Melatonin Potentially Acts as a Widely-Acting Protective Tool in COVID-19
et al., Medicine Research, doi:10.21127/yaoyimr20240006, Jun 2024
Melatonin for COVID-19
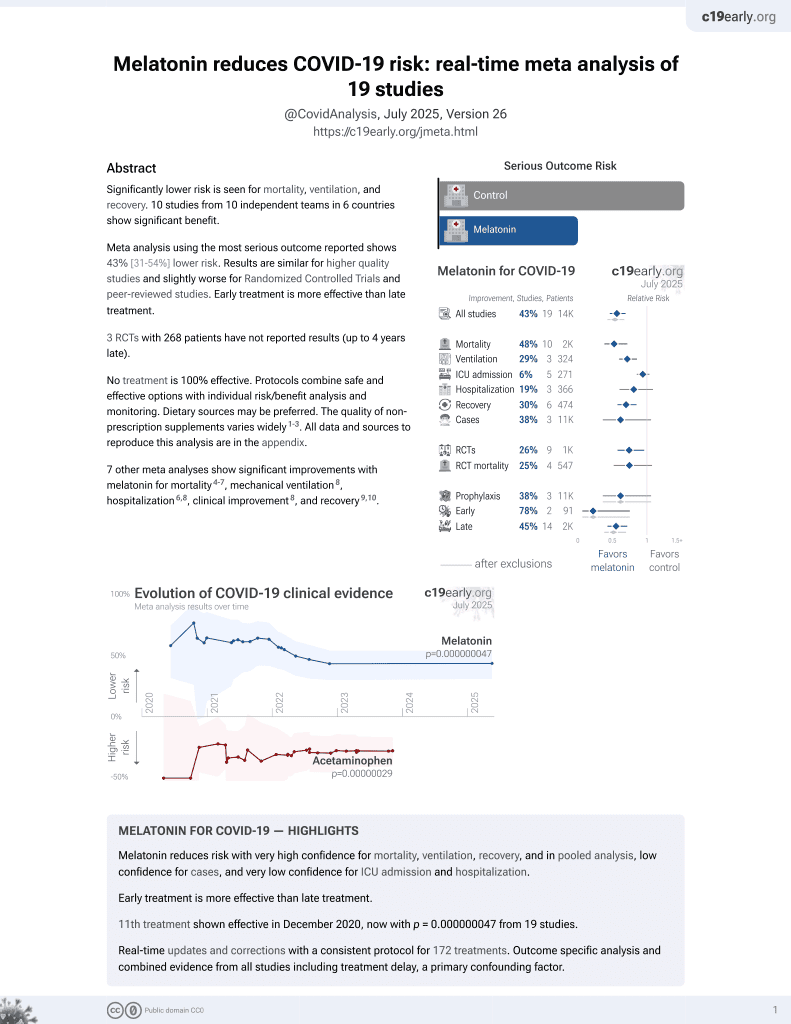
12th treatment shown to reduce risk in
December 2020, now with p = 0.0000000099 from 19 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Review of melatonin for COVID-19. Authors highlight melatonin's role in potentially preventing, treating, and improving recovery from SARS-CoV-2 infection. Melatonin is suggested to boost resistance to COVID-19 by strengthening the immune system and improving sleep quality. As a treatment, melatonin's anti-inflammatory and antioxidant properties may help suppress excessive inflammation and oxidative stress resulting from COVID-19 pathology. Authors note melatonin's ability to preserve mitochondrial function and reduce complications from comorbidities like obesity and diabetes in COVID-19 patients. The molecule is also proposed to protect against lung damage caused by SARS-CoV-2. For long COVID, melatonin is suggested as a potential treatment for neurological symptoms and mood disorders due to its neuroprotective properties. The review emphasizes melatonin's high safety profile and low cost as advantages for its use against COVID-19. However, authors caution that potential side effects and interactions with other medications should be considered, especially in elderly patients.
1.
Chen et al., Viral mitochondriopathy in COVID-19, Redox Biology, doi:10.1016/j.redox.2025.103766.
2.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
3.
Xie et al., The role of reactive oxygen species in severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) infection-induced cell death, Cellular & Molecular Biology Letters, doi:10.1186/s11658-024-00659-6.
4.
Zhao et al., Melatonin Potentially Acts as a Widely-Acting Protective Tool in COVID-19, Medicine Research, doi:10.21127/yaoyimr20240006.
5.
Yehia et al., Melatonin: a ferroptosis inhibitor with potential therapeutic efficacy for the post-COVID-19 trajectory of accelerated brain aging and neurodegeneration, Molecular Neurodegeneration, doi:10.1186/s13024-024-00728-6.
6.
Chacin-Bonilla et al., Melatonin and viral infections: A review focusing on therapeutic effects and SARS-CoV-2, Melatonin Research, doi:10.32794/mr112500168.
7.
Lempesis et al., A mid‑pandemic night's dream: Melatonin, from harbinger of anti‑inflammation to mitochondrial savior in acute and long COVID‑19 (Review), International Journal of Molecular Medicine, doi:10.3892/ijmm.2024.5352.
8.
Alomari et al., Assessing the antiviral potential of melatonin: A comprehensive systematic review, Reviews in Medical Virology, doi:10.1002/rmv.2499.
9.
Donzelli, A., Neglected Effective Early Therapies against COVID-19: Focus on Functional Foods and Related Active Substances. A Review, MDPI AG, doi:10.20944/preprints202312.1178.v1.
10.
Langen, M., Melatonin - the Hormone of Both Sun and Darkness - Protects Your Health and Can Save Your Life, Rounding The Earth, roundingtheearth.substack.com/p/melatonin-the-hormone-of-both-sun.
11.
Hosseinzadeh et al., Melatonin effect on platelets and coagulation: Implications for a prophylactic indication in COVID-19, Life Sciences, doi:10.1016/j.lfs.2022.120866.
12.
Loh et al., Melatonin: Regulation of Viral Phase Separation and Epitranscriptomics in Post-Acute Sequelae of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms23158122.
13.
Reiter et al., Melatonin: highlighting its use as a potential treatment for SARS-CoV-2 infection, Cellular and Molecular Life Sciences, doi:10.1007/s00018-021-04102-3.
14.
Tan et al., Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality, Life Sciences, doi:10.1016/j.lfs.2022.120368.
15.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
16.
Castle et al., Implications for Systemic Approaches to COVID-19: Effect Sizes of Remdesivir, Tocilizumab, Melatonin, Vitamin D3, and Meditation, Journal of Inflammation Research, doi:10.2147/JIR.S323356.
17.
Ramos et al., The Coronavirus Disease 2019 (COVID-19): Key Emphasis on Melatonin Safety and Therapeutic Efficacy, Antioxidants, doi:10.3390/antiox10071152.
18.
Camp et al., Melatonin interferes with COVID-19 at several distinct ROS-related steps, Journal of Inorganic Biochemistry, doi:10.1016/j.jinorgbio.2021.111546.
19.
Cross et al., Melatonin for the Early Treatment of COVID-19: A Narrative Review of Current Evidence and Possible Efficacy, Endocrine Practice, doi:10.1016/j.eprac.2021.06.001.
20.
DiNicolantonio et al., Melatonin may decrease risk for and aid treatment of COVID-19 and other RNA viral infections, Open Heart, doi:10.1136/openhrt-2020-001568.
21.
Reiter (B) et al., Therapeutic Algorithm for Use of Melatonin in Patients With COVID-19, Frontiers in Medicine, doi:10.3389/fmed.2020.00226.
22.
Charaa et al., Prophylactic Treatment Protocol against the Severity of COVID-19 Using Melatonin, SSRN, doi:10.2139/ssrn.3601861.
Zhao et al., 1 Jun 2024, peer-reviewed, 5 authors.
Melatonin
doi:10.21127/yaoyimr20240006
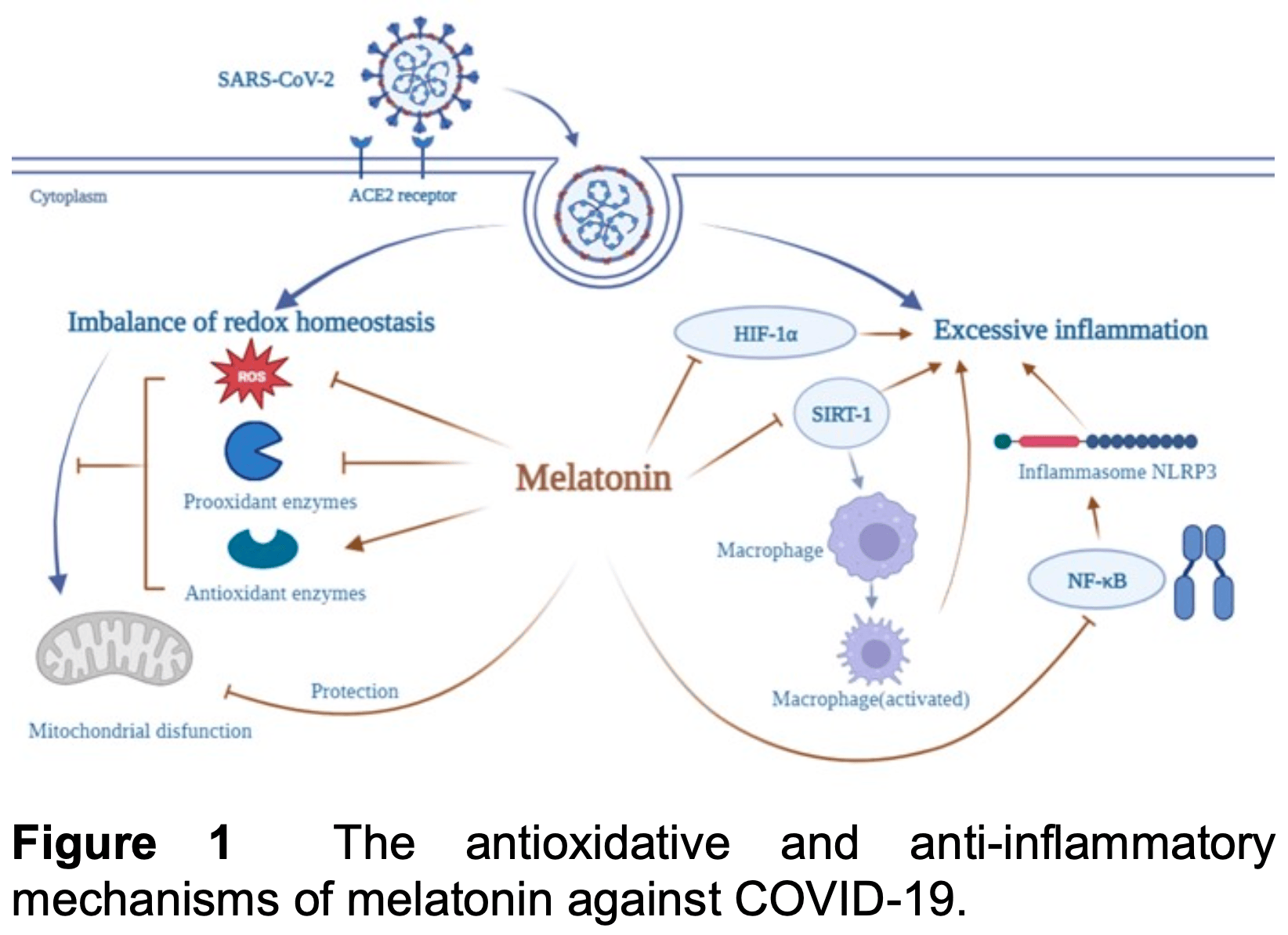
COVID-19 is an infectious disease caused by the SARS-CoV-2. It has resulted in a very large number of infected individuals and numerous deaths. Given the faster mutation rate of this RNA virus exceeds the time required for the development of vaccines, effective drugs for COVID-19 prevention and treatment should be urgently identified to terminate the pandemic. Functioning as an anti-inflammatory, antioxidant, and immune regulator, melatonin is a promising drug as a treatment for COVID-19. This review presents studies on the prophylaxis, therapeutic, and recovery roles of melatonin for this disease. Melatonin remarkably boosts the resistance to COVID-19 by strengthening the immune system, acting as a vaccine adjuvant, and improving sleep. Melatonin has been suggested as a treatment for COVID-19 since it preserves mitochondrial physiology, reduces the consequences of comorbidities, and suppresses excessive inflammation, oxidation, and exaggerated immune response resulting from COVID-19 pathology. Since the sequelae of COVID-19 are also a major health concern worldwide apart from COVID-19 per se, melatonin has been suggested as a potential drug in the treatment of neurological symptoms observed in "LONG COVID". Collectively, these beneficial effects highlight the role of melatonin as a potential alternative drug for the better management of SARS-CoV-2 infection.
Author Contributions Following are the details of the contributions made by each of the authors for the manuscript: Er-Qiang Zhao and Wen-Xiu Lu equally contributed to this work. Da-Ke Zhao conceived the study and revised the manuscript. Er-Qiang Zhao and Wen-Xiu Lu collected data and drafted manuscript. Zong-Min Mou and En-Da Sun analyzed the data and provided suggestions. All authors agree to be accountable for all aspects of work ensuring integrity and accuracy.
Conflict of Interest The authors declare no conflict of interest.
References
Acuña-Castroviejo, Escames, Venegas, Díaz-Casado, Lima-Cabello et al., Extrapineal melatonin: sources, regulation, and potential functions, Cell. Mol. Life Sci
Ahmad, Feigen, Vazquez, Kobets, Altschul, Neurological sequelae of COVID-19, J. Integr. Neurosci
Ahmed, The coronavirus disease 2019, (covid-19): a review, J. Adv. Med. Med. Res
Andersen, Gögenur, Rosenberg, Reiter, The safety of melatonin in humans, Clin. Drug Invest
Beck, Léger, Fressard, Peretti-Watel, Verger et al., Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level, J. Sleep Res
Berkhout, Herrera-Carrillo, SARS-CoV-2 Evolution: on the sudden appearance of the omicron variant, J. Virol
Bowe, Xie, Al-Aly, Postacute sequelae of COVID-19 at 2 years, Nat. Med
Brown, Karthikeyan, Pandi-Perumal, Cardinali, Autism spectrum disorder patients may be susceptible to COVID-19 disease due to deficiency in melatonin, Med. Hypotheses
Camini, Da Silva Caetano, Almeida, De Brito Magalhães, Implications of oxidative stress on viral pathogenesis, Arch. Virol
Campos, Cipolla-Neto, Amaral, Michelini, Bader et al., The angiotensin-melatonin axis, Int. J. Hypertens
Cardinali, Brown, Pandi-Perumal, Can melatonin be a potential "Silver Bullet" in treating COVID-19 patients?, Diseases
Cardinali, Hardeland, Inflammaging, Zhao, syndrome and melatonin: a call for treatment studies, metabolic Med. Res
Cardinali, Srinivasan, Brzezinski, Brown, Melatonin and its analogs in insomnia and depression, J. Pineal Res
Carrillo-Vico, Lardone, Álvarez-Sánchez, Rodríguez-Rodríguez, Guerrero, Melatonin: buffering the immune system, Int. J. Mol. Sci
Chitimus, Popescu, Voiculescu, Panaitescu, Pavel et al., Melatonin's impact on antioxidative and anti-inflammatory reprogramming in homeostasis and disease, Biomolecules
Chowdhury, Hossain, Kashem, Shahid, Alam, Immune response in COVID-19: A review, J. Infect. Public Heal
Codo, Davanzo, Monteiro, De Souza, Muraro et al., Elevated glucose levels favor SARS-CoV-2 infection and monocyte response through a HIF-1α/Glycolysis-dependent axis, Cell Metab
Daryani, Montazeri, Pagheh, Sharif, Sarvi et al., The potential use of melatonin to treat protozoan parasitic infections: A review, Biomed. Pharmacother
El-Missiry, El-Missiry, Othman, Melatonin is a potential adjuvant to improve clinical outcomes in individuals with obesity and diabetes with coexistence of Covid-19, Eur. Pharmacol
Escames, León, Macías, Khaldy, Acuña-Castroviejo, Melatonin counteracts lipopolysaccharide-induced expression and activity of mitochondrial nitric oxide synthase in rats, FASEB J
Estrada-Reyes, Valdés-Tovar, Arrieta-Baez, Dorantes-Barrón, Quero-Chávez et al., The timing of melatonin administration is crucial for its antidepressant-like effect in mice, Int. J. Mol. Sci
Foster, Cvijovic, Boon, Tam, Liu et al., Melatonin interaction resulting in severe sedation, J. Pharm. Pharmaceut. Sci
Galano, Tan, Reiter, Melatonin: A Versatile Protector against Oxidative DNA Damage, Molecules
Gorbalenya, Baker, Baric, De Groot, Drosten et al., The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2, Nat. Microbiol
Grifoni, Weiskopf, Ramirez, Mateus, Dan et al., Targets of T cell responses to SARS-CoV-2 coronavirus in hHumans with COVID-19 disease and unexposed individuals, Cell
Guo, Li, Dong, Zhou, Zhang et al., Diabetes is a risk factor for the progression and prognosis of COVID-19, Diabetes/Metab. Res
Hardeland, Melatonin and inflammation-story of a double-edged blade, J. Pineal Res
Hardeland, Melatonin and the electron transport chain, Cell. Mol. Life Sci
Hu, Ma, Jiang, Fan, Deng et al., Melatonin: the dawning of a treatment for fibrosis?, J. Pineal Res
Huang, Chiou, Liu, Hu, Su et al., Melatonin attenuates TNF-α and IL-1β expression in synovial fibroblasts and diminishes cartilage degradation: Implications for the treatment of rheumatoid arthritis, J. Pineal Res
Huang, Liao, Chen, Shi, Lin et al., Melatonin possesses an anti-influenza potential through its immune modulatory effect, J. Funct. Foods
Huang, Wang, Li, Ren, Zhao et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, The Lancet
Jacob, Poeggeler, Weishaupt, Sirén, Hardeland et al., Melatonin as a candidate compound for neuroprotection in amyotrophic lateral sclerosis (ALS): high tolerability of daily oral melatonin 6 www, medicineresearch.org Med. Res
Jafari-Vayghan, Saleh-Ghadimi, Maleki, Moludi, Alizadeh, The effects of melatonin on neurohormonal regulation in cardiac cachexia: A mechanistic review, J. Cell. Biochem
James, Mark, Jorge, Melatonin may decrease risk for and aid treatment of COVID-19 and other RNA viral infections, Open Heart
Jarrott, Head, Pringle, Lumbers, Martin, LONG COVID"-A hypothesis for understanding the biological basis and pharmacological treatment strategy, Pharmacol. Res. Perspect
Juybari, Pourhanifeh, Hosseinzadeh, Hemati, Mehrzadi, Melatonin potentials against viral infections including COVID-19: Current evidence and new findings, Virus Res
Kleszczyński, Slominski, Steinbrink, Reiter, Clinical trials for use of melatonin to fight against COVID-19 are urgently needed, Nutrients
Lin, Lu, Cao, Li, Hypothesis for potential pathogenesis of SARS-CoV-2 infection-a review of immune changes in patients with viral pneumonia, Emerg. Microbes Infec
Lowes, Almawash, Webster, Reid, Galley, Melatonin and structurally similar compounds have differing effects on inflammation and mitochondrial function in endothelial cells under conditions mimicking sepsis, Brit. J. Anaesth
López, Escames, Ortiz, Ros, Acuña-Castroviejo, Melatonin restores the mitochondrial production of ATP in septic mice, Neuro. Endocrinol. Lett
Ma, Chen, Feng, Zhang, Fan et al., Melatonin ameliorates the progression of atherosclerosis via mitophagy activation and NLRP3 inflammasome inhibition, Oxid. Med. Cell. Longev
Maclaren, Fisher, Brodie, Preparing for the most critically Ill patients with COVID-19: the potential role of extracorporeal membrane oxygenation, JAMA-J. Am. Med. Assoc
Maestroni, Exogenous melatonin as potential adjuvant in anti-SarsCov2 vaccines, J. Neuroimmune Pharmacol
Man, Karki, Kanneganti, Molecular mechanisms and functions of pyroptosis, inflammatory caspases and inflammasomes in infectious diseases, Immunol. Rev
Marie, Emotion, emotion regulation and sleep: An intimate relationship, AIMS Neurosci
Martorina, Tavares, Possible role of exogenous melatonin in preventing more serious COVID-19 infection in patients with type 2 diabetes mellitus, Rev. Assoc. Med. Bras
Martín Giménez, Prado, Diez, Manucha, Reiter, New proposal involving nanoformulated melatonin targeted to the mitochondria as a potential COVID-19 treatment, Nanomedicine
Morin, Carrier, Bastien, Godbout, On Behalf Of The Canadian et al., Sleep and circadian rhythm in response to the COVID-19 pandemic, Can. J. Pub. Health
Mouffak, Shubbar, Saleh, El-Awady, Recent advances in management of COVID-19: A review, Biomed. Pharmacother
Muniyappa, Gubbi, COVID-19 pandemic, coronaviruses, and diabetes mellitus, Am. J. Physiol.-Endocrinol. Metab
Méndez, Balanzá-Martínez, Luperdi, Estrada, Latorre et al., Short-term neuropsychiatric outcomes and quality of life in COVID-19 survivors, J. Int. Med
Parlakpinar, Polat, Acet, Pharmacological agents under investigation in the treatment of coronavirus disease 2019 and the importance of melatonin, Fund. Clin. Pharmacol
Priyal, Dean, Hasan, Long COVID' syndrome, BMJ Case Rep
Ragab, Salah Eldin, Taeimah, Khattab, Salem, The COVID-19 cytokine storm; what we know so far, Front. Immunol
Rahimi, Mohebbi, Vakilzadeh, Biglari, Razeghi et al., Enhancement of therapeutic DNA vaccine potency by melatonin through inhibiting VEGF expression and induction of antitumor immunity mediated by CD8+ T cells, Arch. Virol
Rahman, Hasan, Kobori, Melatonin in chronic kidney disease: a promising chronotherapy targeting the intrarenal renin-angiotensin system, Hypertens. Res
Ramos, Míguez, Morgado, Sanchez-Correa, Gordillo et al., Melatonin Enhances Responsiveness to Dichelobacter Nodosus Vaccine in Sheep and Increases Peripheral Blood CD4 T Lymphocytes and IgG-Expressing B Lymphocytes, Vet. Immunol. Immunopathol
Ramos, Míguez, Morgado, Sanchez-Correa, Gordillo et al., Melatonin enhances responsiveness to Dichelobacter nodosus vaccine in sheep and increases peripheral blood CD4+ T lymphocytes and IgG-expressing B lymphocytes, Vet. Immunol. Immunopathol
Regodón, Martín-Palomino, Fernández-Montesinos, Herrera, Carrascosa-Salmoral et al., The use of melatonin as a vaccine agent, Vaccine
Reiter, Abreu-Gonzalez, Marik, Dominguez-Rodriguez, Therapeutic algorithm for use of melatonin in patients with COVID-19, Front. Med
Reiter, Mayo, Tan, Sainz, Alatorre-Jimenez et al., Melatonin as an antioxidant: under promises but over delivers, J. Pineal Res
Reiter, Sharma, Ma, Dominquez-Rodriguez, Marik et al., Melatonin inhibits COVID-19-induced cytokine storm by reversing aerobic glycolysis in immune cells: a mechanistic analysis, Med. Drug Discov
Reiter, Sharma, Rosales-Corral, De Mange, Phillips et al., Melatonin in ventricular and subarachnoid cerebrospinal fluid: Its function in the neural glymphatic network and biological significance for neurocognitive health, Biochem. Bioph. Res. Co
Reiter, Sharma, Simko, Dominguez-Rodriguez, Tesarik et al., Melatonin: highlighting its use as a potential treatment for SARS-CoV-2 infection, Cell. Mol. Life Sci
Rodríguez-Rubio, Figueira, Acuña-Castroviejo, Borobia, Escames et al., A phase II, single-center, double-blind, randomized placebo-controlled trial to explore the efficacy and safety of intravenous melatonin in patients with COVID-19 admitted to the intensive care unit (MelCOVID study): a structured summary of a study protocol for a randomized controlled trial, Trials
Romero, Ramos, López-Muñoz, Gil-Martín, Escames et al., Coronavirus disease 2019 (COVID-19) and its neuroinvasive capacity: is it time for melatonin? Cell, Mol. Neurobiol
Samaee, Mohsenzadegan, Ala, Maroufi, Moradimajd, Tocilizumab for treatment patients with COVID-19: Recommended medication for novel disease, Int. Immunopharmacol
Sanders, Monogue, Jodlowski, Cutrell, Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review, JAMA-J. Am. Med. Assoc
Satyanarayanan, Su, Lin, Su, Circadian Rhythm and Melatonin in the Treatment of Depression, Curr. Pharmaceut. Design
Schönrich, Raftery, Samstag, Devilishly radical NETwork in COVID-19: Oxidative stress, neutrophil extracellular traps (NETs), and T cell suppression, Adv. Biol. Regul
Shang, Song, Li, Xie, Xu et al., Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery, eClinicalMedicine
Shi, Gao, Shao, Pyroptosis: Gasdermin-Mediated Programmed Necrotic Cell Death, Trends Biochem. Sci
Shi, Nabar, Huang, Kehrl, SARS-Coronavirus Open Reading Frame-8b triggers intracellular stress pathways and activates NLRP3 inflammasomes, Cell Death Discov
Shi, Wang, Yin, Ouyang, Pang et al., The inhibition of IL-2/IL-2R gives rise to CD8+ T cell and lymphocyte decrease through JAK1-STAT5 in critical patients with COVID-19 pneumonia, Cell Death Dis
Shin, Ko, Kim, Park, Kim et al., Role of melatonin as an SIRT1 enhancer in chronic obstructive pulmonary disease induced by cigarette smoke, J. Cell. Mol. Med
Shneider, Kudriavtsev, Vakhrusheva, Can melatonin reduce the severity of COVID-19 pandemic?, Int. Rev. Immunol
Shrestha, Foster, Rawlinson, Tedla, Bull, Evolution of the SARS-CoV-2 omicron variants BA.1 to BA.5: Implications for immune escape and transmission, Rev. Med. Virol
Shukla, Chinchalongporn, Govitrapong, Reiter, The role of melatonin in targeting cell signaling pathways in neurodegeneration, Ann. N. Y. Acad. Sci
Siddiqi, Mehra, COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal, J. Heart Lung Transpl
Silman, Melatonin: a contraceptive for the nineties, Eur. J. Obstet. Gyn. Reprod. Biol
Srinivasan, Maestroni, Cardinali, Esquifino, Perumal et al., Melatonin, immune function and aging, Immun. Ageing
Sun, Lee, Kao, Chiang, Sung et al., Systemic combined melatonin-mitochondria treatment improves acute respiratory distress syndrome in the rat, J. Pineal Res
Suofu, Li, Jean-Alphonse, Jia, Khattar et al., Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome c release, Proc. Natl. Acad. Sci. U. S. A
Tan, Hardeland, Potential utility of melatonin in deadly infectious diseases related to the overreaction of innate immune response and destructive inflammation: focus on COVID-19, Melatonin Res
Tan, Kheirandish-Gozal, Gozal, Sleep, Allergy and Sleep: Basic Principles and Clinical Practice
Tan, Manchester, Terron, Flores, Reiter, One molecule, many derivatives: A never-ending interaction of melatonin with reactive oxygen and nitrogen species?, J. Pineal Res
Tan, Reiter, Melatonin reduces the mortality of severely-infected COVID-19 patients, Melatonin Res
Taquet, Geddes, Husain, Luciano, Harrison, 6-month neurological and psychiatric outcomes in 236379 survivors of COVID-19: a retrospective cohort study using electronic health records, Lancet Psychiat
Teixeira, Santos, De Medeiros, Mendes, Cunha et al., Night workers have lower levels of antioxidant defenses and higher levels of oxidative stress damage when compared to day workers, Sci. Rep
Tong, Tang, Li, Li, Wang et al., Potential Presymptomatic Transmission of SARS-CoV-2, Zhejiang Province, China, Emerg. Infect. Dis. J
Tordjman, Chokron, Delorme, Charrier, Bellissant et al., Melatonin: pharmacology, functions and therapeutic benefits, Curr. Neuropharmacol
Tseng, Yang, Lu, Two hits to the renin-angiotensin system may play a key role in severe COVID-19, Kaohsiung J. Med. Sci
Tuft, Matar, Menczel Schrire, Grunstein, Yee et al., Current insights into the risks of using melatonin as a treatment for sleep disorders in older adults, Clin. Interv. Aging
Tütüncüler, Eskiocak, Başaran, Ekuklu, Ayvaz et al., The protective role of melatonin in experimental hypoxic brain damage, Pediatr. Int
Valdés-Tovar, Estrada-Reyes, Solís-Chagoyán, Argueta, Dorantes-Barrón et al., Circadian modulation of neuroplasticity by melatonin: a target in the treatment of depression, Brit. J. Pharmacol
Vlachou, Siamidi, Dedeloudi, Konstantinidou, Papanastasiou, Pineal hormone melatonin as an adjuvant treatment for COVID-19 (Review), Int. J. Mol. Med
Vriend, Reiter, The Keap1-Nrf2-antioxidant response element pathway: A review of its regulation by melatonin and the proteasome, Mol. Cell. Endocrinol
Wells, Paterson, Bacchi, Page, Baumert et al., Brain fog in postural tachycardia syndrome: An objective cerebral blood flow and neurocognitive analysis, J. Arrhythm
Wichniak, Kania, Siemiński, Cubała, Melatonin as a potential adjuvant treatment for covid-19 beyond sleep disorders, Int. J. Mol. Sci
Wongchitrat, Shukla, Sharma, Govitrapong, Reiter, Role of melatonin on virus-induced neuropathogenesis-a concomitant therapeutic strategy to understand SARS-CoV-2 infection, Antioxidants
Wu, Ji, Wang, Gu, Gu et al., Melatonin alleviates radiation-induced lung injury via regulation of miR-30e/NLRP3 axis, Oxid. Med. Cell. Longev
Wu, Mcgoogan, Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) outbreak in china: summary of a report of 72 314 cases from the Chinese center for disease control and prevention, JAMA-J. Am. Med. Assoc
Wu, Peng, Liao, Pao, Huang et al., Melatonin receptor agonist protects against acute lung injury induced by ventilator through up-regulation of IL-10 production, Resp. Res
Xia, Chen, Zeng, Zhao, Zhu et al., Melatonin in macrophage biology: Current understanding and future perspectives, J. Pineal Res
Xu, Xie, Al-Aly, Long-term gastrointestinal outcomes of COVID-19, Nat. Commun
Xue, Lin, Zhang, Gong, Liu et al., Sleep problems and medical isolation during the SARS-CoV-2 outbreak, Sleep Med
Yeong-Min, Su Kil, Gwang-Hoon, Jung-Youl, Seong-Soo, Pharmacological advantages of melatonin in immunosenescence by improving activity of T lymphocytes, J. Biomed. Res
Yong, Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments, Infect. Dis
Zhang, Dong, Liu, Gao, Risk and protective factors for COVID-19 morbidity, severity, and mortality, Clin. Rev. Allergy Immunol
Zhang, Wang, Ni, Di, Ma et al., COVID-19: Melatonin as a potential adjuvant treatment, Life Sci
Zhao, Sun, Su, Shan, Zhang et al., Melatonin Protects against Lung Fibrosis by Regulating the Hippo/YAP Pathway, Int. J. Mol. Sci
Zhao, administration in ALS patients, J. Pineal Res
Zhou, Tan, Letter to the Editor: Diabetes patients with COVID-19 need better blood glucose management in Wuhan, China, Metabolism