Melatonin: a ferroptosis inhibitor with potential therapeutic efficacy for the post-COVID-19 trajectory of accelerated brain aging and neurodegeneration
et al., Molecular Neurodegeneration, doi:10.1186/s13024-024-00728-6, Apr 2024
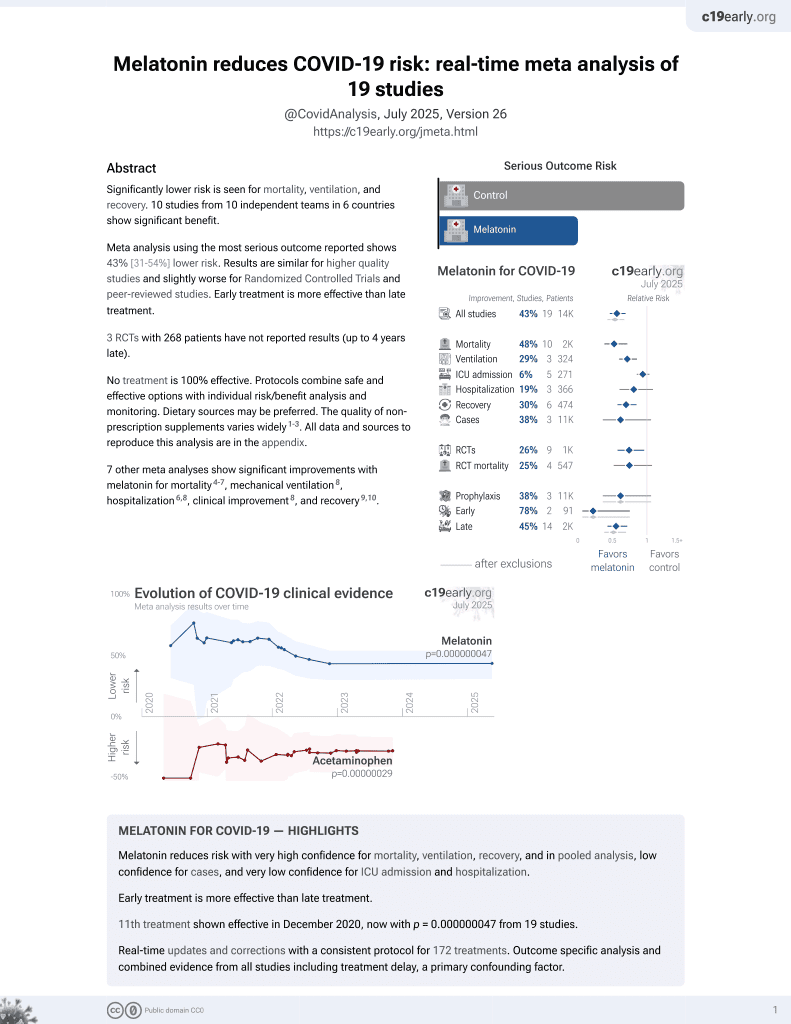
Melatonin for COVID-19
12th treatment shown to reduce risk in
December 2020, now with p = 0.0000000099 from 19 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Review of melatonin as a potential ferroptosis inhibitor for the post-COVID-19 trajectory of accelerated brain aging and neurodegeneration. Authors propose that ferroptosis, an iron-dependent cell death triggered by lipid peroxidation, may underlie post-COVID cognitive impairment and neurodegeneration. SARS-CoV-2 infection induces neuroinflammation, iron dysregulation, oxidative stress, antioxidant system repression, renin-angiotensin system disruption, and clock gene alteration, which can all promote ferroptosis. Melatonin is suggested as a potential treatment due to its anti-inflammatory, antioxidant, iron chelating, and clock gene regulating properties that could inhibit the events leading to ferroptosis. Authors outline the detailed mechanisms by which melatonin may counter ferroptosis in the post-COVID-19 context.
1.
Chen et al., Viral mitochondriopathy in COVID-19, Redox Biology, doi:10.1016/j.redox.2025.103766.
2.
Sanduzzi Zamparelli et al., Immune-Boosting and Antiviral Effects of Antioxidants in COVID-19 Pneumonia: A Therapeutic Perspective, Life, doi:10.3390/life15010113.
3.
Xie et al., The role of reactive oxygen species in severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) infection-induced cell death, Cellular & Molecular Biology Letters, doi:10.1186/s11658-024-00659-6.
4.
Zhao et al., Melatonin Potentially Acts as a Widely-Acting Protective Tool in COVID-19, Medicine Research, doi:10.21127/yaoyimr20240006.
5.
Yehia et al., Melatonin: a ferroptosis inhibitor with potential therapeutic efficacy for the post-COVID-19 trajectory of accelerated brain aging and neurodegeneration, Molecular Neurodegeneration, doi:10.1186/s13024-024-00728-6.
6.
Chacin-Bonilla et al., Melatonin and viral infections: A review focusing on therapeutic effects and SARS-CoV-2, Melatonin Research, doi:10.32794/mr112500168.
7.
Lempesis et al., A mid‑pandemic night's dream: Melatonin, from harbinger of anti‑inflammation to mitochondrial savior in acute and long COVID‑19 (Review), International Journal of Molecular Medicine, doi:10.3892/ijmm.2024.5352.
8.
Alomari et al., Assessing the antiviral potential of melatonin: A comprehensive systematic review, Reviews in Medical Virology, doi:10.1002/rmv.2499.
9.
Donzelli, A., Neglected Effective Early Therapies against COVID-19: Focus on Functional Foods and Related Active Substances. A Review, MDPI AG, doi:10.20944/preprints202312.1178.v1.
10.
Langen, M., Melatonin - the Hormone of Both Sun and Darkness - Protects Your Health and Can Save Your Life, Rounding The Earth, roundingtheearth.substack.com/p/melatonin-the-hormone-of-both-sun.
11.
Hosseinzadeh et al., Melatonin effect on platelets and coagulation: Implications for a prophylactic indication in COVID-19, Life Sciences, doi:10.1016/j.lfs.2022.120866.
12.
Loh et al., Melatonin: Regulation of Viral Phase Separation and Epitranscriptomics in Post-Acute Sequelae of COVID-19, International Journal of Molecular Sciences, doi:10.3390/ijms23158122.
13.
Reiter et al., Melatonin: highlighting its use as a potential treatment for SARS-CoV-2 infection, Cellular and Molecular Life Sciences, doi:10.1007/s00018-021-04102-3.
14.
Tan et al., Mechanisms and clinical evidence to support melatonin's use in severe COVID-19 patients to lower mortality, Life Sciences, doi:10.1016/j.lfs.2022.120368.
15.
Behl et al., CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target, Science of The Total Environment, doi:10.1016/j.scitotenv.2021.152072.
16.
Castle et al., Implications for Systemic Approaches to COVID-19: Effect Sizes of Remdesivir, Tocilizumab, Melatonin, Vitamin D3, and Meditation, Journal of Inflammation Research, doi:10.2147/JIR.S323356.
17.
Ramos et al., The Coronavirus Disease 2019 (COVID-19): Key Emphasis on Melatonin Safety and Therapeutic Efficacy, Antioxidants, doi:10.3390/antiox10071152.
18.
Camp et al., Melatonin interferes with COVID-19 at several distinct ROS-related steps, Journal of Inorganic Biochemistry, doi:10.1016/j.jinorgbio.2021.111546.
19.
Cross et al., Melatonin for the Early Treatment of COVID-19: A Narrative Review of Current Evidence and Possible Efficacy, Endocrine Practice, doi:10.1016/j.eprac.2021.06.001.
20.
DiNicolantonio et al., Melatonin may decrease risk for and aid treatment of COVID-19 and other RNA viral infections, Open Heart, doi:10.1136/openhrt-2020-001568.
21.
Reiter (B) et al., Therapeutic Algorithm for Use of Melatonin in Patients With COVID-19, Frontiers in Medicine, doi:10.3389/fmed.2020.00226.
22.
Charaa et al., Prophylactic Treatment Protocol against the Severity of COVID-19 Using Melatonin, SSRN, doi:10.2139/ssrn.3601861.
Yehia et al., 19 Apr 2024, peer-reviewed, 2 authors.
Contact: abulseoud.osama@mayo.edu.
Melatonin: a ferroptosis inhibitor with potential therapeutic efficacy for the post-COVID-19 trajectory of accelerated brain aging and neurodegeneration
Molecular Neurodegeneration, doi:10.1186/s13024-024-00728-6
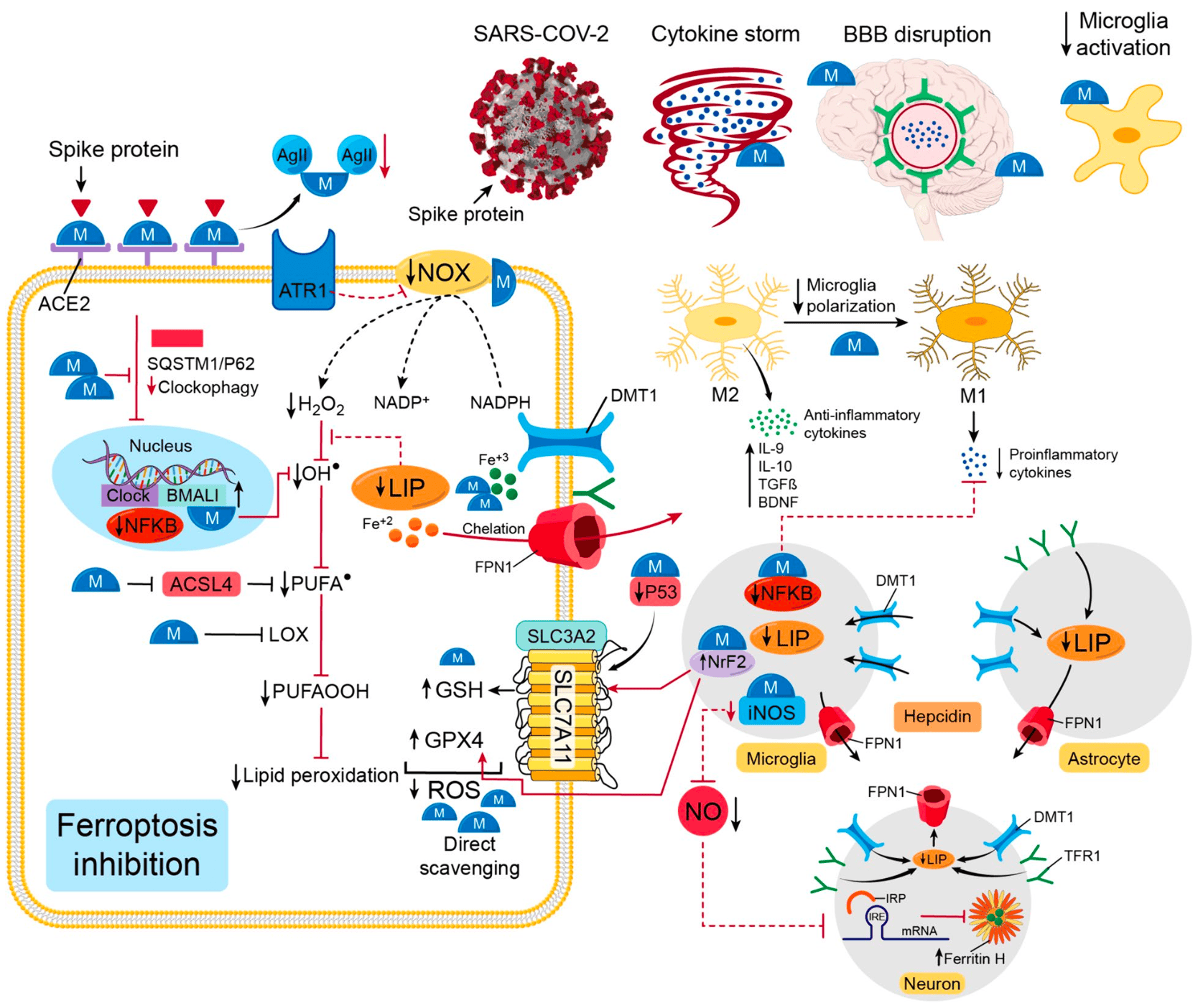
The unprecedented pandemic of COVID-19 swept millions of lives in a short period, yet its menace continues among its survivors in the form of post-COVID syndrome. An exponentially growing number of COVID-19 survivors suffer from cognitive impairment, with compelling evidence of a trajectory of accelerated aging and neurodegeneration. The novel and enigmatic nature of this yet-to-unfold pathology demands extensive research seeking answers for both the molecular underpinnings and potential therapeutic targets. Ferroptosis, an iron-dependent cell death, is a strongly proposed underlying mechanism in post-COVID-19 aging and neurodegeneration discourse. COVID-19 incites neuroinflammation, iron dysregulation, reactive oxygen species (ROS) accumulation, antioxidant system repression, renin-angiotensin system (RAS) disruption, and clock gene alteration. These events pave the way for ferroptosis, which shows its signature in COVID-19, premature aging, and neurodegenerative disorders. In the search for a treatment, melatonin shines as a promising ferroptosis inhibitor with its repeatedly reported safety and tolerability. According to various studies, melatonin has proven efficacy in attenuating the severity of certain COVID-19 manifestations, validating its reputation as an anti-viral compound. Melatonin has well-documented anti-aging properties and combating neurodegenerative-related pathologies. Melatonin can block the leading events of ferroptosis since it is an efficient anti-inflammatory, iron chelator, antioxidant, angiotensin II antagonist, and clock gene regulator. Therefore, we propose ferroptosis as the culprit behind the post-COVID-19 trajectory of aging and neurodegeneration and melatonin, a well-fitting ferroptosis inhibitor, as a potential treatment.
Yehia and Abulseoud Molecular Neurodegeneration (2024) 19:36 against the ferroptosis-induced post-COVID-19 aging and neurodegeneration. Authors' contributions AY wrote the first draft under the supervision of OAA. Both authors read and approved the final manuscript.
Declarations Consent for publication This manuscript does not contain data from any individual person so the consent for publication is not applicable.
Ethics approval and consent to participate Not applicable. Ethics approval and consent are not indicated due to the review nature of this paper.
Competing interests The authors declare that they have no competing interests.
Publisher's Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Abbaspour, Hurrell, Kelishadi, Review on iron and its importance for human health, J Res Med Sci
Abdel-Gawad, Post-COVID-19 Syndrome Clinical Manifestations: A Systematic Review, Antiinflamm Antiallergy Agents Med Chem
Abulseoud, Attenuated initial serum ferritin concentration in critically ill coronavirus disease 2019 geriatric patients with comorbid psychiatric conditions, Front Psychiatry
Acufla-Castroviejo, Minireview: Cell protective role of melatonin in the brain, J Pineal Res
Acuña-Castroviejo, Extrapineal melatonin: sources, regulation, and potential functions, Cell Mol Life Sci
Agmon, Modeling the effects of lipid peroxidation during ferroptosis on membrane properties, Sci Rep
Aguado, Senolytic therapy alleviates physiological human brain aging and COVID-19 neuropathology, bioRxiv
Ahmadi, Ashrafizadeh, Melatonin as a potential modulator of Nrf2, Fundam Clin Pharmacol
Alagiakrishnan, Melatonin based therapies for delirium and dementia, Discov Med
Ali, Melatonin attenuates D-galactose-induced memory impairment, neuroinflammation and neurodegeneration via RAGE/ NF-KB/JNK signaling pathway in aging mouse model, J Pineal Res
Ali, Premature aging of the hippocampal neurogenic niche in adult Bmal1-deficient mice, Front Pharmacol
Ameri, Efficacy and safety of oral melatonin in patients with severe COVID-19: a randomized controlled trial, Inflammopharmacology
Amidfar, Garcez, Kim, Kondratov, The shared molecular mechanisms underlying aging of the brain, major depressive disorder, and Alzheimer's disease: The role of circadian rhythm disturbances, Prog Neuropsychopharmacol Biol Psychiatry
Anderson, Frazer, Current understanding of iron homeostasis, Am J Clin Nutr
Angeli, Conrad, Selenium and GPX4, a vital symbiosis, Free Radical Biol Med
Anjana, Manifestations and risk factors of post COVID syndrome among COVID-19 patients presented with minimal symptoms -A study from Kerala, India, J Family Med Prim Care
Antolıń, Protective effect of melatonin in a chronic experimental model of Parkinson' s disease, Brain research
Aoyama, Glutathione in the Brain, Int J Mol Sci
Arangino, Effects of melatonin on vascular reactivity, catecholamine levels, and blood pressure in healthy men, Am J Cardiol
Arendt, Brainard, Action spectrum for melatonin regulation in humans: evidence for a novel circadian photoreceptor, J Neurosci
Arendt, Molecular dissection of two distinct actions of melatonin on the suprachiasmatic circadian clock
Ariza, COVID-19 severity is related to poor executive function in people with post-COVID conditions, J Neurol
Ashy, Shroff, Ashy, Evaluation of the potential drug interaction of melatonin and warfarin: a case series, Life Sci J
Axelrod, The Pineal Gland: a neurochemical transducer: chemical signals from nerves regulate synthesis of melatonin and convey information about internal clocks, Science
Axelrod, Wurtman, Photic and Neural Control of Indoleamine Metabolism in the Rat Pineal Gland
Ayton, Brain iron is associated with accelerated cognitive decline in people with Alzheimer pathology, Mol Psychiatry
Bakhtazad, Paying attention to circadian rhythms in the treatment of COVID-19, Basic Clin Neurosci J
Bald, Nance, Schultz, Melatonin may slow disease progression in amyotrophic lateral sclerosis: findings from the Pooled Resource Open-Access ALS Clinic Trials database, Muscle Nerve
Bao, Loss of ferroportin induces memory impairment by promoting ferroptosis in Alzheimer's disease, Cell Death Differ
Bao, Targeting miR-124/Ferroportin signaling ameliorated neuronal cell death through inhibiting apoptosis and Yehia and Abulseoud Molecular Neurodegeneration (2024) 19:36 ferroptosis in aged intracerebral hemorrhage murine model, Aging Cell
Basso, Protective effect of the inhibition of the renin-angiotensin system on aging, Regul Pept
Bayr, Reactive oxygen species, Crit Care Med
Becker-André, Pineal gland hormone melatonin binds and activates an orphan of the nuclear receptor superfamily, J Biol Chem
Beker, Interaction of melatonin and Bmal1 in the regulation of PI3K/AKT pathway components and cellular survival, Sci Rep
Benicky, Anti-Inflammatory Effects of Angiotensin Receptor Blockers in the Brain and the Periphery, Cell Mol Neurobiol
Berson, Dunn, Takao, Phototransduction by retinal ganglion cells that set the circadian clock, Science
Besag, Vasey, Adverse events in long-term studies of exogenous melatonin, Expert Opin Drug Saf
Bindoni, Rizzo, Effects of electrolytic lesions of the pineal gland on the electric activity of some brain structures in the rabbit, Bollettino Della Societa Italiana di Biologia Sperimentale
Bitto, p62/SQSTM1 at the interface of aging, autophagy, and disease, Age
Boga, Beneficial actions of melatonin in the management of viral infections: a new use for this "molecular handyman, Rev Med Virol
Bonilla, Melatonin and viral infections, J Pineal Res
Bonilla, Melatonin protects mice infected with Venezuelan equine encephalomyelitis virus, Cell Mol Life Sci CMLS
Borrmann, Mckeating, Zhuang, The circadian clock and viral infections, J Biol Rhythms
Boutin, Quinone reductase 2 as a promising target of melatonin therapeutic actions, Expert Opin Ther Targets
Brown, The effect of the COVID-19 pandemic on people with Parkinson's disease, J Parkinsons Dis
Brugger, Marktl, Herold, Impaired nocturnal secretion of melatonin in coronary heart disease, Lancet
Brzezinski, Melatonin in humans, N Engl J Med
Cabantchik, Labile iron in cells and body fluids: physiology, pathology, and pharmacology, Front Pharmacol
Cagnacci, Elliott, Yen, Arendt, Melatonin and the pineal gland: influence on mammalian seasonal and circadian physiology, J Clin Endocrinol Metab
Cameron, Landreth, Inflammation, microglia, and Alzheimer's disease, Neurobiol Dis
Campos, The angiotensin-melatonin axis, Int J Hypertens
Cao, Accelerated biological aging in COVID-19 patients, Nat Commun
Caroleo, Doria, Nistico, Melatonin restores immunodepression in aged and cyclophosphamide-treated mice, Ann N Y Acad Sci
Catalá, Five decades with polyunsaturated fatty acids: chemical synthesis, enzymatic formation, lipid peroxidation and its biological effects, J Lipids
Cecchini, Cecchini, Lovell, Decreased thioredoxin and increased thioredoxin reductase levels in Alzheimer's disease brain, Free Radical Biol Med
Cecon, Oishi, Jockers, Melatonin receptors: molecular pharmacology and signalling in the context of system bias, Br J Pharmacol
Cecon, Therapeutic potential of melatonin and melatonergic drugs on K18-hACE2 mice infected with SARS-CoV-2, J Pineal Res
Checa, Aran, Reactive oxygen species: drivers of physiological and pathological processes, J Inflamm Res
Chen, Cellular degradation systems in ferroptosis, Cell Death Differ
Chen, Characteristics and biomarkers of ferroptosis, Front Cell Dev Biol
Chen, Enhanced defense against ferroptosis ameliorates cognitive impairment and reduces neurodegeneration in 5xFAD mice, Free Radical Biol Med
Chen, Ferritin reduction is essential for cerebral ischemiainduced hippocampal neuronal death through p53/SLC7A11-mediated ferroptosis, Brain Res
Cheng, Li, What is responsible for the initiating chemistry of ironmediated lipid peroxidation: an update, Chem Rev
Cheng, TrkB agonist N-acetyl serotonin promotes functional recovery after traumatic brain injury by suppressing ferroptosis via the PI3K/Akt/Nrf2/Ferritin H pathway, Free Radical Biol Med
Chiang, Relationships among cortical glutathione levels, brain amyloidosis, and memory in healthy older adults investigated in vivo with 1H-MRS and Pittsburgh compound-B PET, Am J Neuroradiol
Cho, Regulation of circadian behaviour and metabolism by REV-ERB-α and REV-ERB-β, Nature
Chung, Association of Alzheimer's disease with COVID-19 susceptibility and severe complications: a nationwide cohort study, J Alzheimer's Dis
Cipolla-Neto, Amaral, Lph, Melatonin as a hormone: new physiological and clinical insights, Clin Drug Investig
Claise, Low transferrin levels predict heightened inflammation in patients with COVID-19: New insights, Int J Infect Dis
Claustrat, Brun, Chazot, The basic physiology and pathophysiology of melatonin, Sleep Med Rev
Costa, Lopes, Lamy-Freund, Permeability of pure lipid bilayers to melatonin, J Pineal Res
Cozzi, Stem cell modeling of neuroferritinopathy reveals iron as a determinant of senescence and ferroptosis during neuronal aging, Stem Cell Reports
Crivelli, Changes in cognitive functioning after COVID-19: a systematic review and meta-analysis, Alzheimers Dement
Cui, ACSL4 exacerbates ischemic stroke by promoting ferroptosis-induced brain injury and neuroinflammation, Brain Behav Immun
Dang, Activation of angiotensin-converting enzyme 2/angiotensin (1-7)/mas receptor axis triggers autophagy and suppresses microglia proinflammatory polarization via forkhead box class O1 signaling, Aging Cell
Darban, Efficacy of high dose vitamin C, melatonin and zinc in Iranian patients with acute respiratory syndrome due to coronavirus infection: a pilot randomized trial, J Cell Mol Anesth
Del Quilesrey, Mancias, NCOA4-mediated ferritinophagy: a potential link to neurodegeneration, Front Neurosci
Delgado-Alonso, Cognitive dysfunction associated with COVID-19: a comprehensive neuropsychological study, J Psychiatr Res
Delgado-Lara, Effect of melatonin administration on the PER1 and BMAL1 clock genes in patients with Parkinson's disease, Biomed Pharmacother
Diallo, Daytime variation in SARS-CoV-2 infection and cytokine production, Microb Pathog
Dixon, Ferroptosis: an iron-dependent form of nonapoptotic cell death, Cell
Dixon, Stockwell, The hallmarks of ferroptosis, Ann Rev Cancer Biol
Dodson, Castro-Portuguez, Zhang, NRF2 plays a critical role in mitigating lipid peroxidation and ferroptosis, Redox Biol
Doll, ACSL4 dictates ferroptosis sensitivity by shaping cellular lipid composition, Nat Chem Biol
Dou, Targeting iNOS alleviates early brain injury after experimental subarachnoid hemorrhage via promoting ferroptosis of M1 microglia and reducing neuroinflammation, J Cell Mol Med
Duan, ACE2 activator diminazene aceturate ameliorates Alzheimer's disease-like neuropathology and rescues cognitive impairment in SAMP8 mice, Aging
Duez, Staels, The nuclear receptors Rev-erbs and RORs integrate circadian rhythms and metabolism, Diab Vasc Dis Res
Eroğlu, Eroğlu, Güven, Altered tryptophan absorption and metabolism could underlie long-term symptoms in survivors of coronavirus disease 2019 (COVID-19), Nutrition
Evans, ACE2 activation protects against cognitive decline and reduces amyloid pathology in the Tg2576 mouse model of Alzheimer's disease, Acta Neuropathol
Fan, Melatonin ameliorates the progression of Alzheimer's disease by inducing TFEB nuclear translocation, promoting mitophagy, and regulating NLRP3 inflammasome activity, BioMed Res Int
Fan, The effect of melatonin on early postoperative cognitive decline in elderly patients undergoing hip arthroplasty: a randomized controlled trial, J Clin Anesth
Fang, Inhibiting ferroptosis through disrupting the NCOA4-FTH1 interaction: a new mechanism of action, ACS Cent Sci
Fara, Cytokine storm and COVID-19: a chronicle of pro-inflammatory cytokines, Open Biol
Faridzadeh, Melatonin drugs inhibit SARS-CoV-2 entry into the brain and virus-induced damage of cerebral small vessels, Cell Mol Life Sci
Fariello, Bubenik, Melatonin-induced changes in the sensory activation of acute epileptic foci, Neurosci Lett
Farnoosh, Efficacy of a low dose of melatonin as an adjunctive therapy in hospitalized patients with COVID-19: a randomized, double-blind clinical trial, Arch Med Res
Fedeli, Parkinson's disease related mortality: Long-term trends and impact of COVID-19 pandemic waves, Parkinsonism Relat Disord
Feng, Transferrin receptor is a specific ferroptosis marker, Cell Rep
Feng, Wang, Li, Change of telomere length in angiotensin IIinduced human glomerular mesangial cell senescence and the protective role of losartan, Mol Med Rep
Ferlazzo, Is melatonin the cornucopia of the 21st century?, Antioxidants
Ferrando, Neuropsychological, Medical, and Psychiatric Findings After Recovery From Acute COVID-19: A Cross-sectional Study, J Acad Consult Liaison Psychiatry
Ferrucci, Brain positron emission tomography (PET) and cognitive abnormalities one year after COVID-19, J Neurol
Finch, Plasma ferritin determination as a diagnostic tool, West J Med
Fiske, Bryant, Putnam, Effect of light on the weight of the pineal in the rat, ENDOCRINE SOC 4350 EAST WEST HIGHWAY SUITE
Fj, Post-COVID-19 syndrome: epidemiology, diagnostic criteria and pathogenic mechanisms involved, Rev Neurol
Fogleman, A pilot of a randomized control trial of melatonin and vitamin C for mild-to-moderate COVID-19, J Am Board Fam Med
Forcina, Dixon, GPX4 at the crossroads of lipid homeostasis and ferroptosis, Proteomics
Forman, Zhang, Rinna, Glutathione: overview of its protective roles, measurement, and biosynthesis, Mol Aspects Med
Fowler, Circadian rhythms and melatonin metabolism in patients with disorders of gut-brain interactions, Front Neurosci
Friedman, Why is the nervous system vulnerable to oxidative stress? Oxidative Stress Free Radical Damage, Neurol
Frontera, Comparison of serum neurodegenerative biomarkers among hospitalized COVID-19 patients versus non-COVID subjects with normal cognition, mild cognitive impairment, or Alzheimer's dementia, Alzheimers Dement
Fuqua, Vulpe, Anderson, Intestinal iron absorption, J Trace Elem Med Biol
Furio, Brusco, Cardinali, Possible therapeutic value of melatonin in mild cognitive impairment: a retrospective study, J Pineal Res
Ganz, Hepcidin and iron regulation, 10 years later, Blood
Ganz, Nemeth, Iron homeostasis in host defence and inflammation, Nat Rev Immunol
Gao, Glutaminolysis and transferrin regulate ferroptosis, Mol Cell
Gao, Melatonin ameliorates neurological deficits through MT2/ IL-33/ferritin H signaling-mediated inhibition of neuroinflammation and ferroptosis after traumatic brain injury, Free Radical Biol Med
Garcia-Sanchez, Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 "long haulers, Ann Clin Transl Neurol
Garrido-Gil, Brain angiotensin regulates iron homeostasis in dopaminergic neurons and microglial cells, Exp Neurol
Gaschler, Stockwell, Lipid peroxidation in cell death, Biochem Biophys Res Commun
Geng, Knockdown of ferroportin accelerates erastin-induced ferroptosis in neuroblastoma cells, Eur Rev Med Pharmacol Sci
Gilbert, Thiol/disulfide exchange equilibria and disulfidebond stability, Methods Enzymol
Girotti, Mechanisms of lipid peroxidation, J Free Radic Biol Med
Gou, Melatonin improves hypoxic-ischemic brain damage through the Akt/Nrf2/Gpx4 signaling pathway, Brain Res Bull
Gulcin, Buyukokuroglu, Kufrevioglu, Metal chelating and hydrogen peroxide scavenging effects of melatonin, J Pineal Res
Guohua, Melatonin protects against PM2. 5-induced lung injury by inhibiting ferroptosis of lung epithelial cells in a Nrf2dependent manner, Ecotoxicol Environ Safety
Gupta, Role of iron (Fe) in body, IOSR J Appl Chem
Guéraud, Chemistry and biochemistry of lipid peroxidation products, Free Radical Res
Habib, The role of iron in the pathogenesis of COVID-19 and possible treatment with lactoferrin and other iron chelators, Biomed Pharmacother
Halliwell, Chirico, Lipid peroxidation: its mechanism, measurement, and significance, Am J Clin Nutr
Halliwell, Gutteridge, Oxygen toxicity, oxygen radicals, transition metals and disease, Biochem J
Han, Nrf2 knockout altered brain iron deposition and mitigated age-related motor dysfunction in aging mice, Free Radical Biol Med
Hardeland, Melatonin and Microglia, Int J Mol Sci
Hardeland, Melatonin and brain inflammaging, Prog Neurobiol
Harrison, Arosio, The ferritins: molecular properties, iron storage function and cellular regulation, Biochim Biophys Acta
Harvey, Nrf2-regulated glutathione recycling independent of biosynthesis is critical for cell survival during oxidative stress, Free Radical Biol Med
Hasan, Atrakji, Mehuaiden, The effect of melatonin on thrombosis, sepsis and mortality rate in COVID-19 patients, Int J Infect Dis
Haskologlu, Melatonin and REGN-CoV2 combination as a vaccine adjuvant for Omicron variant of SARS-CoV-2, Mol Biol Rep
Hayter, Bishop, Robinson, Pharmacological but not physiological concentrations of melatonin reduce iron-induced neuronal death in rat cerebral cortex, Neurosci Lett
Heneka, Neuroinflammation in Alzheimer's disease, The Lancet Neurology
Herrera, Cognitive impairment in young adults with post COVID-19 syndrome, Sci Rep
Herxheimer, Petrie, Group, Melatonin for the prevention and treatment of jet lag, Cochrane Database Syst Rev
Hirayama, Sassone-Corsi, Structural and functional features of transcription factors controlling the circadian clock, Curr Opin Genet Dev
Hortová-Kohoutková, Hepcidin and ferritin levels as markers of immune cell activation during septic shock, severe COVID-19 and sterile inflammation, J Trace Elem Med Biol
Hosseinzadeh, Melatonin effect on platelets and coagulation: Implications for a prophylactic indication in COVID-19, Life Sci
Hou, Autophagy promotes ferroptosis by degradation of ferritin, Autophagy
Hu, Melatonin decreases M1 polarization via attenuating mitochondrial oxidative damage depending on UCP2 pathway in prorenintreated microglia, PLoS ONE
Huang, Ferroptosis in a sarcopenia model of senescence accelerated mouse prone 8 (SAMP8), Int J Biol Sci
Huang, Melatonin alleviates acute kidney injury by inhibiting NRF2/Slc7a11 axis-mediated ferroptosis, Oxidative Med Cell Longevity
Idrees, Kumar, SARS-CoV-2 spike protein interactions with amyloidogenic proteins: Potential clues to neurodegeneration, Biochem Biophys Res Commun
Iguchi, Kato, Ibayashi, Age-dependent reduction in serum melatonin concentrations in healthy human subjects, J Clin Endocrinol Metab
Ineichen, Worsened Parkinson's disease progression: impact of the COVID-19 pandemic, J Parkinsons Dis
Jallouli, Effect of melatonin intake on postural balance, functional mobility and fall risk in persons with multiple sclerosis: a pilot study, Int J Neurosci
Jand, Melatonin ameliorates disease severity in a mouse model of multiple sclerosis by modulating the kynurenine pathway, Sci Rep
Jankauskas, COVID-19 causes ferroptosis and oxidative stress in human endothelial cells, Antioxidants
Jennings, A systematic review of persistent symptoms and residual abnormal functioning following acute COVID-19: ongoing symptomatic phase vs. post-COVID-19 syndrome, J Clin Med
Ji, Xu, Melatonin protects podocytes from angiotensin II-induced injury in an in vitro diabetic nephropathy model, Mol Med Rep
Jiang, Ferroptosis as a p53-mediated activity during tumour suppression, Nature
Jilg, Melatonin modulates daytime-dependent synaptic plasticity and learning efficiency, J Pineal Res
Jing, Association between inflammatory cytokines and anti-SARS-CoV-2 antibodies in hospitalized patients with COVID-19, Immunity Ageing
Juan, The Chemistry of Reactive Oxygen Species (ROS) Revisited: Outlining Their Role in Biological Macromolecules (DNA, Lipids and Proteins) and Induced Pathologies, Int J Mol Sci
Jumnongprakhon, Inhibitory effect of melatonin on cerebral endothelial cells dysfunction induced by methamphetamine via NADPH oxidase-2, Brain Res
Kakhaki, Melatonin supplementation and the effects on clinical and metabolic status in Parkinson's disease: A randomized, double-blind, placebo-controlled trial, Clin Neurol Neurosurg
Kapralov, Redox lipid reprogramming commands susceptibility of macrophages and microglia to ferroptotic death, Nat Chem Biol
Kaptanoglu, Different responsiveness of central nervous system tissues to oxidative conditions and to the antioxidant effect of melatonin, J Pineal Res
Katsarou, Pantopoulos, Basics and principles of cellular and systemic iron homeostasis, Mol Aspects Med
Kaushal, Serum ferritin as a predictive biomarker in COVID-19. A systematic review, meta-analysis and meta-regression analysis, J Crit Care
Kawabata, Transferrin and transferrin receptors update, Free Radical Biol Med
Kehoe, Angiotensin-converting enzyme 2 is reduced in Alzheimer's disease in association with increasing amyloid-β and tau pathology, Alzheimer's Res Ther
Kempuraj, COVID-19, mast cells, cytokine storm, psychological stress, and neuroinflammation, Neuroscientist
Keskin-Aktan, SIRT2 and FOXO3a expressions in the cerebral cortex and hippocampus of young and aged male rats: antioxidant and anti-apoptotic effects of melatonin, Biologia Futura
King, Richardson, Reiter, Regulation of rat pineal melatonin synthesis: effect of monoamine oxidase inhibition, Mol Cell Endocrinol
Klein, Moore, Pineal N-acetyltransferase and hydroxyindole-Omethyl-transferase: control by the retinohypothalamic tract and the suprachiasmatic nucleus, Brain Res
Knovich, Ferritin for the clinician, Blood Rev
Kojetin, Burris, REV-ERB and ROR nuclear receptors as drug targets, Nat Rev Drug Discovery
Kondratova, Kondratov, The circadian clock and pathology of the ageing brain, Nat Rev Neurosci
Kong, Melatonin attenuates angiotensin II-induced abdominal aortic aneurysm through the down-regulation of matrix metalloproteinases, Oncotarget
Koppula, Zhuang, Gan, Cystine transporter SLC7A11/xCT in cancer: ferroptosis, nutrient dependency, and cancer therapy, Protein Cell
Krause, Dubocovich, Regulatory sites in the melatonin system of mammals, Trends Neurosci
Kroner, TNF and increased intracellular iron alter macrophage polarization to a detrimental M1 phenotype in the injured spinal cord, Neuron
Kruszewski, Labile iron pool: the main determinant of cellular response to oxidative stress, Mutat Res
Kubben, Repression of the antioxidant NRF2 pathway in premature aging, Cell
Kumar, Mills, Lapierre, Selective autophagy receptor p62/ SQSTM1, a pivotal player in stress and aging, Front Cell Dev Biol
Kumar, Severe glutathione deficiency, oxidative stress and oxidant damage in adults hospitalized with COVID-19: implications for GlyNAC (glycine and N-acetylcysteine) supplementation, Antioxidants
Kuwata, Hara, Role of acyl-CoA synthetase ACSL4 in arachidonic acid metabolism, Prostaglandins Other Lipid Mediat
Kyriakopoulos, Mitogen Activated Protein Kinase (MAPK) Activation, p53, and Autophagy Inhibition Characterize the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Spike Protein Induced Neurotoxicity, Cureus
Kühn, Borchert, Regulation of enzymatic lipid peroxidation: the interplay of peroxidizing and peroxide reducing enzymes1 1This article is part of a series of reviews on "Regulatory and Cytoprotective Aspects of Lipid Hydroperoxide Metabolism. " The full list of papers may be found on the homepage of the journal, Free Rad Biol Med
Labban, Effects of melatonin and resveratrol on recognition memory and passive avoidance performance in a mouse model of Alzheimer's disease, Behav Brain Res
Lara, Macías-Verde, Burgos-Burgos, Age-induced NLRP3 inflammasome over-activation increases lethality of SARS-CoV-2 pneumonia in elderly patients, Aging Dis
Larson, Impaired hippocampal long-term potentiation in melatonin MT2 receptor-deficient mice, Neurosci Lett
Lee, Lipid metabolism and ferroptosis, Biology
Lemoine, Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects, J Sleep Res
Leon, Modification of nitric oxide synthase activity and neuronal response in rat striatum by melatonin and kynurenine derivatives, J Neuroendocrinol
Lerner, Isolation of melatonin, the pineal gland factor that lightens melanocyteS1, J Am Chem Soc
Lesnikov, Pierpaoli, Pineal cross-transplantation (old-to-young and vice versa) as evidence for an endogenous" aging clock, Ann N Y Acad Sci
Lewerenz, The cystine/glutamate antiporter system xc-in health and disease: from molecular mechanisms to novel therapeutic opportunities, Antioxid Redox Signal
Lewy, Melatonin shifts human orcadian rhythms according to a phase-response curve, Chronobiol Int
León, Structure-related inhibition of calmodulin-dependent neuronal nitric-oxide synthase activity by melatonin and synthetic kynurenines, Mol Pharmacol
Li, Alterations in the time course of expression of the Nox family in the brain in a rat experimental cerebral ischemia and reperfusion model: effects of melatonin, J Pineal Res
Li, Exogenous melatonin ameliorates steroid-induced osteonecrosis of the femoral head by modulating ferroptosis through GDF15mediated signaling, Free Radical Biol Med
Li, Ferrostatin-1 alleviates angiotensin II (Ang II)-induced inflammation and ferroptosis in astrocytes, Int Immunopharmacol
Li, Melatonin ameliorates Parkinson's disease via regulating microglia polarization in a RORα-depend4ent pathway, npj Parkinson's Dis
Li, Peripheral clock system abnormalities in patients with Parkinson's disease, Front Aging Neurosci
Li, System Xc-/GSH/GPX4 axis: An important antioxidant system for the ferroptosis in drug-resistant solid tumor therapy, Front Pharmacol
Liang, Minikes, Jiang, Ferroptosis at the intersection of lipid metabolism and cellular signaling, Mol Cell
Liao, CD8+ T cells and fatty acids orchestrate tumor ferroptosis and immunity via ACSL4, Cancer Cell
Limson, Nyokong, Daya, The interaction of melatonin and its precursors with aluminium, cadmium, copper, iron, lead, and zinc: an adsorptive voltammetric study, J Pineal Res
Lin, Chiu, Lane, Trough Melatonin Levels Differ between Early and Late Phases of Alzheimer Disease, Clin Psychopharmacol Neurosci
Lin, Ho, Melatonin suppresses iron-induced neurodegeneration in rat brain, Free Radical Biol Med
Lino, Ferritin in the coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis, Brazilian J Infect Dis
Liu, Angiotensin II-induced vascular endothelial cells ferroptosis via P53-ALOX12 signal axis, Clin Exp Hypertens
Liu, Autophagy-dependent ferroptosis: machinery and regulation, Cell Chem Biol
Liu, BMAL1 regulation of microglia-mediated neuroinflammation in MPTP-induced Parkinson's disease mouse model, FASEB J
Liu, Iron accumulation with age alters metabolic pattern and circadian clock gene expression through the reduction of AMP-modulated histone methylation, J Biol Chem
Liu, Liang, Soong, Nitric oxide, iron and neurodegeneration, Front Neurosci
Liu, Paeonol improves angiotensin II-induced cardiac hypertrophy by suppressing ferroptosis, Heliyon
Liu, Post-infection cognitive impairments in a cohort of elderly patients with COVID-19, Mol Neurodegener
Liu, The role of ferroptosis mediated by NRF2/ERK-regulated ferritinophagy in CdTe QDs-induced inflammation in macrophage, Yehia and Abulseoud Molecular Neurodegeneration
Lu, Glutathione synthesis, Biochim Biophys Acta
Lynch, Role of senescence and aging in SARS-CoV-2 infection and COVID-19 disease, Cells
Ma, Melatonin alleviates early brain injury by inhibiting the NRF2-mediated ferroptosis pathway after subarachnoid hemorrhage, Free Radical Biol Med
Ma, Melatonin suppresses ferroptosis induced by high glucose via activation of the Nrf2/HO-1 signaling pathway in type 2 diabetic osteoporosis, Oxidative Med Cell Longevity
Magri, Changes in endocrine orcadian rhythms as markers of physiological and pathological brain aging, Chronobiol Int
Mahalanobish, Melatonin counteracts necroptosis and pulmonary edema in cadmium-induced chronic lung injury through the inhibition of angiotensin II, J Biochem Mol Toxicol
Maharaj, Melatonin and 6-hydroxymelatonin protect against iron-induced neurotoxicity, J Neurochem
Mandal, System xc-and thioredoxin reductase 1 cooperatively rescue glutathione deficiency, J Biol Chem
Marzouk, Modeling COVID-19 Effects on Sustainable Development Goals in Egypt Using System Dynamics
Matias-Guiu, Development of criteria for cognitive dysfunction in post-COVID syndrome: the IC-CoDi-COVID approach, Psychiatry Res
Mattam, Jagota, Differential role of melatonin in restoration of age-induced alterations in daily rhythms of expression of various clock genes in suprachiasmatic nucleus of male Wistar rats, Biogerontology
Mazhar, Implication of ferroptosis in aging, Cell Death Discovery
Mckie, An iron-regulated ferric reductase associated with the absorption of dietary iron, Science
Meo, Magnetic Resonance Imaging (MRI) and neurological manifestations in SARS-CoV-2 patients, Eur Rev Med Pharmacol Sci
Meyer, SARS-CoV-2 spike protein induces paracrine senescence and leukocyte adhesion in endothelial cells, J Virol
Mezzanotte, Activation of the Hepcidin-Ferroportin1 pathway in the brain and astrocytic-neuronal crosstalk to counteract iron dyshomeostasis during aging, Sci Rep
Mi, Melatonin inhibits ferroptosis and delays age-related cataract by regulating SIRT6/p-Nrf2/GPX4 and SIRT6/NCOA4/FTH1 pathways, Biomed Pharmacother
Min, Signaling mechanisms of angiotensin II in regulating vascular senescence, Ageing Res Rev
Minotti, Aust, The role of iron in oxygen radical mediated lipid peroxidation, Chem Biol Interact
Miyamoto, Singlet molecular oxygen generated by biological hydroperoxides, J Photochem Photobiol, B
Montesinos, Guardia-Laguarta, Gomez, The fat brain, Curr Opin Clin Nutr Metab Care
Moradkhani, Immunoregulatory role of melatonin in cancer, J Cell Physiol
Morgan, Effects of the endogenous clock and sleep time on melatonin, insulin, glucose and lipid metabolism, J Endocrinol
Mu, The role of iron homeostasis in remodeling immune function and regulating inflammatory disease, Science Bulletin
Muckenthaler, Galy, Hentze, Systemic iron homeostasis and the iron-responsive element/iron-regulatory protein (IRE/IRP) regulatory network, Annu Rev Nutr
Muhammad, Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: a cross-sectional comparative study in Jigawa, Northwestern Nigeria, SAGE Open Med
Najafi, Melatonin modulates regulation of NOX2 and NOX4 following irradiation in the lung, Curr Clin Pharmacol
Naskar, Melatonin enhances L-DOPA therapeutic effects, helps to reduce its dose, and protects dopaminergic neurons in 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine-induced Parkinsonism in mice, J Pineal Res
Ni, An impaired intrinsic microglial clock system induces neuroinflammatory alterations in the early stage of amyloid precursor protein knock-in mouse brain, J Neuroinflammation
Nie, Melatonin ameliorates anxiety and depression-like behaviors and modulates proteomic changes in triple transgenic mice of Alzheimer's disease, BioFactors
Nielsen, Serum ferritin iron in iron overload and liver damage: correlation to body iron stores and diagnostic relevance, J Lab Clin Med
Niki, Lipid peroxidation: mechanisms, inhibition, and biological effects, Biochem Biophys Res Commun
Nir, Changes in the electrical activity of the brain following pinealectomy, Neuroendocrinology
Normandin, Intrathecal inflammatory responses in the absence of SARS-CoV-2 nucleic acid in the CSF of COVID-19 hospitalized patients, J Neurol Sci
Nosjean, Identification of the Melatonin-binding SiteMT 3 as the Quinone Reductase 2, J Biol Chem
Nous, Serum daytime melatonin levels reflect cerebrospinal fluid melatonin levels in Alzheimer's disease but are not correlated with cognitive decline, J Alzheimers Dis
O'neal-Moffitt, Prophylactic melatonin significantly reduces Alzheimer's neuropathology and associated cognitive deficits independent of antioxidant pathways in AβPPswe/PS1 mice, Mol Neurodegener
Obayashi, Physiological levels of melatonin relate to cognitive function and depressive symptoms: the HEIJO-KYO cohort, J Clin Endocrinol Metab
Olagnier, SARS-CoV2-mediated suppression of NRF2-signaling reveals potent antiviral and anti-inflammatory activity of 4-octyl-itaconate and dimethyl fumarate, Nat Commun
Oronsky, A review of persistent post-COVID syndrome (PPCS), Clin Rev Allergy Immunol
Ortega-Gutiérrez, Melatonin improves deferoxamine antioxidant activity in protecting against lipid peroxidation caused by hydrogen peroxide in rat brain homogenates, Neurosci Lett
Pamplona, Membrane phospholipids, lipoxidative damage and molecular integrity: a causal role in aging and longevity, Biochim Biophys Acta
Pang, Influence of aging on deterioration of patients with COVID-19, Aging
Papagiannidou, Skene, Ioannides, Potential drug interactions with melatonin, Physiol Behav
Parihar, Outcome of Hospitalized Parkinson's Disease Patients with and without COVID-19, Movement Disorders Clinical Practice
Pasini, Is ferroptosis a key component of the process leading to multiorgan damage in COVID-19?, Antioxidants
Patel, Diabetes mellitus and melatonin: where are we? Biochimie, J Pineal Res
Patiño, Melatonin protects against oxygen and glucose deprivation by decreasing extracellular glutamate and Nox-derived ROS in rat hippocampal slices, Neurotoxicology
Patki, Lau, Melatonin protects against neurobehavioral and mitochondrial deficits in a chronic mouse model of Parkinson's disease, Pharmacol Biochem Behav
Pei, Research progress of glutathione peroxidase family (GPX) in redoxidation, Front Pharmacol
Perez, Dietary lipids induce ferroptosis in caenorhabditiselegans and human cancer cells, Dev Cell
Perrottelli, Cognitive impairment after post-acute COVID-19 infection: a systematic review of the literature, J Pers Med
Pevet, Challet, Melatonin: both master clock output and internal time-giver in the circadian clocks network, Journal of Physiology-Paris
Pevet, The chronobiotic properties of melatonin, Cell Tissue Res
Pierrefiche, Zerbib, Laborit, Anxiolytic activity of melatonin in mice: involvement of benzodiazepine receptors, Res Commun Chem Pathol Pharmacol
Pizzimenti, Interaction of aldehydes derived from lipid peroxidation and membrane proteins, Front Physiol
Poeggeler, Melatonin-a highly potent endogenous radical scavenger and electron donor: new aspects of the oxidation chemistry of this indole in vitro a, Ann N Y Sci
Ponnappan, Ponnappan, Liguori, Aging and immune function: molecular mechanisms to interventions, Clin Interv Aging
Potes, Benefits of the neurogenic potential of melatonin for treating neurological and neuropsychiatric disorders, Int J Mol Sci
Premraj, Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis, J Neurol Sci
Qiao, Hepcidin-induced endocytosis of ferroportin is dependent on ferroportin ubiquitination, Cell Metab
Raghavendra, Kaur, Kulkarni, Anti-depressant action of melatonin in chronic forced swimming-induced behavioral despair in mice, role of peripheral benzodiazepine receptor modulation, Eur Neuropsychopharmacol
Raghavendra, Kulkarni, Reversal of morphine tolerance and dependence by melatonin: possible role of central and peripheral benzodiazepine receptors, Brain Res
Raveendran, Jayadevan, Sashidharan, Long COVID: an overview, Diabetes Metab Syndr
Recalcati, Molecular regulation of cellular iron balance, IUBMB Life
Reiter, Delivery of pineal melatonin to the brain and SCN: role of canaliculi, cerebrospinal fluid, tanycytes and Virchow-Robin perivascular spaces, Brain Struct Funct
Reiter, Melatonin and its relation to the immune system and inflammation, Ann N Y Acad Sci
Reiter, Melatonin as an antioxidant: under promises but over delivers, J Pineal Res
Reiter, Melatonin: reproductive effects
Reiter, Melatonin: the chemical expression of darkness, Mol Cell Endocrinol
Reiter, Tan, Galano, Melatonin: exceeding expectations, Physiology
Ren, Melatonin reduces radiation-induced ferroptosis in hippocampal neurons by activating the PKM2/NRF2/GPX4 signaling pathway, Prog Neuropsychopharmacol Biol Psychiatry
Reppert, Molecular characterization of a second melatonin receptor expressed in human retina and brain: the Mel1b melatonin receptor, Proc Natl Acad Sci
Reppert, Weaver, Ebisawa, Cloning and characterization of a mammalian melatonin receptor that mediates reproductive and circadian responses, Neuron
Rocha, Cerebrospinal fluid levels of angiotensin-converting enzyme are associated with amyloid-β 42 burden in Alzheimer's disease, J Alzheimers Dis
Rodencal, Dixon, A tale of two lipids: Lipid unsaturation commands ferroptosis sensitivity, Proteomics
Rodriguez, Hepcidin induction by pathogens and pathogenderived molecules is strongly dependent on interleukin-6, Infect Immun
Rodriguez, Regulation of antioxidant enzymes: a significant role for melatonin, J Pineal Res
Romero, A review of metal-catalyzed molecular damage: protection by melatonin, J Pineal Res
Rossi, Oxidized forms of glutathione in peripheral blood as biomarkers of oxidative stress, Clin Chem
Roth, Melatonin promotes osteoblast differentiation and bone formation*, J Biol Chem
Roy, Belsham, Reiter, Melatonin receptor activation regulates GnRH Gene expression and secretion in GT1-7 GnRH neurons: signal transduction mechanisms, J Biol Chem
Rozengurt, Mitogenic signaling pathways induced by G proteincoupled receptors, J Cell Physiol
Ruddick, Tryptophan metabolism in the central nervous system: medical implications, Expert Rev Mol Med
Rudnicka-Drożak, Links between COVID-19 and Alzheimer's disease-what do we already know?, Int J Environ Res Public Health
Rui, Deletion of ferritin H in neurons counteracts the protective effect of melatonin against traumatic brain injury-induced ferroptosis, J Pineal Res
Régrigny, Melatonin improves cerebral circulation security margin in rats, Am J Physiology-Heart Circulatory Physiol
Sahu, Retrospective review of melatonin in patients with COVID-19, Chest
Salimi, Hamlyn, COVID-19 and crosstalk with the hallmarks of aging, J Gerontol Series A
Santana-Codina, Mancias, The role of NCOA4-mediated ferritinophagy in health and disease, Pharmaceuticals
Sargiacomo, Sotgia, Lisanti, COVID-19 and chronological aging: senolytics and other anti-aging drugs for the treatment or prevention of corona virus infection?, Aging
Sato, Aging is associated with increased brain iron through cortex-derived hepcidin expression, Mech Ageing Dev
Savla, Prabhavalkar, Bhatt, Cytokine storm associated coagulation complications in COVID-19 patients: pathogenesis and management, Expert Rev Anti Infect Ther
Schild, Multidomain cognitive impairment in non-hospitalized patients with the post-COVID-19 syndrome: results from a prospective monocentric cohort, J Neurol
Seibt, Proneth, Conrad, Role of GPX4 in ferroptosis and its pharmacological implication, Free Radical Biol Med
Sengupta, Clocks, viruses, and immunity: lessons for the COVID-19 pandemic, J Biol Rhythms
Sfera, Ferrosenescence: the iron age of neurodegeneration?, Mech Ageing Dev
Shen, Melatonin induces autophagy in amyotrophic lateral sclerosis mice via upregulation of SIRT1, Mol Neurobiol
Shih, Coordinate regulation of glutathione biosynthesis and release by Nrf2-expressing glia potently protects neurons from oxidative stress, J Neurosci
Shiu, Urgent search for safe and effective treatments of severe acute respiratory syndrome: is melatonin a promising candidate drug?, J Pineal Res
Sies, Defining roles of specific reactive oxygen species (ROS) in cell biology and physiology, Nat Rev Mol Cell Biol
Sies, Jones, Reactive oxygen species (ROS) as pleiotropic physiological signalling agents, Nat Rev Mol Cell Biol
Slominski, Melatonin membrane receptors in peripheral tissues: Distribution and functions, Mol Cell Endocrinol
Song, Human umbilical cord blood-derived MSCs exosome attenuate myocardial injury by inhibiting ferroptosis in acute myocardial infarction mice, Cell Biol Toxicol
Song, Temozolomide drives ferroptosis via a DMT1-dependent pathway in glioblastoma cells, Yonsei Med J
Sr, Physiological effects of melatonin: role of melatonin receptors and signal transduction pathways, Prog Neurobiol
Stankov, Melatonin signal transduction and mechanism of action in the central nervous system: using the rabbit cortex as a model, Endocrinology
Strassman, Elevated rectal temperature produced by all-night bright light is reversed by melatonin infusion in men, J Appl Physiol
Styś, Iron regulatory protein 1 outcompetes iron regulatory protein 2 in regulating cellular iron homeostasis in response to nitric oxide, J Biol Chem
Su, Melatonin attenuates angiotensin II-induced cardiomyocyte hypertrophy through the CyPA/CD147 signaling pathway, Mol Cell Biochem
Su, Reactive oxygen species-induced lipid peroxidation in apoptosis, autophagy, and ferroptosis, Oxid Med Cell Longev
Sun, Melatonin alleviates doxorubicin-induced mitochondrial oxidative damage and ferroptosis in cardiomyocytes by regulating YAP expression, Toxicol Appl Pharmacol
Sun, Protective effects of melatonin on male fertility preservation and reproductive system, Cryobiology
Suriawinata, Mehta, Iron and iron-related proteins in COVID-19, Clin Exp Med
Sánchez-Rico, Melatonin does not reduce mortality in adult hospitalized patients with COVID-19: a multicenter retrospective observational study, J Travel Med
Takahashi, Transcriptional architecture of the mammalian circadian clock, Nat Rev Genet
Tamarkin, Effect of melatonin on the reproductive systems of male and female Syrian hamsters: a diurnal rhythm in sensitivity to melatonin, Endocrinology
Tamura, Melatonin and the ovary: physiological and pathophysiological implications, Fertil Steril
Tan, Ebola virus disease: potential use of melatonin as a treatment, J Pineal Res
Taquet, 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records, Lancet Psychiatry
Taquet, Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA, Lancet Psychiatry
Taquet, Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients, Lancet Psychiatry
Taso, Lipid peroxidation products and their role in neurodegenerative diseases, Ann Res Hosp
Tomar, Raghav, Association of circadian clock and severe acute respiratory syndrome coronavirus 2 infection, Chronobiol Med
Tonelli, Chio, Tuveson, Transcriptional regulation by Nrf2, Antioxid Redox Signal
Touitou, Age-and mental health-related circadian rhythms of plasma levels of melatonin, prolactin, luteinizing hormone and folliclestimulating hormone in man, J Endocrinol
Touitou, Age-related changes in both circadian and seasonal rhythms of rectal temperature with special reference to senile dementia of Alzheimer type, Gerontology
Toyokuni, Ferroptosis at the crossroads of infection, aging and cancer, Cancer Sci
Tresguerres, Melatonin dietary supplement as an anti-aging therapy for age-related bone loss, Rejuvenation Res
Tripathi, SARS-CoV-2 causes senescence in human cells and exacerbates the senescence-associated secretory phenotype through TLR-3, Aging
Tseng, The dose and duration-dependent association between melatonin treatment and overall cognition in Alzheimer's dementia: a network meta-analysis of randomized placebo-controlled trials, Curr Neuropharmacol
Tu, Insights into the novel function of system Xc-in regulated cell death, Eur Rev Med Pharmacol Sci
Urrutia, Bórquez, Núñez, Inflaming the Brain with Iron, Antioxidants
Urrutia, Inflammation alters the expression of DMT1, FPN1 and hepcidin, and it causes iron accumulation in central nervous system cells, J Neurochem
Ursini, Maiorino, Lipid peroxidation and ferroptosis: The role of GSH and GPx4, Free Radical Biol Med
Vega, Chronic treatment with melatonin improves hippocampal neurogenesis in the aged brain and under neurodegeneration, Molecules
Vishnoi, Raisuddin, Parvez, Reiter, Glutamate excitotoxicity and oxidative stress in epilepsy: modulatory role of melatonin, J Environ Pathol Toxicol Oncol
Vriend, Reiter, Melatonin feedback on clock genes: a theory involving the proteasome, J Pineal Res
Wagner, Buettner, Burns, Free radical-mediated lipid peroxidation in cells: oxidizability is a function of cell lipid bis-allylic hydrogen content, Biochemistry
Waldhauser, Fall in nocturnal serum melatonin during prepuberty and pubescence, Lancet
Waldhauser, Serum melatonin in central precocious puberty is lower than in age-matched prepubertal children, J Clin Endocrinol Metab
Wan, Iron deposition leads to hyperphosphorylation of tau and disruption of insulin signaling, Front Neurol
Wang, Association of COVID-19 with new-onset Alzheimer's disease, J Alzheimer's Dis
Wang, Chemistry and biology of ω-3 PUFA peroxidation-derived compounds, Prostaglandins Other Lipid Mediat
Wang, Deficiency of angiotensin-converting enzyme 2 causes deterioration of cognitive function, npj Aging Mechanisms Dis
Wang, Revisiting the intersection of microglial activation and neuroinflammation in Alzheimer's disease from the perspective of ferroptosis, Chem Biol Interact
Weaver, Skouta, The selenoprotein glutathione peroxidase 4: from molecular mechanisms to novel therapeutic opportunities, Biomedicines
Wen, Sulforaphane triggers iron overload-mediated ferroptosis in gastric carcinoma cells by activating the PI3K/IRP2/DMT1 pathway, Hum Exp Toxicol
Wendimu, Hooks, Microglia phenotypes in aging and neurodegenerative diseases, Cells
Winterbourn, Toxicity of iron and hydrogen peroxide: the Fenton reaction, Toxicol Lett
Wu, A novel mechanism linking ferroptosis and endoplasmic reticulum stress via the circPtpn14/miR-351-5p/5-LOX signaling in melatonin-mediated treatment of traumatic brain injury, Free Radical Biol Med
Wurtman, Armstrong, Melatonin as a hormone in humans: a history, Yale J Biol Med
Wurtman, Axelrod, Chu, Melatonin, a pineal substance: effect on the rat ovary, Science
Wurtman, Interactions of the pineal and exposure to continuous light on organ weights of female rats, Eur J Endocrinol
Wójtowicz, Jakiel, Olcese, Melatonin and female reproduction: an expanding universe, Front Endocrinol
Xia, An update on inflamm-aging: mechanisms, prevention, and treatment, J Immunol Res
Xie, A review of sleep disorders and melatonin, Neurol Res
Xu, Melatonin alleviates PTSD-like behaviors and restores serum GABA and cortisol levels in mice, Psychopharmacology
Xu, Role of ferroptosis in stroke, Cell Mol Neurobiol
Yadalam, Assessing the therapeutic potential of agomelatine, ramelteon, and melatonin against SARS-CoV-2, Saudi J Biol Sci
Yanatori, Kishi, DMT1 and iron transport, Free Radical Biol Med
Yang, Clockophagy is a novel selective autophagy process favoring ferroptosis, Int J Equity Health
Yang, Lai, SARS-CoV-2 infection: can ferroptosis be a potential treatment target for multiple organ involvement?, Cell Death Discovery
Yang, Melatonin alleviates angiotensin-II-induced cardiac hypertrophy via activating MICU1 pathway, Aging
Yang, Tang, Zeng, Melatonin: potential avenue for treating iron overload disorders, Ageing Res Rev
Yao, Iron regulatory protein 1 promotes ferroptosis by sustaining cellular iron homeostasis in melanoma, Oncol Lett
Yasmin, The melatonin receptor in the human brain: cloning experiments and distribution studies, Gen Comp Endocrinol
Yin, Xu, Porter, Free radical lipid peroxidation: mechanisms and analysis, Chem Rev
Yoo, Melatonin improves D-galactose-induced aging effects on behavior, neurogenesis, and lipid peroxidation in the mouse dentate gyrus via increasing pCREB expression, J Pineal Res
You, Astrocyte hepcidin is a key factor in LPS-induced neuronal apoptosis, Cell Death Dis
Yu, Activation of PKG-CREB-KLF15 by melatonin attenuates Angiotensin II-induced vulnerability to atrial fibrillation via enhancing branched-chain amino acids catabolism, Free Radical Biol Med
Yılmaz, Öner, Melatonin levels are low in COVID-19 positive patients and these levels are associated with depression, death anxiety and insomnia, Scandinavian J Clin Lab Investig
Yılmaz, Öner, Melatonin levels are low in COVID-19 positive patients and these levels are associated with depression, death anxiety and insomnia, Yehia and Abulseoud Molecular Neurodegeneration
Zenesini, Risk of SARS-CoV-2 infection, hospitalization, and death for COVID-19 in people with Parkinson disease or parkinsonism over a 15-month period: A cohort study, Eur J Neurol
Zhang, COVID-19-related brain injury: the potential role of ferroptosis, J Inflammation Res
Zhang, Cellular iron status influences the functional relationship between microglia and oligodendrocytes, Redox Biol
Zhang, Hepcidin promoted ferroptosis through iron metabolism which is associated with DMT1 signaling activation in early brain injury following subarachnoid hemorrhage, Oxidative Med Cell Longevity
Zhang, Impairment of hepcidin upregulation by lipopolysaccharide in the interleukin-6 knockout mouse brain, Front Mol Neurosci
Zhang, Melatonin alleviates retinal ischemia-reperfusion injury by inhibiting p53-mediated ferroptosis, Antioxidants
Zhang, Melatonin inhibits adipogenesis and enhances osteogenesis of human mesenchymal stem cells by suppressing PPARγ expression and enhancing Runx2 expression, J Pineal Res
Zhang, SARS-COV-2 spike protein promotes RPE cell senescence via the ROS/P53/P21 pathway, Biogerontology
Zhao, Melatonin prevents against ethanol-induced liver injury by mitigating ferroptosis via targeting brain and muscle ARNT-like 1 in mice liver and HepG2 cells, J Agric Food Chem
Zhou, Increased serum levels of hepcidin and ferritin are associated with severity of COVID-19, Med Sci Monitor
Zhou, Iron overloaded polarizes macrophage to proinflammation phenotype through ROS/acetyl-p53 pathway, Cancer Med
Zhou, Melatonin reduces neuroinflammation and improves axonal hypomyelination by modulating M1/M2 microglia polarization via JAK2-STAT3-telomerase pathway in postnatal exposed to lipopolysaccharide, Mol Neurobiol
Zhou, Novel insights into ferroptosis: Implications for agerelated diseases, Theranostics
Zhuang, The circadian clock component BMAL1 regulates SARS-CoV-2 entry and replication in lung epithelial cells, IScience
Zimmermann, Effects of acute tryptophan depletion on nocturnal melatonin secretion in humans, J Clin Endocrinol Metab
DOI record:
{
"DOI": "10.1186/s13024-024-00728-6",
"ISSN": [
"1750-1326"
],
"URL": "http://dx.doi.org/10.1186/s13024-024-00728-6",
"abstract": "<jats:title>Abstract</jats:title><jats:p>The unprecedented pandemic of COVID-19 swept millions of lives in a short period, yet its menace continues among its survivors in the form of post-COVID syndrome. An exponentially growing number of COVID-19 survivors suffer from cognitive impairment, with compelling evidence of a trajectory of accelerated aging and neurodegeneration. The novel and enigmatic nature of this yet-to-unfold pathology demands extensive research seeking answers for both the molecular underpinnings and potential therapeutic targets. Ferroptosis, an iron-dependent cell death, is a strongly proposed underlying mechanism in post-COVID-19 aging and neurodegeneration discourse. COVID-19 incites neuroinflammation, iron dysregulation, reactive oxygen species (ROS) accumulation, antioxidant system repression, renin-angiotensin system (RAS) disruption, and clock gene alteration. These events pave the way for ferroptosis, which shows its signature in COVID-19, premature aging, and neurodegenerative disorders. In the search for a treatment, melatonin shines as a promising ferroptosis inhibitor with its repeatedly reported safety and tolerability. According to various studies, melatonin has proven efficacy in attenuating the severity of certain COVID-19 manifestations, validating its reputation as an anti-viral compound. Melatonin has well-documented anti-aging properties and combating neurodegenerative-related pathologies. Melatonin can block the leading events of ferroptosis since it is an efficient anti-inflammatory, iron chelator, antioxidant, angiotensin II antagonist, and clock gene regulator. Therefore, we propose ferroptosis as the culprit behind the post-COVID-19 trajectory of aging and neurodegeneration and melatonin, a well-fitting ferroptosis inhibitor, as a potential treatment.</jats:p>",
"alternative-id": [
"728"
],
"article-number": "36",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "7 February 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "15 April 2024"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "19 April 2024"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Consent for publication",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "This manuscript does not contain data from any individual person so the consent for publication is not applicable."
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "Not applicable. Ethics approval and consent are not indicated due to the review nature of this paper."
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 4,
"value": "The authors declare that they have no competing interests."
}
],
"author": [
{
"affiliation": [],
"family": "Yehia",
"given": "Asmaa",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-0652-0862",
"affiliation": [],
"authenticated-orcid": false,
"family": "Abulseoud",
"given": "Osama A.",
"sequence": "additional"
}
],
"container-title": "Molecular Neurodegeneration",
"container-title-short": "Mol Neurodegeneration",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2024,
4,
19
]
],
"date-time": "2024-04-19T13:02:03Z",
"timestamp": 1713531723000
},
"deposited": {
"date-parts": [
[
2024,
4,
19
]
],
"date-time": "2024-04-19T14:03:31Z",
"timestamp": 1713535411000
},
"indexed": {
"date-parts": [
[
2024,
4,
19
]
],
"date-time": "2024-04-19T14:40:50Z",
"timestamp": 1713537650210
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2024,
4,
19
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2024,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
4,
19
]
],
"date-time": "2024-04-19T00:00:00Z",
"timestamp": 1713484800000
}
},
{
"URL": "https://creativecommons.org/licenses/by/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2024,
4,
19
]
],
"date-time": "2024-04-19T00:00:00Z",
"timestamp": 1713484800000
}
}
],
"link": [
{
"URL": "https://link.springer.com/content/pdf/10.1186/s13024-024-00728-6.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/article/10.1186/s13024-024-00728-6/fulltext.html",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://link.springer.com/content/pdf/10.1186/s13024-024-00728-6.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1186",
"published": {
"date-parts": [
[
2024,
4,
19
]
]
},
"published-online": {
"date-parts": [
[
2024,
4,
19
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"DOI": "10.21203/rs.3.rs-1313103/v1",
"author": "M Marzouk",
"doi-asserted-by": "publisher",
"key": "728_CR1",
"unstructured": "Marzouk M, et al. Modeling COVID-19 Effects on Sustainable Development Goals in Egypt Using System Dynamics. 2022.",
"volume-title": "Modeling COVID-19 Effects on Sustainable Development Goals in Egypt Using System Dynamics",
"year": "2022"
},
{
"DOI": "10.3390/jcm10245913",
"author": "G Jennings",
"doi-asserted-by": "publisher",
"first-page": "5913",
"issue": "24",
"journal-title": "J Clin Med",
"key": "728_CR2",
"unstructured": "Jennings G, et al. A systematic review of persistent symptoms and residual abnormal functioning following acute COVID-19: ongoing symptomatic phase vs. post-COVID-19 syndrome. J Clin Med. 2021;10(24):5913.",
"volume": "10",
"year": "2021"
},
{
"author": "FJ Carod-Artal",
"first-page": "384",
"issue": "11",
"journal-title": "Rev Neurol",
"key": "728_CR3",
"unstructured": "Carod-Artal FJ. Post-COVID-19 syndrome: epidemiology, diagnostic criteria and pathogenic mechanisms involved. Rev Neurol. 2021;72(11):384–96.",
"volume": "72",
"year": "2021"
},
{
"DOI": "10.1016/j.dsx.2021.04.007",
"author": "AV Raveendran",
"doi-asserted-by": "publisher",
"first-page": "869",
"issue": "3",
"journal-title": "Diabetes Metab Syndr",
"key": "728_CR4",
"unstructured": "Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: an overview. Diabetes Metab Syndr. 2021;15(3):869–75.",
"volume": "15",
"year": "2021"
},
{
"author": "SA Meo",
"first-page": "1101",
"issue": "2",
"journal-title": "Eur Rev Med Pharmacol Sci",
"key": "728_CR5",
"unstructured": "Meo SA, et al. Magnetic Resonance Imaging (MRI) and neurological manifestations in SARS-CoV-2 patients. Eur Rev Med Pharmacol Sci. 2021;25(2):1101–8.",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.4103/jfmpc.jfmpc_851_21",
"author": "NKN Anjana",
"doi-asserted-by": "publisher",
"first-page": "4023",
"issue": "11",
"journal-title": "J Family Med Prim Care",
"key": "728_CR6",
"unstructured": "Anjana NKN, et al. Manifestations and risk factors of post COVID syndrome among COVID-19 patients presented with minimal symptoms - A study from Kerala, India. J Family Med Prim Care. 2021;10(11):4023–9.",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.2174/1871523021666220328115818",
"doi-asserted-by": "crossref",
"key": "728_CR7",
"unstructured": "Abdel-Gawad M. et al. Post-COVID-19 Syndrome Clinical Manifestations: A Systematic Review. Antiinflamm Antiallergy Agents Med Chem. 2022."
},
{
"DOI": "10.1016/S2215-0366(21)00084-5",
"author": "M Taquet",
"doi-asserted-by": "publisher",
"first-page": "416",
"issue": "5",
"journal-title": "Lancet Psychiatry",
"key": "728_CR8",
"unstructured": "Taquet M, et al. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8(5):416–27.",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/S2215-0366(20)30462-4",
"author": "M Taquet",
"doi-asserted-by": "publisher",
"first-page": "130",
"issue": "2",
"journal-title": "Lancet Psychiatry",
"key": "728_CR9",
"unstructured": "Taquet M, et al. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8(2):130–40.",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/S2215-0366(22)00260-7",
"author": "M Taquet",
"doi-asserted-by": "publisher",
"first-page": "815",
"issue": "10",
"journal-title": "Lancet Psychiatry",
"key": "728_CR10",
"unstructured": "Taquet M, et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. Lancet Psychiatry. 2022;9(10):815–27.",
"volume": "9",
"year": "2022"
},
{
"DOI": "10.3390/jpm12122070",
"author": "A Perrottelli",
"doi-asserted-by": "publisher",
"first-page": "2070",
"issue": "12",
"journal-title": "J Pers Med",
"key": "728_CR11",
"unstructured": "Perrottelli A, et al. Cognitive impairment after post-acute COVID-19 infection: a systematic review of the literature. J Pers Med. 2022;12(12):2070.",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1002/alz.12644",
"author": "L Crivelli",
"doi-asserted-by": "publisher",
"first-page": "1047",
"issue": "5",
"journal-title": "Alzheimers Dement",
"key": "728_CR12",
"unstructured": "Crivelli L, et al. Changes in cognitive functioning after COVID-19: a systematic review and meta-analysis. Alzheimers Dement. 2022;18(5):1047–66.",
"volume": "18",
"year": "2022"
},
{
"DOI": "10.1016/j.jns.2022.120162",
"author": "L Premraj",
"doi-asserted-by": "publisher",
"first-page": "120162",
"journal-title": "J Neurol Sci",
"key": "728_CR13",
"unstructured": "Premraj L, et al. Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis. J Neurol Sci. 2022;434:120162.",
"volume": "434",
"year": "2022"
},
{
"DOI": "10.1016/j.cell.2012.03.042",
"author": "SJ Dixon",
"doi-asserted-by": "publisher",
"first-page": "1060",
"issue": "5",
"journal-title": "Cell",
"key": "728_CR14",
"unstructured": "Dixon SJ, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149(5):1060–72.",
"volume": "149",
"year": "2012"
},
{
"DOI": "10.1146/annurev-cancerbio-030518-055844",
"author": "SJ Dixon",
"doi-asserted-by": "publisher",
"first-page": "35",
"journal-title": "Ann Rev Cancer Biol",
"key": "728_CR15",
"unstructured": "Dixon SJ, Stockwell BR. The hallmarks of ferroptosis. Ann Rev Cancer Biol. 2019;3:35–54.",
"volume": "3",
"year": "2019"
},
{
"DOI": "10.3389/fcell.2021.637162",
"author": "X Chen",
"doi-asserted-by": "publisher",
"first-page": "637162",
"journal-title": "Front Cell Dev Biol",
"key": "728_CR16",
"unstructured": "Chen X, et al. Characteristics and biomarkers of ferroptosis. Front Cell Dev Biol. 2021;9:637162.",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1038/s41598-018-23408-0",
"author": "E Agmon",
"doi-asserted-by": "publisher",
"first-page": "5155",
"issue": "1",
"journal-title": "Sci Rep",
"key": "728_CR17",
"unstructured": "Agmon E, et al. Modeling the effects of lipid peroxidation during ferroptosis on membrane properties. Sci Rep. 2018;8(1):5155.",
"volume": "8",
"year": "2018"
},
{
"DOI": "10.1155/2019/5080843",
"author": "L-J Su",
"doi-asserted-by": "publisher",
"first-page": "5080843",
"journal-title": "Oxid Med Cell Longev",
"key": "728_CR18",
"unstructured": "Su L-J, et al. Reactive oxygen species-induced lipid peroxidation in apoptosis, autophagy, and ferroptosis. Oxid Med Cell Longev. 2019;2019:5080843.",
"volume": "2019",
"year": "2019"
},
{
"DOI": "10.1038/s41580-022-00456-z",
"author": "H Sies",
"doi-asserted-by": "publisher",
"first-page": "499",
"issue": "7",
"journal-title": "Nat Rev Mol Cell Biol",
"key": "728_CR19",
"unstructured": "Sies H, et al. Defining roles of specific reactive oxygen species (ROS) in cell biology and physiology. Nat Rev Mol Cell Biol. 2022;23(7):499–515.",
"volume": "23",
"year": "2022"
},
{
"DOI": "10.2147/JIR.S275595",
"author": "J Checa",
"doi-asserted-by": "publisher",
"first-page": "1057",
"journal-title": "J Inflamm Res",
"key": "728_CR20",
"unstructured": "Checa J, Aran JM. Reactive oxygen species: drivers of physiological and pathological processes. J Inflamm Res. 2020;13:1057–73.",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1016/0378-4274(95)03532-X",
"author": "CC Winterbourn",
"doi-asserted-by": "publisher",
"first-page": "969",
"journal-title": "Toxicol Lett",
"key": "728_CR21",
"unstructured": "Winterbourn CC. Toxicity of iron and hydrogen peroxide: the Fenton reaction. Toxicol Lett. 1995;82:969–74.",
"volume": "82",
"year": "1995"
},
{
"DOI": "10.1042/bj2190001",
"author": "B Halliwell",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "Biochem J",
"key": "728_CR22",
"unstructured": "Halliwell B, Gutteridge J. Oxygen toxicity, oxygen radicals, transition metals and disease. Biochem J. 1984;219(1):1.",
"volume": "219",
"year": "1984"
},
{
"DOI": "10.1038/s41580-020-0230-3",
"author": "H Sies",
"doi-asserted-by": "publisher",
"first-page": "363",
"issue": "7",
"journal-title": "Nat Rev Mol Cell Biol",
"key": "728_CR23",
"unstructured": "Sies H, Jones DP. Reactive oxygen species (ROS) as pleiotropic physiological signalling agents. Nat Rev Mol Cell Biol. 2020;21(7):363–83.",
"volume": "21",
"year": "2020"
},
{
"DOI": "10.3390/ijms22094642",
"author": "CA Juan",
"doi-asserted-by": "publisher",
"first-page": "4642",
"issue": "9",
"journal-title": "Int J Mol Sci",
"key": "728_CR24",
"unstructured": "Juan CA, et al. The Chemistry of Reactive Oxygen Species (ROS) Revisited: Outlining Their Role in Biological Macromolecules (DNA, Lipids and Proteins) and Induced Pathologies. Int J Mol Sci. 2021;22(9):4642.",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1016/j.prostaglandins.2016.12.004",
"author": "W Wang",
"doi-asserted-by": "publisher",
"first-page": "84",
"journal-title": "Prostaglandins Other Lipid Mediat",
"key": "728_CR25",
"unstructured": "Wang W, et al. Chemistry and biology of ω-3 PUFA peroxidation-derived compounds. Prostaglandins Other Lipid Mediat. 2017;132:84–91.",
"volume": "132",
"year": "2017"
},
{
"DOI": "10.1155/2013/710290",
"author": "A Catalá",
"doi-asserted-by": "publisher",
"first-page": "710290",
"journal-title": "J Lipids",
"key": "728_CR26",
"unstructured": "Catalá A. Five decades with polyunsaturated fatty acids: chemical synthesis, enzymatic formation, lipid peroxidation and its biological effects. J Lipids. 2013;2013:710290.",
"volume": "2013",
"year": "2013"
},
{
"DOI": "10.1021/bi00181a003",
"author": "BA Wagner",
"doi-asserted-by": "publisher",
"first-page": "4449",
"issue": "15",
"journal-title": "Biochemistry",
"key": "728_CR27",
"unstructured": "Wagner BA, Buettner GR, Burns CP. Free radical-mediated lipid peroxidation in cells: oxidizability is a function of cell lipid bis-allylic hydrogen content. Biochemistry. 1994;33(15):4449–53.",
"volume": "33",
"year": "1994"
},
{
"DOI": "10.1097/01.CCM.0000186787.64500.12",
"author": "H Bayr",
"doi-asserted-by": "publisher",
"first-page": "S498",
"issue": "12",
"journal-title": "Crit Care Med",
"key": "728_CR28",
"unstructured": "Bayr H. Reactive oxygen species. Crit Care Med. 2005;33(12):S498–501.",
"volume": "33",
"year": "2005"
},
{
"DOI": "10.1021/cr200084z",
"author": "H Yin",
"doi-asserted-by": "publisher",
"first-page": "5944",
"issue": "10",
"journal-title": "Chem Rev",
"key": "728_CR29",
"unstructured": "Yin H, Xu L, Porter NA. Free radical lipid peroxidation: mechanisms and analysis. Chem Rev. 2011;111(10):5944–72.",
"volume": "111",
"year": "2011"
},
{
"DOI": "10.1016/0748-5514(85)90011-X",
"author": "AW Girotti",
"doi-asserted-by": "publisher",
"first-page": "87",
"issue": "2",
"journal-title": "J Free Radic Biol Med",
"key": "728_CR30",
"unstructured": "Girotti AW. Mechanisms of lipid peroxidation. J Free Radic Biol Med. 1985;1(2):87–95.",
"volume": "1",
"year": "1985"
},
{
"DOI": "10.1016/j.bbrc.2016.10.086",
"author": "MM Gaschler",
"doi-asserted-by": "publisher",
"first-page": "419",
"issue": "3",
"journal-title": "Biochem Biophys Res Commun",
"key": "728_CR31",
"unstructured": "Gaschler MM, Stockwell BR. Lipid peroxidation in cell death. Biochem Biophys Res Commun. 2017;482(3):419–25.",
"volume": "482",
"year": "2017"
},
{
"DOI": "10.1093/ajcn/57.5.715S",
"author": "B Halliwell",
"doi-asserted-by": "publisher",
"first-page": "715S",
"issue": "5",
"journal-title": "Am J Clin Nutr",
"key": "728_CR32",
"unstructured": "Halliwell B, Chirico S. Lipid peroxidation: its mechanism, measurement, and significance. Am J Clin Nutr. 1993;57(5):715S–725S.",
"volume": "57",
"year": "1993"
},
{
"DOI": "10.1016/j.bbrc.2005.08.072",
"author": "E Niki",
"doi-asserted-by": "publisher",
"first-page": "668",
"issue": "1",
"journal-title": "Biochem Biophys Res Commun",
"key": "728_CR33",
"unstructured": "Niki E, et al. Lipid peroxidation: mechanisms, inhibition, and biological effects. Biochem Biophys Res Commun. 2005;338(1):668–76.",
"volume": "338",
"year": "2005"
},
{
"DOI": "10.1016/S0891-5849(02)00855-9",
"author": "H Kühn",
"doi-asserted-by": "publisher",
"first-page": "154",
"issue": "2",
"journal-title": "Free Rad Biol Med",
"key": "728_CR34",
"unstructured": "Kühn H, Borchert A. Regulation of enzymatic lipid peroxidation: the interplay of peroxidizing and peroxide reducing enzymes1 1This article is part of a series of reviews on “Regulatory and Cytoprotective Aspects of Lipid Hydroperoxide Metabolism.” The full list of papers may be found on the homepage of the journal. Free Rad Biol Med. 2002;33(2):154–72.",
"volume": "33",
"year": "2002"
},
{
"DOI": "10.1016/j.molcel.2022.03.022",
"author": "D Liang",
"doi-asserted-by": "publisher",
"first-page": "2215",
"issue": "12",
"journal-title": "Mol Cell",
"key": "728_CR35",
"unstructured": "Liang D, Minikes AM, Jiang X. Ferroptosis at the intersection of lipid metabolism and cellular signaling. Mol Cell. 2022;82(12):2215–27.",
"volume": "82",
"year": "2022"
},
{
"DOI": "10.3390/biology10030184",
"author": "J-Y Lee",
"doi-asserted-by": "publisher",
"first-page": "184",
"issue": "3",
"journal-title": "Biology",
"key": "728_CR36",
"unstructured": "Lee J-Y, et al. Lipid metabolism and ferroptosis. Biology. 2021;10(3):184.",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1016/0009-2797(89)90087-2",
"author": "G Minotti",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "Chem Biol Interact",
"key": "728_CR37",
"unstructured": "Minotti G, Aust SD. The role of iron in oxygen radical mediated lipid peroxidation. Chem Biol Interact. 1989;71(1):1–19.",
"volume": "71",
"year": "1989"
},
{
"DOI": "10.1021/cr040077w",
"author": "Z Cheng",
"doi-asserted-by": "publisher",
"first-page": "748",
"issue": "3",
"journal-title": "Chem Rev",
"key": "728_CR38",
"unstructured": "Cheng Z, Li Y. What is responsible for the initiating chemistry of iron-mediated lipid peroxidation: an update. Chem Rev. 2007;107(3):748–66.",
"volume": "107",
"year": "2007"
},
{
"DOI": "10.1016/j.bbabio.2008.07.003",
"author": "R Pamplona",
"doi-asserted-by": "publisher",
"first-page": "1249",
"issue": "10",
"journal-title": "Biochim Biophys Acta",
"key": "728_CR39",
"unstructured": "Pamplona R. Membrane phospholipids, lipoxidative damage and molecular integrity: a causal role in aging and longevity. Biochim Biophys Acta. 2008;1777(10):1249–62.",
"volume": "1777",
"year": "2008"
},
{
"DOI": "10.3389/fphys.2013.00242",
"author": "S Pizzimenti",
"doi-asserted-by": "publisher",
"first-page": "242",
"journal-title": "Front Physiol",
"key": "728_CR40",
"unstructured": "Pizzimenti S, et al. Interaction of aldehydes derived from lipid peroxidation and membrane proteins. Front Physiol. 2013;4:242.",
"volume": "4",
"year": "2013"
},
{
"author": "OV Taso",
"first-page": "10.21037",
"issue": "2",
"journal-title": "Ann Res Hosp",
"key": "728_CR41",
"unstructured": "Taso OV, et al. Lipid peroxidation products and their role in neurodegenerative diseases. Ann Res Hosp. 2019;3(2):10.21037.",
"volume": "3",
"year": "2019"
},
{
"DOI": "10.3109/10715762.2010.498477",
"author": "F Guéraud",
"doi-asserted-by": "publisher",
"first-page": "1098",
"issue": "10",
"journal-title": "Free Radical Res",
"key": "728_CR42",
"unstructured": "Guéraud F, et al. Chemistry and biochemistry of lipid peroxidation products. Free Radical Res. 2010;44(10):1098–124.",
"volume": "44",
"year": "2010"
},
{
"DOI": "10.1016/j.jphotobiol.2014.03.028",
"author": "S Miyamoto",
"doi-asserted-by": "publisher",
"first-page": "24",
"journal-title": "J Photochem Photobiol, B",
"key": "728_CR43",
"unstructured": "Miyamoto S, et al. Singlet molecular oxygen generated by biological hydroperoxides. J Photochem Photobiol, B. 2014;139:24–33.",
"volume": "139",
"year": "2014"
},
{
"DOI": "10.3389/fphar.2023.1147414",
"author": "J Pei",
"doi-asserted-by": "publisher",
"first-page": "1147414",
"journal-title": "Front Pharmacol",
"key": "728_CR44",
"unstructured": "Pei J, et al. Research progress of glutathione peroxidase family (GPX) in redoxidation. Front Pharmacol. 2023;14:1147414.",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1016/j.freeradbiomed.2018.03.001",
"author": "JPF Angeli",
"doi-asserted-by": "publisher",
"first-page": "153",
"journal-title": "Free Radical Biol Med",
"key": "728_CR45",
"unstructured": "Angeli JPF, Conrad M. Selenium and GPX4, a vital symbiosis. Free Radical Biol Med. 2018;127:153–9.",
"volume": "127",
"year": "2018"
},
{
"DOI": "10.3390/biomedicines10040891",
"author": "K Weaver",
"doi-asserted-by": "publisher",
"first-page": "891",
"issue": "4",
"journal-title": "Biomedicines",
"key": "728_CR46",
"unstructured": "Weaver K, Skouta R. The selenoprotein glutathione peroxidase 4: from molecular mechanisms to novel therapeutic opportunities. Biomedicines. 2022;10(4):891.",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1016/j.bbagen.2012.09.008",
"author": "SC Lu",
"doi-asserted-by": "publisher",
"first-page": "3143",
"issue": "5",
"journal-title": "Biochim Biophys Acta",
"key": "728_CR47",
"unstructured": "Lu SC. Glutathione synthesis. Biochim Biophys Acta. 2013;1830(5):3143–53.",
"volume": "1830",
"year": "2013"
},
{
"DOI": "10.1016/j.mam.2008.08.006",
"author": "HJ Forman",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1–2",
"journal-title": "Mol Aspects Med",
"key": "728_CR48",
"unstructured": "Forman HJ, Zhang H, Rinna A. Glutathione: overview of its protective roles, measurement, and biosynthesis. Mol Aspects Med. 2009;30(1–2):1–12.",
"volume": "30",
"year": "2009"
},
{
"DOI": "10.3390/ijms22095010",
"author": "K Aoyama",
"doi-asserted-by": "publisher",
"first-page": "5010",
"issue": "9",
"journal-title": "Int J Mol Sci",
"key": "728_CR49",
"unstructured": "Aoyama K. Glutathione in the Brain. Int J Mol Sci. 2021;22(9):5010.",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1016/0076-6879(95)51107-5",
"author": "HF Gilbert",
"doi-asserted-by": "publisher",
"first-page": "8",
"journal-title": "Methods Enzymol",
"key": "728_CR50",
"unstructured": "Gilbert HF. [2] Thiol/disulfide exchange equilibria and disulfidebond stability. Methods Enzymol. 1995;251:8–28.",
"volume": "251",
"year": "1995"
},
{
"DOI": "10.1373/clinchem.2006.067793",
"author": "R Rossi",
"doi-asserted-by": "publisher",
"first-page": "1406",
"issue": "7",
"journal-title": "Clin Chem",
"key": "728_CR51",
"unstructured": "Rossi R, et al. Oxidized forms of glutathione in peripheral blood as biomarkers of oxidative stress. Clin Chem. 2006;52(7):1406–14.",
"volume": "52",
"year": "2006"
},
{
"DOI": "10.3389/fphar.2022.910292",
"author": "F-J Li",
"doi-asserted-by": "publisher",
"first-page": "910292",
"journal-title": "Front Pharmacol",
"key": "728_CR52",
"unstructured": "Li F-J, et al. System Xc−/GSH/GPX4 axis: An important antioxidant system for the ferroptosis in drug-resistant solid tumor therapy. Front Pharmacol. 2022;13:910292.",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1074/jbc.M110.121327",
"author": "PK Mandal",
"doi-asserted-by": "publisher",
"first-page": "22244",
"issue": "29",
"journal-title": "J Biol Chem",
"key": "728_CR53",
"unstructured": "Mandal PK, et al. System xc− and thioredoxin reductase 1 cooperatively rescue glutathione deficiency. J Biol Chem. 2010;285(29):22244–53.",
"volume": "285",
"year": "2010"
},
{
"DOI": "10.1089/ars.2011.4391",
"author": "J Lewerenz",
"doi-asserted-by": "publisher",
"first-page": "522",
"issue": "5",
"journal-title": "Antioxid Redox Signal",
"key": "728_CR54",
"unstructured": "Lewerenz J, et al. The cystine/glutamate antiporter system xc− in health and disease: from molecular mechanisms to novel therapeutic opportunities. Antioxid Redox Signal. 2013;18(5):522–55.",
"volume": "18",
"year": "2013"
},
{
"DOI": "10.1016/j.freeradbiomed.2008.10.040",
"author": "C Harvey",
"doi-asserted-by": "publisher",
"first-page": "443",
"issue": "4",
"journal-title": "Free Radical Biol Med",
"key": "728_CR55",
"unstructured": "Harvey C, et al. Nrf2-regulated glutathione recycling independent of biosynthesis is critical for cell survival during oxidative stress. Free Radical Biol Med. 2009;46(4):443–53.",
"volume": "46",
"year": "2009"
},
{
"DOI": "10.1523/JNEUROSCI.23-08-03394.2003",
"author": "AY Shih",
"doi-asserted-by": "publisher",
"first-page": "3394",
"issue": "8",
"journal-title": "J Neurosci",
"key": "728_CR56",
"unstructured": "Shih AY, et al. Coordinate regulation of glutathione biosynthesis and release by Nrf2-expressing glia potently protects neurons from oxidative stress. J Neurosci. 2003;23(8):3394–406.",
"volume": "23",
"year": "2003"
},
{
"DOI": "10.1089/ars.2017.7342",
"author": "C Tonelli",
"doi-asserted-by": "publisher",
"first-page": "1727",
"issue": "17",
"journal-title": "Antioxid Redox Signal",
"key": "728_CR57",
"unstructured": "Tonelli C, Chio IIC, Tuveson DA. Transcriptional regulation by Nrf2. Antioxid Redox Signal. 2018;29(17):1727–45.",
"volume": "29",
"year": "2018"
},
{
"DOI": "10.1016/j.redox.2019.101107",
"author": "M Dodson",
"doi-asserted-by": "publisher",
"first-page": "101107",
"journal-title": "Redox Biol",
"key": "728_CR58",
"unstructured": "Dodson M, Castro-Portuguez R, Zhang DD. NRF2 plays a critical role in mitigating lipid peroxidation and ferroptosis. Redox Biol. 2019;23:101107.",
"volume": "23",
"year": "2019"
},
{
"DOI": "10.9790/5736-071123846",
"author": "C Gupta",
"doi-asserted-by": "publisher",
"first-page": "38",
"issue": "11",
"journal-title": "IOSR J Appl Chem",
"key": "728_CR59",
"unstructured": "Gupta C. Role of iron (Fe) in body. IOSR J Appl Chem. 2014;7(11):38–46.",
"volume": "7",
"year": "2014"
},
{
"author": "N Abbaspour",
"first-page": "164",
"issue": "2",
"journal-title": "J Res Med Sci",
"key": "728_CR60",
"unstructured": "Abbaspour N, Hurrell R, Kelishadi R. Review on iron and its importance for human health. J Res Med Sci. 2014;19(2):164.",
"volume": "19",
"year": "2014"
},
{
"DOI": "10.3389/fphar.2014.00045",
"author": "ZI Cabantchik",
"doi-asserted-by": "publisher",
"first-page": "45",
"journal-title": "Front Pharmacol",
"key": "728_CR61",
"unstructured": "Cabantchik ZI. Labile iron in cells and body fluids: physiology, pathology, and pharmacology. Front Pharmacol. 2014;5:45.",
"volume": "5",
"year": "2014"
},
{
"DOI": "10.3945/ajcn.117.155804",
"author": "GJ Anderson",
"doi-asserted-by": "publisher",
"first-page": "1559S",
"issue": "6",
"journal-title": "Am J Clin Nutr",
"key": "728_CR62",
"unstructured": "Anderson GJ, Frazer DM. Current understanding of iron homeostasis. Am J Clin Nutr. 2017;106(6):1559S–1566S.",
"volume": "106",
"year": "2017"
},
{
"DOI": "10.1016/j.mam.2020.100866",
"author": "A Katsarou",
"doi-asserted-by": "publisher",
"first-page": "100866",
"journal-title": "Mol Aspects Med",
"key": "728_CR63",
"unstructured": "Katsarou A, Pantopoulos K. Basics and principles of cellular and systemic iron homeostasis. Mol Aspects Med. 2020;75:100866.",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1182/blood-2011-01-258467",
"author": "T Ganz",
"doi-asserted-by": "publisher",
"first-page": "4425",
"issue": "17",
"journal-title": "Blood",
"key": "728_CR64",
"unstructured": "Ganz T. Hepcidin and iron regulation, 10 years later. Blood. 2011;117(17):4425–33.",
"volume": "117",
"year": "2011"
},
{
"DOI": "10.1016/j.cmet.2012.03.018",
"author": "B Qiao",
"doi-asserted-by": "publisher",
"first-page": "918",
"issue": "6",
"journal-title": "Cell Metab",
"key": "728_CR65",
"unstructured": "Qiao B, et al. Hepcidin-induced endocytosis of ferroportin is dependent on ferroportin ubiquitination. Cell Metab. 2012;15(6):918–24.",
"volume": "15",
"year": "2012"
},
{
"DOI": "10.1126/science.1057206",
"author": "AT McKie",
"doi-asserted-by": "publisher",
"first-page": "1755",
"issue": "5509",
"journal-title": "Science",
"key": "728_CR66",
"unstructured": "McKie AT, et al. An iron-regulated ferric reductase associated with the absorption of dietary iron. Science. 2001;291(5509):1755–9.",
"volume": "291",
"year": "2001"
},
{
"DOI": "10.1016/j.jtemb.2012.03.015",
"author": "BK Fuqua",
"doi-asserted-by": "publisher",
"first-page": "115",
"issue": "2",
"journal-title": "J Trace Elem Med Biol",
"key": "728_CR67",
"unstructured": "Fuqua BK, Vulpe CD, Anderson GJ. Intestinal iron absorption. J Trace Elem Med Biol. 2012;26(2):115–9.",
"volume": "26",
"year": "2012"
},
{
"DOI": "10.1016/j.freeradbiomed.2018.06.037",
"author": "H Kawabata",
"doi-asserted-by": "publisher",
"first-page": "46",
"journal-title": "Free Radical Biol Med",
"key": "728_CR68",
"unstructured": "Kawabata H. Transferrin and transferrin receptors update. Free Radical Biol Med. 2019;133:46–54.",
"volume": "133",
"year": "2019"
},
{
"DOI": "10.1016/j.freeradbiomed.2018.07.020",
"author": "I Yanatori",
"doi-asserted-by": "publisher",
"first-page": "55",
"journal-title": "Free Radical Biol Med",
"key": "728_CR69",
"unstructured": "Yanatori I, Kishi F. DMT1 and iron transport. Free Radical Biol Med. 2019;133:55–63.",
"volume": "133",
"year": "2019"
},
{
"DOI": "10.1016/0005-2728(96)00022-9",
"author": "PM Harrison",
"doi-asserted-by": "publisher",
"first-page": "161",
"issue": "3",
"journal-title": "Biochim Biophys Acta",
"key": "728_CR70",
"unstructured": "Harrison PM, Arosio P. The ferritins: molecular properties, iron storage function and cellular regulation. Biochim Biophys Acta. 1996;1275(3):161–203.",
"volume": "1275",
"year": "1996"
},
{
"DOI": "10.3389/fnins.2019.00238",
"author": "M del QuilesRey",
"doi-asserted-by": "publisher",
"first-page": "238",
"journal-title": "Front Neurosci",
"key": "728_CR71",
"unstructured": "del QuilesRey M, Mancias JD. NCOA4-mediated ferritinophagy: a potential link to neurodegeneration. Front Neurosci. 2019;13:238.",
"volume": "13",
"year": "2019"
},
{
"DOI": "10.3390/ph11040114",
"author": "N Santana-Codina",
"doi-asserted-by": "publisher",
"first-page": "114",
"issue": "4",
"journal-title": "Pharmaceuticals",
"key": "728_CR72",
"unstructured": "Santana-Codina N, Mancias JD. The role of NCOA4-mediated ferritinophagy in health and disease. Pharmaceuticals. 2018;11(4):114.",
"volume": "11",
"year": "2018"
},
{
"DOI": "10.1080/15548627.2016.1187366",
"author": "W Hou",
"doi-asserted-by": "publisher",
"first-page": "1425",
"issue": "8",
"journal-title": "Autophagy",
"key": "728_CR73",
"unstructured": "Hou W, et al. Autophagy promotes ferroptosis by degradation of ferritin. Autophagy. 2016;12(8):1425–8.",
"volume": "12",
"year": "2016"
},
{
"DOI": "10.1111/jpi.12704",
"author": "T Rui",
"doi-asserted-by": "publisher",
"first-page": "e12704",
"issue": "2",
"journal-title": "J Pineal Res",
"key": "728_CR74",
"unstructured": "Rui T, et al. Deletion of ferritin H in neurons counteracts the protective effect of melatonin against traumatic brain injury-induced ferroptosis. J Pineal Res. 2021;70(2):e12704.",
"volume": "70",
"year": "2021"
},
{
"author": "CA Finch",
"first-page": "657",
"issue": "5",
"journal-title": "West J Med",
"key": "728_CR75",
"unstructured": "Finch CA, et al. Plasma ferritin determination as a diagnostic tool. West J Med. 1986;145(5):657.",
"volume": "145",
"year": "1986"
},
{
"DOI": "10.1067/mlc.2000.106456",
"author": "P Nielsen",
"doi-asserted-by": "publisher",
"first-page": "413",
"issue": "5",
"journal-title": "J Lab Clin Med",
"key": "728_CR76",
"unstructured": "Nielsen P, et al. Serum ferritin iron in iron overload and liver damage: correlation to body iron stores and diagnostic relevance. J Lab Clin Med. 2000;135(5):413–8.",
"volume": "135",
"year": "2000"
},
{
"DOI": "10.1016/j.blre.2008.08.001",
"author": "MA Knovich",
"doi-asserted-by": "publisher",
"first-page": "95",
"issue": "3",
"journal-title": "Blood Rev",
"key": "728_CR77",
"unstructured": "Knovich MA, et al. Ferritin for the clinician. Blood Rev. 2009;23(3):95–104.",
"volume": "23",
"year": "2009"
},
{
"DOI": "10.1016/j.mrfmmm.2003.08.004",
"author": "M Kruszewski",
"doi-asserted-by": "publisher",
"first-page": "81",
"issue": "1–2",
"journal-title": "Mutat Res",
"key": "728_CR78",
"unstructured": "Kruszewski M. Labile iron pool: the main determinant of cellular response to oxidative stress. Mutat Res. 2003;531(1–2):81–92.",
"volume": "531",
"year": "2003"
},
{
"DOI": "10.1146/annurev.nutr.28.061807.155521",
"author": "MU Muckenthaler",
"doi-asserted-by": "publisher",
"first-page": "197",
"journal-title": "Annu Rev Nutr",
"key": "728_CR79",
"unstructured": "Muckenthaler MU, Galy B, Hentze MW. Systemic iron homeostasis and the iron-responsive element/iron-regulatory protein (IRE/IRP) regulatory network. Annu Rev Nutr. 2008;28:197–213.",
"volume": "28",
"year": "2008"
},
{
"DOI": "10.1074/jbc.M111.231902",
"author": "A Styś",
"doi-asserted-by": "publisher",
"first-page": "22846",
"issue": "26",
"journal-title": "J Biol Chem",
"key": "728_CR80",
"unstructured": "Styś A, et al. Iron regulatory protein 1 outcompetes iron regulatory protein 2 in regulating cellular iron homeostasis in response to nitric oxide. J Biol Chem. 2011;286(26):22846–54.",
"volume": "286",
"year": "2011"
},
{
"DOI": "10.1002/iub.1628",
"author": "S Recalcati",
"doi-asserted-by": "publisher",
"first-page": "389",
"issue": "6",
"journal-title": "IUBMB Life",
"key": "728_CR81",
"unstructured": "Recalcati S, et al. Molecular regulation of cellular iron balance. IUBMB Life. 2017;69(6):389–98.",
"volume": "69",
"year": "2017"
},
{
"DOI": "10.1097/MCO.0000000000000634",
"author": "J Montesinos",
"doi-asserted-by": "publisher",
"first-page": "68",
"issue": "2",
"journal-title": "Curr Opin Clin Nutr Metab Care",
"key": "728_CR82",
"unstructured": "Montesinos J, Guardia-Laguarta C, Area-Gomez E. The fat brain. Curr Opin Clin Nutr Metab Care. 2020;23(2):68–75.",
"volume": "23",
"year": "2020"
},
{
"DOI": "10.1007/978-1-60327-514-9_2",
"doi-asserted-by": "crossref",
"key": "728_CR83",
"unstructured": "Friedman J. Why is the nervous system vulnerable to oxidative stress? Oxidative Stress Free Radical Damage Neurol. 2011:19–27."
},
{
"DOI": "10.1002/pmic.202100308",
"author": "J Rodencal",
"doi-asserted-by": "publisher",
"first-page": "2100308",
"issue": "6",
"journal-title": "Proteomics",
"key": "728_CR84",
"unstructured": "Rodencal J, Dixon SJ. A tale of two lipids: Lipid unsaturation commands ferroptosis sensitivity. Proteomics. 2023;23(6):2100308.",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.1016/j.devcel.2020.06.019",
"author": "MA Perez",
"doi-asserted-by": "publisher",
"first-page": "447",
"issue": "4",
"journal-title": "Dev Cell",
"key": "728_CR85",
"unstructured": "Perez MA, et al. Dietary lipids induce ferroptosis in caenorhabditiselegans and human cancer cells. Dev Cell. 2020;54(4):447–45. e44.",
"volume": "54",
"year": "2020"
},
{
"DOI": "10.1016/j.ccell.2022.02.003",
"author": "P Liao",
"doi-asserted-by": "publisher",
"first-page": "365",
"issue": "4",
"journal-title": "Cancer Cell",
"key": "728_CR86",
"unstructured": "Liao P, et al. CD8+ T cells and fatty acids orchestrate tumor ferroptosis and immunity via ACSL4. Cancer Cell. 2022;40(4):365–378. e6.",
"volume": "40",
"year": "2022"
},
{
"DOI": "10.1016/j.prostaglandins.2019.106363",
"author": "H Kuwata",
"doi-asserted-by": "publisher",
"first-page": "106363",
"journal-title": "Prostaglandins Other Lipid Mediat",
"key": "728_CR87",
"unstructured": "Kuwata H, Hara S. Role of acyl-CoA synthetase ACSL4 in arachidonic acid metabolism. Prostaglandins Other Lipid Mediat. 2019;144:106363.",
"volume": "144",
"year": "2019"
},
{
"DOI": "10.1038/nchembio.2239",
"author": "S Doll",
"doi-asserted-by": "publisher",
"first-page": "91",
"issue": "1",
"journal-title": "Nat Chem Biol",
"key": "728_CR88",
"unstructured": "Doll S, et al. ACSL4 dictates ferroptosis sensitivity by shaping cellular lipid composition. Nat Chem Biol. 2017;13(1):91–8.",
"volume": "13",
"year": "2017"
},
{
"DOI": "10.1016/j.freeradbiomed.2018.09.014",
"author": "TM Seibt",
"doi-asserted-by": "publisher",
"first-page": "144",
"journal-title": "Free Radical Biol Med",
"key": "728_CR89",
"unstructured": "Seibt TM, Proneth B, Conrad M. Role of GPX4 in ferroptosis and its pharmacological implication. Free Radical Biol Med. 2019;133:144–52.",
"volume": "133",
"year": "2019"
},
{
"DOI": "10.1016/j.freeradbiomed.2020.02.027",
"author": "F Ursini",
"doi-asserted-by": "publisher",
"first-page": "175",
"journal-title": "Free Radical Biol Med",
"key": "728_CR90",
"unstructured": "Ursini F, Maiorino M. Lipid peroxidation and ferroptosis: The role of GSH and GPx4. Free Radical Biol Med. 2020;152:175–85.",
"volume": "152",
"year": "2020"
},
{
"DOI": "10.1002/pmic.201800311",
"author": "GC Forcina",
"doi-asserted-by": "publisher",
"first-page": "1800311",
"issue": "18",
"journal-title": "Proteomics",
"key": "728_CR91",
"unstructured": "Forcina GC, Dixon SJ. GPX4 at the crossroads of lipid homeostasis and ferroptosis. Proteomics. 2019;19(18):1800311.",
"volume": "19",
"year": "2019"
},
{
"DOI": "10.1038/nature14344",
"author": "L Jiang",
"doi-asserted-by": "publisher",
"first-page": "57",
"issue": "7545",
"journal-title": "Nature",
"key": "728_CR92",
"unstructured": "Jiang L, et al. Ferroptosis as a p53-mediated activity during tumour suppression. Nature. 2015;520(7545):57–62.",
"volume": "520",
"year": "2015"
},
{
"DOI": "10.1007/s13238-020-00789-5",
"author": "P Koppula",
"doi-asserted-by": "publisher",
"first-page": "599",
"issue": "8",
"journal-title": "Protein Cell",
"key": "728_CR93",
"unstructured": "Koppula P, Zhuang L, Gan B. Cystine transporter SLC7A11/xCT in cancer: ferroptosis, nutrient dependency, and cancer therapy. Protein Cell. 2021;12(8):599–620.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.molcel.2015.06.011",
"author": "M Gao",
"doi-asserted-by": "publisher",
"first-page": "298",
"issue": "2",
"journal-title": "Mol Cell",
"key": "728_CR94",
"unstructured": "Gao M, et al. Glutaminolysis and transferrin regulate ferroptosis. Mol Cell. 2015;59(2):298–308.",
"volume": "59",
"year": "2015"
},
{
"DOI": "10.1016/j.celrep.2020.02.049",
"author": "H Feng",
"doi-asserted-by": "publisher",
"first-page": "3411",
"issue": "10",
"journal-title": "Cell Rep",
"key": "728_CR95",
"unstructured": "Feng H, et al. Transferrin receptor is a specific ferroptosis marker. Cell Rep. 2020;30(10):3411–3423. e7.",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.3349/ymj.2021.62.9.843",
"author": "Q Song",
"doi-asserted-by": "publisher",
"first-page": "843",
"issue": "9",
"journal-title": "Yonsei Med J",
"key": "728_CR96",
"unstructured": "Song Q, et al. Temozolomide drives ferroptosis via a DMT1-dependent pathway in glioblastoma cells. Yonsei Med J. 2021;62(9):843.",
"volume": "62",
"year": "2021"
},
{
"DOI": "10.1007/s10565-020-09530-8",
"author": "Y Song",
"doi-asserted-by": "publisher",
"first-page": "51",
"journal-title": "Cell Biol Toxicol",
"key": "728_CR97",
"unstructured": "Song Y, et al. Human umbilical cord blood–derived MSCs exosome attenuate myocardial injury by inhibiting ferroptosis in acute myocardial infarction mice. Cell Biol Toxicol. 2021;37:51–64.",
"volume": "37",
"year": "2021"
},
{
"DOI": "10.3892/ol.2021.12918",
"author": "F Yao",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "3",
"journal-title": "Oncol Lett",
"key": "728_CR98",
"unstructured": "Yao F, et al. Iron regulatory protein 1 promotes ferroptosis by sustaining cellular iron homeostasis in melanoma. Oncol Lett. 2021;22(3):1–12.",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1177/09603271231177295",
"author": "J Wen",
"doi-asserted-by": "publisher",
"first-page": "096032712311772",
"journal-title": "Hum Exp Toxicol",
"key": "728_CR99",
"unstructured": "Wen J, et al. Sulforaphane triggers iron overload-mediated ferroptosis in gastric carcinoma cells by activating the PI3K/IRP2/DMT1 pathway. Hum Exp Toxicol. 2023;42:09603271231177295.",
"volume": "42",
"year": "2023"
},
{
"author": "N Geng",
"first-page": "3826",
"issue": "12",
"journal-title": "Eur Rev Med Pharmacol Sci",
"key": "728_CR100",
"unstructured": "Geng N, et al. Knockdown of ferroportin accelerates erastin-induced ferroptosis in neuroblastoma cells. Eur Rev Med Pharmacol Sci. 2018;22(12):3826–36.",
"volume": "22",
"year": "2018"
},
{
"DOI": "10.1038/s41418-020-00685-9",
"author": "W-D Bao",
"doi-asserted-by": "publisher",
"first-page": "1548",
"issue": "5",
"journal-title": "Cell Death Differ",
"key": "728_CR101",
"unstructured": "Bao W-D, et al. Loss of ferroportin induces memory impairment by promoting ferroptosis in Alzheimer’s disease. Cell Death Differ. 2021;28(5):1548–62.",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1155/2021/9800794",
"doi-asserted-by": "crossref",
"key": "728_CR102",
"unstructured": "Zhang H. et al. Hepcidin promoted ferroptosis through iron metabolism which is associated with DMT1 signaling activation in early brain injury following subarachnoid hemorrhage. Oxidative Med Cell Longevity. 2021;2021."
},
{
"DOI": "10.1021/acscentsci.0c01592",
"author": "Y Fang",
"doi-asserted-by": "publisher",
"first-page": "980",
"issue": "6",
"journal-title": "ACS Cent Sci",
"key": "728_CR103",
"unstructured": "Fang Y, et al. Inhibiting ferroptosis through disrupting the NCOA4–FTH1 interaction: a new mechanism of action. ACS Cent Sci. 2021;7(6):980–9.",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1016/j.jhazmat.2022.129043",
"author": "N Liu",
"doi-asserted-by": "publisher",
"first-page": "129043",
"journal-title": "J Hazard Mater",
"key": "728_CR104",
"unstructured": "Liu N, et al. The role of ferroptosis mediated by NRF2/ERK-regulated ferritinophagy in CdTe QDs-induced inflammation in macrophage. J Hazard Mater. 2022;436:129043.",
"volume": "436",
"year": "2022"
},
{
"DOI": "10.1016/j.freeradbiomed.2022.12.002",
"author": "Y Cheng",
"doi-asserted-by": "publisher",
"first-page": "184",
"journal-title": "Free Radical Biol Med",
"key": "728_CR105",
"unstructured": "Cheng Y, et al. TrkB agonist N-acetyl serotonin promotes functional recovery after traumatic brain injury by suppressing ferroptosis via the PI3K/Akt/Nrf2/Ferritin H pathway. Free Radical Biol Med. 2023;194:184–98.",
"volume": "194",
"year": "2023"
},
{
"DOI": "10.1126/sciadv.aaw2238",
"doi-asserted-by": "crossref",
"key": "728_CR106",
"unstructured": "Yang, M., et al., Clockophagy is a novel selective autophagy process favoring ferroptosis. Science advances, 2019. 5(7): p. eaaw2238."
},
{
"DOI": "10.1186/s12939-020-01242-z",
"author": "Y Rozenfeld",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "Int J Equity Health",
"key": "728_CR107",
"unstructured": "Rozenfeld Y, et al. A model of disparities: risk factors associated with COVID-19 infection. Int J Equity Health. 2020;19(1):1–10.",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.18632/aging.202136",
"author": "L Pang",
"doi-asserted-by": "publisher",
"first-page": "26248",
"issue": "24",
"journal-title": "Aging (Albany NY)",
"key": "728_CR108",
"unstructured": "Pang L, et al. Influence of aging on deterioration of patients with COVID-19. Aging (Albany NY). 2020;12(24):26248.",
"volume": "12",
"year": "2020"
},
{
"key": "728_CR109",
"unstructured": "Aguado J. et al. Senolytic therapy alleviates physiological human brain aging and COVID-19 neuropathology. bioRxiv, 2023: p. 2023.01. 17.524329."
},
{
"DOI": "10.18632/aging.103001",
"author": "C Sargiacomo",
"doi-asserted-by": "publisher",
"first-page": "6511",
"issue": "8",
"journal-title": "Aging (Albany NY)",
"key": "728_CR110",
"unstructured": "Sargiacomo C, Sotgia F, Lisanti MP. COVID-19 and chronological aging: senolytics and other anti-aging drugs for the treatment or prevention of corona virus infection? Aging (Albany NY). 2020;12(8):6511.",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.18632/aging.203560",
"author": "U Tripathi",
"doi-asserted-by": "publisher",
"first-page": "21838",
"issue": "18",
"journal-title": "Aging (albany NY)",
"key": "728_CR111",
"unstructured": "Tripathi U, et al. SARS-CoV-2 causes senescence in human cells and exacerbates the senescence-associated secretory phenotype through TLR-3. Aging (albany NY). 2021;13(18):21838.",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1128/JVI.00794-21",
"author": "K Meyer",
"doi-asserted-by": "publisher",
"first-page": "e00794",
"issue": "17",
"journal-title": "J Virol",
"key": "728_CR112",
"unstructured": "Meyer K, et al. SARS-CoV-2 spike protein induces paracrine senescence and leukocyte adhesion in endothelial cells. J Virol. 2021;95(17):e00794–e821.",
"volume": "95",
"year": "2021"
},
{
"DOI": "10.1038/s41467-022-29801-8",
"author": "X Cao",
"doi-asserted-by": "publisher",
"first-page": "2135",
"issue": "1",
"journal-title": "Nat Commun",
"key": "728_CR113",
"unstructured": "Cao X, et al. Accelerated biological aging in COVID-19 patients. Nat Commun. 2022;13(1):2135.",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.3233/JPD-202249",
"author": "EG Brown",
"doi-asserted-by": "publisher",
"first-page": "1365",
"issue": "4",
"journal-title": "J Parkinsons Dis",
"key": "728_CR114",
"unstructured": "Brown EG, et al. The effect of the COVID-19 pandemic on people with Parkinson’s disease. J Parkinsons Dis. 2020;10(4):1365–77.",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.3233/JPD-212779",
"author": "C Ineichen",
"doi-asserted-by": "publisher",
"first-page": "1579",
"issue": "4",
"journal-title": "J Parkinsons Dis",
"key": "728_CR115",
"unstructured": "Ineichen C, et al. Worsened Parkinson’s disease progression: impact of the COVID-19 pandemic. J Parkinsons Dis. 2021;11(4):1579–83.",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.parkreldis.2022.04.011",
"author": "U Fedeli",
"doi-asserted-by": "publisher",
"first-page": "75",
"journal-title": "Parkinsonism Relat Disord",
"key": "728_CR116",
"unstructured": "Fedeli U, et al. Parkinson’s disease related mortality: Long-term trends and impact of COVID-19 pandemic waves. Parkinsonism Relat Disord. 2022;98:75–7.",
"volume": "98",
"year": "2022"
},
{
"DOI": "10.1002/mdc3.13231",
"author": "R Parihar",
"doi-asserted-by": "publisher",
"first-page": "859",
"issue": "6",
"journal-title": "Movement Disorders Clinical Practice",
"key": "728_CR117",
"unstructured": "Parihar R, et al. Outcome of Hospitalized Parkinson’s Disease Patients with and without COVID-19. Movement Disorders Clinical Practice. 2021;8(6):859–67.",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1111/ene.15505",
"author": "C Zenesini",
"doi-asserted-by": "publisher",
"first-page": "3205",
"issue": "11",
"journal-title": "Eur J Neurol",
"key": "728_CR118",
"unstructured": "Zenesini C, et al. Risk of SARS-CoV-2 infection, hospitalization, and death for COVID-19 in people with Parkinson disease or parkinsonism over a 15-month period: A cohort study. Eur J Neurol. 2022;29(11):3205–17.",
"volume": "29",
"year": "2022"
},
{
"key": "728_CR119",
"unstructured": "Wang L. et al. Association of COVID-19 with new-onset Alzheimer’s disease. J Alzheimer's Dis. 2022(Preprint):1–4."
},
{
"DOI": "10.3233/JAD-220031",
"doi-asserted-by": "crossref",
"key": "728_CR120",
"unstructured": "Chung SJ. et al. Association of Alzheimer’s disease with COVID-19 susceptibility and severe complications: a nationwide cohort study. J Alzheimer's Dis. 2022(Preprint):1–10."
},
{
"DOI": "10.3390/ijerph20032146",
"author": "E Rudnicka-Drożak",
"doi-asserted-by": "publisher",
"first-page": "2146",
"issue": "3",
"journal-title": "Int J Environ Res Public Health",
"key": "728_CR121",
"unstructured": "Rudnicka-Drożak E, et al. Links between COVID-19 and Alzheimer’s disease—what do we already know? Int J Environ Res Public Health. 2023;20(3):2146.",
"volume": "20",
"year": "2023"
},
{
"DOI": "10.1002/alz.12556",
"author": "JA Frontera",
"doi-asserted-by": "publisher",
"first-page": "899",
"issue": "5",
"journal-title": "Alzheimers Dement",
"key": "728_CR122",
"unstructured": "Frontera JA, et al. Comparison of serum neurodegenerative biomarkers among hospitalized COVID-19 patients versus non-COVID subjects with normal cognition, mild cognitive impairment, or Alzheimer’s dementia. Alzheimers Dement. 2022;18(5):899–910.",
"volume": "18",
"year": "2022"
},
{
"DOI": "10.1016/j.bbrc.2021.03.100",
"author": "D Idrees",
"doi-asserted-by": "publisher",
"first-page": "94",
"journal-title": "Biochem Biophys Res Commun",
"key": "728_CR123",
"unstructured": "Idrees D, Kumar V. SARS-CoV-2 spike protein interactions with amyloidogenic proteins: Potential clues to neurodegeneration. Biochem Biophys Res Commun. 2021;554:94–8.",
"volume": "554",
"year": "2021"
},
{
"DOI": "10.1007/s00415-022-11543-8",
"author": "R Ferrucci",
"doi-asserted-by": "publisher",
"first-page": "1823",
"issue": "4",
"journal-title": "J Neurol",
"key": "728_CR124",
"unstructured": "Ferrucci R, et al. Brain positron emission tomography (PET) and cognitive abnormalities one year after COVID-19. J Neurol. 2023;270(4):1823–34.",
"volume": "270",
"year": "2023"
},
{
"DOI": "10.1016/j.psychres.2022.115006",
"author": "JA Matias-Guiu",
"doi-asserted-by": "publisher",
"first-page": "115006",
"journal-title": "Psychiatry Res",
"key": "728_CR125",
"unstructured": "Matias-Guiu JA, et al. Development of criteria for cognitive dysfunction in post-COVID syndrome: the IC-CoDi-COVID approach. Psychiatry Res. 2023;319:115006.",
"volume": "319",
"year": "2023"
},
{
"DOI": "10.1038/s41598-023-32939-0",
"author": "E Herrera",
"doi-asserted-by": "publisher",
"first-page": "6378",
"issue": "1",
"journal-title": "Sci Rep",
"key": "728_CR126",
"unstructured": "Herrera E, et al. Cognitive impairment in young adults with post COVID-19 syndrome. Sci Rep. 2023;13(1):6378.",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.1002/brb3.2508",
"author": "C Garcia-Sanchez",
"doi-asserted-by": "publisher",
"first-page": "e2508",
"issue": "3",
"journal-title": "Brain Behav",
"key": "728_CR127",
"unstructured": "Garcia-Sanchez C, et al. Neuropsychological deficits in patients with cognitive complaints after COVID-19. Brain Behav. 2022;12(3):e2508.",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1002/acn3.51350",
"author": "EL Graham",
"doi-asserted-by": "publisher",
"first-page": "1073",
"issue": "5",
"journal-title": "Ann Clin Transl Neurol",
"key": "728_CR128",
"unstructured": "Graham EL, et al. Persistent neurologic symptoms and cognitive dysfunction in non-hospitalized Covid-19 “long haulers.” Ann Clin Transl Neurol. 2021;8(5):1073–85.",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.1016/j.jaclp.2022.01.003",
"author": "SJ Ferrando",
"doi-asserted-by": "publisher",
"first-page": "474",
"issue": "5",
"journal-title": "J Acad Consult Liaison Psychiatry",
"key": "728_CR129",
"unstructured": "Ferrando SJ, et al. Neuropsychological, Medical, and Psychiatric Findings After Recovery From Acute COVID-19: A Cross-sectional Study. J Acad Consult Liaison Psychiatry. 2022;63(5):474–84.",
"volume": "63",
"year": "2022"
},
{
"DOI": "10.1007/s00415-022-11444-w",
"author": "AK Schild",
"doi-asserted-by": "publisher",
"first-page": "1215",
"issue": "3",
"journal-title": "J Neurol",
"key": "728_CR130",
"unstructured": "Schild AK, et al. Multidomain cognitive impairment in non-hospitalized patients with the post-COVID-19 syndrome: results from a prospective monocentric cohort. J Neurol. 2023;270(3):1215–23.",
"volume": "270",
"year": "2023"
},
{
"DOI": "10.1186/s13024-021-00469-w",
"author": "YH Liu",
"doi-asserted-by": "publisher",
"first-page": "48",
"issue": "1",
"journal-title": "Mol Neurodegener",
"key": "728_CR131",
"unstructured": "Liu YH, et al. Post-infection cognitive impairments in a cohort of elderly patients with COVID-19. Mol Neurodegener. 2021;16(1):48.",
"volume": "16",
"year": "2021"
},
{
"DOI": "10.1016/j.jpsychires.2022.03.033",
"author": "C Delgado-Alonso",
"doi-asserted-by": "publisher",
"first-page": "40",
"journal-title": "J Psychiatr Res",
"key": "728_CR132",
"unstructured": "Delgado-Alonso C, et al. Cognitive dysfunction associated with COVID-19: a comprehensive neuropsychological study. J Psychiatr Res. 2022;150:40–6.",
"volume": "150",
"year": "2022"
},
{
"key": "728_CR133",
"unstructured": "Ariza M. et al. COVID-19 severity is related to poor executive function in people with post-COVID conditions. J Neurol. 2023:1–17."
},
{
"DOI": "10.1021/ja01543a060",
"author": "AB Lerner",
"doi-asserted-by": "publisher",
"first-page": "2587",
"issue": "10",
"journal-title": "J Am Chem Soc",
"key": "728_CR134",
"unstructured": "Lerner AB, et al. Isolation of melatonin, the pineal gland factor that lightens melanocyteS1. J Am Chem Soc. 1958;80(10):2587–2587.",
"volume": "80",
"year": "1958"
},
{
"DOI": "10.1056/NEJM199701163360306",
"author": "A Brzezinski",
"doi-asserted-by": "publisher",
"first-page": "186",
"issue": "3",
"journal-title": "N Engl J Med",
"key": "728_CR135",
"unstructured": "Brzezinski A. Melatonin in humans. N Engl J Med. 1997;336(3):186–95.",
"volume": "336",
"year": "1997"
},
{
"DOI": "10.1016/j.smrv.2004.08.001",
"author": "B Claustrat",
"doi-asserted-by": "publisher",
"first-page": "11",
"issue": "1",
"journal-title": "Sleep Med Rev",
"key": "728_CR136",
"unstructured": "Claustrat B, Brun J, Chazot G. The basic physiology and pathophysiology of melatonin. Sleep Med Rev. 2005;9(1):11–24.",
"volume": "9",
"year": "2005"
},
{
"DOI": "10.1016/0303-7207(91)90087-9",
"author": "RJ Reiter",
"doi-asserted-by": "publisher",
"first-page": "C153",
"issue": "1–3",
"journal-title": "Mol Cell Endocrinol",
"key": "728_CR137",
"unstructured": "Reiter RJ. Melatonin: the chemical expression of darkness. Mol Cell Endocrinol. 1991;79(1–3):C153–8.",
"volume": "79",
"year": "1991"
},
{
"author": "RJ Wurtman",
"first-page": "547",
"issue": "6",
"journal-title": "Yale J Biol Med",
"key": "728_CR138",
"unstructured": "Wurtman RJ. Melatonin as a hormone in humans: a history. Yale J Biol Med. 1985;58(6):547.",
"volume": "58",
"year": "1985"
},
{
"DOI": "10.1007/BF01953050",
"author": "SM Armstrong",
"doi-asserted-by": "publisher",
"first-page": "932",
"issue": "10",
"journal-title": "Experientia",
"key": "728_CR139",
"unstructured": "Armstrong SM. Melatonin and circadian control in mammals. Experientia. 1989;45(10):932–8.",
"volume": "45",
"year": "1989"
},
{
"author": "A Cagnacci",
"first-page": "447",
"issue": "2",
"journal-title": "J Clin Endocrinol Metab",
"key": "728_CR140",
"unstructured": "Cagnacci A, Elliott J, Yen S. Melatonin: a major regulator of the circadian rhythm of core temperature in humans. J Clin Endocrinol Metab. 1992;75(2):447–52.",
"volume": "75",
"year": "1992"
},
{
"DOI": "10.1530/ror.0.0030013",
"author": "J Arendt",
"doi-asserted-by": "publisher",
"first-page": "13",
"journal-title": "Rev Reprod",
"key": "728_CR141",
"unstructured": "Arendt J. Melatonin and the pineal gland: influence on mammalian seasonal and circadian physiology. Rev Reprod. 1998;3:13–22.",
"volume": "3",
"year": "1998"
},
{
"DOI": "10.1016/S1054-3589(08)61169-2",
"doi-asserted-by": "crossref",
"key": "728_CR142",
"unstructured": "Axelrod J, Wurtman RJ. Photic and Neural Control of Indoleamine Metabolism in the Rat Pineal Gland, in Advances in Pharmacology, S. Garattini and P.A. Shore, Editors. 1968, Academic Press. p. 157–166."
},
{
"DOI": "10.1126/science.184.4144.1341",
"author": "J Axelrod",
"doi-asserted-by": "publisher",
"first-page": "1341",
"issue": "4144",
"journal-title": "Science",
"key": "728_CR143",
"unstructured": "Axelrod J. The Pineal Gland: a neurochemical transducer: chemical signals from nerves regulate synthesis of melatonin and convey information about internal clocks. Science. 1974;184(4144):1341–8.",
"volume": "184",
"year": "1974"
},
{
"DOI": "10.1126/science.1067262",
"author": "DM Berson",
"doi-asserted-by": "publisher",
"first-page": "1070",
"issue": "5557",
"journal-title": "Science",
"key": "728_CR144",
"unstructured": "Berson DM, Dunn FA, Takao M. Phototransduction by retinal ganglion cells that set the circadian clock. Science. 2002;295(5557):1070–3.",
"volume": "295",
"year": "2002"
},
{
"DOI": "10.1016/j.jphysparis.2011.07.001",
"author": "P Pevet",
"doi-asserted-by": "publisher",
"first-page": "170",
"issue": "4–6",
"journal-title": "Journal of Physiology-Paris",
"key": "728_CR145",
"unstructured": "Pevet P, Challet E. Melatonin: both master clock output and internal time-giver in the circadian clocks network. Journal of Physiology-Paris. 2011;105(4–6):170–82.",
"volume": "105",
"year": "2011"
},
{
"DOI": "10.1016/0166-2236(90)90100-O",
"author": "DN Krause",
"doi-asserted-by": "publisher",
"first-page": "464",
"issue": "11",
"journal-title": "Trends Neurosci",
"key": "728_CR146",
"unstructured": "Krause DN, Dubocovich ML. Regulatory sites in the melatonin system of mammals. Trends Neurosci. 1990;13(11):464–70.",
"volume": "13",
"year": "1990"
},
{
"DOI": "10.1016/0006-8993(79)90848-5",
"author": "DC Klein",
"doi-asserted-by": "publisher",
"first-page": "245",
"issue": "2",
"journal-title": "Brain Res",
"key": "728_CR147",
"unstructured": "Klein DC, Moore RY. Pineal N-acetyltransferase and hydroxyindole-O-methyl-transferase: control by the retinohypothalamic tract and the suprachiasmatic nucleus. Brain Res. 1979;174(2):245–62.",
"volume": "174",
"year": "1979"
},
{
"author": "R Zimmermann",
"first-page": "1160",
"issue": "5",
"journal-title": "J Clin Endocrinol Metab",
"key": "728_CR148",
"unstructured": "Zimmermann R, et al. Effects of acute tryptophan depletion on nocturnal melatonin secretion in humans. J Clin Endocrinol Metab. 1993;76(5):1160–4.",
"volume": "76",
"year": "1993"
},
{
"DOI": "10.1017/S1462399406000068",
"author": "JP Ruddick",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "20",
"journal-title": "Expert Rev Mol Med",
"key": "728_CR149",
"unstructured": "Ruddick JP, et al. Tryptophan metabolism in the central nervous system: medical implications. Expert Rev Mol Med. 2006;8(20):1–27.",
"volume": "8",
"year": "2006"
},
{
"DOI": "10.1016/0303-7207(82)90088-0",
"author": "TS King",
"doi-asserted-by": "publisher",
"first-page": "327",
"issue": "3",
"journal-title": "Mol Cell Endocrinol",
"key": "728_CR150",
"unstructured": "King TS, Richardson BA, Reiter RJ. Regulation of rat pineal melatonin synthesis: effect of monoamine oxidase inhibition. Mol Cell Endocrinol. 1982;25(3):327–38.",
"volume": "25",
"year": "1982"
},
{
"DOI": "10.1007/s00018-014-1579-2",
"author": "D Acuña-Castroviejo",
"doi-asserted-by": "publisher",
"first-page": "2997",
"issue": "16",
"journal-title": "Cell Mol Life Sci",
"key": "728_CR151",
"unstructured": "Acuña-Castroviejo D, et al. Extrapineal melatonin: sources, regulation, and potential functions. Cell Mol Life Sci. 2014;71(16):2997–3025.",
"volume": "71",
"year": "2014"
},
{
"DOI": "10.1152/physiol.00011.2014",
"author": "RJ Reiter",
"doi-asserted-by": "publisher",
"first-page": "325",
"issue": "5",
"journal-title": "Physiology",
"key": "728_CR152",
"unstructured": "Reiter RJ, Tan DX, Galano A. Melatonin: exceeding expectations. Physiology. 2014;29(5):325–33.",
"volume": "29",
"year": "2014"
},
{
"DOI": "10.1111/j.1600-079X.1995.tb00180.x",
"author": "EJ Costa",
"doi-asserted-by": "publisher",
"first-page": "123",
"issue": "3",
"journal-title": "J Pineal Res",
"key": "728_CR153",
"unstructured": "Costa EJ, Lopes RH, Lamy-Freund MT. Permeability of pure lipid bilayers to melatonin. J Pineal Res. 1995;19(3):123–6.",
"volume": "19",
"year": "1995"
},
{
"DOI": "10.3390/antiox9111088",
"author": "N Ferlazzo",
"doi-asserted-by": "publisher",
"first-page": "1088",
"issue": "11",
"journal-title": "Antioxidants",
"key": "728_CR154",
"unstructured": "Ferlazzo N, et al. Is melatonin the cornucopia of the 21st century? Antioxidants. 2020;9(11):1088.",
"volume": "9",
"year": "2020"
},
{
"DOI": "10.1016/0896-6273(94)90055-8",
"author": "SM Reppert",
"doi-asserted-by": "publisher",
"first-page": "1177",
"issue": "5",
"journal-title": "Neuron",
"key": "728_CR155",
"unstructured": "Reppert SM, Weaver DR, Ebisawa T. Cloning and characterization of a mammalian melatonin receptor that mediates reproductive and circadian responses. Neuron. 1994;13(5):1177–85.",
"volume": "13",
"year": "1994"
},
{
"DOI": "10.1073/pnas.92.19.8734",
"author": "SM Reppert",
"doi-asserted-by": "publisher",
"first-page": "8734",
"issue": "19",
"journal-title": "Proc Natl Acad Sci",
"key": "728_CR156",
"unstructured": "Reppert SM, et al. Molecular characterization of a second melatonin receptor expressed in human retina and brain: the Mel1b melatonin receptor. Proc Natl Acad Sci. 1995;92(19):8734–8.",
"volume": "92",
"year": "1995"
},
{
"DOI": "10.1002/jcp.21246",
"author": "E Rozengurt",
"doi-asserted-by": "publisher",
"first-page": "589",
"issue": "3",
"journal-title": "J Cell Physiol",
"key": "728_CR157",
"unstructured": "Rozengurt E. Mitogenic signaling pathways induced by G protein-coupled receptors. J Cell Physiol. 2007;213(3):589–602.",
"volume": "213",
"year": "2007"
},
{
"DOI": "10.1111/bph.13950",
"author": "E Cecon",
"doi-asserted-by": "publisher",
"first-page": "3263",
"issue": "16",
"journal-title": "Br J Pharmacol",
"key": "728_CR158",
"unstructured": "Cecon E, Oishi A, Jockers R. Melatonin receptors: molecular pharmacology and signalling in the context of system bias. Br J Pharmacol. 2018;175(16):3263–80.",
"volume": "175",
"year": "2018"
},
{
"DOI": "10.1016/j.mce.2012.01.004",
"author": "RM Slominski",
"doi-asserted-by": "publisher",
"first-page": "152",
"issue": "2",
"journal-title": "Mol Cell Endocrinol",
"key": "728_CR159",
"unstructured": "Slominski RM, et al. Melatonin membrane receptors in peripheral tissues: Distribution and functions. Mol Cell Endocrinol. 2012;351(2):152–66.",
"volume": "351",
"year": "2012"
},
{
"DOI": "10.1074/jbc.M005141200",
"author": "O Nosjean",
"doi-asserted-by": "publisher",
"first-page": "31311",
"issue": "40",
"journal-title": "J Biol Chem",
"key": "728_CR160",
"unstructured": "Nosjean O, et al. Identification of the Melatonin-binding SiteMT 3 as the Quinone Reductase 2. J Biol Chem. 2000;275(40):31311–7.",
"volume": "275",
"year": "2000"
},
{
"DOI": "10.1517/14728222.2016.1091882",
"author": "JA Boutin",
"doi-asserted-by": "publisher",
"first-page": "303",
"issue": "3",
"journal-title": "Expert Opin Ther Targets",
"key": "728_CR161",
"unstructured": "Boutin JA. Quinone reductase 2 as a promising target of melatonin therapeutic actions. Expert Opin Ther Targets. 2016;20(3):303–17.",
"volume": "20",
"year": "2016"
},
{
"DOI": "10.1016/S0021-9258(19)61934-4",
"author": "M Becker-André",
"doi-asserted-by": "publisher",
"first-page": "28531",
"issue": "46",
"journal-title": "J Biol Chem",
"key": "728_CR162",
"unstructured": "Becker-André M, et al. Pineal gland hormone melatonin binds and activates an orphan of the nuclear receptor superfamily. J Biol Chem. 1994;269(46):28531–4.",
"volume": "269",
"year": "1994"
},
{
"DOI": "10.1038/nrd4100",
"author": "DJ Kojetin",
"doi-asserted-by": "publisher",
"first-page": "197",
"issue": "3",
"journal-title": "Nat Rev Drug Discovery",
"key": "728_CR163",
"unstructured": "Kojetin DJ, Burris TP. REV-ERB and ROR nuclear receptors as drug targets. Nat Rev Drug Discovery. 2014;13(3):197–216.",
"volume": "13",
"year": "2014"
},
{
"DOI": "10.1126/science.141.3577.277",
"author": "RJ Wurtman",
"doi-asserted-by": "publisher",
"first-page": "277",
"issue": "3577",
"journal-title": "Science",
"key": "728_CR164",
"unstructured": "Wurtman RJ, Axelrod J, Chu EW. Melatonin, a pineal substance: effect on the rat ovary. Science. 1963;141(3577):277–8.",
"volume": "141",
"year": "1963"
},
{
"key": "728_CR165",
"unstructured": "Reiter, R., et al. Melatonin: reproductive effects. in The Pineal Gland: Proceedings of the International Symposium, Jerusalem, November 14–17, 1977. 1978. Springer."
},
{
"key": "728_CR166",
"unstructured": "Fiske V, Bryant G, Putnam J. Effect of light on the weight of the pineal in the rat. 1960, ENDOCRINE SOC 4350 EAST WEST HIGHWAY SUITE 500, BETHESDA, MD 20814-4110. p. 489-491."
},
{
"DOI": "10.1530/acta.0.0360617",
"author": "RJ Wurtman",
"doi-asserted-by": "publisher",
"first-page": "617",
"issue": "4",
"journal-title": "Eur J Endocrinol",
"key": "728_CR167",
"unstructured": "Wurtman RJ, et al. Interactions of the pineal and exposure to continuous light on organ weights of female rats. Eur J Endocrinol. 1961;36(4):617–24.",
"volume": "36",
"year": "1961"
},
{
"DOI": "10.1210/endo-99-6-1534",
"author": "L Tamarkin",
"doi-asserted-by": "publisher",
"first-page": "1534",
"issue": "6",
"journal-title": "Endocrinology",
"key": "728_CR168",
"unstructured": "Tamarkin L, et al. Effect of melatonin on the reproductive systems of male and female Syrian hamsters: a diurnal rhythm in sensitivity to melatonin. Endocrinology. 1976;99(6):1534–41.",
"volume": "99",
"year": "1976"
},
{
"DOI": "10.3109/07420529209064550",
"author": "AJ Lewy",
"doi-asserted-by": "publisher",
"first-page": "380",
"issue": "5",
"journal-title": "Chronobiol Int",
"key": "728_CR169",
"unstructured": "Lewy AJ, et al. Melatonin shifts human orcadian rhythms according to a phase-response curve. Chronobiol Int. 1992;9(5):380–92.",
"volume": "9",
"year": "1992"
},
{
"DOI": "10.1152/jappl.1991.71.6.2178",
"author": "RJ Strassman",
"doi-asserted-by": "publisher",
"first-page": "2178",
"issue": "6",
"journal-title": "J Appl Physiol",
"key": "728_CR170",
"unstructured": "Strassman RJ, et al. Elevated rectal temperature produced by all-night bright light is reversed by melatonin infusion in men. J Appl Physiol. 1991;71(6):2178–82.",
"volume": "71",
"year": "1991"
},
{
"DOI": "10.1111/j.1749-6632.1994.tb21831.x",
"author": "B Poeggeler",
"doi-asserted-by": "publisher",
"first-page": "419",
"issue": "1",
"journal-title": "Ann N Y Acad Sci",
"key": "728_CR171",
"unstructured": "Poeggeler B, et al. Melatonin—a highly potent endogenous radical scavenger and electron donor: new aspects of the oxidation chemistry of this indole accessed in vitro a. Ann N Y Acad Sci. 1994;738(1):419–20.",
"volume": "738",
"year": "1994"
},
{
"DOI": "10.1111/j.1749-6632.2000.tb05402.x",
"author": "RJ Reiter",
"doi-asserted-by": "publisher",
"first-page": "376",
"issue": "1",
"journal-title": "Ann N Y Acad Sci",
"key": "728_CR172",
"unstructured": "Reiter RJ, et al. Melatonin and its relation to the immune system and inflammation. Ann N Y Acad Sci. 2000;917(1):376–86.",
"volume": "917",
"year": "2000"
},
{
"DOI": "10.1677/joe.0.1570443",
"author": "L Morgan",
"doi-asserted-by": "publisher",
"first-page": "443",
"issue": "3",
"journal-title": "J Endocrinol",
"key": "728_CR173",
"unstructured": "Morgan L, et al. Effects of the endogenous clock and sleep time on melatonin, insulin, glucose and lipid metabolism. J Endocrinol. 1998;157(3):443–52.",
"volume": "157",
"year": "1998"
},
{
"key": "728_CR174",
"unstructured": "Arendt J. Melatonin and the mammalian pineal gland. 1994: Springer Science & Business Media."
},
{
"DOI": "10.1523/JNEUROSCI.21-16-06405.2001",
"author": "GC Brainard",
"doi-asserted-by": "publisher",
"first-page": "6405",
"issue": "16",
"journal-title": "J Neurosci",
"key": "728_CR175",
"unstructured": "Brainard GC, et al. Action spectrum for melatonin regulation in humans: evidence for a novel circadian photoreceptor. J Neurosci. 2001;21(16):6405–12.",
"volume": "21",
"year": "2001"
},
{
"DOI": "10.1007/s00441-002-0584-1",
"author": "P Pevet",
"doi-asserted-by": "publisher",
"first-page": "183",
"journal-title": "Cell Tissue Res",
"key": "728_CR176",
"unstructured": "Pevet P, et al. The chronobiotic properties of melatonin. Cell Tissue Res. 2002;309:183–91.",
"volume": "309",
"year": "2002"
},
{
"DOI": "10.1002/9780470720981.ch16",
"doi-asserted-by": "crossref",
"key": "728_CR177",
"unstructured": "Arendt J et al. Some effects of melatonin and the control of its secretion in humans. in Ciba Foundation Symposium 117‐Photoperiodism, Melatonin and the Pineal. 1985. Wiley Online Library."
},
{
"DOI": "10.1016/S0896-6273(00)80350-5",
"author": "C Liu",
"doi-asserted-by": "publisher",
"first-page": "91",
"issue": "1",
"journal-title": "Neuron",
"key": "728_CR178",
"unstructured": "Liu C, et al. Molecular dissection of two distinct actions of melatonin on the suprachiasmatic circadian clock. Neuron. 1997;19(1):91–102.",
"volume": "19",
"year": "1997"
},
{
"author": "U Albrecht",
"first-page": "8",
"issue": "48–55",
"journal-title": "Front Biosci",
"key": "728_CR179",
"unstructured": "Albrecht U. The mammalian circadian clock: a network of gene expression. Front Biosci. 2004;9(48–55):8.",
"volume": "9",
"year": "2004"
},
{
"DOI": "10.1111/jpi.12189",
"author": "J Vriend",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "J Pineal Res",
"key": "728_CR180",
"unstructured": "Vriend J, Reiter RJ. Melatonin feedback on clock genes: a theory involving the proteasome. J Pineal Res. 2015;58(1):1–11.",
"volume": "58",
"year": "2015"
},
{
"DOI": "10.1038/nrg.2016.150",
"author": "JS Takahashi",
"doi-asserted-by": "publisher",
"first-page": "164",
"issue": "3",
"journal-title": "Nat Rev Genet",
"key": "728_CR181",
"unstructured": "Takahashi JS. Transcriptional architecture of the mammalian circadian clock. Nat Rev Genet. 2017;18(3):164–79.",
"volume": "18",
"year": "2017"
},
{
"DOI": "10.1016/j.gde.2005.07.003",
"author": "J Hirayama",
"doi-asserted-by": "publisher",
"first-page": "548",
"issue": "5",
"journal-title": "Curr Opin Genet Dev",
"key": "728_CR182",
"unstructured": "Hirayama J, Sassone-Corsi P. Structural and functional features of transcription factors controlling the circadian clock. Curr Opin Genet Dev. 2005;15(5):548–56.",
"volume": "15",
"year": "2005"
},
{
"DOI": "10.1038/nature11048",
"author": "H Cho",
"doi-asserted-by": "publisher",
"first-page": "123",
"issue": "7396",
"journal-title": "Nature",
"key": "728_CR183",
"unstructured": "Cho H, et al. Regulation of circadian behaviour and metabolism by REV-ERB-α and REV-ERB-β. Nature. 2012;485(7396):123–7.",
"volume": "485",
"year": "2012"
},
{
"DOI": "10.3132/dvdr.2008.0014",
"author": "H Duez",
"doi-asserted-by": "publisher",
"first-page": "82",
"issue": "2",
"journal-title": "Diab Vasc Dis Res",
"key": "728_CR184",
"unstructured": "Duez H, Staels B. The nuclear receptors Rev-erbs and RORs integrate circadian rhythms and metabolism. Diab Vasc Dis Res. 2008;5(2):82–8.",
"volume": "5",
"year": "2008"
},
{
"DOI": "10.1038/s41598-019-55663-0",
"author": "MC Beker",
"doi-asserted-by": "publisher",
"first-page": "19082",
"issue": "1",
"journal-title": "Sci Rep",
"key": "728_CR185",
"unstructured": "Beker MC, et al. Interaction of melatonin and Bmal1 in the regulation of PI3K/AKT pathway components and cellular survival. Sci Rep. 2019;9(1):19082.",
"volume": "9",
"year": "2019"
},
{
"DOI": "10.1074/jbc.M108890200",
"author": "D Roy",
"doi-asserted-by": "publisher",
"first-page": "251",
"issue": "1",
"journal-title": "J Biol Chem",
"key": "728_CR186",
"unstructured": "Roy D, Belsham DD. Melatonin receptor activation regulates GnRH Gene expression and secretion in GT1–7 GnRH neurons: signal transduction mechanisms. J Biol Chem. 2002;277(1):251–8.",
"volume": "277",
"year": "2002"
},
{
"DOI": "10.3109/07853899808999391",
"author": "RJ Reiter",
"doi-asserted-by": "publisher",
"first-page": "103",
"issue": "1",
"journal-title": "Ann Med",
"key": "728_CR187",
"unstructured": "Reiter RJ. Melatonin and human reproduction. Ann Med. 1998;30(1):103–8.",
"volume": "30",
"year": "1998"
},
{
"DOI": "10.1016/S0140-6736(84)90412-4",
"author": "F Waldhauser",
"doi-asserted-by": "publisher",
"first-page": "362",
"issue": "8373",
"journal-title": "Lancet",
"key": "728_CR188",
"unstructured": "Waldhauser F, et al. Fall in nocturnal serum melatonin during prepuberty and pubescence. Lancet. 1984;323(8373):362–5.",
"volume": "323",
"year": "1984"
},
{
"author": "M Wójtowicz",
"first-page": "1231",
"issue": "12",
"journal-title": "Ginekol Pol",
"key": "728_CR189",
"unstructured": "Wójtowicz M, Jakiel G. Melatonin and its role in human reproduction. Ginekol Pol. 2002;73(12):1231–7.",
"volume": "73",
"year": "2002"
},
{
"DOI": "10.3389/fendo.2020.00085",
"author": "JM Olcese",
"doi-asserted-by": "publisher",
"first-page": "85",
"journal-title": "Front Endocrinol",
"key": "728_CR190",
"unstructured": "Olcese JM. Melatonin and female reproduction: an expanding universe. Front Endocrinol. 2020;11:85.",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1016/j.cryobiol.2020.01.018",
"author": "T-C Sun",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Cryobiology",
"key": "728_CR191",
"unstructured": "Sun T-C, et al. Protective effects of melatonin on male fertility preservation and reproductive system. Cryobiology. 2020;95:1–8.",
"volume": "95",
"year": "2020"
},
{
"DOI": "10.1074/jbc.274.31.22041",
"author": "JA Roth",
"doi-asserted-by": "publisher",
"first-page": "22041",
"issue": "31",
"journal-title": "J Biol Chem",
"key": "728_CR192",
"unstructured": "Roth JA, et al. Melatonin promotes osteoblast differentiation and bone formation*. J Biol Chem. 1999;274(31):22041–7.",
"volume": "274",
"year": "1999"
},
{
"DOI": "10.1111/j.1600-079X.2010.00803.x",
"author": "L Zhang",
"doi-asserted-by": "publisher",
"first-page": "364",
"issue": "4",
"journal-title": "J Pineal Res",
"key": "728_CR193",
"unstructured": "Zhang L, et al. Melatonin inhibits adipogenesis and enhances osteogenesis of human mesenchymal stem cells by suppressing PPARγ expression and enhancing Runx2 expression. J Pineal Res. 2010;49(4):364–72.",
"volume": "49",
"year": "2010"
},
{
"DOI": "10.1016/S0002-9149(99)00112-5",
"author": "S Arangino",
"doi-asserted-by": "publisher",
"first-page": "1417",
"issue": "9",
"journal-title": "Am J Cardiol",
"key": "728_CR194",
"unstructured": "Arangino S, et al. Effects of melatonin on vascular reactivity, catecholamine levels, and blood pressure in healthy men. Am J Cardiol. 1999;83(9):1417–9.",
"volume": "83",
"year": "1999"
},
{
"DOI": "10.1155/2013/521783",
"author": "LA Campos",
"doi-asserted-by": "publisher",
"first-page": "521783",
"journal-title": "Int J Hypertens",
"key": "728_CR195",
"unstructured": "Campos LA, et al. The angiotensin-melatonin axis. Int J Hypertens. 2013;2013:521783.",
"volume": "2013",
"year": "2013"
},
{
"DOI": "10.1152/ajpheart.1998.275.1.H139",
"author": "O Régrigny",
"doi-asserted-by": "publisher",
"first-page": "H139",
"issue": "1",
"journal-title": "Am J Physiology-Heart Circulatory Physiol",
"key": "728_CR196",
"unstructured": "Régrigny O, et al. Melatonin improves cerebral circulation security margin in rats. Am J Physiology-Heart Circulatory Physiol. 1998;275(1):H139–44.",
"volume": "275",
"year": "1998"
},
{
"DOI": "10.1016/j.ygcen.2020.113693",
"author": "F Yasmin",
"doi-asserted-by": "publisher",
"first-page": "113693",
"journal-title": "Gen Comp Endocrinol",
"key": "728_CR197",
"unstructured": "Yasmin F, et al. Gut melatonin: a potent candidate in the diversified journey of melatonin research. Gen Comp Endocrinol. 2021;303:113693.",
"volume": "303",
"year": "2021"
},
{
"DOI": "10.1016/0169-328X(96)00017-4",
"author": "C Mazzucchelli",
"doi-asserted-by": "publisher",
"first-page": "117",
"issue": "1–2",
"journal-title": "Mol Brain Res",
"key": "728_CR198",
"unstructured": "Mazzucchelli C, et al. The melatonin receptor in the human brain: cloning experiments and distribution studies. Mol Brain Res. 1996;39(1–2):117–26.",
"volume": "39",
"year": "1996"
},
{
"DOI": "10.1016/j.pneurobio.2008.04.001",
"author": "SR Pandi-Perumal",
"doi-asserted-by": "publisher",
"first-page": "335",
"issue": "3",
"journal-title": "Prog Neurobiol",
"key": "728_CR199",
"unstructured": "Pandi-Perumal SR, et al. Physiological effects of melatonin: role of melatonin receptors and signal transduction pathways. Prog Neurobiol. 2008;85(3):335–53.",
"volume": "85",
"year": "2008"
},
{
"DOI": "10.1007/s00429-014-0719-7",
"author": "RJ Reiter",
"doi-asserted-by": "publisher",
"first-page": "1873",
"journal-title": "Brain Struct Funct",
"key": "728_CR200",
"unstructured": "Reiter RJ, et al. Delivery of pineal melatonin to the brain and SCN: role of canaliculi, cerebrospinal fluid, tanycytes and Virchow-Robin perivascular spaces. Brain Struct Funct. 2014;219:1873–87.",
"volume": "219",
"year": "2014"
},
{
"DOI": "10.1007/s00429-017-1439-6",
"author": "KY Ng",
"doi-asserted-by": "publisher",
"first-page": "2921",
"journal-title": "Brain Struct Funct",
"key": "728_CR201",
"unstructured": "Ng KY, et al. Melatonin receptors: distribution in mammalian brain and their respective putative functions. Brain Struct Funct. 2017;222:2921–39.",
"volume": "222",
"year": "2017"
},
{
"DOI": "10.1159/000121744",
"author": "I Nir",
"doi-asserted-by": "publisher",
"first-page": "122",
"issue": "2",
"journal-title": "Neuroendocrinology",
"key": "728_CR202",
"unstructured": "Nir I, et al. Changes in the electrical activity of the brain following pinealectomy. Neuroendocrinology. 1969;4(2):122–7.",
"volume": "4",
"year": "1969"
},
{
"key": "728_CR203",
"unstructured": "Bindoni M, Rizzo R. Effects of electrolytic lesions of the pineal gland on the electric activity of some brain structures in the rabbit. Bollettino Della Societa Italiana di Biologia Sperimentale. 1964;40(24): p. Suppl: 2010–3."
},
{
"DOI": "10.1016/0304-3940(76)90085-9",
"author": "RG Fariello",
"doi-asserted-by": "publisher",
"first-page": "151",
"issue": "3",
"journal-title": "Neurosci Lett",
"key": "728_CR204",
"unstructured": "Fariello RG, Bubenik GA. Melatonin-induced changes in the sensory activation of acute epileptic foci. Neurosci Lett. 1976;3(3):151–5.",
"volume": "3",
"year": "1976"
},
{
"author": "B Stankov",
"first-page": "2152",
"issue": "4",
"journal-title": "Endocrinology",
"key": "728_CR205",
"unstructured": "Stankov B, et al. Melatonin signal transduction and mechanism of action in the central nervous system: using the rabbit cortex as a model. Endocrinology. 1992;130(4):2152–9.",
"volume": "130",
"year": "1992"
},
{
"DOI": "10.1007/s00213-023-06312-y",
"author": "Z Xu",
"doi-asserted-by": "publisher",
"first-page": "259",
"issue": "2",
"journal-title": "Psychopharmacology",
"key": "728_CR206",
"unstructured": "Xu Z, et al. Melatonin alleviates PTSD-like behaviors and restores serum GABA and cortisol levels in mice. Psychopharmacology. 2023;240(2):259–69.",
"volume": "240",
"year": "2023"
},
{
"author": "G Pierrefiche",
"first-page": "131",
"issue": "2",
"journal-title": "Res Commun Chem Pathol Pharmacol",
"key": "728_CR207",
"unstructured": "Pierrefiche G, Zerbib R, Laborit H. Anxiolytic activity of melatonin in mice: involvement of benzodiazepine receptors. Res Commun Chem Pathol Pharmacol. 1993;82(2):131–42.",
"volume": "82",
"year": "1993"
},
{
"DOI": "10.1016/S0006-8993(99)01520-6",
"author": "V Raghavendra",
"doi-asserted-by": "publisher",
"first-page": "178",
"issue": "1–2",
"journal-title": "Brain Res",
"key": "728_CR208",
"unstructured": "Raghavendra V, Kulkarni SK. Reversal of morphine tolerance and dependence by melatonin: possible role of central and peripheral benzodiazepine receptors. Brain Res. 1999;834(1–2):178–81.",
"volume": "834",
"year": "1999"
},
{
"DOI": "10.1016/S0924-977X(00)00115-2",
"author": "V Raghavendra",
"doi-asserted-by": "publisher",
"first-page": "473",
"issue": "6",
"journal-title": "Eur Neuropsychopharmacol",
"key": "728_CR209",
"unstructured": "Raghavendra V, Kaur G, Kulkarni SK. Anti-depressant action of melatonin in chronic forced swimming-induced behavioral despair in mice, role of peripheral benzodiazepine receptor modulation. Eur Neuropsychopharmacol. 2000;10(6):473–81.",
"volume": "10",
"year": "2000"
},
{
"DOI": "10.1111/j.1600-079X.1995.tb00171.x",
"author": "D Acufla-Castroviejo",
"doi-asserted-by": "publisher",
"first-page": "57",
"issue": "2",
"journal-title": "J Pineal Res",
"key": "728_CR210",
"unstructured": "Acufla-Castroviejo D, et al. Minireview: Cell protective role of melatonin in the brain. J Pineal Res. 1995;19(2):57–63.",
"volume": "19",
"year": "1995"
},
{
"DOI": "10.1615/JEnvironPatholToxicolOncol.2016016399",
"doi-asserted-by": "crossref",
"key": "728_CR211",
"unstructured": "Vishnoi S, Raisuddin S, Parvez S. Glutamate excitotoxicity and oxidative stress in epilepsy: modulatory role of melatonin. J Environ Pathol Toxicol Oncol. 2016. 35(4)."
},
{
"DOI": "10.1016/S0301-0082(98)00052-5",
"author": "RJ Reiter",
"doi-asserted-by": "publisher",
"first-page": "359",
"issue": "3",
"journal-title": "Prog Neurobiol",
"key": "728_CR212",
"unstructured": "Reiter RJ. Oxidative damage in the central nervous system: protection by melatonin. Prog Neurobiol. 1998;56(3):359–84.",
"volume": "56",
"year": "1998"
},
{
"DOI": "10.1046/j.1365-2826.1998.00203.x",
"author": "J Leon",
"doi-asserted-by": "publisher",
"first-page": "297",
"issue": "4",
"journal-title": "J Neuroendocrinol",
"key": "728_CR213",
"unstructured": "Leon J, et al. Modification of nitric oxide synthase activity and neuronal response in rat striatum by melatonin and kynurenine derivatives. J Neuroendocrinol. 1998;10(4):297–302.",
"volume": "10",
"year": "1998"
},
{
"DOI": "10.1124/mol.58.5.967",
"author": "J León",
"doi-asserted-by": "publisher",
"first-page": "967",
"issue": "5",
"journal-title": "Mol Pharmacol",
"key": "728_CR214",
"unstructured": "León J, et al. Structure-related inhibition of calmodulin-dependent neuronal nitric-oxide synthase activity by melatonin and synthetic kynurenines. Mol Pharmacol. 2000;58(5):967–75.",
"volume": "58",
"year": "2000"
},
{
"DOI": "10.1016/j.neulet.2005.09.040",
"author": "J Larson",
"doi-asserted-by": "publisher",
"first-page": "23",
"issue": "1",
"journal-title": "Neurosci Lett",
"key": "728_CR215",
"unstructured": "Larson J, et al. Impaired hippocampal long-term potentiation in melatonin MT2 receptor-deficient mice. Neurosci Lett. 2006;393(1):23–6.",
"volume": "393",
"year": "2006"
},
{
"DOI": "10.1111/jpi.12553",
"author": "A Jilg",
"doi-asserted-by": "publisher",
"first-page": "e12553",
"issue": "3",
"journal-title": "J Pineal Res",
"key": "728_CR216",
"unstructured": "Jilg A, et al. Melatonin modulates daytime-dependent synaptic plasticity and learning efficiency. J Pineal Res. 2019;66(3):e12553.",
"volume": "66",
"year": "2019"
},
{
"DOI": "10.1210/er.2018-00084",
"author": "J Cipolla-Neto",
"doi-asserted-by": "publisher",
"first-page": "990",
"issue": "6",
"journal-title": "Endocrine Rev",
"key": "728_CR217",
"unstructured": "Cipolla-Neto J, Amaral FGD. Melatonin as a hormone: new physiological and clinical insights. Endocrine Rev. 2018;39(6):990–1028.",
"volume": "39",
"year": "2018"
},
{
"DOI": "10.1007/s40261-015-0368-5",
"author": "LPH Andersen",
"doi-asserted-by": "publisher",
"first-page": "169",
"journal-title": "Clin Drug Investig",
"key": "728_CR218",
"unstructured": "Andersen LPH, et al. The safety of melatonin in humans. Clin Drug Investig. 2016;36:169–75.",
"volume": "36",
"year": "2016"
},
{
"DOI": "10.1080/14740338.2022.2160444",
"author": "FM Besag",
"doi-asserted-by": "publisher",
"first-page": "1469",
"issue": "12",
"journal-title": "Expert Opin Drug Saf",
"key": "728_CR219",
"unstructured": "Besag FM, Vasey MJ. Adverse events in long-term studies of exogenous melatonin. Expert Opin Drug Saf. 2022;21(12):1469–81.",
"volume": "21",
"year": "2022"
},
{
"DOI": "10.1016/j.physbeh.2014.04.016",
"author": "E Papagiannidou",
"doi-asserted-by": "publisher",
"first-page": "17",
"journal-title": "Physiol Behav",
"key": "728_CR220",
"unstructured": "Papagiannidou E, Skene DJ, Ioannides C. Potential drug interactions with melatonin. Physiol Behav. 2014;131:17–24.",
"volume": "131",
"year": "2014"
},
{
"author": "NI Ashy",
"first-page": "124",
"issue": "6",
"journal-title": "Life Sci J",
"key": "728_CR221",
"unstructured": "Ashy NI, Shroff KV, Ashy N. Evaluation of the potential drug interaction of melatonin and warfarin: a case series. Life Sci J. 2016;13(6):124.",
"volume": "13",
"year": "2016"
},
{
"DOI": "10.1016/j.lfs.2022.120866",
"author": "A Hosseinzadeh",
"doi-asserted-by": "publisher",
"first-page": "120866",
"journal-title": "Life Sci",
"key": "728_CR222",
"unstructured": "Hosseinzadeh A, et al. Melatonin effect on platelets and coagulation: Implications for a prophylactic indication in COVID-19. Life Sci. 2022;307:120866.",
"volume": "307",
"year": "2022"
},
{
"DOI": "10.1080/01616412.2017.1315864",
"author": "Z Xie",
"doi-asserted-by": "publisher",
"first-page": "559",
"issue": "6",
"journal-title": "Neurol Res",
"key": "728_CR223",
"unstructured": "Xie Z, et al. A review of sleep disorders and melatonin. Neurol Res. 2017;39(6):559–65.",
"volume": "39",
"year": "2017"
},
{
"DOI": "10.1002/14651858.CD001520",
"doi-asserted-by": "crossref",
"key": "728_CR224",
"unstructured": "Herxheimer A, Petrie KJ, C.C.M.D. Group. Melatonin for the prevention and treatment of jet lag. Cochrane Database Syst Rev. 1996;2010(1)."
},
{
"DOI": "10.1210/jcem-73-4-793",
"author": "F Waldhauser",
"doi-asserted-by": "publisher",
"first-page": "793",
"issue": "4",
"journal-title": "J Clin Endocrinol Metab",
"key": "728_CR225",
"unstructured": "Waldhauser F, et al. Serum melatonin in central precocious puberty is lower than in age-matched prepubertal children. J Clin Endocrinol Metab. 1991;73(4):793–6.",
"volume": "73",
"year": "1991"
},
{
"DOI": "10.1016/j.fertnstert.2008.05.016",
"author": "H Tamura",
"doi-asserted-by": "publisher",
"first-page": "328",
"issue": "1",
"journal-title": "Fertil Steril",
"key": "728_CR226",
"unstructured": "Tamura H, et al. Melatonin and the ovary: physiological and pathophysiological implications. Fertil Steril. 2009;92(1):328–43.",
"volume": "92",
"year": "2009"
},
{
"DOI": "10.1016/S0140-6736(95)92600-3",
"author": "P Brugger",
"doi-asserted-by": "publisher",
"first-page": "1408",
"issue": "8962",
"journal-title": "Lancet",
"key": "728_CR227",
"unstructured": "Brugger P, Marktl W, Herold M. Impaired nocturnal secretion of melatonin in coronary heart disease. Lancet. 1995;345(8962):1408.",
"volume": "345",
"year": "1995"
},
{
"DOI": "10.3389/fnins.2022.825246",
"author": "S Fowler",
"doi-asserted-by": "publisher",
"first-page": "825246",
"journal-title": "Front Neurosci",
"key": "728_CR228",
"unstructured": "Fowler S, et al. Circadian rhythms and melatonin metabolism in patients with disorders of gut-brain interactions. Front Neurosci. 2022;16:825246.",
"volume": "16",
"year": "2022"
},
{
"DOI": "10.1002/jcp.29036",
"author": "F Moradkhani",
"doi-asserted-by": "publisher",
"first-page": "745",
"issue": "2",
"journal-title": "J Cell Physiol",
"key": "728_CR229",
"unstructured": "Moradkhani F, et al. Immunoregulatory role of melatonin in cancer. J Cell Physiol. 2020;235(2):745–57.",
"volume": "235",
"year": "2020"
},
{
"DOI": "10.1016/j.biochi.2022.01.001",
"doi-asserted-by": "crossref",
"key": "728_CR230",
"unstructured": "Patel R. et al. Diabetes mellitus and melatonin: where are we? Biochimie. 2022."
},
{
"DOI": "10.1111/jpi.12137",
"author": "J Cipolla-Neto",
"doi-asserted-by": "publisher",
"first-page": "371",
"issue": "4",
"journal-title": "J Pineal Res",
"key": "728_CR231",
"unstructured": "Cipolla-Neto J, et al. Melatonin, energy metabolism, and obesity: a review. J Pineal Res. 2014;56(4):371–81.",
"volume": "56",
"year": "2014"
},
{
"DOI": "10.3390/ijms24054803",
"author": "Y Potes",
"doi-asserted-by": "publisher",
"first-page": "4803",
"issue": "5",
"journal-title": "Int J Mol Sci",
"key": "728_CR232",
"unstructured": "Potes Y, et al. Benefits of the neurogenic potential of melatonin for treating neurological and neuropsychiatric disorders. Int J Mol Sci. 2023;24(5):4803.",
"volume": "24",
"year": "2023"
},
{
"DOI": "10.1677/joe.0.0910467",
"author": "Y Touitou",
"doi-asserted-by": "publisher",
"first-page": "467",
"issue": "3",
"journal-title": "J Endocrinol",
"key": "728_CR233",
"unstructured": "Touitou Y, et al. Age-and mental health-related circadian rhythms of plasma levels of melatonin, prolactin, luteinizing hormone and follicle-stimulating hormone in man. J Endocrinol. 1981;91(3):467–75.",
"volume": "91",
"year": "1981"
},
{
"DOI": "10.1210/jcem-55-1-27",
"author": "H Iguchi",
"doi-asserted-by": "publisher",
"first-page": "27",
"issue": "1",
"journal-title": "J Clin Endocrinol Metab",
"key": "728_CR234",
"unstructured": "Iguchi H, Kato K-I, Ibayashi H. Age-dependent reduction in serum melatonin concentrations in healthy human subjects. J Clin Endocrinol Metab. 1982;55(1):27–9.",
"volume": "55",
"year": "1982"
},
{
"DOI": "10.1159/000212774",
"author": "Y Touitou",
"doi-asserted-by": "publisher",
"first-page": "110",
"issue": "2",
"journal-title": "Gerontology",
"key": "728_CR235",
"unstructured": "Touitou Y, et al. Age-related changes in both circadian and seasonal rhythms of rectal temperature with special reference to senile dementia of Alzheimer type. Gerontology. 1986;32(2):110–8.",
"volume": "32",
"year": "1986"
},
{
"DOI": "10.3109/07420529709001459",
"author": "F Magri",
"doi-asserted-by": "publisher",
"first-page": "385",
"issue": "4",
"journal-title": "Chronobiol Int",
"key": "728_CR236",
"unstructured": "Magri F, et al. Changes in endocrine orcadian rhythms as markers of physiological and pathological brain aging. Chronobiol Int. 1997;14(4):385–96.",
"volume": "14",
"year": "1997"
},
{
"DOI": "10.1089/rej.2013.1542",
"author": "IF Tresguerres",
"doi-asserted-by": "publisher",
"first-page": "341",
"issue": "4",
"journal-title": "Rejuvenation Res",
"key": "728_CR237",
"unstructured": "Tresguerres IF, et al. Melatonin dietary supplement as an anti-aging therapy for age-related bone loss. Rejuvenation Res. 2014;17(4):341–6.",
"volume": "17",
"year": "2014"
},
{
"DOI": "10.1111/j.1749-6632.1994.tb56850.x",
"author": "VA Lesnikov",
"doi-asserted-by": "publisher",
"first-page": "456",
"journal-title": "Ann N Y Acad Sci",
"key": "728_CR238",
"unstructured": "Lesnikov VA, Pierpaoli W. Pineal cross-transplantation (old-to-young and vice versa) as evidence for an endogenous\" aging clock\". Ann N Y Acad Sci. 1994;719:456–60.",
"volume": "719",
"year": "1994"
},
{
"DOI": "10.1111/j.1749-6632.1994.tb56841.x",
"author": "MC Caroleo",
"doi-asserted-by": "publisher",
"first-page": "343",
"journal-title": "Ann N Y Acad Sci",
"key": "728_CR239",
"unstructured": "Caroleo MC, Doria G, Nistico G. Melatonin restores immunodepression in aged and cyclophosphamide-treated mice. Ann N Y Acad Sci. 1994;719:343–52.",
"volume": "719",
"year": "1994"
},
{
"DOI": "10.1111/j.1600-079X.2011.00912.x",
"author": "DY Yoo",
"doi-asserted-by": "publisher",
"first-page": "21",
"issue": "1",
"journal-title": "J Pineal Res",
"key": "728_CR240",
"unstructured": "Yoo DY, et al. Melatonin improves D-galactose-induced aging effects on behavior, neurogenesis, and lipid peroxidation in the mouse dentate gyrus via increasing pCREB expression. J Pineal Res. 2012;52(1):21–8.",
"volume": "52",
"year": "2012"
},
{
"DOI": "10.3390/molecules27175543",
"author": "C Cachán-Vega",
"doi-asserted-by": "publisher",
"first-page": "5543",
"issue": "17",
"journal-title": "Molecules",
"key": "728_CR241",
"unstructured": "Cachán-Vega C, et al. Chronic treatment with melatonin improves hippocampal neurogenesis in the aged brain and under neurodegeneration. Molecules. 2022;27(17):5543.",
"volume": "27",
"year": "2022"
},
{
"DOI": "10.1016/j.pneurobio.2015.02.001",
"author": "R Hardeland",
"doi-asserted-by": "publisher",
"first-page": "46",
"journal-title": "Prog Neurobiol",
"key": "728_CR242",
"unstructured": "Hardeland R, et al. Melatonin and brain inflammaging. Prog Neurobiol. 2015;127:46–63.",
"volume": "127",
"year": "2015"
},
{
"DOI": "10.1007/s42977-021-00102-3",
"doi-asserted-by": "crossref",
"key": "728_CR243",
"unstructured": "Keskin-Aktan A et al. SIRT2 and FOXO3a expressions in the cerebral cortex and hippocampus of young and aged male rats: antioxidant and anti-apoptotic effects of melatonin. Biologia Futura. 2022:1–15."
},
{
"DOI": "10.1111/j.1365-2869.2007.00613.x",
"author": "P Lemoine",
"doi-asserted-by": "publisher",
"first-page": "372",
"issue": "4",
"journal-title": "J Sleep Res",
"key": "728_CR244",
"unstructured": "Lemoine P, et al. Prolonged-release melatonin improves sleep quality and morning alertness in insomnia patients aged 55 years and older and has no withdrawal effects. J Sleep Res. 2007;16(4):372–80.",
"volume": "16",
"year": "2007"
},
{
"DOI": "10.1016/j.jclinane.2017.03.023",
"author": "Y Fan",
"doi-asserted-by": "publisher",
"first-page": "77",
"journal-title": "J Clin Anesth",
"key": "728_CR245",
"unstructured": "Fan Y, et al. The effect of melatonin on early postoperative cognitive decline in elderly patients undergoing hip arthroplasty: a randomized controlled trial. J Clin Anesth. 2017;39:77–81.",
"volume": "39",
"year": "2017"
},
{
"DOI": "10.1111/j.1600-079X.2007.00491.x",
"author": "AM Furio",
"doi-asserted-by": "publisher",
"first-page": "404",
"issue": "4",
"journal-title": "J Pineal Res",
"key": "728_CR246",
"unstructured": "Furio AM, Brusco LI, Cardinali DP. Possible therapeutic value of melatonin in mild cognitive impairment: a retrospective study. J Pineal Res. 2007;43(4):404–9.",
"volume": "43",
"year": "2007"
},
{
"DOI": "10.1186/s13024-015-0027-6",
"author": "G O’Neal-Moffitt",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "Mol Neurodegener",
"key": "728_CR247",
"unstructured": "O’Neal-Moffitt G, et al. Prophylactic melatonin significantly reduces Alzheimer’s neuropathology and associated cognitive deficits independent of antioxidant pathways in AβPPswe/PS1 mice. Mol Neurodegener. 2015;10(1):1–21.",
"volume": "10",
"year": "2015"
},
{
"DOI": "10.1016/j.bbr.2020.113100",
"author": "S Labban",
"doi-asserted-by": "publisher",
"first-page": "113100",
"journal-title": "Behav Brain Res",
"key": "728_CR248",
"unstructured": "Labban S, et al. Effects of melatonin and resveratrol on recognition memory and passive avoidance performance in a mouse model of Alzheimer’s disease. Behav Brain Res. 2021;402:113100.",
"volume": "402",
"year": "2021"
},
{
"DOI": "10.1002/biof.1369",
"author": "L Nie",
"doi-asserted-by": "publisher",
"first-page": "593",
"issue": "4",
"journal-title": "BioFactors",
"key": "728_CR249",
"unstructured": "Nie L, et al. Melatonin ameliorates anxiety and depression-like behaviors and modulates proteomic changes in triple transgenic mice of Alzheimer’s disease. BioFactors. 2017;43(4):593–611.",
"volume": "43",
"year": "2017"
},
{
"DOI": "10.1016/j.pbb.2011.06.026",
"author": "G Patki",
"doi-asserted-by": "publisher",
"first-page": "704",
"issue": "4",
"journal-title": "Pharmacol Biochem Behav",
"key": "728_CR250",
"unstructured": "Patki G, Lau Y-S. Melatonin protects against neurobehavioral and mitochondrial deficits in a chronic mouse model of Parkinson’s disease. Pharmacol Biochem Behav. 2011;99(4):704–11.",
"volume": "99",
"year": "2011"
},
{
"DOI": "10.1016/S0006-8993(02)02551-9",
"doi-asserted-by": "crossref",
"key": "728_CR251",
"unstructured": "Antolı́n, I., et al., Protective effect of melatonin in a chronic experimental model of Parkinson’s disease. Brain research, 2002. 943(2): p. 163–173."
},
{
"DOI": "10.1111/jpi.12212",
"author": "A Naskar",
"doi-asserted-by": "publisher",
"first-page": "262",
"issue": "3",
"journal-title": "J Pineal Res",
"key": "728_CR252",
"unstructured": "Naskar A, et al. Melatonin enhances L-DOPA therapeutic effects, helps to reduce its dose, and protects dopaminergic neurons in 1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine-induced Parkinsonism in mice. J Pineal Res. 2015;58(3):262–74.",
"volume": "58",
"year": "2015"
},
{
"DOI": "10.1038/s41598-022-20164-0",
"author": "Y Jand",
"doi-asserted-by": "publisher",
"first-page": "15963",
"issue": "1",
"journal-title": "Sci Rep",
"key": "728_CR253",
"unstructured": "Jand Y, et al. Melatonin ameliorates disease severity in a mouse model of multiple sclerosis by modulating the kynurenine pathway. Sci Rep. 2022;12(1):15963.",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1007/s12035-022-02875-7",
"author": "X Shen",
"doi-asserted-by": "publisher",
"first-page": "4747",
"issue": "8",
"journal-title": "Mol Neurobiol",
"key": "728_CR254",
"unstructured": "Shen X, et al. Melatonin induces autophagy in amyotrophic lateral sclerosis mice via upregulation of SIRT1. Mol Neurobiol. 2022;59(8):4747–60.",
"volume": "59",
"year": "2022"
},
{
"DOI": "10.2174/1570159X20666220420122322",
"author": "P-T Tseng",
"doi-asserted-by": "publisher",
"first-page": "1816",
"issue": "10",
"journal-title": "Curr Neuropharmacol",
"key": "728_CR255",
"unstructured": "Tseng P-T, et al. The dose and duration-dependent association between melatonin treatment and overall cognition in Alzheimer’s dementia: a network meta-analysis of randomized placebo-controlled trials. Curr Neuropharmacol. 2022;20(10):1816.",
"volume": "20",
"year": "2022"
},
{
"author": "K Alagiakrishnan",
"first-page": "363",
"issue": "117",
"journal-title": "Discov Med",
"key": "728_CR256",
"unstructured": "Alagiakrishnan K. Melatonin based therapies for delirium and dementia. Discov Med. 2016;21(117):363–71.",
"volume": "21",
"year": "2016"
},
{
"DOI": "10.3233/JAD-210562",
"author": "A Nous",
"doi-asserted-by": "publisher",
"first-page": "693",
"issue": "2",
"journal-title": "J Alzheimers Dis",
"key": "728_CR257",
"unstructured": "Nous A, et al. Serum daytime melatonin levels reflect cerebrospinal fluid melatonin levels in Alzheimer’s disease but are not correlated with cognitive decline. J Alzheimers Dis. 2021;83(2):693–704.",
"volume": "83",
"year": "2021"
},
{
"DOI": "10.9758/cpn.2021.19.1.135",
"author": "CH Lin",
"doi-asserted-by": "publisher",
"first-page": "135",
"issue": "1",
"journal-title": "Clin Psychopharmacol Neurosci",
"key": "728_CR258",
"unstructured": "Lin CH, Chiu CC, Lane HY. Trough Melatonin Levels Differ between Early and Late Phases of Alzheimer Disease. Clin Psychopharmacol Neurosci. 2021;19(1):135–44.",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1210/jc.2015-1859",
"author": "K Obayashi",
"doi-asserted-by": "publisher",
"first-page": "3090",
"issue": "8",
"journal-title": "J Clin Endocrinol Metab",
"key": "728_CR259",
"unstructured": "Obayashi K, et al. Physiological levels of melatonin relate to cognitive function and depressive symptoms: the HEIJO-KYO cohort. J Clin Endocrinol Metab. 2015;100(8):3090–6.",
"volume": "100",
"year": "2015"
},
{
"DOI": "10.1016/j.clineuro.2020.105878",
"author": "R Daneshvar Kakhaki",
"doi-asserted-by": "publisher",
"first-page": "105878",
"journal-title": "Clin Neurol Neurosurg",
"key": "728_CR260",
"unstructured": "Daneshvar Kakhaki R, et al. Melatonin supplementation and the effects on clinical and metabolic status in Parkinson’s disease: A randomized, double-blind, placebo-controlled trial. Clin Neurol Neurosurg. 2020;195:105878.",
"volume": "195",
"year": "2020"
},
{
"key": "728_CR261",
"unstructured": "Jallouli S et al. Effect of melatonin intake on postural balance, functional mobility and fall risk in persons with multiple sclerosis: a pilot study. Int J Neurosci. 2022:1–11."
},
{
"DOI": "10.1002/mus.27168",
"author": "EM Bald",
"doi-asserted-by": "publisher",
"first-page": "572",
"issue": "4",
"journal-title": "Muscle Nerve",
"key": "728_CR262",
"unstructured": "Bald EM, Nance CS, Schultz JL. Melatonin may slow disease progression in amyotrophic lateral sclerosis: findings from the Pooled Resource Open-Access ALS Clinic Trials database. Muscle Nerve. 2021;63(4):572–6.",
"volume": "63",
"year": "2021"
},
{
"DOI": "10.1002/rmv.1714",
"author": "JA Boga",
"doi-asserted-by": "publisher",
"first-page": "323",
"issue": "5",
"journal-title": "Rev Med Virol",
"key": "728_CR263",
"unstructured": "Boga JA, et al. Beneficial actions of melatonin in the management of viral infections: a new use for this “molecular handyman”? Rev Med Virol. 2012;22(5):323–38.",
"volume": "22",
"year": "2012"
},
{
"DOI": "10.1007/s000180050051",
"author": "E Bonilla",
"doi-asserted-by": "publisher",
"first-page": "430",
"journal-title": "Cell Mol Life Sci CMLS",
"key": "728_CR264",
"unstructured": "Bonilla E, et al. Melatonin protects mice infected with Venezuelan equine encephalomyelitis virus. Cell Mol Life Sci CMLS. 1997;53:430–4.",
"volume": "53",
"year": "1997"
},
{
"DOI": "10.1046/j.1600-079X.2003.00105.x",
"author": "E Bonilla",
"doi-asserted-by": "publisher",
"first-page": "73",
"issue": "2",
"journal-title": "J Pineal Res",
"key": "728_CR265",
"unstructured": "Bonilla E, et al. Melatonin and viral infections. J Pineal Res. 2004;36(2):73–9.",
"volume": "36",
"year": "2004"
},
{
"DOI": "10.1034/j.1600-079X.2003.00068.x",
"author": "SY Shiu",
"doi-asserted-by": "publisher",
"first-page": "69",
"issue": "1",
"journal-title": "J Pineal Res",
"key": "728_CR266",
"unstructured": "Shiu SY, et al. Urgent search for safe and effective treatments of severe acute respiratory syndrome: is melatonin a promising candidate drug? J Pineal Res. 2003;35(1):69.",
"volume": "35",
"year": "2003"
},
{
"DOI": "10.1111/jpi.12186",
"author": "D-X Tan",
"doi-asserted-by": "publisher",
"first-page": "381",
"issue": "4",
"journal-title": "J Pineal Res",
"key": "728_CR267",
"unstructured": "Tan D-X, et al. Ebola virus disease: potential use of melatonin as a treatment. J Pineal Res. 2014;57(4):381–4.",
"volume": "57",
"year": "2014"
},
{
"DOI": "10.1080/00365513.2023.2175236",
"author": "S Yılmaz",
"doi-asserted-by": "publisher",
"first-page": "86",
"issue": "2",
"journal-title": "Scand J Clin Lab Invest",
"key": "728_CR268",
"unstructured": "Yılmaz S, Öner P. Melatonin levels are low in COVID-19 positive patients and these levels are associated with depression, death anxiety and insomnia. Scand J Clin Lab Invest. 2023;83(2):86–94.",
"volume": "83",
"year": "2023"
},
{
"DOI": "10.1016/j.nut.2021.111308",
"author": "İ Eroğlu",
"doi-asserted-by": "publisher",
"journal-title": "Nutrition",
"key": "728_CR269",
"unstructured": "Eroğlu İ, Eroğlu BÇ, Güven GS. Altered tryptophan absorption and metabolism could underlie long-term symptoms in survivors of coronavirus disease 2019 (COVID-19). Nutrition. 2021;90: 111308.",
"volume": "90",
"year": "2021"
},
{
"DOI": "10.1016/j.arcmed.2021.06.006",
"author": "G Farnoosh",
"doi-asserted-by": "publisher",
"first-page": "79",
"issue": "1",
"journal-title": "Arch Med Res",
"key": "728_CR270",
"unstructured": "Farnoosh G, et al. Efficacy of a low dose of melatonin as an adjunctive therapy in hospitalized patients with COVID-19: a randomized, double-blind clinical trial. Arch Med Res. 2022;53(1):79–85.",
"volume": "53",
"year": "2022"
},
{
"DOI": "10.3122/jabfm.2022.04.210529",
"author": "C Fogleman",
"doi-asserted-by": "publisher",
"first-page": "695",
"issue": "4",
"journal-title": "J Am Board Fam Med",
"key": "728_CR271",
"unstructured": "Fogleman C, et al. A pilot of a randomized control trial of melatonin and vitamin C for mild-to-moderate COVID-19. J Am Board Fam Med. 2022;35(4):695–707.",
"volume": "35",
"year": "2022"
},
{
"DOI": "10.1007/s10787-022-01096-7",
"author": "A Ameri",
"doi-asserted-by": "publisher",
"first-page": "265",
"issue": "1",
"journal-title": "Inflammopharmacology",
"key": "728_CR272",
"unstructured": "Ameri A, et al. Efficacy and safety of oral melatonin in patients with severe COVID-19: a randomized controlled trial. Inflammopharmacology. 2023;31(1):265–74.",
"volume": "31",
"year": "2023"
},
{
"DOI": "10.1016/j.ijid.2021.10.012",
"author": "ZT Hasan",
"doi-asserted-by": "publisher",
"first-page": "79",
"journal-title": "Int J Infect Dis",
"key": "728_CR273",
"unstructured": "Hasan ZT, Atrakji D, Mehuaiden DAK. The effect of melatonin on thrombosis, sepsis and mortality rate in COVID-19 patients. Int J Infect Dis. 2022;114:79–84.",
"volume": "114",
"year": "2022"
},
{
"author": "M Darban",
"first-page": "164",
"journal-title": "J Cell Mol Anesth",
"key": "728_CR274",
"unstructured": "Darban M, et al. Efficacy of high dose vitamin C, melatonin and zinc in Iranian patients with acute respiratory syndrome due to coronavirus infection: a pilot randomized trial. J Cell Mol Anesth. 2021;6:164–7.",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.1093/jtm/taab195",
"author": "M Sánchez-Rico",
"doi-asserted-by": "publisher",
"first-page": "taab195",
"issue": "3",
"journal-title": "J Travel Med",
"key": "728_CR275",
"unstructured": "Sánchez-Rico M, et al. Melatonin does not reduce mortality in adult hospitalized patients with COVID-19: a multicenter retrospective observational study. J Travel Med. 2022;29(3):taab195.",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1016/j.chest.2021.07.541",
"author": "N Sahu",
"doi-asserted-by": "publisher",
"first-page": "A560",
"issue": "4",
"journal-title": "Chest",
"key": "728_CR276",
"unstructured": "Sahu N, et al. Retrospective review of melatonin in patients with COVID-19. Chest. 2021;160(4):A560.",
"volume": "160",
"year": "2021"
},
{
"DOI": "10.1016/j.heliyon.2022.e10906",
"doi-asserted-by": "crossref",
"key": "728_CR277",
"unstructured": "Faridzadeh A et al. The role of melatonin as an adjuvant in the treatment of COVID-19: a systematic review. Heliyon. 2022."
},
{
"DOI": "10.1007/s00018-022-04390-3",
"author": "E Cecon",
"doi-asserted-by": "publisher",
"first-page": "361",
"issue": "7",
"journal-title": "Cell Mol Life Sci",
"key": "728_CR278",
"unstructured": "Cecon E, et al. Melatonin drugs inhibit SARS-CoV-2 entry into the brain and virus-induced damage of cerebral small vessels. Cell Mol Life Sci. 2022;79(7):361.",
"volume": "79",
"year": "2022"
},
{
"DOI": "10.1016/j.sjbs.2022.01.049",
"author": "PK Yadalam",
"doi-asserted-by": "publisher",
"first-page": "3140",
"issue": "5",
"journal-title": "Saudi J Biol Sci",
"key": "728_CR279",
"unstructured": "Yadalam PK, et al. Assessing the therapeutic potential of agomelatine, ramelteon, and melatonin against SARS-CoV-2. Saudi J Biol Sci. 2022;29(5):3140–50.",
"volume": "29",
"year": "2022"
},
{
"DOI": "10.1111/jpi.12772",
"author": "E Cecon",
"doi-asserted-by": "publisher",
"first-page": "e12772",
"issue": "1",
"journal-title": "J Pineal Res",
"key": "728_CR280",
"unstructured": "Cecon E, et al. Therapeutic potential of melatonin and melatonergic drugs on K18-hACE2 mice infected with SARS-CoV-2. J Pineal Res. 2022;72(1):e12772.",
"volume": "72",
"year": "2022"
},
{
"DOI": "10.3390/antiox11010050",
"author": "P Kumar",
"doi-asserted-by": "publisher",
"first-page": "50",
"issue": "1",
"journal-title": "Antioxidants",
"key": "728_CR281",
"unstructured": "Kumar P, et al. Severe glutathione deficiency, oxidative stress and oxidant damage in adults hospitalized with COVID-19: implications for GlyNAC (glycine and N-acetylcysteine) supplementation. Antioxidants. 2022;11(1):50.",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1177/2050312121991246",
"author": "Y Muhammad",
"doi-asserted-by": "publisher",
"first-page": "205031212199124",
"journal-title": "SAGE Open Med",
"key": "728_CR282",
"unstructured": "Muhammad Y, et al. Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: a cross-sectional comparative study in Jigawa, Northwestern Nigeria. SAGE Open Med. 2021;9:2050312121991246.",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1038/s41420-020-00369-w",
"author": "M Yang",
"doi-asserted-by": "publisher",
"first-page": "130",
"issue": "1",
"journal-title": "Cell Death Discovery",
"key": "728_CR283",
"unstructured": "Yang M, Lai CL. SARS-CoV-2 infection: can ferroptosis be a potential treatment target for multiple organ involvement? Cell Death Discovery. 2020;6(1):130.",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.1016/j.bbi.2021.01.003",
"author": "Y Cui",
"doi-asserted-by": "publisher",
"first-page": "312",
"journal-title": "Brain Behav Immun",
"key": "728_CR284",
"unstructured": "Cui Y, et al. ACSL4 exacerbates ischemic stroke by promoting ferroptosis-induced brain injury and neuroinflammation. Brain Behav Immun. 2021;93:312–21.",
"volume": "93",
"year": "2021"
},
{
"DOI": "10.3389/fpsyt.2022.1035986",
"author": "OA Abulseoud",
"doi-asserted-by": "publisher",
"first-page": "1035986",
"journal-title": "Front Psychiatry",
"key": "728_CR285",
"unstructured": "Abulseoud OA, et al. Attenuated initial serum ferritin concentration in critically ill coronavirus disease 2019 geriatric patients with comorbid psychiatric conditions. Front Psychiatry. 2022;13:1035986.",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2023.1110540",
"author": "M Hortová-Kohoutková",
"doi-asserted-by": "publisher",
"first-page": "1110540",
"journal-title": "Front Immunol",
"key": "728_CR286",
"unstructured": "Hortová-Kohoutková M, et al. Hepcidin and ferritin levels as markers of immune cell activation during septic shock, severe COVID-19 and sterile inflammation. Front Immunol. 2023;14:1110540.",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1016/j.jtemb.2022.127109",
"author": "ACM Gaiatto",
"doi-asserted-by": "publisher",
"first-page": "127109",
"journal-title": "J Trace Elem Med Biol",
"key": "728_CR287",
"unstructured": "Gaiatto ACM, et al. COVID-19 compromises iron homeostasis: Transferrin as a target of investigation. J Trace Elem Med Biol. 2023;76:127109.",
"volume": "76",
"year": "2023"
},
{
"DOI": "10.1016/j.ijid.2021.12.340",
"author": "C Claise",
"doi-asserted-by": "publisher",
"first-page": "74",
"journal-title": "Int J Infect Dis",
"key": "728_CR288",
"unstructured": "Claise C, et al. Low transferrin levels predict heightened inflammation in patients with COVID-19: New insights. Int J Infect Dis. 2022;116:74–9.",
"volume": "116",
"year": "2022"
},
{
"DOI": "10.1016/j.jcrc.2021.09.023",
"author": "K Kaushal",
"doi-asserted-by": "publisher",
"first-page": "172",
"journal-title": "J Crit Care",
"key": "728_CR289",
"unstructured": "Kaushal K, et al. Serum ferritin as a predictive biomarker in COVID-19. A systematic review, meta-analysis and meta-regression analysis. J Crit Care. 2022;67:172–81.",
"volume": "67",
"year": "2022"
},
{
"DOI": "10.12659/MSM.926178",
"author": "C Zhou",
"doi-asserted-by": "publisher",
"first-page": "e926178",
"journal-title": "Med Sci Monitor",
"key": "728_CR290",
"unstructured": "Zhou C, et al. Increased serum levels of hepcidin and ferritin are associated with severity of COVID-19. Med Sci Monitor. 2020;26:e926178–81.",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1007/s10238-022-00851-y",
"doi-asserted-by": "crossref",
"key": "728_CR291",
"unstructured": "Suriawinata E, Mehta KJ. Iron and iron-related proteins in COVID-19. Clin Exp Med. 2022:1–23."
},
{
"DOI": "10.1177/1073858420941476",
"author": "D Kempuraj",
"doi-asserted-by": "publisher",
"first-page": "402",
"issue": "5–6",
"journal-title": "Neuroscientist",
"key": "728_CR292",
"unstructured": "Kempuraj D, et al. COVID-19, mast cells, cytokine storm, psychological stress, and neuroinflammation. Neuroscientist. 2020;26(5–6):402–14.",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1098/rsob.200160",
"author": "A Fara",
"doi-asserted-by": "publisher",
"first-page": "200160",
"issue": "9",
"journal-title": "Open Biol",
"key": "728_CR293",
"unstructured": "Fara A, et al. Cytokine storm and COVID-19: a chronicle of pro-inflammatory cytokines. Open Biol. 2020;10(9):200160.",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1080/14787210.2021.1915129",
"author": "SR Savla",
"doi-asserted-by": "publisher",
"first-page": "1397",
"issue": "11",
"journal-title": "Expert Rev Anti Infect Ther",
"key": "728_CR294",
"unstructured": "Savla SR, Prabhavalkar KS, Bhatt LK. Cytokine storm associated coagulation complications in COVID-19 patients: pathogenesis and management. Expert Rev Anti Infect Ther. 2021;19(11):1397–413.",
"volume": "19",
"year": "2021"
},
{
"DOI": "10.1016/j.bjid.2021.101569",
"doi-asserted-by": "crossref",
"key": "728_CR295",
"unstructured": "Lino K et al. Serum ferritin at admission in hospitalized COVID-19 patients as a predictor of mortality. Brazilian J Infect Dis. 2021;25."
},
{
"DOI": "10.1002/jcla.23618",
"author": "L Cheng",
"doi-asserted-by": "publisher",
"first-page": "e23618",
"issue": "10",
"journal-title": "J Clin Lab Anal",
"key": "728_CR296",
"unstructured": "Cheng L, et al. Ferritin in the coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. J Clin Lab Anal. 2020;34(10):e23618.",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.3389/fmed.2021.745789",
"author": "MM Almutairi",
"doi-asserted-by": "publisher",
"first-page": "745789",
"journal-title": "Front Med",
"key": "728_CR297",
"unstructured": "Almutairi MM, et al. Neuroinflammation and Its Impact on the Pathogenesis of COVID-19. Front Med. 2021;8:745789.",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3390/antiox10010061",
"author": "PJ Urrutia",
"doi-asserted-by": "publisher",
"first-page": "61",
"issue": "1",
"journal-title": "Antioxidants",
"key": "728_CR298",
"unstructured": "Urrutia PJ, Bórquez DA, Núñez MT. Inflaming the Brain with Iron. Antioxidants. 2021;10(1):61.",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1038/nri3863",
"author": "T Ganz",
"doi-asserted-by": "publisher",
"first-page": "500",
"issue": "8",
"journal-title": "Nat Rev Immunol",
"key": "728_CR299",
"unstructured": "Ganz T, Nemeth E. Iron homeostasis in host defence and inflammation. Nat Rev Immunol. 2015;15(8):500–10.",
"volume": "15",
"year": "2015"
},
{
"DOI": "10.1016/j.scib.2021.02.010",
"author": "Q Mu",
"doi-asserted-by": "publisher",
"first-page": "1806",
"issue": "17",
"journal-title": "Science Bulletin",
"key": "728_CR300",
"unstructured": "Mu Q, et al. The role of iron homeostasis in remodeling immune function and regulating inflammatory disease. Science Bulletin. 2021;66(17):1806–16.",
"volume": "66",
"year": "2021"
},
{
"DOI": "10.1128/IAI.00983-13",
"author": "R Rodriguez",
"doi-asserted-by": "publisher",
"first-page": "745",
"issue": "2",
"journal-title": "Infect Immun",
"key": "728_CR301",
"unstructured": "Rodriguez R, et al. Hepcidin induction by pathogens and pathogen-derived molecules is strongly dependent on interleukin-6. Infect Immun. 2014;82(2):745–52.",
"volume": "82",
"year": "2014"
},
{
"DOI": "10.3389/fnmol.2017.00367",
"author": "F-L Zhang",
"doi-asserted-by": "publisher",
"first-page": "367",
"journal-title": "Front Mol Neurosci",
"key": "728_CR302",
"unstructured": "Zhang F-L, et al. Impairment of hepcidin upregulation by lipopolysaccharide in the interleukin-6 knockout mouse brain. Front Mol Neurosci. 2017;10:367.",
"volume": "10",
"year": "2017"
},
{
"DOI": "10.1111/jnc.12244",
"author": "P Urrutia",
"doi-asserted-by": "publisher",
"first-page": "541",
"issue": "4",
"journal-title": "J Neurochem",
"key": "728_CR303",
"unstructured": "Urrutia P, et al. Inflammation alters the expression of DMT1, FPN1 and hepcidin, and it causes iron accumulation in central nervous system cells. J Neurochem. 2013;126(4):541–9.",
"volume": "126",
"year": "2013"
},
{
"DOI": "10.1038/cddis.2017.93",
"author": "L-H You",
"doi-asserted-by": "publisher",
"first-page": "e2676",
"issue": "3",
"journal-title": "Cell Death Dis",
"key": "728_CR304",
"unstructured": "You L-H, et al. Astrocyte hepcidin is a key factor in LPS-induced neuronal apoptosis. Cell Death Dis. 2017;8(3):e2676–e2676.",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.3389/fnins.2018.00740",
"author": "D Vela",
"doi-asserted-by": "publisher",
"first-page": "740",
"journal-title": "Front Neurosci",
"key": "728_CR305",
"unstructured": "Vela D. The dual role of hepcidin in brain iron load and inflammation. Front Neurosci. 2018;12:740.",
"volume": "12",
"year": "2018"
},
{
"DOI": "10.1016/j.neuron.2014.07.027",
"author": "A Kroner",
"doi-asserted-by": "publisher",
"first-page": "1098",
"issue": "5",
"journal-title": "Neuron",
"key": "728_CR306",
"unstructured": "Kroner A, et al. TNF and increased intracellular iron alter macrophage polarization to a detrimental M1 phenotype in the injured spinal cord. Neuron. 2014;83(5):1098–116.",
"volume": "83",
"year": "2014"
},
{
"DOI": "10.1002/glia.20416",
"author": "X Zhang",
"doi-asserted-by": "publisher",
"first-page": "795",
"issue": "8",
"journal-title": "Glia",
"key": "728_CR307",
"unstructured": "Zhang X, et al. Cellular iron status influences the functional relationship between microglia and oligodendrocytes. Glia. 2006;54(8):795–804.",
"volume": "54",
"year": "2006"
},
{
"key": "728_CR308",
"unstructured": "!!! INVALID CITATION !!!"
},
{
"DOI": "10.1016/j.redox.2021.101984",
"author": "Z Feng",
"doi-asserted-by": "publisher",
"first-page": "101984",
"journal-title": "Redox Biol",
"key": "728_CR309",
"unstructured": "Feng Z, et al. Iron overload in the motor cortex induces neuronal ferroptosis following spinal cord injury. Redox Biol. 2021;43:101984.",
"volume": "43",
"year": "2021"
},
{
"DOI": "10.1016/j.cbi.2023.110387",
"author": "M Wang",
"doi-asserted-by": "publisher",
"first-page": "110387",
"journal-title": "Chem Biol Interact",
"key": "728_CR310",
"unstructured": "Wang M, et al. Revisiting the intersection of microglial activation and neuroinflammation in Alzheimer’s disease from the perspective of ferroptosis. Chem Biol Interact. 2023;375:110387.",
"volume": "375",
"year": "2023"
},
{
"DOI": "10.3389/fnins.2019.00114",
"author": "C Liu",
"doi-asserted-by": "publisher",
"first-page": "114",
"journal-title": "Front Neurosci",
"key": "728_CR311",
"unstructured": "Liu C, Liang MC, Soong TW. Nitric oxide, iron and neurodegeneration. Front Neurosci. 2019;13:114.",
"volume": "13",
"year": "2019"
},
{
"DOI": "10.1038/s41589-019-0462-8",
"author": "AA Kapralov",
"doi-asserted-by": "publisher",
"first-page": "278",
"issue": "3",
"journal-title": "Nat Chem Biol",
"key": "728_CR312",
"unstructured": "Kapralov AA, et al. Redox lipid reprogramming commands susceptibility of macrophages and microglia to ferroptotic death. Nat Chem Biol. 2020;16(3):278–90.",
"volume": "16",
"year": "2020"
},
{
"author": "S Ponnappan",
"key": "728_CR313",
"unstructured": "Ponnappan S, Ponnappan U. Aging and immune function: molecular mechanisms to interventions. 2011.",
"volume-title": "Aging and immune function: molecular mechanisms to interventions",
"year": "2011"
},
{
"DOI": "10.2147/CIA.S158513",
"doi-asserted-by": "crossref",
"key": "728_CR314",
"unstructured": "Liguori I et al. Oxidative stress, aging, and diseases. Clin Interv Aging. 2018:757–772."
},
{
"DOI": "10.1155/2016/8426874",
"doi-asserted-by": "crossref",
"key": "728_CR315",
"unstructured": "Xia S et al. An update on inflamm-aging: mechanisms, prevention, and treatment. J Immunol Res. 2016;2016."
},
{
"DOI": "10.3390/cells10123367",
"author": "SM Lynch",
"doi-asserted-by": "publisher",
"first-page": "3367",
"issue": "12",
"journal-title": "Cells",
"key": "728_CR316",
"unstructured": "Lynch SM, et al. Role of senescence and aging in SARS-CoV-2 infection and COVID-19 disease. Cells. 2021;10(12):3367.",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.1093/gerona/glaa149",
"author": "S Salimi",
"doi-asserted-by": "publisher",
"first-page": "e34",
"issue": "9",
"journal-title": "J Gerontol Series A",
"key": "728_CR317",
"unstructured": "Salimi S, Hamlyn JM. COVID-19 and crosstalk with the hallmarks of aging. J Gerontol Series A. 2020;75(9):e34–41.",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1007/s12016-021-08848-3",
"author": "B Oronsky",
"doi-asserted-by": "publisher",
"first-page": "66",
"issue": "1",
"journal-title": "Clin Rev Allergy Immunol",
"key": "728_CR318",
"unstructured": "Oronsky B, et al. A review of persistent post-COVID syndrome (PPCS). Clin Rev Allergy Immunol. 2023;64(1):66–74.",
"volume": "64",
"year": "2023"
},
{
"DOI": "10.1186/s12979-022-00271-2",
"author": "X Jing",
"doi-asserted-by": "publisher",
"first-page": "12",
"issue": "1",
"journal-title": "Immunity Ageing",
"key": "728_CR319",
"unstructured": "Jing X, et al. Association between inflammatory cytokines and anti-SARS-CoV-2 antibodies in hospitalized patients with COVID-19. Immunity Ageing. 2022;19(1):12.",
"volume": "19",
"year": "2022"
},
{
"DOI": "10.1016/j.jns.2021.120023",
"author": "E Normandin",
"doi-asserted-by": "publisher",
"first-page": "120023",
"journal-title": "J Neurol Sci",
"key": "728_CR320",
"unstructured": "Normandin E, et al. Intrathecal inflammatory responses in the absence of SARS-CoV-2 nucleic acid in the CSF of COVID-19 hospitalized patients. J Neurol Sci. 2021;430:120023.",
"volume": "430",
"year": "2021"
},
{
"DOI": "10.7554/eLife.73456",
"author": "T Sato",
"doi-asserted-by": "publisher",
"first-page": "e73456",
"journal-title": "Elife",
"key": "728_CR321",
"unstructured": "Sato T, et al. Aging is associated with increased brain iron through cortex-derived hepcidin expression. Elife. 2022;11:e73456.",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1016/j.mad.2013.11.005",
"author": "SJ Fairweather-Tait",
"doi-asserted-by": "publisher",
"first-page": "22",
"journal-title": "Mech Ageing Dev",
"key": "728_CR322",
"unstructured": "Fairweather-Tait SJ, et al. Iron status in the elderly. Mech Ageing Dev. 2014;136:22–8.",
"volume": "136",
"year": "2014"
},
{
"DOI": "10.1111/cas.14496",
"author": "S Toyokuni",
"doi-asserted-by": "publisher",
"first-page": "2665",
"issue": "8",
"journal-title": "Cancer Sci",
"key": "728_CR323",
"unstructured": "Toyokuni S, et al. Ferroptosis at the crossroads of infection, aging and cancer. Cancer Sci. 2020;111(8):2665–71.",
"volume": "111",
"year": "2020"
},
{
"DOI": "10.1111/acel.13235",
"author": "WD Bao",
"doi-asserted-by": "publisher",
"first-page": "e13235",
"issue": "11",
"journal-title": "Aging Cell",
"key": "728_CR324",
"unstructured": "Bao WD, et al. Targeting miR-124/Ferroportin signaling ameliorated neuronal cell death through inhibiting apoptosis and ferroptosis in aged intracerebral hemorrhage murine model. Aging Cell. 2020;19(11):e13235.",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1038/s41420-021-00553-6",
"author": "M Mazhar",
"doi-asserted-by": "publisher",
"first-page": "149",
"issue": "1",
"journal-title": "Cell Death Discovery",
"key": "728_CR325",
"unstructured": "Mazhar M, et al. Implication of ferroptosis in aging. Cell Death Discovery. 2021;7(1):149.",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.1016/j.biopha.2021.111228",
"author": "HM Habib",
"doi-asserted-by": "publisher",
"first-page": "111228",
"journal-title": "Biomed Pharmacother",
"key": "728_CR326",
"unstructured": "Habib HM, et al. The role of iron in the pathogenesis of COVID-19 and possible treatment with lactoferrin and other iron chelators. Biomed Pharmacother. 2021;136:111228.",
"volume": "136",
"year": "2021"
},
{
"DOI": "10.1016/j.mad.2017.11.012",
"author": "A Sfera",
"doi-asserted-by": "publisher",
"first-page": "63",
"journal-title": "Mech Ageing Dev",
"key": "728_CR327",
"unstructured": "Sfera A, et al. Ferrosenescence: the iron age of neurodegeneration? Mech Ageing Dev. 2018;174:63–75.",
"volume": "174",
"year": "2018"
},
{
"DOI": "10.14336/AD.2020.0601",
"author": "PC Lara",
"doi-asserted-by": "publisher",
"first-page": "756",
"issue": "4",
"journal-title": "Aging Dis",
"key": "728_CR328",
"unstructured": "Lara PC, Macías-Verde D, Burgos-Burgos J. Age-induced NLRP3 inflammasome over-activation increases lethality of SARS-CoV-2 pneumonia in elderly patients. Aging Dis. 2020;11(4):756.",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1002/cam4.1670",
"author": "Y Zhou",
"doi-asserted-by": "publisher",
"first-page": "4012",
"issue": "8",
"journal-title": "Cancer Med",
"key": "728_CR329",
"unstructured": "Zhou Y, et al. Iron overloaded polarizes macrophage to proinflammation phenotype through ROS/acetyl-p53 pathway. Cancer Med. 2018;7(8):4012–22.",
"volume": "7",
"year": "2018"
},
{
"DOI": "10.1038/s41598-022-15812-4",
"author": "M Mezzanotte",
"doi-asserted-by": "publisher",
"first-page": "11724",
"issue": "1",
"journal-title": "Sci Rep",
"key": "728_CR330",
"unstructured": "Mezzanotte M, et al. Activation of the Hepcidin-Ferroportin1 pathway in the brain and astrocytic–neuronal crosstalk to counteract iron dyshomeostasis during aging. Sci Rep. 2022;12(1):11724.",
"volume": "12",
"year": "2022"
},
{
"DOI": "10.1016/S1474-4422(15)70016-5",
"author": "MT Heneka",
"doi-asserted-by": "publisher",
"first-page": "388",
"issue": "4",
"journal-title": "The Lancet Neurology",
"key": "728_CR331",
"unstructured": "Heneka MT, et al. Neuroinflammation in Alzheimer’s disease. The Lancet Neurology. 2015;14(4):388–405.",
"volume": "14",
"year": "2015"
},
{
"DOI": "10.1016/j.nbd.2009.10.006",
"author": "B Cameron",
"doi-asserted-by": "publisher",
"first-page": "503",
"issue": "3",
"journal-title": "Neurobiol Dis",
"key": "728_CR332",
"unstructured": "Cameron B, Landreth GE. Inflammation, microglia, and Alzheimer’s disease. Neurobiol Dis. 2010;37(3):503–9.",
"volume": "37",
"year": "2010"
},
{
"DOI": "10.3390/cells11132091",
"author": "MY Wendimu",
"doi-asserted-by": "publisher",
"first-page": "2091",
"issue": "13",
"journal-title": "Cells",
"key": "728_CR333",
"unstructured": "Wendimu MY, Hooks SB. Microglia phenotypes in aging and neurodegenerative diseases. Cells. 2022;11(13):2091.",
"volume": "11",
"year": "2022"
},
{
"DOI": "10.1038/s41380-019-0375-7",
"author": "S Ayton",
"doi-asserted-by": "publisher",
"first-page": "2932",
"issue": "11",
"journal-title": "Mol Psychiatry",
"key": "728_CR334",
"unstructured": "Ayton S, et al. Brain iron is associated with accelerated cognitive decline in people with Alzheimer pathology. Mol Psychiatry. 2020;25(11):2932–41.",
"volume": "25",
"year": "2020"
},
{
"DOI": "10.3389/fneur.2019.00607",
"author": "W Wan",
"doi-asserted-by": "publisher",
"first-page": "607",
"journal-title": "Front Neurol",
"key": "728_CR335",
"unstructured": "Wan W, et al. Iron deposition leads to hyperphosphorylation of tau and disruption of insulin signaling. Front Neurol. 2019;10:607.",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.2147/JIR.S353467",
"doi-asserted-by": "crossref",
"key": "728_CR336",
"unstructured": "Zhang R et al. COVID-19-related brain injury: the potential role of ferroptosis. J Inflammation Res. 2022: 2181–2198."
},
{
"DOI": "10.3390/antiox10111677",
"author": "AM Fratta Pasini",
"doi-asserted-by": "publisher",
"first-page": "1677",
"issue": "11",
"journal-title": "Antioxidants",
"key": "728_CR337",
"unstructured": "Fratta Pasini AM, et al. Is ferroptosis a key component of the process leading to multiorgan damage in COVID-19? Antioxidants. 2021;10(11):1677.",
"volume": "10",
"year": "2021"
},
{
"DOI": "10.3390/antiox12020326",
"author": "SS Jankauskas",
"doi-asserted-by": "publisher",
"first-page": "326",
"issue": "2",
"journal-title": "Antioxidants",
"key": "728_CR338",
"unstructured": "Jankauskas SS, et al. COVID-19 causes ferroptosis and oxidative stress in human endothelial cells. Antioxidants. 2023;12(2):326.",
"volume": "12",
"year": "2023"
},
{
"author": "H Tu",
"first-page": "1650",
"issue": "3",
"journal-title": "Eur Rev Med Pharmacol Sci",
"key": "728_CR339",
"unstructured": "Tu H, et al. Insights into the novel function of system Xc-in regulated cell death. Eur Rev Med Pharmacol Sci. 2021;25(3):1650–62.",
"volume": "25",
"year": "2021"
},
{
"DOI": "10.1007/s10571-022-01196-6",
"author": "Y Xu",
"doi-asserted-by": "publisher",
"first-page": "205",
"issue": "1",
"journal-title": "Cell Mol Neurobiol",
"key": "728_CR340",
"unstructured": "Xu Y, et al. Role of ferroptosis in stroke. Cell Mol Neurobiol. 2023;43(1):205–22.",
"volume": "43",
"year": "2023"
},
{
"DOI": "10.1016/j.brainres.2020.147216",
"author": "W Chen",
"doi-asserted-by": "publisher",
"first-page": "147216",
"journal-title": "Brain Res",
"key": "728_CR341",
"unstructured": "Chen W, et al. Ferritin reduction is essential for cerebral ischemia-induced hippocampal neuronal death through p53/SLC7A11-mediated ferroptosis. Brain Res. 2021;1752:147216.",
"volume": "1752",
"year": "2021"
},
{
"DOI": "10.1016/j.stemcr.2019.09.002",
"author": "A Cozzi",
"doi-asserted-by": "publisher",
"first-page": "832",
"issue": "5",
"journal-title": "Stem Cell Reports",
"key": "728_CR342",
"unstructured": "Cozzi A, et al. Stem cell modeling of neuroferritinopathy reveals iron as a determinant of senescence and ferroptosis during neuronal aging. Stem Cell Reports. 2019;13(5):832–46.",
"volume": "13",
"year": "2019"
},
{
"DOI": "10.7150/ijbs.53126",
"author": "Y Huang",
"doi-asserted-by": "publisher",
"first-page": "151",
"issue": "1",
"journal-title": "Int J Biol Sci",
"key": "728_CR343",
"unstructured": "Huang Y, et al. Ferroptosis in a sarcopenia model of senescence accelerated mouse prone 8 (SAMP8). Int J Biol Sci. 2021;17(1):151–62.",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.7150/thno.50663",
"author": "RP Zhou",
"doi-asserted-by": "publisher",
"first-page": "11976",
"issue": "26",
"journal-title": "Theranostics",
"key": "728_CR344",
"unstructured": "Zhou RP, et al. Novel insights into ferroptosis: Implications for age-related diseases. Theranostics. 2020;10(26):11976–97.",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1016/j.freeradbiomed.2020.11.019",
"author": "K Han",
"doi-asserted-by": "publisher",
"first-page": "592",
"journal-title": "Free Radical Biol Med",
"key": "728_CR345",
"unstructured": "Han K, et al. Nrf2 knockout altered brain iron deposition and mitigated age-related motor dysfunction in aging mice. Free Radical Biol Med. 2021;162:592–602.",
"volume": "162",
"year": "2021"
},
{
"DOI": "10.1016/j.cell.2016.05.017",
"author": "N Kubben",
"doi-asserted-by": "publisher",
"first-page": "1361",
"issue": "6",
"journal-title": "Cell",
"key": "728_CR346",
"unstructured": "Kubben N, et al. Repression of the antioxidant NRF2 pathway in premature aging. Cell. 2016;165(6):1361–74.",
"volume": "165",
"year": "2016"
},
{
"DOI": "10.1038/s41467-020-18764-3",
"author": "D Olagnier",
"doi-asserted-by": "publisher",
"first-page": "4938",
"issue": "1",
"journal-title": "Nat Commun",
"key": "728_CR347",
"unstructured": "Olagnier D, et al. SARS-CoV2-mediated suppression of NRF2-signaling reveals potent antiviral and anti-inflammatory activity of 4-octyl-itaconate and dimethyl fumarate. Nat Commun. 2020;11(1):4938.",
"volume": "11",
"year": "2020"
},
{
"author": "AM Kyriakopoulos",
"first-page": "e32361",
"issue": "12",
"journal-title": "Cureus",
"key": "728_CR348",
"unstructured": "Kyriakopoulos AM, et al. Mitogen Activated Protein Kinase (MAPK) Activation, p53, and Autophagy Inhibition Characterize the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Spike Protein Induced Neurotoxicity. Cureus. 2022;14(12):e32361.",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1007/s10522-023-10019-0",
"doi-asserted-by": "crossref",
"key": "728_CR349",
"unstructured": "Zhang Y et al. SARS-COV-2 spike protein promotes RPE cell senescence via the ROS/P53/P21 pathway. Biogerontology. 2023."
},
{
"DOI": "10.1016/j.mehy.2020.110102",
"author": "R Cecchini",
"doi-asserted-by": "publisher",
"first-page": "110102",
"journal-title": "Med Hypotheses",
"key": "728_CR350",
"unstructured": "Cecchini R, Cecchini AL. SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression. Med Hypotheses. 2020;143:110102.",
"volume": "143",
"year": "2020"
},
{
"DOI": "10.1016/S0891-5849(99)00258-0",
"author": "MA Lovell",
"doi-asserted-by": "publisher",
"first-page": "418",
"issue": "3",
"journal-title": "Free Radical Biol Med",
"key": "728_CR351",
"unstructured": "Lovell MA, et al. Decreased thioredoxin and increased thioredoxin reductase levels in Alzheimer’s disease brain. Free Radical Biol Med. 2000;28(3):418–27.",
"volume": "28",
"year": "2000"
},
{
"DOI": "10.3174/ajnr.A5143",
"author": "GC Chiang",
"doi-asserted-by": "publisher",
"first-page": "1130",
"issue": "6",
"journal-title": "Am J Neuroradiol",
"key": "728_CR352",
"unstructured": "Chiang GC, et al. Relationships among cortical glutathione levels, brain amyloidosis, and memory in healthy older adults investigated in vivo with 1H-MRS and Pittsburgh compound-B PET. Am J Neuroradiol. 2017;38(6):1130–7.",
"volume": "38",
"year": "2017"
},
{
"DOI": "10.1016/j.freeradbiomed.2022.01.002",
"author": "L Chen",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "Free Radical Biol Med",
"key": "728_CR353",
"unstructured": "Chen L, et al. Enhanced defense against ferroptosis ameliorates cognitive impairment and reduces neurodegeneration in 5xFAD mice. Free Radical Biol Med. 2022;180:1–12.",
"volume": "180",
"year": "2022"
},
{
"DOI": "10.3389/fnagi.2017.00129",
"author": "JL Labandeira-Garcia",
"doi-asserted-by": "publisher",
"first-page": "129",
"journal-title": "Front Aging Neurosci",
"key": "728_CR354",
"unstructured": "Labandeira-Garcia JL, et al. Brain renin-angiotensin system and microglial polarization: implications for aging and neurodegeneration. Front Aging Neurosci. 2017;9:129.",
"volume": "9",
"year": "2017"
},
{
"DOI": "10.1111/acel.13480",
"author": "R Dang",
"doi-asserted-by": "publisher",
"first-page": "e13480",
"issue": "10",
"journal-title": "Aging Cell",
"key": "728_CR355",
"unstructured": "Dang R, et al. Activation of angiotensin-converting enzyme 2/angiotensin (1–7)/mas receptor axis triggers autophagy and suppresses microglia proinflammatory polarization via forkhead box class O1 signaling. Aging Cell. 2021;20(10):e13480.",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1016/j.arr.2008.12.002",
"author": "L-J Min",
"doi-asserted-by": "publisher",
"first-page": "113",
"issue": "2",
"journal-title": "Ageing Res Rev",
"key": "728_CR356",
"unstructured": "Min L-J, et al. Signaling mechanisms of angiotensin II in regulating vascular senescence. Ageing Res Rev. 2009;8(2):113–21.",
"volume": "8",
"year": "2009"
},
{
"DOI": "10.1080/10641963.2023.2180019",
"author": "C Liu",
"doi-asserted-by": "publisher",
"first-page": "2180019",
"issue": "1",
"journal-title": "Clin Exp Hypertens",
"key": "728_CR357",
"unstructured": "Liu C, et al. Angiotensin II-induced vascular endothelial cells ferroptosis via P53-ALOX12 signal axis. Clin Exp Hypertens. 2023;45(1):2180019.",
"volume": "45",
"year": "2023"
},
{
"DOI": "10.1007/s10571-009-9368-4",
"author": "J Benicky",
"doi-asserted-by": "publisher",
"first-page": "781",
"issue": "6",
"journal-title": "Cell Mol Neurobiol",
"key": "728_CR358",
"unstructured": "Benicky J, et al. Anti-Inflammatory Effects of Angiotensin Receptor Blockers in the Brain and the Periphery. Cell Mol Neurobiol. 2009;29(6):781–92.",
"volume": "29",
"year": "2009"
},
{
"DOI": "10.1016/j.regpep.2004.12.027",
"author": "N Basso",
"doi-asserted-by": "publisher",
"first-page": "247",
"issue": "3",
"journal-title": "Regul Pept",
"key": "728_CR359",
"unstructured": "Basso N, et al. Protective effect of the inhibition of the renin–angiotensin system on aging. Regul Pept. 2005;128(3):247–52.",
"volume": "128",
"year": "2005"
},
{
"DOI": "10.1016/j.expneurol.2013.10.013",
"author": "P Garrido-Gil",
"doi-asserted-by": "publisher",
"first-page": "384",
"journal-title": "Exp Neurol",
"key": "728_CR360",
"unstructured": "Garrido-Gil P, et al. Brain angiotensin regulates iron homeostasis in dopaminergic neurons and microglial cells. Exp Neurol. 2013;250:384–96.",
"volume": "250",
"year": "2013"
},
{
"author": "X Feng",
"first-page": "255",
"issue": "2",
"journal-title": "Mol Med Rep",
"key": "728_CR361",
"unstructured": "Feng X, Wang L, Li Y. Change of telomere length in angiotensin II-induced human glomerular mesangial cell senescence and the protective role of losartan. Mol Med Rep. 2011;4(2):255–60.",
"volume": "4",
"year": "2011"
},
{
"DOI": "10.18632/aging.103544",
"author": "R Duan",
"doi-asserted-by": "publisher",
"first-page": "14819",
"issue": "14",
"journal-title": "Aging (Albany NY)",
"key": "728_CR362",
"unstructured": "Duan R, et al. ACE2 activator diminazene aceturate ameliorates Alzheimer’s disease-like neuropathology and rescues cognitive impairment in SAMP8 mice. Aging (Albany NY). 2020;12(14):14819–29.",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3233/JAD-180282",
"author": "NP Rocha",
"doi-asserted-by": "publisher",
"first-page": "1085",
"issue": "4",
"journal-title": "J Alzheimers Dis",
"key": "728_CR363",
"unstructured": "Rocha NP, et al. Cerebrospinal fluid levels of angiotensin-converting enzyme are associated with amyloid-β 42 burden in Alzheimer’s disease. J Alzheimers Dis. 2018;64(4):1085–90.",
"volume": "64",
"year": "2018"
},
{
"DOI": "10.1007/s00401-019-02098-6",
"author": "CE Evans",
"doi-asserted-by": "publisher",
"first-page": "485",
"issue": "3",
"journal-title": "Acta Neuropathol",
"key": "728_CR364",
"unstructured": "Evans CE, et al. ACE2 activation protects against cognitive decline and reduces amyloid pathology in the Tg2576 mouse model of Alzheimer’s disease. Acta Neuropathol. 2020;139(3):485–502.",
"volume": "139",
"year": "2020"
},
{
"DOI": "10.1186/s13195-016-0217-7",
"author": "PG Kehoe",
"doi-asserted-by": "publisher",
"first-page": "50",
"issue": "1",
"journal-title": "Alzheimer's Res Ther",
"key": "728_CR365",
"unstructured": "Kehoe PG, et al. Angiotensin-converting enzyme 2 is reduced in Alzheimer’s disease in association with increasing amyloid-β and tau pathology. Alzheimer’s Res Ther. 2016;8(1):50.",
"volume": "8",
"year": "2016"
},
{
"DOI": "10.1038/npjamd.2016.24",
"author": "X-L Wang",
"doi-asserted-by": "publisher",
"first-page": "16024",
"issue": "1",
"journal-title": "npj Aging Mechanisms Dis",
"key": "728_CR366",
"unstructured": "Wang X-L, et al. Deficiency of angiotensin-converting enzyme 2 causes deterioration of cognitive function. npj Aging Mechanisms Dis. 2016;2(1):16024.",
"volume": "2",
"year": "2016"
},
{
"DOI": "10.1177/0748730420987669",
"author": "S Sengupta",
"doi-asserted-by": "publisher",
"first-page": "23",
"issue": "1",
"journal-title": "J Biol Rhythms",
"key": "728_CR367",
"unstructured": "Sengupta S, et al. Clocks, viruses, and immunity: lessons for the COVID-19 pandemic. J Biol Rhythms. 2021;36(1):23–34.",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.32598/bcn.11.covid19.2584.1",
"author": "A Bakhtazad",
"doi-asserted-by": "publisher",
"first-page": "233",
"issue": "2",
"journal-title": "Basic Clin Neurosci J",
"key": "728_CR368",
"unstructured": "Bakhtazad A, et al. Paying attention to circadian rhythms in the treatment of COVID-19. Basic Clin Neurosci J. 2020;11(2):233–46.",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.33069/cim.2021.0010",
"author": "R Tomar",
"doi-asserted-by": "publisher",
"first-page": "60",
"issue": "2",
"journal-title": "Chronobiol Med",
"key": "728_CR369",
"unstructured": "Tomar R, Raghav A. Association of circadian clock and severe acute respiratory syndrome coronavirus 2 infection. Chronobiol Med. 2021;3(2):60–3.",
"volume": "3",
"year": "2021"
},
{
"DOI": "10.1016/j.isci.2021.103144",
"author": "X Zhuang",
"doi-asserted-by": "publisher",
"first-page": "103144",
"issue": "10",
"journal-title": "IScience",
"key": "728_CR370",
"unstructured": "Zhuang X, et al. The circadian clock component BMAL1 regulates SARS-CoV-2 entry and replication in lung epithelial cells. IScience. 2021;24(10):103144.",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1016/j.micpath.2021.105067",
"author": "AB Diallo",
"doi-asserted-by": "publisher",
"first-page": "105067",
"journal-title": "Microb Pathog",
"key": "728_CR371",
"unstructured": "Diallo AB, et al. Daytime variation in SARS-CoV-2 infection and cytokine production. Microb Pathog. 2021;158:105067.",
"volume": "158",
"year": "2021"
},
{
"DOI": "10.1177/0748730420967768",
"author": "H Borrmann",
"doi-asserted-by": "publisher",
"first-page": "9",
"issue": "1",
"journal-title": "J Biol Rhythms",
"key": "728_CR372",
"unstructured": "Borrmann H, McKeating JA, Zhuang X. The circadian clock and viral infections. J Biol Rhythms. 2021;36(1):9–22.",
"volume": "36",
"year": "2021"
},
{
"DOI": "10.1007/s11033-022-07419-9",
"author": "IC Haskologlu",
"doi-asserted-by": "publisher",
"first-page": "4061",
"issue": "5",
"journal-title": "Mol Biol Rep",
"key": "728_CR373",
"unstructured": "Haskologlu IC, et al. Melatonin and REGN-CoV2 combination as a vaccine adjuvant for Omicron variant of SARS-CoV-2. Mol Biol Rep. 2022;49(5):4061–8.",
"volume": "49",
"year": "2022"
},
{
"DOI": "10.1038/s41418-020-00728-1",
"author": "X Chen",
"doi-asserted-by": "publisher",
"first-page": "1135",
"issue": "4",
"journal-title": "Cell Death Differ",
"key": "728_CR374",
"unstructured": "Chen X, et al. Cellular degradation systems in ferroptosis. Cell Death Differ. 2021;28(4):1135–48.",
"volume": "28",
"year": "2021"
},
{
"DOI": "10.1007/s11357-014-9626-3",
"author": "A Bitto",
"doi-asserted-by": "publisher",
"first-page": "1123",
"issue": "3",
"journal-title": "Age",
"key": "728_CR375",
"unstructured": "Bitto A, et al. p62/SQSTM1 at the interface of aging, autophagy, and disease. Age. 2014;36(3):1123–37.",
"volume": "36",
"year": "2014"
},
{
"DOI": "10.3389/fcell.2022.793328",
"author": "AV Kumar",
"doi-asserted-by": "publisher",
"first-page": "793328",
"journal-title": "Front Cell Dev Biol",
"key": "728_CR376",
"unstructured": "Kumar AV, Mills J, Lapierre LR. Selective autophagy receptor p62/SQSTM1, a pivotal player in stress and aging. Front Cell Dev Biol. 2022;10:793328.",
"volume": "10",
"year": "2022"
},
{
"DOI": "10.1016/j.jbc.2022.101968",
"doi-asserted-by": "crossref",
"key": "728_CR377",
"unstructured": "Liu J et al. Iron accumulation with age alters metabolic pattern and circadian clock gene expression through the reduction of AMP-modulated histone methylation. J Biol Chem. 2022;298(6)."
},
{
"DOI": "10.1038/nrn3208",
"author": "AA Kondratova",
"doi-asserted-by": "publisher",
"first-page": "325",
"issue": "5",
"journal-title": "Nat Rev Neurosci",
"key": "728_CR378",
"unstructured": "Kondratova AA, Kondratov RV. The circadian clock and pathology of the ageing brain. Nat Rev Neurosci. 2012;13(5):325–35.",
"volume": "13",
"year": "2012"
},
{
"DOI": "10.1016/j.pnpbp.2023.110721",
"author": "M Amidfar",
"doi-asserted-by": "publisher",
"journal-title": "Prog Neuropsychopharmacol Biol Psychiatry",
"key": "728_CR379",
"unstructured": "Amidfar M, Garcez ML, Kim Y-K. The shared molecular mechanisms underlying aging of the brain, major depressive disorder, and Alzheimer’s disease: The role of circadian rhythm disturbances. Prog Neuropsychopharmacol Biol Psychiatry. 2023;123: 110721.",
"volume": "123",
"year": "2023"
},
{
"DOI": "10.1101/gad.1432206",
"author": "RV Kondratov",
"doi-asserted-by": "publisher",
"first-page": "1868",
"issue": "14",
"journal-title": "Genes Dev",
"key": "728_CR380",
"unstructured": "Kondratov RV, et al. Early aging and age-related pathologies in mice deficient in BMAL1, the core componentof the circadian clock. Genes Dev. 2006;20(14):1868–73.",
"volume": "20",
"year": "2006"
},
{
"DOI": "10.18632/aging.100764",
"author": "AA Ali",
"doi-asserted-by": "publisher",
"first-page": "435",
"issue": "6",
"journal-title": "Aging (Albany NY)",
"key": "728_CR381",
"unstructured": "Ali AA, et al. Premature aging of the hippocampal neurogenic niche in adult Bmal1-deficient mice. Aging (Albany NY). 2015;7(6):435.",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.3389/fphar.2015.00029",
"doi-asserted-by": "crossref",
"key": "728_CR382",
"unstructured": "Musiek ES. Circadian clock disruption in neurodegenerative diseases: cause and effect? Front Pharmacol. 2015;6."
},
{
"DOI": "10.1096/fj.201901565RR",
"author": "W-W Liu",
"doi-asserted-by": "publisher",
"first-page": "6570",
"issue": "5",
"journal-title": "FASEB J",
"key": "728_CR383",
"unstructured": "Liu W-W, et al. BMAL1 regulation of microglia-mediated neuroinflammation in MPTP-induced Parkinson’s disease mouse model. FASEB J. 2020;34(5):6570–81.",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1186/s12974-019-1562-9",
"author": "J Ni",
"doi-asserted-by": "publisher",
"first-page": "173",
"issue": "1",
"journal-title": "J Neuroinflammation",
"key": "728_CR384",
"unstructured": "Ni J, et al. An impaired intrinsic microglial clock system induces neuroinflammatory alterations in the early stage of amyloid precursor protein knock-in mouse brain. J Neuroinflammation. 2019;16(1):173.",
"volume": "16",
"year": "2019"
},
{
"DOI": "10.1016/j.chembiol.2020.02.005",
"author": "J Liu",
"doi-asserted-by": "publisher",
"first-page": "420",
"issue": "4",
"journal-title": "Cell Chem Biol",
"key": "728_CR385",
"unstructured": "Liu J, et al. Autophagy-dependent ferroptosis: machinery and regulation. Cell Chem Biol. 2020;27(4):420–35.",
"volume": "27",
"year": "2020"
},
{
"DOI": "10.1371/journal.pone.0212138",
"author": "L Hu",
"doi-asserted-by": "publisher",
"first-page": "e0212138",
"issue": "2",
"journal-title": "PLoS ONE",
"key": "728_CR386",
"unstructured": "Hu L, et al. Melatonin decreases M1 polarization via attenuating mitochondrial oxidative damage depending on UCP2 pathway in prorenin-treated microglia. PLoS ONE. 2019;14(2):e0212138.",
"volume": "14",
"year": "2019"
},
{
"DOI": "10.1007/s12035-021-02568-7",
"author": "Q Zhou",
"doi-asserted-by": "publisher",
"first-page": "6552",
"issue": "12",
"journal-title": "Mol Neurobiol",
"key": "728_CR387",
"unstructured": "Zhou Q, et al. Melatonin reduces neuroinflammation and improves axonal hypomyelination by modulating M1/M2 microglia polarization via JAK2-STAT3-telomerase pathway in postnatal rats exposed to lipopolysaccharide. Mol Neurobiol. 2021;58(12):6552–76.",
"volume": "58",
"year": "2021"
},
{
"DOI": "10.3390/ijms22158296",
"author": "R Hardeland",
"doi-asserted-by": "publisher",
"first-page": "8296",
"issue": "15",
"journal-title": "Int J Mol Sci",
"key": "728_CR388",
"unstructured": "Hardeland R. Melatonin and Microglia. Int J Mol Sci. 2021;22(15):8296.",
"volume": "22",
"year": "2021"
},
{
"DOI": "10.1038/s41531-022-00352-5",
"author": "J Li",
"doi-asserted-by": "publisher",
"first-page": "90",
"issue": "1",
"journal-title": "npj Parkinson's Dis",
"key": "728_CR389",
"unstructured": "Li J, et al. Melatonin ameliorates Parkinson’s disease via regulating microglia polarization in a RORα-depend4ent pathway. npj Parkinson’s Dis. 2022;8(1):90.",
"volume": "8",
"year": "2022"
},
{
"DOI": "10.1111/jpi.12194",
"author": "T Ali",
"doi-asserted-by": "publisher",
"first-page": "71",
"issue": "1",
"journal-title": "J Pineal Res",
"key": "728_CR390",
"unstructured": "Ali T, et al. Melatonin attenuates D-galactose-induced memory impairment, neuroinflammation and neurodegeneration via RAGE/NF-KB/JNK signaling pathway in aging mouse model. J Pineal Res. 2015;58(1):71–85.",
"volume": "58",
"year": "2015"
},
{
"DOI": "10.1111/jcmm.17818",
"doi-asserted-by": "crossref",
"key": "728_CR391",
"unstructured": "Dou X et al. Therapeutic potential of melatonin in the intervertebral disc degeneration through inhibiting the ferroptosis of nucleus pulpous cells. J Cell Mol Med. 2023."
},
{
"DOI": "10.1007/s12035-022-02788-5",
"author": "W Qu",
"doi-asserted-by": "publisher",
"first-page": "3124",
"issue": "5",
"journal-title": "Mol Neurobiol",
"key": "728_CR392",
"unstructured": "Qu W, et al. Targeting iNOS alleviates early brain injury after experimental subarachnoid hemorrhage via promoting ferroptosis of M1 microglia and reducing neuroinflammation. Mol Neurobiol. 2022;59(5):3124–39.",
"volume": "59",
"year": "2022"
},
{
"DOI": "10.1034/j.1600-079X.2003.00042.x",
"author": "İ Gulcin",
"doi-asserted-by": "publisher",
"first-page": "278",
"issue": "4",
"journal-title": "J Pineal Res",
"key": "728_CR393",
"unstructured": "Gulcin İ, Buyukokuroglu ME, Kufrevioglu OI. Metal chelating and hydrogen peroxide scavenging effects of melatonin. J Pineal Res. 2003;34(4):278–81.",
"volume": "34",
"year": "2003"
},
{
"DOI": "10.1111/j.1600-079X.1998.tb00361.x",
"author": "J Limson",
"doi-asserted-by": "publisher",
"first-page": "15",
"issue": "1",
"journal-title": "J Pineal Res",
"key": "728_CR394",
"unstructured": "Limson J, Nyokong T, Daya S. The interaction of melatonin and its precursors with aluminium, cadmium, copper, iron, lead, and zinc: an adsorptive voltammetric study. J Pineal Res. 1998;24(1):15–21.",
"volume": "24",
"year": "1998"
},
{
"DOI": "10.1111/jpi.12132",
"author": "A Romero",
"doi-asserted-by": "publisher",
"first-page": "343",
"issue": "4",
"journal-title": "J Pineal Res",
"key": "728_CR395",
"unstructured": "Romero A, et al. A review of metal-catalyzed molecular damage: protection by melatonin. J Pineal Res. 2014;56(4):343–70.",
"volume": "56",
"year": "2014"
},
{
"DOI": "10.1016/j.neulet.2004.02.024",
"author": "CL Hayter",
"doi-asserted-by": "publisher",
"first-page": "182",
"issue": "3",
"journal-title": "Neurosci Lett",
"key": "728_CR396",
"unstructured": "Hayter CL, Bishop GM, Robinson SR. Pharmacological but not physiological concentrations of melatonin reduce iron-induced neuronal death in rat cerebral cortex. Neurosci Lett. 2004;362(3):182–4.",
"volume": "362",
"year": "2004"
},
{
"DOI": "10.1111/j.1471-4159.2005.03532.x",
"author": "DS Maharaj",
"doi-asserted-by": "publisher",
"first-page": "78",
"issue": "1",
"journal-title": "J Neurochem",
"key": "728_CR397",
"unstructured": "Maharaj DS, et al. Melatonin and 6-hydroxymelatonin protect against iron-induced neurotoxicity. J Neurochem. 2006;96(1):78–81.",
"volume": "96",
"year": "2006"
},
{
"DOI": "10.1034/j.1600-079X.2003.02934.x",
"author": "E Kaptanoglu",
"doi-asserted-by": "publisher",
"first-page": "32",
"issue": "1",
"journal-title": "J Pineal Res",
"key": "728_CR398",
"unstructured": "Kaptanoglu E, et al. Different responsiveness of central nervous system tissues to oxidative conditions and to the antioxidant effect of melatonin. J Pineal Res. 2003;34(1):32–5.",
"volume": "34",
"year": "2003"
},
{
"DOI": "10.1016/S0891-5849(00)00169-6",
"author": "AM-Y Lin",
"doi-asserted-by": "publisher",
"first-page": "904",
"issue": "6",
"journal-title": "Free Radical Biol Med",
"key": "728_CR399",
"unstructured": "Lin AM-Y, Ho L-T. Melatonin suppresses iron-induced neurodegeneration in rat brain. Free Radical Biol Med. 2000;28(6):904–11.",
"volume": "28",
"year": "2000"
},
{
"DOI": "10.1016/S0304-3940(01)02530-7",
"author": "S Ortega-Gutiérrez",
"doi-asserted-by": "publisher",
"first-page": "55",
"issue": "1",
"journal-title": "Neurosci Lett",
"key": "728_CR400",
"unstructured": "Ortega-Gutiérrez S, et al. Melatonin improves deferoxamine antioxidant activity in protecting against lipid peroxidation caused by hydrogen peroxide in rat brain homogenates. Neurosci Lett. 2002;323(1):55–9.",
"volume": "323",
"year": "2002"
},
{
"DOI": "10.1016/j.biopha.2022.114048",
"author": "Y Mi",
"doi-asserted-by": "publisher",
"first-page": "114048",
"journal-title": "Biomed Pharmacother",
"key": "728_CR401",
"unstructured": "Mi Y, et al. Melatonin inhibits ferroptosis and delays age-related cataract by regulating SIRT6/p-Nrf2/GPX4 and SIRT6/NCOA4/FTH1 pathways. Biomed Pharmacother. 2023;157:114048.",
"volume": "157",
"year": "2023"
},
{
"DOI": "10.1016/j.freeradbiomed.2023.02.014",
"author": "Y Gao",
"doi-asserted-by": "publisher",
"first-page": "97",
"journal-title": "Free Radical Biol Med",
"key": "728_CR402",
"unstructured": "Gao Y, et al. Melatonin ameliorates neurological deficits through MT2/IL-33/ferritin H signaling-mediated inhibition of neuroinflammation and ferroptosis after traumatic brain injury. Free Radical Biol Med. 2023;199:97–112.",
"volume": "199",
"year": "2023"
},
{
"DOI": "10.3389/fphar.2021.708645",
"author": "X Wang",
"doi-asserted-by": "publisher",
"first-page": "708645",
"journal-title": "Front Pharmacol",
"key": "728_CR403",
"unstructured": "Wang X, et al. Melatonin alleviates acute sleep deprivation-induced memory loss in mice by suppressing hippocampal ferroptosis. Front Pharmacol. 2021;12:708645.",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1016/j.arr.2022.101717",
"author": "J Yang",
"doi-asserted-by": "publisher",
"first-page": "101717",
"journal-title": "Ageing Res Rev",
"key": "728_CR404",
"unstructured": "Yang J, Tang Q, Zeng Y. Melatonin: potential avenue for treating iron overload disorders. Ageing Res Rev. 2022;81:101717.",
"volume": "81",
"year": "2022"
},
{
"DOI": "10.1046/j.1600-079X.2003.00092.x",
"author": "C Rodriguez",
"doi-asserted-by": "publisher",
"first-page": "1",
"issue": "1",
"journal-title": "J Pineal Res",
"key": "728_CR405",
"unstructured": "Rodriguez C, et al. Regulation of antioxidant enzymes: a significant role for melatonin. J Pineal Res. 2004;36(1):1–9.",
"volume": "36",
"year": "2004"
},
{
"DOI": "10.1111/jpi.12360",
"author": "RJ Reiter",
"doi-asserted-by": "publisher",
"first-page": "253",
"issue": "3",
"journal-title": "J Pineal Res",
"key": "728_CR406",
"unstructured": "Reiter RJ, et al. Melatonin as an antioxidant: under promises but over delivers. J Pineal Res. 2016;61(3):253–78.",
"volume": "61",
"year": "2016"
},
{
"DOI": "10.1111/fcp.12498",
"author": "Z Ahmadi",
"doi-asserted-by": "publisher",
"first-page": "11",
"issue": "1",
"journal-title": "Fundam Clin Pharmacol",
"key": "728_CR407",
"unstructured": "Ahmadi Z, Ashrafizadeh M. Melatonin as a potential modulator of Nrf2. Fundam Clin Pharmacol. 2020;34(1):11–9.",
"volume": "34",
"year": "2020"
},
{
"DOI": "10.1016/j.freeradbiomed.2023.09.012",
"author": "S-J Ma",
"doi-asserted-by": "publisher",
"first-page": "555",
"journal-title": "Free Radical Biol Med",
"key": "728_CR408",
"unstructured": "Ma S-J, et al. Melatonin alleviates early brain injury by inhibiting the NRF2-mediated ferroptosis pathway after subarachnoid hemorrhage. Free Radical Biol Med. 2023;208:555–70.",
"volume": "208",
"year": "2023"
},
{
"DOI": "10.1016/j.pnpbp.2023.110777",
"author": "C Ren",
"doi-asserted-by": "publisher",
"first-page": "110777",
"journal-title": "Prog Neuropsychopharmacol Biol Psychiatry",
"key": "728_CR409",
"unstructured": "Ren C, et al. Melatonin reduces radiation-induced ferroptosis in hippocampal neurons by activating the PKM2/NRF2/GPX4 signaling pathway. Prog Neuropsychopharmacol Biol Psychiatry. 2023;126:110777.",
"volume": "126",
"year": "2023"
},
{
"DOI": "10.1016/j.brainresbull.2020.07.011",
"author": "Z Gou",
"doi-asserted-by": "publisher",
"first-page": "40",
"journal-title": "Brain Res Bull",
"key": "728_CR410",
"unstructured": "Gou Z, et al. Melatonin improves hypoxic-ischemic brain damage through the Akt/Nrf2/Gpx4 signaling pathway. Brain Res Bull. 2020;163:40–8.",
"volume": "163",
"year": "2020"
},
{
"DOI": "10.1155/2022/4776243",
"doi-asserted-by": "crossref",
"key": "728_CR411",
"unstructured": "Huang Y-B et al. Melatonin alleviates acute kidney injury by inhibiting NRF2/Slc7a11 axis-mediated ferroptosis. Oxidative Med Cell Longevity. 2022;2022."
},
{
"DOI": "10.1016/j.ecoenv.2021.112588",
"author": "F Guohua",
"doi-asserted-by": "publisher",
"first-page": "112588",
"journal-title": "Ecotoxicol Environ Safety",
"key": "728_CR412",
"unstructured": "Guohua F, et al. Melatonin protects against PM2. 5-induced lung injury by inhibiting ferroptosis of lung epithelial cells in a Nrf2-dependent manner. Ecotoxicol Environ Safety. 2021;223:112588.",
"volume": "223",
"year": "2021"
},
{
"DOI": "10.1155/2020/9067610",
"doi-asserted-by": "crossref",
"key": "728_CR413",
"unstructured": "Ma H et al. Melatonin suppresses ferroptosis induced by high glucose via activation of the Nrf2/HO-1 signaling pathway in type 2 diabetic osteoporosis. Oxidative Med Cell Longevity. 2020;2020."
},
{
"DOI": "10.3390/antiox12061173",
"author": "F Zhang",
"doi-asserted-by": "publisher",
"first-page": "1173",
"issue": "6",
"journal-title": "Antioxidants",
"key": "728_CR414",
"unstructured": "Zhang F, et al. Melatonin alleviates retinal ischemia-reperfusion injury by inhibiting p53–mediated ferroptosis. Antioxidants. 2023;12(6):1173.",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.1016/j.freeradbiomed.2023.06.017",
"doi-asserted-by": "crossref",
"key": "728_CR415",
"unstructured": "Li N et al. PM2. 5 contributed to pulmonary epithelial senescence and ferroptosis by regulating USP3-SIRT3-P53 axis. Free Radical Biol Med. 2023."
},
{
"DOI": "10.1186/s13287-023-03371-y",
"author": "W Li",
"doi-asserted-by": "publisher",
"first-page": "171",
"issue": "1",
"journal-title": "Stem Cell Res Ther",
"key": "728_CR416",
"unstructured": "Li W, et al. Exogenous melatonin ameliorates steroid-induced osteonecrosis of the femoral head by modulating ferroptosis through GDF15-mediated signaling. Stem Cell Res Ther. 2023;14(1):171.",
"volume": "14",
"year": "2023"
},
{
"DOI": "10.1016/j.taap.2022.115902",
"author": "X Sun",
"doi-asserted-by": "publisher",
"first-page": "115902",
"journal-title": "Toxicol Appl Pharmacol",
"key": "728_CR417",
"unstructured": "Sun X, et al. Melatonin alleviates doxorubicin-induced mitochondrial oxidative damage and ferroptosis in cardiomyocytes by regulating YAP expression. Toxicol Appl Pharmacol. 2022;437:115902.",
"volume": "437",
"year": "2022"
},
{
"DOI": "10.1016/j.freeradbiomed.2021.12.007",
"author": "C Wu",
"doi-asserted-by": "publisher",
"first-page": "271",
"journal-title": "Free Radical Biol Med",
"key": "728_CR418",
"unstructured": "Wu C, et al. A novel mechanism linking ferroptosis and endoplasmic reticulum stress via the circPtpn14/miR-351-5p/5-LOX signaling in melatonin-mediated treatment of traumatic brain injury. Free Radical Biol Med. 2022;178:271–94.",
"volume": "178",
"year": "2022"
},
{
"DOI": "10.1111/jpi.12148",
"author": "H Li",
"doi-asserted-by": "publisher",
"first-page": "110",
"issue": "1",
"journal-title": "J Pineal Res",
"key": "728_CR419",
"unstructured": "Li H, et al. Alterations in the time course of expression of the Nox family in the brain in a rat experimental cerebral ischemia and reperfusion model: effects of melatonin. J Pineal Res. 2014;57(1):110–9.",
"volume": "57",
"year": "2014"
},
{
"DOI": "10.1016/j.neuro.2016.09.002",
"author": "P Patiño",
"doi-asserted-by": "publisher",
"first-page": "61",
"journal-title": "Neurotoxicology",
"key": "728_CR420",
"unstructured": "Patiño P, et al. Melatonin protects against oxygen and glucose deprivation by decreasing extracellular glutamate and Nox-derived ROS in rat hippocampal slices. Neurotoxicology. 2016;57:61–8.",
"volume": "57",
"year": "2016"
},
{
"DOI": "10.1016/j.brainres.2016.08.045",
"author": "P Jumnongprakhon",
"doi-asserted-by": "publisher",
"first-page": "84",
"journal-title": "Brain Res",
"key": "728_CR421",
"unstructured": "Jumnongprakhon P, et al. Inhibitory effect of melatonin on cerebral endothelial cells dysfunction induced by methamphetamine via NADPH oxidase-2. Brain Res. 2016;1650:84–92.",
"volume": "1650",
"year": "2016"
},
{
"DOI": "10.2174/1574884714666190502151733",
"author": "M Najafi",
"doi-asserted-by": "publisher",
"first-page": "224",
"issue": "3",
"journal-title": "Curr Clin Pharmacol",
"key": "728_CR422",
"unstructured": "Najafi M, et al. Melatonin modulates regulation of NOX2 and NOX4 following irradiation in the lung. Curr Clin Pharmacol. 2019;14(3):224–31.",
"volume": "14",
"year": "2019"
},
{
"DOI": "10.1080/00365513.2023.2175236",
"doi-asserted-by": "crossref",
"key": "728_CR423",
"unstructured": "Yılmaz S, Öner P. Melatonin levels are low in COVID-19 positive patients and these levels are associated with depression, death anxiety and insomnia. Scandinavian J Clin Lab Investig. 2023: 1–9."
},
{
"DOI": "10.1016/j.intimp.2020.107179",
"author": "S Li",
"doi-asserted-by": "publisher",
"first-page": "107179",
"journal-title": "Int Immunopharmacol",
"key": "728_CR424",
"unstructured": "Li S, et al. Ferrostatin-1 alleviates angiotensin II (Ang II)-induced inflammation and ferroptosis in astrocytes. Int Immunopharmacol. 2021;90:107179.",
"volume": "90",
"year": "2021"
},
{
"DOI": "10.1016/j.heliyon.2023.e19149",
"doi-asserted-by": "crossref",
"key": "728_CR425",
"unstructured": "Liu C et al. Paeonol improves angiotensin II-induced cardiac hypertrophy by suppressing ferroptosis. Heliyon. 2023;9(9)."
},
{
"DOI": "10.3892/mmr.2016.5313",
"author": "ZZ Ji",
"doi-asserted-by": "publisher",
"first-page": "920",
"issue": "1",
"journal-title": "Mol Med Rep",
"key": "728_CR426",
"unstructured": "Ji ZZ, Xu YC. Melatonin protects podocytes from angiotensin II-induced injury in an in vitro diabetic nephropathy model. Mol Med Rep. 2016;14(1):920–6.",
"volume": "14",
"year": "2016"
},
{
"DOI": "10.1007/s11010-016-2808-9",
"author": "H Su",
"doi-asserted-by": "publisher",
"first-page": "85",
"journal-title": "Mol Cell Biochem",
"key": "728_CR427",
"unstructured": "Su H, et al. Melatonin attenuates angiotensin II-induced cardiomyocyte hypertrophy through the CyPA/CD147 signaling pathway. Mol Cell Biochem. 2016;422:85–95.",
"volume": "422",
"year": "2016"
},
{
"DOI": "10.18632/oncotarget.15093",
"author": "J Kong",
"doi-asserted-by": "publisher",
"first-page": "14283",
"issue": "9",
"journal-title": "Oncotarget",
"key": "728_CR428",
"unstructured": "Kong J, et al. Melatonin attenuates angiotensin II-induced abdominal aortic aneurysm through the down-regulation of matrix metalloproteinases. Oncotarget. 2017;8(9):14283.",
"volume": "8",
"year": "2017"
},
{
"DOI": "10.18632/aging.202159",
"author": "Y Yang",
"doi-asserted-by": "publisher",
"first-page": "493",
"issue": "1",
"journal-title": "Aging (Albany NY)",
"key": "728_CR429",
"unstructured": "Yang Y, et al. Melatonin alleviates angiotensin-II-induced cardiac hypertrophy via activating MICU1 pathway. Aging (Albany NY). 2021;13(1):493.",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.1016/j.freeradbiomed.2021.11.043",
"author": "L-M Yu",
"doi-asserted-by": "publisher",
"first-page": "202",
"journal-title": "Free Radical Biol Med",
"key": "728_CR430",
"unstructured": "Yu L-M, et al. Activation of PKG-CREB-KLF15 by melatonin attenuates Angiotensin II-induced vulnerability to atrial fibrillation via enhancing branched-chain amino acids catabolism. Free Radical Biol Med. 2022;178:202–14.",
"volume": "178",
"year": "2022"
},
{
"DOI": "10.1002/jbt.23163",
"author": "S Mahalanobish",
"doi-asserted-by": "publisher",
"first-page": "e23163",
"issue": "10",
"journal-title": "J Biochem Mol Toxicol",
"key": "728_CR431",
"unstructured": "Mahalanobish S, et al. Melatonin counteracts necroptosis and pulmonary edema in cadmium-induced chronic lung injury through the inhibition of angiotensin II. J Biochem Mol Toxicol. 2022;36(10):e23163.",
"volume": "36",
"year": "2022"
},
{
"DOI": "10.1021/acs.jafc.2c04337",
"author": "Y Zhao",
"doi-asserted-by": "publisher",
"first-page": "12953",
"issue": "40",
"journal-title": "J Agric Food Chem",
"key": "728_CR432",
"unstructured": "Zhao Y, et al. Melatonin prevents against ethanol-induced liver injury by mitigating ferroptosis via targeting brain and muscle ARNT-like 1 in mice liver and HepG2 cells. J Agric Food Chem. 2022;70(40):12953–67.",
"volume": "70",
"year": "2022"
},
{
"DOI": "10.1155/2022/8099459",
"doi-asserted-by": "crossref",
"key": "728_CR433",
"unstructured": "Fan L et al. Melatonin ameliorates the progression of Alzheimer's disease by inducing TFEB nuclear translocation, promoting mitophagy, and regulating NLRP3 inflammasome activity. BioMed Res Int. 2022. 2022."
},
{
"DOI": "10.3389/fnagi.2021.736026",
"doi-asserted-by": "crossref",
"key": "728_CR434",
"unstructured": "Li T et al. Peripheral clock system abnormalities in patients with Parkinson’s disease. Front Aging Neurosci. 2021;13."
},
{
"DOI": "10.1016/j.biopha.2020.110485",
"author": "D Delgado-Lara",
"doi-asserted-by": "publisher",
"first-page": "110485",
"journal-title": "Biomed Pharmacother",
"key": "728_CR435",
"unstructured": "Delgado-Lara D, et al. Effect of melatonin administration on the PER1 and BMAL1 clock genes in patients with Parkinson’s disease. Biomed Pharmacother. 2020;129:110485.",
"volume": "129",
"year": "2020"
},
{
"DOI": "10.1007/s10522-014-9495-2",
"author": "U Mattam",
"doi-asserted-by": "publisher",
"first-page": "257",
"journal-title": "Biogerontology",
"key": "728_CR436",
"unstructured": "Mattam U, Jagota A. Differential role of melatonin in restoration of age-induced alterations in daily rhythms of expression of various clock genes in suprachiasmatic nucleus of male Wistar rats. Biogerontology. 2014;15:257–68.",
"volume": "15",
"year": "2014"
}
],
"reference-count": 436,
"references-count": 436,
"relation": {},
"resource": {
"primary": {
"URL": "https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-024-00728-6"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Cellular and Molecular Neuroscience",
"Neurology (clinical)",
"Molecular Biology"
],
"subtitle": [],
"title": "Melatonin: a ferroptosis inhibitor with potential therapeutic efficacy for the post-COVID-19 trajectory of accelerated brain aging and neurodegeneration",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1007/springer_crossmark_policy",
"volume": "19"
}