol. Life Sci, doi:10.1007/s00018-019-03438-1
Reiter, Tan, Rosales-Corral, Galano, Zhou et al., Mitochondria: Central Organelles for Melatonin's Antioxidant and Anti-Aging Actions, Molecules, doi:10.3390/molecules23020509
Reutrakul, Sumritsopak, Saetung, Chanprasertyothin, Chailurkit et al., Lower nocturnal urinary 6-sulfatoxymelatonin is associated with more severe insulin resistance in patients with prediabetes, Neurobiol. Sleep Circadian Rhythm, doi:10.1016/j.nbscr.2017.06.001
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area, JAMA, doi:10.1001/jama.2020.6775
Rivero Vaccari, Dietrich, Keane, De Rivero, Vaccari, The inflammasome in times of COVID-19, Front. Immunol, doi:10.3389/fimmu.2020.583373
Rodriguez-Rubio, Figueira, Acuna-Castroviejo, Borobia, Escames et al., A phase II, single-center, double-blind, randomized placebo-controlled trial to explore the efficacy and safety of intravenous melatonin in patients with COVID-19 admitted to the intensive care unit (MelCOVID study): A structured summary of a study protocol for a randomized controlled trial, Trials, doi:10.1186/s13063-020-04632-4
Romero, Ramos, Lopez-Munoz, Gil-Martin, Escames et al., Coronavirus disease 2019 (COVID-19) and its neuroinvasive capacity: Is it time for melatonin?, Cell. Mol. Neurobiol, doi:10.1007/s10571-020-00938-8
Russell, Gorman, Lightowlers, Turnbull, Mitochondrial diseases: Hope for the future, Cell, doi:10.1016/j.cell.2020.02.051
Sanchez-Barcelo, Mediavilla, Tan, Reiter, Clinical uses of melatonin: Evaluation of human trials, Curr. Med. Chem, doi:10.2174/092986710791233689
Sehirli, Sayiner, Serakinci, Role of melatonin in the treatment of COVID-19; as an adjuvant through cluster differentiation 147 (CD147), Mol. Biol. Rep, doi:10.1007/s11033-020-05830-8
Seifirad, Alquran, Commentary: Antifibrotics in COVID-19 Lung Disease: Let Us Stay Focused, Front. Med, doi:10.3389/fmed.2020.625440
Shatilo, Bondarenko, Antoniuk-Shcheglova, Pineal gland melatonin-producing function in elderly patients with hypertensive disease: Age peculiarities, Adv. Gerontol, doi:10.1134/S2079057011030131
Shenoy, Coronavirus (Covid-19) sepsis: Revisiting mitochondrial dysfunction in pathogenesis, aging, inflammation, and mortality, Inflamm. Res, doi:10.1007/s00011-020-01389-z
Sher, Rabkin, Maldonado, Mohabir, COVID-19-Associated hyperactive intensive care unit delirium with proposed pathophysiology and treatment: A case report, Psychosomatics, doi:10.1016/j.psym.2020.05.007
Shneider, Kudriavtsev, Vakhrusheva, Can melatonin reduce the severity of COVID-19 pandemic?, Int. Rev. Immunol, doi:10.1080/08830185.2020.1756284
Silvestri, Rossi, Melatonin: Its possible role in the management of viral infections-A brief review, Ital. J. Pediatr, doi:10.1186/1824-7288-39-61
Simmons, Gosalia, Rennekamp, Reeves, Diamond et al., Inhibitors of cathepsin L prevent severe acute respiratory syndrome coronavirus entry, Proc. Natl. Acad. Sci, doi:10.1073/pnas.0505577102
Singh, Chaubey, Chen, Suravajhala, Decoding SARS-CoV-2 hijacking of host mitochondria in COVID-19 pathogenesis, Am. J. Physiol. Cell Physiol, doi:10.1152/ajpcell.00224.2020
Singh, Chen, Judy, Seifuddin, Tunc et al., Network analysis and transcriptome profiling identify autophagic and mitochondrial dysfunctions in SARS-CoV-2 infection, bioRxiv, doi:10.1101/2020.05.13.092536
Slominski, Fischer, Zmijewski, Wortsman, Semak et al., On the role of melatonin in skin physiology and pathology, Endocrine, doi:10.1385/ENDO:27:2:137
Song, Li, Xie, Hou, You, Cytokine storm induced by SARS-CoV-2, Clin. Chim. Acta, doi:10.1016/j.cca.2020.06.017
Srinivasan, Cui, Gao, Liu, Lu et al., Structural genomics of SARS-CoV-2 indicates evolutionary conserved functional regions of viral proteins, Viruses, doi:10.3390/v12040360
Stevens, Light-at-night, circadian disruption and breast cancer: Assessment of existing evidence, Int. J. Epidemiol, doi:10.1093/ije/dyp178
Stokes, Zambrano, Anderson, Marder, Raz et al., Coronavirus disease 2019 case surveillance-United States, 22, Morb. Mortal. Wkly. Rep, doi:10.15585/mmwr.mm6924e2
Su, Li, Chen, Li, Xiao et al., Melatonin attenuates angiotensin II-induced cardiomyocyte hypertrophy through the CyPA/CD147 signaling pathway, Mol. Cell. Biochem, doi:10.1007/s11010-016-2808-9
Suofu, Li, Jean-Alphonse, Jia, Khattar et al., Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release, Proc. Natl. Acad. Sci, doi:10.1073/pnas.1705768114
Tamtaji, Mobini, Reiter, Azami, Gholami et al., Melatonin, a toll-like receptor inhibitor: Current status and future perspectives, J. Cell. Physiol, doi:10.1002/jcp.27698
Tan, Hardeland, Potential utility of melatonin in deadly infectious diseases related to the overreaction of innate immune response and destructive inflammation: Focus on COVID-19, Melatonin Res, doi:10.32794/mr11250052
Tan, Manchester, Qin, Reiter, Melatonin: A mitochondrial targeting molecule involving mitochondrial protection and dynamics, Int. J. Mol. Sci, doi:10.3390/ijms17122124
Tan, Manchester, Terron, Flores, Reiter, One molecule, many derivatives: A never-ending interaction of melatonin with reactive oxygen and nitrogen species?, J. Pineal Res, doi:10.1111/j.1600-079X.2006.00407.x
Tan, Reiter, Mitochondria: The birth place, battle ground and the site of melatonin metabolism in cells, Melatonin Res, doi:10.32794/mr11250011
Tay, Poh, Renia, Macary, Ng, The trinity of COVID-19: Immunity, inflammation and intervention, Nat. Rev. Immunol, doi:10.1038/s41577-020-0311-8
Team, -R, Preliminary estimates of the prevalence of selected underlying health conditions among patients with Coronavirus Disease 2019-United States, Morb. Mortal. Wkly. Rep, doi:10.15585/mmwr.mm6913e2
Tesarik, Melatonin attenuates growth factor receptor signaling required for SARS-CoV-2 replication, Melatonin Res, doi:10.32794/mr11250077
Thompson, Cascino, Ordonez, Zhou, Vaghasia et al., Mitochondrial induced T cell apoptosis and aberrant myeloid metabolic programs define distinct immune cell subsets during acute and recovered SARS-CoV-2 infection, medRxiv, doi:10.1101/2020.09.10.20186064
Tiku, Tan, Dikic, Mitochondrial functions in infection and immunity, Trends Cell Biol, doi:10.1016/j.tcb.2020.01.006
Tordjman, Chokron, Delorme, Charrier, Bellissant et al., Melatonin: Pharmacology, functions and therapeutic benefits, Curr. Neuropharmacol, doi:10.2174/1570159X14666161228122115
Ulrich, Pillat, CD147 as a target for COVID-19 treatment: Suggested effects of azithromycin and stem cell engagement, Stem Cell Rev. Rep, doi:10.1007/s12015-020-09976-7
Vabret, Britton, Gruber, Hegde, Kim et al., Immunology of COVID-19: Current state of the science, Immunity, doi:10.1016/j.immuni.2020.05.002
Valero, Mosquera, Alcocer, Bonilla, Salazar et al., Melatonin, minocycline and ascorbic acid reduce oxidative stress and viral titers and increase survival rate in experimental Venezuelan equine encephalitis, Brain Res, doi:10.1016/j.brainres.2015.06.034
Van Doremalen, Bushmaker, Morris, Holbrook, Gamble et al., Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1, N. Engl. J. Med, doi:10.1056/NEJMc2004973
Vazquez, Horner, MAVS coordination of antiviral innate immunity, J. Virol, doi:10.1128/JVI.01918-14
Venegas, Garcia, Escames, Ortiz, Lopez et al., Extrapineal melatonin: Analysis of its subcellular distribution and daily fluctuations, J. Pineal Res, doi:10.1111/j.1600-079X.2011.00931.x
Ventura-Clapier, Moulin, Piquereau, Lemaire, Mericskay et al., Mitochondria: A central target for sex differences in pathologies, Clin. Sci, doi:10.1042/CS20160485
Volt, Garcia, Doerrier, Diaz-Casado, Guerra-Librero et al., Same molecule but different expression: Aging and sepsis trigger NLRP3 inflammasome activation, a target of melatonin, J. Pineal Res, doi:10.1111/jpi.12303
Waldhauser, Weiszenbacher, Frisch, Zeitlhuber, Waldhauser et al., Fall in nocturnal serum melatonin during prepuberty and pubescence, Lancet, doi:10.1016/S0140-6736(84)90412-4
Wang, Han, Zhou, Zhang, Liu et al., Melatonin ameliorates aortic valve calcification via the regulation of circular RNA CircRIC3/miR-204-5p/DPP4 signaling in valvular interstitial cells, J. Pineal Res, doi:10.1111/jpi.12666
Wang, Li, Lu, Huang, Does comorbidity increase the risk of patients with COVID-19: Evidence from meta-analysis, Aging, doi:10.18632/aging.103000
Wang, Luan, Medzhitov, An evolutionary perspective on immunometabolism, Science, doi:10.1126/science.aar3932
Wang, Xie, Zhao, Fei, Zhang et al., Alveolar macrophage dysfunction and cytokine storm in the pathogenesis of two severe COVID-19 patients, EBioMedicine, doi:10.1016/j.ebiom.2020.102833
Wongchitrat, Shukla, Sharma, Govitrapong, Reiter, Role of melatonin on virus-induced neuropathogenesis-A concomitant therapeutic strategy to understand SARS-CoV-2 infection, Antioxidants, doi:10.3390/antiox10010047
Wu, Peng, Huang, Ding, Wang et al., Genome composition and divergence of the Novel Coronavirus (2019-nCoV) originating in China, Cell Host Microbe, doi:10.1016/j.chom.2020.02.001
Wu, Zou, Chang, RNA-GPS predicts SARS-CoV-2 RNA localization to host mitochondria and nucleolus, bioRxiv, doi:10.1101/2020.04.28.065201
Xia, Chen, Zeng, Zhao, Zhu et al., Melatonin in macrophage biology: Current understanding and future perspectives, J. Pineal Res, doi:10.1111/jpi.12547
Xiao, Tang, Zheng, Liu, Li et al., Evidence for gastrointestinal infection of SARS-CoV-2, Gastroenterology, doi:10.1053/j.gastro.2020.02.055
Xu, Shu, Kang, Wu, Zhou et al., Temporal profiling of plasma cytokines, chemokines and growth factors from mild, severe and fatal COVID-19 patients, Signal Transduct. Target. Ther
Yang, Petitjean, Koehler, Zhang, Dumitru et al., Molecular interaction and inhibition of SARS-CoV-2 binding to the ACE2 receptor, Nat. Commun, doi:10.1038/s41467-020-18319-6
Yang, Zheng, Gou, Pu, Chen et al., Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis, Int. J. Infect. Dis, doi:10.1016/j.ijid.2020.03.017
Zambrelli, Canevini, Gambini, D'agostino, Delirium and sleep disturbances in COVID-19: A possible role for melatonin in hospitalized patients?, Sleep Med, doi:10.1016/j.sleep.2020.04.006
Zarezadeh, Khorshidi, Emami, Janmohammadi, Kord-Varkaneh et al., Melatonin supplementation and pro-inflammatory mediators: A systematic review and meta-analysis of clinical trials, Eur. J. Nutr, doi:10.1007/s00394-019-02123-0
Zeppa, Agostini, Piccoli, Stocchi, Sestili, Gut microbiota status in COVID-19: An unrecognized player? Front, Cell. Infect. Microbiol, doi:10.3389/fcimb.2020.576551
Zhang, Li, Grailer, Wang, Wang et al., Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome, J. Pineal Res, doi:10.1111/jpi.12322
Zhang, Wang, Ni, Di, Ma et al., COVID-19: Melatonin as a potential adjuvant treatment, Life Sci, doi:10.1016/j.lfs.2020.117583
Zhao, Sun, Su, Shan, Zhang et al., Melatonin protects against lung fibrosis by regulating the Hippo/YAP pathway, Int. J. Mol. Sci, doi:10.3390/ijms19041118
Zhou, Hou, Shen, Huang, Martin et al., Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2, Cell Discov, doi:10.1038/s41421-020-0153-3
Zhou, Hou, Shen, Kallianpur, Zein et al., A network medicine approach to investigation and population-based validation of disease manifestations and drug repurposing for COVID-19, ChemRxiv, doi:10.1371/journal.pbio.3000970
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study, Lancet
Ziaei, Davoodian, Dadvand, Safa, Hassanipour et al., Evaluation of the efficacy and safety of Melatonin in moderately ill patients with COVID-19: A structured summary of a study protocol for a randomized controlled trial, Trials, doi:10.1186/s13063-020-04737-w
Zou, Chen, Zou, Han, Hao et al., Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection, Front. Med, doi:10.1007/s11684-020-0754-0
Zuo, Zhang, Lui, Yeoh, Li et al., Alterations in gut microbiota of patients with COVID-19 during time of hospitalization, Gastroenterology, doi:10.1053/j.gastro.2020.05.048
DOI record:
{
"DOI": "10.3390/antiox10071152",
"ISSN": [
"2076-3921"
],
"URL": "http://dx.doi.org/10.3390/antiox10071152",
"abstract": "<jats:p>Viral infections constitute a tectonic convulsion in the normophysiology of the hosts. The current coronavirus disease 2019 (COVID-19) pandemic is not an exception, and therefore the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, like any other invading microbe, enacts a generalized immune response once the virus contacts the body. Melatonin is a systemic dealer that does not overlook any homeostasis disturbance, which consequently brings into play its cooperative triad, antioxidant, anti-inflammatory, and immune-stimulant backbone, to stop the infective cycle of SARS-CoV-2 or any other endogenous or exogenous threat. In COVID-19, the corporal propagation of SARS-CoV-2 involves an exacerbated oxidative activity and therefore the overproduction of great amounts of reactive oxygen and nitrogen species (RONS). The endorsement of melatonin as a possible protective agent against the current pandemic is indirectly supported by its widely demonstrated beneficial role in preclinical and clinical studies of other respiratory diseases. In addition, focusing the therapeutic action on strengthening the host protection responses in critical phases of the infective cycle makes it likely that multi-tasking melatonin will provide multi-protection, maintaining its efficacy against the virus variants that are already emerging and will emerge as long as SARS-CoV-2 continues to circulate among us.</jats:p>",
"alternative-id": [
"antiox10071152"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5791-0687",
"affiliation": [],
"authenticated-orcid": false,
"family": "Ramos",
"given": "Eva",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-5188-6038",
"affiliation": [],
"authenticated-orcid": false,
"family": "López-Muñoz",
"given": "Francisco",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-9435-0444",
"affiliation": [],
"authenticated-orcid": false,
"family": "Gil-Martín",
"given": "Emilio",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-4704-3019",
"affiliation": [],
"authenticated-orcid": false,
"family": "Egea",
"given": "Javier",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Álvarez-Merz",
"given": "Iris",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8941-2006",
"affiliation": [],
"authenticated-orcid": false,
"family": "Painuli",
"given": "Sakshi",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5137-5169",
"affiliation": [],
"authenticated-orcid": false,
"family": "Semwal",
"given": "Prabhakar",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5934-5201",
"affiliation": [],
"authenticated-orcid": false,
"family": "Martins",
"given": "Natália",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Hernández-Guijo",
"given": "Jesús M.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-5483-4973",
"affiliation": [],
"authenticated-orcid": false,
"family": "Romero",
"given": "Alejandro",
"sequence": "additional"
}
],
"container-title": "Antioxidants",
"container-title-short": "Antioxidants",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
7,
20
]
],
"date-time": "2021-07-20T15:26:10Z",
"timestamp": 1626794770000
},
"deposited": {
"date-parts": [
[
2021,
7,
21
]
],
"date-time": "2021-07-21T16:02:50Z",
"timestamp": 1626883370000
},
"indexed": {
"date-parts": [
[
2024,
4,
22
]
],
"date-time": "2024-04-22T13:16:26Z",
"timestamp": 1713791786451
},
"is-referenced-by-count": 20,
"issue": "7",
"issued": {
"date-parts": [
[
2021,
7,
20
]
]
},
"journal-issue": {
"issue": "7",
"published-online": {
"date-parts": [
[
2021,
7
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
7,
20
]
],
"date-time": "2021-07-20T00:00:00Z",
"timestamp": 1626739200000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2076-3921/10/7/1152/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "1152",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
7,
20
]
]
},
"published-online": {
"date-parts": [
[
2021,
7,
20
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/j.scitotenv.2020.138882",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1038/s41564-020-0695-z",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1385/ENDO:27:2:137",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.2174/1570159X14666161228122115",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1016/j.bbabio.2006.03.012",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1016/j.intimp.2015.12.020",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1111/j.1749-6632.2001.tb03626.x",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1007/s12640-012-9337-4",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1016/j.smrv.2004.05.002",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.3390/diseases8040044",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"DOI": "10.3389/fmed.2020.00226",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.3389/fphar.2020.01169",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1096/fj.10-154450",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"article-title": "Role of melatonin in cancer treatment",
"author": "Cutando",
"first-page": "2747",
"journal-title": "Anticancer Res.",
"key": "ref14",
"volume": "32",
"year": "2012"
},
{
"DOI": "10.1038/s41577-020-0311-8",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1046/j.1600-079X.2003.00105.x",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.32794/mr11250047",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.32794/mr11250052",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1016/j.virusres.2020.198108",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1093/emph/eoaa036",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/j.exger.2004.04.012",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1016/S0140-6736(84)90412-4",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1080/08830185.2020.1756284",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1038/s41421-020-0153-3",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1371/journal.pbio.3000970",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1016/j.molliq.2020.114082",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.7150/ijms.48053",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1016/j.chest.2020.05.580",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.3390/nu12092561",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1007/s11481-020-09956-1",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1016/j.lfs.2020.117583",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.32794/mr11250091",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1002/jmv.26232",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1016/j.cca.2020.06.017",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1016/j.ebiom.2020.102833",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1007/s10735-020-09915-3",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1002/rmv.1714",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1016/j.brainres.2015.06.034",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1016/j.jff.2019.04.062",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.1034/j.1600-079X.2002.02943.x",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.1002/jcph.592",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.3389/fimmu.2020.01748",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1016/j.immuni.2020.05.002",
"doi-asserted-by": "publisher",
"key": "ref44"
},
{
"DOI": "10.1186/s12979-020-00204-x",
"doi-asserted-by": "publisher",
"key": "ref45"
},
{
"DOI": "10.1177/1178646918802282",
"doi-asserted-by": "publisher",
"key": "ref46"
},
{
"DOI": "10.1002/vms3.360",
"doi-asserted-by": "publisher",
"key": "ref47"
},
{
"DOI": "10.1016/S0140-6736(20)30251-8",
"doi-asserted-by": "publisher",
"key": "ref48"
},
{
"DOI": "10.1128/JVI.00543-20",
"doi-asserted-by": "publisher",
"key": "ref49"
},
{
"DOI": "10.1016/j.chom.2020.02.001",
"doi-asserted-by": "publisher",
"key": "ref50"
},
{
"DOI": "10.1080/22221751.2020.1719902",
"doi-asserted-by": "publisher",
"key": "ref51"
},
{
"DOI": "10.1093/nar/gkx932",
"doi-asserted-by": "publisher",
"key": "ref52"
},
{
"DOI": "10.1073/pnas.0505577102",
"doi-asserted-by": "publisher",
"key": "ref53"
},
{
"DOI": "10.1038/s41579-020-00459-7",
"doi-asserted-by": "publisher",
"key": "ref54"
},
{
"DOI": "10.1146/annurev-virology-110615-042301",
"doi-asserted-by": "publisher",
"key": "ref55"
},
{
"DOI": "10.1038/nature02145",
"doi-asserted-by": "publisher",
"key": "ref56"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "ref57"
},
{
"DOI": "10.1161/01.RES.87.5.e1",
"doi-asserted-by": "publisher",
"key": "ref58"
},
{
"DOI": "10.1007/s11684-020-0754-0",
"doi-asserted-by": "publisher",
"key": "ref59"
},
{
"DOI": "10.1053/j.gastro.2020.02.055",
"doi-asserted-by": "publisher",
"key": "ref60"
},
{
"DOI": "10.1016/j.kint.2020.03.005",
"doi-asserted-by": "publisher",
"key": "ref61"
},
{
"DOI": "10.3760/cma.j.issn.1007-3418.2020.02.002",
"doi-asserted-by": "publisher",
"key": "ref62"
},
{
"DOI": "10.1016/S0140-6736(20)31281-2",
"doi-asserted-by": "publisher",
"key": "ref63"
},
{
"DOI": "10.18632/aging.103000",
"doi-asserted-by": "publisher",
"key": "ref64"
},
{
"DOI": "10.1056/NEJMc2004973",
"doi-asserted-by": "publisher",
"key": "ref65"
},
{
"DOI": "10.1096/fasebj.9.7.7737461",
"doi-asserted-by": "publisher",
"key": "ref66"
},
{
"DOI": "10.3390/antiox9111088",
"doi-asserted-by": "publisher",
"key": "ref67"
},
{
"DOI": "10.1016/j.ctim.2018.11.003",
"doi-asserted-by": "publisher",
"key": "ref68"
},
{
"DOI": "10.2174/092986710791233689",
"doi-asserted-by": "publisher",
"key": "ref69"
},
{
"DOI": "10.1016/j.yfrne.2018.06.004",
"doi-asserted-by": "publisher",
"key": "ref70"
},
{
"DOI": "10.1007/s10787-018-0508-7",
"doi-asserted-by": "publisher",
"key": "ref71"
},
{
"DOI": "10.18632/oncotarget.16379",
"doi-asserted-by": "publisher",
"key": "ref72"
},
{
"DOI": "10.1016/j.critrevonc.2017.12.018",
"doi-asserted-by": "publisher",
"key": "ref73"
},
{
"DOI": "10.1016/j.ejphar.2020.173471",
"doi-asserted-by": "publisher",
"key": "ref74"
},
{
"DOI": "10.3390/cancers11111712",
"doi-asserted-by": "publisher",
"key": "ref75"
},
{
"DOI": "10.1002/med.21582",
"doi-asserted-by": "publisher",
"key": "ref76"
},
{
"DOI": "10.1002/rmv.2109",
"doi-asserted-by": "publisher",
"key": "ref77"
},
{
"DOI": "10.3390/antiox10010047",
"doi-asserted-by": "publisher",
"key": "ref78"
},
{
"DOI": "10.1007/s10571-020-00938-8",
"doi-asserted-by": "publisher",
"key": "ref79"
},
{
"DOI": "10.1186/s13063-020-04436-6",
"doi-asserted-by": "publisher",
"key": "ref80"
},
{
"DOI": "10.1186/s13063-020-04632-4",
"doi-asserted-by": "publisher",
"key": "ref81"
},
{
"DOI": "10.1111/jpi.12683",
"doi-asserted-by": "publisher",
"key": "ref82"
},
{
"DOI": "10.1186/s13063-020-04737-w",
"doi-asserted-by": "publisher",
"key": "ref83"
},
{
"DOI": "10.1016/j.taap.2020.114933",
"doi-asserted-by": "publisher",
"key": "ref84"
},
{
"DOI": "10.1093/ije/dyp178",
"doi-asserted-by": "publisher",
"key": "ref85"
},
{
"DOI": "10.1016/S1521-690X(03)00016-2",
"doi-asserted-by": "publisher",
"key": "ref86"
},
{
"DOI": "10.1007/s41782-020-00111-7",
"doi-asserted-by": "publisher",
"key": "ref87"
},
{
"DOI": "10.1016/j.exphem.2019.08.008",
"doi-asserted-by": "publisher",
"key": "ref88"
},
{
"DOI": "10.1186/s13054-015-0842-8",
"doi-asserted-by": "publisher",
"key": "ref89"
},
{
"DOI": "10.32794/mr11250073",
"doi-asserted-by": "publisher",
"key": "ref90"
},
{
"DOI": "10.1016/j.mehy.2020.110147",
"doi-asserted-by": "publisher",
"key": "ref91"
},
{
"DOI": "10.1708/3503.34891",
"doi-asserted-by": "publisher",
"key": "ref92"
},
{
"DOI": "10.1001/jamaneurol.2020.1127",
"doi-asserted-by": "publisher",
"key": "ref93"
},
{
"DOI": "10.1016/j.sleep.2020.04.006",
"doi-asserted-by": "publisher",
"key": "ref94"
},
{
"DOI": "10.1016/j.psym.2020.05.007",
"doi-asserted-by": "publisher",
"key": "ref95"
},
{
"DOI": "10.1001/jama.2020.6775",
"doi-asserted-by": "publisher",
"key": "ref96"
},
{
"DOI": "10.1038/s41574-018-0130-1",
"doi-asserted-by": "publisher",
"key": "ref97"
},
{
"DOI": "10.5935/1984-0063.20200038",
"doi-asserted-by": "publisher",
"key": "ref98"
},
{
"DOI": "10.1016/j.smrv.2020.101382",
"doi-asserted-by": "publisher",
"key": "ref99"
},
{
"DOI": "10.1016/j.mehy.2021.110544",
"doi-asserted-by": "publisher",
"key": "ref100"
},
{
"DOI": "10.1007/s12015-020-09976-7",
"doi-asserted-by": "publisher",
"key": "ref101"
},
{
"DOI": "10.32794/mr11250069",
"doi-asserted-by": "publisher",
"key": "ref102"
},
{
"DOI": "10.1007/s11010-016-2808-9",
"doi-asserted-by": "publisher",
"key": "ref103"
},
{
"DOI": "10.1007/s11033-020-05830-8",
"doi-asserted-by": "publisher",
"key": "ref104"
},
{
"DOI": "10.1111/jpi.12666",
"doi-asserted-by": "publisher",
"key": "ref105"
},
{
"DOI": "10.3390/biology9090249",
"doi-asserted-by": "publisher",
"key": "ref106"
},
{
"DOI": "10.1128/JVI.01743-19",
"doi-asserted-by": "publisher",
"key": "ref107"
},
{
"DOI": "10.1053/j.gastro.2020.05.048",
"doi-asserted-by": "publisher",
"key": "ref108"
},
{
"DOI": "10.3390/ijms20215500",
"doi-asserted-by": "publisher",
"key": "ref109"
},
{
"DOI": "10.3390/ijms22041597",
"doi-asserted-by": "publisher",
"key": "ref110"
},
{
"DOI": "10.3949/ccjm.87a.ccc037",
"doi-asserted-by": "publisher",
"key": "ref111"
},
{
"DOI": "10.1111/fcp.12589",
"doi-asserted-by": "publisher",
"key": "ref112"
},
{
"DOI": "10.1101/2020.10.15.20213546",
"doi-asserted-by": "publisher",
"key": "ref113"
},
{
"DOI": "10.1016/j.medidd.2020.100039",
"doi-asserted-by": "publisher",
"key": "ref114"
},
{
"DOI": "10.1016/j.molcel.2020.08.006",
"doi-asserted-by": "publisher",
"key": "ref115"
},
{
"DOI": "10.32794/mr11250077",
"doi-asserted-by": "publisher",
"key": "ref116"
},
{
"DOI": "10.1210/endocr/bqaa112",
"doi-asserted-by": "publisher",
"key": "ref117"
},
{
"DOI": "10.1016/j.heliyon.2020.e05684",
"doi-asserted-by": "publisher",
"key": "ref118"
},
{
"DOI": "10.1159/000512592",
"doi-asserted-by": "publisher",
"key": "ref119"
},
{
"DOI": "10.2337/dbi19-0023",
"doi-asserted-by": "publisher",
"key": "ref120"
},
{
"DOI": "10.1016/j.ijid.2020.03.017",
"doi-asserted-by": "publisher",
"key": "ref121"
},
{
"DOI": "10.15585/mmwr.mm6924e2",
"doi-asserted-by": "publisher",
"key": "ref122"
},
{
"DOI": "10.15585/mmwr.mm6913e2",
"doi-asserted-by": "publisher",
"key": "ref123"
},
{
"DOI": "10.1128/mBio.03647-20",
"doi-asserted-by": "publisher",
"key": "ref124"
},
{
"DOI": "10.1126/science.aar3932",
"doi-asserted-by": "publisher",
"key": "ref125"
},
{
"DOI": "10.1179/2295333715Y.0000000004",
"doi-asserted-by": "publisher",
"key": "ref126"
},
{
"DOI": "10.1172/JCI29881",
"doi-asserted-by": "publisher",
"key": "ref127"
},
{
"DOI": "10.1111/imr.12858",
"doi-asserted-by": "publisher",
"key": "ref128"
},
{
"DOI": "10.1038/nature05485",
"doi-asserted-by": "publisher",
"key": "ref129"
},
{
"DOI": "10.1038/s41366-021-00804-7",
"doi-asserted-by": "publisher",
"key": "ref130"
},
{
"DOI": "10.1007/s00018-017-2611-0",
"doi-asserted-by": "publisher",
"key": "ref131"
},
{
"DOI": "10.1016/j.pharmthera.2021.107825",
"doi-asserted-by": "publisher",
"key": "ref132"
},
{
"article-title": "Melatonin in aging and disease -multiple consequences of reduced secretion, options and limits of treatment",
"author": "Hardeland",
"first-page": "194",
"journal-title": "Aging Dis.",
"key": "ref133",
"volume": "3",
"year": "2012"
},
{
"DOI": "10.1159/000446543",
"doi-asserted-by": "publisher",
"key": "ref134"
},
{
"DOI": "10.32794/mr11250064",
"doi-asserted-by": "publisher",
"key": "ref135"
},
{
"DOI": "10.1007/s00210-020-01822-4",
"doi-asserted-by": "publisher",
"key": "ref136"
},
{
"DOI": "10.1007/s11357-011-9267-8",
"doi-asserted-by": "publisher",
"key": "ref137"
},
{
"DOI": "10.1186/s13098-015-0041-4",
"doi-asserted-by": "publisher",
"key": "ref138"
},
{
"DOI": "10.7556/jaoa.2020.020",
"doi-asserted-by": "publisher",
"key": "ref139"
},
{
"DOI": "10.3390/ijms14048638",
"doi-asserted-by": "publisher",
"key": "ref140"
},
{
"DOI": "10.1016/j.ejphar.2020.173329",
"doi-asserted-by": "publisher",
"key": "ref141"
},
{
"DOI": "10.1016/j.biopha.2021.111397",
"doi-asserted-by": "publisher",
"key": "ref142"
},
{
"DOI": "10.3390/ijms17122124",
"doi-asserted-by": "publisher",
"key": "ref143"
},
{
"DOI": "10.1007/s00018-017-2609-7",
"doi-asserted-by": "publisher",
"key": "ref144"
},
{
"DOI": "10.3389/fphys.2018.00199",
"doi-asserted-by": "publisher",
"key": "ref145"
},
{
"DOI": "10.1016/j.medidd.2020.100044",
"doi-asserted-by": "publisher",
"key": "ref146"
},
{
"DOI": "10.3389/fendo.2019.00488",
"doi-asserted-by": "publisher",
"key": "ref147"
},
{
"DOI": "10.1134/S2079057011030131",
"doi-asserted-by": "publisher",
"key": "ref148"
},
{
"DOI": "10.1186/1758-5996-6-124",
"doi-asserted-by": "publisher",
"key": "ref149"
},
{
"DOI": "10.1111/jpi.12240",
"doi-asserted-by": "publisher",
"key": "ref150"
},
{
"DOI": "10.1016/j.nbscr.2017.06.001",
"doi-asserted-by": "publisher",
"key": "ref151"
},
{
"DOI": "10.3390/scipharm88020028",
"doi-asserted-by": "publisher",
"key": "ref152"
},
{
"DOI": "10.1111/jpi.12137",
"doi-asserted-by": "publisher",
"key": "ref153"
},
{
"DOI": "10.1007/s00011-020-01389-z",
"doi-asserted-by": "publisher",
"key": "ref154"
},
{
"DOI": "10.1002/jmv.25685",
"doi-asserted-by": "publisher",
"key": "ref155"
},
{
"DOI": "10.3389/fimmu.2020.579220",
"doi-asserted-by": "publisher",
"key": "ref156"
},
{
"DOI": "10.1038/d41586-020-02483-2",
"doi-asserted-by": "publisher",
"key": "ref157"
},
{
"DOI": "10.1186/s12931-020-01465-2",
"doi-asserted-by": "publisher",
"key": "ref158"
},
{
"DOI": "10.1101/2020.07.02.20145003",
"doi-asserted-by": "publisher",
"key": "ref159"
},
{
"DOI": "10.1038/s41392-020-0211-1",
"doi-asserted-by": "publisher",
"key": "ref160"
},
{
"DOI": "10.1016/j.cell.2020.04.026",
"doi-asserted-by": "publisher",
"key": "ref161"
},
{
"DOI": "10.1038/s41467-020-18319-6",
"doi-asserted-by": "publisher",
"key": "ref162"
},
{
"DOI": "10.1038/s41375-020-0887-9",
"doi-asserted-by": "publisher",
"key": "ref163"
},
{
"DOI": "10.1007/s11427-020-1643-8",
"doi-asserted-by": "publisher",
"key": "ref164"
},
{
"DOI": "10.32794/mr11250068",
"doi-asserted-by": "publisher",
"key": "ref165"
},
{
"DOI": "10.32794/mr11250061",
"doi-asserted-by": "publisher",
"key": "ref166"
},
{
"DOI": "10.1016/j.lfs.2018.03.032",
"doi-asserted-by": "publisher",
"key": "ref167"
},
{
"DOI": "10.3390/ijms19041118",
"doi-asserted-by": "publisher",
"key": "ref168"
},
{
"DOI": "10.3390/ijms20051223",
"doi-asserted-by": "publisher",
"key": "ref169"
},
{
"DOI": "10.32794/mr11250070",
"doi-asserted-by": "publisher",
"key": "ref170"
},
{
"DOI": "10.3389/fcimb.2020.576551",
"doi-asserted-by": "publisher",
"key": "ref171"
},
{
"DOI": "10.1371/journal.pone.0146643",
"doi-asserted-by": "publisher",
"key": "ref172"
},
{
"DOI": "10.32794/mr11250066",
"doi-asserted-by": "publisher",
"key": "ref173"
},
{
"DOI": "10.1007/s00394-019-02123-0",
"doi-asserted-by": "publisher",
"key": "ref174"
},
{
"DOI": "10.1002/jcp.27698",
"doi-asserted-by": "publisher",
"key": "ref175"
},
{
"DOI": "10.3390/antiox9121299",
"doi-asserted-by": "publisher",
"key": "ref176"
},
{
"DOI": "10.1002/jmv.26776",
"doi-asserted-by": "publisher",
"key": "ref177"
},
{
"DOI": "10.1111/jpi.12303",
"doi-asserted-by": "publisher",
"key": "ref178"
},
{
"DOI": "10.1111/jpi.12322",
"doi-asserted-by": "publisher",
"key": "ref179"
},
{
"DOI": "10.3389/fimmu.2020.583373",
"doi-asserted-by": "publisher",
"key": "ref180"
},
{
"DOI": "10.1016/j.tips.2020.07.003",
"doi-asserted-by": "publisher",
"key": "ref181"
},
{
"DOI": "10.1111/jpi.12547",
"doi-asserted-by": "publisher",
"key": "ref182"
},
{
"DOI": "10.1096/fj.03-0694fje",
"doi-asserted-by": "publisher",
"key": "ref183"
},
{
"DOI": "10.1111/j.1600-079X.2006.00373.x",
"doi-asserted-by": "publisher",
"key": "ref184"
},
{
"DOI": "10.1002/phar.2222",
"doi-asserted-by": "publisher",
"key": "ref185"
},
{
"DOI": "10.1080/10715760290032593",
"doi-asserted-by": "publisher",
"key": "ref186"
},
{
"DOI": "10.1016/j.cell.2020.02.051",
"doi-asserted-by": "publisher",
"key": "ref187"
},
{
"DOI": "10.1155/2013/738794",
"doi-asserted-by": "publisher",
"key": "ref188"
},
{
"DOI": "10.1016/j.tcb.2020.01.006",
"doi-asserted-by": "publisher",
"key": "ref189"
},
{
"DOI": "10.1152/ajpcell.00224.2020",
"doi-asserted-by": "publisher",
"key": "ref190"
},
{
"DOI": "10.1101/2020.09.10.20186064",
"doi-asserted-by": "publisher",
"key": "ref191"
},
{
"DOI": "10.3390/jcm9040982",
"doi-asserted-by": "publisher",
"key": "ref192"
},
{
"DOI": "10.3390/v12040360",
"doi-asserted-by": "publisher",
"key": "ref193"
},
{
"DOI": "10.1101/2020.04.28.065201",
"doi-asserted-by": "publisher",
"key": "ref194"
},
{
"DOI": "10.3389/fphar.2020.578599",
"doi-asserted-by": "publisher",
"key": "ref195"
},
{
"DOI": "10.3390/ijms18050933",
"doi-asserted-by": "publisher",
"key": "ref196"
},
{
"DOI": "10.3389/fimmu.2020.01636",
"doi-asserted-by": "publisher",
"key": "ref197"
},
{
"DOI": "10.1101/2020.05.13.092536",
"doi-asserted-by": "publisher",
"key": "ref198"
},
{
"DOI": "10.3389/fpubh.2020.00152",
"doi-asserted-by": "publisher",
"key": "ref199"
},
{
"DOI": "10.1042/CS20160485",
"doi-asserted-by": "publisher",
"key": "ref200"
},
{
"DOI": "10.1159/000508560",
"doi-asserted-by": "publisher",
"key": "ref201"
},
{
"DOI": "10.1128/JVI.01918-14",
"doi-asserted-by": "publisher",
"key": "ref202"
},
{
"DOI": "10.1038/s41423-020-0514-8",
"doi-asserted-by": "publisher",
"key": "ref203"
},
{
"DOI": "10.1038/s41598-020-79552-z",
"doi-asserted-by": "publisher",
"key": "ref204"
},
{
"DOI": "10.1111/j.1600-079X.2011.00931.x",
"doi-asserted-by": "publisher",
"key": "ref205"
},
{
"DOI": "10.1073/pnas.1705768114",
"doi-asserted-by": "publisher",
"key": "ref206"
},
{
"DOI": "10.32794/mr11250011",
"doi-asserted-by": "publisher",
"key": "ref207"
},
{
"DOI": "10.1111/jpi.12390",
"doi-asserted-by": "publisher",
"key": "ref208"
},
{
"DOI": "10.3390/molecules23020509",
"doi-asserted-by": "publisher",
"key": "ref209"
},
{
"DOI": "10.1007/s00018-019-03438-1",
"doi-asserted-by": "publisher",
"key": "ref210"
},
{
"DOI": "10.1111/j.1600-079X.2006.00407.x",
"doi-asserted-by": "publisher",
"key": "ref211"
},
{
"DOI": "10.3390/v10080392",
"doi-asserted-by": "publisher",
"key": "ref212"
},
{
"DOI": "10.1111/j.1749-6632.2000.tb05402.x",
"doi-asserted-by": "publisher",
"key": "ref213"
},
{
"DOI": "10.2174/0929867322666150619104143",
"doi-asserted-by": "publisher",
"key": "ref214"
},
{
"DOI": "10.1016/j.cca.2020.06.033",
"doi-asserted-by": "publisher",
"key": "ref215"
},
{
"DOI": "10.1111/j.1440-1797.2005.00488.x",
"doi-asserted-by": "publisher",
"key": "ref216"
},
{
"DOI": "10.1056/NEJMc2011400",
"doi-asserted-by": "publisher",
"key": "ref217"
},
{
"DOI": "10.1016/j.lfs.2020.117739",
"doi-asserted-by": "publisher",
"key": "ref218"
},
{
"DOI": "10.32794/mr11250063",
"doi-asserted-by": "publisher",
"key": "ref219"
},
{
"DOI": "10.1016/j.lfs.2020.117808",
"doi-asserted-by": "publisher",
"key": "ref220"
},
{
"DOI": "10.1136/openhrt-2020-001568",
"doi-asserted-by": "publisher",
"key": "ref221"
},
{
"DOI": "10.1016/j.csbj.2021.02.009",
"doi-asserted-by": "publisher",
"key": "ref222"
},
{
"DOI": "10.1016/j.vetimm.2018.11.006",
"doi-asserted-by": "publisher",
"key": "ref223"
},
{
"DOI": "10.1371/journal.pone.0240149",
"doi-asserted-by": "publisher",
"key": "ref224"
},
{
"DOI": "10.3389/fmed.2020.625440",
"doi-asserted-by": "publisher",
"key": "ref225"
},
{
"DOI": "10.2174/1568026616666160824120338",
"doi-asserted-by": "publisher",
"key": "ref226"
},
{
"DOI": "10.1186/1824-7288-39-61",
"doi-asserted-by": "publisher",
"key": "ref227"
},
{
"article-title": "Melatonin as a probable cause of diarrhoea",
"author": "Grilo-Bensusan",
"first-page": "119",
"journal-title": "Rev. Esp. Enferm. Dig.",
"key": "ref228",
"volume": "107",
"year": "2015"
},
{
"DOI": "10.1212/WNL.53.2.435",
"doi-asserted-by": "publisher",
"key": "ref229"
},
{
"DOI": "10.1034/k.1600-079x.2002.01881.x",
"doi-asserted-by": "publisher",
"key": "ref230"
}
],
"reference-count": 230,
"references-count": 230,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2076-3921/10/7/1152"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "The Coronavirus Disease 2019 (COVID-19): Key Emphasis on Melatonin Safety and Therapeutic Efficacy",
"type": "journal-article",
"volume": "10"
}