Can melatonin reduce the severity of COVID-19 pandemic?
et al., International Reviews of Immunology, doi:10.1080/08830185.2020.1756284, Apr 2020
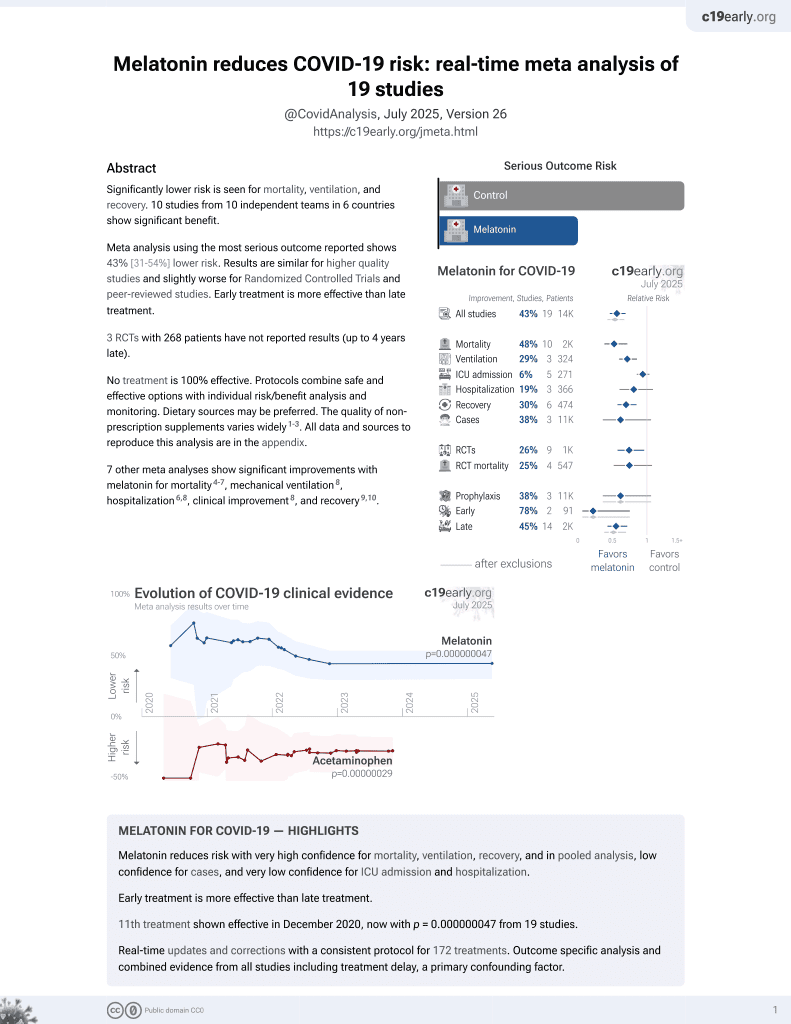
Melatonin for COVID-19
12th treatment shown to reduce risk in
December 2020, now with p = 0.0000000099 from 19 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Review of the potential benefits of melatonin for COVID-19.
1.
Chen et al., Viral mitochondriopathy in COVID-19, Redox Biology, doi:10.1016/j.redox.2025.103766.
2.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
3.
Xie et al., The role of reactive oxygen species in severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) infection-induced cell death, Cellular & Molecular Biology Letters, doi:10.1186/s11658-024-00659-6.
4.
Zhao et al., Melatonin Potentially Acts as a Widely-Acting Protective Tool in COVID-19, Medicine Research, doi:10.21127/yaoyimr20240006.
5.
Yehia et al., Melatonin: a ferroptosis inhibitor with potential therapeutic efficacy for the post-COVID-19 trajectory of accelerated brain aging and neurodegeneration, Molecular Neurodegeneration, doi:10.1186/s13024-024-00728-6.
6.
Chacin-Bonilla et al., Melatonin and viral infections: A review focusing on therapeutic effects and SARS-CoV-2, Melatonin Research, doi:10.32794/mr112500168.
7.
Lempesis et al., A mid‑pandemic night's dream: Melatonin, from harbinger of anti‑inflammation to mitochondrial savior in acute and long COVID‑19 (Review), International Journal of Molecular Medicine, doi:10.3892/ijmm.2024.5352.
8.
Alomari et al., Assessing the antiviral potential of melatonin: A comprehensive systematic review, Reviews in Medical Virology, doi:10.1002/rmv.2499.
9.
Donzelli, A., Neglected Effective Early Therapies against COVID-19: Focus on Functional Foods and Related Active Substances. A Review, MDPI AG, doi:10.20944/preprints202312.1178.v1.
10.
Langen, M., Melatonin - the Hormone of Both Sun and Darkness - Protects Your Health and Can Save Your Life, Rounding The Earth, roundingtheearth.substack.com/p/melatonin-the-hormone-of-both-sun.
11.
Hosseinzadeh et al., Melatonin effect on platelets and coagulation: Implications for a prophylactic indication in COVID-19, Life Sciences, doi:10.1016/j.lfs.2022.120866.
12.
Loh et al., Melatonin: Regulation of Viral Phase Separation and Epitranscriptomics in Post-Acute Sequelae of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms23158122.
13.
Reiter et al., Melatonin: highlighting its use as a potential treatment for SARS-CoV-2 infection, Cellular and Molecular Life Sciences, doi:10.1007/s00018-021-04102-3.
14.
Tan et al., Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality, Life Sciences, doi:10.1016/j.lfs.2022.120368.
15.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
16.
Castle et al., Implications for Systemic Approaches to COVID-19: Effect Sizes of Remdesivir, Tocilizumab, Melatonin, Vitamin D3, and Meditation, Journal of Inflammation Research, doi:10.2147/JIR.S323356.
17.
Ramos et al., The Coronavirus Disease 2019 (COVID-19): Key Emphasis on Melatonin Safety and Therapeutic Efficacy, Antioxidants, doi:10.3390/antiox10071152.
18.
Camp et al., Melatonin interferes with COVID-19 at several distinct ROS-related steps, Journal of Inorganic Biochemistry, doi:10.1016/j.jinorgbio.2021.111546.
19.
Cross et al., Melatonin for the Early Treatment of COVID-19: A Narrative Review of Current Evidence and Possible Efficacy, Endocrine Practice, doi:10.1016/j.eprac.2021.06.001.
20.
DiNicolantonio et al., Melatonin may decrease risk for and aid treatment of COVID-19 and other RNA viral infections, Open Heart, doi:10.1136/openhrt-2020-001568.
21.
Reiter (B) et al., Therapeutic Algorithm for Use of Melatonin in Patients With COVID-19, Frontiers in Medicine, doi:10.3389/fmed.2020.00226.
22.
Charaa et al., Prophylactic Treatment Protocol against the Severity of COVID-19 Using Melatonin, SSRN, doi:10.2139/ssrn.3601861.
Shneider et al., 29 Apr 2020, peer-reviewed, 3 authors.
Can melatonin reduce the severity of COVID-19 pandemic?
International Reviews of Immunology, doi:10.1080/08830185.2020.1756284
The current COVID-19 pandemic is one of the most devastating events in recent history. The virus causes relatively minor damage to young, healthy populations, imposing life-threatening danger to the elderly and people with diseases of chronic inflammation. Therefore, if we could reduce the risk for vulnerable populations, it would make the COVID-19 pandemic more similar to other typical outbreaks. Children don't suffer from COVID-19 as much as their grandparents and have a much higher melatonin level. Bats are nocturnal animals possessing high levels of melatonin, which may contribute to their high anti-viral resistance. Viruses induce an explosion of inflammatory cytokines and reactive oxygen species, and melatonin is the best natural antioxidant that is lost with age. The programmed cell death coronaviruses cause, which can result in significant lung damage, is also inhibited by melatonin. Coronavirus causes inflammation in the lungs which requires inflammasome activity. Melatonin blocks these inflammasomes. General immunity is impaired by anxiety and sleep deprivation. Melatonin improves sleep habits, reduces anxiety and stimulates immunity. Fibrosis may be the most dangerous complication after COVID-19. Melatonin is known to prevent fibrosis. Mechanical ventilation may be necessary but yet imposes risks due to oxidative stress, which can be reduced by melatonin. Thus, by using the safe over-the-counter drug melatonin, we may be immediately able to prevent the development of severe disease symptoms in coronavirus patients, reduce the severity of their symptoms, and/or reduce the immuno-pathology of coronavirus infection on patients' health after the active phase of the infection is over.
Disclosure statement The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported. The authors declare that they did not receive financial support from any private or public institution for performing this work, writing and publishing this paper.
References
Adikwu, Brambaifa, Obianime, Melatonin and alpha lipoic acid restore electrolytes and kidney morphology of lopinavir/ritonavir-treated rats, J Nephropharmacol, doi:10.15171/npj.2020.06
Akbulut, Icli, B€ Uy€ Ukcelik, The role of granulocyte-macrophage-colony stimulating factor, cortisol, and melatonin in the regulation of the circadian rhythms of peripheral blood cells in healthy volunteers and patients with breast cancer, J Pineal Res, doi:10.1111/j.1600-079X.1999.tb00560.x
Arioz, Tastan, Tarakcioglu, Melatonin attenuates LPS-induced acute depressive-like behaviors and microglial NLRP3 inflammasome activation through the SIRT1/Nrf2 pathway, Front Immunol, doi:10.3389/fimmu.2019.01511
Ben-Nathan, Maestroni, Lustig, Protective effects of melatonin in mice infected with encephalitis viruses, Arch Virol, doi:10.1007/BF01309858
Bryant, Trinder, Curtis, Sick and tired: does sleep have a vital role in the immune system?, Nat Rev Immunol, doi:10.1038/nri1369
Cabrera-Ben Itez, Parotto, Post, Mechanical stress induces lung fibrosis by epithelialmesenchymal transition, Crit Care Med, doi:10.1097/ccm.0b013e31822f09d7
Calisher, Childs, Field, Bats: Important reservoir hosts of emerging viruses, CMR, doi:10.1128/CMR.00017-06
Cao, Wang, Wen, A trial of Lopinavir-Ritonavir in adults hospitalized with severe Covid-19, New Eng J Med, doi:10.1056/nejmoa2001282
Carrillo-Vico, Reiter, Lardone, The modulatory role of melatonin on immune responsiveness, Curr Opin Investig Drugs
Cayli, Kocak, Yilmaz, Effect of combined treatment with melatonin and methylprednisolone on neurological recovery after experimental spinal cord injury, Eur Spine J, doi:10.1007/s00586-003-0550-y
Chen, Kozlovsky, Effros, Vaccination in the elderly: an immunological perspective, Trends Immunol, doi:10.1016/j.it.2009.05.002
Colson, Rolain, Lagier, Chloroquine and hydroxychloroquine as available weapons to fight COVID-19, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.105932
Cookson, Brennan, Pro-inflammatory programmed cell death, Trends Microbiol, doi:10.1016/S0966-842X(00)01936-3
Demas, Klein, Nelson, Reproductive and immune responses to photoperiod and melatonin are linked in Peromyscus subspecies, J Comp Physiol A, doi:10.1007/BF00207360
Dhabhar, Enhancing versus suppressive effects of stress on immune function: Implications for immunoprotection and immunopathology, Neuroimmunomodulation, doi:10.1159/000216188
Duflo, Debon, Goudable, Alveolar and serum oxidative stress in ventilator-associated pneumonia, Br J Anaesthesia, doi:10.1093/bja/aef169
Elfiky, Anti-HCV, nucleotide inhibitors, repurposing against COVID-19, Life Sci, doi:10.1016/j.lfs.2020.117477
Emerit, Filipe, Freitas, Protective effect of superoxide dismutase against hair graying in a mouse model, Photochem Photobiol, doi:10.1562/0031-8655(2004)0800579:PEOSDA2.0.CO;2
Everson, Sustained sleep deprivation impairs host defense, Integr Comparative Physiol, doi:10.1152/ajpregu.1993.265.5.R1148
Fan, Zhao, Shi, Bat coronaviruses in China, Viruses, doi:10.3390/v11030210
Figueiro, Rea, The effects of red and blue lights on circadian variations in cortisol, alpha amylase, and melatonin, Int J Endocrinol, doi:10.1155/2010/829351
Gautret, Lagier, Parola, Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label nonrandomized clinical trial, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.105949
Goodwin, Viboud, Simonsen, Antibody response to influenza vaccination in the elderly: A quantitative review, Vaccine, doi:10.1016/j.vaccine.2005.08.105
Gurkan, Donnell, Brower, Differential effects of mechanical ventilatory strategy on lung injury and systemic organ inflammation in mice, Am J Physiol, doi:10.1152/ajplung.00044.2003
Habtemariam, Daglia, Sureda, Melatonin and respiratory diseases: a review, CTMC, doi:10.2174/1568026616666160824120338
Hajak, Rodenbeck, Staedt, Nocturnal plasma melatonin levels in patients suffering from chronic primary insomnia, J Pineal Res, doi:10.1111/j.1600-079X.1995.tb00179.x
Haldar, Singh, Guchhait, Relationship between the annual rhythms in melatonin and immune system status in the tropical palm squirrel, Funambulus Pennanti, Chronobiol Int, doi:10.1081/CBI-100001174
Haldar, Yadav, Alipreeta, Annual reproductive synchronization in ovary and pineal gland function of female short-nosed fruit bat, Cynopterus sphinx, Comparative Biochem Physiol Part A: Mol Integr Physiol, doi:10.1016/j.cbpa.2006.02.041
Han, Lu, Huang, Synergy effect of melatonin on anti-respiratory syscytical virus activity of Ribavirin in vitro
Heideman, Bhatnagar, Hilton, Melatonin rhythms and pineal structure in a tropical bat, Anoura geoffroyi, that does not use photoperiod to regulate seasonal reproduction, J Pineal Res, doi:10.1111/j.1600-079X.1996.tb00245.x
Hu, Zeng, Yang, Discovery of a rich gene pool of bat SARS-related coronaviruses provides new insights into the origin of SARS coronavirus, PLoS Pathog, doi:10.1371/journal.ppat.1006698
Huang, Liao, Chen, Melatonin possesses an anti-influenza potential through its immune modulatory effect, J Funct Foods, doi:10.1016/j.jff.2019.04.062
Ibarra-Coronado, Pantale On-Mart Inez, Velazqu Ez-Moctezuma, The bidirectional relationship between sleep and immunity against infections, J Immunol Res, doi:10.1155/2015/678164
Iguchi, Kato, Ibayashi, Age-dependent reduction in serum melatonin concentrations in healthy human subjects, J. Clin. Endocrinol. Metabol, doi:10.1210/jcem-55-1-27
Imai, Kuba, Neely, Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury, Cell, doi:10.1016/j.cell.2008.02.043
Kapoor, Kapoor, Role of Chloroquine and Hydroxychloroquine in the Treatment of COVID-19 Infection -A Systematic Literature Review, Medrxiv, doi:10.1101/2020.03.24.20042366
Kaptanoglu, Tuncel, Palaoglu, Comparison of the effects of melatonin and methylprednisolone in experimental spinal cord injury, Journal of Neurosurgery: Spine, doi:10.3171/spi.2000.93.1.0077
Khomich, Kochetkov, Bartosch, Redox biology of respiratory viral infections, Viruses, doi:10.3390/v10080392
Ko, Rolain, Lee, Arguments in favour of remdesivir for treating SARS-CoV-2 infections, Int J Antimicrob Agents, doi:10.1016/j.ijantimicag.2020.105933
Lange, Dimitrov, Born, Effects of sleep and circadian rhythm on the human immune system, Ann NY Acad Sci, doi:10.1111/j.1749-6632.2009.05300.x
Lange, Perras, Fehm, Sleep enhances the human antibody response to hepatitis A vaccination, Psychosomatic Med, doi:10.1097/01.psy.0000091382.61178.f1
Lau, Woo, Li, Complete genome sequence of bat coronavirus HKU2 from Chinese horseshoe bats revealed a much smaller spike gene with a different evolutionary lineage from the rest of the genome, Virology, doi:10.1016/j.virol.2007.06.009
Lim, Jeon, Shin, Case of the index patient who caused tertiary transmission of coronavirus disease 2019 in Korea: the application of Lopinavir/Ritonavir for the treatment of COVID-19 pneumonia monitored by quantitative RT-PCR, J Korean Med Sci, doi:10.3346/jkms.2020.35.e79
Lionetti, Recchia, Ranieri, Overview of ventilator-induced lung injury mechanisms, Curr Opin Crit Care, doi:10.1097/00075198-200502000-00013
Liu, Gan, Xu, Melatonin alleviates inflammasome-induced pyroptosis through inhibiting NF-jB/GSDMD signal in mice adipose tissue, J Pineal Res, doi:10.1111/jpi.12414
Ma, Chen, Feng, Melatonin ameliorates the progression of atherosclerosis via mitophagy activation and NLRP3 inflammasome inhibition, Oxid Med Cell Longevity, doi:10.1155/2018/9286458
Mackiewicz, Sollars, Ogilvie, Modulation of IL-1b gene expression in the rat CNS during sleep deprivation, NeuroReport, doi:10.1097/00001756-199601310-00037
Maestroni, Conti, Pierpaoli, Role of the pineal gland in immunity. III. Melatonin antagonizes the immunosuppressive effect of acute stress via an opiatergic mechanism, Immunology
Malhotra, Sawhney, Pandhi, The therapeutic potential of melatonin: a review of the science, MedGenMed
Man, Karki, Kanneganti, Molecular mechanisms and functions of pyroptosis, inflammatory caspases and inflammasomes in infectious diseases, Immunol Rev, doi:10.1111/imr.12534
Mandl, Schneider, Schneider, Going to bat(s) for studies of disease tolerance, Front Immunol, doi:10.3389/fimmu.2018.02112
Max, Menaker, Regulation of melatonin production by light, darkness, and temperature in the trout pineal, J Comp Physiol A, doi:10.1007/BF00191463
Michaelides, Retinal toxicity associated with hydroxychloroquine and chloroquine, Arch Ophthalmol, doi:10.1001/archophthalmol.2010.321
Naveenkumar, Hemshekhar, Kemparaju, Hemin-induced platelet activation and ferroptosis is mediated through ROS-driven proteasomal activity and inflammasome activation: Protection by Melatonin, Biochimica Et Biophys Acta, doi:10.1016/j.bbadis.2019.05.009
Nordlund, Lerner, The effects of oral melatonin on skin color and on the release of pituitary hormones, J Clin Endocrinol Metabolism, doi:10.1210/jcem-45-4-768
Onk, Onk, Erol, Effect of melatonin on antioxidant capacity, ınflammation and apoptotic cell death in lung tissue of diabetic rats, Acta Cir Bras, doi:10.1590/s0102-865020180040000009
Palmblad, Cantell, Strander, Stressor exposure and immunological response in man: Interferon-producing capacity and phagocytosis, J Psychosomatic Res, doi:10.1016/0022-3999(76)90020-9
Palmblad, Petrini, Wasserman, Lymphocyte and granulocyte reactions during sleep deprivation, Psychosom Med, doi:10.1097/00006842-197906000-00001
Palmer, Post, Klapaukh, The Association between supraphysiologic arterial oxygen levels and mortality in critically Ill patients. A multicenter observational cohort study, Am J Respir Crit Care Med, doi:10.1164/rccm.201904-0849OC
Panesar, Lymphopenia in SARS, The Lancet, doi:10.1016/S0140-6736(03)13557-X
Pangerl, Pangerl, Reiter, Circadian variations of adrenergic receptors in the mammalian pineal gland: A review, J Neural Transmission, doi:10.1007/BF01245442
Papavasiliou, Cotzias, Se, Melatonin and parkinsonism, JAMA, doi:10.1001/jama.1972.03200140072031
Parrish, Holmes, Morens, Crossspecies virus transmission and the emergence of new epidemic diseases, MMBR, doi:10.1128/MMBR.00004-08
Persengiev, Kanchev, Vezenkova, Crcadian patterns of melatonin, corticosterone, and progesterone in male rats subjected to chronic stress: Effect of constant illumination, J Pineal Res, doi:10.1111/j.1600-079X.1991.tb00456.x
Prasad, Ronk, Widen, Ebola virus produces discrete small noncoding RNAs independently of the host microRNA pathway which lack RNA interference activity in bat and human cells, J Virol, doi:10.1128/JVI.01441-19
Ramanathan, Gulyani, Nienhuis, Sleep deprivation decreases superoxide dismutase activity in rat hippocampus and brainstem, Neuroreport, doi:10.1097/00001756-200208070-00007
Reiter, Aging and oxygen toxicity: Relation to changes in melatonin, Age, doi:10.1007/s11357-997-0020-2
Reiter, Melatonin: lowering the high price of free radicals, Physiology, doi:10.1152/physiologyonline.2000.15.5.246
Reiter, Tang, Garcia, Pharmacological actions of melatonin in oxygen radical pathophysiology, Life Sci, doi:10.1016/S0024-3205(97)00030-1
Reppert, Chez, Anderson, Maternalfetal transfer of melatonin in the non-human primate, Pediatr Res, doi:10.1203/00006450-197906000-00015
Rodhain, Chauves-souris et virus: des relations complexes, Bull Soc Pathol Exot, doi:10.1007/s13149-015-0448-z
Rodriguez, Marchena, Nogales, Correlation between the circadian rhythm of melatonin, phagocytosis, and superoxide anion levels in ring dove heterophils, J Pineal Res, doi:10.1111/j.1600-079X.1999.tb00564.x
Said, Al-Abri, Saidi, Sleep deprivation alters neutrophil functions and levels of Th1-related chemokines and CD4 T cells in the blood, Sleep Breath, doi:10.1007/s11325-019-01851-1
Scheer, Montfrans, Someren, Daily nighttime melatonin reduces blood pressure in male patients with essential hypertension
Scholtens, Munster, Kempen, Physiological melatonin levels in healthy older people: A systematic review, J Psychosomatic Res, doi:10.1016/j.jpsychores.2016.05.005
Shao, Lan, Duan, Upregulation of mitochondrial gene expression in PBMC from convalescent SARS Patients, J Clin Immunol, doi:10.1007/s10875-006-9046-y
Shearer, Reuben, Mullington, Soluble TNF-a receptor 1 and IL-6 plasma levels in humans subjected to the sleep deprivation model of spaceflight, J Allergy Clin Immunol, doi:10.1067/mai.2001.112270
Shi, Gao, Shao, Pyroptosis: gasdermin-mediated programmed necrotic cell death, Trends Biochem Sci, doi:10.1016/j.tibs.2016.10.004
Shi, Nabar, Huang, SARS-Coronavirus Open Reading Frame-8b triggers intracellular stress pathways and activates NLRP3 inflammasomes, Cell Death Discov, doi:10.1038/s41420-019-0181-7
Shneider, Mental inertia in the biological sciences, Trends Biochem Sci, doi:10.1016/j.tibs.2009.12.004
Silman, Melatonin: a contraceptive for the nineties, Eur J Obstetr Gynecol Reproductive Biol, doi:10.1016/0028-2243(93)90099-X
Spiegel, Effect of sleep deprivation on response to immunizaton, JAMA, doi:10.1001/jama.288.12.1471-a
Srinivasan, Maestroni, Cardinali, Melatonin, immune function and aging, Immun Ageing, doi:10.1186/1742-4933-2-17
Srinivasan, Spence, Moscovitch, Malaria: therapeutic implications of melatonin, J Pineal Res, doi:10.1111/j.1600-079X.2009.00728.x
Su, Wan, Song, Oxidative stress and renal fibrosis: mechanisms and therapies, Adv Exper Med Biol, doi:10.1007/978-981-13-8871-2_29
Tan, Kheirandish-Gozal, Sleep, Sleep disorders, and immune function, Allergy Sleep, doi:10.1007/978-3-030-14738-9_1
Tan, Manchester, Terron, One molecule, many derivatives: A never-ending interaction of melatonin with reactive oxygen and nitrogen species, J Pineal Res, doi:10.1111/j.1600-079X.2006.00407.x
Teixeira, Santos, Medeiros, Night workers have lower levels of antioxidant defenses and higher levels of oxidative stress damage when compared to day workers, Sci Rep, doi:10.1038/s41598-019-40989-6
Touitou, Reinberg, Touitou, Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption, Life Sci, doi:10.1016/j.lfs.2017.02.008
Venkataraman, Coleman, Frieman, Overactive epidermal growth factor receptor signaling leads to increased fibrosis after severe acute respiratory syndrome coronavirus infection, J Virol, doi:10.1128/JVI.00182-17
Vijay, Hua, Meyerholz, Critical role of phospholipase A2 group IID in age-related susceptibility to severe acute respiratory syndrome-CoV infection, J Exper Med, doi:10.1084/jem.20150632
Waldhauser, Weiszenbacher, Tatzer, Alterations in nocturnal serum melatonin levels in humans with growth and aging, J Clin Endocrinol Metabol, doi:10.1210/jcem-66-3-648
Wang, Bian, Zhang, Melatonin alleviates cigarette smoke-induced endothelial cell pyroptosis through inhibiting ROS/NLRP3 axis, Biochem Biophys Res Commun, doi:10.1016/j.bbrc.2019.09.005
Wang, Shi, Zhang, Review of bats and SARS, Emerg Infect Dis, doi:10.3201/eid1212.060401
Wei, Smits, Tang, Efficacy and safety of melatonin for sleep onset insomnia in children and adolescents: a meta-analysis of randomized controlled trials, Sleep Medicine, doi:10.1016/j.sleep.2019.02.017
Wichmann, Zellweger, Demaso, Melatonin administration attenuates depressed immune functions after trauma-hemorrhage, J Surg Res, doi:10.1006/jsre.1996.0257
Wong, Li, Lau, Global epidemiology of bat coronaviruses, Viruses, doi:10.3390/v11020174
Woo, Lau, Lam, Discovery of seven novel mammalian and avian coronaviruses in the genus Deltacoronavirus supports bat coronaviruses as the gene source of Alphacoronavirus and Betacoronavirus and avian coronaviruses as the gene source of Gammacoronavirus and Deltacoronavirus, J Virol, doi:10.1128/JVI.06540-11
Wu, Wang, Wang, Renalase contributes to protection against renal fibrosis via inhibiting oxidative stress in rats, Int Urol Nephrol, doi:10.1007/s11255-018-1820-2
Xu, Shi, Wang, Pathological findings of COVID-19 associated with acute respiratory distress syndrome, Lancet Respiratory Med, doi:10.1016/S2213-2600(20)30076-X
Yang, Cell pyroptosis, a potential pathogenic mechanism of 2019-nCoV infection, doi:10.2139/ssrn.3527420
Yao, Ye, Zhang, In vitro antiviral activity and projection of optimized dosing design of hydroxychloroquine for the treatment of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), Clin Infectious Dis, doi:10.1093/cid/ciaa237
Zahid, Li, Kombe, Pharmacological Inhibitors of the NLRP3 Inflammasome, Front Immunol, doi:10.3389/fimmu.2019.02538
Zhang, Li, Grailer, Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome, J Pineal Res, doi:10.1111/jpi.12322
Zhang, Liu, Bai, Melatonin prevents endothelial cell pyroptosis via regulation of long noncoding RNA MEG3/miR-223/NLRP3 axis, J Pineal Res, doi:10.1111/jpi.12449
Zhao, Sun, Su, Melatonin protects against lung fibrosis by regulating the Hippo/YAP pathway, IJMS, doi:10.3390/ijms19041118
Zhou, Qin, Lu, Effectiveness of glucocorticoid therapy in patients with severe novel coronavirus pneumonia, Chinese Med J, doi:10.1097/CM9.0000000000000791
Zhou, Yang, Wang, A pneumonia outbreak associated with a new coronavirus of probable bat origin, Nature, doi:10.1038/s41586-020-2012-7
Zisapel, New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation, Br J Pharmacol, doi:10.1111/bph.14116
DOI record:
{
"DOI": "10.1080/08830185.2020.1756284",
"ISSN": [
"0883-0185",
"1563-5244"
],
"URL": "http://dx.doi.org/10.1080/08830185.2020.1756284",
"alternative-id": [
"10.1080/08830185.2020.1756284"
],
"assertion": [
{
"label": "Peer Review Statement",
"name": "peerreview_statement",
"order": 1,
"value": "The publishing and review policy for this title is described in its Aims & Scope."
},
{
"URL": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=iiri20",
"label": "Aim & Scope",
"name": "aims_and_scope_url",
"order": 2,
"value": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=iiri20"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2020-04-02"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Revised",
"name": "revised",
"order": 1,
"value": "2020-04-03"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "2020-04-06"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 3,
"value": "2020-04-29"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-2150-6727",
"affiliation": [
{
"name": "CureLab Oncology, Inc, Dedham, Massachusetts, USA;"
},
{
"name": "Department of Molecular Biology, Ariel University, Ariel, Israel;"
},
{
"name": "Peter the Great St. Petersburg Polytechnic University, St. Petersburg, Russia"
}
],
"authenticated-orcid": false,
"family": "Shneider",
"given": "Alex",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-3918-5618",
"affiliation": [
{
"name": "Biological Faculty, Lomonosov Moscow State University, Moscow, Russia;"
},
{
"name": "Emanuel Institute of Biochemical Phisics, RAS, Moscow, Russia"
}
],
"authenticated-orcid": false,
"family": "Kudriavtsev",
"given": "Aleksandr",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7948-1254",
"affiliation": [
{
"name": "Biological Faculty, Lomonosov Moscow State University, Moscow, Russia;"
}
],
"authenticated-orcid": false,
"family": "Vakhrusheva",
"given": "Anna",
"sequence": "additional"
}
],
"container-title": "International Reviews of Immunology",
"container-title-short": "International Reviews of Immunology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"www.tandfonline.com"
]
},
"created": {
"date-parts": [
[
2020,
4,
29
]
],
"date-time": "2020-04-29T14:56:47Z",
"timestamp": 1588172207000
},
"deposited": {
"date-parts": [
[
2020,
9,
11
]
],
"date-time": "2020-09-11T07:34:15Z",
"timestamp": 1599809655000
},
"indexed": {
"date-parts": [
[
2024,
4,
25
]
],
"date-time": "2024-04-25T13:05:49Z",
"timestamp": 1714050349713
},
"is-referenced-by-count": 114,
"issue": "4",
"issued": {
"date-parts": [
[
2020,
4,
29
]
]
},
"journal-issue": {
"issue": "4",
"published-print": {
"date-parts": [
[
2020,
7,
3
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://www.tandfonline.com/doi/pdf/10.1080/08830185.2020.1756284",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "153-162",
"prefix": "10.1080",
"published": {
"date-parts": [
[
2020,
4,
29
]
]
},
"published-online": {
"date-parts": [
[
2020,
4,
29
]
]
},
"published-print": {
"date-parts": [
[
2020,
7,
3
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1210/jcem-55-1-27",
"doi-asserted-by": "publisher",
"key": "CIT0001"
},
{
"DOI": "10.1210/jcem-66-3-648",
"doi-asserted-by": "publisher",
"key": "CIT0002"
},
{
"DOI": "10.1016/j.jpsychores.2016.05.005",
"doi-asserted-by": "publisher",
"key": "CIT0003"
},
{
"DOI": "10.1161/01.HYP.0000113293.15186.3b",
"doi-asserted-by": "publisher",
"key": "CIT0004"
},
{
"DOI": "10.1111/bph.14116",
"doi-asserted-by": "publisher",
"key": "CIT0005"
},
{
"DOI": "10.1128/MMBR.00004-08",
"doi-asserted-by": "publisher",
"key": "CIT0006"
},
{
"DOI": "10.1128/CMR.00017-06",
"doi-asserted-by": "publisher",
"key": "CIT0007"
},
{
"DOI": "10.3390/v11020174",
"doi-asserted-by": "publisher",
"key": "CIT0008"
},
{
"DOI": "10.3201/eid1212.060401",
"doi-asserted-by": "publisher",
"key": "CIT0009"
},
{
"DOI": "10.1016/j.virol.2007.06.009",
"doi-asserted-by": "publisher",
"key": "CIT0010"
},
{
"DOI": "10.1128/JVI.06540-11",
"doi-asserted-by": "publisher",
"key": "CIT0011"
},
{
"DOI": "10.3389/fimmu.2018.02112",
"doi-asserted-by": "publisher",
"key": "CIT0012"
},
{
"DOI": "10.1128/JVI.01441-19",
"doi-asserted-by": "publisher",
"key": "CIT0013"
},
{
"DOI": "10.1038/s41586-020-2012-7",
"doi-asserted-by": "publisher",
"key": "CIT0014"
},
{
"DOI": "10.1007/s13149-015-0448-z",
"doi-asserted-by": "publisher",
"key": "CIT0015"
},
{
"DOI": "10.1371/journal.ppat.1006698",
"doi-asserted-by": "publisher",
"key": "CIT0016"
},
{
"DOI": "10.3390/v11030210",
"doi-asserted-by": "publisher",
"key": "CIT0017"
},
{
"DOI": "10.1007/BF01245442",
"doi-asserted-by": "publisher",
"key": "CIT0018"
},
{
"DOI": "10.1007/BF00191463",
"doi-asserted-by": "publisher",
"key": "CIT0019"
},
{
"DOI": "10.1111/j.1600-079X.1996.tb00245.x",
"doi-asserted-by": "publisher",
"key": "CIT0020"
},
{
"DOI": "10.1016/j.cbpa.2006.02.041",
"doi-asserted-by": "publisher",
"key": "CIT0021"
},
{
"DOI": "10.3390/v10080392",
"doi-asserted-by": "publisher",
"key": "CIT0022"
},
{
"DOI": "10.1007/s10875-006-9046-y",
"doi-asserted-by": "publisher",
"key": "CIT0023"
},
{
"DOI": "10.1084/jem.20150632",
"doi-asserted-by": "publisher",
"key": "CIT0024"
},
{
"DOI": "10.1016/j.cell.2008.02.043",
"doi-asserted-by": "publisher",
"key": "CIT0025"
},
{
"DOI": "10.1111/j.1600-079X.2006.00407.x",
"doi-asserted-by": "publisher",
"key": "CIT0026"
},
{
"DOI": "10.1203/00006450-197906000-00015",
"doi-asserted-by": "publisher",
"key": "CIT0027"
},
{
"DOI": "10.1562/0031-8655(2004)080<0579:PEOSDA>2.0.CO;2",
"doi-asserted-by": "publisher",
"key": "CIT0028"
},
{
"DOI": "10.1007/s11357-997-0020-2",
"doi-asserted-by": "publisher",
"key": "CIT0029"
},
{
"DOI": "10.1016/S0024-3205(97)00030-1",
"doi-asserted-by": "publisher",
"key": "CIT0030"
},
{
"DOI": "10.1152/physiologyonline.2000.15.5.246",
"doi-asserted-by": "publisher",
"key": "CIT0031"
},
{
"DOI": "10.2139/ssrn.3527420",
"doi-asserted-by": "publisher",
"key": "CIT0032"
},
{
"DOI": "10.1016/S0966-842X(00)01936-3",
"doi-asserted-by": "publisher",
"key": "CIT0033"
},
{
"DOI": "10.1016/S0140-6736(03)13557-X",
"doi-asserted-by": "publisher",
"key": "CIT0034"
},
{
"DOI": "10.1038/s41420-019-0181-7",
"doi-asserted-by": "publisher",
"key": "CIT0035"
},
{
"DOI": "10.1016/j.tibs.2016.10.004",
"doi-asserted-by": "publisher",
"key": "CIT0036"
},
{
"DOI": "10.1111/imr.12534",
"doi-asserted-by": "publisher",
"key": "CIT0037"
},
{
"DOI": "10.3389/fimmu.2019.02538",
"doi-asserted-by": "publisher",
"key": "CIT0038"
},
{
"DOI": "10.1155/2018/9286458",
"doi-asserted-by": "publisher",
"key": "CIT0039"
},
{
"DOI": "10.1111/jpi.12322",
"doi-asserted-by": "publisher",
"key": "CIT0040"
},
{
"DOI": "10.1016/j.bbrc.2019.09.005",
"doi-asserted-by": "publisher",
"key": "CIT0041"
},
{
"DOI": "10.3389/fimmu.2019.01511",
"doi-asserted-by": "publisher",
"key": "CIT0042"
},
{
"DOI": "10.1016/j.bbadis.2019.05.009",
"doi-asserted-by": "publisher",
"key": "CIT0043"
},
{
"DOI": "10.1590/s0102-865020180040000009",
"doi-asserted-by": "publisher",
"key": "CIT0044"
},
{
"DOI": "10.1111/jpi.12449",
"doi-asserted-by": "publisher",
"key": "CIT0045"
},
{
"DOI": "10.1111/jpi.12414",
"doi-asserted-by": "publisher",
"key": "CIT0046"
},
{
"DOI": "10.1159/000216188",
"doi-asserted-by": "publisher",
"key": "CIT0047"
},
{
"DOI": "10.1038/nri1369",
"doi-asserted-by": "publisher",
"key": "CIT0048"
},
{
"DOI": "10.1007/BF00207360",
"doi-asserted-by": "publisher",
"key": "CIT0049"
},
{
"DOI": "10.1081/CBI-100001174",
"doi-asserted-by": "publisher",
"key": "CIT0050"
},
{
"DOI": "10.1111/j.1600-079X.1999.tb00560.x",
"doi-asserted-by": "publisher",
"key": "CIT0051"
},
{
"DOI": "10.1111/j.1600-079X.1999.tb00564.x",
"doi-asserted-by": "publisher",
"key": "CIT0052"
},
{
"DOI": "10.1111/j.1749-6632.2009.05300.x",
"doi-asserted-by": "publisher",
"key": "CIT0053"
},
{
"DOI": "10.1097/00001756-199601310-00037",
"doi-asserted-by": "publisher",
"key": "CIT0054"
},
{
"DOI": "10.1067/mai.2001.112270",
"doi-asserted-by": "publisher",
"key": "CIT0055"
},
{
"DOI": "10.1007/978-3-030-14738-9_1",
"doi-asserted-by": "publisher",
"key": "CIT0056"
},
{
"DOI": "10.1016/j.lfs.2017.02.008",
"doi-asserted-by": "publisher",
"key": "CIT0057"
},
{
"DOI": "10.1097/00006842-197906000-00001",
"doi-asserted-by": "publisher",
"key": "CIT0058"
},
{
"DOI": "10.1016/0022-3999(76)90020-9",
"doi-asserted-by": "publisher",
"key": "CIT0059"
},
{
"DOI": "10.1007/s11325-019-01851-1",
"doi-asserted-by": "publisher",
"key": "CIT0060"
},
{
"DOI": "10.1001/jama.288.12.1471-a",
"doi-asserted-by": "publisher",
"key": "CIT0061"
},
{
"DOI": "10.1097/01.psy.0000091382.61178.f1",
"doi-asserted-by": "publisher",
"key": "CIT0062"
},
{
"DOI": "10.1152/ajpregu.1993.265.5.R1148",
"doi-asserted-by": "publisher",
"key": "CIT0063"
},
{
"DOI": "10.1038/s41598-019-40989-6",
"doi-asserted-by": "publisher",
"key": "CIT0064"
},
{
"DOI": "10.1097/00001756-200208070-00007",
"doi-asserted-by": "publisher",
"key": "CIT0065"
},
{
"DOI": "10.1111/j.1600-079X.1995.tb00179.x",
"doi-asserted-by": "publisher",
"key": "CIT0066"
},
{
"DOI": "10.1111/j.1600-079X.1991.tb00456.x",
"doi-asserted-by": "publisher",
"key": "CIT0067"
},
{
"DOI": "10.3346/jkms.2020.35.e79",
"doi-asserted-by": "publisher",
"key": "CIT0068"
},
{
"DOI": "10.1016/j.lfs.2020.117477",
"doi-asserted-by": "publisher",
"key": "CIT0069"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105933",
"doi-asserted-by": "publisher",
"key": "CIT0070"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105932",
"doi-asserted-by": "publisher",
"key": "CIT0071"
},
{
"DOI": "10.1016/j.ijantimicag.2020.105949",
"doi-asserted-by": "publisher",
"key": "CIT0072"
},
{
"DOI": "10.1097/CM9.0000000000000791",
"doi-asserted-by": "publisher",
"key": "CIT0073"
},
{
"DOI": "10.1056/nejmoa2001282",
"doi-asserted-by": "publisher",
"key": "CIT0074"
},
{
"DOI": "10.15171/npj.2020.06",
"doi-asserted-by": "publisher",
"key": "CIT0075"
},
{
"DOI": "10.1016/j.jff.2019.04.062",
"doi-asserted-by": "publisher",
"key": "CIT0076"
},
{
"author": "Han Z",
"journal-title": "China Pharmacy",
"key": "CIT0077",
"year": "2007"
},
{
"DOI": "10.1093/cid/ciaa237",
"doi-asserted-by": "publisher",
"key": "CIT0078"
},
{
"DOI": "10.1101/2020.03.24.20042366",
"doi-asserted-by": "publisher",
"key": "CIT0079"
},
{
"DOI": "10.1111/j.1600-079X.2009.00728.x",
"doi-asserted-by": "publisher",
"key": "CIT0080"
},
{
"DOI": "10.1001/archophthalmol.2010.321",
"doi-asserted-by": "publisher",
"key": "CIT0081"
},
{
"DOI": "10.3171/spi.2000.93.1.0077",
"doi-asserted-by": "publisher",
"key": "CIT0082"
},
{
"DOI": "10.1007/s00586-003-0550-y",
"doi-asserted-by": "publisher",
"key": "CIT0083"
},
{
"key": "CIT0084",
"unstructured": "National Institute of Allergy and Infectious Diseases (NIAID). Safety and immunogenicity study of 2019-nCoV vaccine (mRNA-1273) for prophylaxis SARS CoV-2 infection. https://clinicaltrials.gov/ct2/show/study/NCT04283461. NLM identifier: NCT04283461."
},
{
"DOI": "10.1016/j.vaccine.2005.08.105",
"doi-asserted-by": "publisher",
"key": "CIT0085"
},
{
"DOI": "10.1016/j.it.2009.05.002",
"doi-asserted-by": "publisher",
"key": "CIT0086"
},
{
"DOI": "10.1186/1742-4933-2-17",
"doi-asserted-by": "publisher",
"key": "CIT0087"
},
{
"author": "Carrillo-Vico A",
"first-page": "423",
"issue": "5",
"journal-title": "Curr Opin Investig Drugs",
"key": "CIT0088",
"volume": "7",
"year": "2006"
},
{
"author": "Maestroni GJ",
"first-page": "465",
"issue": "3",
"journal-title": "Immunology",
"key": "CIT0089",
"volume": "63",
"year": "1988"
},
{
"DOI": "10.1007/BF01309858",
"doi-asserted-by": "publisher",
"key": "CIT0090"
},
{
"DOI": "10.1006/jsre.1996.0257",
"doi-asserted-by": "publisher",
"key": "CIT0091"
},
{
"DOI": "10.1155/2015/678164",
"doi-asserted-by": "publisher",
"key": "CIT0092"
},
{
"DOI": "10.2174/1568026616666160824120338",
"doi-asserted-by": "publisher",
"key": "CIT0093"
},
{
"DOI": "10.1128/JVI.00182-17",
"doi-asserted-by": "publisher",
"key": "CIT0094"
},
{
"DOI": "10.1097/00075198-200502000-00013",
"doi-asserted-by": "publisher",
"key": "CIT0095"
},
{
"DOI": "10.1097/ccm.0b013e31822f09d7",
"doi-asserted-by": "publisher",
"key": "CIT0096"
},
{
"DOI": "10.1007/978-981-13-8871-2_29",
"doi-asserted-by": "publisher",
"key": "CIT0097"
},
{
"DOI": "10.1007/s11255-018-1820-2",
"doi-asserted-by": "publisher",
"key": "CIT0098"
},
{
"DOI": "10.3390/ijms19041118",
"doi-asserted-by": "publisher",
"key": "CIT0099"
},
{
"DOI": "10.1016/S2213-2600(20)30076-X",
"doi-asserted-by": "publisher",
"key": "CIT0100"
},
{
"DOI": "10.1164/rccm.201904-0849OC",
"doi-asserted-by": "publisher",
"key": "CIT0101"
},
{
"DOI": "10.1152/ajplung.00044.2003",
"doi-asserted-by": "publisher",
"key": "CIT0102"
},
{
"DOI": "10.1093/bja/aef169",
"doi-asserted-by": "publisher",
"key": "CIT0103"
},
{
"DOI": "10.1155/2010/829351",
"doi-asserted-by": "publisher",
"key": "CIT0104"
},
{
"author": "Malhotra S",
"first-page": "46",
"issue": "2",
"journal-title": "MedGenMed",
"key": "CIT0105",
"volume": "6",
"year": "2004"
},
{
"DOI": "10.1210/jcem-45-4-768",
"doi-asserted-by": "publisher",
"key": "CIT0106"
},
{
"DOI": "10.1001/jama.1972.03200140072031",
"doi-asserted-by": "publisher",
"key": "CIT0107"
},
{
"DOI": "10.1016/0028-2243(93)90099-X",
"doi-asserted-by": "publisher",
"key": "CIT0108"
},
{
"DOI": "10.1016/j.sleep.2019.02.017",
"doi-asserted-by": "publisher",
"key": "CIT0109"
},
{
"DOI": "10.1016/j.tibs.2009.12.004",
"doi-asserted-by": "publisher",
"key": "CIT0110"
}
],
"reference-count": 110,
"references-count": 110,
"relation": {
"has-preprint": [
{
"asserted-by": "object",
"id": "10.20944/preprints202004.0122.v2",
"id-type": "doi"
},
{
"asserted-by": "object",
"id": "10.20944/preprints202004.0122.v1",
"id-type": "doi"
}
]
},
"resource": {
"primary": {
"URL": "https://www.tandfonline.com/doi/full/10.1080/08830185.2020.1756284"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Can melatonin reduce the severity of COVID-19 pandemic?",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1080/tandf_crossmark_01",
"volume": "39"
}